Low Alanine-Aminotransferase Blood Activity Is Associated with Increased Mortality in Chronic Lymphocytic Leukemia Patients: A Retrospective Cohort Study of 716 Patients
Abstract
:Simple Summary
Abstract
1. Background
1.1. Chronic Lymphocytic Leukemia as a Common Hematologic Malignancy
1.2. Sarcopenia and Frailty in CLL Patients
1.3. Low Alanine Aminotransferase as a Biomarker for Syndromes of Sarcopenia and Frailty
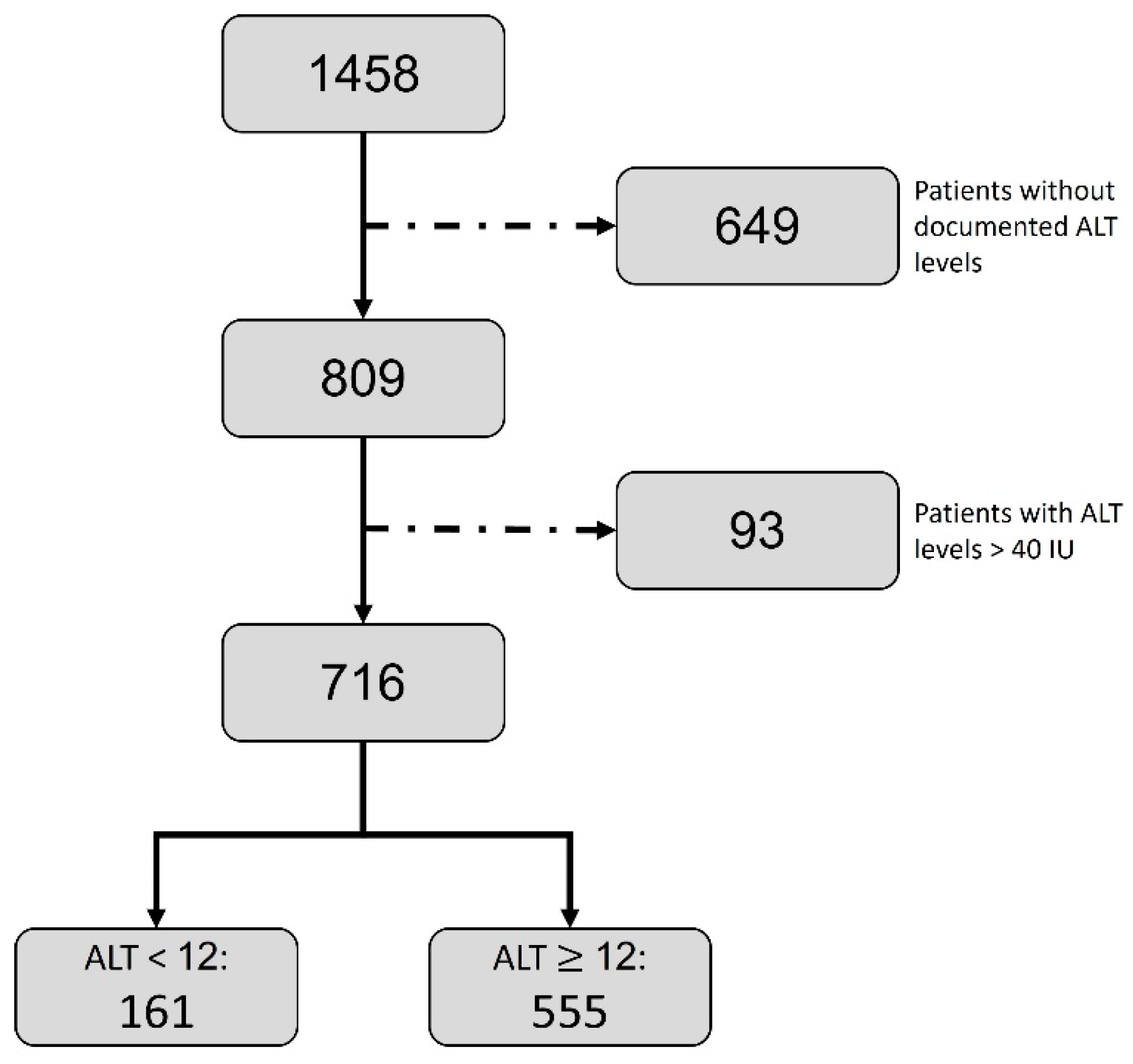
2. Patients and Methods
2.1. Patient Population
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hallek, M. Chronic lymphocytic leukemia: 2020 update on diagnosis, risk stratification and treatment. Am. J. Hematol. 2019, 94, 1266–1287. [Google Scholar] [CrossRef] [PubMed]
- Eichhorst, B.; Robak, T.; Montserrat, E.; Ghia, P.; Niemann, C.U.; Kater, A.P.; Gregor, M.; Cymbalista, F.; Buske, C.; Hillmen, P.; et al. Chronic lymphocytic leukaemia: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2021, 32, 23–33. [Google Scholar] [CrossRef] [PubMed]
- Rhodes, J.M.; Barrientos, J.C.; Rai, K.R. How Have Targeted Agents Changed the Treatment Landscape for Elderly Patients with CLL? Curr. Oncol. Rep. 2022, 24, 1705–1713. Available online: https://pubmed.ncbi.nlm.nih.gov/36334220/ (accessed on 11 April 2023). [CrossRef] [PubMed]
- Shadman, M. Diagnosis and Treatment of Chronic Lymphocytic Leukemia: A Review. JAMA 2023, 329, 918. Available online: https://pubmed.ncbi.nlm.nih.gov/36943212/ (accessed on 11 April 2023). [CrossRef]
- Rai, K.R.; Sawitsky, A.; Cronkite, E.P.; Chanana, A.D.; Levy, R.N.; Pasternack, B.S. Clinical staging of chronic lymphocytic leukemia. Blood 1975, 46, 219–234. [Google Scholar] [CrossRef]
- Binet, J.L.; Auquier, A.; Dighiero, G.; Chastang, C.; Piguet, H.; Goasguen, J.; Vaugier, G.; Potron, G.; Colona, P.; Oberling, F.; et al. A new prognostic classification of chronic lymphocytic leukemia derived from a multivariate survival analysis. Cancer 1981, 48, 198–206. [Google Scholar] [CrossRef]
- Parikh, S.A.; Shanafelt, T.D. Prognostic factors and risk stratification in chronic lymphocytic leukemia. Semin. Oncol. 2016, 43, 233–240. [Google Scholar] [CrossRef]
- The International CLL-IPI Working Group. An international prognostic index for patients with chronic lymphocytic leukaemia (CLL-IPI): A meta-analysis of individual patient data. Lancet Oncol. 2016, 17, 779–790. [Google Scholar] [CrossRef]
- Hallek, M.; Cheson, B.D.; Catovsky, D.; Caligaris-Cappio, F.; Dighiero, G.; Döhner, H.; Hillmen, P.; Keating, M.; Montserrat, E.; Chiorazzi, N.; et al. iwCLL guidelines for diagnosis, indications for treatment, response assessment, and supportive management of CLL. Blood 2018, 131, 2745–2760. [Google Scholar] [CrossRef]
- Salvi, F.; Miller, M.D.; Grilli, A.; Giorgi, R.; Towers, A.L.; Morichi, V.; Spazzafumo, L.; Mancinelli, L.; Espinosa, E.; Rappelli, A.; et al. A manual of guidelines to score the modified Cumulative Illness Rating Scale and its validation in acute hospitalized elderly patients. J. Am. Geriatr. Soc. 2008, 56, 1926–1931. [Google Scholar] [CrossRef]
- Mischel, A.M.; Rosielle, D.A. Eastern Cooperative Oncology Group Performance Status #434. J. Palliat. Med. 2022, 25, 508–510. [Google Scholar]
- Cordoba, R.; Eyre, T.A.; Klepin, H.D.; Wildes, T.M.; Goede, V. A comprehensive approach to therapy of haematological malignancies in older patients. Lancet Haematol. 2021, 8, e840–e852. Available online: https://pubmed.ncbi.nlm.nih.gov/34624238/ (accessed on 11 April 2023). [CrossRef] [PubMed]
- Clegg, A.; Young, J.; Iliffe, S.; Rikkert, M.O.; Rockwood, K. Frailty in elderly people. Lancet 2013, 381, 752–762. [Google Scholar] [CrossRef] [PubMed]
- Cesari, M.; Calvani, R.; Marzetti, E. Frailty in Older Persons. Clin. Geriatr. Med. 2017, 33, 293–303. [Google Scholar] [CrossRef] [PubMed]
- Landi, F.; Calvani, R.; Cesari, M.; Tosato, M.; Martone, A.M.; Ortolani, E.; Savera, G.; Salini, S.; Sisto, A.; Picca, A.; et al. Sarcopenia: An overview on current definitions, diagnosis and treatment. Curr. Protein Pept. Sci. 2018, 19, 633–638. [Google Scholar] [CrossRef]
- Marzetti, E.; Calvani, R.; Cesari, M.; Tosato, M.; Cherubini, A.; Di Bari, M.; Pahor, M.; Savera, G.; Collamati, A.; D’Angelo, E.; et al. Operationalization of the physical frailty & sarcopenia syndrome: Rationale and clinical implementation. Transl. Med. UniSa. 2015, 13, 29–32. [Google Scholar]
- Picca, A.; Coelho-Junior, H.J.; Calvani, R.; Marzetti, E.; Vetrano, D.L. Biomarkers shared by frailty and sarcopenia in older adults: A systematic review and meta-analysis. Ageing Res. Rev. 2022, 73, 101530. [Google Scholar] [CrossRef]
- Lasman, N.; Shalom, M.; Turpashvili, N.; Goldhaber, G.; Lifshitz, Y.; Leibowitz, E.; Berger, G.; Saltzman-Shenhav, G.; Brom, A.; Cohen, D.; et al. Baseline low ALT activity is associated with increased long-term mortality after COPD exacerbations. BMC Pulm. Med. 2020, 20, 133. [Google Scholar] [CrossRef]
- Segev, A.; Itelman, E.; Beigel, R.; Segal, G.; Chernomordik, F.; Matetzky, S.; Grupper, A. Low ALT levels are associated with poor outcomes in acute coronary syndrome patients in the intensive cardiac care unit. J. Cardiol. 2022, 79, 385–390. [Google Scholar] [CrossRef]
- Segev, A.; Itelman, E.; Avaky, C.; Negru, L.; Shenhav-Saltzman, G.; Grupper, A.; Wasserstrum, Y.; Segal, G. Low ALT Levels Associated with Poor Outcomes in 8700 Hospitalized Heart Failure Patients. J. Clin. Med. 2020, 9, 3185. Available online: https://pubmed.ncbi.nlm.nih.gov/33008125/ (accessed on 12 April 2023). [CrossRef]
- Itelman, E.; Segev, A.; Ahmead, L.; Leibowitz, E.; Agbaria, M.; Avaky, C.; Negro, L.; Shenhav-Saltzman, G.; Wasserstrum, Y.; Segal, G. Low ALT values amongst hospitalized patients are associated with increased risk of hypoglycemia and overall mortality: A retrospective, big-data analysis of 51 831 patients. QJM 2021, 114, 843–847. [Google Scholar] [CrossRef]
- Li, J.; Zhao, Z.; Jiang, H.; Jiang, M.; Yu, G.; Li, X. Predictive value of elevated alanine aminotransferase for in-hospital mor-tality in patients with acute myocardial infarction. BMC Cardiovasc. Disord. 2021, 21, 82. [Google Scholar] [CrossRef]
- Anani, S.; Goldhaber, G.; Brom, A.; Lasman, N.; Turpashvili, N.; Shenhav-Saltzman, G.; Avaky, C.; Negru, L.; Agbaria, M.; Ariam, S.; et al. Frailty and Sarcopenia Assessment upon HospitalAdmission to Internal Medicine Predicts Length ofHospital Stay and Re-Admission: A ProspectiveStudy of 980 Patients. J. Clin. Med. 2020, 9, 2659. Available online: http://www.ncbi.nlm.nih.gov/pubmed/32824484 (accessed on 12 April 2023). [CrossRef] [PubMed]
- Portal, D.; Hofstetter, L.; Eshed, I.; Dan-Lantsman, C.; Sella, T.; Urban, D.; Onn, A.; Bar, J.; Segal, G. L3 skeletal muscle index (L3SMI) is a surrogate marker of sarcopenia and frailty in non-small cell lung cancer patients. Cancer Manag. Res. 2019, 11, 2579–2588. Available online: http://www.ncbi.nlm.nih.gov/pubmed/31114324 (accessed on 12 April 2023).
- Portal, D.; Melamed, G.; Segal, G.; Itelman, E. Sarcopenia as Manifested by L3SMI Is Associated with Increased Long-Term Mortality amongst Internal Medicine Patients-A Prospective Cohort Study. J. Clin. Med. 2022, 11, 3500. Available online: https://pubmed.ncbi.nlm.nih.gov/35743568/ (accessed on 12 April 2023). [CrossRef] [PubMed]
- Uliel, N.; Segal, G.; Perri, A.; Turpashvili, N.; Kassif Lerner, R.; Itelman, E. Low ALT, a marker of sarcopenia and frailty, is associated with shortened survival amongst myelodysplastic syndrome patients: A retrospective study. Medicine 2023, 102, e33659. Available online: https://pubmed.ncbi.nlm.nih.gov/37115069/ (accessed on 17 May 2023). [CrossRef] [PubMed]
- Peltz-Sinvani, N.; Klempfner, R.; Ramaty, E.; Sela, B.A.; Goldenberg, I.; Segal, G. Low ALT Levels Independently Associat-ed with 22-Year All-Cause Mortality Among Coronary Heart Disease Patients. J. Gen. Intern. Med. 2016, 31, 209–214. Available online: https://pubmed.ncbi.nlm.nih.gov/26245731/ (accessed on 11 August 2023). [CrossRef] [PubMed]
- Hallek, M.; Al-Sawaf, O. Chronic lymphocytic leukemia: 2022 update on diagnostic and therapeutic procedures. Am. J. Hematol. 2021, 96, 1679–1705. [Google Scholar] [CrossRef]
- Balducci, L.; Dolan, D. Chronic Lymphocytic Leukemia in the Elderly: Epidemiology and Proposed Patient-Related Approach. Cancer Control. 2015, 22 (Suppl. 4), 3–6. [Google Scholar] [CrossRef]

| Whole Cohort N = 716 | ALT < 12 IU/L N = 161 [22.5%] | ALT ≥ 12 IU/L N = 555 [77.5%] | p Value |
|---|---|---|---|
| ALT (IU/L); median [IQR] | 10 [8–11] | 18 [15–24] | <0.001 |
| patient demographics | |||
| Age (years); median [IQR] | 77.6 [68.6–82.9] | 75.05 [66.8–81.6] | 0.05 |
| Weight (Kg); median [IQR] | 70 [61.5–80] | 75 [64–83] | 0.01 |
| laboratory parameters | |||
| Creatinine (mg/dL); median [IQR] | 1.02 [0.8–1.3] | 1.0 [0.8–1.2] | 0.04 |
| HB (g/dL), median [IQR] | 10.8 [9.5–12.2] | 12.2 [10.5–13.6] | <0.001 |
| PLT (109/L); median [IQR] | 142 [97–193] | 164 [114–215] | 0.005 |
| CLL characteristics | |||
| Binet C; N (%) | 78 (48.4) | 170 (31.1) | <0.001 |
| background disease | |||
| CKD; N (%) | 24 (14.9) | 60 (10.8) | 0.2 |
| Solid malignancy; N (%) | 41 (25.5) | 124 (22.3) | 0.47 |
| Diabetes mellitus; N (%) | 26 (16.1) | 100 (18) | 0.667 |
| CHF; N (%) | 19 (11.8) | 69 (12.4) | 0.937 |
| IHD; N (%) | 28 (17.4) | 107 (19.3) | 0.671 |
| AF; N (%) | 18 (11.2) | 90 (16.2) | 0.148 |
| Stroke; N (%) | 11 (6.8) | 27 (4.9) | 0.435 |
| Dementia; N (%) | 5 (3.1) | 11 (2) | 0.585 |
| COPD; N (%) | 11 (6.8) | 36 (6.5) | 1 |
| (a) | ||
| Patient Attribute | HR [95% CI] | p Value |
| ALT (IU/L) < 12 | 1.56 [1.23–1.97] | <0.001 |
| (b) | ||
| Patient Attribute | HR [95% CI] | p Value |
| ALT (IU/L) < 12 | 1.31 [1.02–1.66] | 0.031 |
| Age (years) | 1.01 [1.00–1.02] | 0.005 |
| Binet C | 2.06 [1.66–2.54] | <0.001 |
| Creatinine (mg/dL) | 1.17 [1.04–1.33] | 0.011 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hellou, T.; Dumanis, G.; Badarna, A.; Segal, G. Low Alanine-Aminotransferase Blood Activity Is Associated with Increased Mortality in Chronic Lymphocytic Leukemia Patients: A Retrospective Cohort Study of 716 Patients. Cancers 2023, 15, 4606. https://doi.org/10.3390/cancers15184606
Hellou T, Dumanis G, Badarna A, Segal G. Low Alanine-Aminotransferase Blood Activity Is Associated with Increased Mortality in Chronic Lymphocytic Leukemia Patients: A Retrospective Cohort Study of 716 Patients. Cancers. 2023; 15(18):4606. https://doi.org/10.3390/cancers15184606
Chicago/Turabian StyleHellou, Tamer, Guy Dumanis, Arwa Badarna, and Gad Segal. 2023. "Low Alanine-Aminotransferase Blood Activity Is Associated with Increased Mortality in Chronic Lymphocytic Leukemia Patients: A Retrospective Cohort Study of 716 Patients" Cancers 15, no. 18: 4606. https://doi.org/10.3390/cancers15184606
APA StyleHellou, T., Dumanis, G., Badarna, A., & Segal, G. (2023). Low Alanine-Aminotransferase Blood Activity Is Associated with Increased Mortality in Chronic Lymphocytic Leukemia Patients: A Retrospective Cohort Study of 716 Patients. Cancers, 15(18), 4606. https://doi.org/10.3390/cancers15184606







