Epigenetic Approaches to Overcome Fluoropyrimidines Resistance in Solid Tumors
Abstract
:Simple Summary
Abstract
1. Introduction
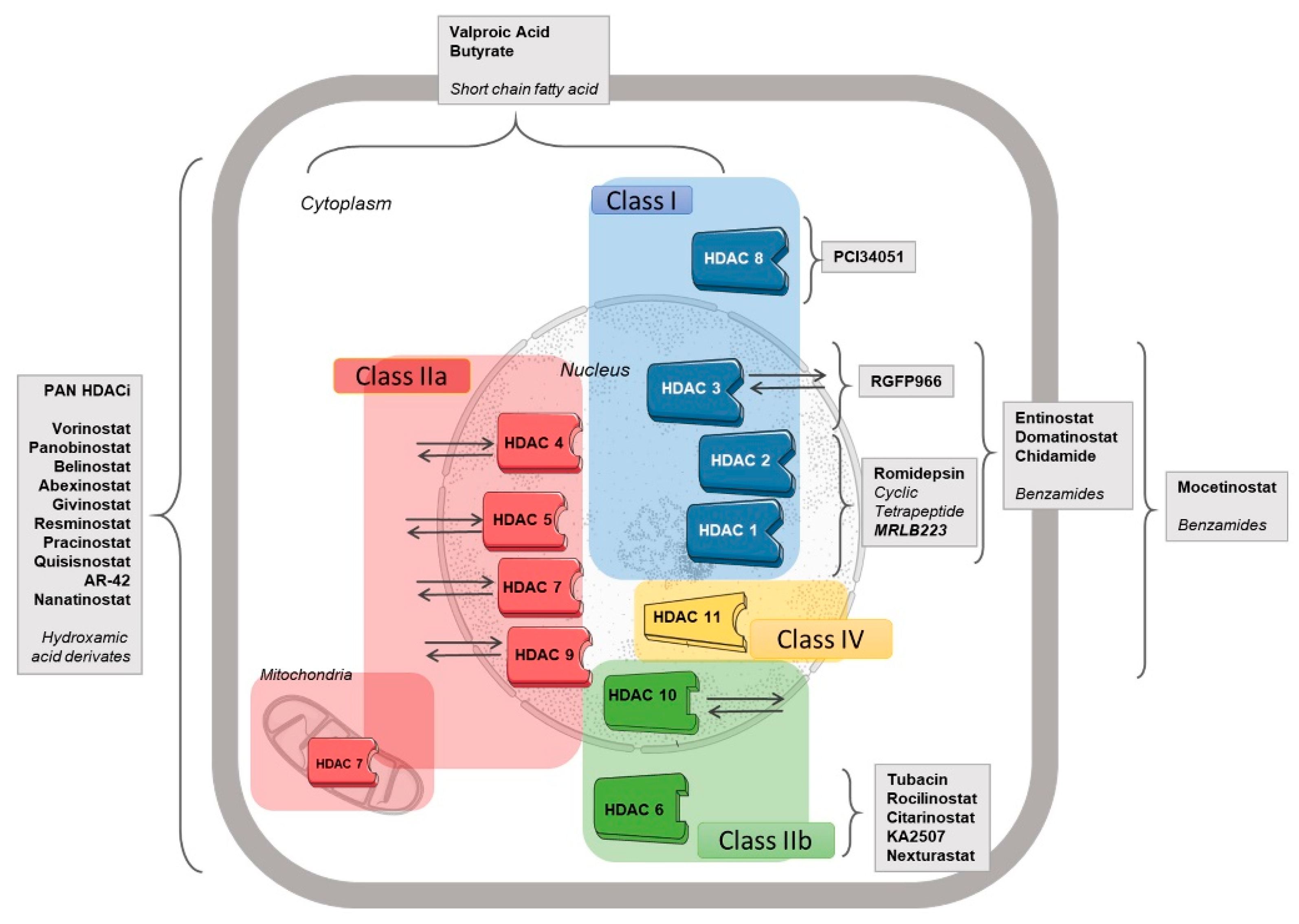
2. HDAC Inhibitors
3. Fluoropyrimidines
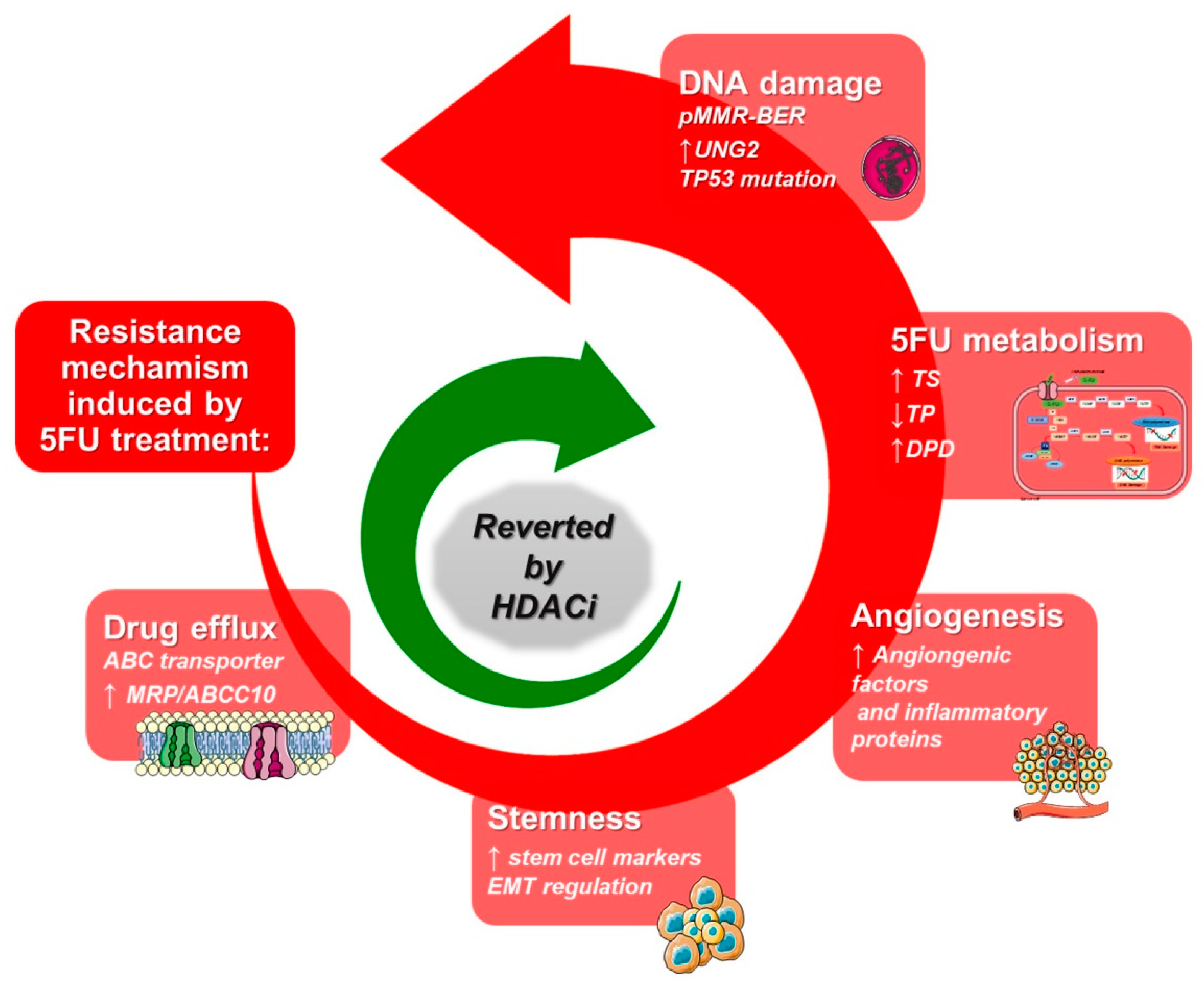
4. Mechanisms of Resistance to Fluoropyrimidines
5. The Role of HDACis in Combination with Fluoropyrimidine-Based Therapy
6. DNA Methylation and Histone Deacetylation
7. Clinical Trials
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Pucci, C.; Martinelli, C.; Ciofani, G. Innovative approaches for cancer treatment: Current perspectives and new challenges. Ecancermedicalscience 2019, 13, 961. [Google Scholar] [CrossRef] [PubMed]
- Vodenkova, S.; Buchler, T.; Cervena, K.; Veskrnova, V.; Vodicka, P.; Vymetalkova, V. 5-fluorouracil and other fluoropyrimidines in colorectal cancer: Past, present and future. Pharmacol. Ther. 2020, 206, 107447. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Seto, E. HDACs and HDAC Inhibitors in Cancer Development and Therapy. Cold Spring Harb. Perspect. Med. 2016, 6, a026831. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Partolina, M.; Thoms, H.C.; MacLeod, K.G.; Rodriguez-Blanco, G.; Clarke, M.N.; Venkatasubramani, A.V.; Beesoo, R.; Larionov, V.; Neergheen-Bhujun, V.S.; Serrels, B.; et al. Global histone modification fingerprinting in human cells using epigenetic reverse phase protein array. Cell Death Discov. 2017, 3, 16077. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eckschlager, T.; Plch, J.; Stiborova, M.; Hrabeta, J. Histone Deacetylase Inhibitors as Anticancer Drugs. Int. J. Mol. Sci. 2017, 18, 1414. [Google Scholar] [CrossRef]
- Cheng, Y.; He, C.; Wang, M.; Ma, X.; Mo, F.; Yang, S.; Han, J.; Wei, X. Targeting epigenetic regulators for cancer therapy: Mechanisms and advances in clinical trials. Signal Transduct. Target Ther. 2019, 4, 62. [Google Scholar] [CrossRef] [Green Version]
- Hontecillas-Prieto, L.; Flores-Campos, R.; Silver, A.; de Alava, E.; Hajji, N.; Garcia-Dominguez, D.J. Synergistic Enhancement of Cancer Therapy Using HDAC Inhibitors: Opportunity for Clinical Trials. Front. Genet. 2020, 11, 578011. [Google Scholar] [CrossRef]
- Park, S.Y.; Kim, J.S. A short guide to histone deacetylases including recent progress on class II enzymes. Exp. Mol. Med. 2020, 52, 204–212. [Google Scholar] [CrossRef]
- Ungerstedt, J.S.; Sowa, Y.; Xu, W.S.; Shao, Y.; Dokmanovic, M.; Perez, G.; Ngo, L.; Holmgren, A.; Jiang, X.; Marks, P.A. Role of thioredoxin in the response of normal and transformed cells to histone deacetylase inhibitors. Proc. Natl. Acad. Sci. USA 2005, 102, 673–678. [Google Scholar] [CrossRef] [Green Version]
- Jung, M. Inhibitors of histone deacetylase as new anticancer agents. Curr. Med. Chem. 2001, 8, 1505–1511. [Google Scholar] [CrossRef]
- Shimizu, T.; LoRusso, P.M.; Papadopoulos, K.P.; Patnaik, A.; Beeram, M.; Smith, L.S.; Rasco, D.W.; Mays, T.A.; Chambers, G.; Ma, A.; et al. Phase I first-in-human study of CUDC-101, a multitargeted inhibitor of HDACs, EGFR, and HER2 in patients with advanced solid tumors. Clin. Cancer Res. 2014, 20, 5032–5040. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qian, C.; Lai, C.J.; Bao, R.; Wang, D.G.; Wang, J.; Xu, G.X.; Atoyan, R.; Qu, H.; Yin, L.; Samson, M.; et al. Cancer network disruption by a single molecule inhibitor targeting both histone deacetylase activity and phosphatidylinositol 3-kinase signaling. Clin. Cancer Res. 2012, 18, 4104–4113. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mann, B.S.; Johnson, J.R.; Cohen, M.H.; Justice, R.; Pazdur, R. FDA approval summary: Vorinostat for treatment of advanced primary cutaneous T-cell lymphoma. Oncologist 2007, 12, 1247–1252. [Google Scholar] [CrossRef] [PubMed]
- Grant, C.; Rahman, F.; Piekarz, R.; Peer, C.; Frye, R.; Robey, R.W.; Gardner, E.R.; Figg, W.D.; Bates, S.E. Romidepsin: A new therapy for cutaneous T-cell lymphoma and a potential therapy for solid tumors. Expert Rev. Anticancer Ther. 2010, 10, 997–1008. [Google Scholar] [CrossRef] [PubMed]
- Sawas, A.; Radeski, D.; O’Connor, O.A. Belinostat in patients with refractory or relapsed peripheral T-cell lymphoma: A perspective review. Ther. Adv. Hematol. 2015, 6, 202–208. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moore, D. Panobinostat (Farydak): A Novel Option for the Treatment of Relapsed or Relapsed and Refractory Multiple Myeloma. Pharm. Ther. 2016, 41, 296–300. [Google Scholar]
- Suraweera, A.; O’Byrne, K.J.; Richard, D.J. Combination Therapy with Histone Deacetylase Inhibitors (HDACi) for the Treatment of Cancer: Achieving the Full Therapeutic Potential of HDACi. Front. Oncol. 2018, 8, 92. [Google Scholar] [CrossRef] [Green Version]
- Mohammad, H.P.; Barbash, O.; Creasy, C.L. Targeting epigenetic modifications in cancer therapy: Erasing the roadmap to cancer. Nat. Med. 2019, 25, 403–418. [Google Scholar] [CrossRef]
- Terranova-Barberio, M.; Pecori, B.; Roca, M.S.; Imbimbo, S.; Bruzzese, F.; Leone, A.; Muto, P.; Delrio, P.; Avallone, A.; Budillon, A.; et al. Synergistic antitumor interaction between valproic acid, capecitabine and radiotherapy in colorectal cancer: Critical role of p53. J. Exp. Clin. Cancer Res. 2017, 36, 177. [Google Scholar] [CrossRef] [Green Version]
- Di Gennaro, E.; Bruzzese, F.; Pepe, S.; Leone, A.; Delrio, P.; Subbarayan, P.R.; Avallone, A.; Budillon, A. Modulation of thymidilate synthase and p53 expression by HDAC inhibitor vorinostat resulted in synergistic antitumor effect in combination with 5FU or raltitrexed. Cancer Biol. Ther. 2009, 8, 782–791. [Google Scholar] [CrossRef] [Green Version]
- Di Gennaro, E.; Piro, G.; Chianese, M.I.; Franco, R.; Di Cintio, A.; Moccia, T.; Luciano, A.; de Ruggiero, I.; Bruzzese, F.; Avallone, A.; et al. Vorinostat synergises with capecitabine through upregulation of thymidine phosphorylase. Br. J. Cancer 2010, 103, 1680–1691. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bruzzese, F.; Rocco, M.; Castelli, S.; Di Gennaro, E.; Desideri, A.; Budillon, A. Synergistic antitumor effect between vorinostat and topotecan in small cell lung cancer cells is mediated by generation of reactive oxygen species and DNA damage-induced apoptosis. Mol. Cancer Ther. 2009, 8, 3075–3087. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bruzzese, F.; Leone, A.; Rocco, M.; Carbone, C.; Piro, G.; Caraglia, M.; Di Gennaro, E.; Budillon, A. HDAC inhibitor vorinostat enhances the antitumor effect of gefitinib in squamous cell carcinoma of head and neck by modulating ErbB receptor expression and reverting EMT. J. Cell Physiol. 2011, 226, 2378–2390. [Google Scholar] [CrossRef] [PubMed]
- Leone, A.; Roca, M.S.; Ciardiello, C.; Terranova-Barberio, M.; Vitagliano, C.; Ciliberto, G.; Mancini, R.; Di Gennaro, E.; Bruzzese, F.; Budillon, A. Vorinostat synergizes with EGFR inhibitors in NSCLC cells by increasing ROS via up-regulation of the major mitochondrial porin VDAC1 and modulation of the c-Myc-NRF2-KEAP1 pathway. Free Radic. Biol. Med. 2015, 89, 287–299. [Google Scholar] [CrossRef]
- Iannelli, F.; Zotti, A.I.; Roca, M.S.; Grumetti, L.; Lombardi, R.; Moccia, T.; Vitagliano, C.; Milone, M.R.; Ciardiello, C.; Bruzzese, F.; et al. Valproic Acid Synergizes With Cisplatin and Cetuximab in vitro and in vivo in Head and Neck Cancer by Targeting the Mechanisms of Resistance. Front. Cell Dev. Biol. 2020, 8, 732. [Google Scholar] [CrossRef]
- Iannelli, F.; Roca, M.S.; Lombardi, R.; Ciardiello, C.; Grumetti, L.; De Rienzo, S.; Moccia, T.; Vitagliano, C.; Sorice, A.; Costantini, S.; et al. Synergistic antitumor interaction of valproic acid and simvastatin sensitizes prostate cancer to docetaxel by targeting CSCs compartment via YAP inhibition. J. Exp. Clin. Cancer Res. 2020, 39, 213. [Google Scholar] [CrossRef]
- Terranova-Barberio, M.; Thomas, S.; Ali, N.; Pawlowska, N.; Park, J.; Krings, G.; Rosenblum, M.D.; Budillon, A.; Munster, P.N. HDAC inhibition potentiates immunotherapy in triple negative breast cancer. Oncotarget 2017, 8, 114156–114172. [Google Scholar] [CrossRef] [Green Version]
- Avallone, A.; Piccirillo, M.C.; Delrio, P.; Pecori, B.; Di Gennaro, E.; Aloj, L.; Tatangelo, F.; D’Angelo, V.; Granata, C.; Cavalcanti, E.; et al. Phase 1/2 study of valproic acid and short-course radiotherapy plus capecitabine as preoperative treatment in low-moderate risk rectal cancer-V-shoRT-R3 (Valproic acid—short Radiotherapy—rectum 3rd trial). BMC Cancer 2014, 14, 875. [Google Scholar] [CrossRef] [Green Version]
- Caponigro, F.; Di Gennaro, E.; Ionna, F.; Longo, F.; Aversa, C.; Pavone, E.; Maglione, M.G.; Di Marzo, M.; Muto, P.; Cavalcanti, E.; et al. Phase II clinical study of valproic acid plus cisplatin and cetuximab in recurrent and/or metastatic squamous cell carcinoma of Head and Neck-V-CHANCE trial. BMC Cancer 2016, 16, 918. [Google Scholar] [CrossRef] [Green Version]
- Longley, D.B.; Harkin, D.P.; Johnston, P.G. 5-fluorouracil: Mechanisms of action and clinical strategies. Nat. Rev. Cancer 2003, 3, 330–338. [Google Scholar] [CrossRef]
- Elamin, Y.Y.; Rafee, S.; Osman, N.; KJ, O.B.; Gately, K. Thymidine Phosphorylase in Cancer; Enemy or Friend? Cancer Microenviron. 2016, 9, 33–43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hashimoto, Y.; Yoshida, Y.; Yamada, T.; Aisu, N.; Yoshimatsu, G.; Yoshimura, F.; Hasegawa, S. Current Status of Therapeutic Drug Monitoring of 5-Fluorouracil Prodrugs. Anticancer Res. 2020, 40, 4655–4661. [Google Scholar] [CrossRef] [PubMed]
- Sethy, C.; Kundu, C.N. 5-Fluorouracil (5-FU) resistance and the new strategy to enhance the sensitivity against cancer: Implication of DNA repair inhibition. Biomed. Pharmacother. 2021, 137, 111285. [Google Scholar] [CrossRef] [PubMed]
- Rahman, L.; Voeller, D.; Rahman, M.; Lipkowitz, S.; Allegra, C.; Barrett, J.C.; Kaye, F.J.; Zajac-Kaye, M. Thymidylate synthase as an oncogene: A novel role for an essential DNA synthesis enzyme. Cancer Cell 2004, 5, 341–351. [Google Scholar] [CrossRef] [Green Version]
- Ackland, S.P.; Clarke, S.J.; Beale, P.; Peters, G.J. Thymidylate synthase inhibitors. Cancer Chemother. Biol. Response. Modif. 2002, 20, 1–36. [Google Scholar] [PubMed]
- Van der Zee, J.A.; van Eijck, C.H.; Hop, W.C.; van Dekken, H.; Dicheva, B.M.; Seynhaeve, A.L.; Koning, G.A.; Eggermont, A.M.; Ten Hagen, T.L. Expression and prognostic significance of thymidylate synthase (TS) in pancreatic head and periampullary cancer. Eur. J. Surg. Oncol. 2012, 38, 1058–1064. [Google Scholar] [CrossRef]
- Popat, S.; Matakidou, A.; Houlston, R.S. Thymidylate synthase expression and prognosis in colorectal cancer: A systematic review and meta-analysis. J. Clin. Oncol. 2004, 22, 529–536. [Google Scholar] [CrossRef]
- Qiu, L.X.; Tang, Q.Y.; Bai, J.L.; Qian, X.P.; Li, R.T.; Liu, B.R.; Zheng, M.H. Predictive value of thymidylate synthase expression in advanced colorectal cancer patients receiving fluoropyrimidine-based chemotherapy: Evidence from 24 studies. Int. J. Cancer 2008, 123, 2384–2389. [Google Scholar] [CrossRef]
- Gao, Y.; Cui, J.; Xi, H.; Cai, A.; Shen, W.; Li, J.; Zhang, K.; Wei, B.; Chen, L. Association of thymidylate synthase expression and clinical outcomes of gastric cancer patients treated with fluoropyrimidine-based chemotherapy: A meta-analysis. Onco Targets Ther. 2016, 9, 1339–1350. [Google Scholar] [CrossRef] [Green Version]
- Chu, E.; Schmitz, J.C. Molecular Regulation of Expression of Thymidylate Synthase. In Cancer Drug Discovery and Development; Jackman, A.L., Ed.; Humana Press: Totowa, NJ, USA, 1999. [Google Scholar]
- Nief, N.; Le Morvan, V.; Robert, J. Involvement of gene polymorphisms of thymidylate synthase in gene expression, protein activity and anticancer drug cytotoxicity using the NCI-60 panel. Eur. J. Cancer 2007, 43, 955–962. [Google Scholar] [CrossRef]
- Sabeti Aghabozorgi, A.; Moradi Sarabi, M.; Jafarzadeh-Esfehani, R.; Koochakkhani, S.; Hassanzadeh, M.; Kavousipour, S.; Eftekhar, E. Molecular determinants of response to 5-fluorouracil-based chemotherapy in colorectal cancer: The undisputable role of micro-ribonucleic acids. World J. Gastrointest. Oncol. 2020, 12, 942–956. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.Y.; Shi, R.; Yu, H.L.; Zeng, Y.; Zheng, W.L.; Ma, W.L. The association between two polymorphisms in the TS gene and risk of cancer: A systematic review and pooled analysis. Int. J. Cancer 2012, 131, 2103–2116. [Google Scholar] [CrossRef]
- Marsh, S.; McKay, J.A.; Cassidy, J.; McLeod, H.L. Polymorphism in the thymidylate synthase promoter enhancer region in colorectal cancer. Int. J. Oncol. 2001, 19, 383–386. [Google Scholar] [CrossRef]
- Banerjee, D.; Gorlick, R.; Liefshitz, A.; Danenberg, K.; Danenberg, P.C.; Danenberg, P.V.; Klimstra, D.; Jhanwar, S.; Cordon-Cardo, C.; Fong, Y.; et al. Levels of E2F-1 expression are higher in lung metastasis of colon cancer as compared with hepatic metastasis and correlate with levels of thymidylate synthase. Cancer Res. 2000, 60, 2365–2367. [Google Scholar] [PubMed]
- Kasahara, M.; Takahashi, Y.; Nagata, T.; Asai, S.; Eguchi, T.; Ishii, Y.; Fujii, M.; Ishikawa, K. Thymidylate synthase expression correlates closely with E2F1 expression in colon cancer. Clin. Cancer Res. 2000, 6, 2707–2711. [Google Scholar] [PubMed]
- Kotwal, A.; Suran, S.; Amere Subbarao, S. Hsp90 chaperone facilitates E2F1/2-dependent gene transcription in human breast cancer cells. Eur. J. Cell Biol. 2021, 100, 151148. [Google Scholar] [CrossRef] [PubMed]
- Ahn, J.Y.; Lee, J.S.; Min, H.Y.; Lee, H.Y. Acquired resistance to 5-fluorouracil via HSP90/Src-mediated increase in thymidylate synthase expression in colon cancer. Oncotarget 2015, 6, 32622–32633. [Google Scholar] [CrossRef] [Green Version]
- Nagaraju, G.P.; Alese, O.B.; Landry, J.; Diaz, R.; El-Rayes, B.F. HSP90 inhibition downregulates thymidylate synthase and sensitizes colorectal cancer cell lines to the effect of 5FU-based chemotherapy. Oncotarget 2014, 5, 9980–9991. [Google Scholar] [CrossRef] [Green Version]
- Welsh, S.J.; Titley, J.; Brunton, L.; Valenti, M.; Monaghan, P.; Jackman, A.L.; Aherne, G.W. Comparison of thymidylate synthase (TS) protein up-regulation after exposure to TS inhibitors in normal and tumor cell lines and tissues. Clin. Cancer Res. 2000, 6, 2538–2546. [Google Scholar]
- Peters, G.J.; Backus, H.H.; Freemantle, S.; van Triest, B.; Codacci-Pisanelli, G.; van der Wilt, C.L.; Smid, K.; Lunec, J.; Calvert, A.H.; Marsh, S.; et al. Induction of thymidylate synthase as a 5-fluorouracil resistance mechanism. Biochim. Biophys. Acta 2002, 1587, 194–205. [Google Scholar] [CrossRef] [Green Version]
- Hollstein, M.; Sidransky, D.; Vogelstein, B.; Harris, C.C. p53 mutations in human cancers. Science 1991, 253, 49–53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soussi, T.; Ishioka, C.; Claustres, M.; Beroud, C. Locus-specific mutation databases: Pitfalls and good practice based on the p53 experience. Nat. Rev. Cancer 2006, 6, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Gao, F.; Zhang, X.P. miR-203 enhances chemosensitivity to 5-fluorouracil by targeting thymidylate synthase in colorectal cancer. Oncol. Rep. 2015, 33, 607–614. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu, W.; Jiang, H.; Zhang, F.; Gao, J.; Hou, J. MicroRNA-330 inhibited cell proliferation and enhanced chemosensitivity to 5-fluorouracil in colorectal cancer by directly targeting thymidylate synthase. Oncol. Lett. 2017, 13, 3387–3394. [Google Scholar] [CrossRef] [PubMed]
- Li, P.L.; Zhang, X.; Wang, L.L.; Du, L.T.; Yang, Y.M.; Li, J.; Wang, C.X. MicroRNA-218 is a prognostic indicator in colorectal cancer and enhances 5-fluorouracil-induced apoptosis by targeting BIRC5. Carcinogenesis 2015, 36, 1484–1493. [Google Scholar] [CrossRef] [Green Version]
- Xu, X.; Chen, X.; Xu, M.; Liu, X.; Pan, B.; Qin, J.; Xu, T.; Zeng, K.; Pan, Y.; He, B.; et al. miR-375-3p suppresses tumorigenesis and partially reverses chemoresistance by targeting YAP1 and SP1 in colorectal cancer cells. Aging 2019, 11, 7357–7385. [Google Scholar] [CrossRef]
- Xu, F.; Ye, M.L.; Zhang, Y.P.; Li, W.J.; Li, M.T.; Wang, H.Z.; Qiu, X.; Xu, Y.; Yin, J.W.; Hu, Q.; et al. MicroRNA-375-3p enhances chemosensitivity to 5-fluorouracil by targeting thymidylate synthase in colorectal cancer. Cancer Sci. 2020, 111, 1528–1541. [Google Scholar] [CrossRef]
- Bronckaers, A.; Gago, F.; Balzarini, J.; Liekens, S. The dual role of thymidine phosphorylase in cancer development and chemotherapy. Med. Res. Rev. 2009, 29, 903–953. [Google Scholar] [CrossRef]
- Furukawa, T.; Tabata, S.; Yamamoto, M.; Kawahara, K.; Shinsato, Y.; Minami, K.; Shimokawa, M.; Akiyama, S.I. Thymidine phosphorylase in cancer aggressiveness and chemoresistance. Pharmacol. Res. 2018, 132, 15–20. [Google Scholar] [CrossRef]
- Takebayashi, Y.; Akiyama, S.; Akiba, S.; Yamada, K.; Miyadera, K.; Sumizawa, T.; Yamada, Y.; Murata, F.; Aikou, T. Clinicopathologic and prognostic significance of an angiogenic factor, thymidine phosphorylase, in human colorectal carcinoma. J. Natl. Cancer Inst. 1996, 88, 1110–1117. [Google Scholar] [CrossRef] [Green Version]
- Shimaoka, S.; Matsushita, S.; Nitanda, T.; Matsuda, A.; Nioh, T.; Suenaga, T.; Nishimata, Y.; Akiba, S.; Akiyama, S.; Nishimata, H. The role of thymidine phosphorylase expression in the invasiveness of gastric carcinoma. Cancer 2000, 88, 2220–2227. [Google Scholar] [CrossRef]
- Imazano, Y.; Takebayashi, Y.; Nishiyama, K.; Akiba, S.; Miyadera, K.; Yamada, Y.; Akiyama, S.; Ohi, Y. Correlation between thymidine phosphorylase expression and prognosis in human renal cell carcinoma. J. Clin. Oncol. 1997, 15, 2570–2578. [Google Scholar] [CrossRef] [PubMed]
- Petrioli, R.; Bargagli, G.; Lazzi, S.; Pascucci, A.; Francini, E.; Bellan, C.; Conca, R.; Martellucci, I.; Fiaschi, A.I.; Lorenzi, B.; et al. Thymidine phosphorylase expression in metastatic sites is predictive for response in patients with colorectal cancer treated with continuous oral capecitabine and biweekly oxaliplatin. Anticancer Drugs 2010, 21, 313–319. [Google Scholar] [CrossRef] [PubMed]
- De Bruin, M.; van Capel, T.; Van der Born, K.; Kruyt, F.A.; Fukushima, M.; Hoekman, K.; Pinedo, H.M.; Peters, G.J. Role of platelet-derived endothelial cell growth factor/thymidine phosphorylase in fluoropyrimidine sensitivity. Br. J. Cancer 2003, 88, 957–964. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meropol, N.J.; Gold, P.J.; Diasio, R.B.; Andria, M.; Dhami, M.; Godfrey, T.; Kovatich, A.J.; Lund, K.A.; Mitchell, E.; Schwarting, R. Thymidine phosphorylase expression is associated with response to capecitabine plus irinotecan in patients with metastatic colorectal cancer. J. Clin. Oncol. 2006, 24, 4069–4077. [Google Scholar] [CrossRef] [PubMed]
- Shigeta, K.; Ishii, Y.; Hasegawa, H.; Okabayashi, K.; Kitagawa, Y. Evaluation of 5-fluorouracil metabolic enzymes as predictors of response to adjuvant chemotherapy outcomes in patients with stage II/III colorectal cancer: A decision-curve analysis. World J. Surg. 2014, 38, 3248–3256. [Google Scholar] [CrossRef] [PubMed]
- Lindskog, E.B.; Derwinger, K.; Gustavsson, B.; Falk, P.; Wettergren, Y. Thymidine phosphorylase expression is associated with time to progression in patients with metastatic colorectal cancer. BMC Clin. Pathol. 2014, 14, 25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahn, M.J.; Choi, J.H.; Oh, H.S.; Lee, Y.Y.; Kim, I.S.; Choi, I.Y.; Lee, K.H.; Song, K.W.; Park, C.K. Thymidylate synthase, thymidine phosphorylase, VEGF and p53 protein expression in primary colorectal cancer for predicting response to 5-fluorouracil-based chemotherapy. Cancer Res. Treat. 2005, 37, 216–222. [Google Scholar] [CrossRef] [PubMed]
- Kugimiya, N.; Harada, E.; Suehiro, Y.; Suga, A.; Takemoto, Y.; Hamano, K. Determination of thymidine phosphorylase expression level facilitates recurrence risk stratification in stage II/III colorectal cancer following adjuvant chemotherapy with oral fluoropyrimidines. Oncol. Lett. 2019, 17, 5267–5274. [Google Scholar] [CrossRef] [Green Version]
- Goto, H.; Kohno, K.; Sone, S.; Akiyama, S.-i.; Kuwano, M.; Ono, M. Interferon γ-dependent Induction of Thymidine Phosphorylase/Platelet-derived Endothelial Growth Factor through γ-Activated Sequence-like Element in Human Macrophages. Cancer Res. 2001, 61, 469–473. [Google Scholar]
- Derwinger, K.; Lindskog, E.B.; Palmqvist, E.; Wettergren, Y. Changes in thymidine phosphorylase gene expression related to treatment of rectal cancer. Anticancer Res. 2013, 33, 2447–2451. [Google Scholar] [PubMed]
- Salonga, D.; Danenberg, K.D.; Johnson, M.; Metzger, R.; Groshen, S.; Tsao-Wei, D.D.; Lenz, H.J.; Leichman, C.G.; Leichman, L.; Diasio, R.B.; et al. Colorectal tumors responding to 5-fluorouracil have low gene expression levels of dihydropyrimidine dehydrogenase, thymidylate synthase, and thymidine phosphorylase. Clin. Cancer Res. 2000, 6, 1322–1327. [Google Scholar] [PubMed]
- Ishikawa, Y.; Kubota, T.; Otani, Y.; Watanabe, M.; Teramoto, T.; Kumai, K.; Takechi, T.; Okabe, H.; Fukushima, M.; Kitajima, M. Thymidylate synthetase and dihydropyrimidine dehydrogenase levels in gastric cancer. Anticancer Res. 1999, 19, 5635–5640. [Google Scholar] [PubMed]
- Huang, C.L.; Yokomise, H.; Kobayashi, S.; Fukushima, M.; Hitomi, S.; Wada, H. Intratumoral expression of thymidylate synthase and dihydropyrimidine dehydrogenase in non-small cell lung cancer patients treated with 5-FU-based chemotherapy. Int. J. Oncol. 2000, 17, 47–54. [Google Scholar] [CrossRef]
- Kobayashi, H.; Koike, T.; Nakatsuka, A.; Kurita, H.; Sagara, J.; Taniguchi, S.; Kurashina, K. Dihydropyrimidine dehydrogenase expression predicts survival outcome and chemosensitivity to 5-fluorouracil in patients with oral squamous cell carcinoma. Oral Oncol. 2005, 41, 38–47. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Diasio, R.B. Regulation of human dihydropyrimidine dehydrogenase: Implications in the pharmacogenetics of 5-FU-based chemotherapy. Pharmacogenomics 2007, 8, 257–265. [Google Scholar] [CrossRef]
- Amstutz, U.; Farese, S.; Aebi, S.; Largiader, C.R. Hypermethylation of the DPYD promoter region is not a major predictor of severe toxicity in 5-fluorouracil based chemotherapy. J. Exp. Clin. Cancer Res. 2008, 27, 54. [Google Scholar] [CrossRef] [Green Version]
- Zhang, X.; Li, L.; Fourie, J.; Davie, J.R.; Guarcello, V.; Diasio, R.B. The role of Sp1 and Sp3 in the constitutive DPYD gene expression. Biochim. Biophys. Acta 2006, 1759, 247–256. [Google Scholar] [CrossRef]
- Zhang, X.; Soong, R.; Wang, K.; Li, L.; Davie, J.R.; Guarcello, V.; Diasio, R.B. Suppression of DPYD expression in RKO cells via DNA methylation in the regulatory region of the DPYD promoter: A potentially important epigenetic mechanism regulating DPYD expression. Biochem. Cell Biol. 2007, 85, 337–346. [Google Scholar] [CrossRef]
- Cameron, E.E.; Bachman, K.E.; Myohanen, S.; Herman, J.G.; Baylin, S.B. Synergy of demethylation and histone deacetylase inhibition in the re-expression of genes silenced in cancer. Nat. Genet. 1999, 21, 103–107. [Google Scholar] [CrossRef]
- Wigle, T.J.; Tsvetkova, E.V.; Welch, S.A.; Kim, R.B. DPYD and Fluorouracil-Based Chemotherapy: Mini Review and Case Report. Pharmaceutics 2019, 11, 199. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Innocenti, F.; Mills, S.C.; Sanoff, H.; Ciccolini, J.; Lenz, H.J.; Milano, G. All You Need to Know About DPYD Genetic Testing for Patients Treated With Fluorouracil and Capecitabine: A Practitioner-Friendly Guide. JCO Oncol. Pract. 2020, 16, 793–798. [Google Scholar] [CrossRef] [PubMed]
- Miyamoto, S.; Ochiai, A.; Boku, N.; Ohtsu, A.; Tahara, M.; Yoshida, S.; Okabe, H.; Takechi, T.; Fukushima, M. Discrepancies between the gene expression, protein expression, and enzymatic activity of thymidylate synthase and dihydropyrimidine dehydrogenase in human gastrointestinal cancers and adjacent normal mucosa. Int. J. Oncol. 2001, 18, 705–713. [Google Scholar] [CrossRef] [PubMed]
- Johnston, S.J.; Ridge, S.A.; Cassidy, J.; McLeod, H.L. Regulation of dihydropyrimidine dehydrogenase in colorectal cancer. Clin. Cancer Res. 1999, 5, 2566–2570. [Google Scholar] [PubMed]
- Chai, J.; Dong, W.; Xie, C.; Wang, L.; Han, D.L.; Wang, S.; Guo, H.L.; Zhang, Z.L. MicroRNA-494 sensitizes colon cancer cells to fluorouracil through regulation of DPYD. IUBMB Life 2015, 67, 191–201. [Google Scholar] [CrossRef]
- Offer, S.M.; Butterfield, G.L.; Jerde, C.R.; Fossum, C.C.; Wegner, N.J.; Diasio, R.B. microRNAs miR-27a and miR-27b directly regulate liver dih.hydropyrimidine dehydrogenase expression through two conserved binding sites. Mol. Cancer Ther. 2014, 13, 742–751. [Google Scholar] [CrossRef] [Green Version]
- Wyatt, M.D.; Wilson, D.M., 3rd. Participation of DNA repair in the response to 5-fluorouracil. Cell. Mol. Life Sci. 2009, 66, 788–799. [Google Scholar] [CrossRef] [Green Version]
- Boland, C.R.; Goel, A. Microsatellite instability in colorectal cancer. Gastroenterology 2010, 138, 2073–2087.e3. [Google Scholar] [CrossRef]
- Kawakami, H.; Zaanan, A.; Sinicrope, F.A. Implications of mismatch repair-deficient status on management of early stage colorectal cancer. J. Gastrointest. Oncol. 2015, 6, 676–684. [Google Scholar] [CrossRef]
- Allan, R.E.; Luis, R.P.; Juan, P. Microsatellite instability in Costa Rican patients with colorectal adenocarcinoma and its association with overall survival and response to fluoropyrimidine-based chemotherapy. Cancer Epidemiol. 2020, 65, 101680. [Google Scholar] [CrossRef]
- Cancer Genome Atlas Network. Comprehensive molecular characterization of human colon and rectal cancer. Nature 2012, 487, 330–337. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hang, B.; Singer, B. Protein-protein interactions involving DNA glycosylases. Chem. Res. Toxicol. 2003, 16, 1181–1195. [Google Scholar] [CrossRef] [PubMed]
- Hagen, L.; Pena-Diaz, J.; Kavli, B.; Otterlei, M.; Slupphaug, G.; Krokan, H.E. Genomic uracil and human disease. Exp. Cell Res. 2006, 312, 2666–2672. [Google Scholar] [CrossRef] [PubMed]
- Yan, Y.; Han, X.; Qing, Y.; Condie, A.G.; Gorityala, S.; Yang, S.; Xu, Y.; Zhang, Y.; Gerson, S.L. Inhibition of uracil DNA glycosylase sensitizes cancer cells to 5-fluorodeoxyuridine through replication fork collapse-induced DNA damage. Oncotarget 2016, 7, 59299–59313. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huehls, A.M.; Huntoon, C.J.; Joshi, P.M.; Baehr, C.A.; Wagner, J.M.; Wang, X.; Lee, M.Y.; Karnitz, L.M. Genomically Incorporated 5-Fluorouracil that Escapes UNG-Initiated Base Excision Repair Blocks DNA Replication and Activates Homologous Recombination. Mol. Pharmacol. 2016, 89, 53–62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blondy, S.; David, V.; Verdier, M.; Mathonnet, M.; Perraud, A.; Christou, N. 5-Fluorouracil resistance mechanisms in colorectal cancer: From classical pathways to promising processes. Cancer Sci. 2020, 111, 3142–3154. [Google Scholar] [CrossRef] [PubMed]
- De la Cruz-Morcillo, M.A.; Valero, M.L.; Callejas-Valera, J.L.; Arias-Gonzalez, L.; Melgar-Rojas, P.; Galan-Moya, E.M.; Garcia-Gil, E.; Garcia-Cano, J.; Sanchez-Prieto, R. P38MAPK is a major determinant of the balance between apoptosis and autophagy triggered by 5-fluorouracil: Implication in resistance. Oncogene 2012, 31, 1073–1085. [Google Scholar] [CrossRef]
- Kulsum, S.; Sudheendra, H.V.; Pandian, R.; Ravindra, D.R.; Siddappa, G.; Nisheena, R.; Chevour, P.; Ramachandran, B.; Sagar, M.; Jayaprakash, A.; et al. Cancer stem cell mediated acquired chemoresistance in head and neck cancer can be abrogated by aldehyde dehydrogenase 1 A1 inhibition. Mol. Carcinogenes. 2017, 56, 694–711. [Google Scholar] [CrossRef]
- Das, P.K.; Islam, F.; Lam, A.K. The Roles of Cancer Stem Cells and Therapy Resistance in Colorectal Carcinoma. Cells 2020, 9, 1392. [Google Scholar] [CrossRef]
- Touil, Y.; Igoudjil, W.; Corvaisier, M.; Dessein, A.F.; Vandomme, J.; Monte, D.; Stechly, L.; Skrypek, N.; Langlois, C.; Grard, G.; et al. Colon cancer cells escape 5FU chemotherapy-induced cell death by entering stemness and quiescence associated with the c-Yes/YAP axis. Clin. Cancer Res. 2014, 20, 837–846. [Google Scholar] [CrossRef] [Green Version]
- Yang, H.; Li, X.D.; Zhou, Y.; Ban, X.; Zeng, T.T.; Li, L.; Zhang, B.Z.; Yun, J.; Xie, D.; Guan, X.Y.; et al. Stemness and chemotherapeutic drug resistance induced by EIF5A2 overexpression in esophageal squamous cell carcinoma. Oncotarget 2015, 6, 26079–26089. [Google Scholar] [CrossRef] [Green Version]
- Wang, B.; Ma, N.; Zheng, X.; Li, X.; Ma, X.; Hu, J.; Cao, B. GDF15 Repression Contributes to 5-Fluorouracil Resistance in Human Colon Cancer by Regulating Epithelial-Mesenchymal Transition and Apoptosis. Biomed. Res. Int. 2020, 2020, 2826010. [Google Scholar] [CrossRef] [PubMed]
- Romano, G.; Santi, L.; Bianco, M.R.; Giuffre, M.R.; Pettinato, M.; Bugarin, C.; Garanzini, C.; Savarese, L.; Leoni, S.; Cerrito, M.G.; et al. The TGF-beta pathway is activated by 5-fluorouracil treatment in drug resistant colorectal carcinoma cells. Oncotarget 2016, 7, 22077–22091. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sakowicz-Burkiewicz, M.; Przybyla, T.; Wesserling, M.; Bielarczyk, H.; Maciejewska, I.; Pawelczyk, T. Suppression of TWIST1 enhances the sensitivity of colon cancer cells to 5-fluorouracil. Int. J. Biochem. Cell Biol. 2016, 78, 268–278. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Hopson, L.M.; Singleton, S.S.; Yang, X.; Jogunoori, W.; Mazumder, R.; Obias, V.; Lin, P.; Nguyen, B.N.; Yao, M.; et al. Mice with Dysfunctional TGF-beta Signaling Develop Altered Intestinal Microbiome and Colorectal Cancer Resistant to 5FU. Biochim. Biophys. Acta Mol. Basis Dis. 2021, 1867, 166179. [Google Scholar] [CrossRef] [PubMed]
- Gottesman, M.M.; Fojo, T.; Bates, S.E. Multidrug resistance in cancer: Role of ATP-dependent transporters. Nat. Rev. Cancer 2002, 2, 48–58. [Google Scholar] [CrossRef] [Green Version]
- Zheng, H.C. The molecular mechanisms of chemoresistance in cancers. Oncotarget 2017, 8, 59950–59964. [Google Scholar] [CrossRef] [Green Version]
- Xie, T.; Geng, J.; Wang, Y.; Wang, L.; Huang, M.; Chen, J.; Zhang, K.; Xue, L.; Liu, X.; Mao, X.; et al. FOXM1 evokes 5-fluorouracil resistance in colorectal cancer depending on ABCC10. Oncotarget 2017, 8, 8574–8589. [Google Scholar] [CrossRef]
- Zheng, M.; Wang, H.; Zhang, H.; Ou, Q.; Shen, B.; Li, N.; Yu, B. The influence of the p53 gene on the in vitro chemosensitivity of colorectal cancer cells. J. Cancer Res. Clin. Oncol. 1999, 125, 357–360. [Google Scholar] [CrossRef]
- Pugacheva, E.N.; Ivanov, A.V.; Kravchenko, J.E.; Kopnin, B.P.; Levine, A.J.; Chumakov, P.M. Novel gain of function activity of p53 mutants: Activation of the dUTPase gene expression leading to resistance to 5-fluorouracil. Oncogene 2002, 21, 4595–4600. [Google Scholar] [CrossRef] [Green Version]
- Benhattar, J.; Cerottini, J.P.; Saraga, E.; Metthez, G.; Givel, J.C. p53 mutations as a possible predictor of response to chemotherapy in metastatic colorectal carcinomas. Int. J. Cancer 1996, 69, 190–192. [Google Scholar] [CrossRef]
- Xie, P.; Mo, J.L.; Liu, J.H.; Li, X.; Tan, L.M.; Zhang, W.; Zhou, H.H.; Liu, Z.Q. Pharmacogenomics of 5-fluorouracil in colorectal cancer: Review and update. Cell. Oncol. 2020, 43, 989–1001. [Google Scholar] [CrossRef] [PubMed]
- Yan, Y.; Qing, Y.; Pink, J.J.; Gerson, S.L. Loss of Uracil DNA Glycosylase Selectively Resensitizes p53-Mutant and -Deficient Cells to 5-FdU. Mol. Cancer Res. 2018, 16, 212–221. [Google Scholar] [CrossRef] [Green Version]
- Giaccia, A.J.; Kastan, M.B. The complexity of p53 modulation: Emerging patterns from divergent signals. Genes Dev. 1998, 12, 2973–2983. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Appella, E.; Anderson, C.W. Post-translational modifications and activation of p53 by genotoxic stresses. Eur. J. Biochem. 2001, 268, 2764–2772. [Google Scholar] [CrossRef] [PubMed]
- Sharpless, N.E.; DePinho, R.A. p53: Good cop/bad cop. Cell 2002, 110, 9–12. [Google Scholar] [CrossRef] [Green Version]
- Vogelstein, B.; Lane, D.; Levine, A.J. Surfing the p53 network. Nature 2000, 408, 307–310. [Google Scholar] [CrossRef]
- Yu, J.; Zhang, L.; Hwang, P.M.; Rago, C.; Kinzler, K.W.; Vogelstein, B. Identification and classification of p53-regulated genes. Proc. Natl. Acad. Sci. USA 1999, 96, 14517–14522. [Google Scholar] [CrossRef] [Green Version]
- Zhao, R.; Gish, K.; Murphy, M.; Yin, Y.; Notterman, D.; Hoffman, W.H.; Tom, E.; Mack, D.H.; Levine, A.J. Analysis of p53-regulated gene expression patterns using oligonucleotide arrays. Genes Dev. 2000, 14, 981–993. [Google Scholar] [CrossRef]
- Van Triest, B.; Pinedo, H.M.; Giaccone, G.; Peters, G.J. Downstream molecular determinants of response to 5-fluorouracil and antifolate thymidylate synthase inhibitors. Ann. Oncol. 2000, 11, 385–391. [Google Scholar] [CrossRef]
- Showler, M.S.; Weiser, B.P. A possible link to uracil DNA glycosylase in the synergistic action of HDAC inhibitors and thymidylate synthase inhibitors. J. Transl. Med. 2020, 18, 377. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.L.; Seo, Y.R. p53 regulation of DNA excision repair pathways. Mutagenesis 2002, 17, 149–156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Offer, H.; Wolkowicz, R.; Matas, D.; Blumenstein, S.; Livneh, Z.; Rotter, V. Direct involvement of p53 in the base excision repair pathway of the DNA repair machinery. FEBS Lett. 1999, 450, 197–204. [Google Scholar] [CrossRef]
- Offer, H.; Zurer, I.; Banfalvi, G.; Reha’k, M.; Falcovitz, A.; Milyavsky, M.; Goldfinger, N.; Rotter, V. p53 modulates base excision repair activity in a cell cycle-specific manner after genotoxic stress. Cancer Res. 2001, 61, 88–96. [Google Scholar]
- Zhou, J.; Ahn, J.; Wilson, S.H.; Prives, C. A role for p53 in base excision repair. EMBO J. 2001, 20, 914–923. [Google Scholar] [CrossRef] [Green Version]
- Shomori, K.; Sakatani, T.; Goto, A.; Matsuura, T.; Kiyonari, H.; Ito, H. Thymidine phosphorylase expression in human colorectal mucosa, adenoma and carcinoma: Role of p53 expression. Pathol. Int. 1999, 49, 491–499. [Google Scholar] [CrossRef]
- Gokare, P.; Finnberg, N.K.; Abbosh, P.H.; Dai, J.; Murphy, M.E.; El-Deiry, W.S. P53 represses pyrimidine catabolic gene dihydropyrimidine dehydrogenase (DPYD) expression in response to thymidylate synthase (TS) targeting. Sci. Rep. 2017, 7, 9711. [Google Scholar] [CrossRef] [Green Version]
- Zhang, N.; Yin, Y.; Xu, S.J.; Chen, W.S. 5-Fluorouracil: Mechanisms of resistance and reversal strategies. Molecules 2008, 13, 1551–1569. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.H.; Park, J.H.; Jung, Y.; Kim, J.H.; Jong, H.S.; Kim, T.Y.; Bang, Y.J. Histone deacetylase inhibitor enhances 5-fluorouracil cytotoxicity by down-regulating thymidylate synthase in human cancer cells. Mol. Cancer Ther. 2006, 5, 3085–3095. [Google Scholar] [CrossRef] [Green Version]
- Crea, F.; Nobili, S.; Paolicchi, E.; Perrone, G.; Napoli, C.; Landini, I.; Danesi, R.; Mini, E. Epigenetics and chemoresistance in colorectal cancer: An opportunity for treatment tailoring and novel therapeutic strategies. Drug Resist. Updates 2011, 14, 280–296. [Google Scholar] [CrossRef]
- Terranova-Barberio, M.; Roca, M.S.; Zotti, A.I.; Leone, A.; Bruzzese, F.; Vitagliano, C.; Scogliamiglio, G.; Russo, D.; D’Angelo, G.; Franco, R.; et al. Valproic acid potentiates the anticancer activity of capecitabine in vitro and in vivo in breast cancer models via induction of thymidine phosphorylase expression. Oncotarget 2016, 7, 7715–7731. [Google Scholar] [CrossRef] [PubMed]
- Fazzone, W.; Wilson, P.M.; Labonte, M.J.; Lenz, H.J.; Ladner, R.D. Histone deacetylase inhibitors suppress thymidylate synthase gene expression and synergize with the fluoropyrimidines in colon cancer cells. Int. J. Cancer 2009, 125, 463–473. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Piro, G.; Roca, M.S.; Bruzzese, F.; Carbone, C.; Iannelli, F.; Leone, A.; Volpe, M.G.; Budillon, A.; Di Gennaro, E. Vorinostat Potentiates 5-Fluorouracil/Cisplatin Combination by Inhibiting Chemotherapy-Induced EGFR Nuclear Translocation and Increasing Cisplatin Uptake. Mol. Cancer Ther. 2019, 18, 1405–1417. [Google Scholar] [CrossRef]
- Iveland, T.S.; Hagen, L.; Sharma, A.; Sousa, M.M.L.; Sarno, A.; Wollen, K.L.; Liabakk, N.B.; Slupphaug, G. HDACi mediate UNG2 depletion, dysregulated genomic uracil and altered expression of oncoproteins and tumor suppressors in B- and T-cell lines. J. Transl. Med. 2020, 18, 159. [Google Scholar] [CrossRef] [PubMed]
- Bao, Y.; Tong, L.; Song, B.; Liu, G.; Zhu, Q.; Lu, X.; Zhang, J.; Lu, Y.F.; Wen, H.; Tian, Y.; et al. UNG2 deacetylation confers cancer cell resistance to hydrogen peroxide-induced cytotoxicity. Free Radic. Biol. Med. 2020, 160, 403–417. [Google Scholar] [CrossRef] [PubMed]
- Alzoubi, S.; Brody, L.; Rahman, S.; Mahul-Mellier, A.L.; Mercado, N.; Ito, K.; El-Bahrawy, M.; Silver, A.; Boobis, A.; Bell, J.D.; et al. Synergy between histone deacetylase inhibitors and DNA-damaging agents is mediated by histone deacetylase 2 in colorectal cancer. Oncotarget 2016, 7, 44505–44521. [Google Scholar] [CrossRef] [Green Version]
- Muller, B.M.; Jana, L.; Kasajima, A.; Lehmann, A.; Prinzler, J.; Budczies, J.; Winzer, K.J.; Dietel, M.; Weichert, W.; Denkert, C. Differential expression of histone deacetylases HDAC1, 2 and 3 in human breast cancer--overexpression of HDAC2 and HDAC3 is associated with clinicopathological indicators of disease progression. BMC Cancer 2013, 13, 215. [Google Scholar] [CrossRef] [Green Version]
- Spurling, C.C.; Godman, C.A.; Noonan, E.J.; Rasmussen, T.P.; Rosenberg, D.W.; Giardina, C. HDAC3 overexpression and colon cancer cell proliferation and differentiation. Mol. Carcinogenes. 2008, 47, 137–147. [Google Scholar] [CrossRef] [PubMed]
- Minami, J.; Suzuki, R.; Mazitschek, R.; Gorgun, G.; Ghosh, B.; Cirstea, D.; Hu, Y.; Mimura, N.; Ohguchi, H.; Cottini, F.; et al. Histone deacetylase 3 as a novel therapeutic target in multiple myeloma. Leukemia 2014, 28, 680–689. [Google Scholar] [CrossRef] [Green Version]
- Roca, M.S.; Di Gennaro, E.; Budillon, A. Implication for Cancer Stem Cells in Solid Cancer Chemo-Resistance: Promising Therapeutic Strategies Based on the Use of HDAC Inhibitors. J. Clin. Med. 2019, 8, 912. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guarcello, V.; Blanquicett, C.; Naguib, F.N.; El Kouni, M.H. Suppression of thymidine phosphorylase expression by promoter methylation in human cancer cells lacking enzyme activity. Cancer Chemother. Pharmacol. 2008, 62, 85–96. [Google Scholar] [CrossRef] [PubMed]
- Puppin, C.; Puglisi, F.; Pandolfi, M.; Di Loreto, C.; Damante, G. Histone deacetylase inhibitors induce thymidine phosphorylase expression in cultured breast cancer cell lines. Oncol. Rep. 2011, 26, 309–314. [Google Scholar] [CrossRef] [PubMed]
- Nishizawa, Y.; Ikeda, R.; Yamamoto, M.; Kawahara, K.; Shinsato, Y.; Minami, K.; Nitta, M.; Terazono, H.; Akiyama, S.I.; Furukawa, T.; et al. 5-Aza-2-deoxycytidine Enhances the Sensitivity of 5-Fluorouracil by Demethylation of the Thymidine Phosphorylase Promoter. Anticancer Res. 2019, 39, 4129–4136. [Google Scholar] [CrossRef] [PubMed]
- Peng, W.; Zhang, H.; Tan, S.; Li, Y.; Zhou, Y.; Wang, L.; Liu, C.; Li, Q.; Cen, X.; Yang, S.; et al. Synergistic antitumor effect of 5-fluorouracil with the novel LSD1 inhibitor ZY0511 in colorectal cancer. Ther. Adv. Med. Oncol. 2020, 12, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Wu, R.; Nie, Q.; Tapper, E.E.; Jerde, C.R.; Dunlap, G.S.; Shrestha, S.; Elraiyah, T.A.; Offer, S.M.; Diasio, R.B. Histone H3K27 Trimethylation Modulates 5-Fluorouracil Resistance by Inhibiting PU.1 Binding to the DPYD Promoter. Cancer Res. 2016, 76, 6362–6373. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Manzotti, G.; Ciarrocchi, A.; Sancisi, V. Inhibition of BET Proteins and Histone Deacetylase (HDACs): Crossing Roads in Cancer Therapy. Cancers 2019, 11, 304. [Google Scholar] [CrossRef] [Green Version]
- Cheng, X.; Huang, Z.; Long, D.; Jin, W. BET inhibitor bromosporine enhances 5-FU effect in colorectal cancer cells. Biochem. Biophys. Res. Commun. 2020, 521, 840–845. [Google Scholar] [CrossRef]
- Tan, X.; Tong, J.; Wang, Y.J.; Fletcher, R.; Schoen, R.E.; Yu, J.; Shen, L.; Zhang, L. BET Inhibitors Potentiate Chemotherapy and Killing of SPOP-Mutant Colon Cancer Cells via Induction of DR5. Cancer Res. 2019, 79, 1191–1203. [Google Scholar] [CrossRef] [Green Version]
- Mazur, P.K.; Herner, A.; Mello, S.S.; Wirth, M.; Hausmann, S.; Sanchez-Rivera, F.J.; Lofgren, S.M.; Kuschma, T.; Hahn, S.A.; Vangala, D.; et al. Combined inhibition of BET family proteins and histone deacetylases as a potential epigenetics-based therapy for pancreatic ductal adenocarcinoma. Nat. Med. 2015, 21, 1163–1171. [Google Scholar] [CrossRef] [Green Version]
- Huan, S.; Gui, T.; Xu, Q.; Zhuang, S.; Li, Z.; Shi, Y.; Lin, J.; Gong, B.; Miao, G.; Tam, M.; et al. Combination BET Family Protein and HDAC Inhibition Synergistically Elicits Chondrosarcoma Cell Apoptosis through RAD51-Related DNA Damage Repair. Cancer Manag. Res. 2020, 12, 4429–4439. [Google Scholar] [CrossRef]
- Fakih, M.G.; Pendyala, L.; Fetterly, G.; Toth, K.; Zwiebel, J.A.; Espinoza-Delgado, I.; Litwin, A.; Rustum, Y.M.; Ross, M.E.; Holleran, J.L.; et al. A phase I, pharmacokinetic and pharmacodynamic study on vorinostat in combination with 5-fluorouracil, leucovorin, and oxaliplatin in patients with refractory colorectal cancer. Clin. Cancer Res. 2009, 15, 3189–3195. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilson, P.M.; El-Khoueiry, A.; Iqbal, S.; Fazzone, W.; LaBonte, M.J.; Groshen, S.; Yang, D.; Danenberg, K.D.; Cole, S.; Kornacki, M.; et al. A phase I/II trial of vorinostat in combination with 5-fluorouracil in patients with metastatic colorectal cancer who previously failed 5-FU-based chemotherapy. Cancer Chemother. Pharmacol. 2010, 65, 979–988. [Google Scholar] [CrossRef] [PubMed]
- Fakih, M.G.; Groman, A.; McMahon, J.; Wilding, G.; Muindi, J.R. A randomized phase II study of two doses of vorinostat in combination with 5-FU/LV in patients with refractory colorectal cancer. Cancer Chemother. Pharmacol. 2012, 69, 743–751. [Google Scholar] [CrossRef] [PubMed]
- Avallone, A.; Piccirillo, M.C.; Di Gennaro, E.; Romano, C.; Calabrese, F.; Roca, M.S.; Tatangelo, F.; Granata, V.; Cassata, A.; Cavalcanti, E.; et al. Randomized phase II study of valproic acid in combination with bevacizumab and oxaliplatin/fluoropyrimidine regimens in patients with RAS-mutated metastatic colorectal cancer: The REVOLUTION study protocol. Ther. Adv. Med. Oncol. 2020, 12, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Peacock, N.W.; Jones, S.F.; Yardley, D.A.; Bendell, J.C.; Infante, J.R.; Murphy, P.B.; Burris, H.A.B., III. A phase I study of panobinostat (LBH589) with capecitabine with or without lapatinib. J. Clin. Oncol. 2010, 28, 1115. [Google Scholar] [CrossRef]
- Munster, P.; Marchion, D.; Bicaku, E.; Lacevic, M.; Kim, J.; Centeno, B.; Daud, A.; Neuger, A.; Minton, S.; Sullivan, D. Clinical and biological effects of valproic acid as a histone deacetylase inhibitor on tumor and surrogate tissues: Phase I/II trial of valproic acid and epirubicin/FEC. Clin. Cancer Res. 2009, 15, 2488–2496. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yoo, C.; Ryu, M.H.; Na, Y.S.; Ryoo, B.Y.; Lee, C.W.; Maeng, J.; Kim, S.Y.; Koo, D.H.; Park, I.; Kang, Y.K. Phase I and pharmacodynamic study of vorinostat combined with capecitabine and cisplatin as first-line chemotherapy in advanced gastric cancer. Investig. New Drugs 2014, 32, 271–278. [Google Scholar] [CrossRef] [PubMed]
- Yoo, C.; Ryu, M.H.; Na, Y.S.; Ryoo, B.Y.; Lee, C.W.; Kang, Y.K. Vorinostat in combination with capecitabine plus cisplatin as a first-line chemotherapy for patients with metastatic or unresectable gastric cancer: Phase II study and biomarker analysis. Br. J. Cancer 2016, 114, 1185–1190. [Google Scholar] [CrossRef] [Green Version]
- Iwahashi, S.; Utsunomiya, T.; Imura, S.; Morine, Y.; Ikemoto, T.; Arakawa, Y.; Saito, Y.; Ishikawa, D.; Shimada, M. Effects of valproic acid in combination with S-1 on advanced pancreatobiliary tract cancers: Clinical study phases I/II. Anticancer Res. 2014, 34, 5187–5191. [Google Scholar]
- Chan, E.; Arlinghaus, L.R.; Cardin, D.B.; Goff, L.; Berlin, J.D.; Parikh, A.; Abramson, R.G.; Yankeelov, T.E.; Hiebert, S.; Merchant, N.; et al. Phase I trial of vorinostat added to chemoradiation with capecitabine in pancreatic cancer. Radiother. Oncol. 2016, 119, 312–318. [Google Scholar] [CrossRef] [Green Version]
- Tang, P.; Oza, A.; Townsley, C.; Siu, L.; Pond, G.; Sarveswaran, P.; Webster, S.; Zwiebel, J.; Chen, E. A phase I study of vorinostat (VOR) in combination with capecitabine (CAP) in patients (pts) with advanced solid tumors. J. Clin. Oncol. 2007, 25, 3576. [Google Scholar] [CrossRef]
- Northfelt, D.W.; Marschke, R.F.M., Jr.; Bonnem, E.; Ooi, C.E.; Gerwien, R.; Hawthorne, T.; Clarke, A.; Buhl-Jensen, P.; Hoff, D.V.; Grem, J. A phase Ib/II study of PXD101 alone and in combination with 5-fluorouracil in patients with advanced solid tumors. J. Clin. Oncol. 2007, 25, 3501. [Google Scholar] [CrossRef]
- Budillon, A.; Delrio, P.; Pecori, B.; Tatangelo, F.; Di Gennaro, E.; Romano, C.; D’Angelo, V.; Marone, P.; Granata, C.; Cavalacanti, E.; et al. Phase I/II study of valproic acid (VPA) and short-course radiotherapy (SCRT) plus capecitabine (CAP) as preoperative treatment in low-moderate risk rectal cancer (V-shoRT-R3). In Proceedings of the Annals of Oncology—ESMO 2018 Congress, Munich, Germany, 19–23 October 2018; pp. VIII167–VIII168. [Google Scholar]
- James, E.S.; Chung, G.; Sowers, N.M.; Clark, M.B.; Lilian, R.; Abraham, G.; Chmael, S.; Cappiello, M.; DiGiovanna, M.; Hofstatter, E.W.; et al. Phase I study of the HDAC inhibitor vorinostat in combination with capecitabine in a biweekly schedule in advanced breast cancer. J. Clin. Oncol. 2013, 31, 154. [Google Scholar] [CrossRef]
- Fetterly, G.J.; Brady, W.E.; LeVea, C.M.; Litwin, A.M.; Zagst, P.D.; Prey, J.D.; Tarquini, M.; Giardina, M.K.; Iyer, R.V.; Khushalani, N.I. A phase I pharmacokinetic (PK) study of vorinostat (V) in combination with irinotecan (I), 5-fluorouracil (5FU), and leucovorin (FOLFIRI) in advanced upper gastrointestinal cancers (AGC). J. Clin. Oncol. 2009, 27, e15540. [Google Scholar] [CrossRef]
- Ueno, H.; Ioka, T.; Ikeda, M.; Ohkawa, S.; Yanagimoto, H.; Boku, N.; Fukutomi, A.; Sugimori, K.; Baba, H.; Yamao, K.; et al. Randomized phase III study of gemcitabine plus S-1, S-1 alone, or gemcitabine alone in patients with locally advanced and metastatic pancreatic cancer in Japan and Taiwan: GEST study. J. Clin. Oncol. 2013, 31, 1640–1648. [Google Scholar] [CrossRef] [PubMed]


| Trial | Phase | Setting | Regimen | Status | Ref | |
|---|---|---|---|---|---|---|
| Multiorgan | Vorinostat and Capecitabine in Treating Patients With Metastatic or Unresectable Solid Tumors | Phase I | Unresectable or metastatic solid tumors | Vorinostat + capecitabine | ClinicalTrials.gov: NCT00121277 | |
| Study of PXD101 Alone and in Combination With 5-Fluorouracil (5-FU) in Patients With Advanced Solid Tumors | Phase I | Belinostat (PXD101) + 5-fluorouracil | ClinicalTrials.gov: NCT00413322 | |||
| Colorectal cancer | A Phase I, Pharmacokinetic, and Pharmacodynamic Study of Vorinostat in Combination with 5-Fluorouracil, Leucovorin, and Oxaliplatin in Patients with Refractory Colorectal | Phase I | Refractory colorectal | Vorinostat and 5-fluorouracil + leucovorin + oxaliplatin | Published | [152] |
| A phase I/II trial of vorinostat in combination with 5-fluorouracil in patients with metastatic colorectal cancer who previously failed 5-FU-based chemotherapy | Phase I/II | Metastatic colorectal who had failed all standard therapeutic options | Vorinostat + 5-FU/LV | Published | [153] | |
| Vorinostat, Fluorouracil, and Leucovorin Calcium in Treating Patients With Metastatic Colorectal Cancer That Has Not Responded to Previous Treatment | Phase II | Adenocarcinoma of the colon and rectum Recurrent colon cancer and rectal cancer Stage IV colon and rectal cancer | Vorinostat + 5-FU/LV | Published | ClinicalTrials.gov: NCT00942266. [154] | |
| Preoperative Valproic Acid and Radiation Therapy for Rectal Cancer | Phase I/II | Rectal cancer | Preoperative radiation therapy + valproic acid + capecitabine | Recruiting | ClinicalTrials.gov: NCT01898104 [28] | |
| Valproic Acid in Combination With Bevacizumab and Oxaliplatin/Fluoropyrimidine Regimens in Patients With Ras-mutated Metastatic Colorectal Cancer | Phase II | Ras-mutated metastatic colorectal cancer | Bevacizumab + mFOLFOX6 or mOXXEL regimen + valproic acid | Recruiting | ClinicalTrials.gov: NCT04310176 [155] | |
| Breast | LBH589 in Combination With Capecitabine Plus/Minus (±) Lapatinib in Breast Cancer Patients | Phase I | Refractory and advanced breast cancer sensitive to 5-fluorouracil | Panobinostat + capecitabine + lapatinib | Completed | ClinicalTrials.gov: NCT00632489 [156] |
| HDAC Inhibitor Vorinostat (SAHA) With Capecitabine (Xeloda) Using a New Weekly Dose Regimen for Advanced Breast Cancer | Phase I | Advanced breast cancer | Vorinostat + capecitabine | Completed | ClinicalTrials.gov: NCT00719875 | |
| A Pilot Study of the Combination of Entinostat With Capecitabine in High Risk Breast Cancer After Neo-adjuvant Therapy | Phase I | Metastatic breast cancer | Entinostat + capecitabine | Recruiting | ClinicalTrials.gov: NCT03473639 | |
| Phase I Trial of Valproic Acid and Epirubicin in Solid Tumor Malignancies | Phase I/II | Neoplasms, advanced (breast) | Valproic acid + FEC (epirubicin, 5-fluorouracil; cyclophosphamide) | Completed | ClinicalTrials.gov: NCT00246103 [157] | |
| Valproic Acid in Combination With FEC100 for Primary Therapy in Patients With Breast Cancer | Phase II | Breast cancer | VPA + FEC100 | Terminated | ClinicalTrials.gov: NCT01010854 | |
| Gastric | Vorinostat, Irinotecan, Fluorouracil, and Leucovorin in Treating Patients With Advanced Upper Gastrointestinal Cancer | Phase I | Esophageal; gastric; liver cancer | Vorinostat + 5-fluorouracil + irinotecan hydrochloride + leucovorin calcium | Completed | ClinicalTrials.gov: NCT00537121 |
| Study of Vorinostat Plus Capecitabine (X) and Cisplatin (P) for 1st Line Treatment of Metastatic or Recurrent Gastric Cancer: Zolinza+XP | Phase I/II | Gastric cancer | Vorinostat + capecitabine + cisplatin | Completed | ClinicalTrials.gov: NCT01045538 [158,159] | |
| Pancreas | Effects of Valproic Acid in Combination with S-1 on Advanced Pancreatobiliary Tract Cancers: Clinical Study Phases I/II | Phase I/II | Advanced pancreatobiliary tract cancers | VPA + tegafur | Published | [160] |
| Capecitabine, Vorinostat, and Radiation Therapy in Treating Patients With Nonmetastatic Pancreatic Cancer | Phase I | Nonmetastatic pancreatic cancers | Vorinostat + capecitabine + radiotherapy + surgery | Completed | ClinicalTrials.gov: NCT00983268 [161] | |
| Vorinostat With XRT and 5-FU for Locally Advanced Adenocarcinoma of the Pancreas | Phase I/II | Pancreas adenocarcinoma | Vorinostat + radiation therapy + 5-FU | Terminated | ClinicalTrials.gov: NCT00948688 | |
| A Study of Entinostat and FOLFOX in Subjects With Pancreatic Adenocarcinoma | Phase I | Pancreas cancer | Entinostat + FOLFOX regimen | Not yet recruiting | ClinicalTrials.gov: NCT03760614 | |
| Head and neck | Capecitabine and Vorinostat in Treating Patients With Recurrent and/or Metastatic Head and Neck Cancer | Phase II | HNSCC | Vorinostat + capecitabine | Terminated | ClinicalTrials.gov: NCT01267240 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grumetti, L.; Lombardi, R.; Iannelli, F.; Pucci, B.; Avallone, A.; Di Gennaro, E.; Budillon, A. Epigenetic Approaches to Overcome Fluoropyrimidines Resistance in Solid Tumors. Cancers 2022, 14, 695. https://doi.org/10.3390/cancers14030695
Grumetti L, Lombardi R, Iannelli F, Pucci B, Avallone A, Di Gennaro E, Budillon A. Epigenetic Approaches to Overcome Fluoropyrimidines Resistance in Solid Tumors. Cancers. 2022; 14(3):695. https://doi.org/10.3390/cancers14030695
Chicago/Turabian StyleGrumetti, Laura, Rita Lombardi, Federica Iannelli, Biagio Pucci, Antonio Avallone, Elena Di Gennaro, and Alfredo Budillon. 2022. "Epigenetic Approaches to Overcome Fluoropyrimidines Resistance in Solid Tumors" Cancers 14, no. 3: 695. https://doi.org/10.3390/cancers14030695







