A Mac-2 Binding Protein Glycosylation Isomer-Based Risk Model Predicts Hepatocellular Carcinoma in HBV-Related Cirrhotic Patients on Antiviral Therapy
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Methods
2.3. Definitions
2.4. Measurement of WFA-Positive M2BPGi
2.5. Serology
2.6. Statistical Analysis
3. Results
3.1. Comparison of Clinical Characteristics of All Patients with or without HCC Development
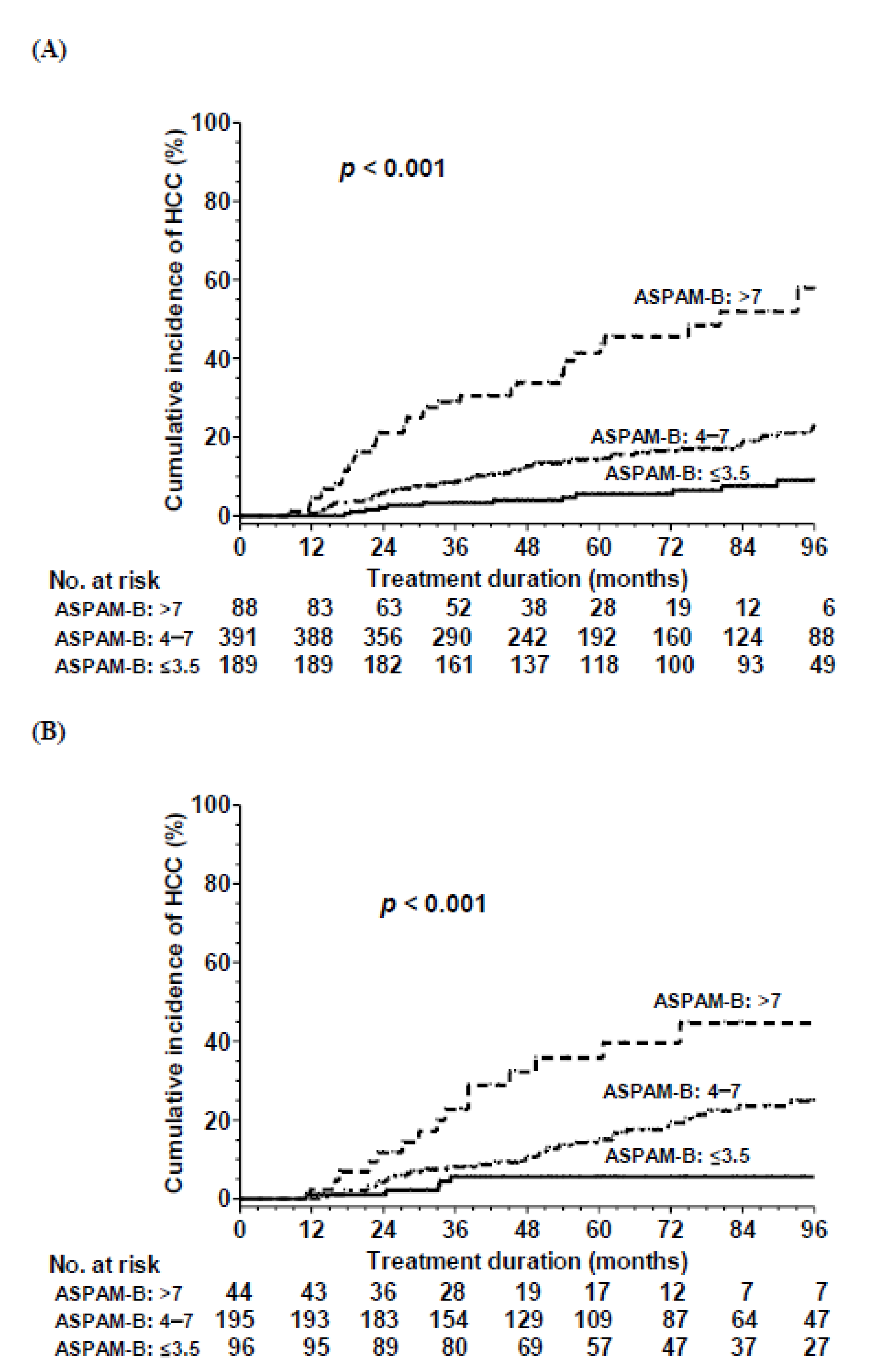
3.2. HCC Risk Predictors and Prediction Model of the Development Group
3.3. Validation of the HCC Risk Prediction Model
3.4. Comparisons of AUROC and C-Statistic between Different Prediction Models of HCC
3.5. Incidences and Predictors of Cirrhotic Events
3.6. Incidences and Predictors of Liver-Related Mortality or Liver Transplantation
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chang, T.-T.; Liaw, Y.-F.; Wu, S.-S.; Schiff, E.; Han, K.-H.; Lai, C.-L.; Safadi, R.; Lee, S.S.; Halota, W.; Goodman, Z.; et al. Long-term entecavir therapy results in the reversal of fibrosis/cirrhosis and continued histological improvement in patients with chronic hepatitis B. Hepatology 2010, 52, 886–893. [Google Scholar] [CrossRef] [PubMed]
- Marcellin, P.; Gane, E.; Buti, M.; Afdhal, N.; Sievert, W.; Jacobson, I.M.; Washington, M.K.; Germanidis, G.; Flaherty, J.F.; Schall, R.A.; et al. Regression of cirrhosis during treatment with tenofovir disoproxil fumarate for chronic hepatitis B: A 5-year open-label follow-up study. Lancet 2013, 381, 468–475. [Google Scholar] [CrossRef]
- Su, T.-H.; Hu, T.-H.; Chen, C.-Y.; Huang, Y.-W.; Chuang, W.-L.; Lin, C.-C.; Wang, C.-C.; Su, W.-W.; Chen, M.-Y.; Peng, C.-Y.; et al. Four-year entecavir therapy reduces hepatocellular carcinoma, cirrhotic events and mortality in chronic hepatitis B patients. Liver Int. 2016, 36, 1755–1764. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, M.H.; Yang, H.-I.; Le, A.; Henry, L.; Nguyen, N.; Lee, M.-H.; Zhang, J.; Wong, C.; Wong, C.; Trinh, H. Reduced Incidence of Hepatocellular Carcinoma in Cirrhotic and Noncirrhotic Patients with Chronic Hepatitis B Treated With Tenofovir—A Propensity Score–Matched Study. J. Infect. Dis. 2019, 219, 10–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Papatheodoridis, G.V.; Dalekos, G.N.; Sypsa, V.; Yurdaydin, C.; Buti, M.; Goulis, J.; Calleja, J.L.; Chi, H.; Manolakopoulos, S.; Mangia, G.; et al. PAGE-B predicts the risk of developing hepatocellular carcinoma in Caucasians with chronic hepatitis B on 5-year antiviral therapy. J. Hepatol. 2016, 64, 800–806. [Google Scholar] [CrossRef]
- Chen, C.H.; Lee, C.M.; Lai, H.C.; Hu, T.H.; Su, W.P.; Lu, S.N.; Lin, C.H.; Hung, C.H.; Wang, J.H.; Lee, M.H.; et al. Prediction model of hepatocellular carcinoma risk in Asian patients with chronic hepatitis B treated with entecavir. Oncotarget 2017, 8, 92431–92441. [Google Scholar] [CrossRef] [Green Version]
- Sohn, W.; Cho, J.-Y.; Kim, J.H.; Lee, J.I.; Kim, H.J.; Woo, M.-A.; Jung, S.-H.; Paik, Y.-H. Risk score model for the development of hepatocellular carcinoma in treatment-naïve patients receiving oral antiviral treatment for chronic hepatitis B. Clin. Mol. Hepatol. 2017, 23, 170–178. [Google Scholar] [CrossRef]
- Hsu, Y.-C.; Yip, T.C.-F.; Ho, H.J.; Wong, V.W.-S.; Huang, Y.-T.; El-Serag, H.B.; Lee, T.-Y.; Wu, M.-S.; Lin, J.-T.; Wong, G.L.-H.; et al. Development of a scoring system to predict hepatocellular carcinoma in Asians on antivirals for chronic hepatitis B. J. Hepatol. 2018, 69, 278–285. [Google Scholar] [CrossRef]
- Kim, J.H.; Kim, Y.D.; Lee, M.; Jun, B.G.; Kim, T.S.; Suk, K.T.; Kang, S.H.; Kim, M.Y.; Cheon, G.J.; Kim, D.J.; et al. Modified PAGE-B score predicts the risk of hepatocellular carcinoma in Asians with chronic hepatitis B on antiviral therapy. J. Hepatol. 2018, 69, 1066–1073. [Google Scholar] [CrossRef]
- Yu, J.H.; Suh, Y.J.; Jin, Y.-J.; Heo, N.-Y.; Jang, J.W.; You, C.R.; An, H.Y.; Lee, J.-W. Prediction model for hepatocellular carcinoma risk in treatment-naive chronic hepatitis B patients receiving entecavir/tenofovir. Eur. J. Gastroenterol. Hepatol. 2019, 31, 865–872. [Google Scholar] [CrossRef]
- Yang, H.-I.; Yeh, M.-L.; Wong, G.L.-H.; Peng, C.-Y.; Chen, C.-H.; Trinh, H.N.; Cheung, K.-S.; Xie, Q.; Su, T.-H.; Kozuka, R.; et al. Real-World Effectiveness from the Asia Pacific Rim Liver Consortium for HBV Risk Score for the Prediction of Hepatocellular Carcinoma in Chronic Hepatitis B Patients Treated with Oral Antiviral Therapy. J. Infect. Dis. 2020, 221, 389–399. [Google Scholar] [CrossRef] [PubMed]
- Fan, R.; Papatheodoridis, G.; Sun, J.; Innes, H.; Toyoda, H.; Xie, Q.; Mo, S.; Sypsa, V.; Guha, I.N.; Kumada, T.; et al. aMAP risk score predicts hepatocellular carcinoma development in patients with chronic hepatitis. J. Hepatol. 2020, 73, 1368–1378. [Google Scholar] [CrossRef] [PubMed]
- Ahn, S.B.; Choi, J.; Jun, D.W.; Oh, H.; Yoon, E.L.; Kim, H.S.; Jeong, S.W.; Kim, S.E.; Shim, J.; Cho, Y.K.; et al. Twelve-month post-treatment parameters are superior in predicting hepatocellular carcinoma in patients with chronic hepatitis B. Liver Int. 2021, 41, 1652–1661. [Google Scholar] [CrossRef] [PubMed]
- Poh, Z.; Shen, L.; Yang, H.-I.; Seto, W.-K.; Wong, V.W.; Lin, C.Y.; Goh, B.-B.G.; Chang, P.-E.J.; Chan, H.L.-Y.; Yuen, M.-F.; et al. Real-world risk score for hepatocellular carcinoma (RWS-HCC): A clinically practical risk predictor for HCC in chronic hepatitis B. Gut 2016, 65, 887–888. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.-S.; Yu, X.; Kramer, J.; Thrift, A.P.; Richardson, P.; Hsu, Y.-C.; Flores, A.; El-Serag, H.B.; Kanwal, F. Comparative performance of risk prediction models for hepatitis B-related hepatocellular carcinoma in the United States. J. Hepatol. 2020, 76, 294–301. [Google Scholar] [CrossRef] [PubMed]
- Tamaki, N.; Kurosaki, M.; Loomba, R.; Izumi, A.N. Clinical Utility of Mac-2 Binding Protein Glycosylation Isomer in Chronic Liver Diseases. Ann. Lab. Med. 2021, 41, 16–24. [Google Scholar] [CrossRef]
- Ishii, A.; Nishikawa, H.; Enomoto, H.; Iwata, Y.; Kishino, K.; Shimono, Y.; Hasegawa, K.; Nakano, C.; Takata, R.; Nishimura, T.; et al. Clinical implications of serum Wisteria floribunda agglutinin-positive Mac-2-binding protein in treatment-naive chronic hepatitis B. Hepatol. Res. 2017, 47, 204–215. [Google Scholar] [CrossRef]
- Ichikawa, Y.; Joshita, S.; Umemura, T.; Shobugawa, Y.; Usami, Y.; Shibata, S.; Yamazaki, T.; Fujimori, N.; Komatsu, M.; Matsumoto, A.; et al. Serum Wisteria floribunda agglutinin-positive human Mac-2 binding protein may predict liver fibrosis and progression to hepatocellular carcinoma in patients with chronic hepatitis B virus infection. Hepatol. Res. 2017, 47, 226–233. [Google Scholar] [CrossRef] [Green Version]
- Kawaguchi, K.; Honda, M.; Ohta, H.; Terashima, T.; Shimakami, T.; Arai, K.; Yamashita, T.; Sakai, Y.; Yamashita, T.; Mizukoshi, E.; et al. Serum Wisteria floribunda agglutinin-positive Mac-2 binding protein predicts hepatocellular carcinoma incidence and recurrence in nucleos(t)ide analogue therapy for chronic hepatitis B. J. Gastroenterol. 2018, 53, 740–751. [Google Scholar] [CrossRef]
- Shinkai, N.; Nojima, M.; Iio, E.; Matsunami, K.; Toyoda, H.; Murakami, S.; Inoue, T.; Ogawa, S.; Kumada, T.; Tanaka, Y. High levels of serum Mac-2-binding protein glycosylation isomer (M2BPGi) predict the development of hepatocellular carcinoma in hepatitis B patients treated with nucleot(s)ide analogues. J. Gastroenterol. 2018, 53, 883–889. [Google Scholar] [CrossRef]
- Toyoda, H.; Kumada, T.; Tada, T.; Kaneoka, Y.; Maeda, A.; Korenaga, M.; Mizokami, M.; Narimatsu, H. Serum WFA+ -M2BP levels as a prognostic factor in patients with early hepatocellular carcinoma undergoing curative resection. Liver Int. 2016, 36, 293–301. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.S.; Kim, S.U.; Kim, B.K.; Park, J.Y.; Kim, D.Y.; Ahn, S.H.; Han, K.H.; Park, Y.N.; Han, D.H.; Kim, K.S.; et al. Serum Wisteria floribunda agglutinin-positive human Mac-2 binding protein level predicts recurrence of hepatitis B virus-related hepatocellular carcinoma after curative resection. Clin. Mol. Hepatol. 2020, 26, 33–44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marrero, J.A.; Kulik, L.M.; Sirlin, C.B.; Zhu, A.X.; Finn, R.S.; Abecassis, M.M.; Roberts, L.R.; Heimbach, J.K. Diagnosis, Staging, and Management of Hepatocellular Carcinoma: 2018 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology 2018, 68, 723–750. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Handelsman, Y.; Bloomgarden, Z.T.; Grunberger, G.; Umpierrez, G.; Zimmerman, R.S.; Bailey, T.S.; Blonde, L.; Bray, G.A.; Cohen, A.J.; Dagogo-Jack, S.; et al. American Association of Clinical Endocrinologists and American College of Endocrinology- clinical practice guidelines for developing a diabetes mellitus comprehensive care plan- 2015. Endocr. Pract. 2015, 21 (Suppl. 1), 1–87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuno, A.; Ikehara, Y.; Tanaka, Y.; Ito, K.; Matsuda, A.; Sekiya, S.; Hige, S.; Sakamoto, M.; Kage, M.; Mizokami, M.; et al. A serum “sweet-doughnut” protein facilitates fibrosis evaluation and therapy assessment in patients with viral hepatitis. Sci. Rep. 2013, 3, 1065. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seto, W.-K.; Wong, D.K.-H.; Fung, J.; Huang, F.-Y.; Liu, K.S.-H.; Lai, C.-L.; Yuen, M.-F. Linearized hepatitis B surface antigen and hepatitis B core-related antigen in the natural history of chronic hepatitis B. Clin. Microbiol. Infect. 2014, 20, 1173–1180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rubin, D.B.; Schenker, N. Multiple imputation in health-care databases: An overview and some applications. Stat. Med. 1991, 10, 585–598. [Google Scholar] [CrossRef]
- Sullivan, L.M.; Massaro, J.M.; D’Agostino, R.B., Sr. Presentation of multivariate data for clinical use: The Framingham Study risk score functions. Stat. Med. 2004, 23, 1631–1660. [Google Scholar] [CrossRef]
- Uno, H.; Cai, T.; Pencina, M.J.; D’Agostino, R.B.; Wei, L.J. On the C-statistics for evaluating overall adequacy of risk prediction procedures with censored survival data. Stat Med. 2011, 30, 1105–1117. [Google Scholar] [CrossRef] [Green Version]
- Blanche, P.; Dartigues, J.F.; Jacqmin-Gadda, H. Estimating and comparing time-dependent areas under receiver operating characteristic curves for censored event times with competing risks. Stat. Med. 2013, 32, 5381–5397. [Google Scholar] [CrossRef]
- Sharma, S.A.; Kowgier, M.; Hansen, B.E.; Brouwer, W.P.; Maan, R.; Wong, D.; Shah, H.; Khalili, K.; Yim, C.; Heathcote, E.J.; et al. Toronto HCC risk index: A validated scoring system to predict 10-year risk of HCC in patients with cirrhosis. J. Hepatol. 2018, 68, 92–99. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.Y.; Lampertico, P.; Nam, J.Y.; Lee, H.-C.; Kim, S.U.; Sinn, D.H.; Seo, Y.S.; Lee, H.A.; Park, S.Y.; Lim, Y.-S.; et al. An artificial intelligence model to predict hepatocellular carcinoma risk in Korean and Caucasian patients with chronic hepatitis B. J. Hepatol. 2022, 76, 311–318. [Google Scholar] [CrossRef] [PubMed]
- Qamar, A.A.; Grace, N.D.; Groszmann, R.J.; Garcia-Tsao, G.; Bosch, J.; Burroughs, A.K.; Maurer, R.; Planas, R.; Escorsell, A.; Garcia-Pagan, J.C.; et al. Platelet count is not a predictor of the presence or development of gastroesophageal varices in cirrhosis. Hepatology 2008, 47, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Ripoll, C.; Groszmann, R.J.; Garcia-Tsao, G.; Bosch, J.; Grace, N.; Burroughs, A.; Planas, R.; Escorsell, A.; Garcia-Pagan, J.C.; Makuch, R.; et al. Hepatic venous pressure gradient predicts development of hepatocellular carcinoma independently of severity of cirrhosis. J. Hepatol. 2009, 50, 923–928. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hosaka, T.; Suzuki, F.; Kobayashi, M.; Fujiyama, S.; Kawamura, Y.; Sezaki, H.; Akuta, N.; Suzuki, Y.; Saitoh, S.; Arase, Y.; et al. Impact of hepatitis B core-related antigen on the incidence of hepatocellular carcinoma in patients treated with nucleos(t)ide analogues. Aliment. Pharmacol. Ther. 2019, 49, 457–471. [Google Scholar] [CrossRef]


| Variables | HCC n = 183 | No HCC n = 820 | p Value |
|---|---|---|---|
| Age (year) | 58.1 ± 10.0 | 53.0 ± 12.0 | <0.001 |
| Sex, male | 147 (80.3%) | 599 (73.0%) | 0.041 |
| Entecavir versus TDF | 147 vs. 36 | 542 vs. 278 | <0.001 |
| HBeAg-positive status | 50 (27.3%) | 197 (24.0%) | 0.349 |
| Decompensation status | 49 (26.8%) | 140 (17.1%) | 0.002 |
| NA-naïve | 153 (83.6%) | 696 (84.9%) | 0.666 |
| Diabetes mellitus, yes | 45 (24.6%) | 176 (21.5%) | 0.356 |
| Hypertension, yes | 61 (33.3%) | 202 (24.6%) | 0.016 |
| HBV DNA, log10 IU/mL | 5.53 ± 1.52 | 5.40 ± 1.51 | 0.318 |
| AST, U/L | 119.1 ± 205.4 | 130.5 ± 269.8 | 0.589 |
| ALT, U/L | 134.2 ± 259.2 | 162.3 ± 362.8 | 0.321 |
| Total bilirubin, mg/dL | 2.09 ± 3.75 | 2.03 ± 3.78 | 0.854 |
| INR | 1.19 ± 0.22 | 1.19 ± 0.28 | 0.992 |
| Albumin, g/dL | 3.80 ± 0.64 | 4.02 ± 0.63 | <0.001 |
| Platelet, ×103/μL | 121.0 ± 56.0 | 138.7 ± 56.0 | <0.001 |
| AFP, ng/mL | 32.2 ± 82.3 | 30.2 ± 123.9 | 0.840 |
| M2BPGi, COI | 3.80 ± 3.98 | 2.77 ± 3.50 | <0.001 |
| HBcrAg, log10 U/mL | 5.33 ± 1.49 | 5.07 ± 1.48 | 0.034 |
| Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|
| Variables | HR (95% CI) | p Value | HR (95% CI) | p Value |
| Baseline | ||||
| Age (per year) | 1.034 (1.0180–1.056) | <0.001 | ||
| Sex, male vs. female | 1.458 (0.927–2.295) | 0.103 | 2.152 (1.352–3.425) | 0.001 |
| HBeAg, yes vs. no | 1.051 (0.705–1.566) | 0.808 | ||
| Decompensation, yes vs. no | 1.883 (1.263–2.810) | 0.002 | ||
| NA-naïve, yes vs. no | 0.843 (0.530–1.340) | 0.470 | ||
| TDF vs. entecavir | 0.634 (0.398–1.012) | 0.056 | ||
| Diabetes mellitus, yes vs. no | 1.238 (0.819–1.872) | 0.311 | ||
| Hypertension, yes vs. no | 1.662 (1.151–2.400) | 0.007 | ||
| HBV DNA, per log10 IU/mL | 0.959 (0.856–1.075) | 0.475 | ||
| AST, per U/L | 0.999 (0.998–1.000) | 0.212 | ||
| ALT, per U/L | 0.999 (0.999–1.000) | 0.120 | ||
| Total bilirubin, per mg/dL | 0.998 (0.955–1.044) | 0.944 | ||
| Albumin, per g/L | 0.627 (0.484–0.812) | <0.001 | ||
| INR, per ratio | 0.901 (0.464–1.750) | 0.758 | ||
| Platelet, per 103/μL | 0.993 (0.990–0.997) | <0.001 | ||
| AFP, per ng/mL | 1.001 (0.999–1.003) | 0.375 | ||
| M2BPGi, per COI | 1.054 (1.013–1.098) | 0.010 | ||
| HBcrAg, per log10 U/mL | 1.066 (0.942–1.206) | 0.312 | ||
| 12 months of treatment | ||||
| Age (year) | 1.034 (1.018–1.050) | <0.001 | 1.041 (1.024–1.057) | <0.001 |
| ALT < 40 U/L, per U/L | 0.685 (0.468–1.001) | 0.051 | ||
| AFP, per ng/mL | 1.009 (1.004–1.015) | <0.001 | 1.010 (1.005–1.016) | 0.003 |
| Platelet, per 103/μL | 0.992 (0.988–0.995) | <0.001 | 0.955 (0.991–0.999) | 0.019 |
| M2BPGi, per COI | 1.123 (1.069–1.180) | <0.001 | 1.099 (1.037–1.165) | 0.002 |
| HBcrAg, per log10 U/mL | 1.085 (0.941–1.252) | 0.262 | ||
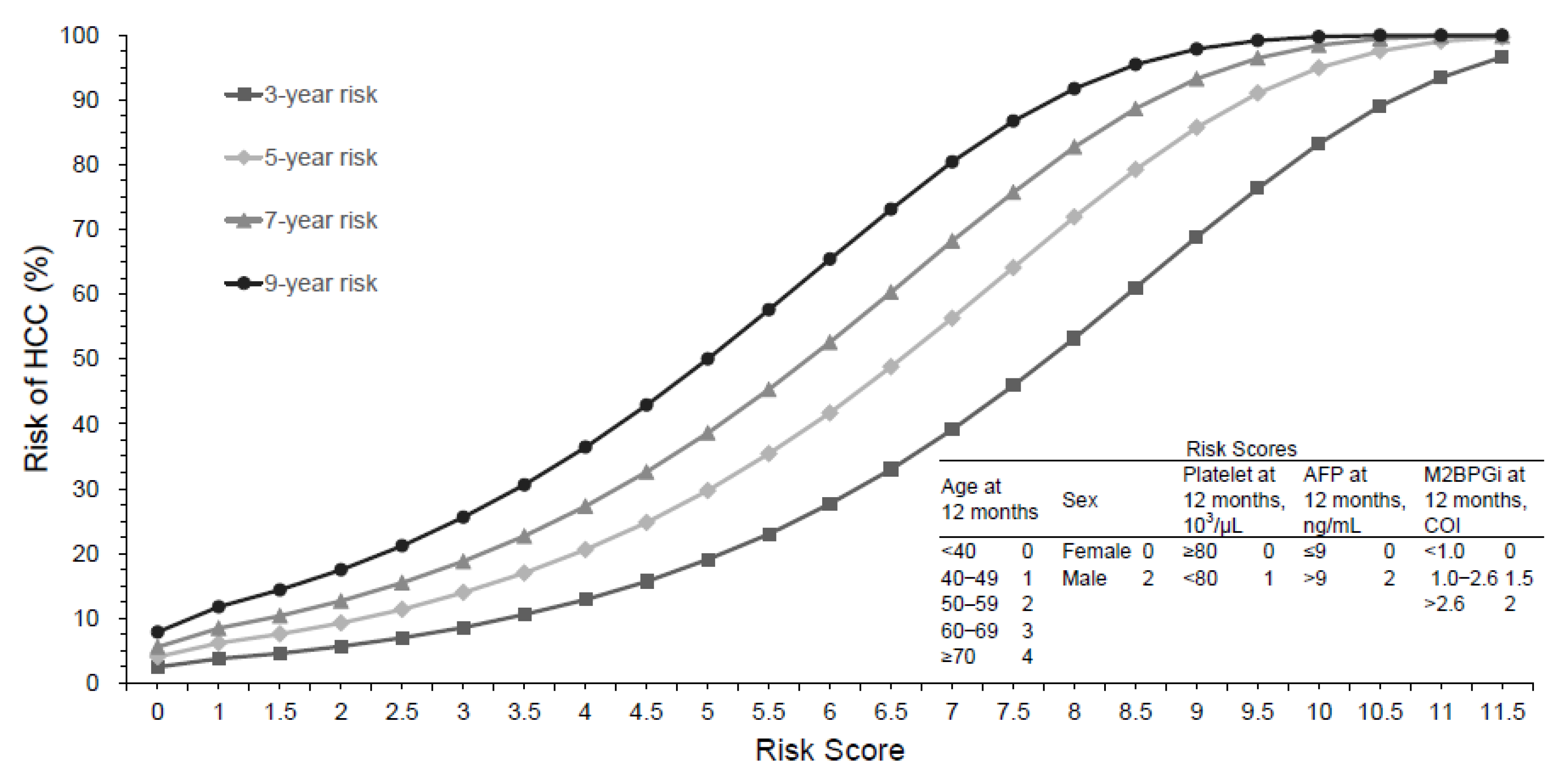
| Variables | HR (95% CI) | Parameter | p Value | Risk Scores |
|---|---|---|---|---|
| Age at 12 months, years <40 40–49 50–59 60–69 ≥70 | 1.532 (1.297–1.809) | 0.4265 | <0.0001 | 0 1 2 3 4 |
| Sex Female Male | 1.000 2.164 (1.356–3.452) | 0.7718 | 0.0012 | 0 2 |
| Platelet at 12 months, 103/μL ≥80 <80 | 1.000 1.779 (1.170–2.706) | 0.5760 | 0.0071 | 0 1.5 |
| AFP at 12 months, ng/mL ≤9 >9 | 1.000 2.264 (1.406–3.645) | 0.8170 | 0.0008 | 0 2 |
| M2BPGi at 12 months, COI <1.0 1.0–2.6 >2.6 | 1.000 1.904 (1.222–2.967) 2.163 (1.336–3.500) | 0.6441 0.7714 | 0.0044 0.0017 | 0 1.5 2 |
| ASPAM-B | APA-B | PAGE-B | RWS-HCC | AASL-HCC | THRI | |
|---|---|---|---|---|---|---|
| Development Cohort (n = 668) | AUROC (95% CI) | AUROC (95% CI) | AUROC (95% CI) | AUROC (95% CI) | AUROC (95% CI) | AUROC (95% CI) |
| 3 years | 0.742 (0.672–0.811) | 0.661 (0.588–0.734) | 0.673 (0.601–0.746) | 0.601 (0.525–0.677) | 0.677 (0.611–0.744) | 0.660 (0.590–0.731) |
| 5 years | 0.728 (0.668–0.788) | 0.669 (0.610–0.729) | 0.676 (0.616–0.736) | 0.604 (0.540–0.668) | 0.654 (0.594–0.714) | 0.663 (0.604–0.722) |
| 7 years | 0.721 (0.665–0.777) | 0.668 (0.612–0.724) | 0.667 (0.611–0.723) | 0.606 (0.546–0.665) | 0.644 (0.588–0.701) | 0.650 (0.593–0.706) |
| 9 years | 0.719 (0.666–0.772) | 0.667 (0.614–0.721) | 0.671 (0.617–0.724) | 0.614 (0.556–0.673) | 0.651 (0.598–0.704) | 0.656 (0.603–0.710) |
| Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|
| Variables | Hazard Ratio (95% CI) | p Value | Hazard Ratio (95% CI) | p Value |
| Baseline | ||||
| Age (year) | 1.005 (0.980–1.031) | 0.680 | ||
| Sex, male vs. female | 1.162 (0.574–2.353) | 0.677 | ||
| HBeAg, yes vs. no | 1.087 (0.560–2.111) | 0.805 | ||
| NA-naïve, yes vs. no | 2.592 (0.802–8.372) | 0.111 | ||
| TDF vs. entecavir | 1.030 (0.534–1.986) | 0.930 | ||
| Diabetes mellitus, yes vs. no | 1.101 (0.544–2.229) | 0.789 | ||
| Hypertension, yes vs. no | 1.284 (0.680–2.422) | 0.441 | ||
| HBV DNA, per log10 IU/mL | 0.965 (0.790–1.179) | 0.729 | ||
| AST, per U/L | 1.000 (0.999–1.002) | 0.614 | ||
| ALT, per U/L | 0.998 (0.994–1.001) | 0.215 | ||
| Total bilirubin, per mg/dL | 1.068 (0.844–1.353) | 0.582 | ||
| Albumin, per g/L | 0.262 (0.154–0.448) | <0.001 | ||
| INR, per ratio | 1.328 (0.412–4.288) | 0.635 | ||
| Platelet, per 103/μL | 0.983 (0.976–0.990) | <0.001 | ||
| AFP at baseline, per ng/mL | 0.996 (0.985–1.006) | 0.412 | ||
| M2BPGi, per COI | 1.180 (1.082–1.288) | <0.001 | ||
| HBcrAg, per log10 U/mL | 0.987 (0.804–1.211) | 0.900 | ||
| 12 months of treatment | ||||
| ALT < 40 U/L, per U/L | 0.536 (0.292–0.984) | 0.044 | ||
| AFP, per ng/mL | 1.011 (1.002–1.020) | 0.016 | ||
| Platelet, per 103/μL | 0.980 (0.973–0.987) | <0.001 | 0.986 (0.979–0.994) | 0.001 |
| Albumin, per g/L | 0.280 (0.197–0.398) | <0.001 | 0.439 (0.283–0.679) | <0.001 |
| M2BPGi, per COI | 1.349 (1.241–1.466) | <0.001 | 1.135(1.026–1.256) | 0.014 |
| HBcrAg, per log10 U/mL | 1.078 (0.853–1.363) | 0.531 | ||
| Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|
| Variables | Hazard Ratio (95% CI) | p Value | Hazard Ratio (95% CI) | p Value |
| Baseline | ||||
| Age (year) | 1.010 (0.988–1.031) | 0.377 | ||
| Sex, male vs. female | 1.096 (0.613–1.960) | 0.757 | ||
| HBeAg, yes vs. no | 1.084 (0.620–1.894) | 0.778 | ||
| Decompensation, yes vs. no | 5.519 (3.352–9.087) | <0.001 | ||
| NA-naïve, yes vs. no | 1.550 (0.706–3.404) | 0.275 | ||
| TDF vs. entecavir | 0.651 (0.346–1.228) | 0.185 | ||
| Diabetes mellitus, yes vs. no | 1.210 (0.676–2.164) | 0.521 | ||
| Hypertension, yes vs. no | 0.958 (0.542–1.692) | 0.882 | ||
| HBV DNA, per log10 IU/mL | 0.948 (0.806–1.117) | 0.525 | ||
| AST, per U/L | 0.999 (0.997–1.001) | 0.190 | ||
| ALT, per U/L | 0.997 (0.994–1.000) | 0.041 | ||
| Total bilirubin, per mg/dL | 1.033 (0.983–1.085) | 0.204 | ||
| Albumin, per g/L | 0.303 (0.219–0.419) | <0.001 | ||
| INR, per ratio | 1.983 (1.078–3.650) | 0.028 | ||
| Platelet, per 103/μL | 0.984 (0.978–0.989) | <0.001 | ||
| AFP at baseline, per ng/mL | 0.999 (0.994–1.003) | 0.491 | ||
| M2BPGi, per COI | 1.137 (1.087–1.189) | <0.001 | ||
| HBcrAg, per log10 U/mL | 0.987 (0.821–1.166) | 0.806 | ||
| 12 months of treatment | ||||
| ALT < 40 U/L, per U/L | 0.763 (0.441–1.321) | 0.335 | ||
| AFP, per ng/mL | 1.011 (1.003–1.019) | 0.011 | ||
| Platelet, per 103/μL | 0.984 (0.978–0.989) | <0.001 | 0.992 (0.986–0.998) | 0.009 |
| Albumin, per g/L | 0.280 (0.197–0.398) | <0.001 | 0.350 (0.250–0.490) | <0.001 |
| M2BPGi, per COI | 1.239 (1.175–1.306) | <0.001 | 1.083 (1.012–1.159) | 0.021 |
| HBcrAg, per log10 U/mL | 1.156 (0.944–1.416) | 0.160 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, C.-H.; Hu, T.-H.; Wang, J.-H.; Lai, H.-C.; Hung, C.-H.; Lu, S.-N.; Peng, C.-Y. A Mac-2 Binding Protein Glycosylation Isomer-Based Risk Model Predicts Hepatocellular Carcinoma in HBV-Related Cirrhotic Patients on Antiviral Therapy. Cancers 2022, 14, 5063. https://doi.org/10.3390/cancers14205063
Chen C-H, Hu T-H, Wang J-H, Lai H-C, Hung C-H, Lu S-N, Peng C-Y. A Mac-2 Binding Protein Glycosylation Isomer-Based Risk Model Predicts Hepatocellular Carcinoma in HBV-Related Cirrhotic Patients on Antiviral Therapy. Cancers. 2022; 14(20):5063. https://doi.org/10.3390/cancers14205063
Chicago/Turabian StyleChen, Chien-Hung, Tsung-Hui Hu, Jing-Houng Wang, Hsueh-Chou Lai, Chao-Hung Hung, Sheng-Nan Lu, and Cheng-Yuan Peng. 2022. "A Mac-2 Binding Protein Glycosylation Isomer-Based Risk Model Predicts Hepatocellular Carcinoma in HBV-Related Cirrhotic Patients on Antiviral Therapy" Cancers 14, no. 20: 5063. https://doi.org/10.3390/cancers14205063





