Assessment of Treatment Response after Pressurized Intra-Peritoneal Aerosol Chemotherapy (PIPAC) for Appendiceal Peritoneal Metastases
Abstract
:Simple Summary
Abstract
1. Introduction
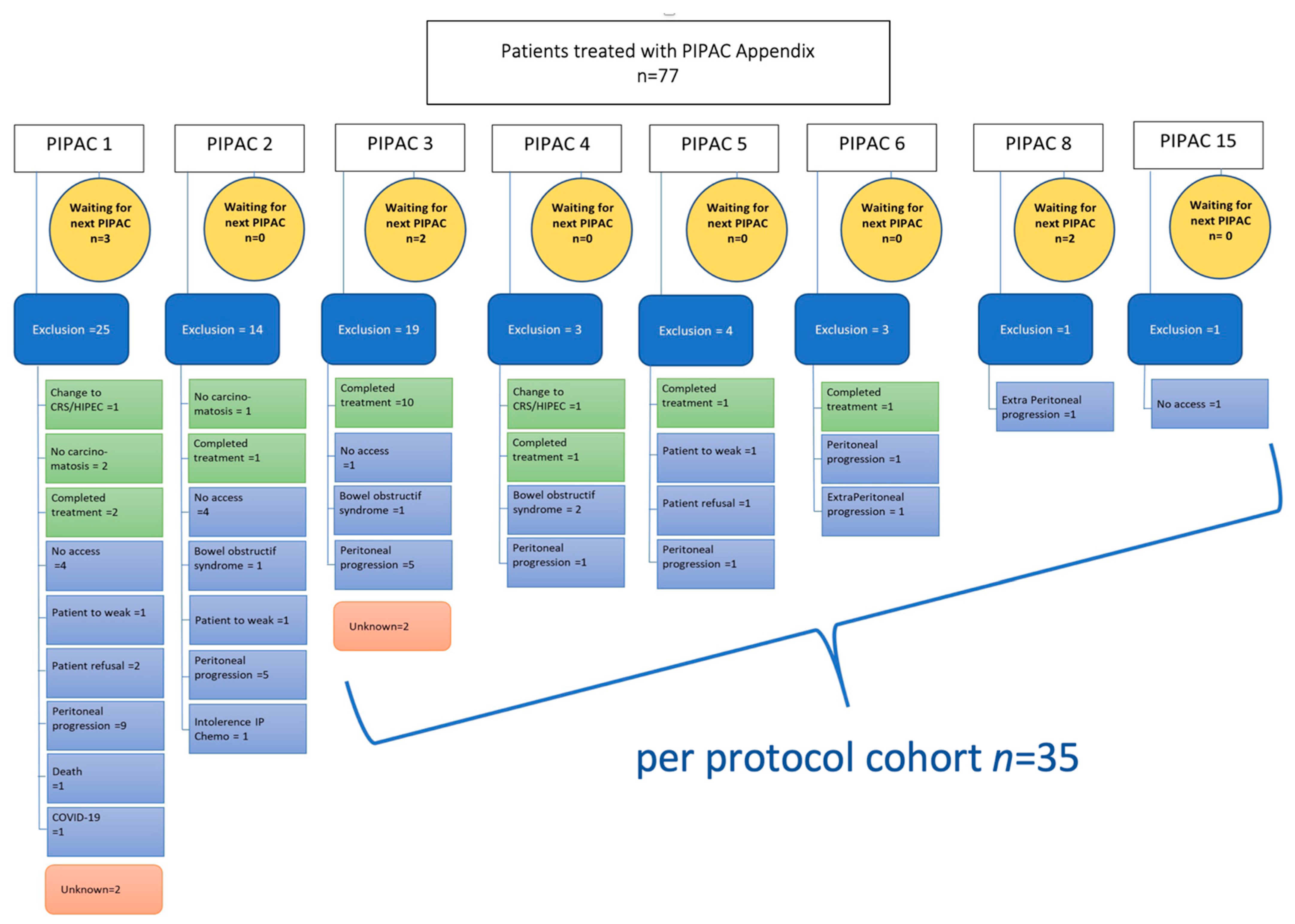
2. Materials and Methods
2.1. Pressurized IntraPeritoneal Aerosol Chemotherapy
2.2. Outcomes Measures
2.3. Statistics
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| PRGS | Peritoneal regression grading system |
| PIPAC | Pressurized IntraPeritoneal Aerosol Chemotherapy |
| PM | Peritoneal Metastasis |
| RECIST | Response Evaluation Criteria in Solid Tumors, |
| OS | overall survival |
| PCI | Peritoneal Cancer Index. |
References
- Votanopoulos, K.I.; Shen, P.; Skardal, A.; Levine, E.A. Peritoneal Metastases from Appendiceal Cancer. Surg. Oncol. Clin. N. Am. 2018, 27, 551–561. [Google Scholar] [CrossRef] [PubMed]
- Tokunaga, R.; Xiu, J.; Johnston, C.; Goldberg, R.M.; Philip, P.A.; Seeber, A.; Naseem, M.; Lo, J.H.; Arai, H.; Battaglin, F.; et al. Molecular Profiling of Appendiceal Adenocarcinoma and Comparison with Right-sided and Left-sided Colorectal Cancer. Clin. Cancer Res. 2019, 25, 3096–3103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shaib, W.L.; Assi, R.; Shamseddine, A.; Alese, O.B.; Staley, C., 3rd; Memis, B.; Adsay, V.; Bekaii-Saab, T.; El-Rayes, B.F. Appendiceal Mucinous Neoplasms: Diagnosis and Management. Oncologist 2017, 22, 1107–1116. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olsen, I.H.; Holt, N.; Langer, S.W.; Hasselby, J.P.; Gronbaek, H.; Hillingso, J.; Mahmoud, M.; Ladekarl, M.; Iversen, L.H.; Kjaer, A.; et al. Goblet cell carcinoids: Characteristics of a Danish cohort of 83 patients. PLoS ONE 2015, 10, e0117627. [Google Scholar] [CrossRef]
- Palmer, K.; Weerasuriya, S.; Chandrakumaran, K.; Rous, B.; White, B.E.; Paisey, S.; Srirajaskanthan, R.; Ramage, J.K. Goblet Cell Adenocarcinoma of the Appendix: A Systematic Review and Incidence and Survival of 1225 Cases From an English Cancer Registry. Front. Oncol. 2022, 12, 915028. [Google Scholar] [CrossRef]
- Govaerts, K.; Lurvink, R.J.; De Hingh, I.; Van der Speeten, K.; Villeneuve, L.; Kusamura, S.; Kepenekian, V.; Deraco, M.; Glehen, O.; Moran, B.J.; et al. Appendiceal tumours and pseudomyxoma peritonei: Literature review with PSOGI/EURACAN clinical practice guidelines for diagnosis and treatment. Eur. J. Surg. Oncol. 2021, 47, 11–35. [Google Scholar] [CrossRef]
- Elias, D.; Gilly, F.; Boutitie, F.; Quenet, F.; Bereder, J.M.; Mansvelt, B.; Lorimier, G.; Dube, P.; Glehen, O. Peritoneal colorectal carcinomatosis treated with surgery and perioperative intraperitoneal chemotherapy: Retrospective analysis of 523 patients from a multicentric French study. J. Clin. Oncol. 2010, 28, 63–68. [Google Scholar] [CrossRef] [Green Version]
- Raghav, K.; Shen, J.P.; Jacome, A.A.; Guerra, J.L.; Scally, C.P.; Taggart, M.W.; Foo, W.C.; Matamoros, A.; Shaw, K.R.; Fournier, K.; et al. Integrated clinico-molecular profiling of appendiceal adenocarcinoma reveals a unique grade-driven entity distinct from colorectal cancer. Br. J. Cancer 2020, 123, 1262–1270. [Google Scholar] [CrossRef]
- Lu, P.; Fields, A.C.; Meyerhardt, J.A.; Davids, J.S.; Shabat, G.; Bleday, R.; Goldberg, J.E.; Nash, G.M.; Melnitchouk, N. Systemic chemotherapy and survival in patients with metastatic low-grade appendiceal mucinous adenocarcinoma. J. Surg. Oncol. 2019, 120, 446–451. [Google Scholar] [CrossRef]
- Tejani, M.A.; ter Veer, A.; Milne, D.; Ottesen, R.; Bekaii-Saab, T.; Benson, A.B., 3rd; Schrag, D.; Shibata, S.; Skibber, J.; Weiser, M.; et al. Systemic therapy for advanced appendiceal adenocarcinoma: An analysis from the NCCN Oncology Outcomes Database for colorectal cancer. J. Natl. Compr. Cancer Netw. 2014, 12, 1123–1130. [Google Scholar] [CrossRef]
- Lieu, C.H.; Lambert, L.A.; Wolff, R.A.; Eng, C.; Zhang, N.; Wen, S.; Rafeeq, S.; Taggart, M.; Fournier, K.; Royal, R.; et al. Systemic chemotherapy and surgical cytoreduction for poorly differentiated and signet ring cell adenocarcinomas of the appendix. Ann. Oncol. 2012, 23, 652–658. [Google Scholar] [CrossRef] [PubMed]
- Chua, T.C.; Moran, B.J.; Sugarbaker, P.H.; Levine, E.A.; Glehen, O.; Gilly, F.N.; Baratti, D.; Deraco, M.; Elias, D.; Sardi, A.; et al. Early- and long-term outcome data of patients with pseudomyxoma peritonei from appendiceal origin treated by a strategy of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. J. Clin. Oncol. 2012, 30, 2449–2456. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- El Halabi, H.; Gushchin, V.; Francis, J.; Athas, N.; Macdonald, R.; Nieroda, C.; Studeman, K.; Sardi, A. The role of cytoreductive surgery and heated intraperitoneal chemotherapy (CRS/HIPEC) in patients with high-grade appendiceal carcinoma and extensive peritoneal carcinomatosis. Ann. Surg. Oncol. 2012, 19, 110–114. [Google Scholar] [CrossRef] [PubMed]
- Solass, W.; Kerb, R.; Murdter, T.; Giger-Pabst, U.; Strumberg, D.; Tempfer, C.; Zieren, J.; Schwab, M.; Reymond, M.A. Intraperitoneal chemotherapy of peritoneal carcinomatosis using pressurized aerosol as an alternative to liquid solution: First evidence for efficacy. Ann. Surg. Oncol. 2014, 21, 553–559. [Google Scholar] [CrossRef]
- Grass, F.; Vuagniaux, A.; Teixeira-Farinha, H.; Lehmann, K.; Demartines, N.; Hubner, M. Systematic review of pressurized intraperitoneal aerosol chemotherapy for the treatment of advanced peritoneal carcinomatosis. Br. J. Surg. 2017, 104, 669–678. [Google Scholar] [CrossRef]
- Alyami, M.; Hubner, M.; Grass, F.; Bakrin, N.; Villeneuve, L.; Laplace, N.; Passot, G.; Glehen, O.; Kepenekian, V. Pressurised intraperitoneal aerosol chemotherapy: Rationale, evidence, and potential indications. Lancet Oncol. 2019, 20, e368–e377. [Google Scholar] [CrossRef]
- Lurvink, R.J.; Rovers, K.P.; Nienhuijs, S.W.; Creemers, G.J.; Burger, J.W.A.; de Hingh, I.H.J. Pressurized intraperitoneal aerosol chemotherapy with oxaliplatin (PIPAC-OX) in patients with colorectal peritoneal metastases-a systematic review. J. Gastrointest. Oncol. 2021, 12, S242–S258. [Google Scholar] [CrossRef]
- Nowacki, M.; Alyami, M.; Villeneuve, L.; Mercier, F.; Hubner, M.; Willaert, W.; Ceelen, W.; Reymond, M.; Pezet, D.; Arvieux, C.; et al. Multicenter comprehensive methodological and technical analysis of 832 pressurized intraperitoneal aerosol chemotherapy (PIPAC) interventions performed in 349 patients for peritoneal carcinomatosis treatment: An international survey study. Eur. J. Surg. Oncol. 2018, 44, 991–996. [Google Scholar] [CrossRef]
- Sgarbura, O.; Villeneuve, L.; Alyami, M.; Bakrin, N.; Torrent, J.J.; Eveno, C.; Hubner, M.; ISSPP PIPAC Study Group. Current practice of pressurized intraperitoneal aerosol chemotherapy (PIPAC): Still standardized or on the verge of diversification? Eur. J. Surg. Oncol. 2021, 47, 149–156. [Google Scholar] [CrossRef]
- Alyami, M.; Gagniere, J.; Sgarbura, O.; Cabelguenne, D.; Villeneuve, L.; Pezet, D.; Quenet, F.; Glehen, O.; Bakrin, N.; Passot, G. Multicentric initial experience with the use of the pressurized intraperitoneal aerosol chemotherapy (PIPAC) in the management of unresectable peritoneal carcinomatosis. Eur. J. Surg. Oncol. 2017, 43, 2178–2183. [Google Scholar] [CrossRef]
- Hubner, M.; Grass, F.; Teixeira-Farinha, H.; Pache, B.; Mathevet, P.; Demartines, N. Pressurized IntraPeritoneal Aerosol Chemotherapy—Practical aspects. Eur. J. Surg. Oncol. 2017, 43, 1102–1109. [Google Scholar] [CrossRef] [PubMed]
- Hubner, M.; Alyami, M.; Villeneuve, L.; Cortes-Guiral, D.; Nowacki, M.; So, J.; Sgarbura, O.; Abba, J.; Afifi, A.; Mortensen, M.B.; et al. Consensus guidelines for pressurized intraperitoneal aerosol chemotherapy: Technical aspects and treatment protocols. Eur. J. Surg. Oncol. 2022, 48, 789–794. [Google Scholar] [CrossRef] [PubMed]
- Girardot-Miglierina, A.; Clerc, D.; Alyami, M.; Villeneuve, L.; Sgarbura, O.; Reymond, M.-A.; Hübner, M.; on behalf of the ISSPP PIPAC Study Group. Consensus statement on safety measures for pressurized intraperitoneal aerosol chemotherapy. Pleura Peritoneum 2021, 6, 139–149. [Google Scholar] [CrossRef] [PubMed]
- Jacquet, P.; Sugarbaker, P.H. Clinical research methodologies in diagnosis and staging of patients with peritoneal carcinomatosis. Cancer Treat. Res. 1996, 82, 359–374. [Google Scholar] [CrossRef]
- Eisenhauer, E.A.; Therasse, P.; Bogaerts, J.; Schwartz, L.H.; Sargent, D.; Ford, R.; Dancey, J.; Arbuck, S.; Gwyther, S.; Mooney, M.; et al. New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1). Eur. J. Cancer 2009, 45, 228–247. [Google Scholar] [CrossRef]
- Solass, W.; Sempoux, C.; Carr, N.J.; Bibeau, F.; Neureiter, D.; Jager, T.; Di Caterino, T.; Brunel, C.; Klieser, E.; Fristrup, C.W.; et al. Reproducibility of the peritoneal regression grading score for assessment of response to therapy in peritoneal metastasis. Histopathology 2019, 74, 1014–1024. [Google Scholar] [CrossRef] [Green Version]
- Solass, W.; Sempoux, C.; Detlefsen, S.; Carr, N.J.; Bibeau, F. Peritoneal sampling and histological assessment of therapeutic response in peritoneal metastasis: Proposal of the Peritoneal Regression Grading Score (PRGS). Pleura Peritoneum 2016, 1, 99–107. [Google Scholar] [CrossRef]
- Teixeira Farinha, H.; Grass, F.; Kefleyesus, A.; Achtari, C.; Romain, B.; Montemurro, M.; Demartines, N.; Hubner, M. Impact of Pressurized Intraperitoneal Aerosol Chemotherapy on Quality of Life and Symptoms in Patients with Peritoneal Carcinomatosis: A Retrospective Cohort Study. Gastroenterol. Res. Pract. 2017, 2017, 4596176. [Google Scholar] [CrossRef]
- Marmor, S.; Portschy, P.R.; Tuttle, T.M.; Virnig, B.A. The rise in appendiceal cancer incidence: 2000–2009. J. Gastrointest. Surg. 2015, 19, 743–750. [Google Scholar] [CrossRef]
- Levine, E.A.; Votanopoulos, K.I.; Shen, P.; Russell, G.; Fenstermaker, J.; Mansfield, P.; Bartlett, D.; Stewart, J.H. A Multicenter Randomized Trial to Evaluate Hematologic Toxicities after Hyperthermic Intraperitoneal Chemotherapy with Oxaliplatin or Mitomycin in Patients with Appendiceal Tumors. J. Am. Coll. Surg. 2018, 226, 434–443. [Google Scholar] [CrossRef]
- Hissong, E.; Yantiss, R.K. The Frontiers of Appendiceal Controversies: Mucinous Neoplasms and Pseudomyxoma Peritonei. Am. J. Surg. Pathol. 2022, 46, e27–e42. [Google Scholar] [CrossRef] [PubMed]
- Kelly, K.J. Management of Appendix Cancer. Clin. Colon Rectal. Surg. 2015, 28, 247–255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Franko, J.; Le, V.H.; Tee, M.C.; Lin, M.; Sedinkin, J.; Raman, S.; Frankova, D. Signet ring cell carcinoma of the gastrointestinal tract: National trends on treatment effects and prognostic outcomes. Cancer Treat. Res. Commun. 2021, 29, 100475. [Google Scholar] [CrossRef] [PubMed]
- Asare, E.A.; Compton, C.C.; Hanna, N.N.; Kosinski, L.A.; Washington, M.K.; Kakar, S.; Weiser, M.R.; Overman, M.J. The impact of stage, grade, and mucinous histology on the efficacy of systemic chemotherapy in adenocarcinomas of the appendix: Analysis of the National Cancer Data Base. Cancer 2016, 122, 213–221. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Uemura, M.; Qiao, W.; Fournier, K.; Morris, J.; Mansfield, P.; Eng, C.; Royal, R.E.; Wolff, R.A.; Raghav, K.; Mann, G.N.; et al. Retrospective study of nonmucinous appendiceal adenocarcinomas: Role of systemic chemotherapy and cytoreductive surgery. BMC Cancer 2017, 17, 331. [Google Scholar] [CrossRef] [Green Version]
- Shapiro, J.F.; Chase, J.L.; Wolff, R.A.; Lambert, L.A.; Mansfield, P.F.; Overman, M.J.; Ohinata, A.; Liu, J.; Wang, X.; Eng, C. Modern systemic chemotherapy in surgically unresectable neoplasms of appendiceal origin: A single-institution experience. Cancer 2010, 116, 316–322. [Google Scholar] [CrossRef] [PubMed]
- Cortes-Guiral, D.; Hubner, M.; Alyami, M.; Bhatt, A.; Ceelen, W.; Glehen, O.; Lordick, F.; Ramsay, R.; Sgarbura, O.; Van Der Speeten, K.; et al. Primary and metastatic peritoneal surface malignancies. Nat. Rev. Dis. Primers 2021, 7, 91. [Google Scholar] [CrossRef]
- Prabhu, A.; Brandl, A.; Wakama, S.; Sako, S.; Ishibashi, H.; Mizumoto, A.; Takao, N.; Noguchi, K.; Motoi, S.; Ichinose, M.; et al. Neoadjuvant Intraperitoneal Chemotherapy in Patients with Pseudomyxoma Peritonei—A Novel Treatment Approach. Cancers 2020, 12, 2212. [Google Scholar] [CrossRef]
- Sgarbura, O.; Eveno, C.; Alyami, M.; Bakrin, N.; Guiral, D.C.; Ceelen, W.; Delgadillo, X.; Dellinger, T.; Di Giorgio, A.; Kefleyesus, A.; et al. Consensus statement for treatment protocols in pressurized intraperitoneal aerosol chemotherapy (PIPAC). Pleura Peritoneum 2022, 7, 1–7. [Google Scholar] [CrossRef]
- Taibi, A.; Hubner, M.; Eveno, C.; Dumont, F.; Glehen, O.; Sgarbura, O. ASO Author Reflections: Is There Still a Role for Intraperitoneal Oxaliplatin for Colorectal Peritoneal Metastases? Ann. Surg. Oncol. 2022, 29, 5252–5253. [Google Scholar] [CrossRef]
- Moaven, O.; Perry, K.C.; Votanopoulos, K.I.; Shen, P.; Levine, E.A. ASO Author Reflections: Patient-Reported Outcomes of Mucinous Appendiceal Cancer Improve with Oxaliplatin HIPEC. Ann. Surg. Oncol. 2020, 27, 781–782. [Google Scholar] [CrossRef] [PubMed]
- Rubbia-Brandt, L.; Giostra, E.; Brezault, C.; Roth, A.D.; Andres, A.; Audard, V.; Sartoretti, P.; Dousset, B.; Majno, P.E.; Soubrane, O.; et al. Importance of histological tumor response assessment in predicting the outcome in patients with colorectal liver metastases treated with neo-adjuvant chemotherapy followed by liver surgery. Ann. Oncol. 2007, 18, 299–304. [Google Scholar] [CrossRef] [PubMed]


| Parameter | All Patients (n = 77) | PP Cohort | p Value | ||
|---|---|---|---|---|---|
| <3 PIPACs (n = 42) | ≥3 PIPACs (n = 35) | ||||
| Median Age (IQR) | 56.7 (47.1–66.2) | 56.8 (47.7–65.4) | 56.8 (47.0–66.6) | 0.999 | |
| Age group, n (%) | ≤30 | 2 (2.56) | 2 (4.76) | 0 (0) | 0.545 |
| 31–40 | 4 (5.13) | 1 (2.38) | 3 (8.57) | ||
| 41–50 | 19 (24.36) | 10 (23.81) | 9 (25.71) | ||
| 51–60 | 25 (32.05) | 15 (35.71) | 10 (28.57) | ||
| 61–70 | 15 (19.23) | 7 (16.67) | 8 (22.86) | ||
| >70 | 13 (16.67) | 8 (19.05) | 5 (14.29) | ||
| Gender, n (%) | Male | 37 (48.72) | 24 (57.14) | 13 (37.14) | 0.080 |
| Female | 40 (51.28) | 18 (42.86) | 22 (62.86) | ||
| Median BMI (kg/m2) (IQR) | 22.86 (20.32–25.66) | 23.15 (20.33–25.70) | 22.93 (20.78–25.39) | 0.934 | |
| ASA | 1 | 8 (12.9) | 4 (9.52) | 4 (11.43) | 0.149 |
| 2 | 30 (48.39) | 12 (28.57) | 18 (51.43) | ||
| 3 | 24 (38.71) | 16 (38.10) | 8 (22.86) | ||
| ECOG | 0 | 28 (43.08) | 15 (35.71) | 13 (37.14) | 0.749 |
| 1 | 25 (38.46) | 14 (33.33) | 11 (31.43) | ||
| 2 + 3 | 12 (18.42) | 6 (14.20) | 6 (17.14) | ||
| Pathology | Synchronous | 64 (85%) | 32 (80%) | 32 (91%) | 0.163 |
| Metachronous | 11 (15%) | 8 (20%) | 3 (91%) | ||
| Histology | G1 | 18 (33%) | 9 (32%) | 9 (33%) | 0.856 |
| G2 | 14 (25%) | 8 (29%) | 6 (22%) | ||
| G3 | 23 (42%) | 11 (39%) | 12 (44%) | ||
| RAS | No | 10 (33%) | 6 (43%) | 4 (25%) | 0.301 |
| Yes | 20 (67%) | 8 (57%) | 12 (75%) | ||
| Previous CRS + HIPEC | No | 63 (82%) | 31 (72%) | 32 (94%) | 0.013 |
| Yes | 14 (18%) | 12 (28%) | 2 (6%) | ||
| Previous CRS | No | 50 (65%) | 26 (60%) | 24 (71%) | 0.355 |
| Yes | 27 (35%) | 17 (40%) | 10 (29%) | ||
| Previous 1st chemo cycle | No | 9 (12%) | 5 (12%) | 4 (12%) | 0.985 |
| Yes | 68 (88%) | 38 (88%) | 30 (88%) | ||
| Oxaliplatin based | 51 (80%) | 29 (85%) | 22 (73%) | 0.663 | |
| Irinotecan based | 6 (9%) | 2 (6%) | 4 (13%) | ||
| Oxiri based | 5 (8%) | 2 (6%) | 3 (10%) | ||
| Biological therapy | 24 (38%) | 11 (32%) | 13 (43%) | 0.365 | |
| Total cycle (IQR) | 8 (6–12) | 8 (6–12) | 8 (6–12) | 0.818 | |
| Previous 2th chemo cycle | 32 (45%) | 15 (38%) | 17 (53%) | 0.217 | |
| Previous 3th chemo cycle | 9 (13%) | 5 (13%) | 4 (13%) | 0.983 | |
| Total cycles (IQR) | 11 (6–14) | 10 (6–14) | 12 (6–14) | 0.772 | |
| Bimodal (PIPAC + IV chemo) | 27 (35%) | 10 (24%) | 17 (49%) | 0.042 | |
| Median PCI at Baseline | 23 (14–30) | 23 (12–31) | 22 (16–28) | 0.948 | |
| Total cycles | ≤12 | 38 (76%) | 20 (71%) | 18 (82%) | 0.393 |
| >12 | 12 (24%) | 8 (29%) | 4 (18%) | ||
| Symptoms prePIPAC | No | 33 (43%) | 19 (45%) | 14 (40%) | 0.644 |
| Yes | 44 (57%) | 23 (55%) | 21 (60%) | ||
| Pain | No | 43 (61%) | 24 (65%) | 19 (56%) | 0.439 |
| Yes | 28 (39%) | 13 (35%) | 15 (44%) | ||
| Ascites | No | 54 (70%) | 27 (64%) | 27 (77%) | 0.220 |
| Yes | 23 (30%) | 15 (36%) | 8 (23%) | ||
| Dysphagia | No | 67 (97%) | 34 (94%) | 33 (100%) | 0.346 |
| Yes | 2 (3%) | 2 (6%) | 0 (0%) | ||
| Obstructive symptoms | No | 65 (92%) | 34 (92%) | 31 (91%) | 0.914 |
| Yes | 6 (8%) | 3 (8%) | 3 (9%) | ||
| Nausea | No | 60 (85%) | 30 (81%) | 30 (88%) | 0.405 |
| Yes | 11 (15%) | 7 (19%) | 4 (12%) | ||
| CEA (µg/l) (SD) | 26.4 ± 52.7 | 26.0 ± 53.6 | 26.7 ± 52.9 | 0.953 | |
| Ca19.9 (U/mL) (SD) | 291.4 ± 645.9 | 449.9 ± 823.6 | 101.2 ± 242.6 | 0.020 | |
| Ca125 (U/mL) (SD) | 109.3 ± 129.2 | 190.2 ± 134.1 | 28.3 ± 51.6 | 0.001 | |
| Creatinin (µmol/L) (SD) | 73.2 ± 22.6 | 71.6 ± 18.5 | 74.9 ± 26.7 | 0.524 | |
| Albumin (g/L) (SD) | 39.4 ± 9.7 | 39.9 ± 13.3 | 39 ± 4.4 | 0.706 | |
| Parameter | PP Cohort n = 35 | p Value | ||
|---|---|---|---|---|
| at Baseline | ≥3 PIPACs | |||
| RECIST | Regression/Stable | - | 15 (43%) | - |
| Progression | - | 5 (25%) | ||
| PRGS | 1–2 | - | 17 (49%) | - |
| 3–4 | - | 5 (25%) | ||
| Cytology | Positive | 7 (20%) | 3 (9%) | 0.606 |
| Negative | 28 (80%) | 32 (91%) | ||
| PCI | 24 (18–29) | 21 (18–28) | 0.104 | |
| ΔPCI (PIPAC1 vs. 3) | ≥3 decrease | - | 13 (37%) | 0.113 |
| <3 or increase | - | 18 (51%) | ||
| Any Symptoms | Yes | 21 (60%) | 18 (51%) | 0.873 |
| No | 14 (40%) | 17 (49%) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Somashekhar, S.; Abba, J.; Sgarbura, O.; Alyami, M.; Teixeira Farinha, H.; Rao, R.G.; Willaert, W.; Hübner, M., on behalf of the PIPAC Study Group. Assessment of Treatment Response after Pressurized Intra-Peritoneal Aerosol Chemotherapy (PIPAC) for Appendiceal Peritoneal Metastases. Cancers 2022, 14, 4998. https://doi.org/10.3390/cancers14204998
Somashekhar S, Abba J, Sgarbura O, Alyami M, Teixeira Farinha H, Rao RG, Willaert W, Hübner M on behalf of the PIPAC Study Group. Assessment of Treatment Response after Pressurized Intra-Peritoneal Aerosol Chemotherapy (PIPAC) for Appendiceal Peritoneal Metastases. Cancers. 2022; 14(20):4998. https://doi.org/10.3390/cancers14204998
Chicago/Turabian StyleSomashekhar, SP, Julio Abba, Olivia Sgarbura, Mohammad Alyami, Hugo Teixeira Farinha, Ramya G. Rao, Wouter Willaert, and Martin Hübner on behalf of the PIPAC Study Group. 2022. "Assessment of Treatment Response after Pressurized Intra-Peritoneal Aerosol Chemotherapy (PIPAC) for Appendiceal Peritoneal Metastases" Cancers 14, no. 20: 4998. https://doi.org/10.3390/cancers14204998
APA StyleSomashekhar, S., Abba, J., Sgarbura, O., Alyami, M., Teixeira Farinha, H., Rao, R. G., Willaert, W., & Hübner, M., on behalf of the PIPAC Study Group. (2022). Assessment of Treatment Response after Pressurized Intra-Peritoneal Aerosol Chemotherapy (PIPAC) for Appendiceal Peritoneal Metastases. Cancers, 14(20), 4998. https://doi.org/10.3390/cancers14204998







