Changing Patterns in Cancer Mortality from 1987 to 2020 in China
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
3. Results
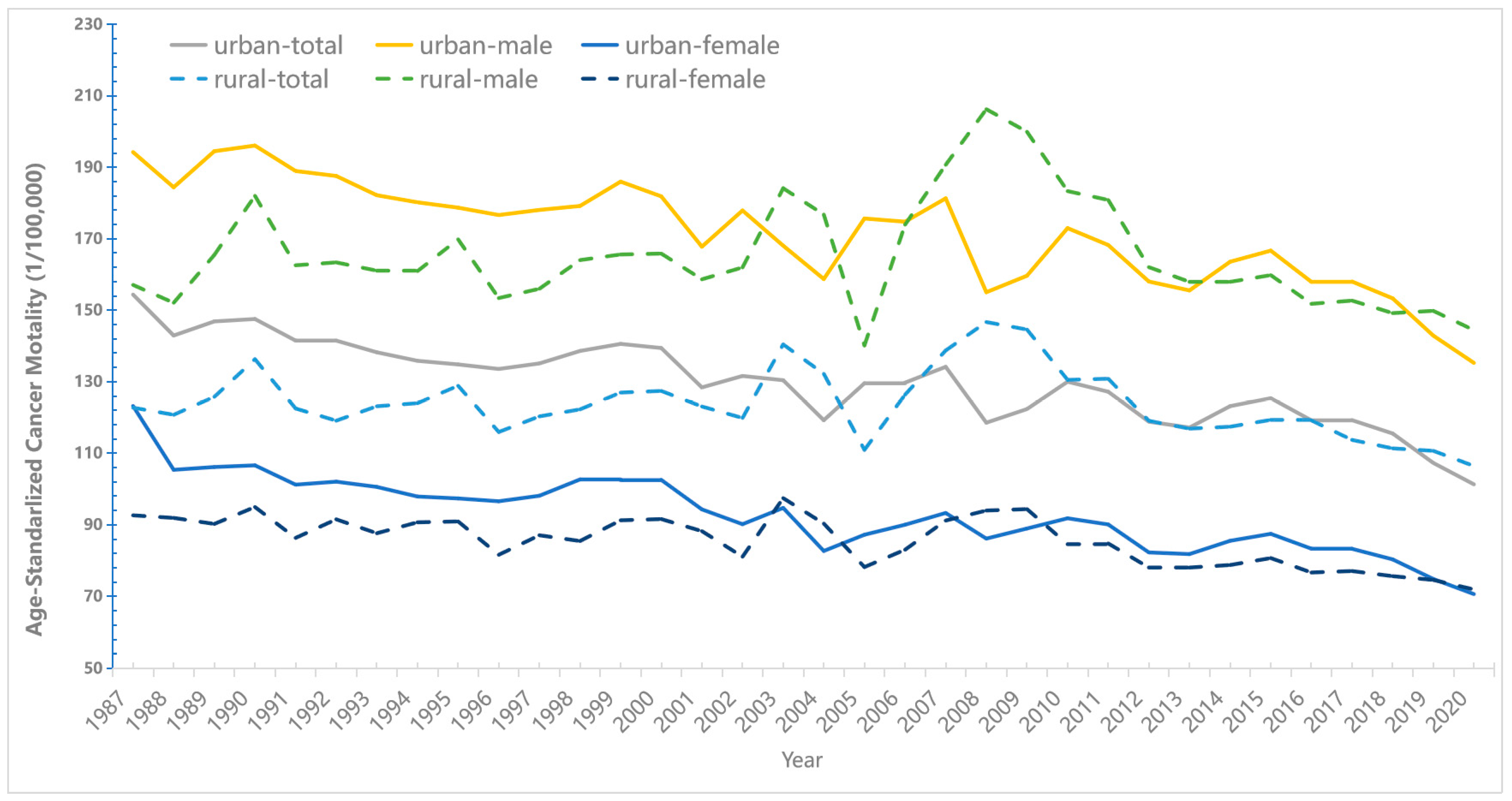
3.1. Long-Term Trends in Cancers Mortality between1987 and 2020
3.2. The Overall and Age-Specific Annual Percentage Change of Cancer Mortality
3.3. Age-Period-Cohort Effects on Cancer Mortality
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Chen, W.; Zheng, R.; Baade, P.D.; Zhang, S.; Zeng, H.; Bray, F.; Jemal, A.; Yu, X.Q.; He, J. Cancer statistics in China, 2015. CA Cancer J. Clin. 2016, 66, 115–132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Zheng, R.; Zhang, S.; Zeng, H.; Wang, S.; Sun, K.; Chen, R.; Li, L.; Wei, W.; He, J. Cancer incidence and mortality in China, 2016. J. Natl. Cancer Cent. 2022, 2, 1–9. [Google Scholar] [CrossRef]
- Sun, D.; Cao, M.; Li, H.; He, S.; Chen, W. Cancer burden and trends in China: A review and comparison with Japan and South Korea. Chin. J. Cancer Res. 2020, 32, 129–139. [Google Scholar] [CrossRef]
- Zhou, M.; Wang, H.; Zeng, X.; Yin, P.; Zhu, J.; Chen, W.; Li, X.; Wang, L.; Wang, L.; Liu, Y.; et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 394, 1145–1158. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, D.; Li, H.; Cao, M.; He, S.; Lei, L.; Peng, J.; Chen, W. Cancer burden in China: Trends, risk factors and prevention. Cancer Biol. Med. 2020, 17, 879. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Lu, F.; Zhang, S. [Analysis of cancer modality and distribution in China from year 1990 through 1992—An epidemiologic study]. Zhonghua Zhong Liu Za Zhi 1996, 18, 403–407. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qiu, H.; Cao, S.; Xu, R. Cancer incidence, mortality, and burden in China: A time-trend analysis and comparison with the United States and United Kingdom based on the global epidemiological data released in 2020. Cancer Commun. 2021, 41, 1037–1048. [Google Scholar] [CrossRef]
- Hanley, A.J.; Choi, B.C.; Holowaty, E.J. Cancer mortality among Chinese migrants: A review. Int. J. Epidemiol. 1995, 24, 255–265. [Google Scholar] [CrossRef]
- Yang, D.; Liu, Y.; Bai, C.; Wang, X.; Powell, C.A. Epidemiology of lung cancer and lung cancer screening programs in China and the United States. Cancer Lett. 2020, 468, 82–87. [Google Scholar] [CrossRef]
- Fang, J.-Y.; Dong, H.-L.; Wu, K.-S.; Du, P.-L.; Xu, Z.-X.; Lin, K. Characteristics and prediction of lung cancer mortality in China from 1991 to 2013. Asian Pac. J. Cancer Prev. 2015, 16, 5829–5834. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lei, S.; Zheng, R.; Zhang, S.; Wang, S.; Chen, R.; Sun, K.; Zeng, H.; Zhou, J.; Wei, W. Global patterns of breast cancer incidence and mortality: A population-based cancer registry data analysis from 2000 to 2020. Cancer Commun. 2021, 41, 1183–1194. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Cao, F.; Zhang, G.; Shi, L.; Chen, S.; Zhang, Z.; Zhi, W.; Ma, T. Trends in and predictions of colorectal cancer incidence and mortality in China from 1990 to 2025. Front. Oncol. 2019, 9, 98. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Zheng, R.; Wang, N.; Yuan, Y.; Liu, S.; Li, H.; Zhang, S.; Zeng, H.; Chen, W. Incidence and mortality of stomach cancer in China, 2014. Chin. J. Cancer Res. 2018, 30, 291. [Google Scholar] [CrossRef] [PubMed]
- Jinyao, W.; Nianping, Z.; Zhiqiang, B.; Zhenkun, W. Age-Period-Cohort Analysis of Secular Trends of Cervical Cancer Incidence and Mortality in China, 1993—2017. Chin. Gen. Pract. 2022, 25, 1564–1568. [Google Scholar] [CrossRef]
- Shi, J.F.; Canfell, K.; Lew, J.B.; Qiao, Y.L. The burden of cervical cancer in China: Synthesis of the evidence. Int. J. Cancer 2012, 130, 641–652. [Google Scholar] [CrossRef] [PubMed]
- Guo, P.; Huang, Z.L.; Yu, P.; Li, K. Trends in cancer mortality in China: An update. Ann. Oncol. 2012, 23, 2755–2762. [Google Scholar] [CrossRef]
- Yang, L.; Parkin, D.M.; Li, L.; Chen, Y. Time trends in cancer mortality in China: 1987–1999. Int. J. Cancer 2003, 106, 771–783. [Google Scholar] [CrossRef]
- Liu, Q.; Wang, B.; Kong, Y.; Cheng, K.K. China’s primary health-care reform. Lancet 2011, 377, 2064–2066. [Google Scholar] [CrossRef]
- Xinhua. China’s GDP Tops 100 Trillion Yuan in 2020. Available online: http://www.ecns.cn/news/2021-01-18/detail-ihafurte1836008.shtml (accessed on 10 October 2022).
- Feng, R.M.; Zong, Y.N.; Cao, S.M.; Xu, R.H. Current cancer situation in China: Good or bad news from the 2018 Global Cancer Statistics? Cancer Commun. 2019, 39, 1–12. [Google Scholar] [CrossRef]
- Cai, Y.; Cui, X.; Su, B.B.; Wu, S.Y. Changes in Mortality Rates of Major Chronic Diseases Among Populations Aged Over 60 Years and Their Contributions to Life Expectancy Increase—China, 2005–2020. China Cdc Weekly 2022, 4, 866. [Google Scholar] [CrossRef] [PubMed]
- Yue, C.; Shiyong, W.; Xiaoxu, W.; Ruixian, W.; Wenling, Z. Improving the Quality of Vital Registration Data Through Multi-source Data Comparison. Chin. J. Health Stat. 2022, 39, 2–6. [Google Scholar] [CrossRef]
- Ahmad, O.B.; Pinto, C.B. Age Standardization of Rates: A New WHO Standard. Available online: https://www.researchgate.net/publication/284696312 (accessed on 2 October 2022).
- National Cancer Institute. Joinpoint Trend Analysis Software Version 4.9.1.0. Available online: https://surveillance.cancer.gov/joinpoint/ (accessed on 11 April 2022).
- Zou, Z.; Cini, K.; Dong, B.; Ma, Y.; Ma, J.; Burgner, D.P.; Patton, G.C. Time trends in cardiovascular disease mortality across the BRICS: An age-period-cohort analysis of key nations with emerging economies using the global burden of disease study 2017. Circulation 2020, 141, 790–799. [Google Scholar] [CrossRef] [PubMed]
- Condon, J.R.; Cunningham, J.; Barnes, T.; Armstrong, B.K. Long-term trends in cancer mortality for Indigenous Australians in the Northern Territory. Med. J. Aust. 2004, 180, 504–507. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rosenberg, P.S.; Check, D.P.; Anderson, W.F. A Web Tool for Age–Period–Cohort Analysis of Cancer Incidence and Mortality RatesSoftware for Cancer Rates and Trends. Cancer Epidemiol. Biomark. Prev. 2014, 23, 2296–2302. [Google Scholar] [CrossRef] [Green Version]
- Qi, H.; Xi, X. Why has China’s urbanization deviated from the goal of narrowing the urban-rural gap?—An analysis of the differences based on different stages of China’s economic development. Nanjing Soc. Sci. 2015, 4, 7–14. [Google Scholar] [CrossRef]
- The Central People’s Government of China. National Disposable Income per Capita in 2020. Available online: http://www.gov.cn/guoqing/2021-04/09/content_5598662.htm (accessed on 6 October 2022).
- Oberg, M.; Jaakkola, M.; Woodward, A.; Peruga, A.; Prüss-Ustün, A. Worldwide burden of disease from exposure to second-hand smoke: A retrospective analysis of data from 192 countries. Lancet 2011, 377, 139–146. [Google Scholar] [CrossRef] [PubMed]
- Hamra, G.B.; Guha, N.; Cohen, A.; Laden, F.; Raaschou-Nielsen, O.; Samet, J.M.; Vineis, P.; Forastiere, F.; Saldiva, P.; Yorifuji, T. Outdoor particulate matter exposure and lung cancer: A systematic review and meta-analysis. Environ. Health Perspect. 2014, 122, A236. [Google Scholar] [CrossRef] [Green Version]
- Loomis, D.; Grosse, Y.; Lauby-Secretan, B.; El Ghissassi, F.; Bouvard, V.; Benbrahim-Tallaa, L.; Guha, N.; Baan, R.; Mattock, H.; Straif, K. The carcinogenicity of outdoor air pollution. Lancet Oncol. 2013, 14, 1262. [Google Scholar] [CrossRef]
- Chen, J.G.; Zhang, S.W. Liver cancer epidemic in China: Past, present and future. Semin. Cancer Biol. 2011, 21, 59–69. [Google Scholar] [CrossRef]
- Tanaka, M.; Katayama, F.; Kato, H.; Tanaka, H.; Wang, J.; Qiao, Y.L.; Inoue, M. Hepatitis B and C virus infection and hepatocellular carcinoma in China: A review of epidemiology and control measures. J. Epidemiol. 2011, 21, 1110190266. [Google Scholar] [CrossRef] [Green Version]
- Balakrishnan, M.; George, R.; Sharma, A.; Graham, D.Y. Changing trends in stomach cancer throughout the world. Curr. Gastroenterol. Rep. 2017, 19, 36. [Google Scholar] [CrossRef]
- Jemal, A.; Center, M.M.; DeSantis, C.; Ward, E.M. Global Patterns of Cancer Incidence and Mortality Rates and TrendsGlobal Patterns of Cancer. Cancer Epidemiol. Biomark. Prev. 2010, 19, 1893–1907. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Plummer, M.; Franceschi, S.; Vignat, J.; Forman, D.; De Martel, C. Global burden of gastric cancer attributable to Helicobacter pylori. Int. J. Cancer 2015, 136, 487–490. [Google Scholar] [CrossRef]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018, 68, 394–424. [Google Scholar] [CrossRef] [Green Version]
- Mehta, R.S.; Song, M.; Nishihara, R.; Drew, D.A.; Wu, K.; Qian, Z.R.; Fung, T.T.; Hamada, T.; Masugi, Y.; da Silva, A. Dietary patterns and risk of colorectal cancer: Analysis by tumor location and molecular subtypes. Gastroenterology 2017, 152, 1944–1953. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jayasekara, H.; English, D.R.; Haydon, A.; Hodge, A.M.; Lynch, B.M.; Rosty, C.; Williamson, E.J.; Clendenning, M.; Southey, M.C.; Jenkins, M.A. Associations of alcohol intake, smoking, physical activity and obesity with survival following colorectal cancer diagnosis by stage, anatomic site and tumor molecular subtype. Int. J. Cancer 2018, 142, 238–250. [Google Scholar] [CrossRef]
- Favoriti, P.; Carbone, G.; Greco, M.; Pirozzi, F.; Pirozzi, R.E.M.; Corcione, F. Worldwide burden of colorectal cancer: A review. Updates Surg. 2016, 68, 7–11. [Google Scholar] [CrossRef]
- Tang, W.-R.; Fang, J.-Y.; Wu, K.-S.; Shi, X.-J.; Luo, J.-Y.; Lin, K. Epidemiological characteristics and prediction of esophageal cancer mortality in China from 1991 to 2012. Asian Pac. J. Cancer Prev. 2014, 15, 6929–6934. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, J.; He, Y.-T.; Zheng, R.-S.; Zhang, S.-W.; Chen, W.-Q. Analysis of esophageal cancer time trends in China, 1989–2008. Asian Pac. J. Cancer Prev. 2012, 13, 4613–4617. [Google Scholar] [CrossRef] [PubMed]
- Liang, H.; Fan, J.-H.; Qiao, Y.-L. Epidemiology, etiology, and prevention of esophageal squamous cell carcinoma in China. Cancer Biol. Med. 2017, 14, 33. [Google Scholar] [CrossRef] [Green Version]
- Fan, L.; Strasser-Weippl, K.; Li, J.-J.; St Louis, J.; Finkelstein, D.M.; Yu, K.-D.; Chen, W.-Q.; Shao, Z.-M.; Goss, P.E. Breast cancer in China. Lancet Oncol. 2014, 15, e279–e289. [Google Scholar] [CrossRef]
- Zhang, M.; Peng, P.; Wu, C.; Gong, Y.; Zhang, S.; Chen, W.; Bao, P. Report of breast cancer incidence and mortality in China registry regions, 2008-2012. Zhonghua Zhong Liu Za Zhi [Chin. J. Oncol. ] 2019, 41, 315–320. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Sun, S.; Yuan, J.-P.; Wang, Y.-H.; Cao, T.-Z.; Zheng, H.-M.; Jiang, X.-Q.; Gong, Y.-P.; Tu, Y.; Yao, F. Characteristics of breast cancer in Central China, literature review and comparison with USA. Breast 2016, 30, 208–213. [Google Scholar] [CrossRef] [Green Version]
- Grayson, M. Bladder cancer. Nature 2017, 551, S33. [Google Scholar] [CrossRef] [Green Version]
- Isa, F.; Xie, L.P.; Hu, Z.; Zhong, Z.; Hemelt, M.; Reulen, R.C.; Wong, Y.C.; Tam, P.C.; Yang, K.; Chai, C.; et al. Dietary consumption and diet diversity and risk of developing bladder cancer: Results from the South and East China case-control study. Cancer Causes Control 2013, 24, 885–895. [Google Scholar] [CrossRef] [PubMed]
- Bi, W.; Hayes, R.B.; Feng, P.; Qi, Y.; You, X.; Zhen, J.; Zhang, M.; Qu, B.; Fu, Z.; Chen, M.; et al. Mortality and incidence of bladder cancer in benzidine-exposed workers in China. Am. J. Ind. Med. 1992, 21, 481–489. [Google Scholar] [CrossRef] [PubMed]
- Tang, L.-L.; Chen, W.-Q.; Xue, W.-Q.; He, Y.-Q.; Zheng, R.-S.; Zeng, Y.-X.; Jia, W.-H. Global trends in incidence and mortality of nasopharyngeal carcinoma. Cancer Lett. 2016, 374, 22–30. [Google Scholar] [CrossRef] [PubMed]
- WHO. Estimated Age-Standardized Incidence Rates (World) in 2020, All Cancers, Both Sexes, All Ages. Available online: https://gco.iarc.fr/today/online-analysis-map (accessed on 7 October 2022).
- Kwok, H.; Wu, C.W.; Palser, A.L.; Kellam, P.; Sham, P.C.; Kwong, D.L.; Chiang, A.K. Genomic diversity of Epstein-Barr virus genomes isolated from primary nasopharyngeal carcinoma biopsy samples. J. Virol. 2014, 88, 10662–10672. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chang, E.T.; Liu, Z.; Hildesheim, A.; Liu, Q.; Cai, Y.; Zhang, Z.; Chen, G.; Xie, S.H.; Cao, S.M.; Shao, J.Y.; et al. Active and Passive Smoking and Risk of Nasopharyngeal Carcinoma: A Population-Based Case-Control Study in Southern China. Am. J. Epidemiol. 2017, 185, 1272–1280. [Google Scholar] [CrossRef] [PubMed]
- Ho, J.H.C.; Huang, D.P.; Fong, Y.Y. Salted Fish and Nasopharyngeal Carcinoma in Southern Chinese. Lancet 1978, 312, 626. [Google Scholar] [CrossRef] [PubMed]
- Hua, Z.Z.; Ying, L.C.; Ye, R.H.; Shaohui, L. A study on the trends of cervical cancer incidence and mortality among Chinese women during 2003-2018. Chin. J. Dis. Control 2022, 26, 14–20. [Google Scholar] [CrossRef]
- Zeng, H.; Chen, W.; Zheng, R.; Zhang, S.; Ji, J.S.; Zou, X.; Xia, C.; Sun, K.; Yang, Z.; Li, H.; et al. Changing cancer survival in China during 2003–15: A pooled analysis of 17 population-based cancer registries. Lancet Glob. Health 2018, 6, e555–e567. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Henley, S.J.; Singh, S.D.; King, J.; Wilson, R.J.; O’Neil, M.E.; Ryerson, A.B. Invasive Cancer Incidence and Survival—United States, 2013. MMWR Morb. Mortal. Wkly. Rep. 2017, 66, 69–75. [Google Scholar] [CrossRef]


| Cancer Site | Mortality Rate (per 100,000) a | Total Study Period b | Period 1 | Period 2 | Period 3 | Period 4 | Period 5 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1987 | 2020 | AAPC (%) | 95% CI | Years | APC (%) | Years | APC (%) | Years | APC (%) | Years | APC (%) | Years | APC (%) | ||
| Cancers in urban areas | total | 154.38 | 101.32 | −0.8 * | (−1.0,−0.7) | 1987–2018 | −0.7 * | 2018–2020 | −7.3 | — | — | — | — | — | — |
| male | 194.25 | 135.26 | −0.8 * | (−0.9,−0.6) | 1987–2017 | −0.6 * | 2017–2020 | −4.8 | — | — | — | — | — | — | |
| female | 123.21 | 70.66 | −1.0 * | (−1.2,−0.9) | 1987–2018 | −0.9 * | 2018–2020 | −6.8 | — | — | — | — | — | — | |
| Nasopharyngeal | total | 2.44 | 0.84 | −2.9 * | (−3.3,−2.5) | 1987–2020 | −2.9 * | — | — | — | — | — | — | — | — |
| male | 3.12 | 1.3 | −2.6 * | (−3.0,−2.2) | 1987–2020 | −2.6 * | — | — | — | — | — | — | — | — | |
| female | 1.63 | 0.39 | −3.6 * | (−4.1,−3.1) | 1987–2020 | −3.6 * | — | — | — | — | — | — | — | — | |
| Esophageal | total | 13.97 | 6.2 | −1.7 * | (−2.2,−1.3) | 1987–2000 | −4.0 * | 2000–2005 | 6.8 | 2005–2008 | −16.3 | 2008–2015 | 4.1 | 2015–2020 | −6.3 * |
| male | 18.96 | 9.85 | −1.5 * | (−1.9,−1.1) | 1987–2001 | −3.0 * | 2001–2005 | 7.7 | 2005–2008 | −14.1 | 2008–2015 | 3 | 2015–2020 | −5.7 * | |
| female | 8.46 | 2.84 | −2.5 * | (−3.2,−1.9) | 1987–1997 | −6.8 * | 1997–2005 | 3.1 | 2005–2008 | −20.5 | 2008–2015 | 6.5 * | 2015–2020 | −7.5 | |
| Stomach | total | 28.82 | 10.54 | −2.4 * | (−2.7,−2.1) | 1987–2020 | −2.4 * | — | — | — | — | — | — | — | — |
| male | 37.76 | 15.29 | −2.4 * | (−2.7,−2.1) | 1987–2020 | −2.4 * | — | — | — | — | — | — | — | — | |
| female | 18.75 | 6.27 | −2.6 * | (−2.9,−2.4) | 1987–2020 | −2.6 * | — | — | — | — | — | — | — | — | |
| Colon, rectum & anus | total | 10.65 | 9.22 | −0.1 | (−0.4,0.1) | 1987–2020 | −0.1 | — | — | — | — | — | — | — | — |
| male | 10.36 | 11.79 | 0.4 * | (0.1,0.6) | 1987–2000 | 1.1 * | 2000–2004 | −5.0 * | 2004–2007 | 11.5 * | 2007–2012 | −3.3 * | 2012–2020 | 0.7 | |
| female | 10.49 | 6.96 | −0.8 * | (−1.0,−0.5) | 1987–1989 | −8.3 | 1989–2000 | 0.6 | 2000–2003 | −9.2 | 2003–2007 | 6.0 | 2007–2020 | −1.6 * | |
| Liver | total | 24.45 | 13.78 | −1.2 * | (−1.6,−0.9) | 1987–2020 | −1.2 * | — | — | — | — | — | — | — | — |
| male | 33.82 | 20.57 | −1.1 * | (−1.5,−0.8) | 1987–2005 | −0.3 | 2005–2020 | −2.3 * | — | — | — | — | — | — | |
| female | 13.79 | 7.26 | −1.4 * | (−1.8,−1.1) | 1987–2020 | −1.4 * | — | — | — | — | — | — | — | — | |
| Lung | total | 40.36 | 29.79 | −0.4 * | (−0.6,−0.1) | 1987–2000 | 0.6 | 2000–2003 | −6 | 2003–2015 | 1.1 * | 2015–2020 | −3.9 * | — | — |
| male | 52.47 | 43.92 | −0.2 * | (−0.4,−0.0) | 1987–2000 | 0.9 * | 2000–2003 | −7.1 | 2003–2006 | 4.1 | 2006–2017 | 0.1 | 2017–2020 | −5.4 * | |
| female | 26.95 | 16.96 | −0.7 * | (−1.0,−0.4) | 1987–2000 | 0.5 | 2000–2004 | −7.8 | 2004–2010 | 4.3 | 2010–2020 | −2.3 * | — | — | |
| Breast | total | 3.85 | 2.96 | −0.4 * | (−0.6,−0.1) | 1987–1996 | −0.5 | 1996–1999 | 4.7 | 1999–2002 | −6 | 2002–2017 | 0.3 | 2017–2020 | −4.9 |
| male | |||||||||||||||
| female | 7.56 | 5.69 | −0.4 * | (−0.6,−0.1) | 1987–2020 | −0.4 * | — | — | — | — | — | — | — | — | |
| Cervix | total | 2.86 | 1.41 | −0.6 | (−1.7,0.5) | 1987–1994 | −10.1 * | 1994–2008 | −2.4 * | 2008–2016 | 9.9 * | 2016–2020 | −6.8 | — | — |
| male | |||||||||||||||
| female | 5.48 | 2.78 | −0.4 | (−1.5,0.7) | 1987–1994 | −9.9 * | 1994–2008 | −2.5 * | 2008–2016 | 11.0 * | 2016–2020 | −7.4 | — | — | |
| Bladder | total | 2.66 | 1.45 | −1.6 * | (−1.9,−1.2) | 1987–1999 | 0.1 | 1999–2002 | −9.3 | 2002–2020 | −0.6 | — | — | — | — |
| male | 3.97 | 2.48 | −1.6 * | (−1.9,−1.2) | 1987–2000 | 0.3 | 2000–2003 | −15.2 * | 2003–2006 | 8.2 | 2006–2020 | −1.4 * | — | — | |
| female | 1.31 | 0.61 | −2.0 * | (−2.4,−1.6) | 1987–2020 | −2.0 * | — | — | — | — | — | — | — | — | |
| Leukemia | total | 4.46 | 2.68 | −0.9 * | (−1.1,−0.6) | 1987–1996 | −2.6 * | 1996–1999 | 4.9 | 1999–2004 | −3.3 | 2004–2007 | 4 | 2007–2020 | −2.0 * |
| male | 5.04 | 3.15 | −0.7 * | (−0.9,−0.4) | 1987–1996 | −2.7 * | 1996–1999 | 6.7 | 1999–2004 | −4.3 | 2004–2007 | 5.7 | 2007–2020 | −2.0 * | |
| female | 3.82 | 2.24 | −1.1 * | (−1.3,−0.8) | 1987–2020 | −1.1 * | — | — | — | — | — | — | — | — | |
| Cancers in rural areas | total | 122.74 | 106.45 | −0.2 | (−0.5,0.1) | 1987–2009 | 0.4 * | 2009–2020 | −1.9 * | — | — | — | — | — | — |
| male | 157.09 | 144.44 | −0.1 | (−0.4,0.2) | 1987–2005 | 0.1 | 2005–2008 | 6.1 | 2008–2020 | −2.8 * | — | — | — | — | |
| female | 92.67 | 71.96 | −0.6 * | (−0.8,−0.4) | 1987–2009 | −0.2 | 2009–2020 | −1.7 * | — | — | — | — | — | — | |
| Nasopharyngeal | total | 2.22 | 1.14 | −1.9 * | (−2.4,−1.4) | 1987–2020 | −1.9 * | — | — | — | — | — | — | — | — |
| male | 3.28 | 1.72 | −1.5 * | (−2.1,−1.0) | 1987–2020 | −1.5 * | — | — | — | — | — | — | — | — | |
| female | 1.26 | 0.59 | −2.6 * | (−3.2,−2.0) | 1987–2020 | −2.6 * | — | — | — | — | — | — | — | — | |
| Esophageal | total | 22.93 | 8.16 | −2.9 * | (−3.7,−2.2) | 1987–2008 | −1.1 | 2008–2020 | −7.0 * | — | — | — | — | — | — |
| male | 29.99 | 12.95 | −2.3 * | (−3.0,−1.6) | 1987–2008 | −0.6 | 2008–2020 | −6.1 * | — | — | — | — | — | — | |
| female | 16.58 | 3.80 | −4.3 * | (−5.1,−3.6) | 1987–2008 | −2.3 * | 2008–2020 | −8.7 * | — | — | — | — | — | — | |
| Gastric cancer | total | 27.37 | 12.45 | −2.2 * | (−2.6,−1.8) | 1987–2008 | −1.1 * | 2008–2020 | −4.7 * | — | — | — | — | — | — |
| male | 36 | 18.21 | −1.9 * | (−2.3,−1.5) | 1987–2008 | −0.9 * | 2008–2020 | −4.3 * | — | — | — | — | — | — | |
| female | 19.58 | 7.26 | −2.8 * | (−3.1,−2.4) | 1987–2006 | −1.6 * | 2006–2020 | −4.7 * | — | — | — | — | — | — | |
| Colon, rectum & anus | total | 7.21 | 7.6 | 0.4 * | (0.0,0.7) | 1987–2020 | 0.4 * | — | — | — | — | — | — | — | — |
| male | 7.93 | 9.63 | 0.6 * | (0.3,0.9) | 1987–1992 | −2 | 1992–2006 | 1.0 * | 2006–2009 | 6.3 | 2009–2013 | −6.6 | 2013–2020 | 3.6 * | |
| female | 6.67 | 5.79 | −0.3 * | (−0.6,−0.0) | 1987–2004 | −0.9 * | 2004–2009 | 3.60 | 2009–2012 | −7.9 | 2012–2020 | 2.3 * | — | — | |
| Liver cancer | total | 24.66 | 17.64 | −1.2 * | (−1.6,−0.7) | 1987–2003 | 0.9 * | 2003–2020 | −3.0 * | — | — | — | — | — | — |
| male | 35.98 | 26.75 | −1.0 * | (−1.4,−0.6) | 1987–2002 | 1.0 * | 2002–2005 | −5.8 | 2005–2008 | 4.9 | 2008–2020 | −3.9 * | — | — | |
| female | 14.14 | 8.92 | −1.6 * | (−2.0,−1.2) | 1987–2000 | 1.0 * | 2000–2020 | −3.0 * | — | — | — | — | — | — | |
| Lung cancer | total | 15.55 | 30.26 | 2.4 * | (2.1,2.8) | 1987–2009 | 3.2 * | 2009–2020 | 0.4 | — | — | — | — | — | — |
| male | 22.96 | 44.37 | 2.3 * | (1.9,2.6) | 1987–2005 | 2.3 * | 2005–2008 | 9.7 | 2008–2020 | −0.8 | — | — | — | — | |
| female | 8.94 | 17.46 | 2.4 * | (2.1,2.8) | 1987–2020 | 2.4 * | — | — | — | — | — | — | — | — | |
| Breast cancer | total | 1.98 | 2.43 | 1.2 * | (0.7,1.6) | 1987–1996 | 0.6 | 1996–2002 | 6.1 | 2002–2005 | −13.3 | 2005–2008 | 13.5 | 2008–2020 | −0.5 |
| male | |||||||||||||||
| female | 3.94 | 4.69 | 1.0 * | (0.6,1.5) | 1987–1993 | −1.1 | 1993–2002 | 5.3 * | 2002–2005 | −12.2 | 2005–2008 | 11.2 | 2008–2020 | −0.8 | |
| Cervical carcinoma | total | 3.97 | 1.81 | −2.0 * | (−3.2,−0.8) | 1987–2001 | −3.1 * | 2001–2006 | −14.4 | 2006–2020 | 6.9 * | — | — | — | — |
| male | |||||||||||||||
| female | 7.82 | 3.53 | −1.9 * | (−3.1,−0.6) | 1987–1990 | −17.1 | 1990–2001 | −0.1 | 2001–2005 | −21.7 | 2005–2020 | 7.2 * | — | — | |
| Bladder cancer | total | 1.11 | 1.33 | 0.2 | (−0.2,0.5) | 1987–2020 | 0.2 | — | — | — | — | — | — | — | — |
| male | 1.85 | 2.34 | 0.1 | (−0.3,0.5) | 1987–2020 | 0.1 | — | — | — | — | — | — | — | — | |
| female | 0.5 | 0.5 | −0.9 * | (−1.4,−0.3) | 1987–2020 | −0.9 * | — | — | — | — | — | — | — | — | |
| Leukemia | total | 3.30 | 3.03 | −0.4 * | (−0.5,−0.2) | 1987–2020 | −0.4 * | 1987–2005 | −0.8 * | 2005–2008 | 4.40 | 2008–2020 | −1.5 * | — | — |
| male | 3.72 | 3.61 | 0 | (−0.3,0.2) | 1987–2020 | 0 | — | — | — | — | — | — | — | — | |
| female | 3.12 | 2.48 | −0.7 * | (−0.9,−0.6) | 1987–2020 | −0.7 * | — | — | — | — | — | — | — | — | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Su, B.; Zhong, P.; Xuan, Y.; Xie, J.; Wu, Y.; Chen, C.; Zhao, Y.; Shen, X.; Zheng, X. Changing Patterns in Cancer Mortality from 1987 to 2020 in China. Cancers 2023, 15, 476. https://doi.org/10.3390/cancers15020476
Su B, Zhong P, Xuan Y, Xie J, Wu Y, Chen C, Zhao Y, Shen X, Zheng X. Changing Patterns in Cancer Mortality from 1987 to 2020 in China. Cancers. 2023; 15(2):476. https://doi.org/10.3390/cancers15020476
Chicago/Turabian StyleSu, Binbin, Panliang Zhong, Yundong Xuan, Junqing Xie, Yu Wu, Chen Chen, Yihao Zhao, Xinran Shen, and Xiaoying Zheng. 2023. "Changing Patterns in Cancer Mortality from 1987 to 2020 in China" Cancers 15, no. 2: 476. https://doi.org/10.3390/cancers15020476
APA StyleSu, B., Zhong, P., Xuan, Y., Xie, J., Wu, Y., Chen, C., Zhao, Y., Shen, X., & Zheng, X. (2023). Changing Patterns in Cancer Mortality from 1987 to 2020 in China. Cancers, 15(2), 476. https://doi.org/10.3390/cancers15020476






