Exploring Posttraumatic Stress Symptoms and Posttraumatic Growth among Children Living beyond Cancer and Their Parents Using an Actor–Partner Interdependence Model
Abstract
:Simple Summary
Abstract
1. Introduction
- (1)
- describing PTSS and PTG in children living beyond cancer and their parents and exploring the relationships between these variables; and,
- (2)
- examining actor and partner effects of PTSS and PTG for children living beyond cancer and their parents.
2. Materials and Methods
2.1. Participants
2.2. Procedures
2.3. Measures
2.3.1. Socio-Demographic and Medical Information
2.3.2. Posttraumatic Stress Symptoms (PTSS)
2.3.3. Posttraumatic Growth (PTG)
2.4. Statistical Analyses
3. Results
3.1. Participants
3.2. Describing PTSS and PTG in Children and Their Parents and Exploring the Relationship between These Variables (Objective 1)
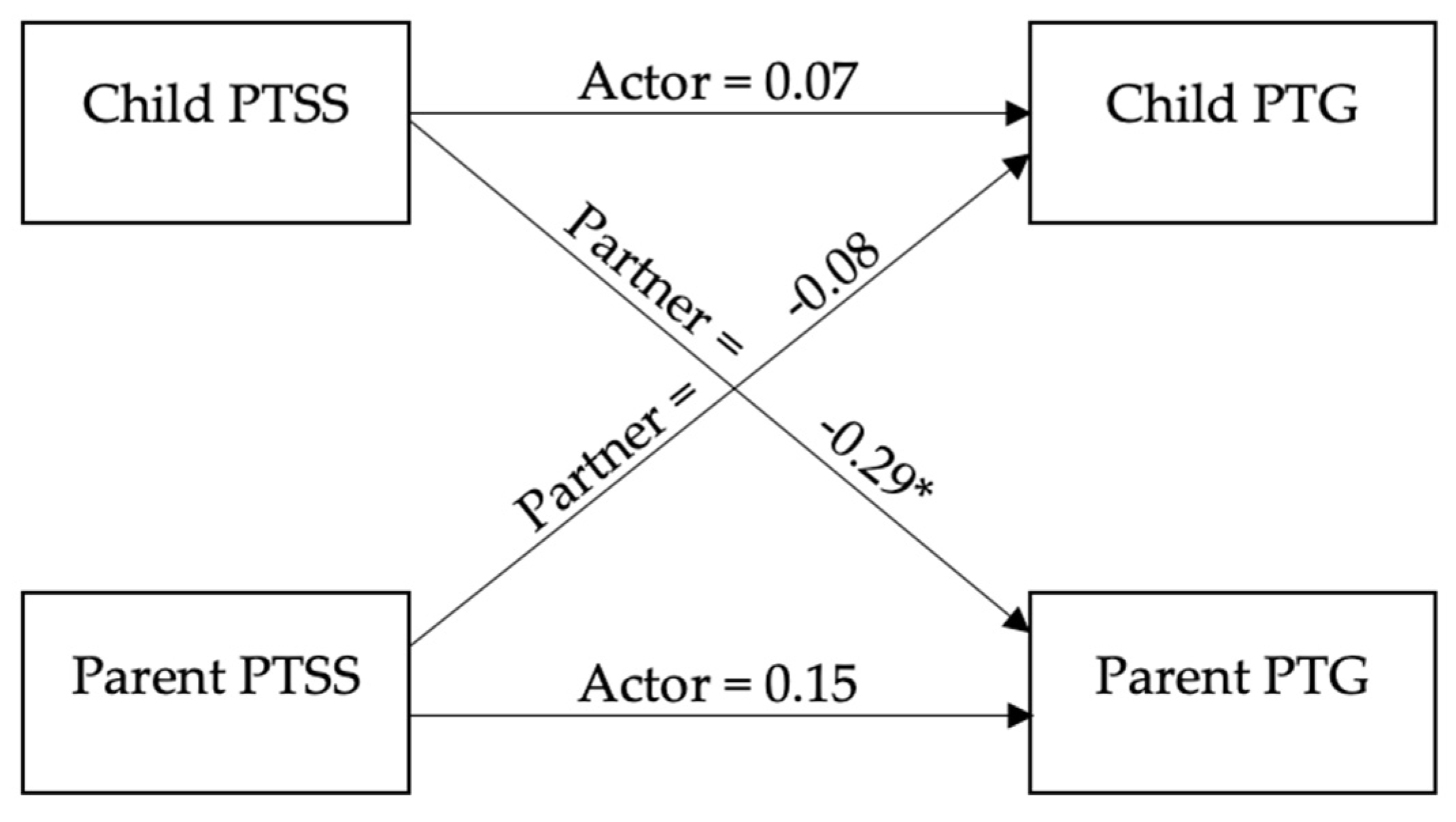
3.3. Examining the Actor and Partner Effects of PTSS on PTG for Children and Parents (Objective 2)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Long, K.A.; Marsland, A.L. Family Adjustment to Childhood Cancer: A Systematic Review. Clin. Child Fam. Psychol. Rev. 2011, 14, 57–88. [Google Scholar] [CrossRef] [PubMed]
- Blaauwbroek, R.; Groenier, K.H.; Kamps, W.A.; Jong, B.M.-D.; Postma, A. Late Effects in Adult Survivors of Childhood Cancer: The Need for Life-Long Follow-Up. Ann. Oncol. 2007, 18, 1898–1902. [Google Scholar] [CrossRef] [PubMed]
- Sohn, I.J.; Han, J.W.; Hahn, S.M.; Song, D.H.; Lyu, C.J.; Cheon, K.-A. Factors Associated with Emotional Distress in Children and Adolescents During Early Treatment for Cancer. Yonsei Med. J. 2017, 58, 816–822. [Google Scholar] [CrossRef] [PubMed]
- Roser, K.; Erdmann, F.; Michel, G.; Winther, J.F.; Mader, L. The Impact of Childhood Cancer on Parents’ Socio-Economic Situation-a Systematic Review. Psychooncology 2019, 28, 1207–1226. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Warmerdam, J.; Zabih, V.; Kurdyak, P.; Sutradhar, R.; Nathan, P.C.; Gupta, S. Prevalence of Anxiety, Depression, and Posttraumatic Stress Disorder in Parents of Children with Cancer: A Meta-Analysis. Pediatr. Blood Cancer 2019, 66, e27677. [Google Scholar] [CrossRef] [PubMed]
- Ljungman, L.; Hovén, E.; Ljungman, G.; Cernvall, M.; von Essen, L. Does Time Heal All Wounds? A Longitudinal Study of the Development of Posttraumatic Stress Symptoms in Parents of Survivors of Childhood Cancer and Bereaved Parents. Psychooncology 2015, 24, 1792–1798. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klosky, J.L.; Krull, K.R.; Kawashima, T.; Leisenring, W.; Randolph, M.E.; Zebrack, B.; Stuber, M.L.; Robison, L.L.; Phipps, S. Relations between Posttraumatic Stress and Posttraumatic Growth in Long-Term Survivors of Childhood Cancer: A Report from the Childhood Cancer Survivor Study. Health Psychol. 2014, 33, 878–882. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bruce, M. A Systematic and Conceptual Review of Posttraumatic Stress in Childhood Cancer Survivors and Their Parents. Clin. Psychol. Rev. 2006, 26, 233–256. [Google Scholar] [CrossRef] [PubMed]
- Stanton, A.L.; Bower, J.E.; Low, C.A. Posttraumatic Growth after Cancer. In Handbook of Posttraumatic Growth: Research and Practice; Calhoun, L.G., Tedeschi, R.G., Eds.; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 2006; pp. 138–175. [Google Scholar]
- Affleck, G.; Tennen, H. Construing Benefits from Adversity: Adaptational Significance and Dispositional Underpinnings. J. Pers. 1996, 64, 899–922. [Google Scholar] [CrossRef] [PubMed]
- Picoraro, J.A.; Womer, J.W.; Kazak, A.E.; Feudtner, C. Posttraumatic Growth in Parents and Pediatric Patients. J. Palliat. Med. 2014, 17, 209–218. [Google Scholar] [CrossRef]
- Tedeschi, R.G.; Calhoun, L.G. Posttraumatic Growth: Conceptual Foundations and Empirical Evidence. Psychol. Inq. 2004, 15, 1–18. [Google Scholar] [CrossRef]
- Arnedo, C.O.; Sánchez, N.; Sumalla, E.C.; Casellas-Grau, A. Stress and Growth in Cancer: Mechanisms and Psychotherapeutic Interventions to Facilitate a Constructive Balance. Front. Psychol. 2019, 10, 177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arpawong, T.E.; Oland, A.; Milam, J.E.; Ruccione, K.; Meeske, K.A. Post-Traumatic Growth among an Ethnically Diverse Sample of Adolescent and Young Adult Cancer Survivors. Psychooncology 2013, 22, 2235–2244. [Google Scholar] [CrossRef] [PubMed]
- Tremolado, M.; Bonichini, S.; Basso, G.; Pillon, M. Post-Traumatic Stress Symptoms and Post-Traumatic Growth in 223 Childhood Cancer Survivors: Predictive Risk Factors. Front. Psychol. 2016, 7, 287. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilson, J.Z.; Marin, D.; Maxwell, K.; Cumming, J.; Berger, R.; Saini, S.; Ferguson, W.; Chibnall, J.T. Association of Posttraumatic Growth and Illness-Related Burden with Psychosocial Factors of Patient, Family, and Provider in Pediatric Cancer Survivors. J. Trauma. Stress 2016, 29, 448–456. [Google Scholar] [CrossRef] [PubMed]
- Yi, J.; Kim, M.A. Postcancer Experiences of Childhood Cancer Survivors: How is Posttraumatic Stress Related to Posttraumatic Growth? J. Trauma. Stress 2014, 27, 461–467. [Google Scholar] [CrossRef]
- Michel, G.; Taylor, N.; Absolom, K.; Eiser, C. Benefit Finding in Survivors of Childhood Cancer and Their Parents: Further Empirical Support for the Benefit Finding Scale for Children. Child Care Health Dev. 2010, 36, 123–129. [Google Scholar] [CrossRef]
- Koutná, V.; Jelínek, M.; Blatný, M.; Kepák, T. Predictors of Posttraumatic Stress and Posttraumatic Growth in Childhood Cancer Survivors. Cancers 2017, 9, 26. [Google Scholar] [CrossRef] [Green Version]
- Barakat, L.P.; Alderfer, M.A.; Kazak, A.E. Posttraumatic Growth in Adolescent Survivors of Cancer and Their Mothers and Fathers. J. Pediatr. Psychol. 2006, 31, 413–419. [Google Scholar] [CrossRef]
- Morris, A.; Gabert-Quillen, C.; Delahanty, D. The Association between Parent PTSD/Depression Symptoms and Child PTSD Symptoms: A Meta-Analysis. J. Pediatr. Psychol. 2012, 37, 1076–1088. [Google Scholar] [CrossRef] [Green Version]
- Sharp, K.M.H.; Willard, V.W.; Barnes, S.; Tillery, R.; Long, A.; Phipps, S. Emotion Socialization in the Context of Childhood Cancer: Perceptions of Parental Support Promotes Posttraumatic Growth. J. Pediatr. Psychol. 2017, 42, 95–103. [Google Scholar]
- Ozono, S.; Saeki, T.; Mantani, T.; Ogata, A.; Okamura, H.; Yamawaki, S. Factors Related to Posttraumatic Stress in Adolescent Survivors of Childhood Cancer and Their Parents. Support Care Cancer 2007, 15, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Langeveld, N.E.; Grootenhuis, M.A.; Voute, P.A.; de Haan, R.J. Posttraumatic Stress Symptoms in Adult Survivors of Childhood Cancer. Pediatr. Blood Cancer 2004, 42, 604–610. [Google Scholar] [CrossRef] [PubMed]
- Schepers, S.A.; Okado, Y.; Russell, K.; Long, A.M.; Phipps, S. Adjustment in Childhood Cancer Survivors, Healthy Peers, and Their Parents: The Mediating Role of the Parent-Child Relationship. J. Pediatr. Psychol. 2019, 44, 186–196. [Google Scholar] [CrossRef]
- Tillery, R.; Willard, V.W.; Sharp, K.M.H.; Klages, K.L.; Long, A.M.; Phipps, S. Impact of the Parent-Child Relationship on Psychological and Social Resilience in Pediatric Cancer Patients. Psychooncology 2020, 29, 339–346. [Google Scholar] [CrossRef]
- Kenny, D.A. Models of Non-Independence in Dyadic Research. J. Soc. Pers. Relatsh. 1996, 13, 279–294. [Google Scholar] [CrossRef]
- Kenny, D.A.; Cook, W. Partner Effects in Relationship Research: Conceptual Issues, Analytic Difficulties, and Illustrations. Pers. Relatsh. 2005, 6, 433–448. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research Electronic Data Capture (Redcap)—A Metadata-Driven Methodology and Workflow Process for Providing Translational Research Informatics Support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [Green Version]
- Kazak, A.E.; Hocking, M.; Ittenbach, R.F.; Meadows, A.T.; Hobbie, W.; DeRosa, B.W.; Leahey, A.; Kersun, L.; Reilly, A. A Revision of the Intensity of Treatment Rating Scale: Classifying the Intensity of Pediatric Cancer Treatment. Pediatr. Blood Cancer 2012, 59, 96–99. [Google Scholar] [CrossRef] [Green Version]
- Foa, E.B.; Johnson, K.M.; Feeny, N.C.; Treadwell, K.R.H. The Child PTSD Symptom Scale: A Preliminary Examination of Its Psychometric Properties. J. Clin. Child Psychol. 2001, 30, 376–384. [Google Scholar] [CrossRef]
- Blevins, C.A.; Weathers, F.W.; Davis, M.T.; Witte, T.K.; Domino, J.L. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and Initial Psychometric Evaluation. J. Trauma. Stress 2015, 28, 489–498. [Google Scholar] [CrossRef] [PubMed]
- Currier, J.M.; Hermes, S.; Phipps, S. Brief Report: Children’s Response to Serious Illness: Perceptions of Benefit and Burden in a Pediatric Cancer Population. J. Pediatr. Psychol. 2009, 34, 1129–1134. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Phipps, S.; Long, A.M.; Ogden, J. Benefit Finding Scale for Children: Preliminary Findings from a Childhood Cancer Population. J. Pediatr. Psychol. 2007, 32, 1264–1271. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tedeschi, R.G.; Calhoun, L.G. The Posttraumatic Growth Inventory: Measuring the Positive Legacy of Trauma. J. Trauma. Stress 1996, 9, 455–471. [Google Scholar] [CrossRef] [PubMed]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics; Pearson: New York, NY, USA, 2007. [Google Scholar]
- Kenny, D.A.; Kashy, D.A.; Cook, W. Dyadic Data Analysis; Guilford Press: New York, NY, USA, 2006. [Google Scholar]
- Kenny, D.A.; Ledermann, T. Detecting, Measuring, and Testing Dyadic Patterns in the Actor-Partner Interdependence Model. J. Fam. Psychol. 2010, 24, 359–366. [Google Scholar] [CrossRef] [PubMed]
- Phipps, S.; Long, A.; Willard, V.W.; Okado, Y.; Hudson, M.; Huang, Q.; Zhang, H.; Noll, R. Parents of Children with Cancer: At-Risk or Resilient? J. Pediatr. Psychol. 2015, 40, 914–925. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wurz, A.; Cho, S.; Tran, A.; Henry, B.; Duong, J.; Schulte, F. Navigating Life after Cancer Treatment: Comparing and Contrasting Children’s and Their Parent’s Experiences (Working Title). Department of Oncology, Division of Psychosocial Oncology, Cumming School of Medicine, University of Calgary, Calgary, AB, Canada. in preparation.
- Cho, S.; Wurz, A.; Henry, B.; Tran, A.; Duong, J.; Schulte, F. Exploring Pain Experiences among Children Diagnosed with Cancer and Their Parent (Working Title). Department of Oncology, Division of Psychosocial Oncology, Cumming School of Medicine, University of Calgary, Calgary, AB, Canada. in preparation.
- Gutermann, J.; Schreiber, F.; Matulis, S.; Schwartzkopff, L.; Deppe, J.; Steil, R. Psychological Treatments for Symptoms of Posttraumatic Stress Disorder in Children, Adolescents, and Young Adults: A Meta-Analysis. Clin. Child Fam. Psychol. Rev. 2016, 19, 77–93. [Google Scholar] [CrossRef]
- Cohen, J.A.; Mannarino, A.P.; Deblinger, E. Treating Trauma and Traumatic Grief in Children and Adolescents; Guilford Publications: New York, NY, USA, 2016. [Google Scholar]
- Driscoll, K.A.; Schatschneider, C.; McGinnity, K.; Modi, A.C. Application of Dyadic Data Analysis in Pediatric Psychology: Cystic Fibrosis Health-Related Quality of Life and Anxiety in Child-Caregiver Dyads. J. Pediatr. Psychol. 2012, 37, 605–611. [Google Scholar] [CrossRef] [Green Version]
| Variable | Mean (SD) n (%) | Range |
|---|---|---|
| Child current age (years) † | 15.82 (4.81) | 8.00–25.00 |
| Child age at diagnosis (years) † | 5.86 (4.66) | 0.10–17.82 |
| Child time since treatment (years) † | 9.32 (4.51) | 2.38–20.54 |
| Child treatment intensity (1–4) | 2.64 (0.83) | 1.00–4.00 |
| Child sex ‡ | ||
| Female | 57 (50.44) | |
| Child diagnosis ‡ | ||
| Blood cancers | 37 (32.74) | |
| CNS tumor | 10 (8.85) | |
| Solid tumor | 41 (36.28) | |
| Lymphoma | 14 (12.39) | |
| Child ethnicity ‡ | ||
| White | 91 (80.53) | |
| African Canadian | 2 (1.77) | |
| East Asian | 2 (1.77) | |
| Southeast Asian | 1 (0.88) | |
| First Nations/Metis/Inuit | 1 (0.88) | |
| South Asian | 1 (0.88) | |
| Arab | 3 (2.65) | |
| Latin America | 1 (0.88) | |
| Other/mixed | 9 (7.96) | |
| Parent ethnicity ‡ | ||
| White | 102 (90.27) | |
| East Asian | 2 (1.77) | |
| Southeast Asian | 1 (0.88) | |
| South Asian | 2 (1.77) | |
| Arab | 2 (1.77) | |
| Latin American | 2 (1.77) | |
| Household income ‡ | ||
| <CAD 10,000 | 2 (1.77) | |
| CAD 10,000–30,000 | 5 (4.42) | |
| CAD 30,000–50,000 | 7 (6.19) | |
| CAD 50,000–70,000 | 15 (13.27) | |
| CAD 70,000–90,000 | 12 (10.62) | |
| >CAD 90,000 | 70 (61.95) | |
| Children’s PTSS † | ||
| 8–17 years | 11.48 (14.81) | 0.00–60.00 |
| 18–25 years | 12.76 (11.68) | 0.00–53.00 |
| Parent’s PTSS † | 11.12 (11.03) | 0.00–48.00 |
| Children’s PTG † | 30.24 (10.00) | 7.00–50.00 |
| Parent’s PTG † | 54.82 (22.49) | 5.00–97.00 |
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Child age | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| 2. Child sex (0 = male; 1 = female) a | −0.11 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| 3. Child years since diagnosis | 0.51 ** | −0.05 | -- | -- | -- | -- | -- | -- | -- | -- |
| 4. Child time off treatment | 0.56 ** | −0.03 | 0.97 ** | -- | -- | -- | -- | -- | -- | -- |
| 5. Child treatment intensity | 0.19 | 0.65 | 0.08 | 0.12 | -- | -- | -- | -- | -- | -- |
| 6. Household income | 0.14 | −0.09 | −0.03 | 0.05 | 0.09 | -- | -- | -- | -- | -- |
| 7. Children’s PTSS | 0.02 | 0.14 | −0.12 | −0.11 | −0.02 | 0.04 | -- | -- | -- | -- |
| 8. Parent’s PTSS | −0.14 | −0.03 | −0.05 | −0.05 | −0.08 | −0.07 | 0.18 | -- | -- | -- |
| 9. Children’s PTG | 0.06 | 0.17 | −0.13 | −0.11 | 0.07 | −0.17 | 0.05 | −0.06 | -- | -- |
| 10. Parent’s PTG | −0.12 | −0.02 | 0.17 | 0.19 | −0.02 | −0.07 | −0.18 | 0.14 | −0.00 | -- |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wurz, A.; Patton, M.; Merz, E.L.; Hou, S.H.J.; Cho, S.; Schulte, F. Exploring Posttraumatic Stress Symptoms and Posttraumatic Growth among Children Living beyond Cancer and Their Parents Using an Actor–Partner Interdependence Model. Cancers 2022, 14, 704. https://doi.org/10.3390/cancers14030704
Wurz A, Patton M, Merz EL, Hou SHJ, Cho S, Schulte F. Exploring Posttraumatic Stress Symptoms and Posttraumatic Growth among Children Living beyond Cancer and Their Parents Using an Actor–Partner Interdependence Model. Cancers. 2022; 14(3):704. https://doi.org/10.3390/cancers14030704
Chicago/Turabian StyleWurz, Amanda, Michaela Patton, Erin L. Merz, Sharon H. J. Hou, Sara Cho, and Fiona Schulte. 2022. "Exploring Posttraumatic Stress Symptoms and Posttraumatic Growth among Children Living beyond Cancer and Their Parents Using an Actor–Partner Interdependence Model" Cancers 14, no. 3: 704. https://doi.org/10.3390/cancers14030704
APA StyleWurz, A., Patton, M., Merz, E. L., Hou, S. H. J., Cho, S., & Schulte, F. (2022). Exploring Posttraumatic Stress Symptoms and Posttraumatic Growth among Children Living beyond Cancer and Their Parents Using an Actor–Partner Interdependence Model. Cancers, 14(3), 704. https://doi.org/10.3390/cancers14030704







