Development of a Three-Dimensional Multi-Modal Perfusion-Thermal Electrode System for Complete Tumor Eradication
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
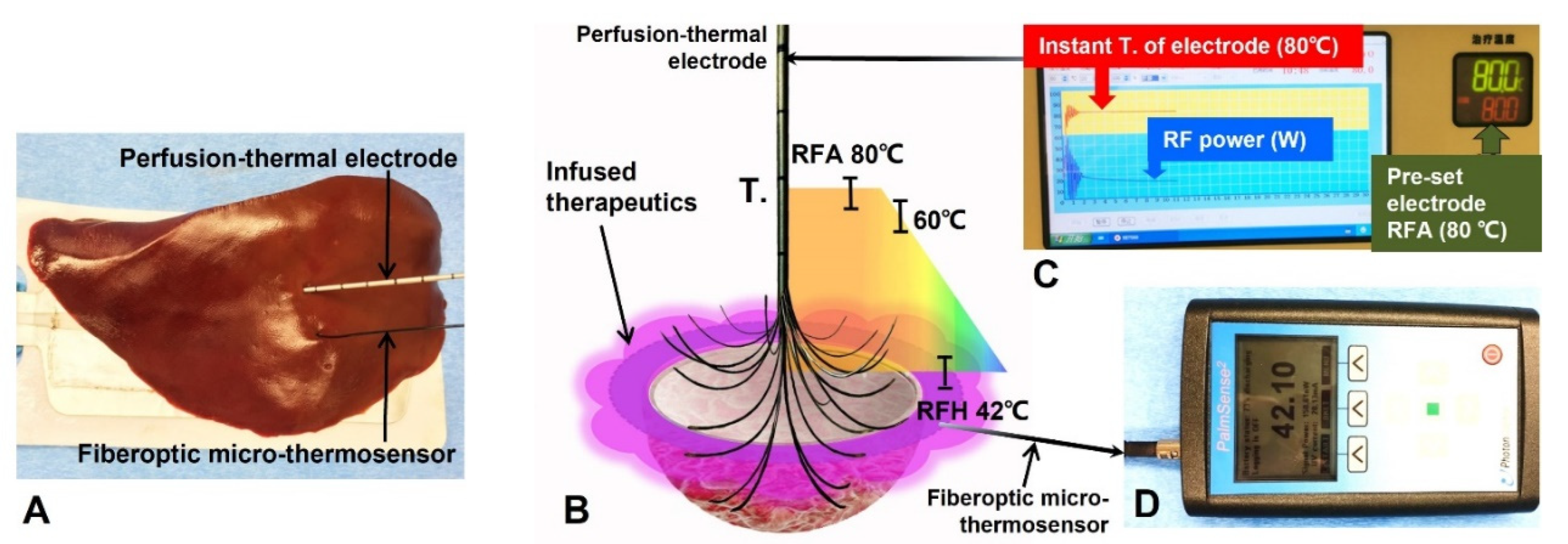
2.2. Design/Production of the 3D/Spherical, Multi-Modal, Perfusion-Thermal Electrode System
2.3. Ex Vivo Evaluation
2.3.1. Evaluating the Function of Peripheral Agent Delivery
2.3.2. Evaluating the Function of Stable RFA/RFH Heat Generation
2.4. In Vivo Validation
2.4.1. Creation of Animal Models with Orthotopic Hepatic Tumors
2.4.2. The Mathematic Modeling and Computer Simulation of the 3D Multi-Modal Electrode Performance
2.4.3. Treatment of VX2 Hepatic Tumors
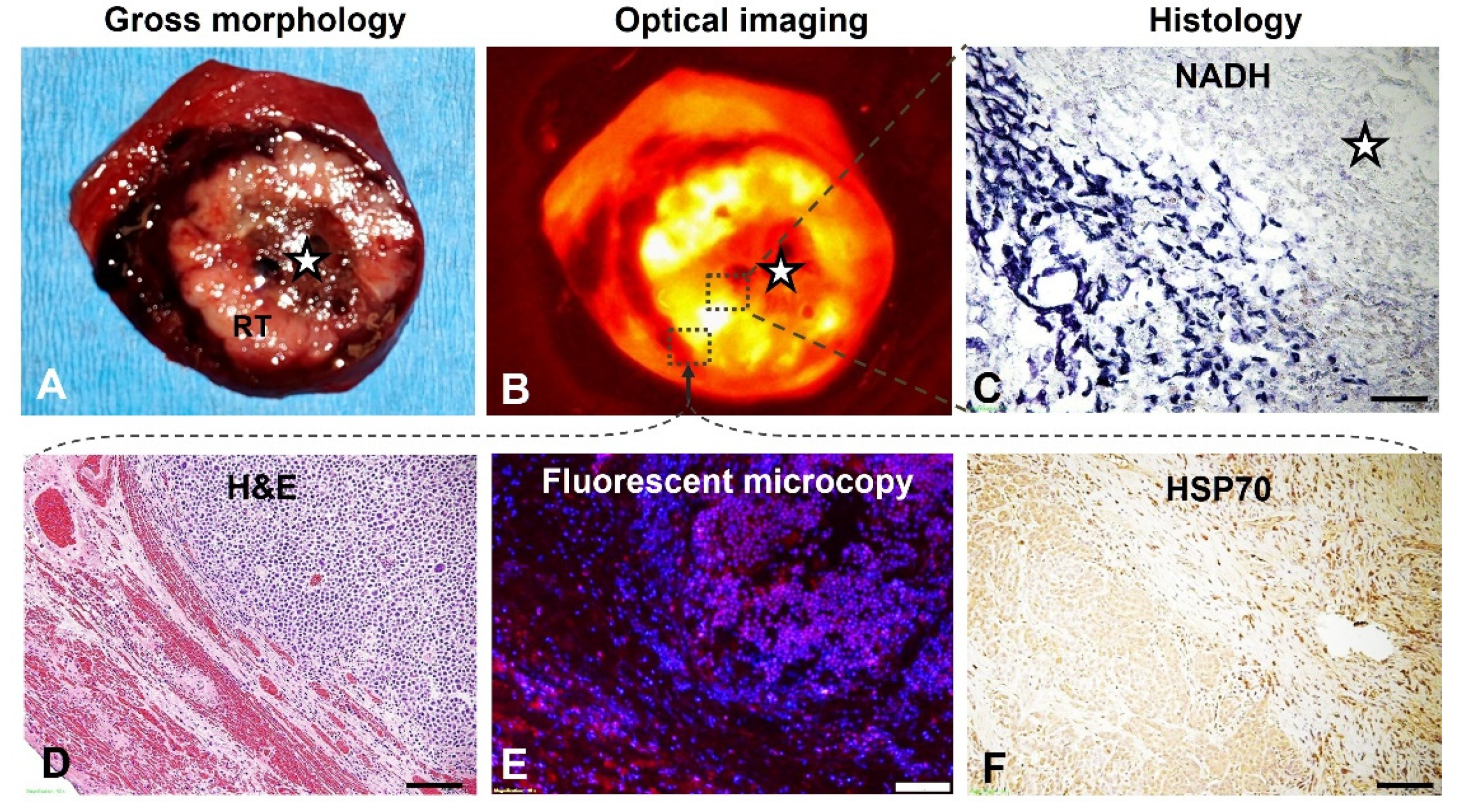
2.5. Optical Imaging of Liver VX2 Tumors
Pathology Correlation/Confirmation
2.6. Statistical Analysis
3. Results
3.1. Ex Vivo Evaluation
3.2. In Vivo Validation
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Takayama, T.; Hasegawa, K.; Izumi, N.; Kudo, M.; Shimada, M.; Yamanaka, N.; Inomata, M.; Kaneko, S.; Nakayama, H.; Kawaguchi, Y.; et al. Surgery versus Radiofrequency Ablation for Small Hepatocellular Carcinoma: A Randomized Controlled Trial (SURF Trial). Liver Cancer 2022, 11, 209–218. [Google Scholar] [CrossRef] [PubMed]
- Deng, Q.; He, M.; Fu, C.; Feng, K.; Ma, K.; Zhang, L. Radiofrequency ablation in the treatment of hepatocellular carcinoma. Int. J. Hyperth. 2022, 39, 1052–1063. [Google Scholar] [CrossRef] [PubMed]
- Shibata, T.; Iimuro, Y.; Yamamoto, Y.; Maetani, Y.; Ametani, F.; Itoh, K.; Konishi, J. Small hepatocellular carcinoma: Comparison of radio-frequency ablation and percutaneous microwave coagulation therapy. Radiology 2002, 223, 331–337. [Google Scholar] [CrossRef] [PubMed]
- Dong, S.C.; Bai, D.S.; Wang, F.A.; Jin, S.J.; Zhang, C.; Zhou, B.H.; Jiang, G.Q. Radiofrequency ablation is an inferior option to liver resection for solitary hepatocellular carcinoma ≤5 cm without cirrhosis: A population-based study with stratification by tumor size. Hepatobiliary Pancreat. Dis. Int. 2022. [Google Scholar] [CrossRef]
- Izzo, F.; Granata, V.; Grassi, R.; Fusco, R.; Palaia, R.; Delrio, P.; Carrafiello, G.; Azoulay, D.; Petrillo, A.; Curley, S.A. Radiofrequency Ablation and Microwave Ablation in Liver Tumors: An Update. Oncologist 2019, 24, e990–e1005. [Google Scholar] [CrossRef]
- Kunzli, B.M.; Abitabile, P.; Maurer, C.A. Radiofrequency ablation of liver tumors: Actual limitations and potential solutions in the future. World J. Hepatol. 2011, 3, 8–14. [Google Scholar] [CrossRef]
- Hwang, J.E.; Kim, S.H.; Jin, J.; Hong, J.Y.; Kim, M.J.; Jung, S.H.; Shim, H.J.; Bae, W.K.; Hwang, E.C.; Kim, J.W.; et al. Combination of percutaneous radiofrequency ablation and systemic chemotherapy are effective treatment modalities for metachronous liver metastases from gastric cancer. Clin. Exp. Metastasis 2014, 31, 25–32. [Google Scholar] [CrossRef]
- Iezzi, R.; Cesario, V.; Siciliani, L.; Campanale, M.; De Gaetano, A.M.; Siciliano, M.; Agnes, S.; Giuliante, F.; Grieco, A.; Pompili, M.; et al. Single-step multimodal locoregional treatment for unresectable hepatocellular carcinoma: Balloon-occluded percutaneous radiofrequency thermal ablation (BO-RFA) plus transcatheter arterial chemoembolization (TACE). Radiol. Med. 2013, 118, 555–569. [Google Scholar] [CrossRef]
- Ji, J.; Weng, Q.; Zhang, F.; Xiong, F.; Jin, Y.; Hui, J.; Song, J.; Gao, J.; Chen, M.; Li, Q.; et al. Non-Small-Cell Lung Cancer: Feasibility of Intratumoral Radiofrequency Hyperthermia-enhanced Herpes Simplex Virus Thymidine Kinase Gene Therapy. Radiology 2018, 288, 612–620. [Google Scholar] [CrossRef]
- Song, J.; Zhang, F.; Ji, J.; Chen, M.; Li, Q.; Weng, Q.; Gu, S.; Kogut, M.J.; Yang, X. Orthotopic hepatocellular carcinoma: Molecular imaging-monitored intratumoral hyperthermia-enhanced direct oncolytic virotherapy. Int. J. Hyperth. 2019, 36, 344–350. [Google Scholar] [CrossRef] [Green Version]
- Zheng, H.; Zhang, F.; Monsky, W.; Ji, H.; Yang, W.; Yang, X. Interventional Optical Imaging-Monitored Synergistic Effect of Radio-Frequency Hyperthermia and Oncolytic Immunotherapy. Front. Oncol. 2021, 11, 821838. [Google Scholar] [CrossRef] [PubMed]
- Ibuki, Y.; Takahashi, Y.; Tamari, K.; Minami, K.; Seo, Y.; Isohashi, F.; Koizumi, M.; Ogawa, K. Local hyperthermia combined with CTLA-4 blockade induces both local and abscopal effects in a murine breast cancer model. Int. J. Hyperth. 2021, 38, 363–371. [Google Scholar] [CrossRef] [PubMed]
- Antanaviciute, I.; Mildaziene, V.; Stankevicius, E.; Herdegen, T.; Skeberdis, V.A. Hyperthermia differently affects connexin43 expression and gap junction permeability in skeletal myoblasts and HeLa cells. Mediat. Inflamm. 2014, 2014, 748290. [Google Scholar] [CrossRef]
- Chu, K.F.; Dupuy, D.E. Thermal ablation of tumours: Biological mechanisms and advances in therapy. Nat. Rev. Cancer 2014, 14, 199–208. [Google Scholar] [CrossRef] [PubMed]
- Wust, P.; Hildebrandt, B.; Sreenivasa, G.; Rau, B.; Gellermann, J.; Riess, H.; Felix, R.; Schlag, P.M. Hyperthermia in combined treatment of cancer. Lancet Oncol. 2002, 3, 487–497. [Google Scholar] [CrossRef]
- Yang, W.; Han, G.H.; Shin, H.Y.; Lee, E.J.; Cho, H.; Chay, D.B.; Kim, J.H. Combined treatment with modulated electro-hyperthermia and an autophagy inhibitor effectively inhibit ovarian and cervical cancer growth. Int. J. Hyperth. 2019, 36, 9–20. [Google Scholar] [CrossRef]
- Qian, K.; Chen, M.; Zhang, F.; Chick, J.F.B.; Ji, H.; Zheng, C.; Yang, X. Image-Guided Radiofrequency Hyperthermia (RFH)-Enhanced Direct Chemotherapy of Hepatic Tumors: The Underlying Biomolecular Mechanisms. Front. Oncol. 2020, 10, 610543. [Google Scholar] [CrossRef]
- Xu, D.; Tang, W.J.; Zhu, Y.Z.; Liu, Z.; Yang, K.; Liang, M.X.; Chen, X.; Wu, Y.; Tang, J.H.; Zhang, W. Hyperthermia promotes exosome secretion by regulating Rab7b while increasing drug sensitivity in adriamycin-resistant breast cancer. Int. J. Hyperth. 2022, 39, 246–257. [Google Scholar] [CrossRef]
- Kan, X.; Zhou, G.; Zhang, F.; Ji, H.; Zheng, H.; Chick, J.F.B.; Valji, K.; Zheng, C.; Yang, X. Interventional Optical Imaging Permits Instant Visualization of Pathological Zones of Ablated Tumor Periphery and Residual Tumor Detection. Cancer Res. 2021, 81, 4594–4602. [Google Scholar] [CrossRef]
- Ni, Y.; Mulier, S.; Miao, Y.; Michel, L.; Marchal, G. A review of the general aspects of radiofrequency ablation. Abdom. Imaging 2005, 30, 381–400. [Google Scholar] [CrossRef] [Green Version]
- McGahan, J.P.; Brock, J.M.; Tesluk, H.; Gu, W.Z.; Schneider, P.; Browning, P.D. Hepatic ablation with use of radio-frequency electrocautery in the animal model. J. Vasc. Interv. Radiol. 1992, 3, 291–297. [Google Scholar] [CrossRef]
- Organ, L.W. Electrophysiologic principles of radiofrequency lesion making. Appl. Neurophysiol. 1976, 39, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Panescu, D.; Whayne, J.G.; Fleischman, S.D.; Mirotznik, M.S.; Swanson, D.K.; Webster, J.G. Three-dimensional finite element analysis of current density and temperature distributions during radio-frequency ablation. IEEE Trans. Biomed. Eng. 1995, 42, 879–890. [Google Scholar] [CrossRef] [PubMed]
- Kan, X.; Zhang, F.; Zhou, G.; Ji, H.; Monsky, W.; Ingraham, C.; Zheng, C.; Yang, X. Interventional real-time optical imaging guidance for complete tumor ablation. Proc. Natl. Acad. Sci. USA 2021, 118, e2113028118. [Google Scholar] [CrossRef]
- Minami, Y.; Kudo, M. Radiofrequency ablation of hepatocellular carcinoma: A literature review. Int. J. Hepatol. 2011, 2011, 104685. [Google Scholar] [CrossRef]
- Zhang, C.; Gao, R.; Guo, S.; Ning, C.; Li, A.; Wang, X.; Li, S.; Ding, J.; Kong, X.; Wang, Q.; et al. Anatomic resection versus radiofrequency ablation with an ablative margin ≥ 1.0 cm for solitary small hepatocellular carcinoma measuring ≤ 3 cm: Comparison of long-term outcomes using propensity score matching analysis. Eur. J. Radiol. 2022, 155, 110498. [Google Scholar] [CrossRef]
- McWilliams, J.P.; Yamamoto, S.; Raman, S.S.; Loh, C.T.; Lee, E.W.; Liu, D.M.; Kee, S.T. Percutaneous ablation of hepatocellular carcinoma: Current status. J. Vasc. Interv. Radiol. 2010, 21, S204–S213. [Google Scholar] [CrossRef]
- Abitabile, P.; Hartl, U.; Lange, J.; Maurer, C.A. Radiofrequency ablation permits an effective treatment for colorectal liver metastasis. Eur. J. Surg. Oncol. 2007, 33, 67–71. [Google Scholar] [CrossRef]
- Bolondi, L.; Gaiani, S.; Celli, N.; Piscaglia, F. Tumor dissemination after radiofrequency ablation of hepatocellular carcinoma. Hepatology 2001, 34, 608, author reply 610–611. [Google Scholar] [CrossRef]
- Lu, D.E.; Cheng, S.W.; Lin, Y.S.; Tu, M.W.; Lee, C.H.; Chen, C.; Chen, K.H. Combination of radiofrequency ablation and percutaneous ethanol injection versus radiofrequency ablation alone for hepatocellular carcinoma: A systematic review and meta-analysis. Ann. Hepatol. 2022, 27, 100729. [Google Scholar] [CrossRef]





| Material | σ (S/m) | Cp (J/kg∙K) | k (W/m∙K) | ωb (s−1) |
|---|---|---|---|---|
| Liver | 0.333 | 3600 | 0.512 | 0.0017 |
| Tumor | 0.1168 | 4200 | 0.552 | 0.0156 |
| Prongs | 9.8 × 105 | 500 | 36.7 | |
| Trocar | 10−16 | 1010 | 0.23 | |
| Blood | 4180 | 0.0064 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zheng, H.; Li, P.; Ma, R.; Zhang, F.; Ji, H.; Monsky, W.L.; Johnson, E.; Yang, W.; Ni, C.; Gao, D.; et al. Development of a Three-Dimensional Multi-Modal Perfusion-Thermal Electrode System for Complete Tumor Eradication. Cancers 2022, 14, 4768. https://doi.org/10.3390/cancers14194768
Zheng H, Li P, Ma R, Zhang F, Ji H, Monsky WL, Johnson E, Yang W, Ni C, Gao D, et al. Development of a Three-Dimensional Multi-Modal Perfusion-Thermal Electrode System for Complete Tumor Eradication. Cancers. 2022; 14(19):4768. https://doi.org/10.3390/cancers14194768
Chicago/Turabian StyleZheng, Hui, Peicheng Li, Ruidong Ma, Feng Zhang, Hongxiu Ji, Wayne L. Monsky, Evan Johnson, Weizhu Yang, Caifang Ni, Dayong Gao, and et al. 2022. "Development of a Three-Dimensional Multi-Modal Perfusion-Thermal Electrode System for Complete Tumor Eradication" Cancers 14, no. 19: 4768. https://doi.org/10.3390/cancers14194768
APA StyleZheng, H., Li, P., Ma, R., Zhang, F., Ji, H., Monsky, W. L., Johnson, E., Yang, W., Ni, C., Gao, D., & Yang, X. (2022). Development of a Three-Dimensional Multi-Modal Perfusion-Thermal Electrode System for Complete Tumor Eradication. Cancers, 14(19), 4768. https://doi.org/10.3390/cancers14194768







