Treatment of Intrahepatic Cholangiocarcinoma—A Multidisciplinary Approach
Abstract
:Simple Summary
Abstract
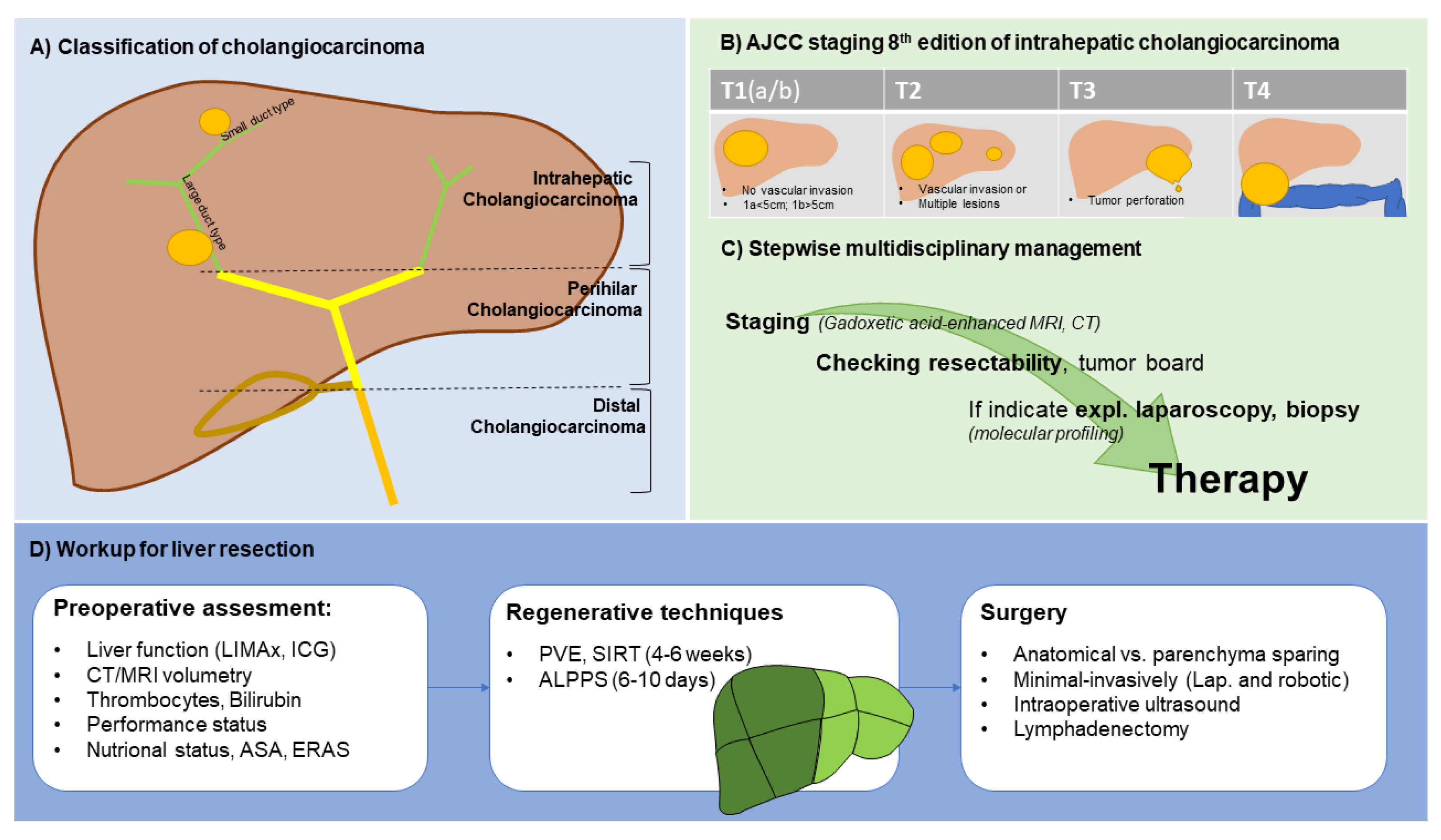
1. Introduction
2. Diagnostics
3. Liver Resection
3.1. Role of Lymphadenectomy
3.2. Role of Resection Margins
3.3. Minimally Invasive Liver Resection
3.4. Management of the Future Liver Remnant
4. Liver Transplantation
5. Systemic Treatment
5.1. Role for Neoadjuvant Chemotherapy in Intrahepatic Cholangiocarcinomas
5.2. Adjuvant Chemotherapy
6. Interventional Treatments
7. Targeted Therapies
8. Role of Immunotherapies
9. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Rizvi, S.; Khan, S.A.; Hallemeier, C.L.; Kelley, R.K.; Gores, G.J. Cholangiocarcinoma—Evolving Concepts and Therapeutic Strategies. Nat. Rev. Clin. Oncol. 2018, 15, 95–111. [Google Scholar] [CrossRef] [Green Version]
- Florio, A.A.; Ferlay, J.; Znaor, A.; Ruggieri, D.; Alvarez, C.S.; Laversanne, M.; Bray, F.; McGlynn, K.A.; Petrick, J.L. Global Trends in Intrahepatic and Extrahepatic Cholangiocarcinoma Incidence from 1993 to 2012. Cancer 2020, 126, 2666–2678. [Google Scholar] [CrossRef]
- Bertuccio, P.; Malvezzi, M.; Carioli, G.; Hashim, D.; Boffetta, P.; El-Serag, H.B.; La Vecchia, C.; Negri, E. Global Trends in Mortality from Intrahepatic and Extrahepatic Cholangiocarcinoma. J. Hepatol. 2019, 71, 104–114. [Google Scholar] [CrossRef]
- Burak, K.; Angulo, P.; Pasha, T.M.; Egan, K.; Petz, J.; Lindor, K.D. Incidence and Risk Factors for Cholangiocarcinoma in Primary Sclerosing Cholangitis. Am. J. Gastroenterol. 2004, 99, 523–526. [Google Scholar] [CrossRef]
- Boberg, K.M.; Bergquist, A.; Mitchell, S.; Pares, A.; Rosina, F.; Broomé, U.; Chapman, R.; Fausa, O.; Egeland, T.; Rocca, G.; et al. Cholangiocarcinoma in Primary Sclerosing Cholangitis: Risk Factors and Clinical Presentation. Scand. J. Gastroenterol. 2002, 37, 1205–1211. [Google Scholar] [CrossRef]
- Palmer, W.C.; Patel, T. Are Common Factors Involved in the Pathogenesis of Primary Liver Cancers? A Meta-Analysis of Risk Factors for Intrahepatic Cholangiocarcinoma. J. Hepatol. 2012, 57, 69–76. [Google Scholar] [CrossRef] [Green Version]
- Sripa, B.; Brindley, P.J.; Mulvenna, J.; Laha, T.; Smout, M.J.; Mairiang, E.; Bethony, J.M.; Loukas, A. The Tumorigenic Liver Fluke Opisthorchis Viverrini--Multiple Pathways to Cancer. Trends Parasitol. 2012, 28, 395–407. [Google Scholar] [CrossRef] [Green Version]
- Kim, T.-S.; Pak, J.H.; Kim, J.-B.; Bahk, Y.Y. Clonorchis Sinensis, an Oriental Liver Fluke, as a Human Biological Agent of Cholangiocarcinoma: A Brief Review. BMB Rep. 2016, 49, 590–597. [Google Scholar] [CrossRef] [Green Version]
- Corrao, S.; Natoli, G.; Argano, C. Nonalcoholic Fatty Liver Disease Is Associated with Intrahepatic Cholangiocarcinoma and Not with Extrahepatic Form: Definitive Evidence from Meta-Analysis and Trial Sequential Analysis. Eur. J. Gastroenterol. Hepatol. 2021, 33, 62–68. [Google Scholar] [CrossRef]
- Zhang, H.; Yang, T.; Wu, M.; Shen, F. Intrahepatic Cholangiocarcinoma: Epidemiology, Risk Factors, Diagnosis and Surgical Management. Cancer Lett. 2016, 379, 198–205. [Google Scholar] [CrossRef]
- Banales, J.M.; Marin, J.J.G.; Lamarca, A.; Rodrigues, P.M.; Khan, S.A.; Roberts, L.R.; Cardinale, V.; Carpino, G.; Andersen, J.B.; Braconi, C.; et al. Cholangiocarcinoma 2020: The next Horizon in Mechanisms and Management. Nat. Rev. Gastroenterol. Hepatol. 2020, 17, 557–588. [Google Scholar] [CrossRef]
- Yamamoto, M.; Ariizumi, S.; Otsubo, T.; Katsuragawa, H.; Katagiri, S.; Nakano, M.; Takasaki, K. Intrahepatic Cholangiocarcinoma Diagnosed Preoperatively as Hepatocellular Carcinoma. J. Surg. Oncol. 2004, 87, 80–83, discussion 83–84. [Google Scholar] [CrossRef]
- Galassi, M.; Iavarone, M.; Rossi, S.; Bota, S.; Vavassori, S.; Rosa, L.; Leoni, S.; Venerandi, L.; Marinelli, S.; Sangiovanni, A.; et al. Patterns of Appearance and Risk of Misdiagnosis of Intrahepatic Cholangiocarcinoma in Cirrhosis at Contrast Enhanced Ultrasound. Liver Int. 2013, 33, 771–779. [Google Scholar] [CrossRef]
- Bridgewater, J.; Galle, P.R.; Khan, S.A.; Llovet, J.M.; Park, J.-W.; Patel, T.; Pawlik, T.M.; Gores, G.J. Guidelines for the Diagnosis and Management of Intrahepatic Cholangiocarcinoma. J. Hepatol. 2014, 60, 1268–1289. [Google Scholar] [CrossRef] [Green Version]
- Cai, Y.; Cheng, N.; Ye, H.; Li, F.; Song, P.; Tang, W. The Current Management of Cholangiocarcinoma: A Comparison of Current Guidelines. Biosci. Trends 2016, 10, 92–102. [Google Scholar] [CrossRef] [Green Version]
- Khaderi, S.A.; Sussman, N.L. Screening for Malignancy in Primary Sclerosing Cholangitis (PSC). Curr. Gastroenterol. Rep. 2015, 17, 17. [Google Scholar] [CrossRef]
- Banales, J.M.; Cardinale, V.; Carpino, G.; Marzioni, M.; Andersen, J.B.; Invernizzi, P.; Lind, G.E.; Folseraas, T.; Forbes, S.J.; Fouassier, L.; et al. Expert Consensus Document: Cholangiocarcinoma: Current Knowledge and Future Perspectives Consensus Statement from the European Network for the Study of Cholangiocarcinoma (ENS-CCA). Nat. Rev. Gastroenterol. Hepatol. 2016, 13, 261–280. [Google Scholar] [CrossRef]
- Kim, Y.-Y.; Yeom, S.-K.; Shin, H.; Choi, S.H.; Rhee, H.; Park, J.H.; Cho, E.-S.; Park, S.; Lee, S.S.; Park, M.-S. Clinical Staging of Mass-Forming Intrahepatic Cholangiocarcinoma: Computed Tomography versus Magnetic Resonance Imaging. Hepatol. Commun. 2021, 5, 2009–2018. [Google Scholar] [CrossRef]
- Choi, S.H.; Lee, S.S.; Kim, S.Y.; Park, S.H.; Park, S.H.; Kim, K.M.; Hong, S.-M.; Yu, E.; Lee, M.-G. Intrahepatic Cholangiocarcinoma in Patients with Cirrhosis: Differentiation from Hepatocellular Carcinoma by Using Gadoxetic Acid-Enhanced MR Imaging and Dynamic CT. Radiology 2017, 282, 771–781. [Google Scholar] [CrossRef]
- Promsorn, J.; Soontrapa, W.; Somsap, K.; Chamadol, N.; Limpawattana, P.; Harisinghani, M. Evaluation of the Diagnostic Performance of Apparent Diffusion Coefficient (ADC) Values on Diffusion-Weighted Magnetic Resonance Imaging (DWI) in Differentiating between Benign and Metastatic Lymph Nodes in Cases of Cholangiocarcinoma. Abdom. Radiol. 2019, 44, 473–481. [Google Scholar] [CrossRef]
- Songthamwat, M.; Chamadol, N.; Khuntikeo, N.; Thinkhamrop, J.; Koonmee, S.; Chaichaya, N.; Bethony, J.; Thinkhamrop, B. Evaluating a Preoperative Protocol That Includes Magnetic Resonance Imaging for Lymph Node Metastasis in the Cholangiocarcinoma Screening and Care Program (CASCAP) in Thailand. World J. Surg. Oncol. 2017, 15, 176. [Google Scholar] [CrossRef] [Green Version]
- Lamarca, A.; Barriuso, J.; Chander, A.; McNamara, M.G.; Hubner, R.A.; ÓReilly, D.; Manoharan, P.; Valle, J.W. F-Fluorodeoxyglucose Positron Emission Tomography (FDG-PET) for Patients with Biliary Tract Cancer: Systematic Review and Meta-Analysis. J. Hepatol. 2019, 71, 115–129. [Google Scholar] [CrossRef] [Green Version]
- Nagtegaal, I.D.; Odze, R.D.; Klimstra, D.; Paradis, V.; Rugge, M.; Schirmacher, P.; Washington, K.M.; Carneiro, F.; Cree, I.A. WHO Classification of Tumours Editorial Board The 2019 WHO Classification of Tumours of the Digestive System. Histopathology 2020, 76, 182–188. [Google Scholar] [CrossRef] [Green Version]
- Squires, M.H.; Cloyd, J.M.; Dillhoff, M.; Schmidt, C.; Pawlik, T.M. Challenges of Surgical Management of Intrahepatic Cholangiocarcinoma. Expert Rev. Gastroenterol. Hepatol. 2018, 12, 671–681. [Google Scholar] [CrossRef]
- Doussot, A.; Groot-Koerkamp, B.; Wiggers, J.K.; Chou, J.; Gonen, M.; DeMatteo, R.P.; Allen, P.J.; Kingham, T.P.; D’Angelica, M.I.; Jarnagin, W.R. Outcomes after Resection of Intrahepatic Cholangiocarcinoma: External Validation and Comparison of Prognostic Models. J. Am. Coll. Surg. 2015, 221, 452–461. [Google Scholar] [CrossRef] [Green Version]
- Amini, N.; Ejaz, A.; Spolverato, G.; Kim, Y.; Herman, J.M.; Pawlik, T.M. Temporal Trends in Liver-Directed Therapy of Patients with Intrahepatic Cholangiocarcinoma in the United States: A Population-Based Analysis. J. Surg. Oncol. 2014, 110, 163–170. [Google Scholar] [CrossRef]
- D’Angelica, M.; Fong, Y.; Weber, S.; Gonen, M.; DeMatteo, R.P.; Conlon, K.; Blumgart, L.H.; Jarnagin, W.R. The Role of Staging Laparoscopy in Hepatobiliary Malignancy: Prospective Analysis of 401 Cases. Ann. Surg. Oncol. 2003, 10, 183–189. [Google Scholar] [CrossRef]
- Goere, D.; Wagholikar, G.D.; Pessaux, P.; Carrère, N.; Sibert, A.; Vilgrain, V.; Sauvanet, A.; Belghiti, J. Utility of Staging Laparoscopy in Subsets of Biliary Cancers: Laparoscopy Is a Powerful Diagnostic Tool in Patients with Intrahepatic and Gallbladder Carcinoma. Surg. Endosc. 2006, 20, 721–725. [Google Scholar] [CrossRef]
- Mavros, M.N.; Economopoulos, K.P.; Alexiou, V.G.; Pawlik, T.M. Treatment and Prognosis for Patients with Intrahepatic Cholangiocarcinoma: Systematic Review and Meta-Analysis. JAMA Surg. 2014, 149, 565–574. [Google Scholar] [CrossRef] [Green Version]
- Groot Koerkamp, B.; Fong, Y. Outcomes in Biliary Malignancy. J. Surg. Oncol. 2014, 110, 585–591. [Google Scholar] [CrossRef]
- Hyder, O.; Hatzaras, I.; Sotiropoulos, G.C.; Paul, A.; Alexandrescu, S.; Marques, H.; Pulitano, C.; Barroso, E.; Clary, B.M.; Aldrighetti, L.; et al. Recurrence after Operative Management of Intrahepatic Cholangiocarcinoma. Surgery 2013, 153, 811–818. [Google Scholar] [CrossRef]
- Buettner, S.; Ten Cate, D.W.G.; Bagante, F.; Alexandrescu, S.; Marques, H.P.; Lamelas, J.; Aldrighetti, L.; Gamblin, T.C.; Maithel, S.K.; Pulitano, C.; et al. Survival after Resection of Multiple Tumor Foci of Intrahepatic Cholangiocarcinoma. J. Gastrointest. Surg. 2019, 23, 2239–2246. [Google Scholar] [CrossRef] [Green Version]
- Addeo, P.; Jedidi, I.; Locicero, A.; Faitot, F.; Oncioiu, C.; Onea, A.; Bachellier, P. Prognostic Impact of Tumor Multinodularity in Intrahepatic Cholangiocarcinoma. J. Gastrointest. Surg. 2019, 23, 1801–1809. [Google Scholar] [CrossRef]
- Cillo, U.; Fondevila, C.; Donadon, M.; Gringeri, E.; Mocchegiani, F.; Schlitt, H.J.; Ijzermans, J.N.M.; Vivarelli, M.; Zieniewicz, K.; Olde Damink, S.W.M.; et al. Surgery for Cholangiocarcinoma. Liver Int. 2019, 39 (Suppl. S1), 143–155. [Google Scholar] [CrossRef] [Green Version]
- Koch, M.; Garden, O.J.; Padbury, R.; Rahbari, N.N.; Adam, R.; Capussotti, L.; Fan, S.T.; Yokoyama, Y.; Crawford, M.; Makuuchi, M.; et al. Bile Leakage after Hepatobiliary and Pancreatic Surgery: A Definition and Grading of Severity by the International Study Group of Liver Surgery. Surgery 2011, 149, 680–688. [Google Scholar] [CrossRef]
- Bartsch, F.; Eberhard, J.; Rückert, F.; Schmelzle, M.; Lehwald-Tywuschik, N.; Fichtner-Feigl, S.; Gaedcke, J.; Oldhafer, K.J.; Oldhafer, F.; Diener, M.; et al. Repeated Resection for Recurrent Intrahepatic Cholangiocarcinoma: A Retrospective German Multicentre Study. Liver Int. 2021, 41, 180–191. [Google Scholar] [CrossRef]
- Martin, S.P.; Drake, J.; Wach, M.M.; Ruff, S.M.; Diggs, L.P.; Wan, J.Y.; Good, M.L.; Dominguez, D.A.; Ayabe, R.I.; Glazer, E.S.; et al. Resection and Chemotherapy Is the Optimal Treatment Approach for Patients with Clinically Node Positive Intrahepatic Cholangiocarcinoma. HPB 2020, 22, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Kizy, S.; Altman, A.M.; Marmor, S.; Wirth, K.; Ching Hui, J.Y.; Tuttle, T.M.; Denbo, J.W.; Jensen, E.H. Surgical Resection of Lymph Node Positive Intrahepatic Cholangiocarcinoma May Not Improve Survival. HPB 2019, 21, 235–241. [Google Scholar] [CrossRef] [Green Version]
- Tran Cao, H.S.; Zhang, Q.; Sada, Y.H.; Chai, C.; Curley, S.A.; Massarweh, N.N. The Role of Surgery and Adjuvant Therapy in Lymph Node-Positive Cancers of the Gallbladder and Intrahepatic Bile Ducts. Cancer 2018, 124, 74–83. [Google Scholar] [CrossRef] [Green Version]
- de Jong, M.C.; Nathan, H.; Sotiropoulos, G.C.; Paul, A.; Alexandrescu, S.; Marques, H.; Pulitano, C.; Barroso, E.; Clary, B.M.; Aldrighetti, L.; et al. Intrahepatic Cholangiocarcinoma: An International Multi-Institutional Analysis of Prognostic Factors and Lymph Node Assessment. J. Clin. Oncol. 2011, 29, 3140–3145. [Google Scholar] [CrossRef] [Green Version]
- Endo, I.; Gonen, M.; Yopp, A.C.; Dalal, K.M.; Zhou, Q.; Klimstra, D.; D’Angelica, M.; DeMatteo, R.P.; Fong, Y.; Schwartz, L.; et al. Intrahepatic Cholangiocarcinoma: Rising Frequency, Improved Survival, and Determinants of Outcome after Resection. Ann. Surg. 2008, 248, 84–96. [Google Scholar] [CrossRef]
- Doussot, A.; Gonen, M.; Wiggers, J.K.; Groot-Koerkamp, B.; DeMatteo, R.P.; Fuks, D.; Allen, P.J.; Farges, O.; Kingham, T.P.; Regimbeau, J.M.; et al. Recurrence Patterns and Disease-Free Survival after Resection of Intrahepatic Cholangiocarcinoma: Preoperative and Postoperative Prognostic Models. J. Am. Coll. Surg. 2016, 223, 493–505.e2. [Google Scholar] [CrossRef] [Green Version]
- Spolverato, G.; Kim, Y.; Alexandrescu, S.; Popescu, I.; Marques, H.P.; Aldrighetti, L.; Clark Gamblin, T.; Miura, J.; Maithel, S.K.; Squires, M.H.; et al. Is Hepatic Resection for Large or Multifocal Intrahepatic Cholangiocarcinoma Justified? Results from a Multi-Institutional Collaboration. Ann. Surg. Oncol. 2015, 22, 2218–2225. [Google Scholar] [CrossRef] [Green Version]
- Yoh, T.; Hatano, E.; Yamanaka, K.; Nishio, T.; Seo, S.; Taura, K.; Yasuchika, K.; Okajima, H.; Kaido, T.; Uemoto, S. Is Surgical Resection Justified for Advanced Intrahepatic Cholangiocarcinoma? Liver Cancer 2016, 5, 280–289. [Google Scholar] [CrossRef] [Green Version]
- Reames, B.N.; Ejaz, A.; Koerkamp, B.G.; Alexandrescu, S.; Marques, H.P.; Aldrighetti, L.; Maithel, S.K.; Pulitano, C.; Bauer, T.W.; Shen, F.; et al. Impact of Major Vascular Resection on Outcomes and Survival in Patients with Intrahepatic Cholangiocarcinoma: A Multi-Institutional Analysis. J. Surg. Oncol. 2017, 116, 133–139. [Google Scholar] [CrossRef]
- Lee, A.J.; Chun, Y.S. Intrahepatic Cholangiocarcinoma: The AJCC/UICC 8th Edition Updates. Chin. Clin. Oncol. 2018, 7, 52. [Google Scholar] [CrossRef]
- Clark, C.J.; Wood-Wentz, C.M.; Reid-Lombardo, K.M.; Kendrick, M.L.; Huebner, M.; Que, F.G. Lymphadenectomy in the Staging and Treatment of Intrahepatic Cholangiocarcinoma: A Population-Based Study Using the National Cancer Institute SEER Database. HPB 2011, 13, 612–620. [Google Scholar] [CrossRef] [Green Version]
- Mazzaferro, V.; Gorgen, A.; Roayaie, S.; Droz Dit Busset, M.; Sapisochin, G. Liver Resection and Transplantation for Intrahepatic Cholangiocarcinoma. J. Hepatol. 2020, 72, 364–377. [Google Scholar] [CrossRef] [Green Version]
- Zhang, X.-F.; Lv, Y.; Weiss, M.; Popescu, I.; Marques, H.P.; Aldrighetti, L.; Maithel, S.K.; Pulitano, C.; Bauer, T.W.; Shen, F.; et al. Should Utilization of Lymphadenectomy Vary According to Morphologic Subtype of Intrahepatic Cholangiocarcinoma? Ann. Surg. Oncol. 2019, 26, 2242–2250. [Google Scholar] [CrossRef]
- Zhou, R.; Lu, D.; Li, W.; Tan, W.; Zhu, S.; Chen, X.; Min, J.; Shang, C.; Chen, Y. Is Lymph Node Dissection Necessary for Resectable Intrahepatic Cholangiocarcinoma? A Systematic Review and Meta-Analysis. HPB 2019, 21, 784–792. [Google Scholar] [CrossRef]
- Sahara, K.; Tsilimigras, D.I.; Merath, K.; Bagante, F.; Guglielmi, A.; Aldrighetti, L.; Weiss, M.; Bauer, T.W.; Alexandrescu, S.; Poultsides, G.A.; et al. Therapeutic Index Associated with Lymphadenectomy among Patients with Intrahepatic Cholangiocarcinoma: Which Patients Benefit the Most from Nodal Evaluation? Ann. Surg. Oncol. 2019, 26, 2959–2968. [Google Scholar] [CrossRef]
- Kang, C.M.; Suh, K.-S.; Yi, N.-J.; Hong, T.H.; Park, S.J.; Ahn, K.S.; Hayashi, H.; Choi, S.B.; Jeong, C.-Y.; Takahara, T.; et al. Should Lymph Nodes Be Retrieved in Patients with Intrahepatic Cholangiocarcinoma? A Collaborative Korea-Japan Study. Cancers 2021, 13, 445. [Google Scholar] [CrossRef]
- Tang, H.; Lu, W.; Li, B.; Meng, X.; Dong, J. Influence of Surgical Margins on Overall Survival after Resection of Intrahepatic Cholangiocarcinoma: A Meta-Analysis. Medicine 2016, 95, e4621. [Google Scholar] [CrossRef]
- Spolverato, G.; Yakoob, M.Y.; Kim, Y.; Alexandrescu, S.; Marques, H.P.; Lamelas, J.; Aldrighetti, L.; Gamblin, T.C.; Maithel, S.K.; Pulitano, C.; et al. The Impact of Surgical Margin Status on Long-Term Outcome After Resection for Intrahepatic Cholangiocarcinoma. Ann. Surg. Oncol. 2015, 22, 4020–4028. [Google Scholar] [CrossRef]
- Si, A.; Li, J.; Yang, Z.; Xia, Y.; Yang, T.; Lei, Z.; Cheng, Z.; Pawlik, T.M.; Lau, W.Y.; Shen, F. Impact of Anatomical Versus Non-Anatomical Liver Resection on Short- and Long-Term Outcomes for Patients with Intrahepatic Cholangiocarcinoma. Ann. Surg. Oncol. 2019, 26, 1841–1850. [Google Scholar] [CrossRef]
- Li, B.; Song, J.L.; Aierken, Y.; Chen, Y.; Zheng, J.L.; Yang, J.Y. Nonanatomic Resection Is Not Inferior to Anatomic Resection for Primary Intrahepatic Cholangiocarcinoma: A Propensity Score Analysis. Sci. Rep. 2018, 8, 17799. [Google Scholar] [CrossRef] [Green Version]
- Haber, P.K.; Wabitsch, S.; Kästner, A.; Andreou, A.; Krenzien, F.; Schöning, W.; Pratschke, J.; Schmelzle, M. Laparoscopic Liver Resection for Intrahepatic Cholangiocarcinoma: A Single-Center Experience. J. Laparoendosc. Adv. Surg. Tech. A 2020, 30, 1354–1359. [Google Scholar] [CrossRef]
- Haber, P.K.; Maier, C.; Kästner, A.; Feldbrügge, L.; Ortiz Galindo, S.A.; Geisel, D.; Fehrenbach, U.; Biebl, M.; Krenzien, F.; Benzing, C.; et al. Predicting the Risk of Postoperative Complications in Patients Undergoing Minimally Invasive Resection of Primary Liver Tumors. J. Clin. Med. Res. 2021, 10, 685. [Google Scholar] [CrossRef]
- Ratti, F.; Rawashdeh, A.; Cipriani, F.; Primrose, J.; Fiorentini, G.; Abu Hilal, M.; Aldrighetti, L. Intrahepatic Cholangiocarcinoma as the New Field of Implementation of Laparoscopic Liver Resection Programs. A Comparative Propensity Score-Based Analysis of Open and Laparoscopic Liver Resections. Surg. Endosc. 2021, 35, 1851–1862. [Google Scholar] [CrossRef]
- Ratti, F.; Cipriani, F.; Ariotti, R.; Gagliano, A.; Paganelli, M.; Catena, M.; Aldrighetti, L. Safety and Feasibility of Laparoscopic Liver Resection with Associated Lymphadenectomy for Intrahepatic Cholangiocarcinoma: A Propensity Score-Based Case-Matched Analysis from a Single Institution. Surg. Endosc. 2016, 30, 1999–2010. [Google Scholar] [CrossRef]
- Levi Sandri, G.B.; Spoletini, G.; Mascianà, G.; Colasanti, M.; Lepiane, P.; Vennarecci, G.; D’Andrea, V.; Ettorre, G.M. The Role of Minimally Invasive Surgery in the Treatment of Cholangiocarcinoma. Eur. J. Surg. Oncol. 2017, 43, 1617–1621. [Google Scholar] [CrossRef]
- Machairas, N.; Kostakis, I.D.; Schizas, D.; Kykalos, S.; Nikiteas, N.; Sotiropoulos, G.C. Meta-Analysis of Laparoscopic versus Open Liver Resection for Intrahepatic Cholangiocarcinoma. Updates Surg. 2021, 73, 59–68. [Google Scholar] [CrossRef]
- Khan, S.; Beard, R.E.; Kingham, P.T.; Fong, Y.; Boerner, T.; Martinie, J.B.; Vrochides, D.; Buell, J.F.; Berber, E.; Kahramangil, B.; et al. Long-Term Oncologic Outcomes Following Robotic Liver Resections for Primary Hepatobiliary Malignancies: A Multicenter Study. Ann. Surg. Oncol. 2018, 25, 2652–2660. [Google Scholar] [CrossRef]
- Kabir, T.; Tan, Z.Z.; Syn, N.L.; Wu, E.; Lin, J.D.; Zhao, J.J.; Tan, A.Y.H.; Hui, Y.; Kam, J.H.; Goh, B.K.P. Laparoscopic versus Open Resection of Hepatocellular Carcinoma in Patients with Cirrhosis: A Meta-Analysis. Br. J. Surg. 2021, 109, 21–29. [Google Scholar] [CrossRef]
- Liu, R.; Wakabayashi, G.; Kim, H.-J.; Choi, G.-H.; Yiengpruksawan, A.; Fong, Y.; He, J.; Boggi, U.; Troisi, R.I.; Efanov, M.; et al. International Consensus Statement on Robotic Hepatectomy Surgery in 2018. World J. Gastroenterol. 2019, 25, 1432–1444. [Google Scholar] [CrossRef]
- Abu Hilal, M.; Aldrighetti, L.; Dagher, I.; Edwin, B.; Troisi, R.I.; Alikhanov, R.; Aroori, S.; Belli, G.; Besselink, M.; Briceno, J.; et al. The Southampton Consensus Guidelines for Laparoscopic Liver Surgery: From Indication to Implementation. Ann. Surg. 2018, 268, 11–18. [Google Scholar] [CrossRef] [Green Version]
- Sunagawa, Y.; Yamada, S.; Kato, Y.; Sonohara, F.; Takami, H.; Inokawa, Y.; Hayashi, M.; Nakayama, G.; Koike, M.; Kodera, Y. Perioperative Assessment of Indocyanine Green Elimination Rate Accurately Predicts Postoperative Liver Failure in Patients Undergoing Hepatectomy. J. Hepatobiliary Pancreat. Sci. 2021, 28, 86–94. [Google Scholar] [CrossRef]
- Stockmann, M.; Lock, J.F.; Malinowski, M.; Niehues, S.M.; Seehofer, D.; Neuhaus, P. The LiMAx Test: A New Liver Function Test for Predicting Postoperative Outcome in Liver Surgery. HPB 2010, 12, 139–146. [Google Scholar] [CrossRef] [Green Version]
- Kim, D.; Cornman-Homonoff, J.; Madoff, D.C. Preparing for Liver Surgery with “Alphabet Soup”: PVE, ALPPS, TAE-PVE, LVD and RL. Hepatobiliary Surg. Nutr. 2020, 9, 136–151. [Google Scholar] [CrossRef]
- Azoulay, D.; Castaing, D.; Krissat, J.; Smail, A.; Hargreaves, G.M.; Lemoine, A.; Emile, J.F.; Bismuth, H. Percutaneous Portal Vein Embolization Increases the Feasibility and Safety of Major Liver Resection for Hepatocellular Carcinoma in Injured Liver. Ann. Surg. 2000, 232, 665–672. [Google Scholar] [CrossRef]
- Adam, R.; Pascal, G.; Castaing, D.; Azoulay, D.; Delvart, V.; Paule, B.; Levi, F.; Bismuth, H. Tumor Progression While on Chemotherapy: A Contraindication to Liver Resection for Multiple Colorectal Metastases? Ann. Surg. 2004, 240, 1052–1061, discussion 1061–1064. [Google Scholar] [CrossRef]
- Petrowsky, H.; Fritsch, R.; Guckenberger, M.; De Oliveira, M.L.; Dutkowski, P.; Clavien, P.-A. Modern Therapeutic Approaches for the Treatment of Malignant Liver Tumours. Nat. Rev. Gastroenterol. Hepatol. 2020, 17, 755–772. [Google Scholar] [CrossRef]
- Laurent, C.; Fernandez, B.; Marichez, A.; Adam, J.-P.; Papadopoulos, P.; Lapuyade, B.; Chiche, L. Radiological Simultaneous Portohepatic Vein Embolization (RASPE) Before Major Hepatectomy: A Better Way to Optimize Liver Hypertrophy Compared to Portal Vein Embolization. Ann. Surg. 2020, 272, 199–205. [Google Scholar] [CrossRef]
- Deshayes, E.; Piron, L.; Bouvier, A.; Lapuyade, B.; Lermite, E.; Vervueren, L.; Laurent, C.; Pinaquy, J.-B.; Chevallier, P.; Dohan, A.; et al. Study Protocol of the HYPER-LIV01 Trial: A Multicenter Phase II, Prospective and Randomized Study Comparing Simultaneous Portal and Hepatic Vein Embolization to Portal Vein Embolization for Hypertrophy of the Future Liver Remnant before Major Hepatectomy for Colo-Rectal Liver Metastases. BMC Cancer 2020, 20, 574. [Google Scholar]
- Hasselgren, K.; Røsok, B.I.; Larsen, P.N.; Sparrelid, E.; Lindell, G.; Schultz, N.A.; Bjørnbeth, B.A.; Isaksson, B.; Larsson, A.L.; Rizell, M.; et al. ALPPS Improves Survival Compared with TSH in Patients Affected of CRLM: Survival Analysis from the Randomized Controlled Trial LIGRO. Ann. Surg. 2021, 273, 442–448. [Google Scholar] [CrossRef]
- Bednarsch, J.; Czigany, Z.; Lurje, I.; Strnad, P.; Bruners, P.; Ulmer, T.F.; den Dulk, M.; Lurje, G.; Neumann, U.P. The Role of ALPPS in Intrahepatic Cholangiocarcinoma. Langenbecks. Arch. Surg. 2019, 404, 885–894. [Google Scholar] [CrossRef]
- Li, J.; Moustafa, M.; Linecker, M.; Lurje, G.; Capobianco, I.; Baumgart, J.; Ratti, F.; Rauchfuss, F.; Balci, D.; Fernandes, E.; et al. ALPPS for Locally Advanced Intrahepatic Cholangiocarcinoma: Did Aggressive Surgery Lead to the Oncological Benefit? An International Multi-Center Study. Ann. Surg. Oncol. 2020, 27, 1372–1384. [Google Scholar] [CrossRef] [Green Version]
- Razumilava, N.; Gores, G.J. Cholangiocarcinoma. Lancet 2014, 383, 2168–2179. [Google Scholar] [CrossRef] [Green Version]
- Pichlmayr, R.; Weimann, A.; Oldhafer, K.J.; Schlitt, H.J.; Klempnauer, J.; Bornscheuer, A.; Chavan, A.; Schmoll, E.; Lang, H.; Tusch, G. Role of Liver Transplantation in the Treatment of Unresectable Liver Cancer. World J. Surg. 1995, 19, 807–813. [Google Scholar] [CrossRef]
- Ziogas, I.A.; Giannis, D.; Economopoulos, K.P.; Hayat, M.H.; Montenovo, M.I.; Matsuoka, L.K.; Alexopoulos, S.P. Liver Transplantation for Intrahepatic Cholangiocarcinoma: A Meta-Analysis and Meta-Regression of Survival Rates. Transplantation 2021, 105, 2263–2271. [Google Scholar] [CrossRef]
- Sapisochin, G.; de Lope, C.R.; Gastaca, M.; de Urbina, J.O.; López-Andujar, R.; Palacios, F.; Ramos, E.; Fabregat, J.; Castroagudín, J.F.; Varo, E.; et al. Intrahepatic Cholangiocarcinoma or Mixed Hepatocellular-Cholangiocarcinoma in Patients Undergoing Liver Transplantation: A Spanish Matched Cohort Multicenter Study. Ann. Surg. 2014, 259, 944–952. [Google Scholar] [CrossRef]
- Sapisochin, G.; Facciuto, M.; Rubbia-Brandt, L.; Marti, J.; Mehta, N.; Yao, F.Y.; Vibert, E.; Cherqui, D.; Grant, D.R.; Hernandez-Alejandro, R.; et al. Liver Transplantation for “Very Early” Intrahepatic Cholangiocarcinoma: International Retrospective Study Supporting a Prospective Assessment. Hepatology 2016, 64, 1178–1188. [Google Scholar] [CrossRef]
- Kim, P.; Littau, M.; Baker, T.B.; Abdelsattar, Z.; Tonelli, C.; Bunn, C.; Kulshrestha, S.; Luchette, F.A.; Baker, M.S. Intrahepatic Cholangiocarcinoma: Is There a Role for Liver Transplantation? Surgery 2021, S0039-6060, 00989–2. [Google Scholar] [CrossRef]
- Lunsford, K.E.; Javle, M.; Heyne, K.; Shroff, R.T.; Abdel-Wahab, R.; Gupta, N.; Mobley, C.M.; Saharia, A.; Victor, D.W.; Nguyen, D.T.; et al. Liver Transplantation for Locally Advanced Intrahepatic Cholangiocarcinoma Treated with Neoadjuvant Therapy: A Prospective Case-Series. Lancet Gastroenterol. Hepatol. 2018, 3, 337–348. [Google Scholar] [CrossRef]
- Czigany, Z.; Pratschke, J.; Froněk, J.; Guba, M.; Schöning, W.; Raptis, D.A.; Andrassy, J.; Kramer, M.; Strnad, P.; Tolba, R.H.; et al. Hypothermic Oxygenated Machine Perfusion Reduces Early Allograft Injury and Improves Post-Transplant Outcomes in Extended Criteria Donation Liver Transplantation from Donation After Brain Death: Results from a Multicenter Randomized Controlled Trial (HOPE ECD-DBD). Ann. Surg. 2021, 274, 705–712. [Google Scholar] [PubMed]
- Avolio, A.W.; Franco, A.; Schlegel, A.; Lai, Q.; Meli, S.; Burra, P.; Patrono, D.; Ravaioli, M.; Bassi, D.; Ferla, F.; et al. Development and Validation of a Comprehensive Model to Estimate Early Allograft Failure among Patients Requiring Early Liver Retransplant. JAMA Surg. 2020, 155, e204095. [Google Scholar] [CrossRef]
- Avolio, A.W.; Lai, Q.; Cillo, U.; Romagnoli, R.; De Simone, P. L-GrAFT and EASE Scores in Liver Transplantation: Need for Reciprocal External Validation and Comparison with Other Scores. J. Hepatol. 2021, 75, 729–731. [Google Scholar] [CrossRef] [PubMed]
- Utuama, O.; Permuth, J.B.; Dagne, G.; Sanchez-Anguiano, A.; Alman, A.; Kumar, A.; Denbo, J.; Kim, R.; Fleming, J.B.; Anaya, D.A. Neoadjuvant Chemotherapy for Intrahepatic Cholangiocarcinoma: A Propensity Score Survival Analysis Supporting Use in Patients with High-Risk Disease. Ann. Surg. Oncol. 2021, 28, 1939–1949. [Google Scholar] [CrossRef]
- Buettner, S.; Koerkamp, B.G.; Ejaz, A.; Buisman, F.E.; Kim, Y.; Margonis, G.A.; Alexandrescu, S.; Marques, H.P.; Lamelas, J.; Aldrighetti, L.; et al. The Effect of Preoperative Chemotherapy Treatment in Surgically Treated Intrahepatic Cholangiocarcinoma Patients-A Multi-Institutional Analysis. J. Surg. Oncol. 2017, 115, 312–318. [Google Scholar] [CrossRef]
- Riby, D.; Mazzotta, A.D.; Bergeat, D.; Verdure, L.; Sulpice, L.; Bourien, H.; Lièvre, A.; Rolland, Y.; Garin, E.; Boudjema, K.; et al. Downstaging with Radioembolization or Chemotherapy for Initially Unresectable Intrahepatic Cholangiocarcinoma. Ann. Surg. Oncol. 2020, 27, 3729–3737. [Google Scholar] [CrossRef] [PubMed]
- Valle, J.; Wasan, H.; Palmer, D.H.; Cunningham, D.; Anthoney, A.; Maraveyas, A.; Madhusudan, S.; Iveson, T.; Hughes, S.; Pereira, S.P.; et al. Cisplatin plus Gemcitabine versus Gemcitabine for Biliary Tract Cancer. N. Engl. J. Med. 2010, 362, 1273–1281. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akateh, C.; Ejaz, A.M.; Pawlik, T.M.; Cloyd, J.M. Neoadjuvant Treatment Strategies for Intrahepatic Cholangiocarcinoma. World J. Hepatol. 2020, 12, 693–708. [Google Scholar] [CrossRef] [PubMed]
- Le Roy, B.; Gelli, M.; Pittau, G.; Allard, M.-A.; Pereira, B.; Serji, B.; Vibert, E.; Castaing, D.; Adam, R.; Cherqui, D.; et al. Neoadjuvant Chemotherapy for Initially Unresectable Intrahepatic Cholangiocarcinoma. Br. J. Surg. 2018, 105, 839–847. [Google Scholar] [CrossRef]
- Konstantinidis, I.T.; Groot Koerkamp, B.; Do, R.K.G.; Gönen, M.; Fong, Y.; Allen, P.J.; D’Angelica, M.I.; Kingham, T.P.; DeMatteo, R.P.; Klimstra, D.S.; et al. Unresectable Intrahepatic Cholangiocarcinoma: Systemic plus Hepatic Arterial Infusion Chemotherapy Is Associated with Longer Survival in Comparison with Systemic Chemotherapy Alone. Cancer 2016, 122, 758–765. [Google Scholar] [CrossRef] [PubMed]
- Rayar, M.; Sulpice, L.; Edeline, J.; Garin, E.; Levi Sandri, G.B.; Meunier, B.; Boucher, E.; Boudjema, K. Intra-Arterial Yttrium-90 Radioembolization Combined with Systemic Chemotherapy Is a Promising Method for Downstaging Unresectable Huge Intrahepatic Cholangiocarcinoma to Surgical Treatment. Ann. Surg. Oncol. 2015, 22, 3102–3108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yadav, S.; Xie, H.; Bin-Riaz, I.; Sharma, P.; Durani, U.; Goyal, G.; Borah, B.; Borad, M.J.; Smoot, R.L.; Roberts, L.R.; et al. Neoadjuvant vs. Adjuvant Chemotherapy for Cholangiocarcinoma: A Propensity Score Matched Analysis. Eur. J. Surg. Oncol. 2019, 45, 1432–1438. [Google Scholar] [CrossRef] [PubMed]
- Mason, M.C.; Massarweh, N.N.; Tzeng, C.-W.D.; Chiang, Y.-J.; Chun, Y.S.; Aloia, T.A.; Javle, M.; Vauthey, J.-N.; Tran Cao, H.S. Time to Rethink Upfront Surgery for Resectable Intrahepatic Cholangiocarcinoma? Implications from the Neoadjuvant Experience. Ann. Surg. Oncol. 2021, 28, 6725–6735. [Google Scholar] [CrossRef]
- Edeline, J.; Benabdelghani, M.; Bertaut, A.; Watelet, J.; Hammel, P.; Joly, J.-P.; Boudjema, K.; Fartoux, L.; Bouhier-Leporrier, K.; Jouve, J.-L.; et al. Gemcitabine and Oxaliplatin Chemotherapy or Surveillance in Resected Biliary Tract Cancer (PRODIGE 12-ACCORD 18-UNICANCER GI): A Randomized Phase III Study. J. Clin. Oncol. 2019, 37, 658–667. [Google Scholar] [CrossRef]
- Primrose, J.N.; Fox, R.P.; Palmer, D.H.; Malik, H.Z.; Prasad, R.; Mirza, D.; Anthony, A.; Corrie, P.; Falk, S.; Finch-Jones, M.; et al. Capecitabine Compared with Observation in Resected Biliary Tract Cancer (BILCAP): A Randomised, Controlled, Multicentre, Phase 3 Study. Lancet Oncol. 2019, 20, 663–673. [Google Scholar] [CrossRef] [Green Version]
- Ma, K.W.; Cheung, T.T.; Leung, B.; She, B.W.H.; Chok, K.S.H.; Chan, A.C.Y.; Dai, W.C.; Lo, C.M. Adjuvant Chemotherapy Improves Oncological Outcomes of Resectable Intrahepatic Cholangiocarcinoma: A Meta-Analysis. Medicine 2019, 98, e14013. [Google Scholar] [CrossRef]
- Shroff, R.T.; Kennedy, E.B.; Bachini, M.; Bekaii-Saab, T.; Crane, C.; Edeline, J.; El-Khoueiry, A.; Feng, M.; Katz, M.H.G.; Primrose, J.; et al. Adjuvant Therapy for Resected Biliary Tract Cancer: ASCO Clinical Practice Guideline. J. Clin. Oncol. 2019, 37, 1015–1027. [Google Scholar] [CrossRef] [Green Version]
- Ricke, J.; Wust, P.; Stohlmann, A.; Beck, A.; Cho, C.H.; Pech, M.; Wieners, G.; Spors, B.; Werk, M.; Rosner, C.; et al. CT-Guided Interstitial Brachytherapy of Liver Malignancies Alone or in Combination with Thermal Ablation: Phase I-II Results of a Novel Technique. Int. J. Radiat. Oncol. Biol. Phys. 2004, 58, 1496–1505. [Google Scholar] [CrossRef] [PubMed]
- Schnapauff, D.; Denecke, T.; Grieser, C.; Collettini, F.; Seehofer, D.; Sinn, M.; Banzer, J.; Lopez-Hänninen, E.; Hamm, B.; Wust, P.; et al. Computed Tomography-Guided Interstitial HDR Brachytherapy (CT-HDRBT) of the Liver in Patients with Irresectable Intrahepatic Cholangiocarcinoma. Cardiovasc. Intervent. Radiol. 2012, 35, 581–587. [Google Scholar] [CrossRef]
- Ingold, J.A.; Reed, G.B.; Kaplan, H.S.; Bagshaw, M.A. Radiation Hepatitis. Am. J. Roentgenol. Radium Ther. Nucl. Med. 1965, 93, 200–208. [Google Scholar] [PubMed]
- Phelip, J.-M.; Vendrely, V.; Rostain, F.; Subtil, F.; Jouve, J.-L.; Gasmi, M.; Michel, P.; Le Malicot, K.; Smith, D.; Seitz, J.-F.; et al. Gemcitabine plus Cisplatin versus Chemoradiotherapy in Locally Advanced Biliary Tract Cancer: Fédération Francophone de Cancérologie Digestive 9902 Phase II Randomised Study. Eur. J. Cancer 2014, 50, 2975–2982. [Google Scholar] [CrossRef] [PubMed]
- Ke, Q.; Lin, N.; Deng, M.; Wang, L.; Zeng, Y.; Liu, J. The Effect of Adjuvant Therapy for Patients with Intrahepatic Cholangiocarcinoma after Surgical Resection: A Systematic Review and Meta-Analysis. PLoS ONE 2020, 15, e0229292. [Google Scholar] [CrossRef] [Green Version]
- Li, J.; Wang, Q.; Lei, Z.; Wu, D.; Si, A.; Wang, K.; Wan, X.; Wang, Y.; Yan, Z.; Xia, Y.; et al. Adjuvant Transarterial Chemoembolization Following Liver Resection for Intrahepatic Cholangiocarcinoma Based on Survival Risk Stratification. Oncologist 2015, 20, 640–647. [Google Scholar] [CrossRef] [Green Version]
- Al-Adra, D.P.; Gill, R.S.; Axford, S.J.; Shi, X.; Kneteman, N.; Liau, S.-S. Treatment of Unresectable Intrahepatic Cholangiocarcinoma with Yttrium-90 Radioembolization: A Systematic Review and Pooled Analysis. Eur. J. Surg. Oncol. 2015, 41, 120–127. [Google Scholar] [CrossRef] [Green Version]
- Apisarnthanarax, S.; Barry, A.; Cao, M.; Czito, B.; DeMatteo, R.; Drinane, M.; Hallemeier, C.L.; Koay, E.J.; Lasley, F.; Meyer, J.; et al. External Beam Radiation Therapy for Primary Liver Cancers: An ASTRO Clinical Practice Guideline. Pract. Radiat. Oncol. 2021. [Google Scholar] [CrossRef]
- Smart, A.C.; Goyal, L.; Horick, N.; Petkovska, N.; Zhu, A.X.; Ferrone, C.R.; Tanabe, K.K.; Allen, J.N.; Drapek, L.C.; Qadan, M.; et al. Hypofractionated Radiation Therapy for Unresectable/Locally Recurrent Intrahepatic Cholangiocarcinoma. Ann. Surg. Oncol. 2020, 27, 1122–1129. [Google Scholar] [CrossRef]
- Rizzo, A.; Ricci, A.D.; Brandi, G. IDH Inhibitors in Advanced Cholangiocarcinoma: Another Arrow in the Quiver? Cancer Treat Res. Commun. 2021, 27, 100356. [Google Scholar] [CrossRef]
- Abou-Alfa, G.K.; Sahai, V.; Hollebecque, A.; Vaccaro, G.; Melisi, D.; Al-Rajabi, R.; Paulson, A.S.; Borad, M.J.; Gallinson, D.; Murphy, A.G.; et al. Pemigatinib for Previously Treated, Locally Advanced or Metastatic Cholangiocarcinoma: A Multicentre, Open-Label, Phase 2 Study. Lancet Oncol. 2020, 21, 671–684. [Google Scholar] [CrossRef]
- Makawita, S.; Abou-Alfa, G.K.; Roychowdhury, S.; Sadeghi, S.; Borbath, I.; Goyal, L.; Cohn, A.; Lamarca, A.; Oh, D.-Y.; Macarulla, T.; et al. Infigratinib in Patients with Advanced Cholangiocarcinoma with Gene Fusions/translocations: The PROOF 301 Trial. Future Oncol. 2020, 16, 2375–2384. [Google Scholar] [CrossRef]
- Zhu, A.X.; Macarulla, T.; Javle, M.M.; Kelley, R.K.; Lubner, S.J.; Adeva, J.; Cleary, J.M.; Catenacci, D.V.T.; Borad, M.J.; Bridgewater, J.A.; et al. Final Overall Survival Efficacy Results of Ivosidenib for Patients with Advanced Cholangiocarcinoma with IDH1 Mutation: The Phase 3 Randomized Clinical ClarIDHy Trial. JAMA Oncol. 2021, 7, 1669–1677. [Google Scholar] [CrossRef] [PubMed]
- Javle, M.; Roychowdhury, S.; Kelley, R.K.; Sadeghi, S.; Macarulla, T.; Weiss, K.H.; Waldschmidt, D.-T.; Goyal, L.; Borbath, I.; El-Khoueiry, A.; et al. Infigratinib (BGJ398) in Previously Treated Patients with Advanced or Metastatic Cholangiocarcinoma with FGFR2 Fusions or Rearrangements: Mature Results from a Multicentre, Open-Label, Single-Arm, Phase 2 Study. Lancet Gastroenterol. Hepatol. 2021, 6, 803–815. [Google Scholar] [CrossRef]
- Rizzo, A.; Ricci, A.D.; Brandi, G. Futibatinib, an Investigational Agent for the Treatment of Intrahepatic Cholangiocarcinoma: Evidence to Date and Future Perspectives. Expert Opin. Investig. Drugs 2021, 30, 317–324. [Google Scholar] [CrossRef]
- Mazzaferro, V.; El-Rayes, B.F.; Droz Dit Busset, M.; Cotsoglou, C.; Harris, W.P.; Damjanov, N.; Masi, G.; Rimassa, L.; Personeni, N.; Braiteh, F.; et al. Derazantinib (ARQ 087) in Advanced or Inoperable FGFR2 Gene Fusion-Positive Intrahepatic Cholangiocarcinoma. Br. J. Cancer 2019, 120, 165–171. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Drilon, A.; Laetsch, T.W.; Kummar, S.; DuBois, S.G.; Lassen, U.N.; Demetri, G.D.; Nathenson, M.; Doebele, R.C.; Farago, A.F.; Pappo, A.S.; et al. Efficacy of Larotrectinib in TRK Fusion-Positive Cancers in Adults and Children. N. Engl. J. Med. 2018, 378, 731–739. [Google Scholar] [CrossRef]
- Kam, A.E.; Masood, A.; Shroff, R.T. Current and Emerging Therapies for Advanced Biliary Tract Cancers. Lancet Gastroenterol. Hepatol. 2021, 6, 956–969. [Google Scholar] [CrossRef]
- Komuta, M. Histological Heterogeneity of Primary Liver Cancers: Clinical Relevance, Diagnostic Pitfalls and the Pathologist’s Role. Cancers 2021, 13, 2871. [Google Scholar] [CrossRef]
- Hyman, D.M.; Puzanov, I.; Subbiah, V.; Faris, J.E.; Chau, I.; Blay, J.-Y.; Wolf, J.; Raje, N.S.; Diamond, E.L.; Hollebecque, A.; et al. Vemurafenib in Multiple Nonmelanoma Cancers with BRAF V600 Mutations. N. Engl. J. Med. 2015, 373, 726–736. [Google Scholar] [CrossRef]
- Oh, D.-Y.; Bang, Y.-J. HER2-Targeted Therapies—A Role beyond Breast Cancer. Nat. Rev. Clin. Oncol. 2020, 17, 33–48. [Google Scholar] [CrossRef]
- Le, D.T.; Durham, J.N.; Smith, K.N.; Wang, H.; Bartlett, B.R.; Aulakh, L.K.; Lu, S.; Kemberling, H.; Wilt, C.; Luber, B.S.; et al. Mismatch Repair Deficiency Predicts Response of Solid Tumors to PD-1 Blockade. Science 2017, 357, 409–413. [Google Scholar] [CrossRef] [Green Version]
- Thornblade, L.W.; Wong, P.; Li, D.; Warner, S.G.; Chang, S.; Raoof, M.; Kessler, J.; Amini, A.; Lin, J.; Chung, V.; et al. Patterns of Whole Exome Sequencing in Resected Cholangiocarcinoma. Cancers 2021, 13, 4062. [Google Scholar] [CrossRef]
- Bezrookove, V.; Patino, J.M.; Nosrati, M.; Desprez, P.-Y.; McAllister, S.; Soroceanu, L.; Baron, A.; Osorio, R.; Kashani-Sabet, M.; Dar, A.A. Niraparib Suppresses Cholangiocarcinoma Tumor Growth by Inducing Oxidative and Replication Stress. Cancers 2021, 13, 4405. [Google Scholar] [CrossRef]
- Mosbeh, A.; Halfawy, K.; Abdel-Mageed, W.S.; Sweed, D.; Rahman, M.H.A. Nuclear BAP1 Loss Is Common in Intrahepatic Cholangiocarcinoma and a Subtype of Hepatocellular Carcinoma but Rare in Pancreatic Ductal Adenocarcinoma. Cancer Genet. 2018, 224–225, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Rizzo, A.; Ricci, A.D.; Brandi, G. Recent Advances of Immunotherapy for Biliary Tract Cancer. Expert Rev. Gastroenterol. Hepatol. 2021, 15, 527–536. [Google Scholar] [CrossRef]
- Kobayashi, M.; Sakabe, T.; Abe, H.; Tanii, M.; Takahashi, H.; Chiba, A.; Yanagida, E.; Shibamoto, Y.; Ogasawara, M.; Tsujitani, S.-I.; et al. Dendritic Cell-Based Immunotherapy Targeting Synthesized Peptides for Advanced Biliary Tract Cancer. J. Gastrointest. Surg. 2013, 17, 1609–1617. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, K.; Kotera, Y.; Aruga, A.; Takeshita, N.; Takasaki, K.; Yamamoto, M. Clinical Utilization of Postoperative Dendritic Cell Vaccine plus Activated T-Cell Transfer in Patients with Intrahepatic Cholangiocarcinoma. J. Hepatobiliary Pancreat. Sci. 2012, 19, 171–178. [Google Scholar] [CrossRef]
- Liu, Y.; Guo, Y.; Wu, Z.; Feng, K.; Tong, C.; Wang, Y.; Dai, H.; Shi, F.; Yang, Q.; Han, W. Anti-EGFR Chimeric Antigen Receptor-Modified T Cells in Metastatic Pancreatic Carcinoma: A Phase I Clinical Trial. Cytotherapy 2020, 22, 573–580. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Chen, M.; Wu, Z.; Tong, C.; Dai, H.; Guo, Y.; Liu, Y.; Huang, J.; Lv, H.; Luo, C.; et al. CD133-Directed CAR T Cells for Advanced Metastasis Malignancies: A Phase I Trial. Oncoimmunology 2018, 7, e1440169. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vaddepally, R.K.; Kharel, P.; Pandey, R.; Garje, R.; Chandra, A.B. Review of Indications of FDA-Approved Immune Checkpoint Inhibitors per NCCN Guidelines with the Level of Evidence. Cancers 2020, 12, 738. [Google Scholar] [CrossRef] [Green Version]
- Le, D.T.; Uram, J.N.; Wang, H.; Bartlett, B.R.; Kemberling, H.; Eyring, A.D.; Skora, A.D.; Luber, B.S.; Azad, N.S.; Laheru, D.; et al. PD-1 Blockade in Tumors with Mismatch-Repair Deficiency. N. Engl. J. Med. 2015, 372, 2509–2520. [Google Scholar] [CrossRef] [Green Version]
- Piha-Paul, S.A.; Oh, D.-Y.; Ueno, M.; Malka, D.; Chung, H.C.; Nagrial, A.; Kelley, R.K.; Ros, W.; Italiano, A.; Nakagawa, K.; et al. Efficacy and Safety of Pembrolizumab for the Treatment of Advanced Biliary Cancer: Results from the KEYNOTE-158 and KEYNOTE-028 Studies. Int. J. Cancer 2020, 147, 2190–2198. [Google Scholar] [CrossRef] [PubMed]
- Kim, R.D.; Chung, V.; Alese, O.B.; El-Rayes, B.F.; Li, D.; Al-Toubah, T.E.; Schell, M.J.; Zhou, J.-M.; Mahipal, A.; Kim, B.H.; et al. A Phase 2 Multi-Institutional Study of Nivolumab for Patients with Advanced Refractory Biliary Tract Cancer. JAMA Oncol. 2020, 6, 888–894. [Google Scholar] [CrossRef]
- Sahai, V.; Griffith, K.A.; Beg, M.S.; Shaib, W.L.; Mahalingam, D.; Zhen, D.B.; Deming, D.A.; Dey, S.; Mendiratta-Lala, M.; Zalupski, M. A Multicenter Randomized Phase II Study of Nivolumab in Combination with Gemcitabine/cisplatin or Ipilimumab as First-Line Therapy for Patients with Advanced Unresectable Biliary Tract Cancer (BilT-01). J. Clin. Oncol. 2020, 38, 4582. [Google Scholar] [CrossRef]
- Feng, K.; Liu, Y.; Zhao, Y.; Yang, Q.; Dong, L.; Liu, J.; Li, X.; Zhao, Z.; Mei, Q.; Han, W. Efficacy and Biomarker Analysis of Nivolumab plus Gemcitabine and Cisplatin in Patients with Unresectable or Metastatic Biliary Tract Cancers: Results from a Phase II Study. J. Immunother. Cancer 2020, 8, e000367. [Google Scholar] [CrossRef]
- Lauterio, A.; De Carlis, R.; Centonze, L.; Buscemi, V.; Incarbone, N.; Vella, I.; De Carlis, L. Current Surgical Management of Peri-Hilar and Intra-Hepatic Cholangiocarcinoma. Cancers 2021, 13, 3657. [Google Scholar] [CrossRef]

| Small Duct Type | Large Duct Type | |
|---|---|---|
| Morphology | Mass-forming | Periductal (±mass-forming) or intraductal growing |
| Histology | Small, tubular or acinar adenocarcinoma with nodular growth, invasive into liver parenchyma and minimal mucin production | Large intrahepatic bile ducts, mucin-producing columnar tumor cells arranged in a large ductal or papillary architecture |
| Precancerous lesions | None | Biliary epithelial neoplasia, IPNB, ITPN, mucinous cystic neoplasm |
| Predisposing Diseases | Hepatitis, cirrhosis | PSC, biliary helminthosis, concrements |
| Mutations Fusions Amplifications | BAP1, BRAF, ARID1A, KRAS, TP53, SMAD4, IDH1/2, FGFR2 fusion | BRCA-1/2-Mut; Her-2-Amp; MSI-high |
| Trial ID | Protocol | Status | Estimated Enrollment | Estimated Study Completion |
|---|---|---|---|---|
| NCT04361331Huang XiaoyongShanghai | Toripalimab (PD1)+Lenvatinib vs. Gemox+Lenvatinib in for nonesectable intrahepatic cholangiocarcinoma | recruiting | 60 | December 2021 |
| NCT02170090 University Medical Center Hamburg, Germany | Adjuvant Chemotherapy With Gemcitabine and Cisplatin Compared to Standard of Care After Curative Intent Resection of Biliary Tract Cancer (ACTICCA-1) | recruiting | 781 | April 2022 |
| NCT03230318 Mayo Clinic Phoenix, Arizona, United States | Derazantinib in Subjects With FGFR2 Gene Fusion-, Mutation- or Amplification- Positive Inoperable or Advanced Intrahepatic Cholangiocarcinoma | recruiting | 143 | June 2022 |
| NCT04057365 Massachusetts General Hospital, USA | Study of the Combination of DKN-01 and Nivolumab in Previously Treated Patients With Advanced Biliary Tract Cancer (BTC) | recruiting | 30 | August 2022 |
| NCT04961788 Shanghai Zhongshan Hospital | Anti-PD1 Antibody Toripalimab Combined With Gemox as First-line Therapy in Late-stage Intrahepatic Cholangiocarcinoma | recruiting | 30 | December 2022 |
| NCT04961788; Shanghai Zhongshan Hospital | PD1 Antibody (Toripalimab), GEMOX and Lenvatinib vs. no neoadjuvant chemotherapy for resectable intrahepatic cholangiocarcinoma With High-risk Recurrence Factors | recruiting | 128 | August 2023 |
| NCT05052099 University Hospital, Essen Germany | Phase Ib/II Single-arm Study of mFOLFOX6, Bevacizumab and Atezolizumab in Advanced Biliary Tract Cancer (COMBATBIL) | recruiting | 35 | June 2024 |
| NCT04989218 University of Alabama at Birmingham | Durvalumab and Tremelimumab With Platinum-based Chemotherapy in Intrahepatic Cholangiocarcinoma (ICC) | not yet recruiting | 20 | October 2024 |
| NCT04301778 Sidney Kimmel Comprehensive Cancer Center Baltimore, United States | Durvalumab in Combination With a CSF-1R Inhibitor (SNDX-6532) Following Chemo or Radio-Embolization for Patients With Intrahepatic Cholangiocarcinoma | recruiting | 30 | September 2025 |
| NCT03673072 Krankenhaus Nordwest, Frankfurt Germany | Neoadjuvant Chemotherapy With Gemcitabine Plus Cisplatin Followed by Radical Liver Resection Versus Immediate Radical Liver Resection Alone With or Without Adjuvant Chemotherapy in in Front of Radical Resection of BTC (GAIN) | recruiting | 300 | November 2024 |
| Molecular Alteration | Frequency (%) | Reference | |
|---|---|---|---|
| Authorized targeting drug available | FGFR2 translocation | 15–18 | Komuta et al. [120] |
| IDH1/2 | 10–15 | Javle et al. [115] | |
| BRAF V600E | 3–6 | Hyman et al. [121] | |
| ERBB2 | 2–3 | Oh and Bang et al. [122] | |
| MSI-H | 1–2 | Le et al. [123] | |
| NTRK1-3 | <1 | Kam et al. [119] | |
| NRG1 | <1 | Kam et al. [119] | |
| Authorized targeting drug not available | TP53 mutation | 20–30 | Thornblade et al. [124] |
| RAS mutation | 10–20 | Thornblade et al. [124] | |
| ARID1A | 5–15 | Bezrookove et al. [125] | |
| BAP1 | 5–15 | Moshbeh et al. [126] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krenzien, F.; Nevermann, N.; Krombholz, A.; Benzing, C.; Haber, P.; Fehrenbach, U.; Lurje, G.; Pelzer, U.; Pratschke, J.; Schmelzle, M.; et al. Treatment of Intrahepatic Cholangiocarcinoma—A Multidisciplinary Approach. Cancers 2022, 14, 362. https://doi.org/10.3390/cancers14020362
Krenzien F, Nevermann N, Krombholz A, Benzing C, Haber P, Fehrenbach U, Lurje G, Pelzer U, Pratschke J, Schmelzle M, et al. Treatment of Intrahepatic Cholangiocarcinoma—A Multidisciplinary Approach. Cancers. 2022; 14(2):362. https://doi.org/10.3390/cancers14020362
Chicago/Turabian StyleKrenzien, Felix, Nora Nevermann, Alina Krombholz, Christian Benzing, Philipp Haber, Uli Fehrenbach, Georg Lurje, Uwe Pelzer, Johann Pratschke, Moritz Schmelzle, and et al. 2022. "Treatment of Intrahepatic Cholangiocarcinoma—A Multidisciplinary Approach" Cancers 14, no. 2: 362. https://doi.org/10.3390/cancers14020362
APA StyleKrenzien, F., Nevermann, N., Krombholz, A., Benzing, C., Haber, P., Fehrenbach, U., Lurje, G., Pelzer, U., Pratschke, J., Schmelzle, M., & Schöning, W. (2022). Treatment of Intrahepatic Cholangiocarcinoma—A Multidisciplinary Approach. Cancers, 14(2), 362. https://doi.org/10.3390/cancers14020362








