Aquaporins as Prognostic Biomarker in Prostate Cancer
Abstract
Simple Summary
Abstract
1. Introduction
2. Prognostic Biomarkers and Their Limitations in Prostate Cancer
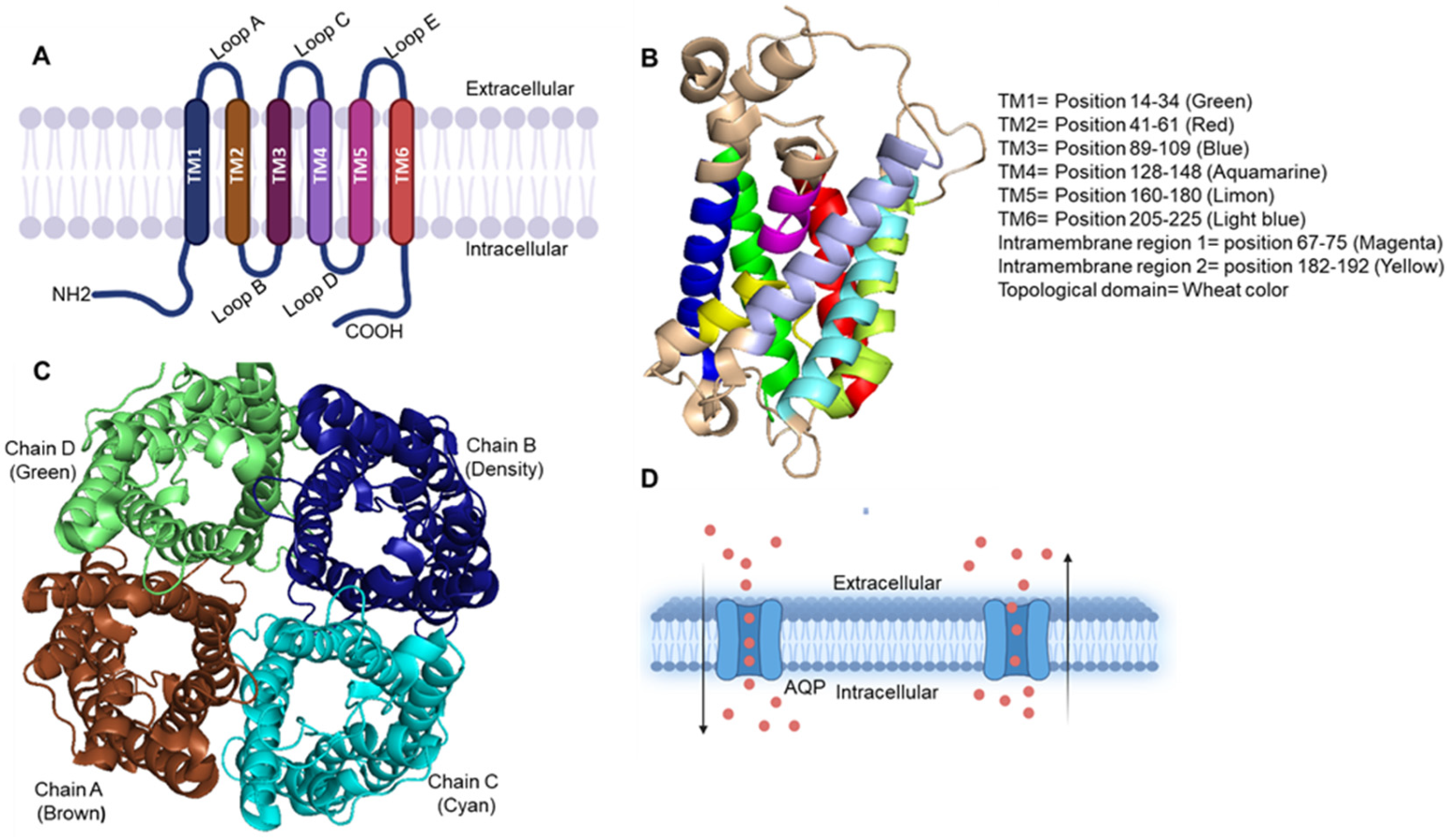
3. Aquaporin Family and Their Function in Normal and Cancer Pathophysiology
4. Aquaporin Expression in Prostate Cancer
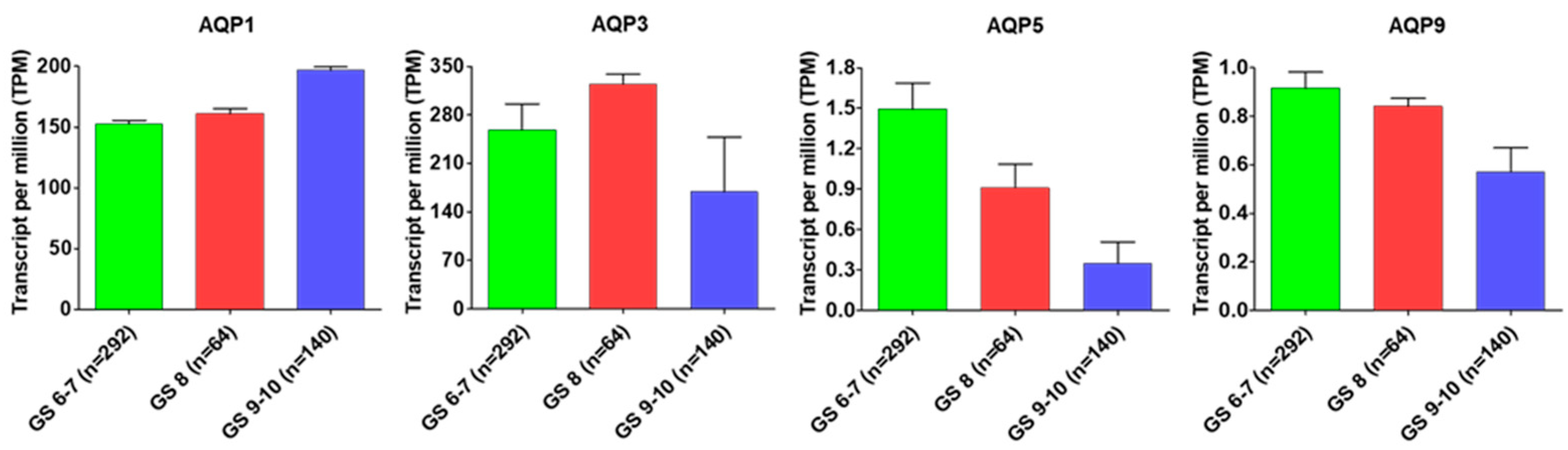
5. Do Aquaporins Serve as Prognostic Biomarkers for Prostate Cancer?
6. Conclusions and Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- American Cancer Society. Cancer Facts & Figures; American Cancer Society: Atlanta, GA, USA, 2022. [Google Scholar]
- Rebello, R.J.; Christoph, O.; Knudsen, K.E.; Loeb, S.; Johnson, D.C.; Reiter, R.E.; Silke Gillessen, S.; Kwast, T.V.D.; Bristow, R.G. Prostate cancer. Nat. Rev. Dis. Prim. 2021, 7, 9. [Google Scholar] [CrossRef]
- Milonas, D.; Venclovas, Z.; Gudinaviciene, I.; Zviniene, K.; Matjosaitis, A.J. Long-term oncological outcomes for young men undergoing radical prostatectomy for localized prostate cancer. Biomed. Res. Int. 2017, 2017, 9858923. [Google Scholar] [CrossRef] [PubMed]
- Humphrey, P.A. Histopathology of prostate cancer. Cold Spring Harb. Perspect. Med. 2017, 7, a030411. [Google Scholar] [CrossRef]
- Bickers, B.; Aukim-Hastie, C. New molecular biomarkers for the prognosis and management of prostate cancer-the post PSA era. Anticancer Res. 2009, 29, 3289–3298. [Google Scholar] [PubMed]
- Lilja, H.; Ulmert, D.; Vickers, A.J. Prostate-specific antigen and prostate cancer: Prediction, detection and monitoring. Nat. Rev. Cancer 2008, 8, 268–278. [Google Scholar] [CrossRef] [PubMed]
- Eggener, S.E.; Badani, K.; Barocas, D.A.; Barrisford, G.W.; Cheng, J.S.; Chin, A.I.; Corcoran, A.; Epstein, J.I.; George, A.K.; Gupta, G.N.; et al. Gleason 6 prostate cancer: Translating biology into population health. J. Urol. 2015, 194, 626–634. [Google Scholar] [CrossRef]
- Ferro, M.; Crocetto, F.; Bruzzese, D.; Imbriaco, M.; Fusco, F.; Longo, N.; Napolitano, L.; Civita, E.L.; Cennamo, M.; Liotti, A.; et al. Prostate health index and multiparametric MRI: Partners in crime fighting overdiagnosis and overtreatment in prostate cancer. Cancers 2021, 13, 4723. [Google Scholar] [CrossRef]
- Crocetto, F.; Russo, G.; Di Zazzo, E.; Pisapia, P.; Mirto, B.F.; Palmieri, A.; Pepe, F.; Bellevicine, C.; Russo, A.; Civita, E.L.; et al. Liquid biopsy in prostate cancer management—Current challenges and future perspectives. Cancers 2022, 14, 3272. [Google Scholar] [CrossRef]
- Kretschmer, A.; Tilki, D. Biomarkers in prostate cancer–current clinical utility and future perspectives. Crit. Rev. Oncol. Hematol. 2017, 120, 180–193. [Google Scholar] [CrossRef]
- Matuszczak, M.; Schalken, J.A.; Salagierski, M. Prostate cancer liquid biopsy biomarkers’ clinical utility in diagnosis and prognosis. Cancers 2021, 13, 3373. [Google Scholar] [CrossRef]
- Legisi, L.; DeSa, E.; Qureshi, M.N. Use of the prostate core mitomic test in repeated biopsy decision-making: Real-world assessment of clinical utility in a multicenter patient population. Am. Health Drug Benefits 2016, 9, 497–502. [Google Scholar] [PubMed]
- Falzarano, S.M.; Ferro, M.; Bollito, E.; Klein, E.A.; Carrieri, G.; Magi-Galluzzi, C. Novel biomarkers and genomic tests in prostate cancer: A critical analysis. Ital. J. Urol. Nephrol. 2015, 67, 211–231. [Google Scholar]
- Bazzichetto, C.; Conciatori, F.; Pallocca, M.; Falcone, I.; Fanciulli, M.; Cognetti, F.; Milella, M.; Ciuffreda, L. PTEN as a prognostic/predictive biomarker in cancer: An unfulfilled promise? Cancers 2019, 11, 435. [Google Scholar] [CrossRef] [PubMed]
- Lotan, T.L.; Wei, W.; Ludkovski, O.; Morais, C.L.; Guedes, L.B.; Jamaspishvili, T.; Lopez, K.; Hawley, S.T.; Feng, Z.; Fazli, L.; et al. Analytic validation of a clinical-grade PTEN immunohistochemistry assay in prostate cancer by comparison with PTEN FISH. Mod. Pathol. 2016, 29, 904–914. [Google Scholar] [CrossRef]
- Kish, E.K.; Choudhry, M.; Gamallat, Y.; Buharideen, S.M.; Bismar, T.A. The expression of proto-oncogene ETS-related gene (ERG) plays a central role in the oncogenic mechanism involved in the development and progression of prostate cancer. Int. J. Mol. Sci. 2022, 23, 4772. [Google Scholar] [CrossRef]
- Krumbholz, M.; Agaimy, A.; Stoehr, R.; Burger, M.; Wach, S.; Taubert, H.; Wullich, B.; Hartmann, A.; Metzler, M. Molecular composition of genomic TMPRSS2-ERG rearrangements in prostate cancer. Dis. Markers 2019, 2019, 5085373. [Google Scholar] [CrossRef]
- Olleik, G.; Kassouf, W.; Aprikian, A.; Hu, J.; Vanhuyse, M.; Cury, F.; Peacock, S.; Bonnevier, E.; Dragomir, A. Evaluation of new tests and interventions for prostate cancer management: A systematic review. J. Natl. Compr. Cancer Netw. 2018, 16, 1340–1351. [Google Scholar] [CrossRef]
- Zhuang, L.; Johnson, M.T. How precisely can prostate cancer be managed? Int. Neurourol. J. 2016, 20 (Suppl. S2), S120–S130. [Google Scholar] [CrossRef]
- Visser, W.C.; de Jong, H.; Melchers, W.J.; Mulders, P.F.; Schalken, J.A. Commercialized blood-, urinary-and tissue-based biomarker tests for prostate cancer diagnosis and prognosis. Cancers 2020, 12, 3790. [Google Scholar] [CrossRef]
- Toribio-Vázquez, C.; Rivas, J.G.; Yebes, Á.; Carrión, D.M.; Barrado, M.Y.; Álvarez-Maestro, M.; Martinez-Piñeiro, L. New strategies for decision making in prostate cancer. The role of oncotypedx. Actas Urol. Esp. 2022, S2173–S5786. [Google Scholar] [CrossRef]
- Lone, Z.; Benidir, T.; Rainey, M.; Nair, M.; Davicioni, E.; Gibb, E.A.; Williamson, S.; Gupta, S.; Ornstein, M.C.; Tendulkar, R.; et al. Transcriptomic features of cribriform and intraductal carcinoma of the prostate. Eur. Urol. Focus. 2022, 8, 1575–1582. [Google Scholar] [CrossRef] [PubMed]
- Boström, P.J.; Bjartell, A.S.; Catto, J.W.; Eggener, S.E.; Lilja, H.; Loeb, S.; Schalken, J.; Schlomm, T.; Cooperberg, M.R. Genomic predictors of outcome in prostate cancer. Eur. Urol. 2015, 68, 1033–1044. [Google Scholar] [CrossRef] [PubMed]
- Khatami, F.; Aghamir, S.M.K.; Salmaninejad, A.; Shivarani, S.; Khorrami, M.H. Biomarkers for prostate cancer diagnosis from genetic perspectives. Transl. Res. Urol. 2020, 2, 51–58. [Google Scholar] [CrossRef]
- Carlsson, S.V.; Roobol, M.J. Improving the evaluation and diagnosis of clinically significant prostate cancer in 2017. Curr. Opin. Urol. 2017, 27, 198–204. [Google Scholar] [CrossRef] [PubMed]
- McGrowder, D.; Anderson-Jackson, L.; Dilworth, L.; Mohansingh, S.; Cross, M.A.; Bryan, S.; Miller, F.; Wilson-Clarke, C.; Nwokocha, C.; Alexander-Lindo, R.; et al. The clinical usefulness of prostate cancer biomarkers: Current and future directions. In Cancer Bioinformatics, 1st ed.; Kais, G., Hamdi, Y., Eds.; IntechOpen: London, UK, 2022; Volume 79, pp. 1–36. [Google Scholar] [CrossRef]
- Sun, Q.P.; Li, L.Y.; Chen, Z.; Pang, J.; Yang, W.J.; Zhou, X.F.; Qiu, J.G.; Su, Z.L.; He, D.; Gao, X. Detection of TMPRSS2-ETS fusions by a multiprobe fluorescence in situ hybridization assay for the early diagnosis of prostate cancer: A pilot study. J. Mol. Diagn. 2010, 12, 718–724. [Google Scholar] [CrossRef]
- Geybels, M.S.; Fang, M.; Wright, J.L.; Qu, X.; Bibikova, M.; Klotzle, B.; Fan, J.B.; Feng, Z.; Ostrander, E.A.; Nelson, P.S.; et al. PTEN loss is associated with prostate cancer recurrence and alterations in tumor DNA methylation profiles. Oncotarget 2017, 8, 84338–84348. [Google Scholar] [CrossRef]
- Alarcón-Zendejas, A.P.; Scavuzzo, A.; Jiménez-Ríos, M.A.; Álvarez-Gómez, R.M.; Montiel-Manríquez, R.; Castro-Hernández, C.; Jiménez-Dávila, M.A.; Pérez-Montiel, D.; González-Barrios, R.; Jiménez-Trejo, F.; et al. The promising role of new molecular biomarkers in prostate cancer: From coding and non-coding genes to artificial intelligence approaches. Prostate Cancer Prostatic Dis. 2022, 25, 431–443. [Google Scholar] [CrossRef]
- Alam, S.; Tortora, J.; Staff, I.; McLaughlin, T.; Wagner, J. Prostate cancer genomics: Comparing results from three molecular assays. Can. J. Urol. 2019, 26, 9758–9762. [Google Scholar]
- Health Quality Ontario. Prolaris Cell Cycle Progression Test for Localized Prostate Cancer: A Health Technology Assessment. Ont. Health Technol. Assess. Ser. 2017, 17, 1–75. [Google Scholar]
- Brawer, M.K.; Cuzick, J.M.; Cooperberg, M.R.; Swanson, G.P.; Freedland, S.J.; Reid, J.E.; Fisher, G.; Lanchbury, J.S.; Gutin, A.; Stone, S.; et al. Prolaris: A novel genetic test for prostate cancer prognosis. J. Clin. Oncol. 2013, 15, 5005. [Google Scholar] [CrossRef]
- Murphy, A.B.; Carbunaru, S.; Nettey, O.S.; Gornbein, C.; Dixon, M.A.; Macias, V.; Sharifi, R.; Kittles, R.A.; Yang, X.; Kajdacsy-Balla, A.; et al. A 17-gene panel genomic prostate score has similar predictive accuracy for adverse pathology at radical prostatectomy in African American and European American Men. Urology 2020, 142, 166–173. [Google Scholar] [CrossRef] [PubMed]
- Basourakos, S.P.; Tzeng, M.; Lewicki, P.J.; Patel, K.; Awamlh, B.A.H.A.; Venkat, S.; Shoag, J.E.; Gorin, M.A.; Barbieri, C.E.; Hu, J.C. Tissue-based biomarkers for the risk stratification of men with clinically localized prostate cancer. Front. Oncol. 2021, 11, 676716. [Google Scholar] [CrossRef] [PubMed]
- Marrone, M.; Potosky, A.L.; Penson, D.; Freedman, A.N. A 22 gene-expression assay, Decipher® (GenomeDx Biosciences) to predict five-year risk of metastatic prostate cancer in men treated with radical prostatectomy. PLoS Curr. 2015, 7. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kruse, E.; Uehlein, N.; Kaldenhoff, R. The aquaporins. Genome Biol. 2006, 7, 206. [Google Scholar] [CrossRef] [PubMed]
- Zannetti, A.; Benga, G.; Brunetti, A.; Napolitano, F.; Avallone, L.; Pelagalli, A. Role of aquaporins in the physiological functions of mesenchymal stem cells. Cells 2020, 9, 2678. [Google Scholar] [CrossRef] [PubMed]
- Pelagalli, A.; Squillacioti, C.; Mirabella, N.; Meli, R. Aquaporins in health and disease: An overview focusing on the gut of different species. Int. J. Mol. Sci. 2016, 17, 1213. [Google Scholar] [CrossRef]
- King, L.S.; Kozono, D.; Agre, P. From structure to disease: The evolving tale of aquaporin biology. Nat. Rev. Mol. Cell Biol. 2004, 5, 687–698. [Google Scholar] [CrossRef]
- Ma, T.; Yang, B.; Gillespie, A.; Carlson, E.J.; Epstein, C.J.; Verkman, A.S. Severely impaired urinary concentrating ability in transgenic mice lacking aquaporin-1 water channels. J. Biol. Chem. 1998, 273, 4296–4299. [Google Scholar] [CrossRef]
- Rash, J.E.; Yasumura, T.; Hudson, C.S.; Agre, P.; Nielsen, S. Direct immunogold labeling of aquaporin-4 in square arrays of astrocyte and ependymocyte plasma membranes in rat brain and spinal cord. Proc. Natl. Acad. Sci. USA 1998, 95, 11981–11986. [Google Scholar] [CrossRef]
- Smith, A.J.; Jin, B.J.; Ratelade, J.; Verkman, A.S. Aggregation state determines the localization and function of M1-and M23-aquaporin-4 in astrocytes. J. Cell. Biol. 2014, 204, 559–573. [Google Scholar] [CrossRef]
- Verkman, A.S.; Ratelade, J.; Rossi, A.; Zhang, H.; Tradtrantip, L. Aquaporin-4: Orthogonal array assembly, CNS functions, and role in neuromyelitis optica. Acta Pharmacol. Sin. 2011, 32, 702–710. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Yang, B. Aquaporins in renal diseases. Int. J. Mol. Sci. 2019, 20, 366. [Google Scholar] [CrossRef] [PubMed]
- Calamita, G.; Perret, J.; Delporte, C. Aquaglyceroporins: Drug targets for metabolic diseases? Front. Physiol. 2018, 9, 851. [Google Scholar] [CrossRef] [PubMed]
- Mukhopadhyay, R.; Bhattacharjee, H.; Rosen, B.P. Aquaglyceroporins: Generalized metalloid channels. Biochim. Biophys. Acta Gen. Subj. 2014, 1840, 1583–1591. [Google Scholar] [CrossRef] [PubMed]
- Borgnia, M.; Nielsen, S.; Engel, A.; Agre, P. Cellular and molecular biology of the aquaporin water channels. Annu. Rev. Biochem. 1999, 68, 425–458. [Google Scholar] [CrossRef]
- Yang, B.; Verkman, A.S. Water and glycerol permeabilities of aquaporins 1–5 and MIP determined quantitatively by expression of epitope-tagged constructs in Xenopus oocytes. J. Biol. Chem. 1997, 272, 16140–16146. [Google Scholar] [CrossRef]
- Li, S.; Li, C.; Wang, W. Molecular aspects of aquaporins. Vitam. Horm. 2020, 113, 129–181. [Google Scholar] [CrossRef]
- Tsukaguchi, H.; Weremowicz, S.; Morton, C.C.; Hediger, M.A. Functional and molecular characterization of the human neutral solute channel aquaporin-9. Am. J. Physiol. Ren. Physiol. 1999, 277, F685–F696. [Google Scholar] [CrossRef]
- Ishibashi, K. Aquaporin subfamily with unusual NPA boxes. Biochim. Biophys. Acta Biomembr. 2006, 1758, 989–993. [Google Scholar] [CrossRef]
- Yang, B. Aquaporins, 1st ed.; Springer: Dordrecht, The Netherlands, 2017; pp. 1–277. [Google Scholar] [CrossRef]
- Dajani, S.; Saripalli, A.; Sharma-Walia, N. Water transport proteins–aquaporins (AQPs) in cancer biology. Oncotarget 2018, 9, 36392–36405. [Google Scholar] [CrossRef]
- Simone, L.; Gargano, C.D.; Pisani, F.; Cibelli, A.; Mola, M.G.; Frigeri, A.; Svelto, M.; Nicchia, G.P. Aquaporin-1 inhibition reduces metastatic formation in a mouse model of melanoma. J. Cell. Mol. Med. 2018, 22, 904–912. [Google Scholar] [CrossRef] [PubMed]
- Zou, L.B.; Shi, S.; Zhang, R.J.; Wang, T.T.; Tan, Y.J.; Zhang, D.; Fei, X.Y.; Ding, G.L.; Gao, Q.; Chen, C.; et al. Aquaporin-1 plays a crucial role in estrogen-induced tubulogenesis of vascular endothelial cells. J. Clin. Endocr. Metab. 2013, 98, E672–E682. [Google Scholar] [CrossRef] [PubMed]
- Milković, L.; Čipak Gašparović, A. AQP3 and AQP5-potential regulators of redox status in breast cancer. Molecules 2021, 26, 2613. [Google Scholar] [CrossRef] [PubMed]
- De Ieso, M.L.; Yool, A.J. Mechanisms of aquaporin-facilitated cancer invasion and metastasis. Front. Chem. 2018, 6, 135. [Google Scholar] [CrossRef] [PubMed]
- Chow, P.H.; Bowen, J.; Yool, A.J. Combined systematic review and transcriptomic analyses of mammalian aquaporin classes 1 to 10 as biomarkers and prognostic indicators in diverse cancers. Cancers 2020, 12, 1911. [Google Scholar] [CrossRef]
- Liu, S.; Zhang, S.; Jiang, H.; Yang, Y.; Jiang, Y. Co-expression of AQP3 and AQP5 in esophageal squamous cell carcinoma correlates with aggressive tumor progression and poor prognosis. Med. Oncol. 2013, 30, 636. [Google Scholar] [CrossRef]
- Ismail, M.; Bokaee, S.; Davies, J.; Harrington, K.J.; Pandha, H. Inhibition of the aquaporin 3 water channel increases the sensitivity of prostate cancer cells to cryotherapy. Br. J. Cancer 2009, 100, 1889–1895. [Google Scholar] [CrossRef]
- Wang, J.; Feng, L.; Zhu, Z.; Zheng, M.; Wang, D.; Chen, Z.; Sun, H. Aquaporins as diagnostic and therapeutic targets in cancer: How far we are? J. Transl. Med. 2015, 13, 96. [Google Scholar] [CrossRef]
- Zhu, L.; Ma, N.; Wang, B.; Wang, L.; Zhou, C.; Yan, Y.; He, J.; Ren, Y. Significant prognostic values of aquaporin mRNA expression in breast cancer. Cancer Manag. Res. 2019, 11, 1503–1515. [Google Scholar] [CrossRef]
- Wang, H.; Zhang, W.; Ding, Z.; Xu, T.; Zhang, X.; Xu, K. Comprehensive exploration of the expression and prognostic value of AQPs in clear cell renal cell carcinoma. Medicine 2022, 101, e29344. [Google Scholar] [CrossRef]
- Abdelrahman, A.E.; Fathy, A.; Elsebai, E.A.; Nawar, N.; Etman, W.M. Prognostic impact of Apaf-1, Cyclin D1, and AQP-5 in serous ovarian carcinoma treated with the first-line chemotherapy. Ann. Diagn. Pathol. 2018, 35, 27–37. [Google Scholar] [CrossRef]
- Bellezza, G.; Vannucci, J.; Bianconi, F.; Metro, G.; Del Sordo, R.; Andolfi, M.; Ferri, I.; Siccu, P.; Ludovini, V.; Puma, F.; et al. Prognostic implication of aquaporin 1 overexpression in resected lung adenocarcinoma. Interact. Cardiovasc. Thorac. Surg. 2017, 25, 856–861. [Google Scholar] [CrossRef]
- Tie, L.; Lu, N.; Pan, X.Y.; Pan, Y.; An, Y.; Gao, J.W.; Lin, Y.H.; Yu, H.M.; Li, X.J. Hypoxia-induced up-regulation of aquaporin-1 protein in prostate cancer cells in a p38-dependent manner. Cell. Physiol. Biochem. 2012, 29, 269–280. [Google Scholar] [CrossRef] [PubMed]
- Mobasheri, A.; Airley, R.; Hewitt, S.M.; Marples, D. Heterogeneous expression of the aquaporin 1 (AQP1) water channel in tumors of the prostate, breast, ovary, colon and lung: A study using high density multiple human tumor tissue microarrays. Int. J. Oncol. 2005, 26, 1149–1158. [Google Scholar] [CrossRef] [PubMed]
- Hwang, I.; Jung, S.I.; Hwang, E.C.; Song, S.H.; Lee, H.S.; Kim, S.O.; Kang, T.W.; Kwon, D.; Park, K. Expression and localization of aquaporins in benign prostate hyperplasia and prostate cancer. Chonnam Med. J. 2012, 48, 174–178. [Google Scholar] [CrossRef]
- Morrissey, J.J.; London, A.N.; Lambert, M.C.; Kharasch, E.D. Sensitivity and specificity of urinary neutrophil gelatinase-associated lipocalin and kidney injury molecule-1 for the diagnosis of renal cell carcinoma. Am. J. Nephrol. 2011, 34, 391–398. [Google Scholar] [CrossRef]
- Arnaoutova, I.; Cawley, N.X.; Patel, N.; Kim, T.; Rathod, T.; Loh, Y.P. Aquaporin 1 is important for maintaining secretory granule biogenesis in endocrine cells. Mol. Endocrinol. 2008, 22, 1924–1934. [Google Scholar] [CrossRef][Green Version]
- Bullock, A.F.; Greenley, S.L.; McKenzie, G.A.; Paton, L.W.; Johnson, M.J. Relationship between markers of malnutrition and clinical outcomes in older adults with cancer: Systematic review, narrative synthesis and meta-analysis. Eur. J. Clin. Nutr. 2020, 74, 1519–1535. [Google Scholar] [CrossRef] [PubMed]
- Furman, D.; Campisi, J.; Verdin, E.; Carrera-Bastos, P.; Targ, S.; Franceschi, C.; Ferrucci, L.; Gilroy, D.W.; Fasano, A.; Miller, G.W.; et al. Chronic inflammation in the etiology of disease across the life span. Nat. Med. 2019, 25, 1822–1832. [Google Scholar] [CrossRef] [PubMed]
- Portela, L.M.; Santos, S.A.; Constantino, F.B.; Camargo, A.C.; Colombelli, K.T.; Fioretto, M.N.; Barquilha, C.N.; Périco, L.L.; Hiruma-Lima, C.A.; Scarano, W.R.; et al. Increased oxidative stress and cancer biomarkers in the ventral prostate of older rats submitted to maternal malnutrition. Mol. Cell. Endocrinol. 2021, 523, 111148. [Google Scholar] [CrossRef]
- Park, J.Y.; Yoon, G. Overexpression of aquaporin-1 is a prognostic factor for biochemical recurrence in prostate adenocarcinoma. Pathol. Oncol. Res. 2017, 23, 189–196. [Google Scholar] [CrossRef]
- Ribatti, D.; Ranieri, G.; Annese, T.; Nico, B. Aquaporins in cancer. Biochim. Biophys. Acta Gen. Subj. 2014, 1840, 1550–1553. [Google Scholar] [CrossRef] [PubMed]
- Li, A.; Lu, D.; Zhang, Y.; Li, J.; Fang, Y.; Li, F.; Sun, J. Critical role of aquaporin-3 in epidermal growth factor-induced migration of colorectal carcinoma cells and its clinical significance. Oncol. Rep. 2013, 29, 535–540. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.L.; Matsuzaki, T.; Nakazawa, T.; Murata, S.; Nakamura, N.; Kondo, T.; Iwashina, M.; Mochizuki, K.; Yamane, T.; Takata, K.; et al. Expression of aquaporin 3 (AQP3) in normal and neoplastic lung tissues. Hum. Pathol. 2007, 38, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Machida, Y.; Ueda, Y.; Shimasaki, M.; Sato, K.; Sagawa, M.; Katsuda, S.; Sakuma, T. Relationship of aquaporin 1, 3, and 5 expression in lung cancer cells to cellular differentiation, invasive growth, and metastasis potential. Hum. Pathol. 2011, 42, 669–678. [Google Scholar] [CrossRef] [PubMed]
- Kusayama, M.; Wada, K.; Nagata, M.; Ishimoto, S.; Takahashi, H.; Yoneda, M.; Nakajima, A.; Okura, M.; Kogo, M.; Kamisaki, Y. Critical role of aquaporin 3 on growth of human esophageal and oral squamous cell carcinoma. Cancer Sci. 2011, 102, 1128–1136. [Google Scholar] [CrossRef]
- Chen, J.; Wang, Z.; Xu, D.; Liu, Y.; Gao, Y. Aquaporin 3 promotes prostate cancer cell motility and invasion via extracellular signal-regulated kinase 1/2-mediated matrix metalloproteinase-3 secretion. Mol. Med. Rep. 2015, 11, 2882–2888. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Tanji, N.; Kikugawa, T.; Shudou, M.; Song, X.; Yokoyama, M. Expression of aquaporin 3 in the human prostate. Int. J. Urol. 2007, 14, 1088–1092. [Google Scholar] [CrossRef] [PubMed]
- Nejsum, L.N.; Nelson, W.J. A molecular mechanism directly linking E-cadherin adhesion to initiation of epithelial cell surface polarity. J. Cell. Biol. 2007, 178, 323–335. [Google Scholar] [CrossRef]
- Chen, Q.; Zhu, L.; Zong, H.; Song, X.; Wang, L.; Wang, X.; Yanh, D.; Wang, J. Subcellular localization of aquaporin 3 in prostate cancer is regulated by RalA. Oncol. Rep. 2018, 39, 2171–2177. [Google Scholar] [CrossRef]
- de Almeida, A.; Parthimos, D.; Dew, H.; Smart, O.; Wiltshire, M.; Errington, R.J. Aquaglyceroporin-3’s expression and cellular localization is differentially modulated by hypoxia in prostate cancer cell lines. Cells 2021, 10, 838. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.; Ricciardelli, C.; Yool, A.J. Targeting aquaporins in novel therapies for male and female breast and reproductive cancers. Cells 2021, 10, 215. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.K.; Chae, Y.K.; Woo, J.; Kim, M.S.; Park, J.C.; Lee, J.; Soria, J.C.; Jang, S.J.; Sidransky, D.; Moon, C. Role of human aquaporin 5 in colorectal carcinogenesis. Am. J. Pathol. 2008, 173, 518–525. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Li, Q.; Yang, T.; Bai, G.; Li, D.; Li, Q.; Sun, H. Expression of AQP5 and AQP8 in human colorectal carcinoma and their clinical significance. World J. Surg. Oncol. 2012, 10, 242. [Google Scholar] [CrossRef] [PubMed]
- Chae, Y.K.; Woo, J.; Kim, M.J.; Kang, S.K.; Kim, M.S.; Lee, J.; Lee, S.K.; Gong, G.; Kim, Y.H.; Soria, J.C.; et al. Expression of aquaporin 5 (AQP5) promotes tumor invasion in human non-small cell lung cancer. PLoS ONE 2008, 3, e2162. [Google Scholar] [CrossRef]
- Zhang, T.; Zhao, C.; Chen, D.; Zhou, Z. Overexpression of AQP5 in cervical cancer: Correlation with clinicopathological features and prognosis. Med. Oncol. 2012, 29, 1998–2004. [Google Scholar] [CrossRef]
- Chae, Y.K.; Kang, S.K.; Kim, M.S.; Woo, J.; Lee, J.; Chang, S.; Kim, D.W.; Kim, M.; Park, S.; Kim, I.; et al. Human AQP5 plays a role in the progression of chronic myelogenous leukemia (CML). PLoS ONE 2008, 3, e2594. [Google Scholar] [CrossRef]
- Yan, C.; Zhu, Y.; Zhang, X.; Chen, X.; Zheng, W.; Yang, J. Down-regulated aquaporin 5 inhibits proliferation and migration of human epithelial ovarian cancer 3AO cells. J. Ovarian Res. 2014, 7, 78. [Google Scholar] [CrossRef]
- Guo, X.; Sun, T.; Yang, M.; Li, Z.; Li, Z.; Gao, Y. Prognostic value of combined aquaporin 3 and aquaporin 5 overexpression in hepatocellular carcinoma. BioMed Res. Int. 2013, 2013, 206525. [Google Scholar] [CrossRef]
- Pust, A.; Kylies, D.; Hube-Magg, C.; Kluth, M.; Minner, S.; Koop, C.; Grob, T.; Graefen, M.; Salomon, G.; Tsourlakis, M.C.; et al. Aquaporin 5 expression is frequent in prostate cancer and shows a dichotomous correlation with tumor phenotype and PSA recurrence. Hum. Pathol. 2016, 48, 102–110. [Google Scholar] [CrossRef]
- Li, J.; Wang, Z.; Chong, T.; Chen, H.; Li, H.; Li, G.; Zhai, X.; Li, Y. Over-expression of a poor prognostic marker in prostate cancer: AQP5 promotes cells growth and local invasion. World J. Surg. Oncol. 2014, 12, 284. [Google Scholar] [CrossRef] [PubMed]
- Lindskog, C.; Asplund, A.; Catrina, A.; Nielsen, S.; Rützler, M. A systematic characterization of aquaporin-9 expression in human normal and pathological tissues. J. Histochem. Cytochem. 2016, 64, 287–300. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Tanji, N.; Sasaki, T.; Kikugawa, T.; Song, X.; Yokoyama, M. Androgens upregulate aquaporin 9 expression in the prostate. Int. J. Urol. 2008, 15, 936–941. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.; Zhu, L.; Zheng, B.; Wang, J.; Song, X.; Zheng, W.; Wang, L.; Yang, D.; Wang, J. Effect of AQP9 expression in androgen-independent prostate cancer cell PC3. Int. J. Mol. Sci. 2016, 17, 738. [Google Scholar] [CrossRef]
- Bründl, J.; Wallinger, S.; Breyer, J.; Weber, F.; Evert, M.; Georgopoulos, N.T.; Rosenhammer, B.; Burger, M.; Otto, W.; Rubenwolf, P. Expression, localisation and potential significance of aquaporins in benign and malignant human prostate tissue. BMC Urol. 2018, 18, 75. [Google Scholar] [CrossRef]
- Pan, X.Y.; Guo, H.; Han, J.; Hao, F.; An, Y.; Xu, Y.; Xiaokaiti, Y.; Pan, Y.; Li, X.J. Ginsenoside Rg3 attenuates cell migration via inhibition of aquaporin 1 expression in PC-3M prostate cancer cells. Eur. J. Pharmacol. 2012, 683, 27–34. [Google Scholar] [CrossRef]
- Siu, M.K.; Suau, F.; Chen, W.Y.; Tsai, Y.C.; Tsai, H.Y.; Yeh, H.L.; Liu, Y. KLF4 functions as an activator of the androgen receptor through reciprocal feedback. Oncogenesis 2016, 5, e282. [Google Scholar] [CrossRef]
- Liu, C.; Sheng, M.; Lin, L.; Li, H.; Guo, S.; Zhang, J.; Chen, G.; Chen, H. NANOG regulates the proliferation of PCSCs via the TGF-β1/SMAD pathway. Open Med. 2020, 15, 841–849. [Google Scholar] [CrossRef]
- Cackowski, F.C.; Heath, E.I. Prostate cancer dormancy and recurrence. Cancer Lett. 2022, 524, 103–108. [Google Scholar] [CrossRef]
- Park, S.H.; Fong, K.W.; Mong, E.; Martin, M.C.; Schiltz, G.E.; Yu, J. Going beyond polycomb: EZH2 functions in prostate cancer. Oncogene 2021, 40, 5788–5798. [Google Scholar] [CrossRef]

| Category | Commercially Available Tests | Limitations | Ref. |
|---|---|---|---|
| Discriminate aggressive vs. indolent prostate tumors | ConfirmMDx | Additional insights/test/biopsy is needed surrounding high-grade prostate cancer tissue after diagnosis in methylation positive patients. | [10,11] |
| Prostate Core Mitomic Test | False negative results in spite high sensitivity, comparable to other biomarker tests. | [12,13] | |
| Phosphatase and tensin homolog (PTEN) gene | Impact in the detection of prostate cancer due to heterogenic behavior and PTEN alterations. | [14,15] | |
| TMPRSS2-ERG gene fusion | Time-consuming test that requires costly equipment, thus limiting its use in clinical diagnostics. | [16,17] | |
| ProMark | Biopsy-based test limited to bleeding complication and miss the high-risk areas of prostate tumor. | [18,19] | |
| Improve risk stratification of patients with prostate cancer | Prolaris | Biopsy based test with high probability of missing the high-risk areas of prostate cancer. | [20] |
| Oncotype DX | Test not designed to take racial discrimination in account. | [19,21] | |
| Decipher | Estimate patient risk and influence treatment decisions. It is time taking test with a limitation to require 10 year or more to complete. | [22,23] |
| AQPs | Cell Lines/Tissue | Methodology | AQPs Expression | Results | Ref. |
|---|---|---|---|---|---|
| AQP1 | PC-3M | shRNA | Down | Inhibits cell migration | [99] |
| AQP1 | PC-3M | Density-induced pericellular hypoxia and CoCl(2)-induced hypoxia | Up | Hypoxia induces AQP1 mRNA levels via intracellular Ca2+, protein kinase C and p38 MAPK signaling pathways. | [66] |
| AQP3 | PC3 | Stable knockdown of RalA and overexpression of E-cadherin | Up | AQP3 redistribution inhibits the cell proliferation, enhance cell apoptosis, and suppress motility/invasion. | [83] |
| DU-145, PC-3 | AQP3-siRNA silencing | Down | Reduces ERK1/2 activation. Inhibited motility/invasion. | [80] | |
| PC-3, DU145 | Cryotherapy of prostate cancer cells, HgCl2 as AQP3 inhibitor and AQP3-siRNA silencing | Down | Inhibition of AQP3 increases the sensitivity of prostate cancer cells to cryotherapy. | [60] | |
| PC-3, DU145, LNCaP, PNT1A Prostate cancer and normal tissue | RT-PCR, IHC | Up | Play a regulatory role in epithelial cell osmolality. Change in the localization of AQP3 in cancer cells as a result of tumorigenesis. | [81] | |
| AQP5 | PC-3, LNCaP | AQP5-siRNA | Down | Cell proliferation and migration attenuated. | [94] |
| Prostate cancer, prostate epithelium | IHC on a tissue array (n = 12,427) | Weak to moderate expression in normal prostate epithelium. Either negative or high expression in prostate cancer | Dichotomous role of AQP5 observed. | [93] | |
| HPrEC, PC-3, DU145, LNCaP | Immunofluorescence | Up | Differential expression of AQP5 in benign and malignant prostate tissue. | [98] | |
| AQP9 | PC-3 Prostate cancer, adjacent tissue | AQP9-siRNA, Western blot, Flow cytometry | Down | Promote apoptosis. Suppressed ERK1/2 phosphorylation, inhibits proliferation, affects the cell motility/invasiveness. | [97] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kushwaha, P.P.; Verma, S.; Gupta, S. Aquaporins as Prognostic Biomarker in Prostate Cancer. Cancers 2023, 15, 331. https://doi.org/10.3390/cancers15020331
Kushwaha PP, Verma S, Gupta S. Aquaporins as Prognostic Biomarker in Prostate Cancer. Cancers. 2023; 15(2):331. https://doi.org/10.3390/cancers15020331
Chicago/Turabian StyleKushwaha, Prem Prakash, Shiv Verma, and Sanjay Gupta. 2023. "Aquaporins as Prognostic Biomarker in Prostate Cancer" Cancers 15, no. 2: 331. https://doi.org/10.3390/cancers15020331
APA StyleKushwaha, P. P., Verma, S., & Gupta, S. (2023). Aquaporins as Prognostic Biomarker in Prostate Cancer. Cancers, 15(2), 331. https://doi.org/10.3390/cancers15020331








