Biomarkers of Venous Thromboembolism Recurrence after Discontinuation of Low Molecular Weight Heparin Treatment for Cancer-Associated Thrombosis (HISPALIS-Study)
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
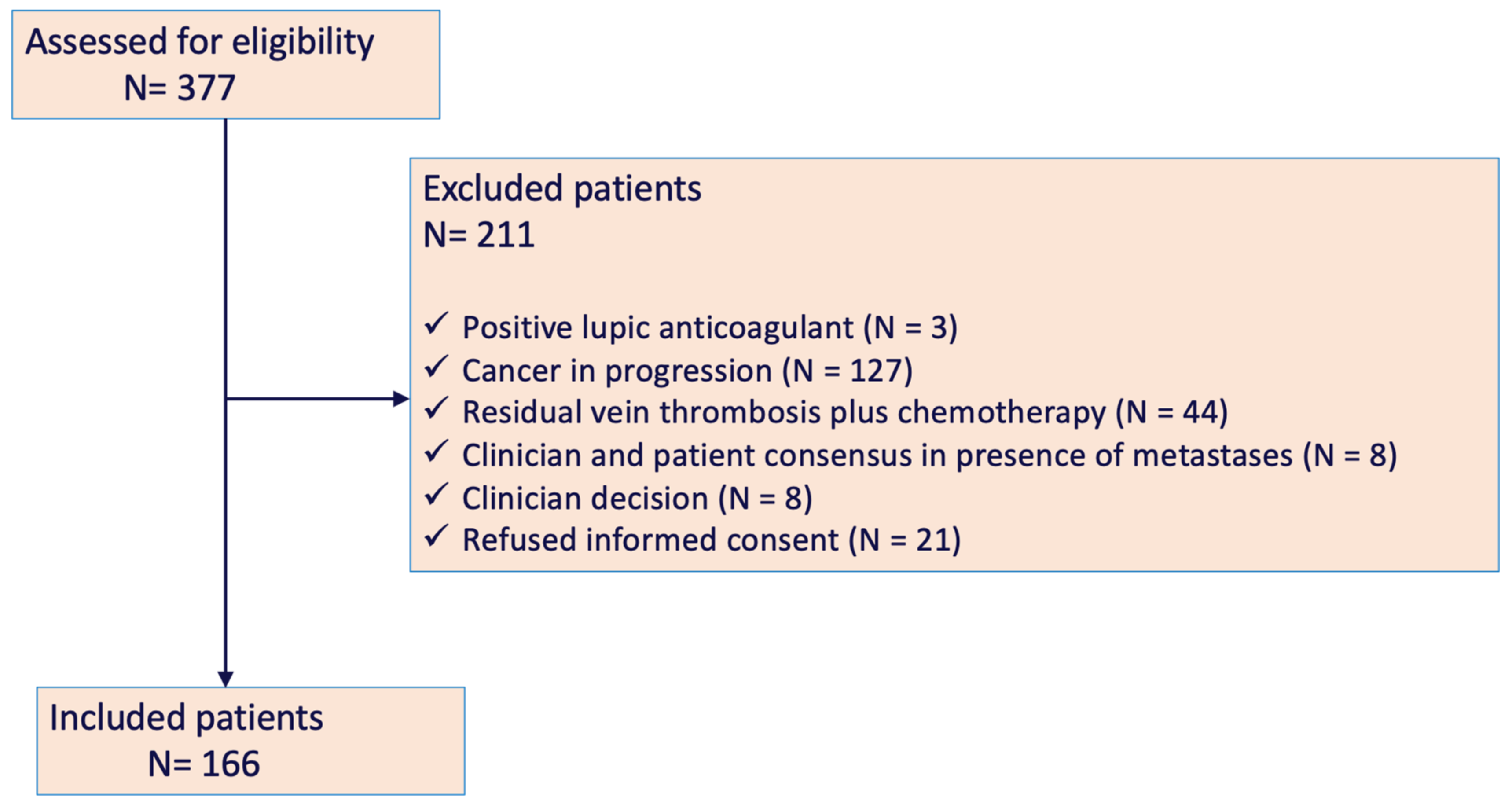
2.2. Patients
2.3. Study Protocol
2.4. Blood Samples and Biomarker Testing
2.5. Study Variables
2.6. Statistical Analysis and Sample Size
3. Results
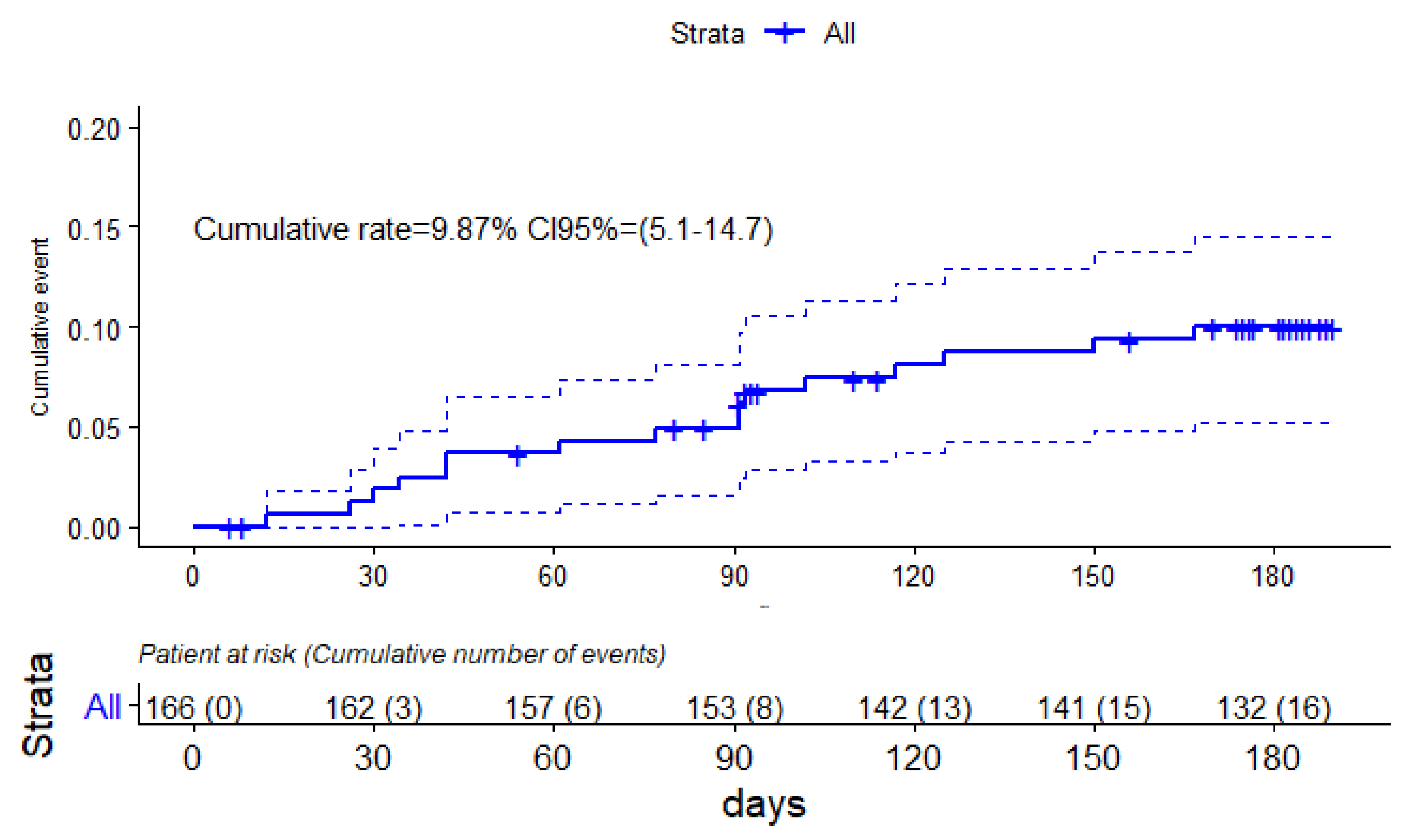
3.1. Incidence of VTE Recurrences after Anticoagulation Withdrawal
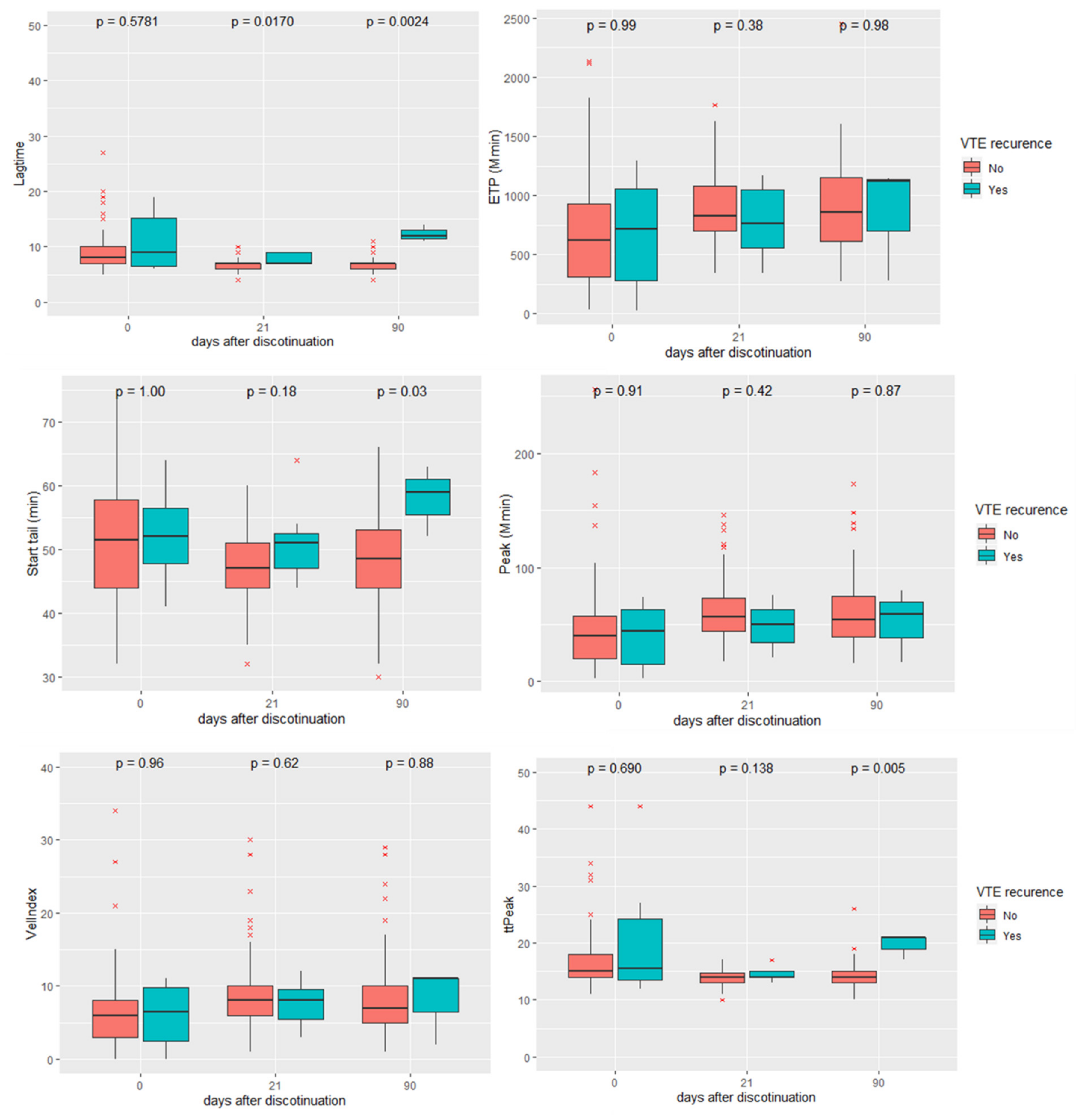
3.2. Evolution of Biomarkers after Anticoagulation Withdrawal
3.3. Predictive Role of Biomarkers in Venous Thromboembolism Recurrence
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Blom, J.W.; Doggen, C.J.M.; Osanto, S.; Rosendaal, F.R. Malignancies, prothrombotic mutations, and the risk of venous thrombosis. JAMA 2005, 293, 715–722. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, H.T.; Mellemkjær, L.; Olsen, J.H.; Baron, J.A. Prognosis of cancers associated with venous thromboembolism. N. Engl. J. Med. 2000, 343, 1846–1850. [Google Scholar] [CrossRef] [PubMed]
- Abdol Razak, N.B.; Jones, G.; Bhandari, M.; Berndt, M.C.; Metharom, P. Cancer-associated thrombosis: An overview of mechanisms, risk factors, and treatment. Cancers 2018, 10, 380. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paneesha, S.; McManus, A.; Arya, R.; Scriven, N.; Farren, T.; Nokes, T.; Bacon, S.; Nieland, A.; Cooper, D.; Smith, H. Frequency, demographics and risk (according to tumour type or site) of cancer-associated thrombosis among patients seen at outpatient DVT clinics. Thromb. Haemost. 2010, 103, 338–343. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chew, H.K.; Wun, T.; Harvey, D.; Zhou, H.; White, R.H. Incidence of Venous Thromboembolism and Its Effect on Survival among Patients With Common Cancers. Arch. Intern. Med. 2006, 166, 458. [Google Scholar] [CrossRef]
- Chee, C.E.; Ashrani, A.A.; Marks, R.S.; Petterson, T.M.; Bailey, K.R.; Melton, L.J., III; Heit, J.A. Predictors of venous thromboembolism recurrence and bleeding among active cancer patients: A population-based cohort study. Blood J. Am. Soc. Hematol. 2014, 123, 3972–3978. [Google Scholar] [CrossRef] [Green Version]
- Khorana, A.A.; Kuderer, N.M.; Culakova, E.; Lyman, G.H.; Francis, C.W. Development and validation of a predictive model for chemotherapy-associated thrombosis. Blood 2008, 111, 4902–4907. [Google Scholar] [CrossRef] [Green Version]
- Patell, R.; Rybicki, L.; McCrae, K.R.; Khorana, A.A. Predicting risk of venous thromboembolism in hospitalized cancer patients: Utility of a risk assessment tool. Am. J. Hematol. 2017, 92, 501–507. [Google Scholar] [CrossRef] [Green Version]
- Kruger, S.; Haas, M.; Burkl, C.; Goehring, P.; Kleespies, A.; Roeder, F.; Gallmeier, E.; Ormanns, S.; Westphalen, C.B.; Heinemann, V. Incidence, outcome and risk stratification tools for venous thromboembolism in advanced pancreatic cancer—A retrospective cohort study. Thromb. Res. 2017, 157, 9–15. [Google Scholar] [CrossRef]
- Muñoz Martín, A.J.; Ortega, I.; Font, C.; Pachón, V.; Castellón, V.; Martínez-Marín, V.; Salgado, M.; Martínez, E.; Calzas, J.; Rupérez, A.; et al. Multivariable clinical-genetic risk model for predicting venous thromboembolic events in patients with cancer. Br. J. Cancer 2018, 118, 1056–1061. [Google Scholar] [CrossRef] [Green Version]
- Fuentes, H.E.; Paz, L.H.; Wang, Y.; Oramas, D.M.; Simons, C.R.; Tafur, A.J. Performance of Current Thromboembolism Risk Assessment Tools in Patients with Gastric Cancer and Validity After First Treatment. Clin. Appl. Thromb. Off. J. Int. Acad. Clin. Appl. Thromb. 2018, 24, 790–796. [Google Scholar] [CrossRef] [Green Version]
- Ay, C.; Dunkler, D.; Marosi, C.; Chiriac, A.-L.; Vormittag, R.; Simanek, R.; Quehenberger, P.; Zielinski, C.; Pabinger, I. Prediction of venous thromboembolism in cancer patients. Blood J. Am. Soc. Hematol. 2010, 116, 5377–5382. [Google Scholar] [CrossRef]
- Tafur, A.J.; Caprini, J.A.; Cote, L.; Trujillo-Santos, J.; Del Toro, J.; Garcia-Bragado, F.; Tolosa, C.; Barillari, G.; Visona, A.; Monreal, M. Predictors of active cancer thromboembolic outcomes. RIETE experience of the Khorana score in cancer-associated thrombosis. Thromb. Haemost. 2017, 117, 1192–1198. [Google Scholar] [CrossRef]
- Van Es, N.; Di Nisio, M.; Cesarman, G.; Kleinjan, A.; Otten, H.-M.; Mahé, I.; Wilts, I.T.; Twint, D.C.; Porreca, E.; Arrieta, O.; et al. Comparison of risk prediction scores for venous thromboembolism in cancer patients: A prospective cohort study. Haematologica 2017, 102, 1494–1501. [Google Scholar] [CrossRef] [Green Version]
- Metcalf, R.L.; Al-Hadithi, E.; Hopley, N.; Henry, T.; Hodgson, C.; McGurk, A.; Mansoor, W.; Hasan, J. Characterisation and risk assessment of venous thromboembolism in gastrointestinal cancers. World J. Gastrointest. Oncol. 2017, 9, 363–371. [Google Scholar] [CrossRef]
- Khorana, A.A.; Francis, C.W. Risk prediction of cancer-associated thrombosis: Appraising the first decade and developing the future. Thromb. Res. 2018, 164 (Suppl. 1), S70–S76. [Google Scholar] [CrossRef]
- Delluc, A.; Miranda, S.; den Exter, P.; Louzada, M.; Alatri, A.; Ahn, S.; Monreal, M.; Khorana, A.; Huisman, M.V.; Wells, P.S. Accuracy of the Ottawa score in risk stratification of recurrent venous thromboembolism in patients with cancer-associated venous thromboembolism: A systematic review and meta-analysis. Haematologica 2020, 105, 1436. [Google Scholar] [CrossRef]
- Douketis, J.; Tosetto, A.; Marcucci, M.; Baglin, T.; Cosmi, B.; Cushman, M.; Kyrle, P.; Poli, D.; Tait, R.C.; Iorio, A. Risk of recurrence after venous thromboembolism in men and women: Patient level meta-analysis. BMJ Clin. Res. Ed. 2011, 342, d813. [Google Scholar] [CrossRef] [Green Version]
- Lyman, G.H.; Khorana, A.A.; Falanga, A.; Clarke-Pearson, D.; Flowers, C.; Jahanzeb, M.; Kakkar, A.; Kuderer, N.M.; Levine, M.N.; Liebman, H.; et al. American Society of Clinical Oncology guideline: Recommendations for venous thromboembolism prophylaxis and treatment in patients with cancer. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2007, 25, 5490–5505. [Google Scholar] [CrossRef] [Green Version]
- Watson, H.G.; Keeling, D.M.; Laffan, M.; Tait, R.C.; Makris, M.; British Committee for Standards in Haematology. Guideline on aspects of cancer-related venous thrombosis. Br. J. Haematol. 2015, 170, 640–648. [Google Scholar] [CrossRef]
- Mandala, M.; Falanga, A.; Roila, F. Management of venous thromboembolism (VTE) in cancer patients: ESMO Clinical Practice Guidelines. Ann. Oncol. 2011, 22, vi85–vi92. [Google Scholar] [CrossRef]
- Kearon, C.; Akl, E.A.; Ornelas, J.; Blaivas, A.; Jimenez, D.; Bounameaux, H.; Huisman, M.; King, C.S.; Morris, T.A.; Sood, N.; et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest 2016, 149, 315–352. [Google Scholar] [CrossRef]
- Wojtukiewicz, M.Z.; Skalij, P.; Tokajuk, P.; Politynska, B.; Wojtukiewicz, A.M.; Tucker, S.C.; Honn, K.V. Direct Oral Anticoagulants in Cancer Patients. Time for a Change in Paradigm. Cancers 2020, 12, 1144. [Google Scholar] [CrossRef]
- Key, N.S.; Khorana, A.A.; Kuderer, N.M.; Bohlke, K.; Lee, A.Y.Y.; Arcelus, J.I.; Wong, S.L.; Balaban, E.P.; Flowers, C.R.; Francis, C.W.; et al. Venous thromboembolism prophylaxis and treatment in patients with cancer: ASCO clinical practice guideline update. J. Clin. Oncol. 2020, 38, 496–520. [Google Scholar] [CrossRef]
- Farge, D.; Frere, C.; Connors, J.M.; Ay, C.; Khorana, A.A.; Munoz, A.; Brenner, B.; Kakkar, A.; Rafii, H.; Solymoss, S. 2019 international clinical practice guidelines for the treatment and prophylaxis of venous thromboembolism in patients with cancer. Lancet Oncol. 2019, 20, e566–e581. [Google Scholar] [CrossRef] [Green Version]
- Muñoz Martín, A.J.; Gallardo Díaz, E.; García Escobar, I.; Macías Montero, R.; Martínez-Marín, V.; Pachón Olmos, V.; Pérez Segura, P.; Quintanar Verdúguez, T.; Salgado Fernández, M. SEOM clinical guideline of venous thromboembolism (VTE) and cancer (2019). Clin. Transl. Oncol. Off. Publ. Fed. Span. Oncol. Soc. Natl. Cancer Inst. Mex. 2020, 22, 171–186. [Google Scholar] [CrossRef] [Green Version]
- Streiff, M.B.; Holmstrom, B.; Angelini, D.; Ashrani, A.; Elshoury, A.; Fanikos, J.; Fertrin, K.Y.; Fogerty, A.E.; Gao, S.; Goldhaber, S.Z.; et al. Cancer-Associated Venous Thromboembolic Disease (Version 2.2021). J. Natl. Compr. Cancer Netw. 2021, 19, 1181–1201. [Google Scholar] [CrossRef]
- Nishimoto, Y.; Yamashita, Y.; Morimoto, T.; Saga, S.; Amano, H.; Takase, T.; Hiramori, S.; Kim, K.; Oi, M.; Akao, M.; et al. Predictive ability of modified Ottawa score for recurrence in patients with cancer-associated venous thromboembolism: From the COMMAND VTE Registry. Thromb. Res. 2020, 191, 66–75. [Google Scholar] [CrossRef]
- Van Es, N.; Louzada, M.; Carrier, M.; Tagalakis, V.; Gross, P.L.; Shivakumar, S.; Rodger, M.A.; Wells, P.S. Predicting the risk of recurrent venous thromboembolism in patients with cancer: A prospective cohort study. Thromb. Res. 2018, 163, 41–46. [Google Scholar] [CrossRef]
- Yang, M.; Qi, J.; Tang, Y.; Wu, D.; Han, Y. Increased D-dimer predicts the risk of cancer-associated recurrent venous thromboembolism and venous thromboembolism: A systematic review and meta-analysis. Thromb. Res. 2020, 196, 410–413. [Google Scholar] [CrossRef]
- Jara-Palomares, L.; Solier-Lopez, A.; Elias-Hernandez, T.; Asensio-Cruz, M.I.; Blasco-Esquivias, I.; Sanchez-Lopez, V.; de la Borbolla, M.R.; Arellano-Orden, E.; Suarez-Valdivia, L.; Marin-Romero, S. D-dimer and high-sensitivity C-reactive protein levels to predict venous thromboembolism recurrence after discontinuation of anticoagulation for cancer-associated thrombosis. Br. J. Cancer 2018, 119, 915–921. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- André, P. P-selectin in haemostasis. Br. J. Haematol. 2004, 126, 298–306. [Google Scholar] [CrossRef] [PubMed]
- Ay, C.; Simanek, R.; Vormittag, R.; Dunkler, D.; Alguel, G.; Koder, S.; Kornek, G.; Marosi, C.; Wagner, O.; Zielinski, C. High plasma levels of soluble P-selectin are predictive of venous thromboembolism in cancer patients: Results from the Vienna Cancer and Thrombosis Study (CATS). Blood J. Am. Soc. Hematol. 2008, 112, 2703–2708. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Linkins, L.; Takach Lapner, S. Review of D-dimer testing: Good, Bad, and Ugly. Int. J. Lab. Hematol. 2017, 39, 98–103. [Google Scholar] [CrossRef] [Green Version]
- Pulivarthi, S.; Gurram, M.K. Effectiveness of d-dimer as a screening test for venous thromboembolism: An update. N. Am. J. Med. Sci. 2014, 6, 491. [Google Scholar]
- Rauch, U.; Nemerson, Y. Circulating tissue factor and thrombosis. Curr. Opin. Hematol. 2000, 7, 273–277. [Google Scholar] [CrossRef]
- Davila, M.; Amirkhosravi, A.; Coll, E.; Desai, H.; Robles, L.; Colon, J.; Baker, C.H.; Francis, J.L. Tissue factor-bearing microparticles derived from tumor cells: Impact on coagulation activation. J. Thromb. Haemost. 2008, 6, 1517–1524. [Google Scholar] [CrossRef]
- Khorana, A.A.; Kamphuisen, P.W.; Meyer, G.; Bauersachs, R.; Janas, M.S.; Jarner, M.F.; Lee, A.Y.Y. Tissue factor as a predictor of recurrent venous thromboembolism in malignancy: Biomarker analyses of the CATCH trial. J. Clin. Oncol. 2017, 35, 1078–1085. [Google Scholar] [CrossRef]
- Vormittag, R.; Simanek, R.; Ay, C.; Dunkler, D.; Quehenberger, P.; Marosi, C.; Zielinski, C.; Pabinger, I. High factor VIII levels independently predict venous thromboembolism in cancer patients: The cancer and thrombosis study. Arterioscler. Thromb. Vasc. Biol. 2009, 29, 2176–2181. [Google Scholar] [CrossRef] [Green Version]
- Sproston, N.R.; Ashworth, J.J. Role of C-reactive protein at sites of inflammation and infection. Front. Immunol. 2018, 9, 754. [Google Scholar] [CrossRef]
- Folsom, A.R.; Lutsey, P.L.; Astor, B.C.; Cushman, M. C-reactive protein and venous thromboembolism. Thromb. Haemost. 2009, 102, 615–619. [Google Scholar]
- Grimnes, G.; Isaksen, T.; Tichelaar, Y.I.G.V.; Brox, J.; Brækkan, S.K.; Hansen, J.-B. C-reactive protein and risk of venous thromboembolism: Results from a population-based case-crossover study. Haematologica 2018, 103, 1245. [Google Scholar] [CrossRef]
- Vormittag, R.; Vukovich, T.; Schönauer, V.; Lehr, S.; Minar, E.; Bialonczyk, C.; Hirschl, M.; Pabinger, I. Basal high-sensitivity-C-reactive protein levels in patients with spontaneous venous thromboembolism. Thromb. Haemost. 2005, 93, 488–493. [Google Scholar] [CrossRef]
- Lundbech, M.; Krag, A.E.; Christensen, T.D.; Hvas, A.-M. Thrombin generation, thrombin-antithrombin complex, and prothrombin fragment F1+ 2 as biomarkers for hypercoagulability in cancer patients. Thromb. Res. 2020, 186, 80–85. [Google Scholar] [CrossRef]
- Hansen, C.H.; Ritschel, V.; Halvorsen, S.; Andersen, G.Ø.; Bjørnerheim, R.; Eritsland, J.; Arnesen, H.; Seljeflot, I. Markers of thrombin generation are associated with myocardial necrosis and left ventricular impairment in patients with ST-elevation myocardial infarction. Thromb. J. 2015, 13, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Bratseth, V.; Pettersen, A.-Å.; Opstad, T.B.; Arnesen, H.; Seljeflot, I. Markers of hypercoagulability in CAD patients. Effects of single aspirin and clopidogrel treatment. Thromb. J. 2012, 10, 1–8. [Google Scholar] [CrossRef] [Green Version]


| Total N = 166 | VTE Recurrence at 3 Months N = 8 | VTE Recurrence at 6 Months N = 16 | |
|---|---|---|---|
| Sex male, N (%) | 89 (53.6) | 6 (75.0) | 11 (68.8) |
| Age (y), median (IQR) | 64 (17.0) | 64.5 (23.5) | 63.5 (16.0) |
| Weight (Kg), median (IQR) | 71 (20.0) | 82.0 (19.0) | 79.5 (14.0) |
| Cancer location, N (%) | |||
| Gastrointestinal | 35 (21.1) | 0 (0.0) | 1 (6.2) |
| Breast and Ovarian | 30 (18.1) | 1 (12.5) | 3 (18.8) |
| Hematologic | 28 (16.9) | 1 (12.5) | 2 (12.5) |
| Urinary | 26 (15.6) | 1 (12.5) | 3 (18.8) |
| Lung | 19 (11.4) | 3 (37.5) | 5 (31.2) |
| Cerebral | 3 (1.8) | 1 (12.5) | 1 (6.2) |
| Other | 25 (15.1) | 1 (12.5) | 1 (6.2) |
| VTE, N (%) | |||
| DVT | 89 (53.6) | 6 (75.0) | 11 (68.8) |
| PE | 47 (28.3) | 0 (0.0) | 0 (0.0) |
| DVT + PE | 18 (10.8) | 2 (25.0) | 5 (31.2) * |
| Atypical VTE | 12 (7.2) | 0 (0.0) | 0 (0.0) * |
| PT g.20210G>A, N (%) | 6 (5.0) | 0 (0.0) | 1 (10.0) |
| FV Leiden, N (%) | 10 (6.0) | 2 (25.0) | 2 (20.0) |
| Anti-phospholipid antibody, N (%) | 2 (1.7) | 0 (0.0) | 0 (0.0) |
| Situation at anticoagulant therapy discontinuation, N (%) | |||
| ECOG status ≥ 2 | 16 (9.6) | 1 (12.5) | 3 (18.8) |
| Active metastasis | 65 (39.2) | 5 (62.5) | 9 (56.2) |
| Active cancer treatment Hormone therapy Alkylating agents Anti-metabolites Immune checkpoint inhibitors Monoclonal antibodies | 56 (33.7) 20 (12.0) 3 (1.8) 15 (9.0) 5 (3.0) 8 (4.8) | 4 (50.0) 2 (25.0) 1 (12.5) 0 (0.0) 2 (25.0) 0 (0.0) | 9 (56.2) * 3 (18.8) 1 (6.3) 3 (18.8) 2 (12.5) 0 (0.0) |
| CV Catheter | 12 (7.2) | 1 (12.5) | 1 (6.2) |
| Months of anticoagulant treatment, median (IQR) | 10 (11.0) | 18 (15.0) | 12 (13.0) |
| DVT resolution, N (%) | 72/107 (67.2) | 5/8 (62.5) | 9/16 (56.2) |
| PE resolution, N (%) | 53/65 (81.5) | 2/2 (100.0) | 3/5 (60.0) |
| HR | CI 95% | sHR | CI 95% | p | |
|---|---|---|---|---|---|
| hs-CRP > 4.5 mg/L | 5.10 | 1.27–20.39 | 4.77 | 1.26–18.07 | 0.021 |
| Ratio (21-day DD/baseline DD) > 2 | 6.00 | 1.52–23.72 | 6.51 | 1.55–27.25 | 0.010 |
| sP-selectin > 40 ng/dL | 5.72 | 1.51–21.59 | 5.58 | 1.58–19.75 | 0.007 |
| Male sex | 3.58 | 0.89–14.36 | 1.29 | 0.86–15.33 | 0.079 |
| Age (years) | 1.00 | 0.96–1.05 | 1.01 | 0.99–1.04 | 0.760 |
| Active metastasis | 2.94 | 0.75–11.43 | 2.78 | 0.51–14.9 | 0.230 |
| Active treatment | 1.67 | 0.46–5.98 | 1.77 | 0.40–7.77 | 0.450 |
| Sen % | 95% CI | Spec % | 95% CI | PNV % | 95% CI | PPV % | 95% CI | |
|---|---|---|---|---|---|---|---|---|
| DD ratio * > 2 | 62.5 | 35.9–83.7 | 65.3 | 57.1–72.8 | 94.2 | 87.4–97.6 | 16.3 | 8.4–28.1 |
| sP-selectin > 40ng/dL | 76.9 | 45.9–93.8 | 72.5 | 64.1–79.5 | 97.1 | 91.1–99.2 | 20.8 | 11.0–35.4 |
| hs-CRP > 4.5mg/L | 75.0 | 47.4–91.7 | 70.7 | 62.6–77.7 | 96.4 | 90.4–98.8 | 21.4 | 12.0–34.8 |
| All (and) | 43.7 | 20.7–69.4 | 98.0 | 93.8–99.5 | 94.2 | 89.0–97.2 | 70.0 | 35.7–91.9 |
| All (or) | 93.7 | 67.7–99.6 | 36.7 | 29.1–44. | 98.2 | 89.2–99.9 | 13.6 | 8.1–21.8 |
| Modified Ottawa score ≥ 1 (high risk) | 22.7 | 10.31–43.4.1 | 84.0 | 77.2–89.1 | 87.7 | 81.2–92.2 | 17.9 | 7.9–35.6 |
| Modified Ottawa score ≥ 1 (high risk) | 38.9 | 31.3–47.0 | 63.6 | 43.0–80.3 | 13.7 | 8.4–21.7 | 36.4 | 19.7–57.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Otero, R.; Solier-López, A.; Sánchez-López, V.; Oto, J.; Arellano, E.; Marín, S.; Jara-Palomares, L.; Elías, T.; Asencio, M.I.; Blasco-Esquivias, I.; et al. Biomarkers of Venous Thromboembolism Recurrence after Discontinuation of Low Molecular Weight Heparin Treatment for Cancer-Associated Thrombosis (HISPALIS-Study). Cancers 2022, 14, 2771. https://doi.org/10.3390/cancers14112771
Otero R, Solier-López A, Sánchez-López V, Oto J, Arellano E, Marín S, Jara-Palomares L, Elías T, Asencio MI, Blasco-Esquivias I, et al. Biomarkers of Venous Thromboembolism Recurrence after Discontinuation of Low Molecular Weight Heparin Treatment for Cancer-Associated Thrombosis (HISPALIS-Study). Cancers. 2022; 14(11):2771. https://doi.org/10.3390/cancers14112771
Chicago/Turabian StyleOtero, Remedios, Aurora Solier-López, Verónica Sánchez-López, Julia Oto, Elena Arellano, Samira Marín, Luis Jara-Palomares, Teresa Elías, María Isabel Asencio, Isabel Blasco-Esquivias, and et al. 2022. "Biomarkers of Venous Thromboembolism Recurrence after Discontinuation of Low Molecular Weight Heparin Treatment for Cancer-Associated Thrombosis (HISPALIS-Study)" Cancers 14, no. 11: 2771. https://doi.org/10.3390/cancers14112771
APA StyleOtero, R., Solier-López, A., Sánchez-López, V., Oto, J., Arellano, E., Marín, S., Jara-Palomares, L., Elías, T., Asencio, M. I., Blasco-Esquivias, I., Rodríguez de la Borbolla, M., Sánchez-Díaz, J. M., Real-Domínguez, M., García-Cabrera, E., Rodríguez-Martorell, F. J., & Medina, P. (2022). Biomarkers of Venous Thromboembolism Recurrence after Discontinuation of Low Molecular Weight Heparin Treatment for Cancer-Associated Thrombosis (HISPALIS-Study). Cancers, 14(11), 2771. https://doi.org/10.3390/cancers14112771






