B7-H3 in Pediatric Tumors: Far beyond Neuroblastoma
Abstract
:Simple Summary
Abstract
1. Introduction
2. Tumors of the Central Nervous System
3. Sarcomas
4. Acute Leukemia
5. B7-H3 as a Target in Other Pediatric Tumors
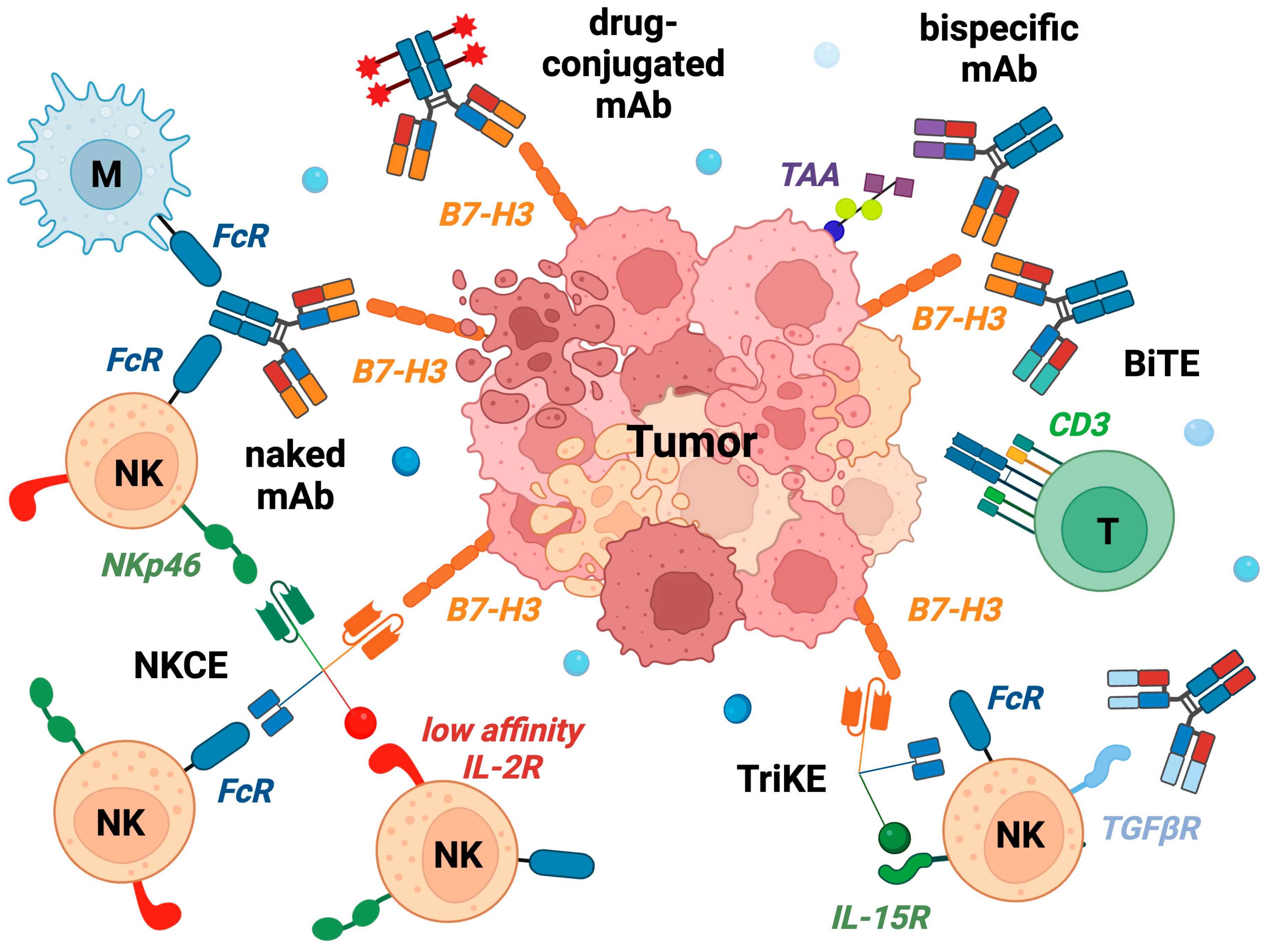
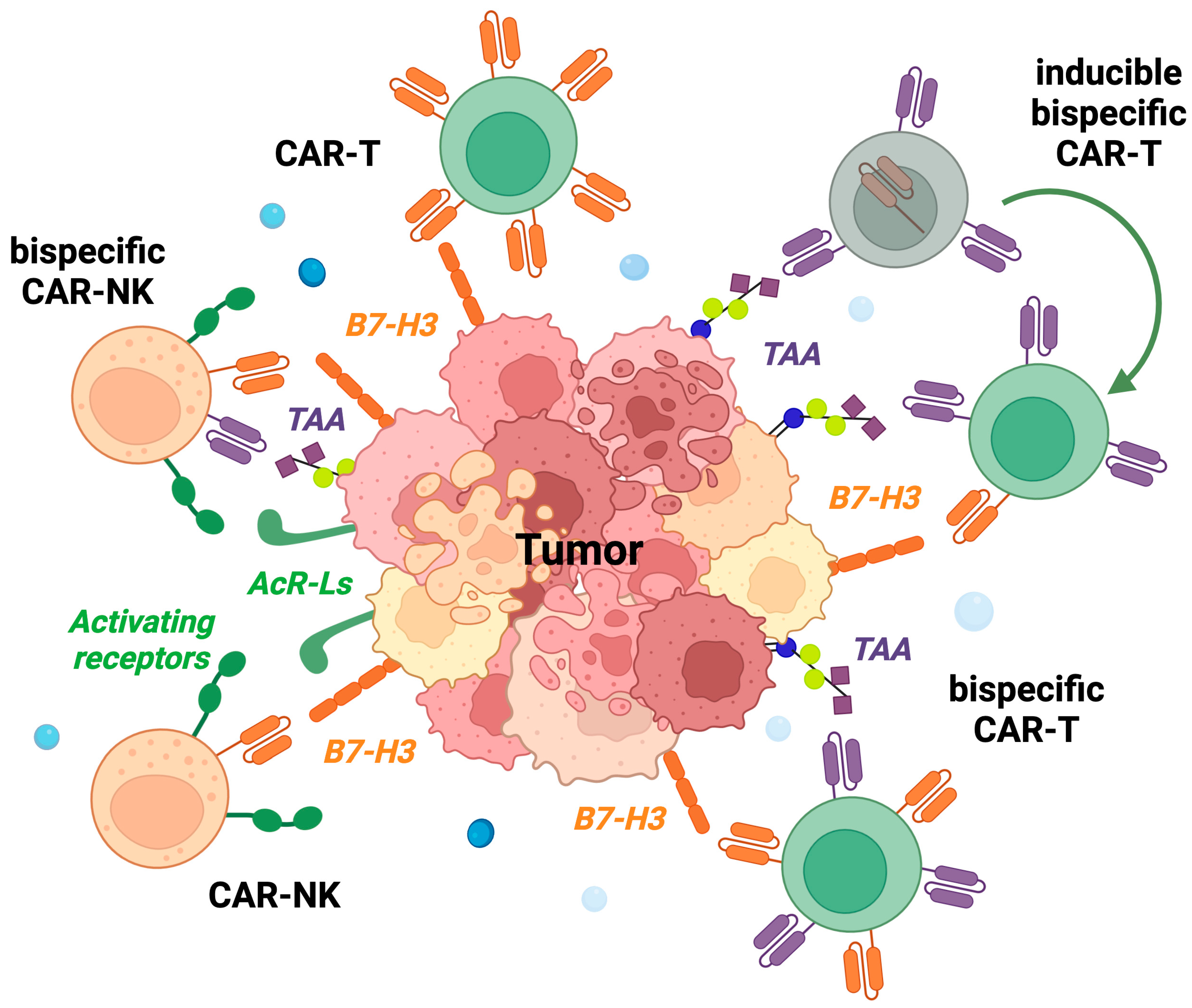
6. Therapeutics Targeting B7-H3
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Castriconi, R.; Dondero, A.; Augugliaro, R.; Cantoni, C.; Carnemolla, B.; Sementa, A.R.; Negri, F.; Conte, R.; Corrias, M.V.; Moretta, L. Identification of 4Ig-B7-H3 as a Neuroblastoma-Associated Molecule That Exerts a Protective Role from an NK Cell-Mediated Lysis. Proc. Natl. Acad. Sci. USA 2004, 101, 12640–12645. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steinberger, P.; Majdic, O.; Derdak, S.V.; Pfistershammer, K.; Kirchberger, S.; Klauser, C.; Zlabinger, G.; Pickl, W.F.; Stöckl, J.; Knapp, W. Molecular Characterization of Human 4Ig-B7-H3, a Member of the B7 Family with Four Ig-Like Domains. J. Immunol. 2004, 172, 2352–2359. [Google Scholar] [CrossRef] [Green Version]
- Chapoval, A.I.; Ni, J.; Lau, J.S.; Wilcox, R.A.; Flies, D.B.; Liu, D.; Dong, H.; Sica, G.L.; Zhu, G.; Tamada, K.; et al. B7-H3: A Costimulatory Molecule for T Cell Activation and IFN-γ Production. Nat. Immunol. 2001, 2, 269–274. [Google Scholar] [CrossRef] [PubMed]
- Sun, M.; Richards, S.; Prasad, D.V.R.; Mai, X.M.; Rudensky, A.; Dong, C. Characterization of Mouse and Human B7-H3 Genes. J. Immunol. 2002, 168, 6294–6297. [Google Scholar] [CrossRef] [Green Version]
- Suh, W.-K.; Gajewska, B.U.; Okada, H.; Gronski, M.A.; Bertram, E.M.; Dawicki, W.; Duncan, G.S.; Bukczynski, J.; Plyte, S.; Elia, A.; et al. The B7 Family Member B7-H3 Preferentially down-Regulates T Helper Type 1-Mediated Immune Responses. Nat. Immunol. 2003, 4, 899–906. [Google Scholar] [CrossRef] [PubMed]
- Prasad, D.V.R.; Nguyen, T.; Li, Z.; Yang, Y.; Duong, J.; Wang, Y.; Dong, C. Murine B7-H3 Is a Negative Regulator of T Cells. J. Immunol. 2004, 173, 2500–2506. [Google Scholar] [CrossRef] [Green Version]
- Castriconi, R.; Dondero, A.; Corrias, M.V.; Lanino, E.; Pende, D.; Moretta, L.; Bottino, C.; Moretta, A. Natural Killer Cell-Mediated Killing of Freshly Isolated Neuroblastoma Cells. Cancer Res. 2004, 64, 9180–9184. [Google Scholar] [CrossRef] [Green Version]
- Leitner, J.; Klauser, C.; Pickl, W.F.; Stöckl, J.; Majdic, O.; Bardet, A.F.; Kreil, D.P.; Dong, C.; Yamazaki, T.; Zlabinger, G.; et al. B7-H3 Is a Potent Inhibitor of Human T-Cell Activation: No Evidence for B7-H3 and TREML2 Interaction: Cellular Immune Response. Eur. J. Immunol. 2009, 39, 1754–1764. [Google Scholar] [CrossRef]
- Flem-Karlsen, K.; Fodstad, Ø.; Nunes-Xavier, C.E. B7-H3 Immune Checkpoint Protein in Human Cancer. Curr. Med. Chem. 2020, 27, 4062–4086. [Google Scholar] [CrossRef]
- Ni, L.; Dong, C. New Checkpoints in Cancer Immunotherapy. Immunol. Rev. 2017, 276, 52–65. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Kang, F.-B.; Shan, B.-E. B7-H3-Mediated Tumor Immunology: Friend or Foe?: B7-H3-Mediated Tumor Immunology. Int. J. Cancer 2014, 134, 2764–2771. [Google Scholar] [CrossRef] [PubMed]
- Hashiguchi, M.; Kobori, H.; Ritprajak, P.; Kamimura, Y.; Kozono, H.; Azuma, M. Triggering Receptor Expressed on Myeloid Cell-like Transcript 2 (TLT-2) Is a Counter-Receptor for B7-H3 and Enhances T Cell Responses. Proc. Natl. Acad. Sci. USA 2008, 105, 10495–10500. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Flem-Karlsen, K.; Fodstad, Ø.; Tan, M.; Nunes-Xavier, C.E. B7-H3 in Cancer—Beyond Immune Regulation. Trends Cancer 2018, 4, 401–404. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mahmoud, A.M.; Frank, I.; Orme, J.J.; Lavoie, R.R.; Thapa, P.; Costello, B.A.; Cheville, J.C.; Gupta, S.; Dong, H.; Lucien, F. Evaluation of PD-L1 and B7-H3 Expression as a Predictor of Response to Adjuvant Chemotherapy in Bladder Cancer. BMC Urol. 2022, 22, 90. [Google Scholar] [CrossRef] [PubMed]
- Gregorio, A.; Corrias, M.V.; Castriconi, R.; Dondero, A.; Mosconi, M.; Gambini, C.; Moretta, A.; Moretta, L.; Bottino, C. Small Round Blue Cell Tumours: Diagnostic and Prognostic Usefulness of the Expression of B7-H3 Surface Molecule. Histopathology 2008, 53, 73–80. [Google Scholar] [CrossRef] [Green Version]
- Khan, M.; Arooj, S.; Wang, H. Soluble B7-CD28 Family Inhibitory Immune Checkpoint Proteins and Anti-Cancer Immunotherapy. Front. Immunol. 2021, 12, 651634. [Google Scholar] [CrossRef] [PubMed]
- Getu, A.A.; Tigabu, A.; Zhou, M.; Lu, J.; Fodstad, Ø.; Tan, M. New Frontiers in Immune Checkpoint B7-H3 (CD276) Research and Drug Development. Mol. Cancer 2023, 22, 43. [Google Scholar] [CrossRef]
- Zhou, W.-T.; Jin, W.-L. B7-H3/CD276: An Emerging Cancer Immunotherapy. Front. Immunol. 2021, 12, 701006. [Google Scholar] [CrossRef]
- Seaman, S.; Stevens, J.; Yang, M.Y.; Logsdon, D.; Graff-Cherry, C.; Croix, B.S. Genes That Distinguish Physiological and Pathological Angiogenesis. Cancer Cell 2007, 11, 539–554. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, A.K.; Gani, F.; Layman, A.J.; Besharati, S.; Zhu, Q.; Succaria, F.; Engle, E.L.; Bhaijee, F.; Goggins, M.B.; Llosa, N.J.; et al. Multiple Immune-Suppressive Mechanisms in Fibrolamellar Carcinoma. Cancer Immunol. Res. 2019, 7, 805–812. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Zhou, C.; Zhang, D.; Huang, Z.; Zhang, G. The Anti-Apoptotic Effect on Cancer-Associated Fibroblasts of B7-H3 Molecule Enhancing the Cell Invasion and Metastasis in Renal Cancer. OncoTargets Ther. 2019, 12, 4119–4127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vitale, C.; Bottino, C.; Castriconi, R. Monocyte and Macrophage in Neuroblastoma: Blocking Their Pro-Tumoral Functions and Strengthening Their Crosstalk with Natural Killer Cells. Cells 2023, 12, 885. [Google Scholar] [CrossRef] [PubMed]
- Dondero, A.; Morini, M.; Cangelosi, D.; Mazzocco, K.; Serra, M.; Spaggiari, G.M.; Rotta, G.; Tondo, A.; Locatelli, F.; Castellano, A.; et al. Multiparametric Flow Cytometry Highlights B7-H3 as a Novel Diagnostic/Therapeutic Target in GD2neg/Low Neuroblastoma Variants. J. Immunother. Cancer 2021, 9, e002293. [Google Scholar] [CrossRef]
- Schumacher-Kuckelkorn, R.; Volland, R.; Gradehandt, A.; Hero, B.; Simon, T.; Berthold, F. Lack of Immunocytological GD2 Expression on Neuroblastoma Cells in Bone Marrow at Diagnosis, during Treatment, and at Recurrence. Pediatr. Blood Cancer 2017, 64, 46–56. [Google Scholar] [CrossRef]
- Kendsersky, N.M.; Lindsay, J.; Kolb, E.A.; Smith, M.A.; Teicher, B.A.; Erickson, S.W.; Earley, E.J.; Mosse, Y.P.; Martinez, D.; Pogoriler, J.; et al. The B7-H3–Targeting Antibody–Drug Conjugate M276-SL-PBD Is Potently Effective Against Pediatric Cancer Preclinical Solid Tumor Models. Clin. Cancer Res. 2021, 27, 2938–2946. [Google Scholar] [CrossRef] [PubMed]
- Tian, M.; Cheuk, A.T.; Wei, J.S.; Abdelmaksoud, A.; Chou, H.-C.; Milewski, D.; Kelly, M.C.; Song, Y.K.; Dower, C.M.; Li, N.; et al. An Optimized Bicistronic Chimeric Antigen Receptor against GPC2 or CD276 Overcomes Heterogeneous Expression in Neuroblastoma. J. Clin. Investig. 2022, 132, e155621. [Google Scholar] [CrossRef]
- Pulido, R.; Nunes-Xavier, C.E. Hopes on Immunotherapy Targeting B7-H3 in Neuroblastoma. Transl. Oncol. 2023, 27, 101580. [Google Scholar] [CrossRef] [PubMed]
- Louis, D.N.; Perry, A.; Wesseling, P.; Brat, D.J.; Cree, I.A.; Figarella-Branger, D.; Hawkins, C.; Ng, H.K.; Pfister, S.M.; Reifenberger, G.; et al. The 2021 WHO Classification of Tumors of the Central Nervous System: A Summary. Neuro-Oncology 2021, 23, 1231–1251. [Google Scholar] [CrossRef]
- Liu, X.; Ding, C.; Tan, W.; Zhang, A. Medulloblastoma: Molecular Understanding, Treatment Evolution, and New Developments. Pharmacol. Ther. 2020, 210, 107516. [Google Scholar] [CrossRef]
- Knight, A.; Karapetyan, L.; Kirkwood, J.M. Immunotherapy in Melanoma: Recent Advances and Future Directions. Cancers 2023, 15, 1106. [Google Scholar] [CrossRef]
- Del Baldo, G.; Del Bufalo, F.; Pinacchio, C.; Carai, A.; Quintarelli, C.; De Angelis, B.; Merli, P.; Cacchione, A.; Locatelli, F.; Mastronuzzi, A. The Peculiar Challenge of Bringing CAR-T Cells into the Brain: Perspectives in the Clinical Application to the Treatment of Pediatric Central Nervous System Tumors. Front. Immunol. 2023, 14, 1142597. [Google Scholar] [CrossRef]
- Vitanza, N.A.; Wilson, A.L.; Huang, W.; Seidel, K.; Brown, C.; Gustafson, J.A.; Yokoyama, J.K.; Johnson, A.J.; Baxter, B.A.; Koning, R.W.; et al. Intraventricular B7-H3 CAR T Cells for Diffuse Intrinsic Pontine Glioma: Preliminary First-in-Human Bioactivity and Safety. Cancer Discov. 2023, 13, 114–131. [Google Scholar] [CrossRef] [PubMed]
- Castriconi, R.; Dondero, A.; Negri, F.; Bellora, F.; Nozza, P.; Carnemolla, B.; Raso, A.; Moretta, L.; Moretta, A.; Bottino, C. Both CD133+ and CD133− Medulloblastoma Cell Lines Express Ligands for Triggering NK Receptors and Are Susceptible to NK-Mediated Cytotoxicity. Eur. J. Immunol. 2007, 37, 3190–3196. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Yang, J.; Zhu, Y.; Zhu, Y.; Zhang, B.; Zhou, Y. Differential Expression of 2IgB7-H3 and 4IgB7-H3 in Cancer Cell Lines and Glioma Tissues. Oncol. Lett. 2015, 10, 2204–2208. [Google Scholar] [CrossRef] [Green Version]
- Nehama, D.; Di Ianni, N.; Musio, S.; Du, H.; Patané, M.; Pollo, B.; Finocchiaro, G.; Park, J.J.H.; Dunn, D.E.; Edwards, D.S.; et al. B7-H3-Redirected Chimeric Antigen Receptor T Cells Target Glioblastoma and Neurospheres. eBioMedicine 2019, 47, 33–43. [Google Scholar] [CrossRef] [Green Version]
- Ravanpay, A.C.; Gust, J.; Johnson, A.J.; Rolczynski, L.S.; Cecchini, M.; Chang, C.A.; Hoglund, V.J.; Mukherjee, R.; Vitanza, N.A.; Orentas, R.J.; et al. EGFR806-CAR T cells selectively target a tumor-restricted EGFR epitope in glioblastoma. Oncotarget 2019, 10, 7080–7095. [Google Scholar] [CrossRef] [Green Version]
- Kahlon, K.S.; Brown, C.; Cooper, L.J.N.; Raubitschek, A.; Forman, S.J.; Jensen, M.C. Specific Recognition and Killing of Glioblastoma Multiforme by Interleukin 13-Zetakine Redirected Cytolytic T Cells. Cancer Res. 2004, 64, 9160–9166. [Google Scholar] [CrossRef] [Green Version]
- Shah, N.N.; Johnson, B.D.; Schneider, D.; Zhu, F.; Szabo, A.; Keever-Taylor, C.A.; Krueger, W.; Worden, A.A.; Kadan, M.J.; Yim, S.; et al. Bispecific Anti-CD20, Anti-CD19 CAR T Cells for Relapsed B Cell Malignancies: A Phase 1 Dose Escalation and Expansion Trial. Nat. Med. 2020, 26, 1569–1575. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Harrison, E.B.; Li, H.; Hirabayashi, K.; Chen, J.; Li, Q.-X.; Gunn, J.; Weiss, J.; Savoldo, B.; Parker, J.S.; et al. Targeting Brain Lesions of Non-Small Cell Lung Cancer by Enhancing CCL2-Mediated CAR-T Cell Migration. Nat. Commun. 2022, 13, 2154. [Google Scholar] [CrossRef]
- Lin, Y.-H.; Jewell, B.E.; Gingold, J.; Lu, L.; Zhao, R.; Wang, L.L.; Lee, D.-F. Osteosarcoma: Molecular Pathogenesis and iPSC Modeling. Trends Mol. Med. 2017, 23, 737–755. [Google Scholar] [CrossRef]
- Evdokimova, V.; Gassmann, H.; Radvanyi, L.; Burdach, S.E.G. Current State of Immunotherapy and Mechanisms of Immune Evasion in Ewing Sarcoma and Osteosarcoma. Cancers 2022, 15, 272. [Google Scholar] [CrossRef] [PubMed]
- Rocca, V.; Blandino, G.; D’Antona, L.; Iuliano, R.; Di Agostino, S. Li–Fraumeni Syndrome: Mutation of TP53 Is a Biomarker of Hereditary Predisposition to Tumor: New Insights and Advances in the Treatment. Cancers 2022, 14, 3664. [Google Scholar] [CrossRef]
- Koucheki, R.; Gazendam, A.M.; Perera, J.R.; Griffin, A.; Ferguson, P.; Wunder, J.; Tsoi, K. Assessment of Risk of Bias in Osteosarcoma and Ewing’s Sarcoma Randomized Controlled Trials: A Systematic Review. Curr. Oncol. 2021, 28, 3771–3794. [Google Scholar] [CrossRef] [PubMed]
- Daher, M.; Zalaquett, Z.; Chalhoub, R.; Abi Farraj, S.; Abdo, M.; Sebaaly, A.; Kourie, H.-R.; Ghanem, I. Molecular and Biologic Biomarkers of Ewing Sarcoma: A Systematic Review. J. Bone Oncol. 2023, 40, 100482. [Google Scholar] [CrossRef] [PubMed]
- Martin-Giacalone, B.A.; Weinstein, P.A.; Plon, S.E.; Lupo, P.J. Pediatric Rhabdomyosarcoma: Epidemiology and Genetic Susceptibility. J. Clin. Med. 2021, 10, 2028. [Google Scholar] [CrossRef]
- Rudzinski, E.R.; Anderson, J.R.; Hawkins, D.S.; Skapek, S.X.; Parham, D.M.; Teot, L.A. The World Health Organization Classification of Skeletal Muscle Tumors in Pediatric Rhabdomyosarcoma: A Report from the Children’s Oncology Group. Arch. Pathol. Lab. Med. 2015, 139, 1281–1287. [Google Scholar] [CrossRef] [Green Version]
- Xia, S.J.; Holder, D.D.; Pawel, B.R.; Zhang, C.; Barr, F.G. High Expression of the PAX3-FKHR Oncoprotein Is Required to Promote Tumorigenesis of Human Myoblasts. Am. J. Pathol. 2009, 175, 2600–2608. [Google Scholar] [CrossRef] [Green Version]
- Kanayama, T.; Miyachi, M.; Sugimoto, Y.; Yagyu, S.; Kikuchi, K.; Tsuchiya, K.; Iehara, T.; Hosoi, H. Reduced B7-H3 Expression by PAX3-FOXO1 Knockdown Inhibits Cellular Motility and Promotes Myogenic Differentiation in Alveolar Rhabdomyosarcoma. Sci. Rep. 2021, 11, 18802. [Google Scholar] [CrossRef]
- Majzner, R.G.; Theruvath, J.L.; Nellan, A.; Heitzeneder, S.; Cui, Y.; Mount, C.W.; Rietberg, S.P.; Linde, M.H.; Xu, P.; Rota, C.; et al. CAR T Cells Targeting B7-H3, a Pan-Cancer Antigen, Demonstrate Potent Preclinical Activity against Pediatric Solid Tumors and Brain Tumors. Clin. Cancer Res. 2019, 25, 2560–2574. [Google Scholar] [CrossRef]
- Algeri, M.; Merli, P.; Locatelli, F.; Pagliara, D. The Role of Allogeneic Hematopoietic Stem Cell Transplantation in Pediatric Leukemia. J. Clin. Med. 2021, 10, 3790. [Google Scholar] [CrossRef]
- Müller, D. Optimized CD19/CD22/CD3 Antibody. Blood 2022, 140, 1750–1751. [Google Scholar] [CrossRef] [PubMed]
- Hokland, P. AML—A Signature Disease in Haematology. Br. J. Haematol. 2020, 188, 7. [Google Scholar] [CrossRef] [PubMed]
- Papaemmanuil, E.; Gerstung, M.; Bullinger, L.; Gaidzik, V.I.; Paschka, P.; Roberts, N.D.; Potter, N.E.; Heuser, M.; Thol, F.; Bolli, N.; et al. Genomic Classification and Prognosis in Acute Myeloid Leukemia. N. Engl. J. Med. 2016, 374, 2209–2221. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Lv, X.; Wu, Y.; Xu, J.; Wang, L.; Chen, W.; Zhang, W.; Li, J.; Zhang, S.; Qiu, H. Expression of Costimulatory Molecule B7-H3 and Its Prognostic Implications in Human Acute Leukemia. Hematology 2015, 20, 187–195. [Google Scholar] [CrossRef]
- Lichtman, E.I.; Du, H.; Shou, P.; Song, F.; Suzuki, K.; Ahn, S.; Li, G.; Ferrone, S.; Su, L.; Savoldo, B.; et al. Preclinical Evaluation of B7-H3–Specific Chimeric Antigen Receptor T Cells for the Treatment of Acute Myeloid Leukemia. Clin. Cancer Res. 2021, 27, 3141–3153. [Google Scholar] [CrossRef] [PubMed]
- Tyagi, A.; Ly, S.; El-Dana, F.; Yuan, B.; Jaggupilli, A.; Grimm, S.; Konopleva, M.; Bühring, H.-J.; Battula, V.L. Evidence Supporting a Role for the Immune Checkpoint Protein B7-H3 in NK Cell-Mediated Cytotoxicity against AML. Blood 2022, 139, 2782–2796. [Google Scholar] [CrossRef]
- Zorn, K.E.; Cunningham, A.M.; Meyer, A.E.; Carlson, K.S.; Rao, S. Pediatric Myeloid Sarcoma, More than Just a Chloroma: A Review of Clinical Presentations, Significance, and Biology. Cancers 2023, 15, 1443. [Google Scholar] [CrossRef]
- Rasic, P.; Jeremic, M.; Jeremic, R.; Dusanovic Pjevic, M.; Rasic, M.; Djuricic, S.M.; Milickovic, M.; Vukadin, M.; Mijovic, T.; Savic, D. Targeting B7-H3—A Novel Strategy for the Design of Anticancer Agents for Extracranial Pediatric Solid Tumors Treatment. Molecules 2023, 28, 3356. [Google Scholar] [CrossRef]
- Bhutani, N.; Kajal, P.; Sharma, U. Many Faces of Wilms Tumor: Recent Advances and Future Directions. Ann. Med. Surg. 2021, 64, 102202. [Google Scholar] [CrossRef]
- Bai, M.; Li, W.; Yu, N.; Zhang, H.; Long, F.; Zeng, A. The Crosstalk between β-Catenin Signaling and Type I, Type II and Type III Interferons in Lung Cancer Cells. Am. J. Transl. Res. 2017, 9, 2788–2797. [Google Scholar]
- Maturu, P.; Overwijk, W.W.; Hicks, J.; Ekmekcioglu, S.; Grimm, E.A.; Huff, V. Characterization of the Inflammatory Microenvironment and Identification of Potential Therapeutic Targets in Wilms Tumors. Transl. Oncol. 2014, 7, 484–492. [Google Scholar] [CrossRef] [Green Version]
- Bottino, C.; Walzer, T.; Santoni, A.; Castriconi, R. Editorial: TGF-β as a Key Regulator of NK and ILCs Development and Functions. Front. Immunol. 2021, 11, 631712. [Google Scholar] [CrossRef]
- Tran, H.C.; Wan, Z.; Sheard, M.A.; Sun, J.; Jackson, J.R.; Malvar, J.; Xu, Y.; Wang, L.; Sposto, R.; Kim, E.S.; et al. TGFβR1 Blockade with Galunisertib (LY2157299) Enhances Anti-Neuroblastoma Activity of the Anti-GD2 Antibody Dinutuximab (Ch14.18) with Natural Killer Cells. Clin. Cancer Res. 2017, 23, 804–813. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feng, Y.; Xie, K.; Yin, Y.; Li, B.; Pi, C.; Xu, X.; Huang, T.; Zhang, J.; Wang, B.; Gu, H.; et al. A Novel Anti-B7-H3 × Anti-CD3 Bispecific Antibody with Potent Antitumor Activity. Life 2022, 12, 157. [Google Scholar] [CrossRef]
- Vallera, D.A.; Ferrone, S.; Kodal, B.; Hinderlie, P.; Bendzick, L.; Ettestad, B.; Hallstrom, C.; Zorko, N.A.; Rao, A.; Fujioka, N.; et al. NK-Cell-Mediated Targeting of Various Solid Tumors Using a B7-H3 Tri-Specific Killer Engager In Vitro and In Vivo. Cancers 2020, 12, 2659. [Google Scholar] [CrossRef] [PubMed]
- Demaria, O.; Gauthier, L.; Vetizou, M.; Blanchard Alvarez, A.; Vagne, C.; Habif, G.; Batista, L.; Baron, W.; Belaïd, N.; Girard-Madoux, M.; et al. Antitumor Immunity Induced by Antibody-Based Natural Killer Cell Engager Therapeutics Armed with Not-Alpha IL-2 Variant. Cell Rep. Med. 2022, 3, 100783. [Google Scholar] [CrossRef] [PubMed]
- Moghimi, B.; Muthugounder, S.; Jambon, S.; Tibbetts, R.; Hung, L.; Bassiri, H.; Hogarty, M.D.; Barrett, D.M.; Shimada, H.; Asgharzadeh, S. Preclinical Assessment of the Efficacy and Specificity of GD2-B7H3 SynNotch CAR-T in Metastatic Neuroblastoma. Nat. Commun. 2021, 12, 511. [Google Scholar] [CrossRef]
- Caruso, S.; De Angelis, B.; Del Bufalo, F.; Ciccone, R.; Donsante, S.; Volpe, G.; Manni, S.; Guercio, M.; Pezzella, M.; Iaffaldano, L.; et al. Safe and Effective Off-the-Shelf Immunotherapy Based on CAR.CD123-NK Cells for the Treatment of Acute Myeloid Leukaemia. J. Hematol. Oncol. 2022, 15, 163. [Google Scholar] [CrossRef]
- Rongvaux, A.; Willinger, T.; Martinek, J.; Strowig, T.; Gearty, S.V.; Teichmann, L.L.; Saito, Y.; Marches, F.; Halene, S.; Palucka, A.K.; et al. Development and Function of Human Innate Immune Cells in a Humanized Mouse Model. Nat. Biotechnol. 2014, 32, 364–372. [Google Scholar] [CrossRef]
- Fitzgerald, A.A.; Li, E.; Weiner, L.M. 3D Culture Systems for Exploring Cancer Immunology. Cancers 2020, 13, 56. [Google Scholar] [CrossRef]
- Marzagalli, M.; Pelizzoni, G.; Fedi, A.; Vitale, C.; Fontana, F.; Bruno, S.; Poggi, A.; Dondero, A.; Aiello, M.; Castriconi, R.; et al. A Multi-Organ-on-Chip to Recapitulate the Infiltration and the Cytotoxic Activity of Circulating NK Cells in 3D Matrix-Based Tumor Model. Front. Bioeng. Biotechnol. 2022, 10, 945149. [Google Scholar] [CrossRef] [PubMed]
| NCT Number | Title | Status | Study Results | Conditions | Interventions | Age | Phases | Locations |
|---|---|---|---|---|---|---|---|---|
| ClinicalTrials.gov Identifier: NCT05063357 | 131I-omburtamab Delivered by Convection-Enhanced Delivery in Patients With Diffuse Intrinsic Pontine Glioma | Not yet recruiting | No Results Available | Diffuse Intrinsic Pontine Glioma | Drug: 131I-Omburtamab|Device: Convention Enhanced Delivery | 3 Years to 21 Years (Child, Adult) | Phase 1 | Y-mAbs Therapeutics, Labcorp Corporation of America Holdings, Inc. Invicro, Burlington, North Carolina |
| ClinicalTrials.gov Identifier: NCT04167618 | 177Lu-DTPA-Omburtamab Radioimmunotherapy for Recurrent or Refractory Medulloblastoma | Terminated | No Results Available | Medulloblastoma, Childhood | Drug: 177Lu-DTPA-omburtamab | 3 Years to 19 Years (Child, Adult) | Phase 1| Phase 2 | Mayo Clinic, Rochester, MN, United States| Memorial Sloan Kettering Cancer Center, New York, NY, United States|Doernbecher Children’s Hospital, Portland, OR, United States|M.D. Anderson Cancer Center, Houston, TX, United States|Rigshospitalet, Børneonkologisk afsnit, Copenhagen, Denmark|Princess Máxima, Utrecht, Netherlands|Hospital Universitari Vall d’Hebron, Barcelona, Spain|Hospital Sant Joan de Déu de Barcelona, Barcelona, Spain|The Royal Marsden Hospital, London, United Kingdom|Great North Children’s Hospital, Newcastle, United Kingdom |
| ClinicalTrials.gov Identifier: NCT03275402 | 131I-omburtamab Radioimmunotherapy for Neuroblastoma Central Nervous System/Leptomeningeal Metastases | Active, not recruiting | No Results Available | Neuroblastoma|CNS Metastases| Leptomeningeal Metastases | Biological: 131I-omburtamab | up to 18 Years (Child, Adult) | Phase 2| Phase 3 | Children’s Hospital Los Angeles, Los Angeles, CA, United States|Riley Hospital for Children, Indianapolis, IN, United States|Memorial Sloan Kettering Cancer Center, New York, NY, United States|Nationwide Children’s Hospital, Columbus, OH, United States|M.D. Anderson Cancer Center, Houston, TX, United States|Rigshospitalet, København, Denmark| Department of Pediatric Oncology Fukushima Medical University Hospital, Fukushima City, Japan|Hospital Sant Joan de Déu, Barcelona, Spain |
| ClinicalTrials.gov Identifier: NCT04743661 | 131I-Omburtamab, in Recurrent Medulloblastoma and Ependymoma | Active, not recruiting | No Results Available | Recurrent Medulloblastoma| Recurrent Ependymoma | Drug: Irinotecan|Drug: Temozolomide|Drug: Bevacizumab|Drug: Omburtamab I-131|Drug: Liothyronine|Drug: SSKI|Drug: Dexamethasone|Drug: Antipyretic|Drug: Antihistamine|Drug: anti-emetics | up to 21 Years (Child, Adult) | Phase 2 | Children’s Hospital Los Angeles, Los Angeles, CA, United States|Memorial Sloan Kettering Cancer Center, New York, NY, United States|Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, United States |
| ClinicalTrials.gov Identifier: NCT01502917 | Convection-Enhanced Delivery of 124I-Omburtamab for Patients With Non-Progressive Diffuse Pontine Gliomas Previously Treated With External Beam Radiation Therapy | Completed | No Results Available | Brain Cancer|Brain Stem Glioma | Drug: Radioactive iodine-labeled monoclonal antibody omburtamab|Radiation: External Beam Radiotherapy | 2 Years to 21 Years (Child, Adult) | Phase 1 | Weill Medical College of Cornell University, New York, NY, United States|Memorial Sloan Kettering Cancer Center, New York, NY, United States |
| ClinicalTrials.gov Identifier: NCT05064306 | 131I-omburtamab for the Treatment of Central Nervous System/Leptomeningeal Neoplasms in Children and Young Adults | Available | No Results Available | Central Nervous System/ Leptomeningeal Neoplasms | Drug: 131I-omburtamab | Child, Adult, Older Adult | Memorial Sloan Kettering Cancer Center, New York, NY, United States | |
| ClinicalTrials.gov Identifier: NCT04022213 | A Study of the Drug I131-Omburtamab in People With Desmoplastic Small Round Cell Tumors and Other Solid Tumors in the Peritoneum | Recruiting | No Results Available | Desmoplastic Small Round Cell Tumor|Peritoneal Cancer| Peritoneal Carcinoma | Drug: 131 I-omburtamab|Radiation: WAP-IMRT | 1 Year and older (Child, Adult, Older Adult) | Phase 2 | Memorial Sloan Kettering Cancer Center, New York, NY, United States |
| ClinicalTrials.gov Identifier: NCT00089245 | Radiolabeled Monoclonal Antibody Therapy in Treating Patients With Refractory, Recurrent, or Advanced CNS or Leptomeningeal Cancer | Active, not recruiting | No Results Available | Brain and Central Nervous System Tumors|Neuroblastoma| Sarcoma | Drug: Iodine I 131 MOAB 8H9 | Child, Adult, Older Adult | Phase 1 | Memorial Sloan Kettering Cancer Center, New York, NY, United States |
| ClinicalTrials.gov Identifier: NCT04185038 | Study of B7-H3-Specific CAR-T Cell Locoregional Immunotherapy for Diffuse Intrinsic Pontine Glioma/Diffuse Midline Glioma and Recurrent or Refractory Pediatric Central Nervous System Tumors | Recruiting | No Results Available | Central Nervous System Tumor|Diffuse Intrinsic Pontine Glioma|Diffuse Midline Glioma|Ependymoma| Medulloblastoma, Childhood|Germ Cell Tumor|Atypical Teratoid/Rhabdoid Tumor| Primitive Neuroectodermal Tumor|Choroid Plexus Carcinoma|Pineoblastoma, Childhood|Glioma | Biological: SCRI-CARB7H3(s); B7H3-specific chimeric antigen receptor (CAR) T cel | 1 Year to 26 Years (Child, Adult) | Phase 1 | Seattle Children’s Hospital Seattle, WA, United State |
| ClinicalTrials.gov Identifier: NCT05768880 | Study of B7-H3, EGFR806, HER2, And IL13-Zetakine (Quad) CAR-T Cell Locoregional Immunotherapy For Pediatric Diffuse Intrinsic Pontine Glioma, Diffuse Midline Glioma, And Recurrent Or Refractory Central Nervous System Tumors | Not yet recruiting | No Results Available | Diffuse Intrinsic Pontine Glioma|Diffuse Midline Glioma|Recurrent CNS Tumor, Adult|Recurrent, CNS Tumor, Childhood|Refractory Primary Malignant Central Nervous System Neoplasm | Biological: SC-CAR4BRAIN | 1 Year to 26 Years (Child, Adult) | Phase 1 | Seattle Children’s Hospital Seattle, WA, United States |
| ClinicalTrials.gov Identifier: NCT02982941 | Enoblituzumab (MGA271) in Children With B7-H3-expressing Solid Tumors | Completed | No Results Available | Neuroblastoma| Rhabdomyosarcoma| Osteosarcoma| Ewing Sarcoma|Wilms Tumor|Desmoplastic Small Round Cell Tumor | Drug: Enoblituzumab | 1 Year to 35 Years (Child, Adult) | Phase 1 | Lucile Packard Children’s Hospital, Stanford, Palo Alto, California; National Cancer Institute, Center for Cancer Research, Bethesda, Maryland; Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania; Texas Children’s Hospital Houston, Texas; Seattle Children’s, Seattle, Washington; University of Wisconsin, American Family Children’s Hospital, Madison, Wisconsin |
| ClinicalTrials.gov Identifier: NCT04897321 | B7-H3-Specific Chimeric Antigen Receptor Autologous T-Cell Therapy for Pediatric Patients With Solid Tumors (3CAR) | Recruiting | No Results Available | Pediatric Solid Tumor| Osteosarcoma| Rhabdomyosarcoma| Neuroblastoma|Ewing Sarcoma|Wilms Tumor| Adrenocortical Cancer| Desmoplastic Small Round Cell Tumor|Germ Cell Cancer|Rhabdoid Tumor|Clear Cell Sarcoma|Hepatoblastoma| Melanoma|Carcinoma|Malignant Peripheral Nerve Sheath Tumors|Soft Tissue Sarcoma | Drug: Fludarabine Drug: Cyclophosphamide Drug: MESNA| Drug: B7-H3 CAR-T cells | up to 21 Years (Child, Adult) | Phase 1 | St. Jude Children’s Research Hospital, Memphis, TN, United States |
| ClinicalTrials.gov Identifier: NCT04864821 | Clinical Study of CD276 Targeted Autologous Chimeric Antigen Receptor T-Cell Infusion in Patients With CD276 Positive Advanced Solid Tumor | Not yet recruiting | No Results Available | Osteosarcoma|Neuroblastoma| Gastric Cancer|Lung Cancer | Drug: Targeting CD276 CAR-T cells | 1 Year to 70 Years (Child, Adult, Older Adult) | Early Phase 1 | PersonGen BioTherapeutics (Suzhou) Co., Ltd., The First Affiliated Hospital of Zhengzhou University |
| ClinicalTrials.gov Identifier: NCT04483778 | B7H3 CAR-T Cell Immunotherapy for Recurrent/Refractory Solid Tumors in Children and Young Adults | Recruiting | No Results Available | Pediatric Solid Tumor|Germ Cell Tumor|Retinoblastoma| Hepatoblastoma|Wilms Tumor|Rhabdoid Tumor| Carcinoma|Osteosarcoma| Ewing Sarcoma| Rhabdomyosarcoma| Synovial Sarcoma|Clear Cell Sarcoma|Malignant Peripheral Nerve Sheath Tumors|Desmoplastic Small Round Cell Tumor|Soft Tissue Sarcoma| Neuroblastoma|Melanoma | Biological: second generation 4-1BBz B7H3-EGFRt-DHFR Biological: second generation 4-1BBz B7H3-EGFRt-DHFR(selected) and a second generation 4-1BBz CD19-Her2tG | 0 Years to 26 Years (Child, Adult) | Phase 1 | Seattle Children’s Hospital, Seattle, WA, United States |
| ClinicalTrials.gov Identifier: NCT04432649 | Targeting CD276 (B7-H3) Positive Solid Tumors by 4SCAR-276 | Recruiting | No Results Available | Solid Tumor | Biological: 4SCAR-276 | 1 Year to 75 Years (Child, Adult, Older Adult) | Phase 1| Phase 2 | Shenzhen Children’s Hospital, Shenzhen Geno-immune Medical Institute, Sun Yat-Sen University, Shenzhen, Guangdong, China |
| ClinicalTrials.gov Identifier: NCT05731219 | UTAA06 Injection in the Treatment of Relapsed/Refractory Acute Myeloid Leukemia | Recruiting | No Results Available | Relapsed/Refractory Acute Myeloid Leukemia | Biological: B7-H3 target, CAR gene-modified gdT cell injection | 18 Years and older (Adult, Older Adult) | Phase 1 | The First Affiliated Hospital, Zhejiang University School of Medicine Hangzhou, Zhejiang, China |
| ClinicalTrials.gov Identifier: NCT05722171 | Clinical Study of UTAA06 Injection in the Treatment of Relapsed/Refractory Acute Myeloid Leukemia | Recruiting | No Results Available | Relapsed/Refractory Acute Myeloid Leukemia | Biological: gdT cell injection targeting B7-H3 chimeric antigen receptor | 18 Years and older (Adult, Older Adult) | Early Phase 1 | PersonGen Anke Cellular Therapeutics Co., Ltd. Hefei, Anhui, China |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bottino, C.; Vitale, C.; Dondero, A.; Castriconi, R. B7-H3 in Pediatric Tumors: Far beyond Neuroblastoma. Cancers 2023, 15, 3279. https://doi.org/10.3390/cancers15133279
Bottino C, Vitale C, Dondero A, Castriconi R. B7-H3 in Pediatric Tumors: Far beyond Neuroblastoma. Cancers. 2023; 15(13):3279. https://doi.org/10.3390/cancers15133279
Chicago/Turabian StyleBottino, Cristina, Chiara Vitale, Alessandra Dondero, and Roberta Castriconi. 2023. "B7-H3 in Pediatric Tumors: Far beyond Neuroblastoma" Cancers 15, no. 13: 3279. https://doi.org/10.3390/cancers15133279







