Single-Isocenter Linac-Based Radiosurgery for Brain Metastases with Coplanar Arcs: A Dosimetric and Clinical Analysis
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Cohort and Treatment Characteristic
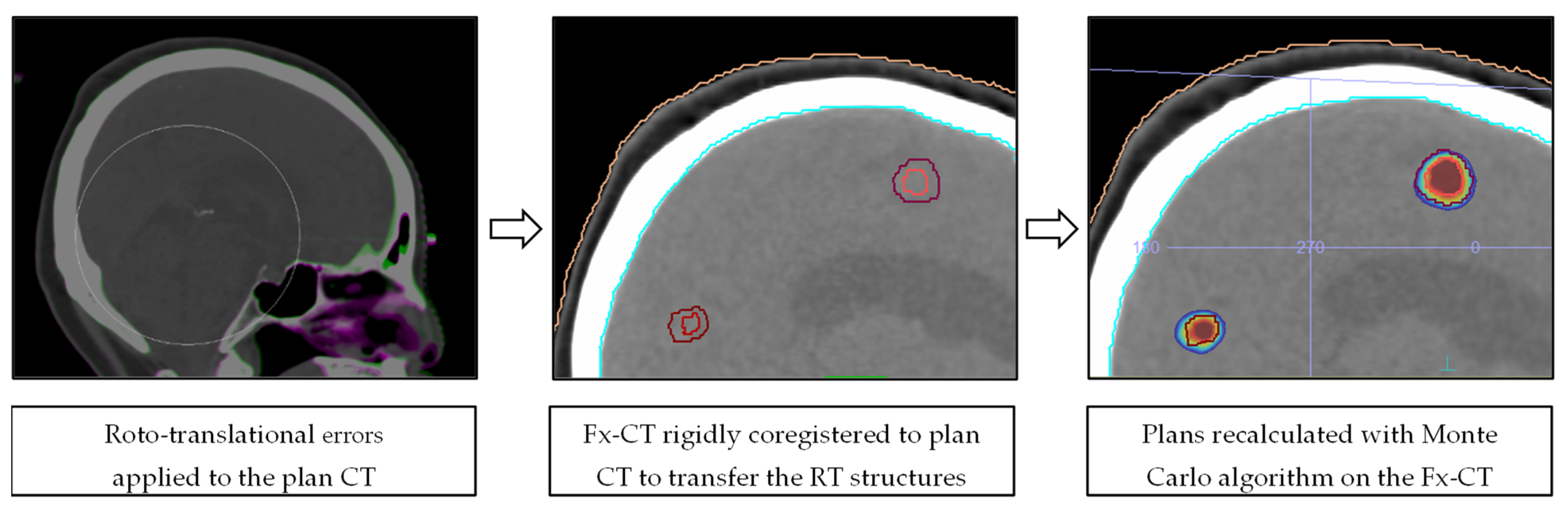
2.2. Dose Recalculation and Data Analysis
3. Results
3.1. Patient Characteristics and Plan Statistics
3.2. Geometric Accuracy
3.3. Dosimetric Accuracy
3.4. Clinical Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mathis, N.J.; Wijetunga, N.A.; Imber, B.S.; Pike, L.R.G.; Yang, J.T. Recent Advances and Applications of Radiation Therapy for Brain Metastases. Curr. Oncol. Rep. 2022, 24, 335–342. [Google Scholar] [CrossRef] [PubMed]
- Tini, P.; Marampon, F.; Giraffa, M.; Bucelli, S.; Niyazi, M.; Belka, C.; Minniti, G. Current status and perspectives of interventional clinical trials for brain metastases: Analysis of ClinicalTrials.gov. Radiat. Oncol. 2023, 18, 62. [Google Scholar] [CrossRef]
- Kondziolka, D.; Patel, A.; Lunsford, L.D.; Kassam, A.; Flickinger, J.C. Stereotactic radiosurgery plus whole brain radiotherapy versus radiotherapy alone for patients with multiple brain metastases. Int. J. Radiat. Oncol. Biol. Phys. 1999, 45, 427–434. [Google Scholar] [CrossRef] [PubMed]
- Andrews, D.W.; Scott, C.B.; Sperduto, P.W.; Flanders, A.E.; Gaspar, L.E.; Schell, M.C.; Werner-Wasik, M.; Demas, W.; Ryu, J.; Bahary, J.; et al. Whole brain radiation therapy with or without stereotactic radiosurgery boost for patients with one to three brain metastases: Phase III results of the RTOG 9508 randomised trial. Lancet 2004, 363, 1665–1672. [Google Scholar] [CrossRef] [PubMed]
- Sperduto, P.W.; Shanley, R.; Luo, X.; Andrews, D.; Werner-Wasik, M.; Valicenti, R.; Bahary, J.; Souhami, L.; Won, M.; Mehta, M. Secondary analysis of RTOG 9508, a phase 3 randomized trial of whole-brain radiation therapy versus WBRT plus stereotactic radiosurgery in patients with 1–3 brain metastases; poststratified by the graded prognostic assessment (GPA). Int. J. Radiat. Oncol. Biol. Phys. 2014, 90, 526–531. [Google Scholar] [CrossRef]
- Aoyama, H.; Shirato, H.; Tago, M.; Nakagawa, K.; Toyoda, T.; Hatano, K.; Kenjyo, M.; Oya, N.; Hirota, S.; Shioura, H.; et al. Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: A randomized controlled trial. JAMA 2006, 295, 2483–2491. [Google Scholar] [CrossRef] [PubMed]
- Chang, E.L.; Wefel, J.S.; Hess, K.R.; Allen, P.K.; Lang, F.F.; Kornguth, D.G.; Arbuckle, R.B.; Swint, J.M.; Shiu, A.S.; Maor, M.H.; et al. Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: A randomised controlled trial. Lancet Oncol. 2009, 10, 1037–1044. [Google Scholar] [CrossRef]
- Kocher, M.; Soffietti, R.; Abacioglu, U.; Villa, S.; Fauchon, F.; Baumert, B.G.; Fariselli, L.; Tzuk-Shina, T.; Kortmann, R.D.; Carrie, C.; et al. Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: Results of the EORTC 22952-26001 study. J. Clin. Oncol. 2011, 29, 134–141. [Google Scholar] [CrossRef]
- Soffietti, R.; Kocher, M.; Abacioglu, U.M.; Villa, S.; Fauchon, F.; Baumert, B.G.; Fariselli, L.; Tzuk-Shina, T.; Kortmann, R.D.; Carrie, C.; et al. A European Organisation for Research and Treatment of Cancer phase III trial of adjuvant whole-brain radiotherapy versus observation in patients with one to three brain metastases from solid tumors after surgical resection or radiosurgery: Quality-of-life results. J. Clin. Oncol. 2013, 31, 65–72. [Google Scholar] [CrossRef]
- Brown, P.D.; Jaeckle, K.; Ballman, K.V.; Farace, E.; Cerhan, J.H.; Anderson, S.K.; Carrero, X.W.; Barker, F.G., 2nd; Deming, R.; Burri, S.H.; et al. Effect of Radiosurgery Alone vs Radiosurgery with Whole Brain Radiation Therapy on Cognitive Function in Patients With 1 to 3 Brain Metastases: A Randomized Clinical Trial. JAMA. 2016, 316, 401–409. [Google Scholar] [CrossRef]
- Le Rhun, E.; Guckenberger, M.; Smits, M.; Dummer, R.; Bachelot, T.; Sahm, F.; Galldiks, N.; de Azambuja, E.; Berghoff, A.S.; Metellus, P.; et al. EANO-ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up of patients with brain metastasis from solid tumours. Ann. Oncol. 2021, 32, 1332–1347. [Google Scholar] [CrossRef] [PubMed]
- Zindler, J.D.; Bruynzeel, A.M.E.; Eekers, D.B.P.; Hurkmans, C.W.; Swinnen, A.; Lambin, P. Whole brain radiotherapy versus stereotactic radiosurgery for 4–10 brain metastases: A phase III randomised multicentre trial. BMC Cancer 2017, 17, 500. [Google Scholar] [CrossRef] [PubMed]
- Sahgal, A.; Ruschin, M.; Ma, L.; Verbakel, W.; Larson, D.; Brown, P.D. Stereotactic radiosurgery alone for multiple brain metastases? A review of clinical and technical issues. Neuro Oncol. 2017, 19 (Suppl. S2), ii2–ii15. [Google Scholar] [CrossRef]
- Chang, W.S.; Kim, H.Y.; Chang, J.W.; Park, Y.G.; Chang, J.H. Analysis of radiosurgical results in patients with brain metastases according to the number of brain lesions: Is stereotactic radiosurgery effective for multiple brain metastases? J. Neurosurg. 2010, 113, 73–78. [Google Scholar] [CrossRef]
- Yamamoto, M.; Serizawa, T.; Shuto, T.; Akabane, A.; Higuchi, Y.; Kawagishi, J.; Yamanaka, K.; Sato, Y.; Jokura, H.; Yomo, S.; et al. Stereotactic radiosurgery for patients with multiple brain metastases (JLGK0901): A multi-institutional prospective observational study. Lancet Oncol. 2014, 15, 387–395. [Google Scholar] [CrossRef] [PubMed]
- Feygelman, V.; Walker, L.; Chinnaiyan, P.; Forster, K. Simulation of intrafraction motion and overall geometrical accuracy of a frameless intracranial radiosurgery process. J. Appl. Clin. Med. Phys. 2008, 9, 68–86. [Google Scholar] [CrossRef]
- Solberg, T.D.; Medin, P.M.; Mullins, J.; Li, S. Quality assurance of immobilization and target localization systems for frameless stereotactic cranial and extracranial hypofractionated radiotherapy. Int. J. Radiat. Oncol. Biol. Phys. 2008, 71, S131–S135. [Google Scholar] [CrossRef]
- Lamba, M.; Breneman, J.C.; Warnick, R.E. Evaluation of image-guided positioning for frameless intracranial radiosurgery. Int. J. Radiat. Oncol. Biol. Phys. 2009, 74, 913–919. [Google Scholar] [CrossRef]
- Hanna, S.A.; Mancini, A.; Dal Col, A.H.; Asso, R.N.; Neves-Junior, W.F.P. Frameless Image-Guided Radiosurgery for Multiple Brain Metastasis Using VMAT: A Review and an Institutional Experience. Front. Oncol. 2019, 9, 703. [Google Scholar] [CrossRef]
- Scorsetti, M.; Navarria, P.; Cozzi, L.; Clerici, E.; Bellu, L.; Franceschini, D.; Marzo, A.M.; Franzese, C.; Torri, V.; Reggiori, G.; et al. Radiosurgery of limited brain metastases from primary solid tumor: Results of the randomized phase III trial (NCT02355613) comparing treatments executed with a specialized or a C-arm linac-based platform. Radiat. Oncol. 2023, 18, 28. [Google Scholar] [CrossRef]
- Ruschin, M.; Nayebi, N.; Carlsson, P.; Brown, K.; Tamerou, M.; Li, W.; Laperriere, N.; Sahgal, A.; Cho, Y.B.; Ménard, C.; et al. Performance of a novel repositioning head frame for gamma knife perfexion and image-guided linac-based intracranial stereotactic radiotherapy. Int. J. Radiat. Oncol. Biol. Phys. 2010, 78, 306–313. [Google Scholar] [CrossRef]
- Ramakrishna, N.; Rosca, F.; Friesen, S.; Tezcanli, E.; Zygmanszki, P.; Hacker, F. A clinical comparison of patient setup and intra-fraction motion using frame-based radiosurgery versus a frameless image-guided radiosurgery system for intracranial lesions. Radiother. Oncol. 2010, 95, 109–115. [Google Scholar] [CrossRef]
- Babic, S.; Lee, Y.; Ruschin, M.; Lochray, F.; Lightstone, A.; Atenafu, E.; Phan, N.; Mainprize, T.; Tsao, M.; Soliman, H.; et al. To frame or not to frame? Cone-beam CT-based analysis of head immobilization devices specific to linac-based stereotactic radiosurgery and radiotherapy. J. Appl. Clin. Med. Phys. 2018, 19, 111–120. [Google Scholar] [CrossRef]
- Ong, C.L.; Giaj-Levra, N.; Nicosia, L.; Figlia, V.; Tomasini, D.; Franken, E.M.; Alongi, F. Intra-fraction and Inter-fraction analysis of a dedicated immobilization device for intracranial radiation treatment. Radiat. Oncol. 2020, 15, 200. [Google Scholar] [CrossRef] [PubMed]
- Meyer, J.; Wilbert, J.; Baier, K.; Guckenberger, M.; Richter, A.; Sauer, O.; Flentje, M. Positioning accuracy of cone-beam computed tomography in combination with a HexaPOD robot treatment table. Int. J. Radiat. Oncol. Biol. Phys. 2007, 67, 1220–1228. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.; Yenice, K.M.; Narayana, A.; Gutin, P.H. Accuracy and feasibility of cone-beam computed tomography for stereotactic radiosurgery setup. Med. Phys. 2007, 34, 2077–2084. [Google Scholar] [CrossRef] [PubMed]
- Lightstone, A.W.; Tsao, M.; Baran, P.S.; Chan, G.; Pang, G.; Ma, L.; Lochray, F.; Sahgal, A. Cone beam CT (CBCT) evaluation of inter- and intra-fraction motion for patients undergoing brain radiotherapy immobilized using a commercial thermoplastic mask on a robotic couch. Technol. Cancer Res. Treat. 2012, 11, 203–209. [Google Scholar] [CrossRef]
- Clark, G.M.; Popple, R.A.; Young, P.E.; Fiveash, J.B. Feasibility of single-isocenter volumetric modulated arc radiosurgery for treatment of multiple brain metastases. Int. J. Radiat. Oncol. Biol. Phys. 2010, 76, 296–302. [Google Scholar] [CrossRef]
- Lau, S.K.; Zakeri, K.; Zhao, X.; Carmona, R.; Knipprath, E.; Simpson, D.R.; Nath, S.K.; Kim, G.Y.; Sanghvi, P.; Hattangadi-Gluth, J.A.; et al. Single-Isocenter Frameless Volumetric Modulated Arc Radiosurgery for Multiple Intracranial Metastases. Neurosurgery. 2015, 77, 233–240. [Google Scholar] [CrossRef]
- Morrison, J.; Hood, R.; Yin, F.F.; Salama, J.K.; Kirkpatrick, J.; Adamson, J. Is a single isocenter sufficient for volumetric modulated arc therapy radiosurgery when multiple intracranial metastases are spatially dispersed? Med. Dosim. 2016, 41, 285–289. [Google Scholar] [CrossRef]
- Ruggieri, R.; Naccarato, S.; Mazzola, R.; Ricchetti, F.; Corradini, S.; Fiorentino, A.; Alongi, F. Linac-based VMAT radiosurgery for multiple brain lesions: Comparison between a conventional multi-isocenter approach and a new dedicated mono-isocenter technique. Radiat. Oncol. 2018, 13, 38. [Google Scholar] [CrossRef] [PubMed]
- Roper, J.; Chanyavanich, V.; Betzel, G.; Switchenko, J.; Dhabaan, A. Single-Isocenter Multiple-Target Stereotactic Radiosurgery: Risk of Compromised Coverage. Int. J. Radiat. Oncol. Biol. Phys. 2015, 93, 540–546. [Google Scholar] [CrossRef] [PubMed]
- Stanhope, C.; Chang, Z.; Wang, Z.; Yin, F.F.; Kim, G.; Salama, J.K.; Kirkpatrick, J.; Adamson, J. Physics considerations for single-isocenter, volumetric modulated arc radiosurgery for treatment of multiple intracranial targets. Pract. Radiat. Oncol. 2016, 6, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Ezzell, G.A. The spatial accuracy of two frameless, linear accelerator-based systems for single-isocenter, multitarget cranial radiosurgery. J. Appl. Clin. Med. Phys. 2017, 18, 37–43. [Google Scholar] [CrossRef]
- Saenz, D.L.; Li, Y.; Rasmussen, K.; Stathakis, S.; Pappas, E.; Papanikolaou, N. Dosimetric and localization accuracy of Elekta high definition dynamic radiosurgery. Phys. Med. 2018, 54, 146–151. [Google Scholar] [CrossRef]
- Prentou, G.; Pappas, E.P.; Logothetis, A.; Koutsouveli, E.; Pantelis, E.; Papagiannis, P.; Karaiskos, P. Dosimetric impact of rotational errors on the quality of VMAT-SRS for multiple brain metastases: Comparison between single- and two-isocenter treatment planning techniques. J. Appl. Clin. Med. Phys. 2020, 21, 32–44. [Google Scholar] [CrossRef]
- Selvan, K.T.; Padma, G.; Revathy, M.K.; Nambi Raj, N.A.; Senthilnathan, K.; Babu, P.R. Dosimetric Effect of Rotational Setup Errors in Single-Isocenter Volumetric-Modulated Arc Therapy of Multiple Brain Metastases. J. Med. Phys. 2019, 44, 84–90. [Google Scholar]
- Audet, C.; Poffenbarger, B.A.; Chang, P.; Jackson, P.S.; Lundahl, R.E.; Ryu, S.I.; Ray, G.R. Evaluation of volumetric modulated arc therapy for cranial radiosurgery using multiple noncoplanar arcs. Med. Phys. 2011, 38, 5863–5872. [Google Scholar] [CrossRef]
- Guckenberger, M.; Roesch, J.; Baier, K.; Sweeney, R.A.; Flentje, M. Dosimetric consequences of translational and rotational errors in frame-less image-guided radiosurgery. Radiat. Oncol. 2012, 7, 63. [Google Scholar] [CrossRef]
- Limon, D.; McSherry, F.; Herndon, J.; Sampson, J.; Fecci, P.; Adamson, J.; Wang, Z.; Yin, F.F.; Floyd, S.; Kirkpatrick, J. Single fraction stereotactic radiosurgery for multiple brain metastases. Adv. Radiat. Oncol. 2017, 2, 555–563. [Google Scholar] [CrossRef] [PubMed]
- Yuan, Y.; Thomas, E.M.; Clark, G.A.; Markert, J.M.; Fiveash, J.B.; Popple, R.A. Evaluation of multiple factors affecting normal brain dose in single-isocenter multiple target radiosurgery. J. Radiosurg. SBRT 2018, 5, 131–144. [Google Scholar] [PubMed]
- Hofmaier, J.; Bodensohn, R.; Garny, S.; Hadi, I.; Fleischmann, D.F.; Eder, M.; Dinc, Y.; Reiner, M.; Corradini, S.; Parodi, K.; et al. Single isocenter stereotactic radiosurgery for patients with multiple brain metastases: Dosimetric comparison of VMAT and a dedicated DCAT planning tool. Radiat. Oncol. 2019, 14, 103. [Google Scholar] [CrossRef] [PubMed]
- Palmer, J.D.; Sebastian, N.T.; Chu, J.; DiCostanzo, D.; Bell, E.H.; Grecula, J.; Arnett, A.; Blakaj, D.M.; McGregor, J.; Elder, J.B.; et al. Single-Isocenter Multitarget Stereotactic Radiosurgery Is Safe and Effective in the Treatment of Multiple Brain Metastases. Adv. Radiat. Oncol. 2019, 5, 70–76. [Google Scholar] [CrossRef]
- Minniti, G.; Capone, L.; Alongi, F.; Figlia, V.; Nardiello, B.; El Gawhary, R.; Scaringi, C.; Bianciardi, F.; Tolu, B.; Gentile, P.; et al. Initial Experience with Single-Isocenter Radiosurgery to Target Multiple Brain Metastases Using an Automated Treatment Planning Software: Clinical Outcomes and Optimal Target Volume Margins Strategy. Adv. Radiat. Oncol. 2020, 5, 856–864. [Google Scholar] [CrossRef]
- Kim, G.J.; Buckley, E.D.; Herndon, J.E.; Allen, K.J.; Dale, T.S.; Adamson, J.D.; Lay, L.; Giles, W.M.; Rodrigues, A.E.; Wang, Z.; et al. Outcomes in Patients With 4 to 10 Brain Metastases Treated with Dose-Adapted Single-Isocenter Multitarget Stereotactic Radiosurgery: A Prospective Study. Adv. Radiat. Oncol. 2021, 6, 100760. [Google Scholar] [CrossRef] [PubMed]
- Fung, N.T.C.; Wong, W.L.; Lee, M.C.H.; Cheung, E.S.N.; Wu, P.Y. Geometric and dosimetric consequences of intra-fractional movement in single isocenter non-coplanar stereotactic radiosurgery. Radiat. Oncol. 2023, 18, 9. [Google Scholar] [CrossRef] [PubMed]
- Thomas, E.M.; Popple, R.A.; Wu, X.; Clark, G.M.; Markert, J.M.; Guthrie, B.L.; Yuan, Y.; Dobelbower, M.C.; Spencer, S.A.; Fiveash, J.B. Comparison of plan quality and delivery time between volumetric arc therapy (RapidArc) and Gamma Knife radiosurgery for multiple cranial metastases. Neurosurgery. 2014, 75, 409–417. [Google Scholar] [CrossRef] [PubMed]
- Tarnavski, N.; Engelholm, S.A.; Af Rosenschold, P.M. Fast intra-fractional image-guidance with 6D positioning correction reduces delivery uncertainty for stereotactic radiosurgery and radiotherapy. J. Radiosurg. SBRT 2016, 4, 15–20. Available online: http://www.ncbi.nlm.nih.gov/pmc/articles/pmc5658830/ (accessed on 11 July 2023).
- Mangesius, J.; Seppi, T.; Weigel, R.; Arnold, C.R.; Vasiljevic, D.; Goebel, G.; Lukas, P.; Ganswindt, U.; Nevinny-Stickel, M. Intrafractional 6D head movement increases with time of mask fixation during stereotactic intracranial RT-sessions. Radiat. Oncol. 2019, 14, 231. [Google Scholar] [CrossRef]
- Redmond, K.J.; Gui, C.; Benedict, S.; Milano, M.T.; Grimm, J.; Vargo, J.A.; Soltys, S.G.; Yorke, E.; Jackson, A.; El Naqa, I.; et al. Tumor Control Probability of Radiosurgery and Fractionated Stereotactic Radiosurgery for Brain Metastases. Int. J. Radiat. Oncol. Biol. Phys. 2021, 110, 53–67. [Google Scholar] [CrossRef]
- Milano, M.T.; Grimm, J.; Niemierko, A.; Soltys, S.G.; Moiseenko, V.; Redmond, K.J.; Yorke, E.; Sahgal, A.; Xue, J.; Mahadevan, A.; et al. Single- and Multifraction Stereotactic Radiosurgery Dose/Volume Tolerances of the Brain. Int. J. Radiat. Oncol. Biol. Phys. 2021, 110, 68–86. [Google Scholar] [CrossRef]
- Lewis, B.C.; Snyder, W.J.; Kim, S.; Kim, T. Monitoring frequency of intra-fraction patient motion using the ExacTrac system for LINAC-based SRS treatments. J. Appl. Clin. Med. Phys. 2018, 19, 58–63. [Google Scholar] [CrossRef]
- Barnes, M.; Yeo, A.; Thompson, K.; Phillips, C.; Kron, T.; Hardcastle, N. A retrospective analysis of setup and intrafraction positional variation in stereotactic radiotherapy treatments. J. Appl. Clin. Med. Phys. 2020, 21, 109–119. [Google Scholar] [CrossRef]
- Agazaryan, N.; Tenn, S.; Lee, C.; Steinberg, M.; Hedge, J.; Chin, R.; Pouratian, N.; Yang, I.; Kim, W.; Kaprealian, T. Simultaneous radiosurgery for multiple brain metastases: Technical overview of the UCLA experience. Radiat. Oncol. 2021, 16, 221. [Google Scholar] [CrossRef] [PubMed]
- Korytko, T.; Radivoyevitch, T.; Colussi, V.; Wessels, B.W.; Pillai, K.; Maciunas, R.J.; Einstein, D.B. 12 Gy gamma knife radiosurgical volume is a predictor for radiation necrosis in non-AVM intracranial tumors. Int. J. Radiat. Oncol. Biol. Phys. 2006, 64, 419–424. [Google Scholar] [CrossRef]
- Blonigen, B.J.; Steinmetz, R.D.; Levin, L.; Lamba, M.A.; Warnick, R.E.; Breneman, J.C. Irradiated volume as a predictor of brain radionecrosis after linear accelerator stereotactic radiosurgery. Int. J. Radiat. Oncol. Biol. Phys. 2010, 77, 996–1001. [Google Scholar] [CrossRef] [PubMed]
- Minniti, G.; Clarke, E.; Lanzetta, G.; Osti, M.F.; Trasimeni, G.; Bozzao, A.; Romano, A.; Enrici, R.M. Stereotactic radiosurgery for brain metastases: Analysis of outcome and risk of brain radionecrosis. Radiat. Oncol. 2011, 6, 48. [Google Scholar] [CrossRef]
- Ma, L.; Sahgal, A.; Larson, D.A.; Pinnaduwage, D.; Fogh, S.; Barani, I.; Nakamura, J.; McDermott, M.; Sneed, P. Impact of millimeter-level margins on peripheral normal brain sparing for gamma knife radiosurgery. Int. J. Radiat. Oncol. Biol. Phys. 2014, 89, 206–213. [Google Scholar] [CrossRef]
- Sagawa, T.; Ohira, S.; Ueda, Y.; Akino, Y.; Mizuno, H.; Matsumoto, M.; Miyazaki, M.; Koizumi, M.; Teshima, T. Dosimetric effect of rotational setup errors in stereotactic radiosurgery with HyperArc for single and multiple brain metastases. J. Appl. Clin. Med. Phys. 2019, 20, 84–91. [Google Scholar] [CrossRef] [PubMed]
- Kraft, J.; van Timmeren, J.E.; Mayinger, M.; Frei, S.; Borsky, K.; Stark, L.S.; Krayenbuehl, J.; Zamburlini, M.; Guckenberger, M.; Tanadini-Lang, S.; et al. Distance to isocenter is not associated with an increased risk for local failure in LINAC-based single-isocenter SRS or SRT for multiple brain metastases. Radiother. Oncol. 2021, 159, 168–175. [Google Scholar] [CrossRef] [PubMed]
- Gevaert, T.; Steenbeke, F.; Pellegri, L.; Engels, B.; Christian, N.; Hoornaert, M.; Verellen, D.; Mitine, C.; De Ridder, M. Evaluation of a dedicated brain metastases treatment planning optimization for radiosurgery: A new treatment paradigm? Radiat. Oncol. 2016, 11, 13. [Google Scholar] [CrossRef] [PubMed]
- Petoukhova, A.; Snijder, R.; Wiggenraad, R.; de Boer-de Wit, L.; Mudde-van der Wouden, I.; Florijn, M.; Zindler, J. Quality of Automated Stereotactic Radiosurgery Plans in Patients with 4 to 10 Brain Metastases. Cancers 2021, 13, 3458. [Google Scholar] [CrossRef] [PubMed]
- Aiyama, H.; Yamamoto, M.; Kawabe, T.; Watanabe, S.; Koiso, T.; Sato, Y.; Higuchi, Y.; Ishikawa, E.; Yamamoto, T.; Matsumura, A.; et al. Clinical significance of conformity index and gradient index in patients undergoing stereotactic radiosurgery for a single metastatic tumor. J. Neurosurg. 2018, 129 (Suppl. S1), 103–110. [Google Scholar] [CrossRef] [PubMed]


| Parameter | No. | |
|---|---|---|
| Number of patients | 70 | |
| Median age | 66 | |
| Sex | F/M | 33/37 |
| Histology | Lung | 31 (44.4%) |
| Melanoma | 15 (21.4%) | |
| Breast | 12 (17.1%) | |
| Other | 12 (17.1%) | |
| No. of lesions per patient | 1 | 38 (54.3%) |
| 2 | 19 (27.1%) | |
| 3–4 | 10 (14.3%) | |
| 5–7 | 3 (4.3%) | |
| Concomitant systemic therapy | Chemotherapy | 10 (14.3%) |
| Immunotherapy | 6 (8.6%) | |
| Molecular targeted agents | 10 (14.3%) | |
| Hormonal therapy | 2 (2.9%) | |
| Dose prescription | 21 Gy/1 fraction | 46 (65.7%) |
| 15–18 Gy/1 fraction | 13 (18.6%) | |
| 27 Gy/3 fractions | 11 (15.7%) | |
| No. of arcs per patient (collimator angle) | 1 (90°) | 20 (28.6%) |
| 2 (0°, 90° or 45°, 315°) | 38 (54.3%) | |
| 3 (45°, 315°, 90°) | 11 (15.7%) | |
| 4 (0°, 45°, 315°, 90°) | 1 (1.4%) | |
| Median MU [range] | 2644.4 [1047.0–5734.3] | |
| Median delivery time [range] | 3.78 min [1.83–9.25] | |
| Median dose metrics [range] | GTV D95% | 98.6% [73.2–105.7] |
| GTV Dmean | 102.8% [75.0–110.6] | |
| PTV D95% | 87.1% [59.7–97.5] | |
| PTV Dmean | 95.9% [70.8–102.7] | |
| Brain V12 Gy (1 fraction) | 7.95 cc [2.23–28.46] | |
| Brain V20 Gy (3 fractions) | 15.43 cc [8.32–23.47] |
| BM Barycenter Shift | Single BM | Multiple BM | All BM |
|---|---|---|---|
| X < 1 mm | 35 (73%) | 111 (89%) | 146 (84%) |
| 1 mm < X < 2 mm | 11 (23%) | 13 (10%) | 24 (14%) |
| X > 2 mm | 2 (4%) | 1 (1%) | 3 (2%) |
| Single BM | Multiple BM | All BM | |||||
|---|---|---|---|---|---|---|---|
| Metrics | Mean [Range] | p-Value | Mean [Range] | p-Value | Mean [Range] | p-Value | |
| GTV | D95% | −0.6% [−4.1–0.6] | 0.666 | −0.8% [−14.8–2.3] | 0.639 | −0.7% [−14.8–2.3] | 0.556 |
| Dmean | 0.0% [−1.1–0.6] | 0.967 | −0.2% [−7.3–0.8] | 0.943 | −0.1% [−7.3–0.8] | 0.952 | |
| PTV | D95% | −1.0% [−8.7–4.0] | 0.529 | −1.3% [−18.8–7.6] | 0.546 | −1.2% [−18.8–7.6] | 0.462 |
| Dmean | 0.0% [−1.4–1.8] | 0.950 | −0.1% [−5.5–0.5] | 0.944 | −0.1% [−5.5–1.8] | 0.989 | |
| Brain | V12–20 Gy | +0.4% [−2.0–7.7] | 0.958 | +0.4% [−0.6–3.6] | 0.898 | 0.4% [−2.0–7.7] | 0.935 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Faccenda, V.; Panizza, D.; Pisoni, V.; Trivellato, S.; Daniotti, M.C.; Bianchi, S.P.; De Ponti, E.; Arcangeli, S. Single-Isocenter Linac-Based Radiosurgery for Brain Metastases with Coplanar Arcs: A Dosimetric and Clinical Analysis. Cancers 2023, 15, 4496. https://doi.org/10.3390/cancers15184496
Faccenda V, Panizza D, Pisoni V, Trivellato S, Daniotti MC, Bianchi SP, De Ponti E, Arcangeli S. Single-Isocenter Linac-Based Radiosurgery for Brain Metastases with Coplanar Arcs: A Dosimetric and Clinical Analysis. Cancers. 2023; 15(18):4496. https://doi.org/10.3390/cancers15184496
Chicago/Turabian StyleFaccenda, Valeria, Denis Panizza, Valerio Pisoni, Sara Trivellato, Martina Camilla Daniotti, Sofia Paola Bianchi, Elena De Ponti, and Stefano Arcangeli. 2023. "Single-Isocenter Linac-Based Radiosurgery for Brain Metastases with Coplanar Arcs: A Dosimetric and Clinical Analysis" Cancers 15, no. 18: 4496. https://doi.org/10.3390/cancers15184496
APA StyleFaccenda, V., Panizza, D., Pisoni, V., Trivellato, S., Daniotti, M. C., Bianchi, S. P., De Ponti, E., & Arcangeli, S. (2023). Single-Isocenter Linac-Based Radiosurgery for Brain Metastases with Coplanar Arcs: A Dosimetric and Clinical Analysis. Cancers, 15(18), 4496. https://doi.org/10.3390/cancers15184496








