Challenges and Prospects of Patient-Derived Xenografts for Cancer Research
Abstract
:Simple Summary
Abstract
1. Introduction
2. Overview of PDXs
2.1. PDX as the Standard in vivo Model for Cancer Research
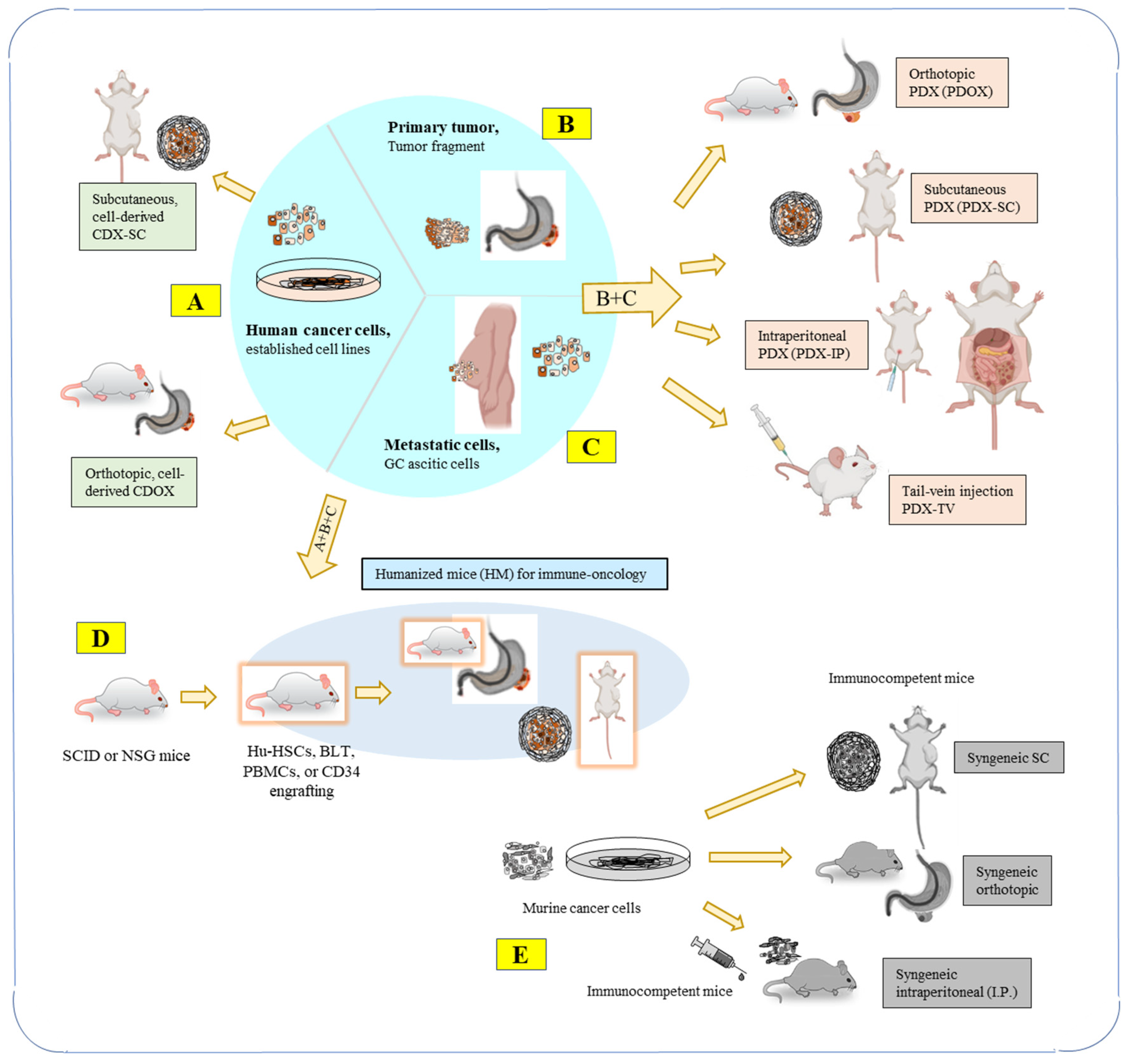
2.2. Types of PDX Models
2.3. Mouse Host Types for PDX Model
2.4. Orthotopic PDX Models (PDOXs) as an Emerging Trend
3. Challenges of the PDX Models
3.1. Heterogeneity Loss, Selection Bias, Clonal Evolution of Tumors and Stroma Replacement
3.2. The Lack of Immune Cells and Low Tumor Take Rate
3.3. Human and Host Viral Infections in PDXs
3.4. Human-to-Host Oncogenic Transformation and Murine Contamination
3.5. Murine Contamination and Host Carryover in Cell Lines and PDX Tumors
3.6. Tumor Microenvironment (TME) within PDXs
4. Prospects and Overcoming limitation of PDXs
4.1. Organoids or 3D Culture
4.2. Immunity and Humanized Mouse (HM) Models
4.3. Syngeneic Mouse Model
4.4. Detection and Quantification of Host Contamination in PDX Tumors and Cell Lines
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Mirabelli, P.; Coppola, L.; Salvatore, M. Cancer Cell Lines Are Useful Model Systems for Medical Research. Cancers 2019, 11, 1098. [Google Scholar] [CrossRef]
- Lee, M.W.; Miljanic, M.; Triplett, T.; Ramirez, C.; Aung, K.L.; Eckhardt, S.G.; Capasso, A. Current methods in translational cancer research. Cancer Metastasis Rev. 2021, 40, 7–30. [Google Scholar] [PubMed]
- Byrne, A.T.; Alférez, D.G.; Amant, F.; Annibali, D.; Arribas, J.; Biankin, A.V.; Bruna, A.; Budinská, E.; Caldas, C.; Chang, D.K.; et al. Interrogating open issues in cancer precision medicine with patient-derived xenografts. Nat. Rev. Cancer 2017, 17, 254–268. [Google Scholar] [CrossRef]
- Hidalgo, M.; Amant, F.; Biankin, A.V.; Budinská, E.; Byrne, A.T.; Caldas, C.; Clarke, R.B.; de Jong, S.; Jonkers, J.; Mælandsmo, C.M.; et al. Patient-derived xenograft models: An emerging platform for translational cancer research. Cancer Discov. 2014, 4, 998–1013. [Google Scholar] [CrossRef] [PubMed]
- Perova, Z.; Martinez, M.; Mandloi, T.; Gomez, F.L.; Halmagyi, C.; Follette, A.; Mason, J.; Newhauser, S.; Begley, D.A.; Krupke, D.M.; et al. PDCM Finder: An open global research platform for patient-derived cancer models. Nucleic Acids Res. 2023, 51, D1360–D1366. [Google Scholar] [CrossRef] [PubMed]
- Jin, J.; Xu, Y.; Huo, L.; Ma, L.; Scott, A.W.; Pizzi, M.P.; Li, Y.; Wang, Y.; Yao, X.; Song, S.; et al. An improved strategy for CRISPR/Cas9 gene knockout and subsequent wildtype and mutant gene rescue. PLoS ONE 2020, 15, e0228910. [Google Scholar] [CrossRef] [PubMed]
- Tian, H.; Lyu, Y.; Yang, Y.-G.; Hu, Z. Humanized Rodent Models for Cancer Research. Front. Oncol. 2020, 10, 1696. [Google Scholar] [CrossRef]
- Yoshida, G.J. Applications of patient-derived tumor xenograft models and tumor organoids. J. Hematol. Oncol. 2020, 13, 4. [Google Scholar] [CrossRef]
- Rivera, M.; Fichtner, I.; Wulf-Goldenberg, A.; Sers, C.; Merk, J.; Patone, G.; Alp, K.M.; Kanashova, T.; Mertins, P.; Hoffmann, J.; et al. Patient-derived xenograft (PDX) models of colorectal carcinoma (CRC) as a platform for chemosensitivity and biomarker analysis in personalized medicine. Neoplasia 2021, 23, 21–35. [Google Scholar] [CrossRef]
- Shi, J.; Li, Y.; Jia, R.; Fan, X. The fidelity of cancer cells in PDX models: Characteristics, mechanism and clinical significance. Int. J. Cancer 2020, 146, 2078–2088. [Google Scholar] [CrossRef]
- Yu, J.; Qin, B.; Moyer, A.M.; Sinnwell, J.P.; Thompson, K.J.; Copland, J.A.; Marlow, L.A.; Miller, J.M.; Yin, P.; Gao, B.; et al. Establishing and characterizing patient- derived xenografts using pre-chemotherapy percutaneous biopsy and post-chemotherapy surgical samples from a prospective neoadjuvant breast cancer study. Breast Cancer Res. 2017, 19, 130. [Google Scholar] [CrossRef] [PubMed]
- Hylander, B.L.; Punt, N.; Tang, H.; Hillman, J.; Vaughan, M.; Bshara, W.; Pitoniak, R.; Repasky, A.E. Origin of the vasculature supporting growth of primary patient tumor xenografts. J. Transl. Med. 2013, 11, 110. [Google Scholar] [CrossRef]
- Kopetz, S.; Lemos, R.; Powis, G. The promise of patient-derived xenografts: The best laid plans of mice and men. Clin. Cancer Res. 2012, 18, 5160–5162. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.-Y.; Kang, W.; Han, J.Y.; Min, S.; Kang, J.; Lee, A.; Kwon, J.Y.; Lee, C.; Park, H. An Integrative Approach to Precision Cancer Medicine Using Patient-Derived Xenografts. Mol. Cells 2016, 39, 77–86. [Google Scholar]
- Murayama, T.; Gotoh, N. Patient-Derived Xenograft Models of Breast Cancer and Their Application. Cells 2019, 8, 621. [Google Scholar] [CrossRef] [PubMed]
- Pan, B.; Wei, X.; Xu, X. Patient-derived xenograft models in hepatopancreatobiliary cancer. Cancer Cell Int. 2022, 22, 41. [Google Scholar] [CrossRef]
- Abdolahi, S.; Ghazvinian, Z.; Muhammadnejad, S.; Saleh, M.; Aghdaei, H.A.; Baghaei, K. Patient-derived xenograft (PDX) models, applications and challenges in cancer research. J. Transl. Med. 2022, 20, 206. [Google Scholar] [CrossRef]
- Shultz, L.D.; Ishikawa, F.; Greiner, D.L. Humanized mice in translational biomedical research. Nat. Rev. Immunol. 2007, 7, 118–130. [Google Scholar] [CrossRef]
- Pauli, C.; Hopkins, B.D.; Prandi, D.; Shaw, R.; Fedrizzi, T.; Sboner, A.; Sailer, V.; Augello, M.; Puca, L.; Rosati, R.; et al. Personalized In Vitro and In Vivo Cancer Models to Guide Precision Medicine. Cancer Discov. 2017, 7, 462–477. [Google Scholar] [CrossRef]
- Ben-David, U.; Ha, G.; Tseng, Y.Y.; Greenwald, N.F.; Oh, C.; Shih, J.; McFarland, J.M.; Wong, B.; Boehm, J.S.; Beroukhim, R.; et al. Patient-derived xenografts undergo mouse-specific tumor evolution. Nat. Genet. 2017, 49, 1567–1575. [Google Scholar] [CrossRef]
- Cassidy, J.W.; Caldas, C.; Bruna, A. Maintaining Tumor Heterogeneity in Patient-Derived Tumor Xenografts. Cancer Res. 2015, 75, 2963–2968. [Google Scholar] [CrossRef]
- Sprouffske, K.; Kerr, G.; Li, C.; Prahallad, A.; Rebmann, R.; Waehle, V.; Naumann, U.; Bitter, H.; Jensen, M.R.; Hofmann, F.; et al. Genetic heterogeneity and clonal evolution during metastasis in breast cancer patient-derived tumor xenograft models. Comput. Struct. Biotechnol. J. 2020, 18, 323–331. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Lin, W.; Huang, Y.; Chen, X.; Wang, H.; Teng, L. The Essential Factors of Establishing Patient-derived Tumor Model. J. Cancer 2021, 12, 28–37. [Google Scholar] [CrossRef] [PubMed]
- Gock, M.; Kühn, F.; Mullins, C.S.; Krohn, M.; Prall, F.; Klar, E.; Linnebacher, M. Tumor Take Rate Optimization for Colorectal Carcinoma Patient-Derived Xenograft Models. BioMed Res. Int. 2016, 2016, 1715053. [Google Scholar] [CrossRef] [PubMed]
- Blomme, A.; Van Simaeys, G.; Doumont, G.; Costanza, B.; Bellier, J.; Otaka, Y.; Sherer, F.; Lovinfosse, P.; Boutry, S.; Palacios, A.P.; et al. Murine stroma adopts a human-like metabolic phenotype in the PDX model of colorectal cancer and liver metastases. Oncogene 2018, 37, 1237–1250. [Google Scholar] [CrossRef]
- Yuan, Z.; Fan, X.; Zhu, J.J.; Fu, T.M.; Wu, J.; Xu, H.; Zhang, N.; An, Z.; Zheng, W.J. Presence of complete murine viral genome sequences in patient-derived xenografts. Nat. Commun. 2021, 12, 2031. [Google Scholar] [CrossRef]
- Bock, S.; Mullins, C.S.; Klar, E.; Pérot, P.; Maletzki, C.; Linnebacher, M. Murine Endogenous Retroviruses Are Detectable in Patient-Derived Xenografts but Not in Patient-Individual Cell Lines of Human Colorectal Cancer. Front. Microbiol. 2018, 9, 789. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Liu, Z.; Zeng, B.; Hu, G.; Gan, R. Epstein-Barr virus-associated gastric cancer: A distinct subtype. Cancer Lett. 2020, 495, 191–199. [Google Scholar] [CrossRef]
- Zhang, L.; Liu, Y.; Wang, X.; Tang, Z.; Li, S.; Hu, Y.; Zong, X.; Wu, X.; Bu, Z.; Wu, A.; et al. The extent of inflammatory infiltration in primary cancer tissues is associated with lymphomagenesis in immunodeficient mice. Sci. Rep. 2015, 5, 9447. [Google Scholar] [CrossRef]
- Sausen, D.G.; Basith, A.; Muqeemuddin, S. EBV and Lymphomagenesis. Cancers 2023, 15, 2133. [Google Scholar] [CrossRef]
- Jin, J.; Huo, L.; Fan, Y.; Wang, R.; Scott, A.W.; Pizzi, M.P.; Yao, X.; Shao, S.; Ma, L.; Da Silva, M.S.; et al. A new intronic quantitative PCR method led to the discovery of transformation from human ascites to murine malignancy in a mouse model. Front. Oncol. 2023, 13, 1062424. [Google Scholar] [CrossRef]
- Multani, A.S.; Ozen, M.; Agrawal, A.; Hopwood, V.L.; von Eschenbach, A.C.; Pathak, S. Amplification of the Y chromosome in three murine tumor cell lines transformed in vivo by different human prostate cancers. In Vitro Cell Dev. Biol. Anim. 1999, 35, 236–239. [Google Scholar] [CrossRef]
- Ozen, M.; Multani, A.S.; Kuniyasu, H.; Chung, L.W.; Von Eschenbach, A.C.; Pathak, S. Specific histologic and cytogenetic evidence for in vivo malignant transformation of murine host cells by three human prostate cancer cell lines. Oncol. Res. 1997, 9, 433–438. [Google Scholar]
- Pathak, S.; Nemeth, M.A.; Multani, A.S.; Thalmann, G.N.; von Eschenbach, A.C.; Chung, L.W. Can cancer cells transform normal host cells into malignant cells? Br. J. Cancer 1997, 76, 1134–1138. [Google Scholar] [CrossRef]
- Goldenberg, D.M. Horizontal transmission of malignancy by cell-cell fusion. Expert Opin. Biol. Ther. 2012, 12 (Suppl. S1), S133–S139. [Google Scholar] [CrossRef]
- Goldenberg, D.M.; Gold, D.V.; Loo, M.; Liu, D.; Chang, C.-H.; Jaffe, E.S. Horizontal transmission of malignancy: In-vivo fusion of human lymphomas with hamster stroma produces tumors retaining human genes and lymphoid pathology. PLoS ONE 2013, 8, e55324. [Google Scholar] [CrossRef]
- Goldenberg, D.M.; Rooney, R.J.; Loo, M.; Liu, D.; Chang, C.-H. In-vivo fusion of human cancer and hamster stromal cells permanently transduces and transcribes human DNA. PLoS ONE 2014, 9, e107927. [Google Scholar] [CrossRef]
- García-Olmo, D.C.; Picazo, M.G.; García-Olmo, D. Transformation of non-tumor host cells during tumor progression: Theories and evidence. Expert Opin. Biol. Ther. 2012, 12 (Suppl. S1), S199–S207. [Google Scholar] [CrossRef]
- Weiler, J.; Dittmar, T. Cell Fusion in Human Cancer: The Dark Matter Hypothesis. Cells 2019, 8, 132. [Google Scholar] [CrossRef]
- Fu, H.; Yang, H.; Zhang, X.; Xu, W. The emerging roles of exosomes in tumor-stroma interaction. J. Cancer Res. Clin. Oncol. 2016, 142, 1897–1907. [Google Scholar] [CrossRef]
- Malkin, E.Z.; Bratman, S.V. Bioactive DNA from extracellular vesicles and particles. Cell Death Dis. 2020, 11, 584. [Google Scholar] [CrossRef]
- Sansone, P.; Berishaj, M.; Rajasekhar, V.K.; Ceccarelli, C.; Chang, Q.; Strillacci, A.; Savini, C.; Shapiro, L.; Bowman, R.L.; Mastroleo, C.; et al. Evolution of Cancer Stem-like Cells in Endocrine-Resistant Metastatic Breast Cancers Is Mediated by Stromal Microvesicles. Cancer Res. 2017, 77, 1927–1941. [Google Scholar] [CrossRef] [PubMed]
- Abdouh, M.; Zhou, S.; Arena, V.; Arena, M.; Lazaris, A.; Onerheim, R.; Metrakos, P.; Arena, G.O. Transfer of malignant trait to immortalized human cells following exposure to human cancer serum. J. Exp. Clin. Cancer Res. 2014, 33, 86. [Google Scholar] [CrossRef] [PubMed]
- Baugh, E.H.; Ke, H.; Levine, A.J.; Bonneau, R.A.; Chan, C.S. Why are there hotspot mutations in the TP53 gene in human cancers? Cell Death Differ. 2018, 25, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Eldar, A.; Rozenberg, H.; Diskin-Posner, Y.; Rohs, R.; Shakked, Z. Structural studies of p53 inactivation by DNA-contact mutations and its rescue by suppressor mutations via alternative protein–DNA interactions. Nucleic Acids Res. 2013, 41, 8748–8759. [Google Scholar] [CrossRef]
- Schneeberger, V.E.; Allaj, V.; Gardner, E.E.; Poirier, J.T.; Rudin, C.M. Quantitation of Murine Stroma and Selective Purification of the Human Tumor Component of Patient-Derived Xenografts for Genomic Analysis. PLoS ONE 2016, 11, e0160587. [Google Scholar] [CrossRef] [PubMed]
- Williams, A.P.; Stewart, J.E.; Stafman, L.L.; Aye, J.M.; Mroczek-Musulman, E.; Ren, C.; Yoon, K.; Whelan, K.; Beierle, E.A. Corruption of neuroblastoma patient derived xenografts with human T cell lymphoma. J. Pediatr. Surg. 2019, 54, 2117–2119. [Google Scholar] [CrossRef] [PubMed]
- El-Hoss, J.; Jing, D.; Evans, K.; Toscan, C.; Xie, J.; Lee, H.; Taylor, R.A.; Lawrence, M.G.; Risbridger, G.P.; MacKenzie, K.L.; et al. A single nucleotide polymorphism genotyping platform for the authentication of patient derived xenografts. Oncotarget 2016, 7, 60475–60490. [Google Scholar] [CrossRef]
- Chen, X.; Qian, W.; Song, Z.; Li, Q.-X.; Guo, S. Authentication, characterization and contamination detection of cell lines, xenografts and organoids by barcode deep NGS sequencing. NAR Genom. Bioinform. 2020, 2, lqaa060. [Google Scholar] [CrossRef]
- Dai, W.; Liu, J.; Li, Q.; Liu, W.; Li, Y.-X.; Li, Y.-Y. A comparison of next-generation sequencing analysis methods for cancer xenograft samples. J. Genet. Genom. 2018, 45, 345–350. [Google Scholar] [CrossRef]
- Khandelwal, G.; Girotti, M.R.; Smowton, C.; Taylor, S.; Wirth, C.; Dynowski, M.; Frese, K.K.; Brady, G.; Dive, C.; Marais, R.; et al. Next-Generation Sequencing Analysis and Algorithms for PDX and CDX Models. Mol. Cancer Res. 2017, 15, 1012–1016. [Google Scholar] [CrossRef] [PubMed]
- Shah, P.K.; Herrera-Loeza, S.G.; Sims, C.E.; Yeh, J.J.; Allbritton, N.L. Small sample sorting of primary adherent cells by automated micropallet imaging and release. Cytom. A 2014, 85, 642–649. [Google Scholar] [CrossRef] [PubMed]
- Valkenburg, K.C.; de Groot, A.E.; Pienta, K.J. Targeting the tumour stroma to improve cancer therapy. Nat. Rev. Clin. Oncol. 2018, 15, 366–381. [Google Scholar] [CrossRef]
- Zheng, P.; Li, W. Crosstalk Between Mesenchymal Stromal Cells and Tumor-Associated Macrophages in Gastric Cancer. Front. Oncol. 2020, 10, 571516. [Google Scholar] [CrossRef] [PubMed]
- Linxweiler, J.; Hajili, T.; Körbel, C.; Berchem, C.; Zeuschner, P.; Müller, A.; Stöckle, M.; Menger, M.D.; Junker, K.; Saar, M. Cancer-associated fibroblasts stimulate primary tumor growth and metastatic spread in an orthotopic prostate cancer xenograft model. Sci. Rep. 2020, 10, 12575. [Google Scholar] [CrossRef]
- Stamatopoulos, A.; Stamatopoulos, T.; Gamie, Z.; Kenanidis, E.; Ribeiro, R.D.C.; Rankin, K.S.; Gerrand, C.; Dalgarno, K.; Tsiridis, E. Mesenchymal stromal cells for bone sarcoma treatment: Roadmap to clinical practice. J. Bone Oncol. 2019, 16, 100231. [Google Scholar] [CrossRef]
- Zervantonakis, I.K.; Poskus, M.D.; Scott, A.L.; Selfors, L.M.; Lin, J.-R.; Dillon, D.A.; Pathania, S.; Sorger, P.K.; Mills, G.B.; Brugge, J.S. Fibroblast-tumor cell signaling limits HER2 kinase therapy response via activation of MTOR and antiapoptotic pathways. Proc. Natl. Acad. Sci. USA 2020, 117, 16500–16508. [Google Scholar] [CrossRef] [PubMed]
- Heinrich, M.A.; Mostafa, A.; Morton, J.P.; Hawinkels, L.; Prakash, J. Translating complexity and heterogeneity of pancreatic tumor: 3D in vitro to in vivo models. Adv. Drug Deliv. Rev. 2021, 174, 265–293. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Qin, T.; Huang, Y.; Li, Y.; Chen, G.; Sun, C. Drug screening model meets cancer organoid technology. Transl. Oncol. 2020, 13, 100840. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Gao, X.; Ni, C.; Zhao, B.; Cheng, X. The application of patient-derived organoid in the research of lung cancer. Cell Oncol. 2023, 46, 503–519. [Google Scholar] [CrossRef]
- Sen, C.; Koloff, C.; Kundu, S.; Wilkinson, D.C.; Yang, J.; Shia, D.W.; Meneses, L.K.; Rickabaugh, T.M.; Gomperts, B.N. Small cell lung cancer co-culture organoids provide insights into cancer cell survival after chemotherapy. bioRxiv 2023. [Google Scholar] [CrossRef]
- Cao, C.; Lu, X.; Guo, X.; Zhao, H.; Gao, Y. Patient-derived models: Promising tools for accelerating the clinical translation of breast cancer research findings. Exp. Cell Res. 2023, 425, 113538. [Google Scholar] [CrossRef]
- Qu, J.; Kalyani, F.S.; Liu, L.; Cheng, T.; Chen, L. Tumor organoids: Synergistic applications, current challenges, and future prospects in cancer therapy. Cancer Commun. 2021, 41, 1331–1353. [Google Scholar] [CrossRef]
- Vivarelli, S.; Candido, S.; Caruso, G.; Falzone, L.; Libra, M. Patient-Derived Tumor Organoids for Drug Repositioning in Cancer Care: A Promising Approach in the Era of Tailored Treatment. Cancers 2020, 12, 3636. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Choung, S.; Sun, R.X.; Ung, N.; Hashemi, N.; Fong, E.J.; Lau, R.; Spiller, E.; Gasho, J.; Foo, J.; et al. Comparison of Cell and Organoid-Level Analysis of Patient-Derived 3D Organoids to Evaluate Tumor Cell Growth Dynamics and Drug Response. SLAS Discov. 2020, 25, 744–754. [Google Scholar] [CrossRef]
- Cho, Y.; Min, D.; Kim, H.; An, Y.; Kim, S.; Youk, J.; Chun, J.; Im, J.P.; Song, S.; Ju, Y.S.; et al. Patient-derived organoids as a preclinical platform for precision medicine in colorectal cancer. Mol. Oncol. 2021, 16, 2396–2412. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Wang, Y.; Guan, A.; Xue, J.; Li, B.; Huang, Z.; Zheng, Z.; Liang, N.; Yang, Y.; Li, S.; et al. Footprints: Stamping hallmarks of lung cancer with patient-derived models, from molecular mechanisms to clinical translation. Front. Bioeng. Biotechnol. 2023, 11, 1132940. [Google Scholar] [CrossRef] [PubMed]
- Morton, J.J.; Alzofon, N.; Jimeno, A. The humanized mouse: Emerging translational potential. Mol. Carcinog. 2020, 59, 830–838. [Google Scholar] [CrossRef] [PubMed]
- Witt, K.; Lundqvist, A. Evaluation of Breast Cancer and Melanoma Metastasis in Syngeneic Mouse Models. Methods Mol. Biol. 2019, 1913, 197–206. [Google Scholar] [PubMed]
- Huang, T.; Yang, J.; Liu, B.; Fu, L. A new mouse esophageal cancer cell line (mEC25)-derived pre-clinical syngeneic tumor model for immunotherapy. Cancer Commun. 2020, 40, 316–320. [Google Scholar] [CrossRef] [PubMed]
- Khalsa, J.K.; Shah, K. Immune Profiling of Syngeneic Murine and Patient GBMs for Effective Translation of Immunotherapies. Cells 2021, 10, 491. [Google Scholar] [CrossRef] [PubMed]
- Sato, K.; Baiocchi, L.; Kennedy, L.; Zhang, W.; Ekser, B.; Glaser, S.; Francis, H.; Alpini, G. Current Advances in Basic and Translational Research of Cholangiocarcinoma. Cancers 2021, 13, 3307. [Google Scholar] [CrossRef] [PubMed]
- Zhong, W.; Myers, J.S.; Wang, F.; Wang, K.; Lucas, J.; Rosfjord, E.; Lucas, J.; Hooper, A.T.; Yang, S.; Lemon, L.A.; et al. Comparison of the molecular and cellular phenotypes of common mouse syngeneic models with human tumors. BMC Genom. 2020, 21, 2. [Google Scholar] [CrossRef] [PubMed]




| PDX Models | Advantages | Disadvantages |
|---|---|---|
| (1) Primary tumor specimens implanted subcutaneously (PDX-SC) |
|
|
| (2) Primary tumor specimens implanted orthotopically (PDOX) |
|
|
| (3) Humanized mouse (HM) models |
|
|
| Strain Name | Phenotype | Strain Name | Phenotype |
|---|---|---|---|
| C57BL/6-nu | Nude, athymic, lacks T cells | NOD-Rag1−/− | NOD+ Rag1 mutation leading to lack of mature T and B cells |
| CB17-SCID | Lacks mature T and B cells; radiation sensitive | NOD-Rag1−/− Prf1−/− | NOD+ Rag1 mutation leading to lack of mature T and B cells; lack of perforin |
| NOD- SCID | No mature T and B cells; radiation sensitive; decreased innate immunity | NOD-SCID HLA-A2.1-transgenic | NOD-SCID+ Transgenic expression of human HLA-A2.1 |
| BALB/c-SCID bg | No mature T and B cells; radiation sensitive; decreased NK-cell activity | NOD/LtSz-SCID Il2rg−/− | No mature T and B cells; radiation sensitive; IL-2Rγ-chain deficiency; reduced multiple cytokine receptors thus many innate immune defects |
| C57BL/6-SCID bg | No mature T and B cells; decreased NK-cell activity | NOD/Shi-SCID Il2rg−/− | Similar to NOD/LtSz-SCID Il2rg−/− mice |
| NOD-SCID B2m−/− | No mature T and B cells; radiation sensitive; no β2m, leading to lack of MHC class I expression | BALB/c-Rag2−/− Il2rg−/− | Similar to NOD/LtSz-SCID Il2rg−/− mice |
| NOD-SCID IL-3-, GM-CSF and SCF transgenic | No mature T and B cells; radiation sensitive; transgenic human cytokine production | H2d -Rag2−/−Il2rg−/− | Similar to NOD/LtSz-SCID Il2rg−/− mice |
| Mouse Model | Attributes of the Human Immune System |
|---|---|
| NSG+ hPBMCs | Adult T cells, educated in a human thymus, infiltrate implanted tumors but are alloreactive to the mouse |
| NSG+ cord blood HSCs | Murine T-cell education; incomplete development of B cells and myeloid cells |
| NSG+ fetal BLT | Human thymic education produces active T cells |
| BRG+ HSCs+ human cytokines | Greater human immune cell populations; improved myeloid cell maturation |
| hHLA-A * 02-NSG | T-cell education guided by a human antigen; improved T-cell activity |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jin, J.; Yoshimura, K.; Sewastjanow-Silva, M.; Song, S.; Ajani, J.A. Challenges and Prospects of Patient-Derived Xenografts for Cancer Research. Cancers 2023, 15, 4352. https://doi.org/10.3390/cancers15174352
Jin J, Yoshimura K, Sewastjanow-Silva M, Song S, Ajani JA. Challenges and Prospects of Patient-Derived Xenografts for Cancer Research. Cancers. 2023; 15(17):4352. https://doi.org/10.3390/cancers15174352
Chicago/Turabian StyleJin, Jiankang, Katsuhiro Yoshimura, Matheus Sewastjanow-Silva, Shumei Song, and Jaffer A. Ajani. 2023. "Challenges and Prospects of Patient-Derived Xenografts for Cancer Research" Cancers 15, no. 17: 4352. https://doi.org/10.3390/cancers15174352
APA StyleJin, J., Yoshimura, K., Sewastjanow-Silva, M., Song, S., & Ajani, J. A. (2023). Challenges and Prospects of Patient-Derived Xenografts for Cancer Research. Cancers, 15(17), 4352. https://doi.org/10.3390/cancers15174352








