Long-Term Cardiovascular Mortality among 80,042 Older Patients with Bladder Cancer
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Study Outcomes
2.3. Statistical Analyses
3. Results
3.1. Patient Characteristics
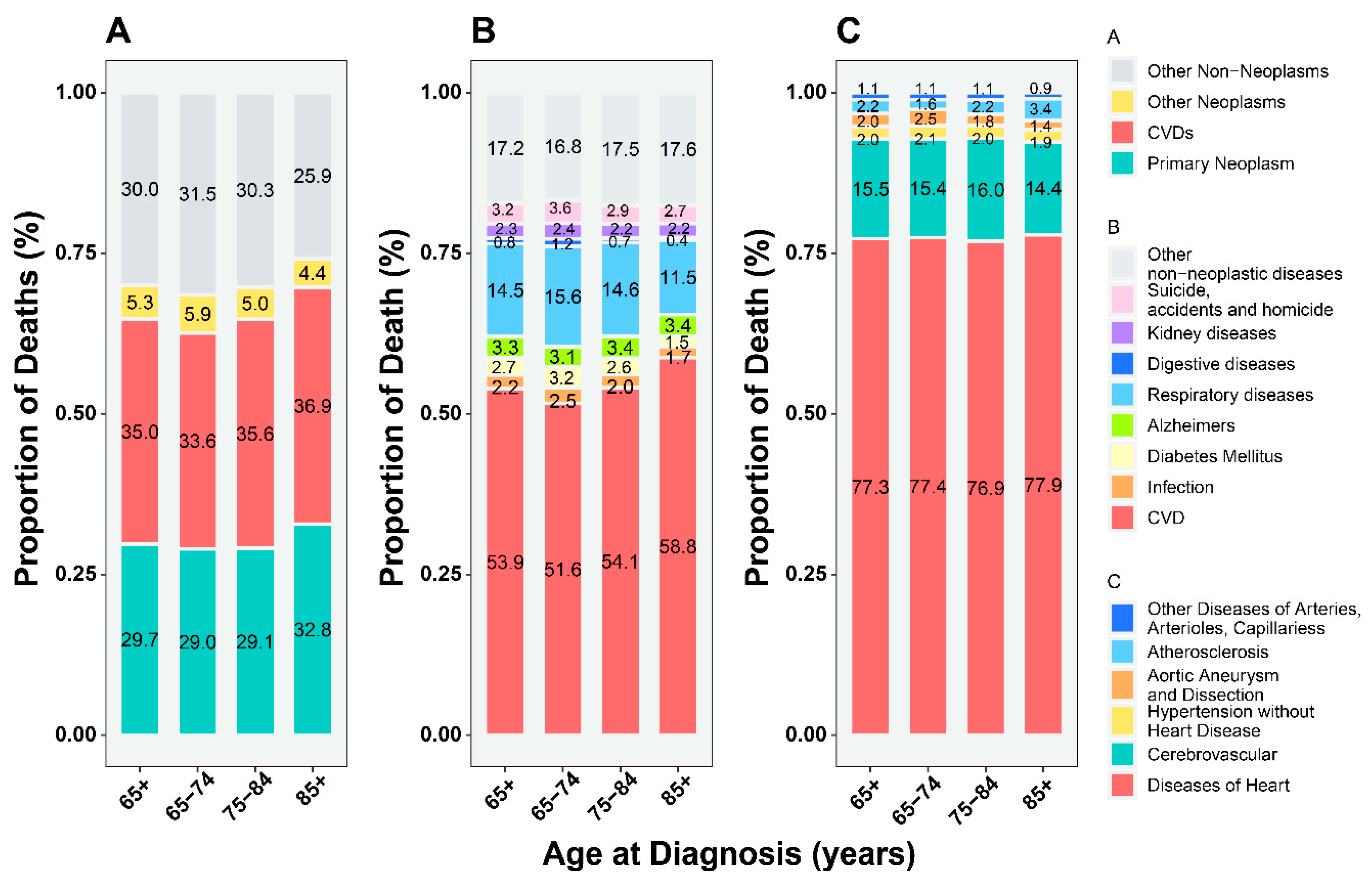
3.2. Proportion of CVD-Related versus Primary Cancer-Related Deaths
3.3. Cumulative Mortality from the CVD versus Primary Cancer
3.4. CVD Mortality Compared to the General Population
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AER | Absolute excess risk |
| BC | Bladder cancer |
| CVD | Cardiovascular disease |
| CI | Confidence interval |
| ESC | The European Society of Cardiology |
| ESMO | The European Society for Medical Oncology |
| SMR | Standardized mortality ratio |
| SEER | Surveillance, Epidemiology, and End Result database |
References
- Babjuk, M.; Burger, M.; Capoun, O.; Cohen, D.; Compérat, E.M.; Dominguez Escrig, J.L.; Gontero, P.; Liedberg, F.; Masson-Lecomte, A.; Mostafid, A.H.; et al. European Association of Urology Guidelines on Non-muscle-invasive Bladder Cancer (Ta, T1, and Carcinoma in Situ). Eur. Urol. 2022, 81, 75–94. [Google Scholar] [CrossRef] [PubMed]
- Sloan, F.A.; Yashkin, A.P.; Akushevich, I.; Inman, B.A. The Cost to Medicare of Bladder Cancer Care. Eur. Urol. Oncol. 2020, 3, 515–522. [Google Scholar] [CrossRef] [PubMed]
- Wong, V.K.; Ganeshan, D.; Jensen, C.T.; Devine, C.E. Imaging and Management of Bladder Cancer. Cancers 2021, 13, 1396. [Google Scholar] [CrossRef] [PubMed]
- Miller, K.D.; Nogueira, L.; Mariotto, A.B.; Rowland, J.H.; Yabroff, K.R.; Alfano, C.M.; Jemal, A.; Kramer, J.L.; Siegel, R.L. Cancer treatment and survivorship statistics, 2019. CA Cancer J. Clin. 2019, 69, 363–385. [Google Scholar] [CrossRef]
- Roth, G.A.; Forouzanfar, M.H.; Moran, A.E.; Barber, R.; Nguyen, G.; Feigin, V.L.; Naghavi, M.; Mensah, G.A.; Murray, C.J. Demographic and epidemiologic drivers of global cardiovascular mortality. N. Engl. J. Med. 2015, 372, 1333–1341. [Google Scholar] [CrossRef]
- Koene, R.J.; Prizment, A.E.; Blaes, A.; Konety, S.H. Shared Risk Factors in Cardiovascular Disease and Cancer. Circulation 2016, 133, 1104–1114. [Google Scholar] [CrossRef]
- Wang, D.Y.; Salem, J.E.; Cohen, J.V.; Chandra, S.; Menzer, C.; Ye, F.; Zhao, S.; Das, S.; Beckermann, K.E.; Ha, L.; et al. Fatal Toxic Effects Associated with Immune Checkpoint Inhibitors: A Systematic Review and Meta-analysis. JAMA Oncol. 2018, 4, 1721–1728. [Google Scholar] [CrossRef]
- Efstathiou, J.A.; Mouw, K.W.; Gibb, E.A.; Liu, Y.; Wu, C.L.; Drumm, M.R.; da Costa, J.B.; du Plessis, M.; Wang, N.Q.; Davicioni, E.; et al. Impact of Immune and Stromal Infiltration on Outcomes Following Bladder-Sparing Trimodality Therapy for Muscle-Invasive Bladder Cancer. Eur. Urol. 2019, 76, 59–68. [Google Scholar] [CrossRef]
- Witjes, J.A.; Bruins, H.M.; Cathomas, R.; Comperat, E.M.; Cowan, N.C.; Gakis, G.; Hernandez, V.; Linares Espinos, E.; Lorch, A.; Neuzillet, Y.; et al. European Association of Urology Guidelines on Muscle-invasive and Metastatic Bladder Cancer: Summary of the 2020 Guidelines. Eur. Urol. 2021, 79, 82–104. [Google Scholar] [CrossRef]
- Babjuk, M.; Burger, M.; Compérat, E.M.; Gontero, P.; Mostafid, A.H.; Palou, J.; van Rhijn, B.W.G.; Rouprêt, M.; Shariat, S.F.; Sylvester, R.; et al. European Association of Urology Guidelines on Non-muscle-invasive Bladder Cancer (TaT1 and Carcinoma In Situ)—2019 Update. Eur. Urol. 2019, 76, 639–657. [Google Scholar] [CrossRef]
- Sturgeon, K.M.; Deng, L.; Bluethmann, S.M.; Zhou, S.; Trifiletti, D.M.; Jiang, C.; Kelly, S.P.; Zaorsky, N.G. A population-based study of cardiovascular disease mortality risk in US cancer patients. Eur. Heart J. 2019, 40, 3889–3897. [Google Scholar] [CrossRef] [PubMed]
- Zaorsky, N.G.; Churilla, T.M.; Egleston, B.L.; Fisher, S.G.; Ridge, J.A.; Horwitz, E.M.; Meyer, J.E. Causes of death among cancer patients. Ann. Oncol. 2017, 28, 400–407. [Google Scholar] [CrossRef] [PubMed]
- Stoltzfus, K.C.; Zhang, Y.; Sturgeon, K.; Sinoway, L.I.; Trifiletti, D.M.; Chinchilli, V.M.; Zaorsky, N.G. Fatal heart disease among cancer patients. Nat. Commun. 2020, 11, 2011. [Google Scholar] [CrossRef] [PubMed]
- Kong, J.; Diao, X.; Diao, F.; Fan, X.; Zheng, J.; Yan, D.; Huang, J.; Qin, H.; Lin, T. Causes of death in long-term bladder cancer survivors: A population-based study. Asia-Pac. J. Clin. Oncol. 2019, 15, e167–e174. [Google Scholar] [CrossRef]
- Scosyrev, E.; Wu, G.; Golijanin, D.; Messing, E. Non-bladder cancer mortality in patients with urothelial cancer of the bladder. Urol. Oncol. 2013, 31, 656–663. [Google Scholar] [CrossRef]
- Noon, A.P.; Albertsen, P.C.; Thomas, F.; Rosario, D.J.; Catto, J.W. Competing mortality in patients diagnosed with bladder cancer: Evidence of undertreatment in the elderly and female patients. Br. J. Cancer 2013, 108, 1534–1540. [Google Scholar] [CrossRef]
- Zhai, M.; Tang, C.; Li, M.; Chen, X.; Jin, Y.; Ying, X.; Tang, Z.; Wang, X.; Wu, Y.; Sun, C.; et al. Short-term mortality risks among patients with non-metastatic bladder cancer. BMC Cancer 2020, 20, 1148. [Google Scholar] [CrossRef]
- National Cancer Institute. About the SEER Program. Available online: https://seer.cancer.gov/about/ (accessed on 16 June 2021).
- Park, H.S.; Lloyd, S.; Decker, R.H.; Wilson, L.D.; Yu, J.B. Overview of the Surveillance, Epidemiology, and End Results database: Evolution, data variables, and quality assurance. Curr. Probl. Cancer 2012, 36, 183–190. [Google Scholar] [CrossRef]
- National Cancer Institute. Casefinding Studies—SEER Quality Improvement. Available online: https://seer.cancer.gov/qi/ (accessed on 16 June 2021).
- Wang, L.; Wang, F.; Chen, L.; Geng, Y.; Yu, S.; Chen, Z. Long-term cardiovascular disease mortality among 160 834 5-year survivors of adolescent and young adult cancer: An American population-based cohort study. Eur. Heart J. 2021, 42, 101–109. [Google Scholar] [CrossRef]
- Chow, R.; Lage, D.E.; Williams, G.R.; Sedrak, M.S.; Greer, J.A.; Temel, J.S.; Nipp, R.D. Representation and Outcomes of Older Adults in Practice-Changing Oncology Trials in the Era of Novel Therapies: A Guideline Appraisal. J. Natl. Compr. Cancer Netw. 2022, 20, 37–44. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention: National Center for Health Statistics. Available online: https://www.cdc.gov/nchs (accessed on 22 August 2022).
- Sung, H.; Hyun, N.; Leach, C.R.; Yabroff, K.R.; Jemal, A. Association of First Primary Cancer with Risk of Subsequent Primary Cancer among Survivors of Adult-Onset Cancers in the United States. JAMA 2020, 324, 2521–2535. [Google Scholar] [CrossRef] [PubMed]
- Feng, W.; Li, Z.; Guo, W.; Fan, X.; Zhou, F.; Zhang, K.; Ou, C.; Huang, F.; Chen, M. Association between Fasting Glucose Variability in Young Adulthood and the Progression of Coronary Artery Calcification in Middle Age. Diabetes Care 2020, 43, 2574–2580. [Google Scholar] [CrossRef] [PubMed]
- Austin, P.C.; Lee, D.S.; Fine, J.P. Introduction to the Analysis of Survival Data in the Presence of Competing Risks. Circulation 2016, 133, 601–609. [Google Scholar] [CrossRef] [PubMed]
- Dores, G.M.; Curtis, R.E.; Dalal, N.H.; Linet, M.S.; Morton, L.M. Cause-Specific Mortality Following Initial Chemotherapy in a Population-Based Cohort of Patients with Classical Hodgkin Lymphoma, 2000–2016. J. Clin. Oncol. 2020, 38, 4149–4162. [Google Scholar] [CrossRef] [PubMed]
- Carioli, G.; Malvezzi, M.; Bertuccio, P.; Hashim, D.; Waxman, S.; Negri, E.; Boffetta, P.; La Vecchia, C. Cancer mortality in the elderly in 11 countries worldwide, 1970–2015. Ann. Oncol. 2019, 30, 1344–1355. [Google Scholar] [CrossRef]
- Fang, F.; Fall, K.; Mittleman, M.A.; Sparén, P.; Ye, W.; Adami, H.O.; Valdimarsdóttir, U. Suicide and cardiovascular death after a cancer diagnosis. N. Engl. J. Med. 2012, 366, 1310–1318. [Google Scholar] [CrossRef]
- Patnaik, J.L.; Byers, T.; DiGuiseppi, C.; Dabelea, D.; Denberg, T.D. Cardiovascular disease competes with breast cancer as the leading cause of death for older females diagnosed with breast cancer: A retrospective cohort study. Breast Cancer Res. 2011, 13, R64. [Google Scholar] [CrossRef]
- Zaorsky, N.G.; Zhang, Y.; Tchelebi, L.T.; Mackley, H.B.; Chinchilli, V.M.; Zacharia, B.E. Stroke among cancer patients. Nat. Commun. 2019, 10, 5172. [Google Scholar] [CrossRef]
- Zhang, H.; Lin, W.; Chen, D.; Wang, K.; Tu, W.; Lin, H.; Li, K.; Ye, S.; Guan, T.; Chen, Y. Cardiovascular and Other Competing Causes of Death in Male Breast Cancer Patients: A Population-Based Epidemiologic Study. Clin. Interv. Aging 2021, 16, 1393–1401. [Google Scholar] [CrossRef]
- Zamorano, J.L.; Lancellotti, P.; Rodriguez Muñoz, D.; Aboyans, V.; Asteggiano, R.; Galderisi, M.; Habib, G.; Lenihan, D.J.; Lip, G.Y.H.; Lyon, A.R.; et al. 2016 ESC Position Paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for Practice Guidelines: The Task Force for cancer treatments and cardiovascular toxicity of the European Society of Cardiology (ESC). Eur. Heart J. 2016, 37, 2768–2801. [Google Scholar] [CrossRef]
- Curigliano, G.; Lenihan, D.; Fradley, M.; Ganatra, S.; Barac, A.; Blaes, A.; Herrmann, J.; Porter, C.; Lyon, A.R.; Lancellotti, P.; et al. Management of cardiac disease in cancer patients throughout oncological treatment: ESMO consensus recommendations. Ann. Oncol. 2020, 31, 171–190. [Google Scholar] [CrossRef]
- Armenian, S.H.; Xu, L.; Ky, B.; Sun, C.; Farol, L.T.; Pal, S.K.; Douglas, P.S.; Bhatia, S.; Chao, C. Cardiovascular Disease among Survivors of Adult-Onset Cancer: A Community-Based Retrospective Cohort Study. J. Clin. Oncol. 2016, 34, 1122–1130. [Google Scholar] [CrossRef] [PubMed]
- Strongman, H.; Gadd, S.; Matthews, A.; Mansfield, K.E.; Stanway, S.; Lyon, A.R.; dos-Santos-Silva, I.; Smeeth, L.; Bhaskaran, K. Medium and long-term risks of specific cardiovascular diseases in survivors of 20 adult cancers: A population-based cohort study using multiple linked UK electronic health records databases. Lancet 2019, 394, 1041–1054. [Google Scholar] [CrossRef]
- Paterson, D.I.; Wiebe, N.; Cheung, W.Y.; Mackey, J.R.; Pituskin, E.; Reiman, A.; Tonelli, M. Incident Cardiovascular Disease among Adults with Cancer: A Population-Based Cohort Study. JACC CardioOncol. 2022, 4, 85–94. [Google Scholar] [CrossRef] [PubMed]
- Schwarzbach, C.J.; Schaefer, A.; Ebert, A.; Held, V.; Bolognese, M.; Kablau, M.; Hennerici, M.G.; Fatar, M. Stroke and cancer: The importance of cancer-associated hypercoagulation as a possible stroke etiology. Stroke 2012, 43, 3029–3034. [Google Scholar] [CrossRef]
- Navi, B.B.; Reiner, A.S.; Kamel, H.; Iadecola, C.; Okin, P.M.; Elkind, M.S.V.; Panageas, K.S.; DeAngelis, L.M. Risk of Arterial Thromboembolism in Patients with Cancer. J. Am. Coll. Cardiol. 2017, 70, 926–938. [Google Scholar] [CrossRef]
- Walker, A.J.; Card, T.R.; West, J.; Crooks, C.; Grainge, M.J. Incidence of venous thromboembolism in patients with cancer—A cohort study using linked United Kingdom databases. Eur. J. Cancer 2013, 49, 1404–1413. [Google Scholar] [CrossRef]
- Cedervall, J.; Herre, M.; Dragomir, A.; Rabelo-Melo, F.; Svensson, A.; Thålin, C.; Rosell, A.; Hjalmar, V.; Wallén, H.; Lindman, H.; et al. Neutrophil extracellular traps promote cancer-associated inflammation and myocardial stress. Oncoimmunology 2022, 11, 2049487. [Google Scholar] [CrossRef]
- Cedervall, J.; Zhang, Y.; Huang, H.; Zhang, L.; Femel, J.; Dimberg, A.; Olsson, A.K. Neutrophil Extracellular Traps Accumulate in Peripheral Blood Vessels and Compromise Organ Function in Tumor-Bearing Animals. Cancer Res. 2015, 75, 2653–2662. [Google Scholar] [CrossRef]
- Döring, Y.; Libby, P.; Soehnlein, O. Neutrophil Extracellular Traps Participate in Cardiovascular Diseases: Recent Experimental and Clinical Insights. Circ. Res. 2020, 126, 1228–1241. [Google Scholar] [CrossRef]
- Khadhouri, S.; Gallagher, K.M.; MacKenzie, K.R.; Shah, T.T.; Gao, C.; Moore, S.; Zimmermann, E.F.; Edison, E.; Jefferies, M.; Nambiar, A.; et al. Developing a Diagnostic Multivariable Prediction Model for Urinary Tract Cancer in Patients Referred with Haematuria: Results from the IDENTIFY Collaborative Study. Eur. Urol. Focus 2022. [Google Scholar] [CrossRef] [PubMed]
- Khadhouri, S.; Gallagher, K.M.; MacKenzie, K.R.; Shah, T.T.; Gao, C.; Moore, S.; Zimmermann, E.F.; Edison, E.; Jefferies, M.; Nambiar, A.; et al. The IDENTIFY study: The investigation and detection of urological neoplasia in patients referred with suspected urinary tract cancer—A multicentre observational study. BJU Int. 2021, 128, 440–450. [Google Scholar] [CrossRef] [PubMed]
- Iseki, K.; Konta, T.; Asahi, K.; Yamagata, K.; Fujimoto, S.; Tsuruya, K.; Narita, I.; Kasahara, M.; Shibagaki, Y.; Moriyama, T.; et al. Higher cardiovascular mortality in men with persistent dipstick hematuria. Clin. Exp. Nephrol. 2021, 25, 150–156. [Google Scholar] [CrossRef]
- Laukhtina, E.; Boehm, A.; Peyronnet, B.; Bravi, C.A.; Batista Da Costa, J.; Soria, F.; D’Andrea, D.; Rajwa, P.; Quhal, F.; Yanagisawa, T.; et al. Urethrectomy at the time of radical cystectomy for non-metastatic urothelial carcinoma of the bladder: A collaborative multicenter study. World J. Urol. 2022, 40, 1689–1696. [Google Scholar] [CrossRef] [PubMed]
- Claps, F.; van de Kamp, M.W.; Mayr, R.; Bostrom, P.J.; Boormans, J.L.; Eckstein, M.; Mertens, L.S.; Boevé, E.R.; Neuzillet, Y.; Burger, M.; et al. Risk factors associated with positive surgical margins’ location at radical cystectomy and their impact on bladder cancer survival. World J. Urol. 2021, 39, 4363–4371. [Google Scholar] [CrossRef]
- Surveillance Research Program, National Cancer Institute. SEER*Stat Software, Version 8.3.9.2. Available online: https://seer.cancer.gov/seerstat/ (accessed on 16 June 2021).



| Age at Diagnosis (n/%) | |||||
|---|---|---|---|---|---|
| Characteristic | Total | 65–74 Years | 75–84 Years | 85+ Years | p Value |
| Overall | 80,042 | 35,841 | 31,676 | 12,525 | |
| Sex | |||||
| Male | 57,634 (72.0) | 26,926 (75.1) | 22,724 (71.7) | 7984 (63.7) | <0.001 |
| Female | 22,408 (28.0) | 8915 (24.9) | 8952 (28.3) | 4541 (36.3) | |
| Race | |||||
| White | 73,151 (91.4) | 32,692 (91.2) | 29,017 (91.6) | 11,442 (91.4) | <0.001 |
| Black | 3320 (4.1) | 1611 (4.5) | 1239 (3.9) | 470 (3.8) | |
| Other * | 3571 (4.5) | 1538 (4.3) | 1420 (4.5) | 613 (4.9) | |
| Stage | |||||
| Localized | 55,374 (69.2) | 25,195 (70.3) | 21,808 (68.8) | 8371 (66.8) | <0.001 |
| Regional | 15,829 (19.8) | 6504 (18.1) | 6519 (20.6) | 2806 (22.4) | |
| Distant | 2702 (3.4) | 1300 (3.6) | 1072 (3.4) | 330 (2.6) | |
| Unknown | 6137 (7.7) | 2842 (7.9) | 2277 (7.2) | 1018 (8.1) | |
| Grade | |||||
| Low | 33,495 (41.8) | 16,072 (44.8) | 12,982 (41.0) | 4441 (35.5) | <0.001 |
| High | 35,222 (44.0) | 14,619 (40.8) | 14,375 (45.4) | 6228 (49.7) | |
| Other # | 50 (0.1) | 14 (0.0) | 23 (0.1) | 13 (0.1) | |
| Unknown | 11,275 (14.1) | 5136 (14.3) | 4296 (13.6) | 1843 (14.7) | |
| Subtype | <0.001 | ||||
| NMIBC | 39,791 (49.7) | 17,670 (49.3) | 15,973 (50.4) | 6148 (49.1) | |
| MMIBC | 12,249 (15.3) | 4793 (13.4) | 5127 (16.2) | 2329 (18.6) | |
| Unknown | 28,002 (35.0) | 13,378 (37.3) | 10,576 (33.4) | 4048 (32.3) | |
| Years of diagnosis | |||||
| 1975–1983 | 12,457 (15.6) | 6027 (16.8) | 4787 (15.1) | 1643 (13.1) | <0.001 |
| 1984–1993 | 16,459 (20.6) | 7902 (22.0) | 6379 (20.1) | 2178 (17.4) | |
| 1994–2003 | 17,991 (22.5) | 7500 (20.9) | 7671 (24.2) | 2820 (22.5) | |
| 2004–2018 | 33,135 (41.4) | 14,412 (40.2) | 12,839 (40.5) | 5884 (47.0) | |
| Surgery | |||||
| Yes | 76,202 (95.2) | 34,192 (95.4) | 30,221 (95.4) | 11,789 (94.1) | <0.001 |
| No | 3445 (4.3) | 1481 (4.1) | 1287 (4.1) | 677 (5.4) | |
| Unknown | 395 (0.5) | 168 (0.5) | 168 (0.5) | 59 (0.5) | |
| Years After Diagnosis | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| <1 | 1–5 | 5–10 | 10–15 | 15+ | ||||||
| Cause of Death | Obs | Smr (95% CI) | Obs | Smr (95% CI) | Obs | Smr (95% CI) | Obs | Smr (95% CI) | Obs | Smr (95% CI) |
| 65+ years | ||||||||||
| CVD | 2686 | 1.57 | 7207 | 1.23 | 5805 | 1.28 | 3244 | 1.3 | 2270 | 1.34 |
| (1.51–1.63) | (1.20–1.26) | (1.25–1.32) | (1.25–1.34) | (1.28–1.39) | ||||||
| Diseases of the Heart | 2124 | 1.62 | 5615 | 1.25 | 4483 | 1.29 | 2472 | 1.29 | 1704 | 1.32 |
| (1.55–1.69) | (1.21–1.28) | (1.25–1.33) | (1.24–1.35) | (1.25–1.38) | ||||||
| Cerebrovascular Diseases | 380 | 1.34 | 1075 | 1.1 | 906 | 1.19 | 523 | 1.22 | 387 | 1.33 |
| (1.21–1.48) | (1.04–1.17) | (1.11–1.27) | (1.12–1.33) | (1.20–1.46) | ||||||
| Hypertension without Heart Disease | 40 | 1.4 | 104 | 1 | 113 | 1.25 | 81 | 1.41 | 86 | 1.82 |
| (1.00–1.90) | (0.82–1.21) | (1.03–1.50) | (1.12–1.76) | (1.46–2.25) | ||||||
| Atherosclerosis | 67 | 1.83 | 161 | 1.34 | 123 | 1.42 | 74 | 1.68 | 40 | 1.46 |
| (1.42–2.32) | (1.14–1.56) | (1.18–1.69) | (1.32–2.11) | (1.05–1.99) | ||||||
| Aortic Aneurysm and Dissection | 46 | 1.55 | 172 | 1.72 | 123 | 1.71 | 53 | 1.49 | 29 | 1.47 |
| (1.14–2.07) | (1.48–2.00) | (1.42–2.04) | (1.12–1.95) | (0.99–2.12) | ||||||
| Other Diseases of the Arteries, Arterioles, and Capillaries | 29 | 1.78 | 80 | 1.44 | 57 | 1.3 | 41 | 1.64 | 24 | 1.38 |
| (1.19–2.56) | (1.14–1.79) | (0.99–1.69) | (1.17–2.22) | (0.89–2.06) | ||||||
| 65–74 years | ||||||||||
| CVD | 632 | 1.94 | 2073 | 1.51 | 2090 | 1.4 | 1628 | 1.19 | 1690 | 1.18 |
| (1.79–2.10) | (1.45–1.58) | (1.34–1.46) | (1.13–1.25) | (1.12–1.24) | ||||||
| Diseases of the Heart | 506 | 1.92 | 1637 | 1.5 | 1652 | 1.42 | 1230 | 1.17 | 1259 | 1.15 |
| (1.76–2.10) | (1.43–1.57) | (1.35–1.49) | (1.11–1.24) | (1.09–1.21) | ||||||
| Cerebrovascular Diseases | 87 | 2.01 | 286 | 1.47 | 297 | 1.25 | 276 | 1.19 | 298 | 1.21 |
| (1.61–2.48) | (1.30–1.65) | (1.11–1.40) | (1.05–1.34) | (1.08–1.36) | ||||||
| Hypertension without Heart Disease | 6 | 1.4 | 23 | 1.19 | 32 | 1.3 | 43 | 1.48 | 62 | 1.56 |
| (0.52–3.06) | (0.76–1.79) | (0.89–1.84) | (1.07–2.00) | (1.20–2.00) | ||||||
| Atherosclerosis | 11 | 2.97 | 34 | 2.01 | 32 | 1.57 | 23 | 1.06 | 27 | 1.19 |
| (1.48–5.32) | (1.39–2.80) | (1.07–2.22) | (0.67–1.59) | (0.78–1.73) | ||||||
| Aortic Aneurysm and Dissection | 10 | 1.22 | 69 | 2.04 | 64 | 1.92 | 35 | 1.52 | 24 | 1.41 |
| (0.59–2.25) | (1.58–2.58) | (1.48–2.45) | (1.06–2.11) | (0.91–2.10) | ||||||
| Other Diseases of the Arteries, Arterioles, and Capillaries | 12 | 3.6 | 24 | 1.71 | 13 | 0.85 | 21 | 1.5 | 20 | 1.36 |
| (1.86–6.30) | (1.10–2.55) | (0.45–1.45) | (0.93–2.29) | (0.83–2.11) | ||||||
| 75–84 years | ||||||||||
| CVD | 1140 | 1.59 | 3179 | 1.08 | 2733 | 1.07 | 1426 | 1.33 | 560 | 2.16 |
| (1.50–1.69) | (1.04–1.12) | (1.03–1.11) | (1.27–1.41) | (1.98–2.35) | ||||||
| Diseases of the Heart | 894 | 1.63 | 2462 | 1.1 | 2077 | 1.07 | 1089 | 1.34 | 429 | 2.18 |
| (1.53–1.74) | (1.05–1.14) | (1.02–1.12) | (1.26–1.42) | (1.98–2.40) | ||||||
| Cerebrovascular Diseases | 169 | 1.37 | 502 | 0.99 | 462 | 1.05 | 223 | 1.21 | 86 | 1.88 |
| (1.17–1.60) | (0.91–1.08) | (0.96–1.16) | (1.06–1.38) | (1.51–2.33) | ||||||
| Hypertension without Heart Disease | 18 | 1.62 | 40 | 0.76 | 61 | 1.12 | 36 | 1.35 | 24 | 3.25 |
| (0.96–2.57) | (0.55–1.04) | (0.85–1.43) | (0.94–1.87) | (2.08–4.84) | ||||||
| Atherosclerosis | 23 | 1.67 | 67 | 1.08 | 56 | 1.02 | 44 | 2.08 | 12 | 2.66 |
| (1.06–2.51) | (0.83–1.37) | (0.77–1.33) | (1.51–2.80) | (1.38–4.65) | ||||||
| Aortic Aneurysm and Dissection | 24 | 1.71 | 70 | 1.44 | 47 | 1.42 | 15 | 1.27 | 5 | 1.88 |
| (1.10–2.55) | (1.12–1.81) | (1.04–1.88) | (0.71–2.09) | (0.61–4.39) | ||||||
| Other Diseases of the Arteries, Arterioles, and Capillaries | 12 | 1.75 | 38 | 1.38 | 30 | 1.26 | 19 | 1.82 | 4 | 1.52 |
| (0.90–3.05) | (0.98–1.90) | (0.85–1.80) | (1.09–2.84) | (0.41–3.89) | ||||||
| 85+ years | ||||||||||
| CVD | 914 | 1.38 | 1955 | 1.27 | 982 | 2.01 | 190 | 3.04 | 20 | 4.39 |
| (1.29–1.47) | (1.21–1.33) | (1.89–2.14) | (2.63–3.51) | (2.68–6.78) | ||||||
| Diseases of the Heart | 724 | 1.45 | 1516 | 1.3 | 754 | 2.04 | 153 | 3.24 | 16 | 4.67 |
| (1.34–1.56) | (1.24–1.37) | (1.89–2.19) | (2.75–3.80) | (2.67–7.59) | ||||||
| Cerebrovascular Diseases | 124 | 1.05 | 287 | 1.06 | 147 | 1.72 | 24 | 2.17 | 3 | 3.63 |
| (0.87–1.25) | (0.94–1.19) | (1.45–2.02) | (1.39–3.23) | (0.75–10.61) | ||||||
| Hypertension without Heart Disease | 16 | 1.21 | 41 | 1.27 | 20 | 1.78 | 2 | 1.24 | 0 | - |
| (0.69–1.96) | (0.91–1.72) | (1.09–2.75) | (0.15–4.49) | - | ||||||
| Atherosclerosis | 33 | 1.72 | 60 | 1.45 | 35 | 3.01 | 7 | 5.45 | 1 | 12.9 |
| (1.19–2.42) | (1.11–1.87) | (2.10–4.19) | (2.19–11.23) | (0.33–71.88) | ||||||
| Aortic Aneurysm and Dissection | 12 | 1.62 | 33 | 1.92 | 12 | 2.28 | 3 | 4.63 | 0 | - |
| (0.84–2.83) | (1.32–2.70) | (1.18–3.98) | (0.96–13.53) | |||||||
| Other Diseases of the Arteries, Arterioles, and Capillaries | 5 | 0.83 | 18 | 1.28 | 14 | 3.09 | 1 | 1.63 | 0 | - |
| (0.27–1.93) | (0.76–2.03) | (1.69–5.18) | (0.04–9.07) | - | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guan, T.; Su, M.; Luo, Z.; Peng, W.; Zhou, R.; Lu, Z.; Feng, M.; Li, W.; Teng, Y.; Jiang, Y.; et al. Long-Term Cardiovascular Mortality among 80,042 Older Patients with Bladder Cancer. Cancers 2022, 14, 4572. https://doi.org/10.3390/cancers14194572
Guan T, Su M, Luo Z, Peng W, Zhou R, Lu Z, Feng M, Li W, Teng Y, Jiang Y, et al. Long-Term Cardiovascular Mortality among 80,042 Older Patients with Bladder Cancer. Cancers. 2022; 14(19):4572. https://doi.org/10.3390/cancers14194572
Chicago/Turabian StyleGuan, Tianwang, Miao Su, Zehao Luo, Weien Peng, Ruoyun Zhou, Zhenxing Lu, Manting Feng, Weirun Li, Yintong Teng, Yanting Jiang, and et al. 2022. "Long-Term Cardiovascular Mortality among 80,042 Older Patients with Bladder Cancer" Cancers 14, no. 19: 4572. https://doi.org/10.3390/cancers14194572
APA StyleGuan, T., Su, M., Luo, Z., Peng, W., Zhou, R., Lu, Z., Feng, M., Li, W., Teng, Y., Jiang, Y., Ou, C., & Chen, M. (2022). Long-Term Cardiovascular Mortality among 80,042 Older Patients with Bladder Cancer. Cancers, 14(19), 4572. https://doi.org/10.3390/cancers14194572






