FLT3-ITD Measurable Residual Disease Monitoring in Acute Myeloid Leukemia Using Next-Generation Sequencing
Abstract
:Simple Summary
Abstract
1. Introduction
2. Patients and Methods
2.1. Samples for Performance Evaluation
2.2. Patients
2.3. NGS-Based FLT3-ITD Assay
2.4. SEED Algorithm for MRD of FLT3-ITD
2.5. Statistical Analysis
3. Results
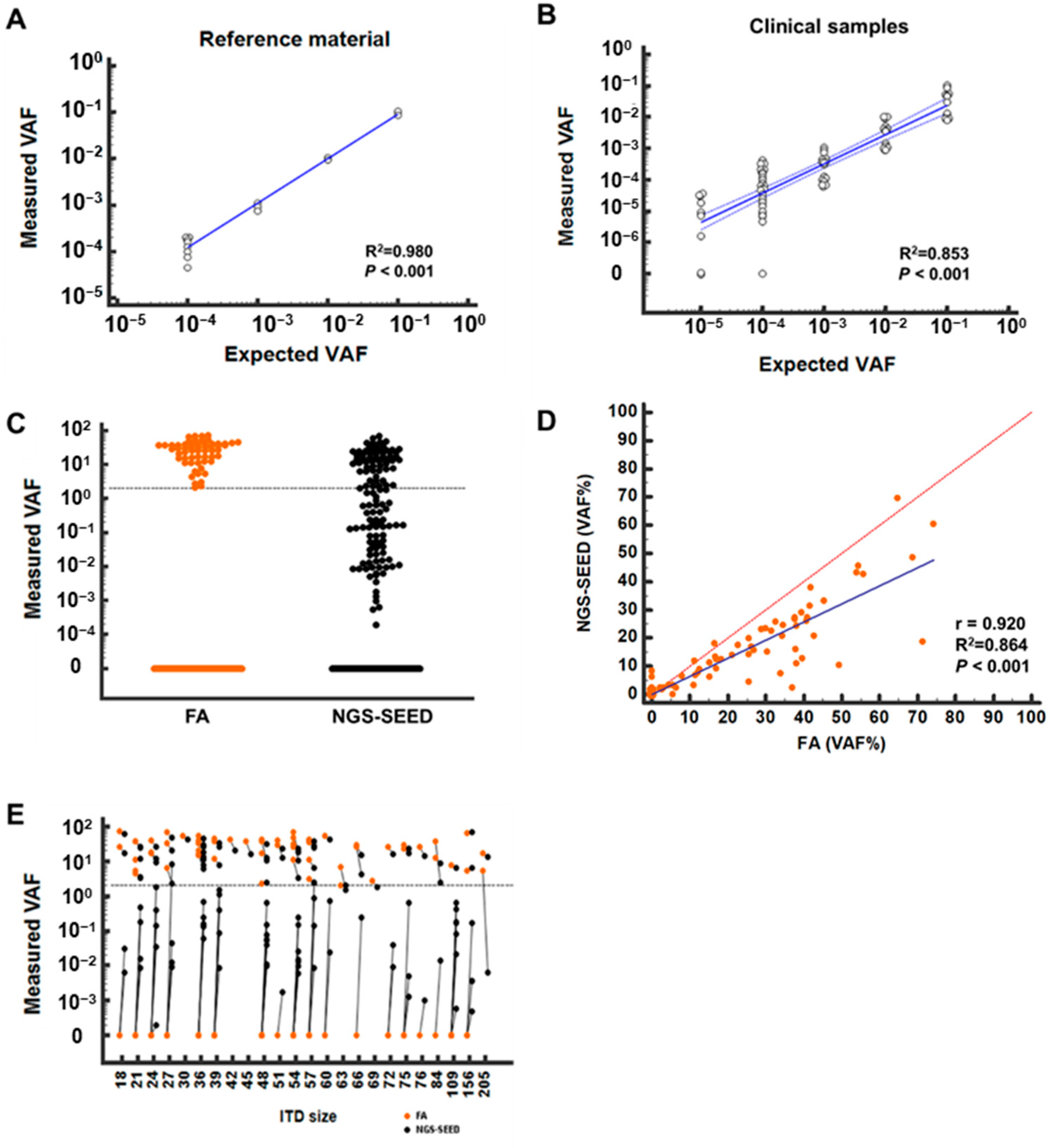
3.1. Assay Performance of NGS with SEED Algorithm for FLT3-ITD
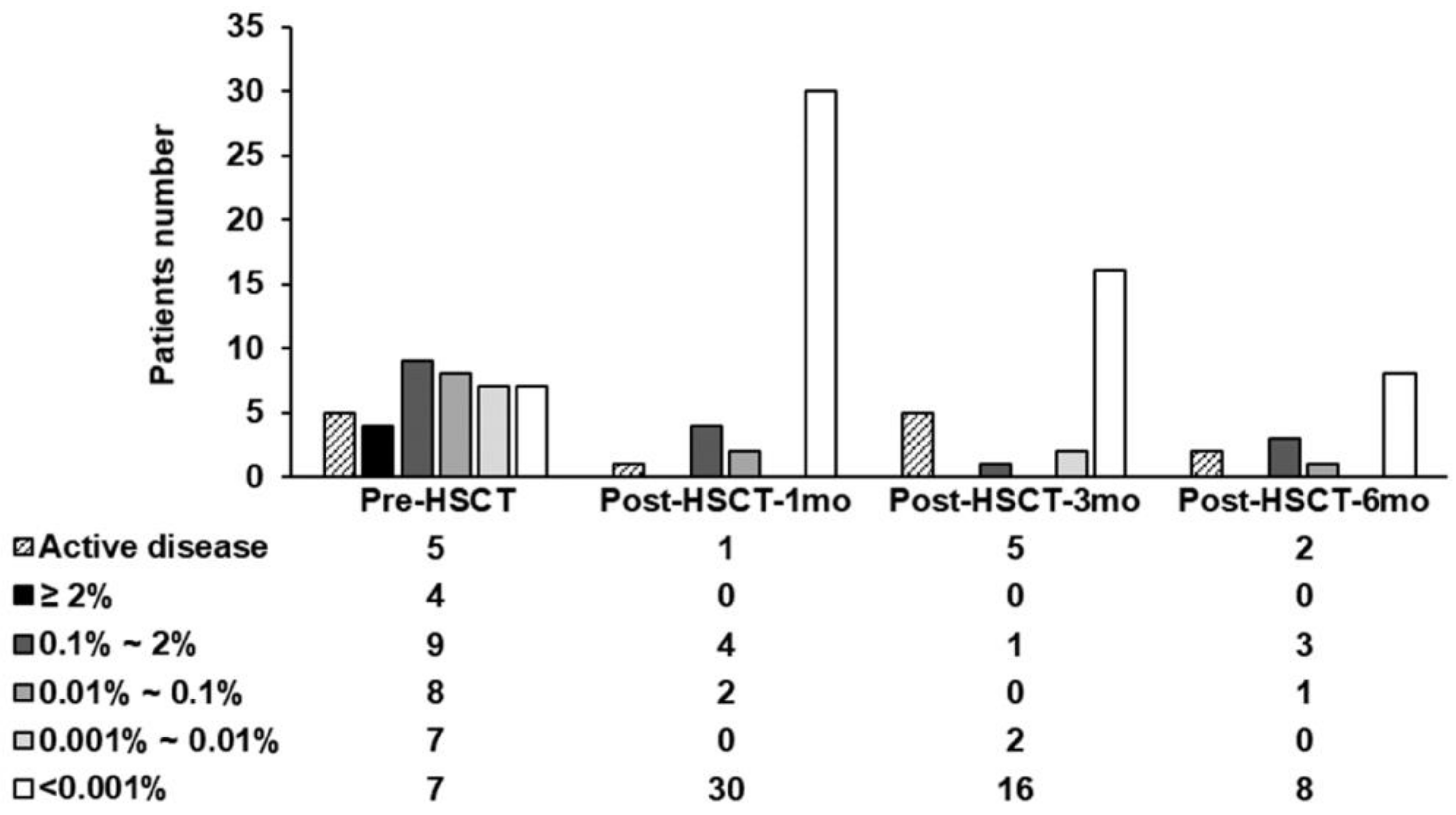
3.2. FLT3-ITD Assessment after Treatment
3.3. Prognostic Impact of FLT3-ITD MRD by NGS-SEED
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Daver, N.; Schlenk, R.F.; Russell, N.H.; Levis, M.J. Targeting FLT3 mutations in AML: Review of current knowledge and evidence. Leukemia 2019, 33, 299–312. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Döhner, H.; Estey, E.; Grimwade, D.; Amadori, S.; Appelbaum, F.R.; Büchner, T.; Dombret, H.; Ebert, B.L.; Fenaux, P.; Larson, R.A.; et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood 2017, 129, 424–447. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gale, R.E.; Green, C.; Allen, C.; Mead, A.J.; Burnett, A.K.; Hills, R.K.; Linch, D.C. The impact of FLT3 internal tandem duplication mutant level, number, size, and interaction with NPM1 mutations in a large cohort of young adult patients with acute myeloid leukemia. Blood 2008, 111, 2776–2784. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gilliland, D.G.; Griffin, J.D. The roles of FLT3 in hematopoiesis and leukemia. Blood 2002, 100, 1532–1542. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Levis, M.; Small, D. FLT3: ITDoes matter in leukemia. Leukemia 2003, 17, 1738–1752. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Welch, J.S.; Ley, T.J.; Link, D.C.; Miller, C.A.; Larson, D.E.; Koboldt, D.C.; Wartman, L.D.; Lamprecht, T.L.; Liu, F.; Xia, J.; et al. The Origin and Evolution of Mutations in Acute Myeloid Leukemia. Cell 2012, 150, 264–278. [Google Scholar] [CrossRef] [Green Version]
- Murphy, K.M.; Levis, M.; Hafez, M.J.; Geiger, T.; Cooper, L.C.; Smith, B.; Small, D.; Berg, K.D. Detection of FLT3 Internal Tandem Duplication and D835 Mutations by a Multiplex Polymerase Chain Reaction and Capillary Electrophoresis Assay. J. Mol. Diagn. 2003, 5, 96–102. [Google Scholar] [CrossRef] [Green Version]
- Kim, Y.; Lee, G.D.; Park, J.; Yoon, J.-H.; Kim, H.-J.; Min, W.-S.; Kim, M. Quantitative fragment analysis of FLT3-ITD efficiently identifying poor prognostic group with high mutant allele burden or long ITD length. Blood Cancer J. 2015, 5, e336. [Google Scholar] [CrossRef] [Green Version]
- Lee, G.; Kim, J.; Lee, S.; Jang, W.; Park, J.; Chae, H.; Kim, M.; Kim, Y. Fragment Analysis for Detection of the FLT3-Internal Tandem Duplication: Comparison with Conventional PCR and Sanger Sequencing. Lab. Med. Online 2017, 7, 3. [Google Scholar] [CrossRef]
- Wang, T.-Y.; Yang, R. ScanITD: Detecting internal tandem duplication with robust variant allele frequency estimation. GigaScience 2020, 9, giaa089. [Google Scholar] [CrossRef]
- Thol, F.; Kölking, B.; Damm, F.; Reinhardt, K.; Klusmann, J.-H.; Reinhardt, D.; von Neuhoff, N.; Brugman, M.H.; Schlegelberger, B.; Suerbaum, S.; et al. Next-generation sequencing for minimal residual disease monitoring in acute myeloid leukemia patients with FLT3-ITD or NPM1 mutations. Genes Chromosom. Cancer 2012, 51, 689–695. [Google Scholar] [CrossRef]
- Bibault, J.-E.; Figeac, M.; Hélevaut, N.; Rodriguez, C.; Quief, S.; Sebda, S.; Renneville, A.; Nibourel, O.; Rousselot, P.; Gruson, B.; et al. Next-generation sequencing of FLT3 internal tandem duplications for minimal residual disease monitoring in acute myeloid leukemia. Oncotarget 2015, 6, 22812–22821. [Google Scholar] [CrossRef] [Green Version]
- Schuurhuis, G.J.; Heuser, M.; Freeman, S.; Béné, M.-C.; Buccisano, F.; Cloos, J.; Grimwade, D.; Haferlach, T.; Hills, R.K.; Hourigan, C.S.; et al. Minimal/measurable residual disease in AML: A consensus document from the European LeukemiaNet MRD Working Party. Blood 2018, 131, 1275–1291. [Google Scholar] [CrossRef] [Green Version]
- Liang, E.C.; Chen, C.; Lu, R.; Mannis, G.N.; Muffly, L. Measurable residual disease status and FLT3 inhibitor therapy in patients with FLT3-ITD mutated AML following allogeneic hematopoietic cell transplantation. Bone Marrow Transplant. 2021, 56, 3091–3093. [Google Scholar] [CrossRef]
- Tsai, H.K.; Brackett, D.G.; Szeto, D.; Frazier, R.; MacLeay, A.; Davineni, P.; Manning, D.K.; Garcia, E.; Lindeman, N.I.; Le, L.P.; et al. Targeted Informatics for Optimal Detection, Characterization, and Quantification of FLT3 Internal Tandem Duplications Across Multiple Next-Generation Sequencing Platforms. J. Mol. Diagn. 2020, 22, 1162–1178. [Google Scholar] [CrossRef]
- Tung, J.K.; Suarez, C.J.; Chiang, T.; Zehnder, J.L.; Stehr, H. Accurate Detection and Quantification of FLT3 Internal Tandem Duplications in Clinical Hybrid Capture Next-Generation Sequencing Data. J. Mol. Diagn. 2021, 23, 1404–1413. [Google Scholar] [CrossRef]
- Schwartz, G.W.; Manning, B.; Zhou, Y.; Velu, P.; Bigdeli, A.; Astles, R.; Lehman, A.W.; Morrissette, J.J.; Perl, A.E.; Li, M. Classes of ITD Predict Outcomes in AML Patients Treated with FLT3 InhibitorsFLT3-ITD Classes Predict Outcomes in FLT3i-Treated AML. Clin. Cancer Res. 2019, 25, 573–583. [Google Scholar] [CrossRef] [Green Version]
- Au, C.H.; Wa, A.; Ho, D.N.; Chan, T.L.; Ma, E.S.K. Clinical evaluation of panel testing by next-generation sequencing (NGS) for gene mutations in myeloid neoplasms. Diagn. Pathol. 2016, 11, 11. [Google Scholar] [CrossRef] [Green Version]
- Blätte, T.J.; Schmalbrock, L.K.; Skambraks, S.; Lux, S.; Cocciardi, S.; Dolnik, A.; Döhner, H.; Döhner, K.; Bullinger, L. getITD for FLT3-ITD-based MRD monitoring in AML. Leukemia 2019, 33, 2535–2539. [Google Scholar] [CrossRef] [Green Version]
- Ye, K.; Schulz, M.H.; Long, Q.; Apweiler, R.; Ning, Z. Pindel: A pattern growth approach to detect break points of large deletions and medium sized insertions from paired-end short reads. Bioinformatics 2009, 25, 2865–2871. [Google Scholar] [CrossRef] [Green Version]
- Scrucca, L.; Santucci, A.; Aversa, F. Competing risk analysis using R: An easy guide for clinicians. Bone Marrow Transplant. 2007, 40, 381–387. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scrucca, L.; Santucci, A.; Aversa, F. Regression modeling of competing risk using R: An in depth guide for clinicians. Bone Marrow Transplant. 2010, 45, 1388–1395. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Austin, P.C.; Latouche, A.; Fine, J.P. A review of the use of time-varying covariates in the Fine-Gray subdistribution hazard competing risk regression model. Stat. Med. 2019, 39, 103–113. [Google Scholar] [CrossRef] [PubMed]
- Rizopoulos, D. JM: An R package for the joint modelling of longitudinal and time-to-event data. J. Stat. Softw. 2010, 35, 1–33. [Google Scholar] [CrossRef]
- Ravandi, F.; Walter, R.B.; Freeman, S.D. Evaluating measurable residual disease in acute myeloid leukemia. Blood Adv. 2018, 2, 1356–1366. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heuser, M.; Freeman, S.D.; Ossenkoppele, G.J.; Buccisano, F.; Hourigan, C.S.; Ngai, L.L.; Tettero, J.M.; Bachas, C.; Baer, C.; Béné, M.-C.; et al. 2021 Update on MRD in acute myeloid leukemia: A consensus document from the European LeukemiaNet MRD Working Party. Blood 2021, 138, 2753–2767. [Google Scholar] [CrossRef]
- Nagler, A.; Baron, F.; Labopin, M.; Polge, E.; Esteve, J.; Bazarbachi, A.; Brissot, E.; Bug, G.; Ciceri, F.; Giebel, S.; et al. Measurable residual disease (MRD) testing for acute leukemia in EBMT transplant centers: A survey on behalf of the ALWP of the EBMT. Bone Marrow Transplant. 2020, 56, 218–224. [Google Scholar] [CrossRef]
- Döhner, H.; Wei, A.H.; Appelbaum, F.R.; Craddock, C.; DiNardo, C.D.; Dombret, H.; Ebert, B.L.; Fenaux, P.; Godley, L.A.; Hasserjian, R.P. Diagnosis and Management of Acute Myeloid Leukemia in Adults: 2022 Recommendations from an International Expert Panel, on Behalf of the European LeukemiaNet. Blood 2022, 115, 453–474. [Google Scholar] [CrossRef] [Green Version]
- Kadri, S.; Zhen, C.J.; Wurst, M.N.; Long, B.C.; Jiang, Z.-F.; Wang, Y.L.; Furtado, L.V.; Segal, J.P. Amplicon Indel Hunter Is a Novel Bioinformatics Tool to Detect Large Somatic Insertion/Deletion Mutations in Amplicon-Based Next-Generation Sequencing Data. J. Mol. Diagn. 2015, 17, 635–643. [Google Scholar] [CrossRef]
- Hourigan, C.S.; Dillon, L.W.; Gui, G.; Logan, B.R.; Fei, M.; Ghannam, J.; Li, Y.; Licon, A.; Alyea, E.P.; Bashey, A.; et al. Impact of Conditioning Intensity of Allogeneic Transplantation for Acute Myeloid Leukemia with Genomic Evidence of Residual Disease. J. Clin. Oncol. 2020, 38, 1273–1283. [Google Scholar] [CrossRef]
- Loo, S.; Dillon, R.; Ivey, A.; Anstee, N.S.; Othman, J.; Tiong, I.S.; Potter, N.; Jovanovic, J.; Runglall, M.; Chua, C.C. Pre-transplant FLT3-ITD MRD assessed by high-sensitivity PCR-NGS determines post-transplant clinical outcome. Blood 2022, 140, 2407–2411. [Google Scholar] [CrossRef]
- Grob, T.; Sanders, M.A.; Vonk, C.M.; Kavelaars, F.G.; Rijken, M.; Hanekamp, D.W.; Gradowska, P.L.; Cloos, J.; Fløisand, Y.; Kooy, M.V.M.; et al. Prognostic Value of FLT3-Internal Tandem Duplication Residual Disease in Acute Myeloid Leukemia. J. Clin. Oncol. 2022, JCO-22. [Google Scholar] [CrossRef]
- Kim, H.-J.; Kim, Y.; Kang, D.; Kim, H.S.; Lee, J.-M.; Kim, M.; Cho, B.-S. Prognostic value of measurable residual disease monitoring by next-generation sequencing before and after allogeneic hematopoietic cell transplantation in acute myeloid leukemia. Blood Cancer J. 2021, 11, 109. [Google Scholar] [CrossRef]
- Levis, M.J.; Perl, A.E.; Altman, J.K.; Gocke, C.D.; Bahceci, E.; Hill, J.; Liu, C.; Xie, Z.; Carson, A.R.; McClain, V.; et al. A next-generation sequencing–based assay for minimal residual disease assessment in AML patients with FLT3-ITD mutations. Blood Adv. 2018, 2, 825–831. [Google Scholar] [CrossRef]
| Characteristics | Total (n = 46) | MRD Assessed Patients * | ||||
|---|---|---|---|---|---|---|
| Pre-HSCT | Post-HSCT | Post-HSCT | Post-HSCT | |||
| (n = 35) | 1 mo (n = 36) | 3 mo (n = 19) | 6 mo (n = 12) | |||
| Age at diagnosis (years) | 43.3 ± 16.6 | 43.5 ± 16.1 | 46.5 ± 17.0 | 40.8 ± 18.5 | 34.3 ± 18.6 | |
| Gender (Male) | 19 (41.3%) | 17 (48.6%) | 11 (30.6%) | 7 (36.8%) | 7 (58.3%) | |
| WBC at diagnosis (×109/L) | 52.5 (19.5–110.4) | 46.0 (16.5–121.4) | 38.5 (8.3–103.6) | 61.9 (2.9–14.6) | 58.1 (9.1–204.6) | |
| Initial ITD maximum length | 46 (35.9–52.3) | 45 (35.0–51.3) | 45.5 (35.0–53.0) | 41.0 (25.6–53.3) | 43.5 (30.6–63.4) | |
| Disease type | De novo AML | 37 (80.4%) | 28 (80.0%) | 28 (77.8%) | 14 (73.7%) | 9 (75.0%) |
| AML-MRC | 7 (15.2%) | 5 (14.3%) | 6 (16.7%) | 3 (15.8%) | 2 (16.7%) | |
| Therapy-related AML | 1 (2.2%) | 1 (2.9%) | 1 (2.8%) | 0 (0%) | 0 (0%) | |
| MPAL (T/M) | 1 (2.2%) | 1 (2.9%) | 1 (2.8%) | 1 (5.3%) | 1 (8.3%) | |
| Mutations | NPM1 | 17 (37.0%) | 14 (40.0%) | 13 (36.1%) | 7 (36.85) | 5 (41.7%) |
| CEBPA | 3 (6.5%) | 3 (8.6%) | 2 (5.6%) | 1 (5.3%) | 1 (8.3%) | |
| 2017 ELN risk group | Favorable | 14 (30.4%) | 14 (40.0%) | 12 (33.3%) | 6 (31.6%) | 3 (25.0) |
| Intermediate | 12 (26.1%) | 8 (22.9%) | 7 (19.4%) | 4 (21.1%) | 4 (33.3%) | |
| Poor | 20 (43.5%) | 13 (37.1%) | 17 (47.2%) | 9 (47.4%) | 5 (41.7%) | |
| Initial induction regimen | Intensive chemotherapy | 42 (91.3%) | 32 (91.4%) | 33 (91.7%) | 16 (84.2%) | 12 (100%) |
| Low-intensive chemotherapy | 3 (6.5%) | 3 (8.6%) | 2 (5.65) | 1 (5.3%) | 0 (0%) | |
| FLT3 inhibitor | 1 (2.2%) | 0 (0%) | 1 (2.8%) | 1 (5.3%) | 0 (0%) | |
| Chemotherapy cycles before CR | 1 cycle | 25 (54.3%) | 24 (68.6%) | 17 (47.2%) | 11 (57.9%) | 6 (50.0%) |
| 2 cycles | 11 (23.9%) | 10 (28.6%) | 10 (27.8%) | 4 (21.1%) | 2 (16.7%) | |
| 3 cycles | 1 (2.2%) | 1 (2.9%) | 1 (2.8%) | 1 (5.3%) | 0 (0%) | |
| Conditioning intensity | Myeloablative | 37 (80.4%) | 30 (85.7%) | 32 (88.9%) | 15 (78.9%) | 10 (83.3%) |
| Reduced intensity | 9 (19.6%) | 5 (14.3%) | 4 (11.1%) | 4 (21.1%) | 2 (16.7%) | |
| FLT3 inhibitor | No | 23 (50.0%) | 20 (57.1%) | 18 (50.0%) | 8 (42.1%) | 4 (33.3%) |
| Yes | 14 (30.4%) | 8 (22.9%) | 13 (36.1%) | 7 (36.8%) | 5 (41.7%) | |
| Clinical trial | 9 (19.6%) | 7 (20.0%) | 5 (13.9%) | 4 (21.1%) | 3 (25.0) | |
| Disease status at HSCT | CR1 | 34 (73.9%) | 32 (91.4%) | 27 (75.0%) | 16 (%) | 7 (58.3%) |
| CR2 | 4 (8.7%) | 3 (8.6%) | 2 (5.65) | 0 (0%) | 3 (25.0%) | |
| Persistent leukemia | 8 (17.4%) | 0 (0%) | 7 (19.4%) | 3 (15.8%) | 2 (16.7%) | |
| Transplant modality | Matched sibling donor | 15 (32.6%) | 13 (37.1%) | 11 (30.6%) | 8 (42.1%) | 5 (41.7%) |
| Matched unrelated donor | 13 (28.3%) | 9 (25.7%) | 10 (27.8%) | 4 (21.1%) | 2 (16.7%) | |
| Haploidentical donor | 18 (39.1%) | 13 (37.1%) | 15 (41.7%) | 7 (36.8%) | 5 (41.7%) | |
| GVHD | Acute GVHD | 22 (66.7%) | - | 13 (48.1%) | 5 (33.3%) | 5 (55.6%) |
| Chronic GVHD | 14 (42.4%) | - | 9 (33.3%) | 3 (20%) | 2 (22.2%) | |
| Clinical outcome | Died without relapse | 9 (19.6%) | 7 (20.0%) | 8 (22.2%) | 3 (15.8%) | 0 (0%) |
| Relapsed and died | 12 (26.1%) | 9 (25.7%) | 9 (25.0%) | 3 (15.8%) | 3 (25.0) | |
| Died with persistent leukemia | 1 (2.2%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | |
| Ongoing CR after reinduction chemotherapy for relapse | 1 (2.2%) | 1 (2.9%) | 1 (2.8%) | 1 (5.3%) | 1 (8.3%) | |
| Ongoing CR | 23 (50.0%) | 18 (51.4%) | 18 (50.0%) | 12 (63.2%) | 8 (66.7%) | |
| Univariate Variables | n | Cumulative Incidence of Relapse | Cumulative Incidence of Non-Relapse Mortality | Event Free Survival | Overall Survival | ||||
|---|---|---|---|---|---|---|---|---|---|
| HR (95% CI) | p Value | HR (95% CI) | p Value | HR (95% CI) | p Value | HR (95% CI) | p Value | ||
| MRD status at pre-HSCT >2% >0.1% >0.01% >0.001% | 35 4 13 21 28 | 2.79 (0.53–14.59) 5.49 (1.55–19.45) 7.50 (1.01–55.69) 1.3 × 107 (5.25 × 106–3.55 × 107) | 0.226 0.008 0.049 <0.001 | 0.26 (0.03–1.98) 0.86 (0.20–3.75) 0.57 (0.11–3.07) NA | 0.192 0.841 0.510 NA | 1.22 (0.28–5.35) 1.80 (0.69–4.70) 2.65 (0.86–8.16) 1.99 (0.45–8.74) | 0.794 0.230 0.090 0.364 | 1.25 (0.28–5.71) 1.48 (0.55–4.02) 2.50 (0.80–7.83) 1.87 (0.42–8.31) | 0.767 0.439 0.116 0.411 |
| MRD status at post-HSCT >0.1% >0.001% | 44 6 10 | - - | - - | - - | - - | 4.73 (1.88–11.93) 2.86 (1.15–7.14) | 0.001 0.024 | 4.04 (1.61–10.18) 2.38 (0.95–5.98) | 0.003 0.065 |
| Age group <60 years ≥60 years | 45 38 7 | 1 1.68 (0.51–5.49) | 0.392 | 1 2.88 (0.80–10.4) | 0.104 | 1 2.37 (0.93–6.06) | 0.072 | 1 2.52 (0.98–6.52) | 0.057 |
| Gender Female Male | 45 26 19 | 1 2.33 (0.79–6.87) | 0.125 | 1 0.34 (0.08–1.52) | 0.157 | 1 1.07 (0.46–2.48) | 0.870 | 1 0.86 (0.36–2.04) | 0.727 |
| WBC group at diagnosis <50 × 109/L ≥50 × 109/L | 45 23 22 | 1 2.75 (0.89–8.49) | 0.079 | 1 0.47 (0.12–1.83) | 0.276 | 1 1.35 (0.58–3.12) | 0.490 | 1 1.21 (0.48–2.65) | 0.794 |
| Initial ITD maximum length ˂50 bp ≥50 bp | 45 27 18 | 1 0.87 (0.30–2.52) | 0.794 | 1 2.04 (0.57–7.27) | 0.272 | 1 1.29 (0.56–2.99) | 0.552 | 1 1.40 (0.59–3.30) | 0.442 |
| 2017 ELN risk group Favorable Intermediate Adverse | 45 14 11 20 | 1 8.20 (0.94–71.80) 5.25 (0.65–42.60) | 0.164 0.057 0.120 | 1 0.56 (0.12–2.74) 0.51 (0.11–2.25) | 0.618 0.477 0.372 | 1 2.51 (0.73–8.63) 2.26 (0.72–7.13) | 0.240 0.143 0.163 | 1 1.89 (0.53–6.69) 2.14 (0.68–6.74) | 0.378 0.327 0.194 |
| Chemotherapy cycles for CR 1 cycle ≥2 cycles | 37 25 12 | 1 2.21 (0.69–7.09) | 0.180 | 1 1.58 (0.38–6.59) | 0.534 | 1 2.10 (0.82–5.35) | 0.121 | 1 2.57 (0.97–6.76) | 0.057 |
| Conditioning intensity Myeloablative Reduced intensity | 45 36 9 | 1 2.83 (1.01–7.92) | 0.048 | 1 1.03 (0.25–4.28) | 0.967 | 1 1.93 (0.79–4.76) | 0.150 | 1 1.87 (0.75–4.64) | 0.177 |
| FLT3 inhibitor No Yes | 36 22 14 | 1 1.73 (0.60–5.00) | 0.311 | 1 0.45 (0.10–2.04) | 0.300 | 1 0.90 (0.37–2.21) | 0.820 | 1 0.77 (0.30–1.95) | 0.579 |
| Disease state at HSCT CR1 CR2 Persistent leukemia | 45 33 4 8 | 1 1.58 (0.39–6.33) NA | NA 0.519 NA | 1 1.29 (0.16–10.40) 0.54 (0.07–4.04) | 0.789 0.811 0.547 | 1 1.52 (0.44–5.22) 0.880 (0.26–3.02) | 0.782 0.507 0.839 | 1 1.58 (0.46–5.45) 0.99 (0.29–3.44) | 0.787 0.473 0.993 |
| Transplant modality Matched sibling Matched unrelated Haploidentical | 45 14 13 18 | 1 3.79 (0.85–17.01) 1.61 (0.29–8.96) | 0.143 0.082 0.586 | 1 1.06 (0.22–5.00) 0.71 (0.15–3.33) | 0.862 0.946 0.667 | 1 2.82 (0.70–11.31) 4.42 (1.25–15.57) | 0.032 0.143 0.021 | 1 2.63 (0.66–10.57) 3.87 (1.09–13.75) | 0.065 0.172 0.036 |
| Acute GVHD None Grade ≥ 1 | 33 11 22 | - | - | - | - | 1 0.97 (0.35–2.71) | 1 0.958 | 1 1.29 (0.44–3.76) | 0.640 |
| Chronic GVHD None Mild to Severe | 33 19 14 | - | - | - | - | 1 0.60 (0.20–1.89) | 0.382 | 1 0.68 (0.21–2.18) | 0.517 |
| Variables | n | Relapse | Event-Free Survival | Overall Survival | |||
|---|---|---|---|---|---|---|---|
| HR (95% CI) | p Value | HR (95% CI) | p Value | HR (95% CI) | p Value | ||
| MRD > 0.1% at pre-HSCT | 13 | 5.10 (1.53–17.02) | 0.008 | - | - | - | - |
| MRD > 0.1% at post-HSCT | 6 | - | - | - | - | 2.61 (1.01–6.75) | 0.049 |
| MRD > 0.001% at post-HSCT | 10 | - | - | 1.90 (0.74–4.88) | 0.185 | - | - |
| Transplant modality = haploidentical | 18 | - | - | 4.72 (1.04–21.45) | 0.044 | 3.62 (0.77–16.96) | 0.103 |
| Conditioning intensity = reduced intensity | 9 | 3.24 (1.13–9.32) | 0.029 | - | - | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.-M.; Park, S.; Hwang, I.; Kang, D.; Cho, B.S.; Kim, H.-J.; Ahn, A.; Kim, M.; Kim, Y. FLT3-ITD Measurable Residual Disease Monitoring in Acute Myeloid Leukemia Using Next-Generation Sequencing. Cancers 2022, 14, 6121. https://doi.org/10.3390/cancers14246121
Lee J-M, Park S, Hwang I, Kang D, Cho BS, Kim H-J, Ahn A, Kim M, Kim Y. FLT3-ITD Measurable Residual Disease Monitoring in Acute Myeloid Leukemia Using Next-Generation Sequencing. Cancers. 2022; 14(24):6121. https://doi.org/10.3390/cancers14246121
Chicago/Turabian StyleLee, Jong-Mi, Silvia Park, Insik Hwang, Dain Kang, Byung Sik Cho, Hee-Je Kim, Ari Ahn, Myungshin Kim, and Yonggoo Kim. 2022. "FLT3-ITD Measurable Residual Disease Monitoring in Acute Myeloid Leukemia Using Next-Generation Sequencing" Cancers 14, no. 24: 6121. https://doi.org/10.3390/cancers14246121





