Expression of miR-24-1-5p in Tumor Tissue Influences Prostate Cancer Recurrence: The PROCA-life Study
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
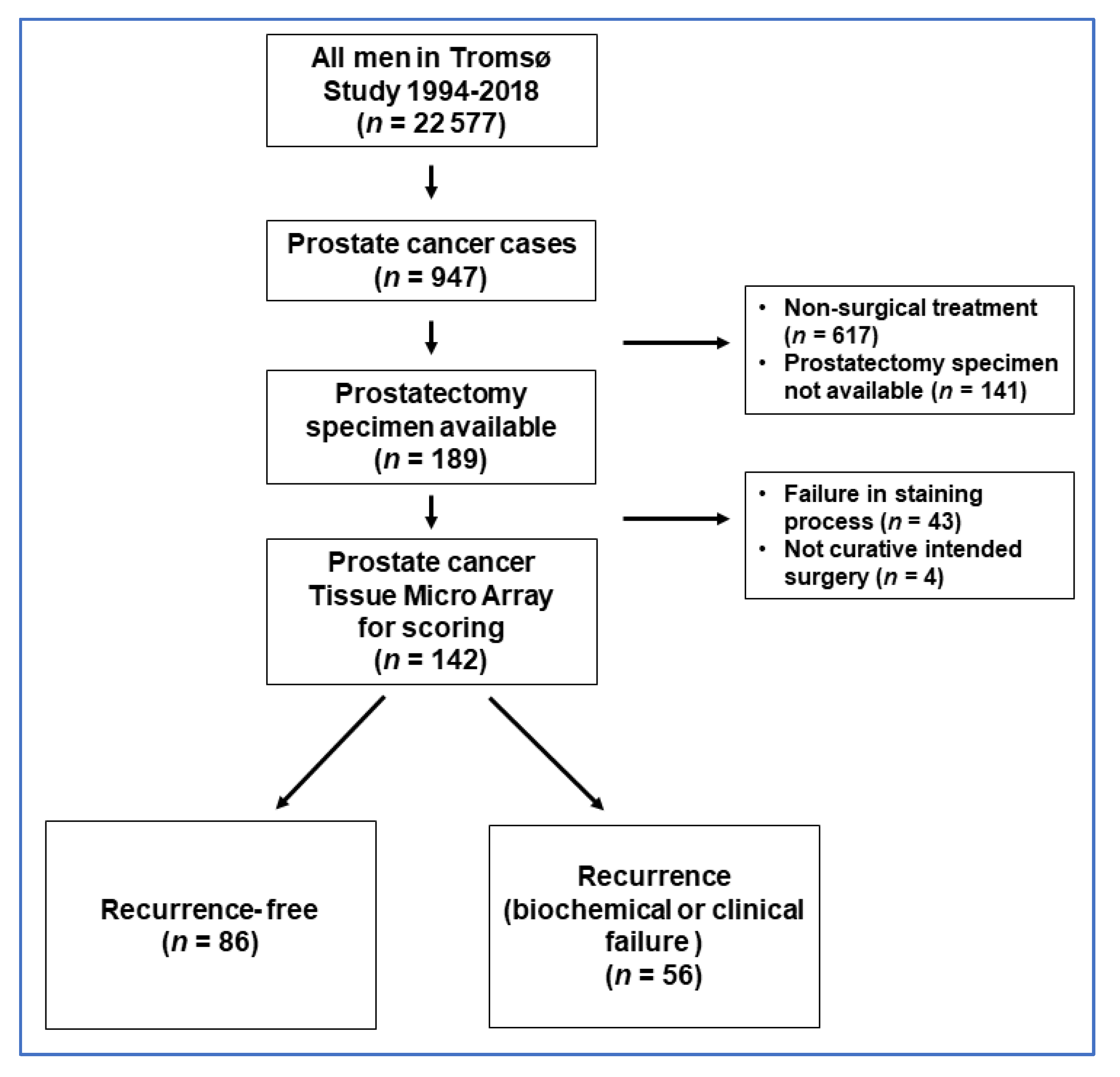
2.1. Study Sample
2.2. Questionnaires, Clinical Assessments, and Assessment of Lipids and PSA
2.3. Identification of Prostate Cancer Cases and Detailed Medical History during Follow-Up
2.4. Microarray Construction
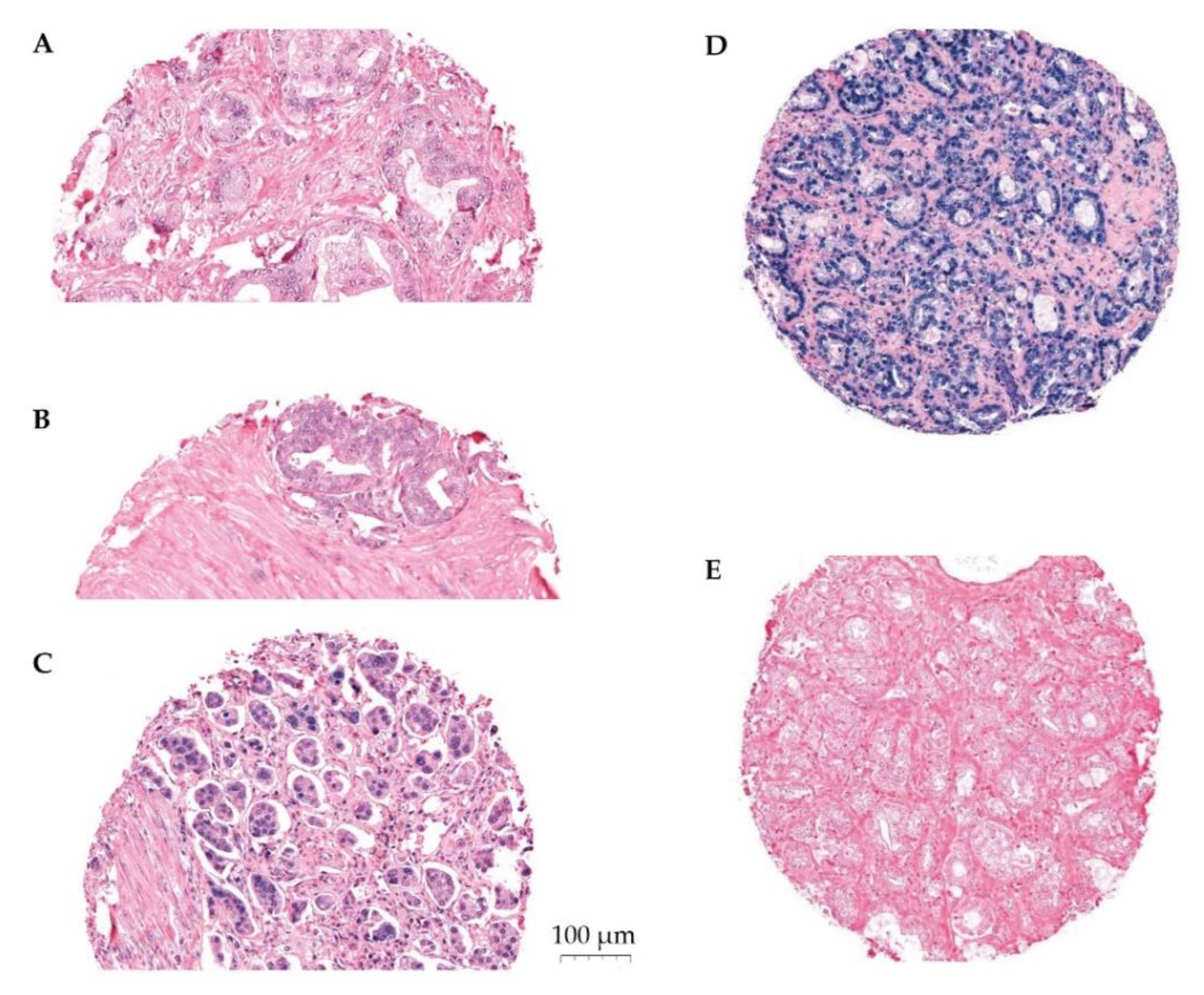
2.5. In Situ Hybridization (ISH)
2.6. Optimization and Validation
2.7. Scoring
2.8. Statistical Methods
3. Results
3.1. Patient Characteristics
3.2. miR-24-1-5p Expression
3.3. miR-24-1-5p Correlations
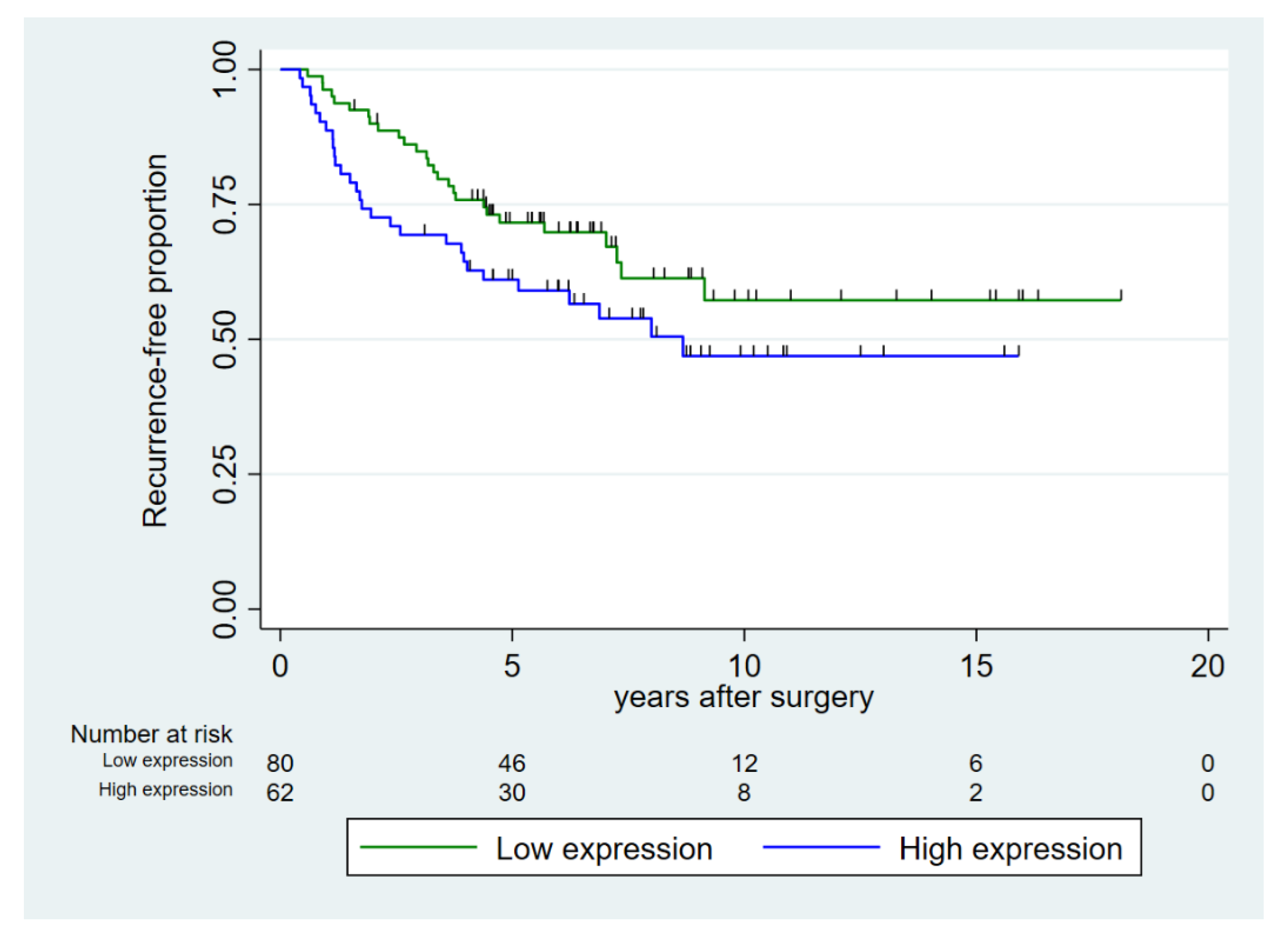
3.4. Recurrence-Free Survival
3.5. Multivariable Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
Appendix A.1. ISH Procedure in Short
| LNA Probe | RNA Tm | Target | Denaturation | Probe | Hybridi-zation Temp. | String | Blocking | Detection | Visuali-sation | Contrast |
|---|---|---|---|---|---|---|---|---|---|---|
| Retrieval | Conc. | Wash | ||||||||
| miR-24-1-5p 1 nmol | 85 °C | CC1 40 min | 90 °C 8 min | 80 nM | 51 °C | Ribo Wash 51 °C 8 min | Ab block | Anti-DIG-AP 32 min | ChromoMa Blue 120 min | Red II 4 min |
| 16 min | ||||||||||
| Scramble-miR 25 µM | 87 °C | CC1 40 min | 90 °C 8 min | 10 nM | 57 °C | Ribo Wash 51 °C 8 min | Ab block | Anti-DIG-AP 32 min | ChromoMap Blue | Red II 4 min |
| 16 min | 120 min | |||||||||
| U6 25 µM | 84 °C | CC1 40 min | 90 °C 8 min | 1.5 nM | 55 °C | Ribo Wash 51 °C 8 min | Ab block | Anti-DIG-AP 32 min | ChromoMap Blue | Red II 4 min |
| 16 min | 120 min |
| Probes and Reagents | Manufacturer |
|---|---|
| LNA miR-24-1-5p Probe | QIAGEN YD00610842-BCG |
| LNA Scramble miR Probe | QIAGEN MiCURY LNA miRNA ISH Control Set (FFPE) 1108515 |
| LNA U6 snRNA Probe | QIAGEN MiCURY LNA miRNA ISH Control Set (FFPE) 1108515 |
| Superfrost Pluss Glass Slides | Thermo Scientific |
| miRCURY LNA miRNA ISH Buffer and Control | QIAGEN 339459 |
| Liquid Coverslip Oil | Roche 5264839001 |
| EZ Prep Solution | Roche 5279755001 |
| Discovery CC1 Buffer | Roche 6414575001 |
| Reaction Buffer | Roche 5353955001 |
| Ribo Wash | Roche 5266262001 |
| Antibody Block | Roche 5268869001 |
| Anti-DIG AP Multimer | Roche 7256302001 |
| ChromoMap Blue Kit | Roche 5266661001 |
| Red Counterstain II | Roche 5272017001 |
Appendix B
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Haffner, M.C.; Zwart, W.; Roudier, M.P.; True, L.D.; Nelson, W.G.; Epstein, J.I.; De Marzo, A.M.; Nelson, P.S.; Yegnasubramanian, S. Genomic and phenotypic heterogeneity in prostate cancer. Nat. Rev. Urol. 2021, 18, 79–92. [Google Scholar] [CrossRef] [PubMed]
- Tahamtan, A.; Teymoori-Rad, M.; Nakstad, B.; Salimi, V. Anti-Inflammatory MicroRNAs and Their Potential for Inflammatory Diseases Treatment. Front. Immunol. 2018, 9, 1377. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rana, S.; Valbuena, G.N.; Curry, E.; Bevan, C.L.; Keun, H.C. MicroRNAs as biomarkers for prostate cancer prognosis: A systematic review and a systematic reanalysis of public data. Br. J. Cancer 2022, 126, 502–513. [Google Scholar] [CrossRef] [PubMed]
- Walter, B.A.; Valera, V.A.; Pinto, P.A.; Merino, M.J. Comprehensive microRNA Profiling of Prostate Cancer. J. Cancer 2013, 4, 350–357. [Google Scholar] [CrossRef] [Green Version]
- Andl, T.; Ganapathy, K.; Bossan, A.; Chakrabarti, R. MicroRNAs as Guardians of the Prostate: Those Who Stand before Cancer. What Do We Really Know about the Role of microRNAs in Prostate Biology? Int. J. Mol. Sci. 2020, 21, 4796. [Google Scholar] [CrossRef]
- Mirzaei, S.; Zarrabi, A.; Hashemi, F.; Zabolian, A.; Saleki, H.; Ranjbar, A.; Seyed Saleh, S.H.; Bagherian, M.; Sharifzadeh, S.; Hushmandi, K.; et al. Regulation of Nuclear Factor-KappaB (NF-κB) signaling pathway by non-coding RNAs in cancer: Inhibiting or promoting carcinogenesis? Cancer Lett. 2021, 509, 63–80. [Google Scholar] [CrossRef]
- Vanacore, D.; Boccellino, M.; Rossetti, S.; Cavaliere, C.; D’Aniello, C.; Di Franco, R.; Romano, F.J.; Montanari, M.; La Mantia, E.; Piscitelli, R.; et al. Micrornas in prostate cancer: An overview. Oncotarget 2017, 8, 50240–50251. [Google Scholar] [CrossRef] [Green Version]
- Arisan, E.D.; Rencuzogullari, O.; Freitas, I.L.; Radzali, S.; Keskin, B.; Kothari, A.; Warford, A.; Uysal-Onganer, P. Upregulated Wnt-11 and miR-21 Expression Trigger Epithelial Mesenchymal Transition in Aggressive Prostate Cancer Cells. Biology 2020, 9, 52. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.H.; Lee, D.Y.; Lee, H.J.; Im, E.; Sim, D.Y.; Park, J.E.; Park, W.Y.; Shim, B.S.; Kim, S.H. Inhibition of STAT3/PD-L1 and Activation of miR193a-5p Are Critically Involved in Apoptotic Effect of Compound K in Prostate Cancer Cells. Cells 2021, 10, 2151. [Google Scholar] [CrossRef]
- Hanahan, D.; Weinberg, R.A. Hallmarks of Cancer: The Next Generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef] [Green Version]
- Hanahan, D. Hallmarks of Cancer: New Dimensions. Cancer Discov. 2022, 12, 31–46. [Google Scholar] [CrossRef]
- Sfanos, K.S.; Yegnasubramanian, S.; Nelson, W.G.; De Marzo, A.M. The inflammatory microenvironment and microbiome in prostate cancer development. Nat. Rev. Urol. 2018, 15, 11–24. [Google Scholar] [CrossRef]
- Sfanos, K.S.; De Marzo, A.M. Prostate cancer and inflammation: The evidence. Histopathology 2012, 60, 199–215. [Google Scholar] [CrossRef] [Green Version]
- Platz, E.A.; Kulac, I.; Barber, J.R.; Drake, C.G.; Joshu, C.E.; Nelson, W.G.; Lucia, M.S.; Klein, E.A.; Lippman, S.M.; Parnes, H.L.; et al. A Prospective Study of Chronic Inflammation in Benign Prostate Tissue and Risk of Prostate Cancer: Linked PCPT and SELECT Cohorts. Cancer Epidemiol. Biomark. Prev. 2017, 26, 1549–1557. [Google Scholar] [CrossRef] [Green Version]
- De Marzo, A.M.; Platz, E.A.; Sutcliffe, S.; Xu, J.; Gronberg, H.; Drake, C.G.; Nakai, Y.; Isaacs, W.B.; Nelson, W.G. Inflammation in prostate carcinogenesis. Nat. Rev. Cancer 2007, 7, 256–269. [Google Scholar] [CrossRef] [Green Version]
- Luo, J.L.; Tan, W.; Ricono, J.M.; Korchynskyi, O.; Zhang, M.; Gonias, S.L.; Cheresh, D.A.; Karin, M. Nuclear cytokine-activated IKKalpha controls prostate cancer metastasis by repressing Maspin. Nature 2007, 446, 690–694. [Google Scholar] [CrossRef]
- De Visser, K.E.; Eichten, A.; Coussens, L.M. Paradoxical roles of the immune system during cancer development. Nat. Rev. Cancer 2006, 6, 24–37. [Google Scholar] [CrossRef]
- De Marzo, A.M.; Marchi, V.L.; Epstein, J.I.; Nelson, W.G. Proliferative inflammatory atrophy of the prostate: Implications for prostatic carcinogenesis. Am. J. Pathol. 1999, 155, 1985–1992. [Google Scholar] [CrossRef]
- Katoh, M. Cardio-miRNAs and onco-miRNAs: Circulating miRNA-based diagnostics for non-cancerous and cancerous diseases. Front. Cell Dev. Biol. 2014, 2, 61. [Google Scholar] [CrossRef] [Green Version]
- Wang, S.; Liu, N.; Tang, Q.; Sheng, H.; Long, S.; Wu, W. MicroRNA-24 in Cancer: A Double Side Medal with Opposite Properties. Front. Oncol. 2020, 10, 553714. [Google Scholar] [CrossRef]
- Ghafouri-Fard, S.; Shoorei, H.; Taheri, M. Role of microRNAs in the development, prognosis and therapeutic response of patients with prostate cancer. Gene 2020, 759, 144995. [Google Scholar] [CrossRef]
- Richardsen, E.; Andersen, S.; Al-Saad, S.; Rakaee, M.; Nordby, Y.; Pedersen, M.I.; Ness, N.; Ingebriktsen, L.M.; Fassina, A.; Taskén, K.A.; et al. Low Expression of miR-424-3p is Highly Correlated with Clinical Failure in Prostate Cancer. Sci. Rep. 2019, 9, 10662. [Google Scholar] [CrossRef]
- Richardsen, E.; Andersen, S.; Melbø-Jørgensen, C.; Rakaee, M.; Ness, N.; Al-Saad, S.; Nordby, Y.; Pedersen, M.I.; Dønnem, T.; Bremnes, R.M.; et al. MicroRNA 141 is associated to outcome and aggressive tumor characteristics in prostate cancer. Sci. Rep. 2019, 9, 386. [Google Scholar] [CrossRef] [Green Version]
- Andersen, S.; Richardsen, E.; Moi, L.; Donnem, T.; Nordby, Y.; Ness, N.; Holman, M.E.; Bremnes, R.M.; Busund, L.-T. Fibroblast miR-210 overexpression is independently associated with clinical failure in Prostate Cancer—A multicenter (in situ hybridization) study. Sci. Rep. 2016, 6, 36573. [Google Scholar] [CrossRef] [Green Version]
- Stoen, M.J.; Andersen, S.; Rakaee, M.; Pedersen, M.I.; Ingebriktsen, L.M.; Bremnes, R.M.; Donnem, T.; Lombardi, A.P.G.; Kilvaer, T.K.; Busund, L.T.; et al. High expression of miR-17-5p in tumor epithelium is a predictor for poor prognosis for prostate cancer patients. Sci. Rep. 2021, 11, 13864. [Google Scholar] [CrossRef]
- Stoen, M.J.; Andersen, S.; Rakaee, M.; Pedersen, M.I.; Ingebriktsen, L.M.; Donnem, T.; Lombardi, A.P.G.; Kilvaer, T.K.; Busund, L.-T.R.; Richardsen, E. Overexpression of miR-20a-5p in Tumor Epithelium Is an Independent Negative Prognostic Indicator in Prostate Cancer—A Multi-Institutional Study. Cancers 2021, 13, 4096. [Google Scholar] [CrossRef]
- Nordby, Y.; Richardsen, E.; Ness, N.; Donnem, T.; Patel, H.R.H.; Busund, L.-T.; Bremnes, R.M.; Andersen, S. High miR-205 expression in normal epithelium is associated with biochemical—An argument for epithelial crosstalk in prostate cancer? Sci. Rep. 2017, 7, 16308. [Google Scholar] [CrossRef]
- Szczyrba, J.; Löprich, E.; Wach, S.; Jung, V.; Unteregger, G.; Barth, S.; Grobholz, R.; Wieland, W.; Stöhr, R.; Hartmann, A.; et al. The MicroRNA Profile of Prostate Carcinoma Obtained by Deep Sequencing. Mol. Cancer Res. 2010, 8, 529–538. [Google Scholar] [CrossRef] [Green Version]
- Hashimoto, Y.; Shiina, M.; Kato, T.; Yamamura, S.; Tanaka, Y.; Majid, S.; Saini, S.; Shahryari, V.; Kulkarni, P.; Dasgupta, P.; et al. The role of miR-24 as a race related genetic factor in prostate cancer. Oncotarget 2017, 8, 16581–16593. [Google Scholar] [CrossRef] [Green Version]
- Li, X.; Han, X.; Wei, P.; Yang, J.; Sun, J. Knockdown of lncRNA CCAT1 enhances sensitivity of paclitaxel in prostate cancer via regulating miR-24-3p and FSCN. Cancer Biol. Ther. 2020, 21, 452–462. [Google Scholar]
- Watahiki, A.; Wang, Y.; Morris, J.; Dennis, K.; O’Dwyer, H.M.; Gleave, M.; Gout, P.W.; Wang, Y. MicroRNAs Associated with Metastatic Prostate Cancer. PLoS ONE 2011, 6, e24950. [Google Scholar] [CrossRef]
- Lynch, S.M.; McKenna, M.M.; Walsh, C.P.; McKenna, D.J. miR-24 regulates CDKN1B/p27 expression in prostate cancer. Prostate 2016, 76, 637–648. [Google Scholar] [CrossRef]
- miRbase. Faculty of Biology, Medicine and Health, University of Manchester. 2018. Available online: http://mirbase.org/ (accessed on 22 July 2021).
- Eggen, A.E.; Mathiesen, E.B.; Wilsgaard, T.; Jacobsen, B.K.; Njølstad, I. The sixth survey of the Tromsø Study (Tromsø 6) in 2007–08: Collaborative research in the interface between clinical medicine and epidemiology: Study objectives, design, data collection procedures, and attendance in a multipurpose population-based health survey. Scand. J. Public Health 2013, 41, 65–80. [Google Scholar]
- Stikbakke, E.; Richardsen, E.; Knutsen, T.; Wilsgaard, T.; Giovannucci, E.L.; McTiernan, A.; Eggen, A.E.; Haugnes, H.S.; Thune, I. Inflammatory serum markers and risk and severity of prostate cancer: The PROCA- life study. Int. J. Cancer 2020, 147, 84–92. [Google Scholar] [CrossRef] [Green Version]
- Jacobsen, B.K.; Eggen, A.E.; Mathiesen, E.B.; Wilsgaard, T.; Njølstad, I. Cohort profile: The Tromso Study. Int. J. Epidemiol. 2011, 41, 961–967. [Google Scholar] [CrossRef]
- Lofterød, T.; Frydenberg, H.; Flote, V.; Eggen, A.E.; McTiernan, A.; Mortensen, E.S.; Akslen, L.A.; Reitan, J.B.; Wilsgaard, T.; Thune, I. Exploring the effects of lifestyle on breast cancer risk, age at diagnosis, and survival: The EBBA-Life study. Breast Cancer Res. Treat. 2020, 182, 215–227. [Google Scholar] [CrossRef]
- Cancer Prevention Recommendations: World Cancer Research Fund. Available online: https://www.wcrf.org/dietandcancer/cancer-prevention-recommendations (accessed on 22 July 2021).
- Epstein, J.I.; Allsbrook, W.C., Jr.; Amin, M.B.; Egevad, L.L.; Committee, I.G. The 2005 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma. Am. J. Surg. Pathol. 2005, 29, 1228–1242. [Google Scholar] [CrossRef] [Green Version]
- Heidenreich, A.; Bastian, P.J.; Bellmunt, J.; Bolla, M.; Joniau, S.; Van der Kwast, T.; Mason, M.; Matveev, V.; Wiegel, T.; Zattoni, F.; et al. EAU Guidelines on Prostate Cancer. Part 1: Screening, Diagnosis, and Local Treatment with Curative Intent—Update. Eur. Urol. 2014, 65, 124–137. [Google Scholar] [CrossRef]
- Cooperberg, M.R.; Hilton, J.F.; Carroll, P.R. The CAPRA-S score: A straightforward tool for improved prediction of outcomes after radical prostatectomy. Cancer 2011, 117, 5039–5046. [Google Scholar] [CrossRef]
- Bremnes, R.M.; Veve, R.; Gabrielson, E.; Hirsch, F.R.; Baron, A.; Bemis, L.; Gemmill, R.M.; Drabkin, H.A.; Franklin, W.A. High-Throughput Tissue Microarray Analysis Used to Evaluate Biology and Prognostic Significance of the E-Cadherin Pathway in Non–Small-Cell Lung Cancer. J. Clin. Oncol. 2002, 20, 2417–2428. [Google Scholar] [CrossRef]
- Stikbakke, E.; Schirmer, H.; Knutsen, T.; Støyten, M.; Wilsgaard, T.; Giovannucci, E.L.; McTiernan, A.; Eggen, A.E.; Haugnes, H.S.; Richardsen, E.; et al. Systolic and diastolic blood pressure, prostate cancer risk, treatment, and survival. The PROCA-life study. Cancer Med. 2021, 11, 1005–1015. [Google Scholar] [CrossRef]
- Weidle, U.H.; Epp, A.; Birzele, F.; Brinkmann, U. The Functional Role of Prostate Cancer Metastasis-related Micro-RNAs. Cancer Genom. Proteom. 2018, 16, e20108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, R.; Kong, W.; Zheng, S.; Yu, C.; Yu, Y.; Xu, Y.; Ye, L.; Shao, Y. Prognostic significance of microRNA miR-24 in cancers: A meta-analysis. Bioengineered 2021, 12, 450–460. [Google Scholar] [CrossRef] [PubMed]
- Kutilin, D. Genetic and epigenetic bases of prostate tumor cell radioresistance. Klin. Onkol. 2021, 86, 220–234. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Liu, C.; Zou, X.; Geng, X.; Zhou, X.; Fan, X.; Zhu, D.; Zhang, H.; Zhu, W. MicroRNA panel in serum reveals novel diagnostic biomarkers for prostate cancer. PeerJ 2021, 9, e11441. [Google Scholar] [CrossRef] [PubMed]
- Fredsøe, J.; Rasmussen, A.K.; Thomsen, A.R.; Mouritzen, P.; Høyer, S.; Borre, M.; Ørntoft, T.F.; Sørensen, K.D. Diagnostic and Prognostic MicroRNA Biomarkers for Prostate Cancer in Cell-free Urine. Eur. Urol. Focus 2018, 4, 825–833. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kong, M.; Li, H.; Yuan, W.; Mao, L.; Chen, J. The role of Circ_PRKCI/miR-24-3p in the metastasis of prostate cancer. JBUON Off. J. Balk. Union Oncol. 2021, 26, 949–955. [Google Scholar]
- Dart, D.A.; Uysal-Onganer, P.; Jiang, W.G. Prostate-specific PTen deletion in mice activates inflammatory microRNA expression pathways in the epithelium early in hyperplasia development. Oncogenesis 2017, 6, 400. [Google Scholar] [CrossRef] [Green Version]
- Naqvi, A.R.; Fordham, J.B.; Nares, S. miR-24, miR-30b, and miR-142-3p Regulate Phagocytosis in Myeloid Inflammatory Cells. J. Immunol. 2015, 194, 1916–1927. [Google Scholar] [CrossRef] [Green Version]
- Maegdefessel, L.; Spin, J.M.; Raaz, U.; Eken, S.; Toh, R.; Azuma, J.; Adam, M.; Nagakami, F.; Heymann, H.M.; Chernogubova, E.; et al. miR-24 limits aortic vascular inflammation and murine abdominal aneurysm development. Nat. Commun. 2014, 5, 5214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Naqvi, J.B.F.A.R.; Nares, S.; Fordham, J.B. miR-24 Regulates Macrophage Polarization and Plasticity. J. Clin. Cell. Immunol. 2015, 6, 362. [Google Scholar] [CrossRef] [Green Version]
- Yang, J.; Chen, L.; Ding, J.; Fan, Z.; Li, S.; Wu, H.; Zhang, J.; Yang, C.; Wang, H.; Zeng, P.; et al. MicroRNA-24 inhibits high glucose-induced vascular smooth muscle cell proliferation and migration by targeting HMGB. Gene 2016, 586, 268–273. [Google Scholar] [CrossRef] [PubMed]
- Nocito, A.; Kononen, J.; Kallioniemi, O.; Sauter, G. Tissue microarrays (TMAs) for high-throughput molecular pathology research. Int. J. Cancer 2001, 94, 1–5. [Google Scholar] [CrossRef]
- Selven, H.; Busund, L.-T.R.; Andersen, S.; Bremnes, R.M.; Kilvær, T.K. High expression of microRNA-126 relates to favorable prognosis for colon cancer patients. Sci. Rep. 2021, 11, 9592. [Google Scholar] [CrossRef]
| Characteristics | Prostatectomy Cases (n = 142) |
|---|---|
| Age at Study Entry, Median, Range (Years) | 58.5 (34–73) |
| Birth Year Median, Range (Year) | 1947 (1934–1967) |
| Age at Surgery, Median, Range (Years) | 65.0 (47–75) |
| Observation Time from Study Entry to Surgery (Years) | 8.0 (6.6) |
| Observation Time from Surgery to End of Follow-Up (Years) | 4.8 (3.4) |
| PSA at Diagnosis (μg/L) | 10.5 (9.5) |
| Relapse Rate (Biochemical + Clinical), % (n) | 26.9 (38) |
| Clinical Assessments at Study Entry | |
| Body Mass Index (kg/m2) | 27.1 (3.15) |
| Systolic Blood Pressure (mmHg) | 134.9 (16.8) |
| Diastolic Blood Pressure (mmHg) | 80.4 (9.4) |
| White Blood Cells (×109/L) | 6.60 (1.67) |
| Total Cholesterol (mmol/L) | 5.78 (1.12) |
| Triglyceride (mmol/L) | 1.70 (0.90) |
| Alcohol Intake (>1 Unit of Alcohol per Month), % (n) | 46.1 (65) |
| Surgical Technique, % (n) | |
| Open Prostatectomy, Retropubic | 38.0 (54) |
| Open Prostatectomy, Perineal | 9.2 (13) |
| Laparoscopic Prostatectomy | 6.3 (9) |
| Robotic-Assisted Laparoscopic Prostatectomy (RALP) | 46.5 (66) |
| Lymph Node Dissection Performed, % (n) | 36.6 (52) |
| Histopathological Stage, % (n) | |
| pT2a | 17.0 (24) |
| pT2b | 8.5 (12) |
| pT2c | 48.2 (68) |
| pT3a | 16.3 (23) |
| pT3b | 9.9 (14) |
| ISUP Grade Group, % (n) | |
| 1 (Gleason 3 + 3) | 29.1 (41) |
| 2 (Gleason 3 + 4) | 44.7 (63) |
| 3 (Gleason 4 + 3) | 18.4 (26) |
| 4 (Gleason 4 + 4) | 6.4 (9) |
| 5 (Gleason 4 + 5/5 + 4/5 + 5) | 1.4 (2) |
| Risk Group, % (n) | |
| Low | 25.5% (36) |
| Intermediate | 56.0% (79) |
| High | 18.4% (26) |
| Other Histopathological Characteristics, % (n) | |
| Positive Lymph Nodes (N+) | 3.6 * |
| Ural Infiltration | 21.3 (30) |
| Extraprostatic Growth | 22.7 (32) |
| Normal Tissue in Surgical Margin | 15.6 (22) |
| Positive Surgical Margin | 30.5 (43) |
| Group | n | Tumor Epithelium (TE) | Normal Epithelium (NE) | Tumor + Normal Epithelium (TE+NE) |
|---|---|---|---|---|
| All Cases | 142 | |||
| Mean Score miR-24-1-5p (SD) | 1.60 (0.73) | 1.35 (0.68) | 1.49 (0.53) | |
| Distribution | ||||
| 0–0.49 Negative % (n) | 3.5 (5) | 7.0 (10) | 2.8 (4) | |
| 0.5–1.49 Weak % (n) | 30.3 (43) | 40.1 (57) | 39.4 (56) | |
| 1.5–2.49 Moderate % (n) | 43.0 (61) | 38.0 (54) | 53.5 (76) | |
| 2.5–3 Strong % (n) | 13.4 (19) | 7.0 (10 | 4.2 (6) | |
| Missing % (n) | 9.9 (14) | 7.8 (11) | - | |
| Age at Surgery | ||||
| <65 Year | 69 | 1.63 (0.67) | 1.45 (0.64) | 1.59 (0.50) |
| ≥65 Year | 73 | 1.58 (0.79) | 1.25 (0.71) | 1.40 (0.55) |
| Capra-S | ||||
| Low (0–2) | 56 | 1.46 (0.69) | 1.42 (0.76) | 1.44 (0.53) |
| Intermediate (3–5) | 66 | 1.69 (0.75) | 1.35 (0.61) | 1.57 (0.49) |
| High (6–12) | 20 | 1.75 (0.73) | 1.11 (0.67) | 1.40 (0.67) |
| Systolic Blood Pressure | ||||
| <130 mmHg | 55 | 1.79 (0.63) | 1.38 (0.60) | 1.62 (0.49) |
| ≥130 mmHg | 77 | 1.48 (0.77) | 1.33 (0.73) | 1.41 (0.55) |
| Characteristics | All Cases | Cases with Pre-Diagnostic Systolic BP ≥ 130 mmHg | ||||
|---|---|---|---|---|---|---|
| n | Five-Year Recurrence-Free Survival, % (95% C.I.) | p * | n | Five-Year Recurrence-Free Survival, % (95% C.I.) | p * | |
| Age at Surgery | 0.59 | 0.27 | ||||
| <65 Year | 69 | 69.3 (56.9–78.8) | 37 | 72.8 (55.4–84.4) | ||
| ≥65 Year | 73 | 65.0 (52.7–74.8) | 50 | 64.9 (49.7–76.5) | ||
| ISUP Grade Group | <0.001 | <0.001 | ||||
| 1 (Gleason 3 + 3) | 33 | 81.4 (63.1–91.2) | 15 | 85.6 (53.3–96.2) | ||
| 2 (Gleason 3 + 4) | 66 | 77.2 (65.1–85.6) | 44 | 77.3 (61.9–87.1) | ||
| 3 (Gleason 4 + 3) | 28 | 41.3 (22.8–59.0) | 21 | 47.1 (25.1–66.4) | ||
| 4 (Gleason 4 + 4) | 9 | 50.8 (15.7–78.1) | 4 | 66.7 (5.4–94.5) | ||
| 5 (Gleason 4 + 5/5 + 4/5 + 5) | 6 | 16.7 (0.8–51.7) | 3 | N.a | ||
| Risk Group | <0.001 | 0.0003 | ||||
| Low | 36 | 85.7 (68.9–93.8) | 18 | 88.2 (60.2–96.9) | ||
| Intermediate | 80 | 70.8 (59.3–79.5) | 54 | 71.8 (57.7–82.0) | ||
| High | 26 | 30.8 (14.6–48.6) | 15 | 33.3 (12.1–56.4) | ||
| Capra-S | <0.001 | <0.001 | ||||
| Low (0–2) | 56 | 89.2 (77.6–95.0) | 33 | 93.9 (77.9–98.4) | ||
| Intermediate (3–5) | 66 | 61.2 (48.1–71.2) | 41 | 62.6 (45.8–75.5) | ||
| High (6–12) | 20 | 25.0 (9.1–44.9) | 13 | 23.1 (5.6–47.5) | ||
| miR-24-1-5p | 0.098 | 0.026 | ||||
| TE+NE Low | 80 | 71.6 (60.1–80.3) | 55 | 75.5 (61.5–85.0) | ||
| TE+NE High | 62 | 61.1 (47.7–72.0) | 32 | 55.8 (37.0–71.0) | ||
| Characteristics | All Cases | Cases with Pre-Diagnostic Hypertension Systolic BP ≥ 130 mmHg | ||||
|---|---|---|---|---|---|---|
| n | Hazard Ratio (95% C.I.) | p | n | Hazard Ratio (95% C.I.) | p | |
| Age per 10 Years | 142 | 1.13 (0.69–1.82) | 0.63 | 87 | 1.17 (0.58–2.36) | 0.66 |
| Capra-S | ||||||
| Low (0–2) | 58 | 1 (Reference) | 33 | 1 (Reference) | ||
| Intermediate (3–5) | 66 | 3.75 (1.17–8.27) | 0.001 | 41 | 6.25 (1.41–27.3) | 0.015 |
| High (6–12) | 21 | 16.0 (6.59–39.2) | <0.001 | 13 | 31.9 (6.50–156.5) | <0.001 |
| miR-24-1-5p | ||||||
| TE+NE low | 82 | 1 (Reference) | 55 | 1 (Reference) | ||
| TE+NE high | 63 | 1.99 (1.13–3.51) | 0.017 | 32 | 2.85 (1.25–6.47) | 0.013 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stikbakke, E.; Wilsgaard, T.; Haugnes, H.S.; Pedersen, M.I.; Knutsen, T.; Støyten, M.; Giovannucci, E.; Eggen, A.E.; Thune, I.; Richardsen, E. Expression of miR-24-1-5p in Tumor Tissue Influences Prostate Cancer Recurrence: The PROCA-life Study. Cancers 2022, 14, 1142. https://doi.org/10.3390/cancers14051142
Stikbakke E, Wilsgaard T, Haugnes HS, Pedersen MI, Knutsen T, Støyten M, Giovannucci E, Eggen AE, Thune I, Richardsen E. Expression of miR-24-1-5p in Tumor Tissue Influences Prostate Cancer Recurrence: The PROCA-life Study. Cancers. 2022; 14(5):1142. https://doi.org/10.3390/cancers14051142
Chicago/Turabian StyleStikbakke, Einar, Tom Wilsgaard, Hege Sagstuen Haugnes, Mona Irene Pedersen, Tore Knutsen, Martin Støyten, Edward Giovannucci, Anne Elise Eggen, Inger Thune, and Elin Richardsen. 2022. "Expression of miR-24-1-5p in Tumor Tissue Influences Prostate Cancer Recurrence: The PROCA-life Study" Cancers 14, no. 5: 1142. https://doi.org/10.3390/cancers14051142






