Recent Advances in Locoregional Therapy of Hepatocellular Carcinoma
Abstract
:Simple Summary
Abstract
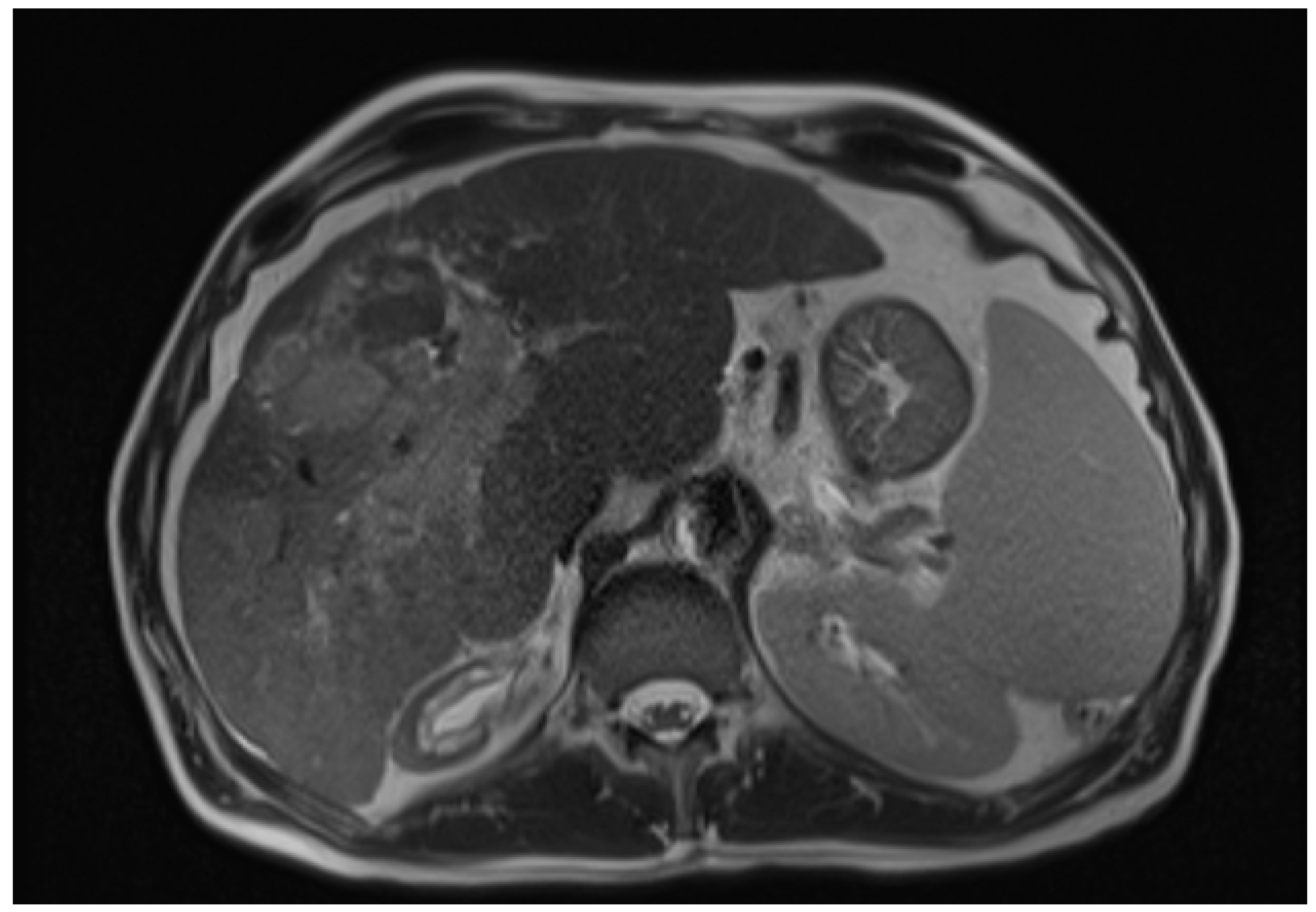
1. Introduction
2. Radiofrequency Ablation (RFA)
- Grade A—absolutely curative with 5 mm ablative margin around the entire tumour.
- Grade B—relatively curative, mostly as grade A with some places with the lower margin.
- Grade C—an incomplete ablative margin around the tumour, although no residual tumour is apparent.
3. TACE
4. Transarterial Radioembolisation (TARE), Also Known as Selective Internal Radiation Therapy (SIRT)
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Garcia-Monaco, R.D.; Chung, J.W.; Vilgrain, V.; Bouattour, M.; Covey, A.M. Summary of key guidelines for locoregional treatment of HCC in Asia, Europe, South and North America. Br. J. Radiol. 2022, 95, 20220179. [Google Scholar] [CrossRef] [PubMed]
- Su, G.L.; Altayar, O.; O’shea, R.; Shah, R.; Estfan, B.; Wenzell, C.; Sultan, S.; Falck-Ytter, Y. AGA Clinical Practice Guideline on Systemic Therapy for Hepatocellular Carcinoma. Gastroenterology 2022, 162, 920–934. [Google Scholar] [CrossRef] [PubMed]
- Ryder, S.D. Guidelines for the diagnosis and treatment of hepatocellular carcinoma (HCC) in adults. Gut 2003, 52, iii1–iii8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Llovet, J.M.; De Baere, T.; Kulik, L.; Haber, P.K.; Greten, T.F.; Meyer, T.; Lencioni, R. Locoregional therapies in the era of molecular and immune treatments for hepatocellular carcinoma. Nat. Rev. Gastroenterol. Hepatol. 2021, 18, 293–313. [Google Scholar] [CrossRef]
- Wen, N.; Cai, Y.; Li, F.; Ye, H.; Tang, W.; Song, P.; Cheng, N. The clinical management of hepatocellular carcinoma worldwide: A concise review and comparison of current guidelines: 2022 update. Biosci. Trends 2022, 16, 20–30. [Google Scholar] [CrossRef]
- Renzulli, M.; Golfieri, R.; Bologna Liver Oncology Group (BLOG). Proposal of a new diagnostic algorithm for hepatocellular carcinoma based on the Japanese guidelines but adapted to the Western world for patients under surveillance for chronic liver disease. J. Gastroenterol. Hepatol. 2016, 31, 69–80. [Google Scholar] [CrossRef] [Green Version]
- Park, H.J.; Jang, H.Y.; Kim, S.Y.; Lee, S.J.; Won, H.J.; Byun, J.H.; Choi, S.H.; Lee, S.S.; An, J.; Lim, Y.-S. Non-enhanced magnetic resonance imaging as a surveillance tool for hepatocellular carcinoma: Comparison with ultrasound. J. Hepatol. 2020, 72, 718–724. [Google Scholar] [CrossRef]
- Zhang, Y.; Numata, K.; Du, Y.; Maeda, S. Contrast Agents for Hepatocellular Carcinoma Imaging: Value and Progression. Front. Oncol. 2022, 12, 921667. [Google Scholar] [CrossRef]
- El-Feky, M. Infiltrative HCC—Portal vein tumour thrombus. Radiopaedia 2020, 75063. [Google Scholar] [CrossRef]
- Apisarnthanarax, S.; Barry, A.; Cao, M.; Czito, B.; DeMatteo, R.; Drinane, M.; Hallemeier, C.L.; Koay, E.J.; Lasley, F.; Meyer, J.; et al. External Beam Radiation Therapy for Primary Liver Cancers: An ASTRO Clinical Practice Guideline. Pract. Radiat. Oncol. 2022, 12, 28–51. [Google Scholar] [CrossRef]
- Zhou, J.; Sun, H.; Wang, Z.; Cong, W.; Wang, J.; Zeng, M.; Zhou, W.; Bie, P.; Liu, L.; Wen, T.; et al. Guidelines for the Diagnosis and Treatment of Hepatocellular Carcinoma (2019 Edition). Liver Cancer 2020, 9, 682–720. [Google Scholar] [CrossRef]
- Chen, L.-C.; Lin, H.-Y.; Hung, S.-K.; Chiou, W.-Y.; Lee, M.-S. Role of modern radiotherapy in managing patients with hepatocellular carcinoma. World J. Gastroenterol. 2021, 27, 2434–2457. [Google Scholar] [CrossRef]
- Delis, S.-G.; Dervenis, C. Selection criteria for liver resection in patients with hepatocellular carcinoma and chronic liver disease. World J. Gastroenterol. 2008, 14, 3452–3460. [Google Scholar] [CrossRef] [PubMed]
- Bruix, J.; Sherman, M.; Llovet, J.M.; Beaugrand, M.; Lencioni, R.; Burroughs, A.K.; Christensen, E.; Pagliaro, L.; Colombo, M.; Rodés, J. Clinical Management of Hepatocellular Carcinoma. Conclusions of the Barcelona-2000 EASL Conference. J. Hepatol. 2001, 35, 421–430. [Google Scholar] [CrossRef] [PubMed]
- Tzartzeva, K.; Obi, J.; Rich, N.E.; Parikh, N.D.; Marrero, J.A.; Yopp, A.; Waljee, A.K.; Singal, A.G. Surveillance Imaging and Alpha Fetoprotein for Early Detection of Hepatocellular Carcinoma in Patients With Cirrhosis: A Meta-analysis. Gastroenterology 2018, 154, 1706–1718.e1. [Google Scholar] [CrossRef] [Green Version]
- Sparchez, Z.; Radu, P.; Bartos, A.; Nenu, I.; Craciun, R.; Mocan, T.; Horhat, A.; Spârchez, M.; Dufour, J.-F. Combined treatments in hepatocellular carcinoma: Time to put them in the guidelines? World J. Gastrointest. Oncol. 2021, 13, 1896–1918. [Google Scholar] [CrossRef]
- Qiu, J.; Chen, S.; Wu, H. Long-term outcomes after hepatic resection combined with radiofrequency ablation for initially unresectable multiple and bilobar liver malignancies. J. Surg. Res. 2014, 188, 14–20. [Google Scholar] [CrossRef]
- Di Martino, M.; Vitale, A.; Ferraro, D.; Maniscalco, M.; Pisaniello, D.; Arenga, G.; Falaschi, F.; Terrone, A.; Iacomino, A.; Lanza, A.G.; et al. Downstaging Therapies for Patients with Hepatocellular Carcinoma Awaiting Liver Transplantation: A Systematic Review and Meta-Analysis on Intention-to-Treat Outcomes. Cancers 2022, 14, 5102. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Lan, T.; Zhong, H.; Zhang, Z.; Xie, H.; Li, Y.; Huang, W. To Systematically Evaluate and Analyze the Efficacy and Safety of Transcatheter Arterial Chemoembolization (TACE) in the Treatment of Primary Liver Cancer. J. Health Eng. 2022, 2022, 8223336. [Google Scholar] [CrossRef]
- Chen, X.; Lai, L.; Ye, J.; Li, L. Downstaging Therapies for Unresectable Hepatocellular Carcinoma Prior to Hepatic Resection: A Systematic Review and Meta-Analysis. Front. Oncol. 2021, 11, 740762. [Google Scholar] [CrossRef]
- Lobo, L.; Yakoub, D.; Picado, O.; Ripat, C.; Pendola, F.; Sharma, R.; ElTawil, R.; Kwon, D.; Venkat, S.; Portelance, L.; et al. Unresectable Hepatocellular Carcinoma: Radioembolization Versus Chemoembolization: A Systematic Review and Meta-analysis. Cardiovasc. Interv. Radiol. 2016, 39, 1580–1588. [Google Scholar] [CrossRef]
- Sangro, B.; Sarobe, P.; Hervás-Stubbs, S.; Melero, I. Advances in immunotherapy for hepatocellular carcinoma. Nat. Rev. Gastroenterol. Hepatol. 2021, 18, 525–543. [Google Scholar] [CrossRef] [PubMed]
- Marrero, J.A.; Kulik, L.M.; Sirlin, C.B.; Zhu, A.X.; Finn, R.S.; Abecassis, M.M.; Roberts, L.R.; Heimbach, J.K. Diagnosis, Staging, and Management of Hepatocellular Carcinoma: 2018 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology 2018, 68, 723–750. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2018, 69, 182–236. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Llovet, J.M.; Lencioni, R. mRECIST for HCC: Performance and novel refinements. J. Hepatol. 2020, 72, 288–306. [Google Scholar] [CrossRef] [Green Version]
- Rosenthal, D.I.; Alexander, A.; Rosenberg, A.A.; Springfield, D. Ablation of osteoid osteomas with a percutaneously placed electrode: A new procedure. Radiology 1992, 183, 29–33. [Google Scholar] [CrossRef]
- Omata, M.; Lesmana, L.A.; Tateishi, R.; Chen, P.-J.; Lin, S.-M.; Yoshida, H.; Kudo, M.; Lee, J.M.; Choi, B.I.; Poon, R.T.P.; et al. Asian Pacific Association for the Study of the Liver consensus recommendations on hepatocellular carcinoma. Hepatol. Int. 2010, 4, 439–474. [Google Scholar] [CrossRef] [Green Version]
- Nishikawa, H.; Kimura, T.; Kita, R.; Osaki, Y. Radiofrequency ablation for hepatocellular carcinoma. Int. J. Hyperth. 2013, 29, 558–568. [Google Scholar] [CrossRef]
- Curley, S.A.; Izzo, F.; Ellis, L.M.; Vauthey, J.N.; Vallone, P. Radiofrequency Ablation of Hepatocellular Cancer in 110 Patients with Cirrhosis. Ann. Surg. 2000, 232, 381–391. [Google Scholar] [CrossRef]
- Ishikawa, T.; Kohno, T.; Shibayama, T.; Fukushima, Y.; Obi, S.; Teratani, T.; Shiina, S.; Shiratori, Y.; Omata, M. Thoracoscopic Thermal Ablation Therapy for Hepatocellular Carcinoma Located Beneath the Diaphragm. Endoscopy 2001, 33, 697–702. [Google Scholar] [CrossRef]
- Tiong, L.; Maddern, G.J. Systematic review and meta-analysis of survival and disease recurrence after radiofrequency ablation for hepatocellular carcinoma. Br. J. Surg. 2011, 98, 1210–1224. [Google Scholar] [CrossRef] [PubMed]
- Kudo, M. Radiofrequency Ablation for Hepatocellular Carcinoma: Updated Review in 2010. Oncology 2010, 78, 113–124. [Google Scholar] [CrossRef] [PubMed]
- HirokiNishikawa, H.; Inuzuka, T.; Takeda, H.; Nakajima, J.; Matsuda, F.; Sakamoto, A.; Henmi, S.; Hatamaru, K.; Ishikawa, T.; Saito, S.; et al. Comparison of percutaneous radiofrequency thermal ablation and surgical resection for small hepatocellular carcinoma. BMC Gastroenterol. 2011, 11, 143. [Google Scholar] [CrossRef] [Green Version]
- Chan, A.C.Y.; Chan, S.C.; Chok, K.S.H.; Cheung, T.T.; Chiu, D.W.; Poon, R.T.P.; Fan, S.T.; Lo, C.M. Treatment strategy for recurrent hepatocellular carcinoma: Salvage transplantation, repeated resection, or radiofrequency ablation? Liver Transplant. 2013, 19, 411–419. [Google Scholar] [CrossRef]
- Lau, W.Y.; Lai, E.C.H. The Current Role of Radiofrequency Ablation in the Management of Hepatocellular Carcinoma. Ann. Surg. 2009, 249, 20–25. [Google Scholar] [CrossRef]
- Lencioni, R. Loco-regional treatment of hepatocellular carcinoma. Hepatology 2010, 52, 762–773. [Google Scholar] [CrossRef]
- Sheiman, R.G.; Mullan, C.; Ahmed, M. In vivo determination of a modified heat capacity of small hepatocellular carcinomas prior to radiofrequency ablation: Correlation with adjacent vasculature and tumour recurrence. Int. J. Hyperth. 2012, 28, 122–131. [Google Scholar] [CrossRef]
- Rossi, S.; Di Stasi, M.; Buscarini, E.; Quaretti, P.; Garbagnati, F.; Squassante, L.; Paties, C.T.; E Silverman, D. Percutaneous RF interstitial thermal ablation in the treatment of hepatic cancer. Am. J. Roentgenol. 1996, 167, 759–768. [Google Scholar] [CrossRef] [Green Version]
- Germani, G.; Pleguezuelo, M.; Gurusamy, K.; Meyer, T.; Isgrò, G.; Burroughs, A.K. Clinical outcomes of radiofrequency ablation, percutaneous alcohol and acetic acid injection for hepatocelullar carcinoma: A meta-analysis. J. Hepatol. 2010, 52, 380–388. [Google Scholar] [CrossRef]
- Kudo, M. Local ablation therapy for hepatocellular carcinoma: Current status and future perspectives. J. Gastroenterol. 2004, 39, 205–214. [Google Scholar] [CrossRef]
- Kasugai, H.; Osaki, Y.; Oka, H.; Kudo, M.; Seki, T. Severe Complications of Radiofrequency Ablation Therapy for Hepatocellular Carcinoma: An Analysis of 3891 Ablations in 2614 Patients. Oncology 2007, 72, 72–75. [Google Scholar] [CrossRef] [PubMed]
- Xuan, D.; Wen, W.; Xu, D.; Jin, T. Survival comparison between radiofrequency ablation and surgical resection for patients with small hepatocellular carcinoma: A systematic review and meta-analysis. Medicine 2021, 100, e24585. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Wang, R.; Liu, S.; Peng, G.; Yu, H.; Wang, X. Comparison of the safety and efficacy of hepatic resection and radiofrequency ablation in the treatment of single small hepatocellular carcinoma: Systematic review and meta-analysis. Transl. Cancer Res. 2022, 11, 580–590. [Google Scholar] [CrossRef] [PubMed]
- Jie, T.; Guoying, F.; Gang, T.; Zhengrong, S.; Maoping, L. Efficacy and Safety of Fusion Imaging in Radiofrequency Ablation of Hepatocellular Carcinoma Compared to Ultrasound: A Meta-Analysis. Front. Surg. 2021, 8, 728098. [Google Scholar] [CrossRef] [PubMed]
- Nishikawa, H.; Inuzuka, T.; Takeda, H.; Nakajima, J.; Sakamoto, A.; Henmi, S.; Matsuda, F.; Eso, Y.; Ishikawa, T.; Saito, S.; et al. Percutaneous radiofrequency ablation therapy for hepatocellular carcinoma: A proposed new grading system for the ablative margin and prediction of local tumor progression and its validation. J. Gastroenterol. 2011, 46, 1418–1426. [Google Scholar] [CrossRef] [PubMed]
- Vestito, A.; Dajti, E.; Cortellini, F.; Montagnani, M.; Bazzoli, F.; Zagari, R.M. Can Liver Ultrasound Elastography Predict the Risk of Hepatocellular Carcinoma Recurrence After Radiofrequency Ablation? A Systematic Review and Meta-Analysis. Ultraschall Med. 2021, 44, e139–e147. [Google Scholar] [CrossRef]
- Yu, Q.; Liu, C.; Navuluri, R.; Ahmed, O. Percutaneous microwave ablation versus radiofrequency ablation of hepatocellular carcinoma: A meta-analysis of randomized controlled trials. Abdom. Radiol. 2021, 46, 4467–4475. [Google Scholar] [CrossRef]
- Spiliotis, A.E.; Gäbelein, G.; Holländer, S.; Scherber, P.-R.; Glanemann, M.; Patel, B. Microwave ablation compared with radiofrequency ablation for the treatment of liver cancer: A systematic review and meta-analysis. Radiol. Oncol. 2021, 55, 247–258. [Google Scholar] [CrossRef]
- Khan, A.; Mostowy, M.; Owusu, M.; Mutambanengwe, M.; Habimana, S.; Bence, S.; Facciorusso, A. Microwave ablation determines similar survival outcomes as compared to radiofrequency ablation for the treatment of hepatocellular carcinoma. Expert Rev. Gastroenterol. Hepatol. 2020, 15, 829–833. [Google Scholar] [CrossRef]
- Ricci, A.D.; Rizzo, A.; Bonucci, C.; Tavolari, S.; Palloni, A.; Frega, G.; Mollica, V.; Tober, N.; Mazzotta, E.; Felicani, C.; et al. The (Eternal) Debate on Microwave Ablation Versus Radiofrequency Ablation in BCLC-A Hepatocellular Carcinoma. Vivo 2020, 34, 3421–3429. [Google Scholar] [CrossRef]
- Han, J.; Fan, Y.-C.; Wang, K. Radiofrequency ablation versus microwave ablation for early stage hepatocellular carcinoma. Medicine 2020, 99, e22703. [Google Scholar] [CrossRef] [PubMed]
- Cui, R.; Yu, J.; Kuang, M.; Duan, F.; Liang, P. Microwave ablation versus other interventions for hepatocellular carcinoma: A systematic review and meta-analysis. J. Cancer Res. Ther. 2020, 16, 379–386. [Google Scholar] [CrossRef]
- Facciorusso, A.; El Aziz, M.A.A.; Tartaglia, N.; Ramai, D.; Mohan, B.P.; Cotsoglou, C.; Pusceddu, S.; Giacomelli, L.; Ambrosi, A.; Sacco, R. Microwave Ablation Versus Radiofrequency Ablation for Treatment of Hepatocellular Carcinoma: A Meta-Analysis of Randomized Controlled Trials. Cancers 2020, 12, 3796. [Google Scholar] [CrossRef]
- Lu, D.-E.; Cheng, S.-W.; Lin, Y.-S.; Tu, M.-W.; Lee, C.-H.; Chen, C.; Chen, K.-H. Radiofrequency ablation and percutaneous ethanol injection versus radiofrequency ablation alone for hepatocellular carcinoma: A systematic review and meta-analysis. Ann. Hepatol. 2022, 27, 100729. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Tong, Y.; Yang, L.; He, X.; Bao, G.; Du, X. Identifying optimal therapies in patients with advanced hepatocellular carcinoma: A systematic review and network meta-analysis. Transl. Gastroenterol. Hepatol. 2022, 7, 38. [Google Scholar] [CrossRef]
- Yang, Y.; Yu, H.; Qi, L.; Liu, C.; Feng, Y.; Qi, J.; Li, J.; Zhu, Q. Combined radiofrequency ablation or microwave ablation with transarterial chemoembolization can increase efficiency in intermediate-stage hepatocellular carcinoma without more complication: A systematic review and meta-analysis. Int. J. Hyperth. 2022, 39, 455–465. [Google Scholar] [CrossRef]
- Gui, C.H.; Baey, S.; D’Cruz, R.T.; Shelat, V.G. Trans-arterial chemoembolization + radiofrequency ablation versus surgical resection in hepatocellular carcinoma—A meta-analysis. Eur. J. Surg. Oncol. 2020, 46, 763–771. [Google Scholar] [CrossRef]
- Kwak, M.H.; Lee, M.W.; Ko, S.E.; Rhim, H.; Kang, T.W.; Song, K.D.; Kim, J.M.; Choi, G.-S. Laparoscopic radiofrequency ablation versus percutaneous radiofrequency ablation for subphrenic hepatocellular carcinoma. Ultrasonography 2022, 41, 543–552. [Google Scholar] [CrossRef] [PubMed]
- Hendriks, P.; Rietbergen, D.D.D.; van Erkel, A.R.; Coenraad, M.J.; Arntz, M.J.; Bennink, R.J.; Braat, A.E.; Crobach, A.S.L.P.; van Delden, O.M.; van der Hulle, T.; et al. Study Protocol: Adjuvant Holmium-166 Radioembolization After Radiofrequency Ablation in Early-Stage Hepatocellular Carcinoma Patients—A Dose-Finding Study (HORA EST HCC Trial). Cardiovasc. Interv. Radiol. 2022, 45, 1057–1063. [Google Scholar] [CrossRef]
- Radosevic, A.; Quesada, R.; Serlavos, C.; Sánchez, J.; Zugazaga, A.; Sierra, A.; Coll, S.; Busto, M.; Aguilar, G.; Flores, D.; et al. Microwave versus radiofrequency ablation for the treatment of liver malignancies: A randomized controlled phase 2 trial. Sci. Rep. 2022, 12, 1–10. [Google Scholar] [CrossRef]
- Suh, Y.S.; Choi, J.W.; Yoon, J.H.; Lee, D.H.; Kim, Y.J.; Lee, J.H.; Yu, S.J.; Cho, E.J.; Yoon, J.H. No-Touch vs. Conventional Radiofrequency Ablation Using Twin Internally Cooled Wet Electrodes for Small Hepatocellular Carcinomas: A Randomized Prospective Comparative Study. Korean J. Radiol. 2022, 22, 1974–1984. [Google Scholar] [CrossRef] [PubMed]
- Bockorny, B.; Bullock, A.J.; Abrams, T.A.; Faintuch, S.; Alsop, D.C.; Goldberg, S.N.; Ahmed, M.; Miksad, R.A. Priming of Sorafenib Prior to Radiofrequency Ablation Does Not Increase Treatment Effect in Hepatocellular Carcinoma. Dig. Dis. Sci. 2022, 67, 3455–3463. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.W.; Lee, J.M.; Lee, D.H.; Yoon, J.-H.; Kim, Y.J.; Yu, S.J.; Cho, E.J. Radiofrequency Ablation Using a Separable Clustered Electrode for the Treatment of Hepatocellular Carcinomas: A Randomized Controlled Trial of a Dual-Switching Monopolar Mode Versus a Single-Switching Monopolar Mode. Korean J. Radiol. 2021, 22, 179–188. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.W.; Lee, J.-H.; Lee, D.H.; Yoon, J.-H.; Kim, Y.J.; Yu, S.J.; Cho, E.J. Radiofrequency ablation using internally cooled wet electrodes in bipolar mode for the treatment of recurrent hepatocellular carcinoma after locoregional treatment: A randomized prospective comparative study. PLoS ONE 2020, 15, e0239733. [Google Scholar] [CrossRef] [PubMed]
- Chong, C.C.; Lee, K.F.; Cheung, S.Y.; Chu, C.C.; Fong, A.K.; Wong, J.; Hui, J.W.; Fung, A.K.; Lok, H.T.; Lo, E.Y.; et al. Prospective double-blinded randomized controlled trial of Microwave versus RadioFrequency Ablation for hepatocellular carcinoma (McRFA trial). HPB 2020, 22, 1121–1127. [Google Scholar] [CrossRef]
- Paul, S.; Acharya, S.; Gamanagatti, S.; Sreenivas, V.; Shalimar, S.; Gulati, M. Acetic acid versus radiofrequency ablation for the treatment of hepatocellular carcinoma: A randomized controlled trial. Diagn. Interv. Imaging 2020, 101, 101–110. [Google Scholar] [CrossRef]
- Virmani, S.; Rhee, T.K.; Ryu, R.K.; Sato, K.T.; Lewandowski, R.J.; Mulcahy, M.F.; Kulik, L.M.; Szolc-Kowalska, B.; Woloschak, G.E.; Yang, G.-Y.; et al. Comparison of Hypoxia-inducible Factor-1α Expression before and after Transcatheter Arterial Embolization in Rabbit VX2 Liver Tumors. J. Vasc. Interv. Radiol. 2008, 19, 1483–1489. [Google Scholar] [CrossRef] [Green Version]
- Bzeizi, K.I.; Arabi, M.; Jamshidi, N.; Albenmousa, A.; Sanai, F.M.; Al-Hamoudi, W.; Alghamdi, S.; Broering, D.; Alqahtani, S.A. Conventional Transarterial Chemoembolization Versus Drug-Eluting Beads in Patients with Hepatocellular Carcinoma: A Systematic Review and Meta-Analysis. Cancers 2021, 13, 6172. [Google Scholar] [CrossRef]
- Guan, Y.-S.; He, Q.; Wang, M.-Q. Transcatheter Arterial Chemoembolization: History for More than 30 Years. ISRN Gastroenterol. 2012, 2012, 480650. [Google Scholar] [CrossRef] [Green Version]
- Renzulli, M.; Peta, G.; Vasuri, F.; Marasco, G.; Caretti, D.; Bartalena, L.; Spinelli, D.; Giampalma, E.; D’errico, A.; Golfieri, R. Standardization of conventional chemoembolization for hepatocellular carcinoma. Ann. Hepatol. 2020, 22, 100278. [Google Scholar] [CrossRef]
- Butcher, D.A.; Brandis, K.J.; Wang, H.; Spannenburg, L.; Bridle, K.R.; Crawford, D.H.; Liang, X. Long-term survival and postoperative complications of pre-liver transplantation transarterial chemoembolisation in hepatocellular carcinoma: A systematic review and meta-analysis. Eur. J. Surg. Oncol. 2021, 48, 621–631. [Google Scholar] [CrossRef] [PubMed]
- Liang, L.; Li, C.; Diao, Y.-K.; Jia, H.-D.; Xing, H.; Pawlik, T.M.; Lau, W.Y.; Shen, F.; Huang, D.-S.; Zhang, C.-W.; et al. Survival benefits from adjuvant transcatheter arterial chemoembolization in patients undergoing liver resection for hepatocellular carcinoma: A systematic review and meta-analysis. Ther. Adv. Gastroenterol. 2020, 13, 1756284820977693. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Ma, T.; Zhang, J.; Zhang, X.; Chen, W.; Shen, Y.; Bai, X.; Liang, T. A systematic review and meta-analysis of adjuvant transarterial chemoembolization after curative resection for patients with hepatocellular carcinoma. HPB 2020, 22, 795–808. [Google Scholar] [CrossRef] [PubMed]
- Huo, Y.R.; Chan, M.V.; Chan, C. Resection Plus Post-operative Adjuvant Transcatheter Arterial Chemoembolization (TACE) Compared with Resection Alone for Hepatocellular Carcinoma: A Systematic Review and Meta-analysis. Cardiovasc. Interv. Radiol. 2020, 43, 572–586. [Google Scholar] [CrossRef] [PubMed]
- De Baere, T.; Arai, Y.; Lencioni, R.; Geschwind, J.-F.; Rilling, W.; Salem, R.; Matsui, O.; Soulen, M.C. Treatment of Liver Tumors with Lipiodol TACE: Technical Recommendations from Experts Opinion. Cardiovasc. Interv. Radiol. 2016, 39, 334–343. [Google Scholar] [CrossRef]
- Li, H.; Wu, F.; Duan, M.; Zhang, G. Drug-eluting bead transarterial chemoembolization (TACE) vs conventional TACE in treating hepatocellular carcinoma patients with multiple conventional TACE treatments history. Medicine 2019, 98, e15314. [Google Scholar] [CrossRef]
- Varela, M.; Real, M.I.; Burrel, M.; Forner, A.; Sala, M.; Brunet, M.; Ayuso, C.; Castells, L.; Montañá, X.; Llovet, J.M.; et al. Chemoembolization of hepatocellular carcinoma with drug eluting beads: Efficacy and doxorubicin pharmacokinetics. J. Hepatol. 2007, 46, 474–481. [Google Scholar] [CrossRef]
- Nouri, Y.M.; Kim, J.H.; Yoon, H.-K.; Ko, H.-K.; Shin, J.H.; Gwon, D.I. Update on Transarterial Chemoembolization with Drug-Eluting Microspheres for Hepatocellular Carcinoma. Korean J. Radiol. 2019, 20, 34–49. [Google Scholar] [CrossRef]
- Mishra, G.; Majeed, A.; Dev, A.; Eslick, G.D.; Pinato, D.J.; Izumoto, H.; Hiraoka, A.; Huo, T.-I.; Liu, P.-H.; Johnson, P.J.; et al. Clinical Utility of Albumin Bilirubin Grade as a Prognostic Marker in Patients with Hepatocellular Carcinoma Undergoing Transarterial Chemoembolization: A Systematic Review and Meta-analysis. J. Gastrointest. Cancer 2022, 1–13. [Google Scholar] [CrossRef]
- Zhang, X.; Svn, Z.; Liv, M.; Liu, M.; Zhang, Y.; Sun, Q. Assessment of Prognostic Value of Aspartate Aminotransferase-to-Platelet Ratio Index in Patients with Hepatocellular Carcinoma: Meta-Analysis of 28 Cohort Studies. Front. Med. 2021, 8, 756210. [Google Scholar] [CrossRef]
- Mou, Z.; Guan, T.; Chen, L. Acute Kidney Injury in Adult Patients With Hepatocellular Carcinoma After TACE or Hepatectomy Treatment. Front. Oncol. 2022, 12, 627895. [Google Scholar] [CrossRef] [PubMed]
- Ho, S.-Y.; Liu, P.-H.; Hsu, C.-Y.; Huang, Y.-H.; Liao, J.-I.; Su, C.-W.; Hou, M.-C.; Huo, T.-I. Comparison of Four Albumin-Based Liver Reserve Models (ALBI/EZ-ALBI/PALBI/PAL) against MELD for Patients with Hepatocellular Carcinoma Undergoing Transarterial Chemoembolization. Cancers 2023, 15, 1925. [Google Scholar] [CrossRef] [PubMed]
- Yang, D.S.; Park, S.; Rim, C.H.; Yoon, W.S.; Shin, I.-S.; Lee, H.A. Salvage External Beam Radiotherapy after Incomplete Transarterial Chemoembolization for Hepatocellular Carcinoma: A Meta-Analysis and Systematic Review. Medicina 2021, 57, 1000. [Google Scholar] [CrossRef]
- Shen, A.; Liu, M.; Zheng, D.; Chen, Q.; Wu, Z. Adjuvant transarterial chemoembolization after curative hepatectomy for hepatocellular carcinoma with microvascular invasion: A systematic review and meta-analysis. Clin. Res. Hepatol. Gastroenterol. 2020, 44, 142–154. [Google Scholar] [CrossRef]
- Wang, L.; Ke, Q.; Lin, N.; Huang, Q.; Zeng, Y.; Liu, J. The efficacy of transarterial chemoembolization combined with microwave ablation for unresectable hepatocellular carcinoma: A systematic review and meta-analysis. Int. J. Hyperth. 2019, 36, 1287–1295. [Google Scholar] [CrossRef] [Green Version]
- Drewes, R.; Heinze, C.; Pech, M.; Powerski, M.; Woidacki, K.; Wienke, A.; Surov, A.; Omari, J. Apparent Diffusion Coefficient Can Predict Therapy Response of Hepatocellular Carcinoma to Transcatheter Arterial Chemoembolization. Dig. Dis. 2022, 40, 596–606. [Google Scholar] [CrossRef]
- Liu, Z.; Fan, J.-M.; He, C.; Li, Z.-F.; Xu, Y.-S.; Liu, H.-F.; Lei, J.-Q.; Li, Z. Utility of diffusion weighted imaging with the quantitative apparent diffusion coefficient in diagnosing residual or recurrent hepatocellular carcinoma after transarterial chemoembolization: A meta-analysis. Cancer Imaging 2020, 20, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Hai, Y.; Savsani, E.; Chong, W.; Eisenbrey, J.; Lyshchik, A. Meta-analysis and systematic review of contrast-enhanced ultrasound in evaluating the treatment response after locoregional therapy of hepatocellular carcinoma. Abdom. Imaging 2021, 46, 5162–5179. [Google Scholar] [CrossRef]
- Granito, A.; Facciorusso, A.; Sacco, R.; Bartalena, L.; Mosconi, C.; Cea, U.V.; Cappelli, A.; Antonino, M.; Modestino, F.; Brandi, N.; et al. TRANS-TACE: Prognostic Role of the Transient Hypertransaminasemia after Conventional Chemoembolization for Hepatocellular Carcinoma. J. Pers. Med. 2021, 11, 1041. [Google Scholar] [CrossRef]
- Katsanos, K.; Kitrou, P.; Spiliopoulos, S.; Maroulis, I.; Petsas, T.; Karnabatidis, D. Comparative effectiveness of different transarterial embolization therapies alone or in combination with local ablative or adjuvant systemic treatments for unresectable hepatocellular carcinoma: A network meta-analysis of randomized controlled trials. PLoS ONE 2017, 12, e0184597. [Google Scholar] [CrossRef]
- Yang, B.; Liang, J.; Qu, Z.; Yang, F.; Liao, Z.; Gou, H. Transarterial strategies for the treatment of unresectable hepatocellular carcinoma: A systematic review. PLoS ONE 2020, 15, e0227475. [Google Scholar] [CrossRef] [Green Version]
- Zhang, X.; Luo, Y.; Tsauo, J.; Zhao, H.; Gong, T.; Li, J.; Li, Y.; Zeng, H.; Sun, W.; Li, X. Transradial versus transfemoral access without closure device for transarterial chemoembolization in patients with hepatocellular carcinoma: A randomized trial. Eur. Radiol. 2022, 32, 6812–6819. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.; Chen, Y.; Liao, H.; Gu, Y.; Meng, X.; Dong, W. Operator radiation dose during trans-hepatic arterial chemoembolization: Different patients’ positions via transradial or transfemoral access. Diagn. Interv. Radiol. 2022, 28, 376–382. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.-D.; Li, X.; Ji, J.-S.; Huang, M.; Shao, G.-L.; Lu, J.; Zhao, X.-Y.; Li, H.-L.; Yang, Z.-Q.; Tu, J.-F.; et al. TACE with dicycloplatin in patients with unresectable hepatocellular carcinoma: A multicenter randomized phase II trial. Eur. Radiol. 2022, 32, 7335–7343. [Google Scholar] [CrossRef]
- Dhondt, E.; Lambert, B.; Hermie, L.; Huyck, L.; Vanlangenhove, P.; Geerts, A.; Verhelst, X.; Aerts, M.; Vanlander, A.; Berrevoet, F.; et al. 90Y Radioembolization versus Drug-eluting Bead Chemoembolization for Unresectable Hepatocellular Carcinoma: Results from the TRACE Phase II Randomized Controlled Trial. Radiology 2022, 303, 699–710. [Google Scholar] [CrossRef]
- Llovet, J.M.; Vogel, A.; Madoff, D.C.; Finn, R.S.; Ogasawara, S.; Ren, Z.; Mody, K.; Li, J.J.; Siegel, A.B.; Dubrovsky, L.; et al. Randomized Phase 3 LEAP-012 Study: Transarterial Chemoembolization with or Without Lenvatinib Plus Pembrolizumab for Intermediate-Stage Hepatocellular Carcinoma Not Amenable to Curative Treatment. Cardiovasc. Interv. Radiol. 2022, 45, 405–412. [Google Scholar] [CrossRef]
- Chen, W.-T.; Lin, S.-M.; Lee, W.-C.; Wu, T.-J.; Lin, C.-C.; Shen, C.-H.; Chang, M.-L.; Lin, C.-L.; Yeh, C.-T. GALNT14 genotype-guided chemoembolization plus sorafenib therapy in hepatocellular carcinoma: A randomized trial. Hepatol. Int. 2022, 16, 148–158. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Zhao, Y.; He, L.; Bo, C.; An, Y.; Li, N.; Ma, W.; Guo, Y.; Guo, Y.; Zhang, C. Effect of camrelizumab plus transarterial chemoembolization on massive hepatocellular carcinoma. Clin. Res. Hepatol. Gastroenterol. 2022, 46, 101851. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Wu, J.-L.; Li, L.-Q. Efficacy comparison of optimal treatments for hepatocellular carcinoma patients with portal vein tumor thrombus. Ann. Hepatol. 2021, 27, 100552. [Google Scholar] [CrossRef]
- Aramaki, O.; Takayama, T.; Moriguchi, M.; Sakamoto, H.; Yodono, H.; Kokudo, N.; Yamanaka, N.; Kawasaki, S.; Sasaki, Y.; Kubota, K.; et al. Arterial chemoembolisation with cisplatin versus epirubicin for hepatocellular carcinoma (ACE 500 study): A multicentre, randomised controlled phase 2/3 trial. Eur. J. Cancer 2021, 157, 373–382. [Google Scholar] [CrossRef]
- Fu, J.; Wang, Y.; Zhang, J.; Yuan, K.; Yan, J.; Yuan, B.; Guan, Y.; Wang, M. The safety and efficacy of transarterial chemoembolisation with bleomycin for hepatocellular carcinoma unresponsive to doxorubicin: A prospective single-centre study. Clin. Radiol. 2021, 76, 864.e7–864.e12. [Google Scholar] [CrossRef]
- Ding, X.; Sun, W.; Li, W.; Shen, Y.; Guo, X.; Teng, Y.; Liu, X.; Zheng, L.; Li, W.; Chen, J. Transarterial chemoembolization plus lenvatinib versus transarterial chemoembolization plus sorafenib as first-line treatment for hepatocellular carcinoma with portal vein tumor thrombus: A prospective randomized study. Cancer 2021, 127, 3782–3793. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Feng, Y.; Liu, Y.; Ye, X.; Ji, X.; Sun, L.; Gao, F.; Zhang, Q.; Li, Y.; Zhu, B.; et al. Fuzheng Jiedu Xiaoji formulation inhibits hepatocellular carcinoma progression in patients by targeting the AKT/CyclinD1/p21/p27 pathway. Phytomedicine 2021, 87, 153575. [Google Scholar] [CrossRef] [PubMed]
- Pan, Y.; Chang, R.; He, Z.; Hong, M. How to prophylactically alleviate postembolization syndrome following transarterial chemoembolization? Medicine 2021, 100, e25360. [Google Scholar] [CrossRef]
- Bessar, A.A.; Farag, A.; Monem, S.M.A.; Wadea, F.M.; Shaker, S.E.; Ebada, M.A.; Bessar, M.A. Transarterial chemoembolisation in patients with hepatocellular carcinoma: Low-dose doxorubicin reduces post-embolisation syndrome without affecting survival—Prospective interventional study. Eur. Radiol. Exp. 2021, 5, 1–10. [Google Scholar] [CrossRef]
- Zaitoun, M.M.A.; Elsayed, S.B.; Zaitoun, N.A.; Soliman, R.K.; Elmokadem, A.H.; Farag, A.A.; Amer, M.; Hendi, A.M.; Mahmoud, N.E.M.; El Deen, D.S.; et al. Combined therapy with conventional trans-arterial chemoembolization (cTACE) and microwave ablation (MWA) for hepatocellular carcinoma >3–<5 cm. Int. J. Hyperth. 2021, 38, 248–256. [Google Scholar] [CrossRef]
- Gjoreski, A.; Jovanoska, I.; Risteski, F.; Veljanova, B.P.; Nedelkovski, D.; Dimov, V.; Jovanovska, R.P.; Angelovska, B.G.; Mitrevski, N.; Dimova, B. Single-center randomized trial comparing conventional chemoembolization versus doxorubicin-loaded polyethylene glycol microspheres for early- and intermediate-stage hepatocellular carcinoma. Eur. J. Cancer Prev. 2021, 30, 258–266. [Google Scholar] [CrossRef]
- Guo, J.-H.; Liu, S.-X.; Gao, S.; Kou, F.-X.; Zhang, X.; Wu, D.; Li, X.-T.; Chen, H.; Wang, X.-D.; Liu, P.; et al. Transarterial chemoembolization with hepatic arterial infusion chemotherapy plus S-1 for hepatocellular carcinoma. World J. Gastroenterol. 2020, 26, 3975–3988. [Google Scholar] [CrossRef] [PubMed]
- Turpin, A.; de Baere, T.; Heurgué, A.; Le Malicot, K.; Ollivier-Hourmand, I.; Lecomte, T.; Perrier, H.; Vergniol, J.; Sefrioui, D.; Rinaldi, Y.; et al. Liver transarterial chemoembolization and sunitinib for unresectable hepatocellular carcinoma: Results of the PRODIGE 16 study. Clin. Res. Hepatol. Gastroenterol. 2021, 45, 101464. [Google Scholar] [CrossRef]
- Kudo, M.; Ueshima, K.; Ikeda, M.; Torimura, T.; Tanabe, N.; Aikata, H.; Izumi, N.; Yamasaki, T.; Nojiri, S.; Hino, K.; et al. Randomised, multicentre prospective trial of transarterial chemoembolisation (TACE) plus sorafenib as compared with TACE alone in patients with hepatocellular carcinoma: TACTICS trial. Gut 2020, 69, 1492–1501. [Google Scholar] [CrossRef]
- Sato, K.; Lewandowski, R.J.; Bui, J.T.; Omary, R.; Hunter, R.D.; Kulik, L.; Mulcahy, M.; Liu, D.; Chrisman, H.; Resnick, S.; et al. Treatment of Unresectable Primary and Metastatic Liver Cancer with Yttrium-90 Microspheres (TheraSphere®): Assessment of Hepatic Arterial Embolization. Cardiovasc. Interv. Radiol. 2006, 29, 522–529. [Google Scholar] [CrossRef] [PubMed]
- Murthy, R.; Kamat, P.; Nuñez, R.; Salem, R. Radioembolization of Yttrium-90 Microspheres for Hepatic Malignancy. Semin. Interv. Radiol. 2008, 25, 048–057. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reinders, M.T.M.; van Erpecum, K.J.; Smits, M.L.J.; Braat, A.J.A.T.; de Bruijne, J.; Bruijnen, R.C.; Sprengers, D.; de Man, R.A.; Vegt, E.; Ijzermans, J.N.; et al. Safety and Efficacy of166Ho Radioembolization in Hepatocellular Carcinoma: The HEPAR Primary Study. J. Nucl. Med. 2022, 63, 1891–1898. [Google Scholar] [CrossRef] [PubMed]
- Radosa, C.G.; Radosa, J.C.; Grosche-Schlee, S.; Zöphel, K.; Plodeck, V.; Kühn, J.P.; Kotzerke, J.; Hoffmann, R.-T. Holmium-166 Radioembolization in Hepatocellular Carcinoma: Feasibility and Safety of a New Treatment Option in Clinical Practice. Cardiovasc. Interv. Radiol. 2019, 42, 405–412. [Google Scholar] [CrossRef]
- Bult, W.; Vente, M.A.; Vandermeulen, E.; Gielen, I.; Seevinck, P.R.; Saunders, J.; Schip, A.D.V.H.; Bakker, C.J.; Krijger, G.C.; Peremans, K.; et al. Microbrachytherapy using holmium-166 acetylacetonate microspheres: A pilot study in a spontaneous cancer animal model. Brachytherapy 2013, 12, 171–177. [Google Scholar] [CrossRef]
- Chen, H.; Nan, G.; Wei, D.; Zhai, R.-Y.; Huang, M.; Yang, W.-W.; Xing, B.-C.; Zhu, X.; Xu, H.-F.; Wang, X.-D.; et al. Hepatic Artery Injection of 131I-Metuximab Combined with Transcatheter Arterial Chemoembolization for Unresectable Hepatocellular Carcinoma: A Prospective Nonrandomized, Multicenter Clinical Trial. J. Nucl. Med. 2022, 63, 556–559. [Google Scholar] [CrossRef]
- Riaz, A.; Gates, V.L.; Atassi, B.; Lewandowski, R.J.; Mulcahy, M.F.; Ryu, R.K.; Sato, K.T.; Baker, T.; Kulik, L.; Gupta, R.; et al. Radiation Segmentectomy: A Novel Approach to Increase Safety and Efficacy of Radioembolization. Int. J. Radiat. Oncol. Biol. Phys. 2011, 79, 163–171. [Google Scholar] [CrossRef]
- Salem, R.; Lewandowski, R.J.; Mulcahy, M.F.; Riaz, A.; Ryu, R.K.; Ibrahim, S.; Atassi, B.; Baker, T.; Gates, V.; Miller, F.H.; et al. Radioembolization for Hepatocellular Carcinoma Using Yttrium-90 Microspheres: A Comprehensive Report of Long-term Outcomes. Gastroenterology 2010, 138, 52–64. [Google Scholar] [CrossRef]
- Mazzaferro, V.; Sposito, C.; Bhoori, S.; Romito, R.; Chiesa, C.; Morosi, C.; Maccauro, M.; Marchianò, A.; Bongini, M.; Lanocita, R.; et al. Yttrium-90 radioembolization for intermediate-advanced hepatocellular carcinoma: A phase 2 study. Hepatology 2013, 57, 1826–1837. [Google Scholar] [CrossRef]
- Rognoni, C.; Ciani, O.; Sommariva, S.; Bargellini, I.; Bhoori, S.; Cioni, R.; Facciorusso, A.; Golfieri, R.; Gramenzi, A.; Mazzaferro, V.; et al. Trans-arterial radioembolization for intermediate-advanced hepatocellular carcinoma: A budget impact analysis. BMC Cancer 2018, 18, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Facciorusso, A.; Chierici, A.; Cincione, I.; Sacco, R.; Ramai, D.; Mohan, B.P.; Chandan, S.; Ofosu, A.; Cotsoglou, C. Stereotactic body radiotherapy vs. radiofrequency ablation for the treatment of hepatocellular carcinoma: A meta-analysis. Expert Rev. Anticancer. Ther. 2021, 21, 681–688. [Google Scholar] [CrossRef]
- Salem, R.; Gordon, A.C.; Mouli, S.; Hickey, R.; Kallini, J.; Gabr, A.; Mulcahy, M.F.; Baker, T.; Abecassis, M.; Miller, F.H.; et al. Y90 Radioembolization Significantly Prolongs Time to Progression Compared with Chemoembolization in Patients with Hepatocellular Carcinoma. Gastroenterology 2016, 151, 1155–1163.e2. [Google Scholar] [CrossRef] [Green Version]
- Facciorusso, A.; Serviddio, G.; Muscatiello, N. Transarterial radioembolization vs. chemoembolization for hepatocarcinoma patients: A systematic review and meta-analysis. World J. Hepatol. 2016, 8, 770–778. [Google Scholar] [CrossRef]
- Facciorusso, A.; Paolillo, R.; Tartaglia, N.; Ramai, D.; Mohan, B.P.; Cotsoglou, C.; Chandan, S.; Ambrosi, A.; Bargellini, I.; Renzulli, M.; et al. Efficacy of combined transarterial radioembolization and sorafenib in the treatment of hepatocarcinoma: A meta-analysis. Dig. Liver Dis. 2022, 54, 316–323. [Google Scholar] [CrossRef]
- Chow, P.K.; Gandhi, M.; Tan, S.-B.; Khin, M.W.; Khasbazar, A.; Ong, J.; Choo, S.P.; Cheow, P.C.; Chotipanich, C.; Lim, K.; et al. SIRveNIB: Selective Internal Radiation Therapy Versus Sorafenib in Asia-Pacific Patients with Hepatocellular Carcinoma. J. Clin. Oncol. 2018, 36, 1913–1921. [Google Scholar] [CrossRef]
- Zou, J.; Zhu, W.; Meng, H.; Luo, P.; Zhang, J. Efficacy and safety of selective internal radiotherapy versus sorafenib for intermediate-locally advanced hepatocellular carcinoma: A systematic review and meta-analysis. Expert Rev. Gastroenterol. Hepatol. 2019, 13, 271–279. [Google Scholar] [CrossRef]
- Torok, J.A.; Salama, J.K. Combining immunotherapy and radiotherapy for the STAR treatment. Nat. Rev. Clin. Oncol. 2019, 16, 666–667. [Google Scholar] [CrossRef]
- Braat, M.N.; Van Erpecum, K.J.; Zonnenberg, B.A.; Bosch, M.A.V.D.; Lam, M.G. Radioembolization-induced liver disease. Eur. J. Gastroenterol. Hepatol. 2017, 29, 144–152. [Google Scholar] [CrossRef]
- Riaz, A.; Awais, R.; Salem, R. Side Effects of Yttrium-90 Radioembolization. Front. Oncol. 2014, 4, 198. [Google Scholar] [CrossRef] [Green Version]
- Yi, Y.; Tongguo, S. Yttrium-90 transarterial radioembolization versus conventional transarterial chemoembolization for patients with hepatocellular carcinoma: A systematic review and meta-analysis. Cancer Biol. Med. 2018, 15, 299–310. [Google Scholar] [CrossRef]
- Lemieux, S.; Buies, A.; Turgeon, A.F.; Hallet, J.; Daigle, G.; Côté, F.; Provencher, S. Effect of Yttrium-90 transarterial radioembolization in patients with non-surgical hepatocellular carcinoma: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0247958. [Google Scholar] [CrossRef]
- Roosen, J.; Klaassen, N.J.M.; Gotby, L.E.L.W.; Overduin, C.G.; Verheij, M.; Konijnenberg, M.W.; Nijsen, J.F.W. To 1000 Gy and back again: A systematic review on dose-response evaluation in selective internal radiation therapy for primary and secondary liver cancer. Eur. J. Nucl. Med. 2021, 48, 3776–3790. [Google Scholar] [CrossRef]
- Alonso, J.C.; Casans, I.; González, F.M.; Fuster, D.; Rodríguez, A.; Sánchez, N.; Oyagüez, I.; Burgos, R.; Williams, A.O.; Espinoza, N. Economic evaluations of radioembolization with Itrium-90 microspheres in hepatocellular carcinoma: A systematic review. BMC Gastroenterol. 2022, 22, 1–23. [Google Scholar] [CrossRef]
- Pereira, H.; Bouattour, M.; Burgio, M.D.; Assenat, E.; Grégory, J.; Bronowicki, J.-P.; Chatellier, G.; Vilgrain, V.; Delhom-Christol, E.; Fourcade, M.; et al. Health-related quality of life in locally advanced hepatocellular carcinoma treated by either radioembolisation or sorafenib (SARAH trial). Eur. J. Cancer 2021, 154, 46–56. [Google Scholar] [CrossRef]
- Eisenbrey, J.R.; Forsberg, F.; Wessner, C.E.; Delaney, L.J.; Bradigan, K.; Gummadi, S.; Tantawi, M.; Lyshchik, A.; O’kane, P.; Liu, J.-B.; et al. US-triggered Microbubble Destruction for Augmenting Hepatocellular Carcinoma Response to Transarterial Radioembolization: A Randomized Pilot Clinical Trial. Radiology 2021, 298, 450–457. [Google Scholar] [CrossRef]
| Author, Year, Trial Name | Population | Sample Size | Intervention | Comparison | Outcome |
|---|---|---|---|---|---|
| Hendriks, 2022, HORA EST HCC Trial [59] | HCC patients with a solitary lesion 2–5 cm, or a maximum of 3 lesions of ≤3 cm each | NA | Day 1 post RFA: selective infusion 99mTc-MAA), days 5–10 post RFA: 166Ho-MS administration | 60 Gy, 90 Gy, and 120 Gy of 166Ho-MS | Perfused liver volume; final outcome not yet available |
| Radosevic, 2022 [60] | HCC and patients with metastatic disease with 1.5–4 cm tumours, suitable for ablation | 82 | Ablation: MWA and RFA | Between MWA and RFA in S.L.R., T.S., LTP | After a median 2-year follow-up, MWA vs. RFA: SLR: 0.5 vs. 0.5 p = 0.229 TS: 98% vs. 90% p = 0.108 LTP: 21% vs. 12% p = 0.238 |
| Suh, 2021 [61] | Eligible patients for RFA with H.C.C. | 73 | RFA: conventional or no NT-RFA using twin internally cooled wet electrodes in the bipolar mode | Between NT-RFA and RFA groups in LTP rates | The 1 and 3 year cumulative LTP rates were 5.6% in the NT-RFA group, and they were 11.8% and 21.3%, respectively, in the conventional RFA group (p = 0.073, log-rank) |
| Bockonry, 2022 [62] | For HCC tumours sized 3.5–7 cm | 20 | Priming with 400 mg sorafenib BD for 10 days prior to RFA or placebo | Priming versus placebo in volume and diameter of the RFA coagulation zone | No increase in ablation volume/diameter; decreased blood perfusion to the tumour by 27.9% (p = 0.01) |
| Kim, 2021 [63] | ≤2 recurrent H.C.C. of <3 cm | 144 | PBT or RFA | PBT vs. RFA in LPFS | PBT showed LPFS values that were noninferior to those for RFA |
| Choi, 2020 [64] | Recurrent HCC after locoregional treatment | 77 | RFA: TICW, bipolar, using twin internally cooled wet electrodes or SC: switching monopolar RFA, using separable clustered electrodes | TICW-RFA vs. SC-RFA in minimum diameter of the ablation zone per unit ablation time | No significant Difference |
| Choi, 2021 [63] | HCC | 80 | RFA; DSM: dual-switching monopolar; SSM conventional single-switching monopolar | DSM-RFA vs. SSM-RFA in minimum diameter of the ablation zone per unit ablation time | No significant Difference |
| Chong, 2020, McRFA trial [65] | HCC suitable for local ablation | 93 | Ablation: MWA and RFA | MWA vs. RFA in treatment-related morbidity, as well as overall and disease-free survival | No significant difference in the treatment-related morbidity or overall and disease-free survival; MWA had a significantly shorter overall ablation time when compared with RFA (12 min vs. 24 min, p < 0.001) |
| Paul, 2020 [66] | HCC < 5 cm | 55 | PAAI, RFA | PAAI vs. RFA in tumour response and survival rate | Similar efficacy |
| Author, Year, Trial Name | Population | Sample Size | Intervention | Comparison | Outcome |
|---|---|---|---|---|---|
| Zhang, 2022 [92] | TACE for HCC | 130 | Femoral or radial approach (radial without the closure device) | Technical success rate, crossover rate, contrast agent dose, fluoroscopy/procedure time, air kerma, dose–area product, length of hospital stay, total cost, incidence and severity of adverse events, overall discomfort, general health, physical/social/emotional function, and mental health | TRA instead of TFA can improve patient satisfaction without compromising procedural variables and safety |
| Jiang, 2022 [93] | TACE for HCC | 120 | Femoral or radial approach with foot or head-first position | Radiation dose at 7 anatomical sites of the operator | TACE via the left TRA, with patients in the feet-first position, reduced the radiation dose received by the operator |
| Zhu, 2022 [94] | TACE for unresectable HCC | 72 | TACE with a distinct chemotherapeutic regimen | A chemotherapeutic regimen of dicycloplatin alone (group A1), dicycloplatin plus epirubicin (group A2), or epirubicin alone (group B) | TACE with dicycloplatin alone or plus epirubicin was comparably safe and well tolerable as epirubicin alone; significant improvements in ORR and DCR when dicycloplatin was applied, and prolonged PFS when dicycloplatin plus epirubicin was applied compared with epirubicin alone |
| Dhondt, 2022 [95] | Intermediate-stage unresectable HCC with ECOG 1 or early-stage HCC not eligible for surgery or thermoablation | 72 | 90Y glass TARE was compared with doxorubicin DEB-TACE | Time to overall tumour progression | 90Y glass TARE superior tumour control and survival compared with doxorubicin DEB-TACE |
| Llovet, 2022, LEAP-012 [96] | HCC localised to the liver without portal vein thrombosis and not amenable to curative treatment, ≥1 measurable tumour per Response Evaluation Criteria in Solid Tumours 1.1 (RECIST 1.1), ECOG 0 or 1, Child–Pugh class A, and no previous systemic treatment for HCC | 950 | Lenvatinib once daily plus pembrolizumab every 6 weeks plus TACE or placebos plus TACE | PFS, objective response rate, disease control rate, response duration and progression time, and safety | Study ongoing |
| Chen, 2022, GALNT14 [97] | Intermediate-stage HCC patients | 84 | GALNT14-rs9679162 genotyping before TACE and division into (1) “TT” genotype receiving TACE, (2) “non-TT” genotype (“GG” or “GT”) randomised into TACE or TACE + sorafenib groups | Time to complete response, time to TACE progression, PFS, and OS | Sorafenib + TACE for “non-TT” partially overcame the genetic disadvantage on treatment outcomes in terms of time to complete response, time to TACE progression, and progression-free survival |
| Zhang, 2022 [98] | Massive HCC | 92 | TACE or TACE + camrelizumab | Clinical efficacy, adverse events, liver function, and AFP, CEA, and CA19-9 levels before and after treatment | Camrelizumab + TACE can significantly improve liver function and enhance the treatment effect |
| Zhang, 2022 [99] | HCC with PVTT | 627 | TACE or liver resection or sorafenib | OS | Liver resection optimal for type I and II PVTT, TACE optimal for type III PVTT, and sorafenib optimal for type IV PVTT |
| Aramaki, 2021, ACE 500 [100] | Liver-confined HCC, ECOG 0–2, and Child–Pugh class A/B | 455 | TACE with cisplatin vs. TACE with epirubicin | OS | Cisplatin is not significantly superior to epirubicin in TACE for patients with HCC |
| Fu, 2021 [101] | HCC patients resistant to TACE with doxorubicin | 170 | TACE with doxorubicin vs. TACE with bleomycin | Objective response rate and post-procedure complications | Bleomycin can be a safe and effective second-line chemotherapeutic agent for HCC patients unresponsive to TACE with doxorubicin |
| Ding, 2021 [102] | HCC with PVTT | 64 | TACE with lenvatinib vs. TACE with sorafenib | Time to progression, objective response rate, and toxicity | TACE plus lenvatinib was safe and well tolerated, and had favourable efficacy versus TACE plus sorafenib in patients with advanced HCC with PVTT and large tumour burden |
| Yang, 2021 [103] | HCC | 291 | TACE with or without FZJDXJ | 1 year OS and PFS | FZJDXJ combined with TACE therapy significantly prolonged OS and PFS and reduced the mortality rate of HCC patient |
| Pan, 2021 [104] | HCC | 50 | Post-TACE: placebo vs. Chaihu Guizhi decoction | Incidence of PES | study ongoing |
| Bessar, 2021 [105] | HCC | 28 | TACE with doxorubicin: 50 mg vs. 100 mg | Incidence of PES, free time to PES, changes in laboratory results, tumour response at 1, 3, and 6 months after TACE, and OS | 50 mg doxorubicin was associated with fewer PES without effects on tumour response or OS |
| Zaitoun, 2021 [106] | HCC >3–<5 cm | 265 | TACE vs. MWA vs. TACE+MWA | Treatment response, adverse events, and AFP | TACE + MWA is safe, well-tolerated, and more effective than TACE or MWA alone for the treatment of HCC >3–<5 cm |
| Gjoreski, 2021 [107] | Unresectable HCC | 60 | TACE vs. DEM-TACE | 12 and 24 month OS, | No significant difference in overall OS, or adverse events; TACE was associated with more severe PES and DEM-TACE with a shorter in-hospital stay |
| Guo, 2020 [108] | Advanced HCC | 117 | TACE + HAIC + oral S1 vs. TACE + HAIC | PFS, OS, objective response rate, disease control rate, and safety | No improvements in tumour response rates, PFS, OS, or adverse events were observed with the addition of S-1 to TACE/HAIC in advanced HCC |
| Turpin, 2020, PRODIGE 16 [109] | Unresectable HCC | 78 | Doxorubicin-TACE + sunitinib vs. doxorubicin-TACE + placebo | Bleeding or liver failure | TACE plus sunitinib in the first-line therapy for patients with HCC not suitable for surgical resection was feasible |
| Kudo, 2020, TACTICS [110] | unresectable HCC | 156 | TACE + placebo vs. TACE + sofafenib | PFS, OS, time to untreatable progression, transient deterioration to Child–Pugh C, and appearance of vascular invasion/extrahepatic spread | TACE plus sorafenib significantly improved PFS |
| Author, Year, Trial Name | Population | Sample Size | Intervention | Comparison | Outcome |
|---|---|---|---|---|---|
| Hendriks, 2022, HORA EST HCC Trial [59] * | HCC patients with a solitary lesion 2–5 cm, or a maximum of 3 lesions of ≤3 cm each | NA | Day 1 post RFA: selective infusion 99mTc-MAA), day 5–10 post RFA: 166Ho-MS administration | 60 Gy, 90 Gy and 120 Gy of 166Ho-MS | Perfused liver volume; final outcome not yet available |
| Dhondt, 2022 [95] ** | Intermediate-stage unresectable HCC with ECOG 1 or early-stage HCC not eligible for surgery or thermoablation | 72 | 90Y glass TARE was compared with doxorubicin DEB TACE | Time to overall tumour progression | 90Y glass TARE superior tumour control and survival compared with doxorubicin DEB TACE |
| Pereira, 2021, SARAH [134] | Locally advanced or inoperable HCC | 285 | TARE vs. sorafenib | HRQoL | HRQoL was preserved longer with TARE than with sorafenib |
| Eisenbrey, 2021 [135] | HCC | 28 | TARE vs. TARE with ultrasound-triggered microbubble destruction | Safety and preliminary efficacy | Microbubbles have an excellent safety profile in this patient population and appear to result in improved hepatocellular carcinoma treatment response |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Podlasek, A.; Abdulla, M.; Broering, D.; Bzeizi, K. Recent Advances in Locoregional Therapy of Hepatocellular Carcinoma. Cancers 2023, 15, 3347. https://doi.org/10.3390/cancers15133347
Podlasek A, Abdulla M, Broering D, Bzeizi K. Recent Advances in Locoregional Therapy of Hepatocellular Carcinoma. Cancers. 2023; 15(13):3347. https://doi.org/10.3390/cancers15133347
Chicago/Turabian StylePodlasek, Anna, Maheeba Abdulla, Dieter Broering, and Khalid Bzeizi. 2023. "Recent Advances in Locoregional Therapy of Hepatocellular Carcinoma" Cancers 15, no. 13: 3347. https://doi.org/10.3390/cancers15133347
APA StylePodlasek, A., Abdulla, M., Broering, D., & Bzeizi, K. (2023). Recent Advances in Locoregional Therapy of Hepatocellular Carcinoma. Cancers, 15(13), 3347. https://doi.org/10.3390/cancers15133347






