Anaplastic Lymphoma Kinase Inhibitor-Induced Neutropenia: A Systematic Review
Abstract
:Simple Summary
Abstract
1. Introduction
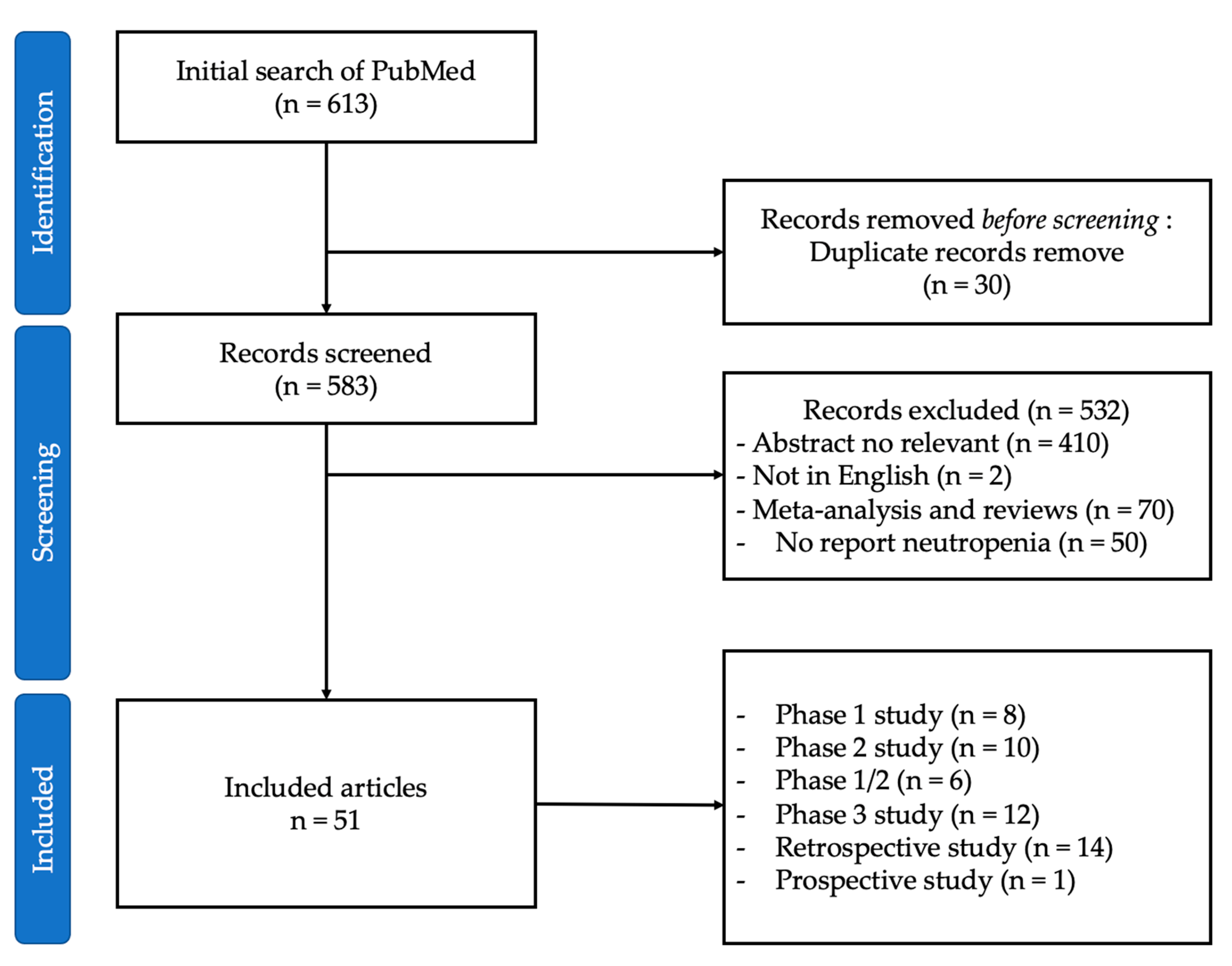
2. Materials and Methods
3. Results
3.1. Population Characteristics
3.2. First-Generation ALK Inhibitors Induce Neutropenia
3.3. Second- and Third-Generation ALK Inhibitors Induce Neutropenia
3.4. ALK Inhibitors Induce Neutropenia in Asian Populations
3.5. Febrile Neutropenia
3.6. Neutropenia Management
3.7. Physiopathological Hypotheses
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Rolfo, C.; Caglevic, C.; Santarpia, M.; Araujo, A.; Giovannetti, E.; Gallardo, C.D.; Pauwels, P.; Mahave, M. Immunotherapy in NSCLC: A promising and revolutionary weapon. Adv. Exp. Med. Biol. 2017, 995, 97–125. [Google Scholar] [CrossRef] [PubMed]
- Devarakonda, S.; Morgensztern, D.; Govindan, R. Genomic alterations in lung adenocarcinoma. Lancet Oncol. 2015, 16, e342–e351. [Google Scholar] [CrossRef]
- Morris, S.W.; Kirstein, M.N.; Valentine, M.B.; Dittmer, K.G.; Shapiro, D.N.; Saltman, D.L.; Look, A.T. Fusion of a kinase gene, ALK, to a nucleolar protein gene, NPM, in non-Hodgkin’s lymphoma. Science 1994, 263, 1281–1284. [Google Scholar] [CrossRef] [PubMed]
- Novello, S.; Mazières, J.; Oh, I.-J.; de Castro, J.; Migliorino, M.; Helland, A.; Dziadziuszko, R.; Griesinger, F.; Kotb, A.; Zeaiter, A.; et al. Alectinib versus chemotherapy in crizotinib-pretreated anaplastic lymphoma kinase (ALK)-positive non-small-cell lung cancer: Results from the phase III ALUR study. Ann. Oncol. 2018, 29, 1409–1416. [Google Scholar] [CrossRef]
- Solomon, B.J.; Kim, D.-W.; Wu, Y.-L.; Nakagawa, K.; Mekhail, T.; Felip, E.; Cappuzzo, F.; Paolini, J.; Usari, T.; Tang, Y.; et al. Final overall survival analysis from a study comparing first-line crizotinib versus chemotherapy in ALK-mutation-positive non–small-cell lung cancer. J. Clin. Oncol. 2018, 36, 2251–2258. [Google Scholar] [CrossRef]
- Shaw, A.T.; Kim, T.M.; Crinò, L.; Gridelli, C.; Kiura, K.; Liu, G.; Novello, S.; Bearz, A.; Gautschi, O.; Mok, T.; et al. Ceritinib versus chemotherapy in patients with ALK-rearranged non-small-cell lung cancer previously given chemotherapy and crizotinib (ASCEND-5): A randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2017, 18, 874–886. [Google Scholar] [CrossRef]
- Hendriks, L.E.; Kerr, K.M.; Menis, J.; Mok, T.S.; Nestle, U.; Passaro, A.; Peters, S.; Planchard, D.; Smit, E.F.; Solomon, B.J.; et al. Oncogene-addicted metastatic non-small-cell lung cancer: ESMO clinical practice guideline for diagnosis, treatment and follow-up. Ann. Oncol. 2023, 34, 339–357. [Google Scholar] [CrossRef] [PubMed]
- Ettinger, D.S.; Wood, D.E.; Aisner, D.L.; Akerley, W.; Bauman, J.R.; Bharat, A.; Bruno, D.S.; Chang, J.Y.; Chirieac, L.R.; D′Amico, T.A.; et al. Non-small cell lung cancer, version 3.2022, NCCN clinical practice guidelines in oncology. J. Natl. Compr. Canc. Netw. 2022, 20, 497–530. [Google Scholar] [CrossRef] [PubMed]
- Cetin, K.; Ettinger, D.S.; Hei, Y.-J.; O′Malley, C.D. Survival by histologic subtype in stage IV nonsmall cell lung cancer based on data from the surveillance, epidemiology and end results program. Clin. Epidemiol. 2011, 3, 139–148. [Google Scholar] [CrossRef]
- Kiura, K.; Imamura, F.; Kagamu, H.; Matsumoto, S.; Hida, T.; Nakagawa, K.; Satouchi, M.; Okamoto, I.; Takenoyama, M.; Fujisaka, Y.; et al. Phase 3 study of ceritinib vs chemotherapy in ALK-rearranged NSCLC patients previously treated with chemotherapy and crizotinib (ASCEND-5): Japanese subset. Jpn. J. Clin. Oncol. 2018, 48, 367–375. [Google Scholar] [CrossRef]
- Nishio, M.; Kim, D.-W.; Wu, Y.-L.; Nakagawa, K.; Solomon, B.J.; Shaw, A.T.; Hashigaki, S.; Ohki, E.; Usari, T.; Paolini, J.; et al. Crizotinib versus chemotherapy in asian patients with ALK-positive advanced non-small cell lung cancer. Cancer Res. Treat. 2017, 50, 691–700. [Google Scholar] [CrossRef]
- Camidge, D.R.; Kim, H.R.; Ahn, M.-J.; Yang, J.C.-H.; Han, J.-Y.; Lee, J.-S.; Hochmair, M.J.; Li, J.Y.-C.; Chang, G.-C.; Lee, K.H.; et al. Brigatinib versus crizotinib in ALK-positive non–small-cell lung cancer. N. Engl. J. Med. 2018, 379, 2027–2039. [Google Scholar] [CrossRef] [PubMed]
- Shaw, A.T.; Gandhi, L.; Gadgeel, S.; Riely, G.J.; Cetnar, J.; West, H.; Camidge, D.R.; Socinski, M.A.; Chiappori, A.; Mekhail, T.; et al. Alectinib in ALK-positive, crizotinib-resistant, non-small-cell lung cancer: A single-group, multicentre, phase 2 trial. Lancet Oncol. 2016, 17, 234–242. [Google Scholar] [CrossRef] [PubMed]
- Shaw, A.T.; Bauer, T.M.; de Marinis, F.; Felip, E.; Goto, Y.; Liu, G.; Mazieres, J.; Kim, D.-W.; Mok, T.; Polli, A.; et al. First-line lorlatinib or crizotinib in advanced ALK-positive lung cancer. N. Engl. J. Med. 2020, 383, 2018–2029. [Google Scholar] [CrossRef] [PubMed]
- Hotta, K.; Hida, T.; Nokihara, H.; Morise, M.; Kim, Y.; Azuma, K.; Seto, T.; Takiguchi, Y.; Nishio, M.; Yoshioka, H.; et al. Final overall survival analysis from the phase III J-ALEX study of alectinib versus crizotinib in ALK inhibitor-naïve Japanese patients with ALK-positive non-small-cell lung cancer. ESMO Open 2022, 7, 100527. [Google Scholar] [CrossRef]
- Solomon, B.J.; Mok, T.; Kim, D.-W.; Wu, Y.-L.; Nakagawa, K.; Mekhail, T.; Felip, E.; Cappuzzo, F.; Paolini, J.; Usari, T.; et al. First-line crizotinib versus chemotherapy in ALK-positive lung cancer. N. Engl. J. Med. 2014, 371, 2167–2177. [Google Scholar] [CrossRef]
- Hida, T.; Nokihara, H.; Kondo, M.; Kim, Y.H.; Azuma, K.; Seto, T.; Takiguchi, Y.; Nishio, M.; Yoshioka, H.; Imamura, F.; et al. Alectinib versus crizotinib in patients with ALK-positive non-small-cell lung cancer (J-ALEX): An open-label, randomised phase 3 trial. Lancet 2017, 390, 29–39. [Google Scholar] [CrossRef] [PubMed]
- Soria, J.-C.; Tan, D.S.W.; Chiari, R.; Wu, Y.-L.; Paz-Ares, L.; Wolf, J.; Geater, S.L.; Orlov, S.; Cortinovis, D.; Yu, C.-J.; et al. First-line ceritinib versus platinum-based chemotherapy in advanced ALK-rearranged non-small-cell lung cancer (ASCEND-4): A randomised, open-label, phase 3 study. Lancet 2017, 389, 917–929. [Google Scholar] [CrossRef]
- Camidge, D.R.; Bang, Y.-J.; Kwak, E.L.; Iafrate, A.J.; Varella-Garcia, M.; Fox, S.B.; Riely, G.J.; Solomon, B.; Ou, S.-H.I.; Kim, D.-W.; et al. Activity and safety of crizotinib in patients with ALK-positive non-small-cell lung cancer: Updated results from a phase 1 study. Lancet Oncol. 2012, 13, 1011–1019. [Google Scholar] [CrossRef] [PubMed]
- Shaw, A.; Riely, G.; Bang, Y.-J.; Kim, D.-W.; Camidge, D.; Solomon, B.; Varella-Garcia, M.; Iafrate, A.; Shapiro, G.; Usari, T.; et al. Crizotinib in ROS1-rearranged advanced non-small-cell lung cancer (NSCLC): Updated results, including overall survival, from PROFILE 1001. Ann. Oncol. 2019, 30, 1121–1126. [Google Scholar] [CrossRef]
- Gambacorti-Passerini, C.; Orlov, S.; Zhang, L.; Braiteh, F.; Huang, H.; Esaki, T.; Horibe, K.; Ahn, J.S.; Beck, J.T.; Edenfield, W.J.; et al. Long-term effects of crizotinib in ALK-positive tumors (excluding NSCLC): A phase 1b open-label study. Am. J. Hematol. 2018, 93, 607–614. [Google Scholar] [CrossRef] [PubMed]
- Mossé, Y.P.; Lim, M.S.; Voss, S.D.; Wilner, K.; Ruffner, K.; Laliberte, J.; Rolland, D.; Balis, F.M.; Maris, J.M.; Weigel, B.J.; et al. Safety and activity of crizotinib for paediatric patients with refractory solid tumours or anaplastic large-cell lymphoma: A children’s oncology group phase 1 consortium study. Lancet Oncol. 2013, 14, 472–480. [Google Scholar] [CrossRef] [PubMed]
- Blackhall, F.; Camidge, D.R.; Shaw, A.T.; Soria, J.-C.; Solomon, B.J.; Mok, T.; Hirsh, V.; Jänne, P.A.; Shi, Y.; Yang, P.-C.; et al. Final results of the large-scale multinational trial PROFILE 1005: Efficacy and safety of crizotinib in previously treated patients with advanced/metastatic ALK-positive non-small-cell lung cancer. ESMO Open 2017, 2, e000219. [Google Scholar] [CrossRef] [PubMed]
- Schöffski, P.; Wozniak, A.; Stacchiotti, S.; Rutkowski, P.; Blay, J.Y.; Lindner, L.H.; Strauss, S.J.; Anthoney, A.; Duffaud, F.; Richter, S.; et al. Activity and safety of crizotinib in patients with advanced clear-cell sarcoma with MET alterations: European or-ganization for research and treatment of cancer phase II trial 90101 ‘CREATE’. Ann. Oncol. 2017, 28, 3000–3008. [Google Scholar] [CrossRef]
- Schöffski, P.; Wozniak, A.; Kasper, B.; Aamdal, S.; Leahy, M.; Rutkowski, P.; Bauer, S.; Gelderblom, H.; Italiano, A.; Lindner, L.; et al. Activity and safety of crizotinib in patients with alveolar soft part sarcoma with rearrangement of TFE3: European organization for research and treatment of cancer (EORTC) phase II trial 90101 ‘CREATE’. Ann. Oncol. 2017, 29, 758–765. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.L.; Lu, S.; Yang, J.C.; Zhou, J.; Seto, T.; Ahn, M.J.; Su, W.C.; Yamamoto, N.; Kim, D.W.; Paolini, J.; et al. Final overall survival, safety, and quality of life results from a phase 2 study of crizotinib in East Asian patients with ROS1-positive ad-vanced NSCLC. JTO Clin. Res. Rep. 2022, 3, 100406. [Google Scholar] [CrossRef]
- Schöffski, P.; Kubickova, M.; Wozniak, A.; Blay, J.-Y.; Strauss, S.J.; Stacchiotti, S.; Switaj, T.; Bücklein, V.; Leahy, M.G.; Italiano, A.; et al. Long-term efficacy update of crizotinib in patients with advanced, inoperable inflammatory myofibroblastic tumour from EORTC trial 90101 CREATE. Eur. J. Cancer 2021, 156, 12–23. [Google Scholar] [CrossRef]
- Michels, S.; Massutí, B.; Schildhaus, H.-U.; Franklin, J.; Sebastian, M.; Felip, E.; Grohé, C.; Rodriguez-Abreu, D.; Abdulla, D.S.; Bischoff, H.; et al. Safety and efficacy of crizotinib in patients with advanced or metastatic ROS1-rearranged lung cancer (EUCROSS): A European Phase II Clinical Trial. J. Thorac. Oncol. 2019, 14, 1266–1276. [Google Scholar] [CrossRef]
- Pal, S.K.; Tangen, C.; Thompson, I.M.; Balzer-Haas, N.; George, D.J.; Heng, D.Y.C.; Shuch, B.; Stein, M.; Tretiakova, M.; Humphrey, P.; et al. A comparison of sunitinib with cabozantinib, crizotinib, and savolitinib for treatment of advanced papillary renal cell carcinoma: A randomised, open-label, phase 2 trial. Lancet 2021, 397, 695–703. [Google Scholar] [CrossRef]
- Wu, Y.L.; Lu, S.; Lu, Y.; Zhou, J.; Shi, Y.K.; Sriuranpong, V.; Ho, J.C.M.; Ong, C.K.; Tsai, C.M.; Chung, C.H.; et al. Results of profile 1029, a phase III comparison of first-line crizotinib versus chemotherapy in East Asian patients with ALK-positive advanced non-small cell lung cancer. J. Thorac. Oncol. 2018, 13, 1539–1548. [Google Scholar] [CrossRef]
- Gambacorti, P.C.; Farina, F.; Stasia, A.; Redaelli, S.; Ceccon, M.; Mologni, L.; Messa, C.; Guerra, L.; Giudici, G.; Sala, E.; et al. Crizotinib in advanced, chemoresistant anaplastic lymphoma kinase-positive lymphoma patients. J. Natl. Cancer Inst. 2014, 106, djt378. [Google Scholar] [CrossRef]
- Rindone, G.; Aroldi, A.; Bossi, E.; Verga, L.; Zambrotta, G.; Tarantino, S.; Piazza, R.; Mussolin, L.; Chiarle, R.; Gambacor-ti-Passerini, C. A monocentric analysis of the long-term safety and efficacy of crizotinib in relapsed/refractory ALK+ lym-phomas. Blood Adv. 2022, 7, 314–316. [Google Scholar] [CrossRef]
- Moro-Sibilot, D.; Cozic, N.; Pérol, M.; Mazières, J.; Otto, J.; Souquet, P.; Bahleda, R.; Wislez, M.; Zalcman, G.; Guibert, S.; et al. Crizotinib in c-MET- or ROS1-positive NSCLC: Results of the AcSé phase II trial. Ann. Oncol. 2019, 30, 1985–1991. [Google Scholar] [CrossRef]
- Liu, C.; Yu, H.; Chang, J.; Chen, H.; Li, Y.; Zhao, W.; Zhao, K.; Zhu, Z.; Sun, S.; Fan, M.; et al. Crizotinib in Chinese patients with ROS1-rearranged advanced non–small-cell lung cancer in routine clinical practice. Target. Oncol. 2019, 14, 315–323. [Google Scholar] [CrossRef]
- Zhang, Q.; Qin, N.; Wang, J.; Lv, J.; Yang, X.; Li, X.; Nong, J.; Zhang, H.; Zhang, X.; Wu, Y.; et al. Crizotinib versus platinum-based double-agent chemotherapy as the first line treatment in advanced anaplastic lymphoma kinase-positive lung adenocarcinoma. Thorac. Cancer 2016, 7, 3–8. [Google Scholar] [CrossRef]
- Mohieldin, A.; Rasmy, A.; Ashour, M.; Al-Nassar, M.; Ali, R.H.; El-Enezi, F.G. Efficacy and safety of crizotinib in patients with anaplastic lymphoma kinase-positive advanced-stage non-small-cell lung cancer. Cancer Manag. Res. 2018, 10, 6555–6561. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Yu, H.; Long, Q.; Chen, H.; Li, Y.; Zhao, W.; Zhao, K.; Zhu, Z.; Sun, S.; Fan, M.; et al. Real world experience of crizotinib in 104 patients with ALK rearrangement non-small-cell lung cancer in a single chinese cancer center. Front. Oncol. 2019, 9, 1116. [Google Scholar] [CrossRef] [PubMed]
- Ueno, N.; Banno, S.; Endo, Y.; Tamura, M.; Sugaya, K.; Hashigaki, S.; Ohki, E.; Yoshimura, A.; Gemma, A. Treatment status and safety of crizotinib in 2028 Japanese patients with ALK-positive NSCLC in clinical settings. Jpn. J. Clin. Oncol. 2019, 49, 676–686. [Google Scholar] [CrossRef] [PubMed]
- Aguado, D.L.R.C.; Cruz, C.P.; Lázaro-Quintela, M.; Dómine, M.; Vázquez, E.S.; López-Vivanco, G.; Fírvida, P.J.L.; Alonso, R.J.L.; Ferrera, D.L.; García, G.C.; et al. Identification of ALK-positive patients with advanced NSCLC and real-world clinical expe-rience with crizotinib in Spain (IDEALK study). Lung Cancer 2022, 173, 83–93. [Google Scholar] [CrossRef]
- Takeuchi, S.; Yanagitani, N.; Seto, T.; Hattori, Y.; Ohashi, K.; Morise, M.; Matsumoto, S.; Yoh, K.; Goto, K.; Nishio, M.; et al. Phase 1/2 study of alectinib in RET-rearranged previously-treated non-small cell lung cancer (ALL-RET). Transl. Lung. Cancer Res. 2021, 10, 314–325. [Google Scholar] [CrossRef]
- Gadgeel, S.M.; Gandhi, L.; Riely, G.J.; Chiappori, A.A.; West, H.L.; Azada, M.C.; Morcos, P.N.; Lee, R.M.; Garcia, L.; Yu, L.; et al. Safety and activity of alectinib against systemic disease and brain metastases in patients with crizotinib-resistant ALK-rearranged non-small-cell lung cancer (AF-002JG): Results from the dose-finding portion of a phase 1/2 study. Lancet Oncol. 2014, 15, 1119–1128. [Google Scholar] [CrossRef] [PubMed]
- Tamura, T.; Kiura, K.; Seto, T.; Nakagawa, K.; Maemondo, M.; Inoue, A.; Hida, T.; Yoshioka, H.; Harada, M.; Ohe, Y.; et al. Three-year follow-up of an alectinib phase I/II study in ALK-positive non–small-cell lung cancer: AF-001JP. J. Clin. Oncol. 2017, 35, 1515–1521. [Google Scholar] [CrossRef]
- Iwama, E.; Goto, Y.; Murakami, H.; Harada, T.; Tsumura, S.; Sakashita, H.; Mori, Y.; Nakagaki, N.; Fujita, Y.; Seike, M.; et al. Alectinib for patients with ALK rearrangement–positive non–small cell lung cancer and a poor performance status (Lung Oncology Group in Kyushu 1401). J. Thorac. Oncol. 2017, 12, 1161–1166. [Google Scholar] [CrossRef] [PubMed]
- Fukano, R.; Mori, T.; Sekimizu, M.; Choi, I.; Kada, A.; Saito, A.M.; Asada, R.; Takeuchi, K.; Terauchi, T.; Tateishi, U.; et al. Alectinib for relapsed or refractory anaplastic lymphoma kinase-positive anaplastic large cell lymphoma: An open-label phase II trial. Cancer Sci. 2020, 111, 4540–4547. [Google Scholar] [CrossRef]
- Mok, T.; Camidge, D.; Gadgeel, S.; Rosell, R.; Dziadziuszko, R.; Kim, D.-W.; Pérol, M.; Ou, S.-H.; Ahn, J.; Shaw, A.; et al. Updated overall survival and final progression-free survival data for patients with treatment-naive advanced ALK-positive non-small-cell lung cancer in the ALEX study. Ann. Oncol. 2020, 31, 1056–1064. [Google Scholar] [CrossRef]
- Zhou, C.; Kim, S.-W.; Reungwetwattana, T.; Zhou, J.; Zhang, Y.; He, J.; Yang, J.-J.; Cheng, Y.; Lee, S.-H.; Bu, L.; et al. Alectinib versus crizotinib in untreated Asian patients with anaplastic lymphoma kinase-positive non-small-cell lung cancer (ALESIA): A randomised phase 3 study. Lancet Respir. Med. 2019, 7, 437–446. [Google Scholar] [CrossRef] [PubMed]
- Masuda, N.; Ohe, Y.; Gemma, A.; Kusumoto, M.; Yamada, I.; Ishii, T.; Yamamoto, N. Safety and effectiveness of alectinib in a real-world surveillance study in patients with ALK-positive non-small-cell lung cancer in Japan. Cancer Sci. 2019, 110, 1401–1407. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.-W.; Mehra, R.; Tan, D.S.W.; Felip, E.; Chow, L.Q.M.; Camidge, D.R.; Vansteenkiste, J.; Sharma, S.; De Pas, T.; Riely, G.J.; et al. Activity and safety of ceritinib in patients with ALK-rearranged non-small-cell lung cancer (ASCEND-1): Updated results from the multicentre, open-label, phase 1 trial. Lancet Oncol. 2016, 17, 452–463. [Google Scholar] [CrossRef]
- Fischer, M.; Moreno, L.; Ziegler, D.S.; Marshall, L.V.; Zwaan, C.M.; Irwin, M.S.; Casanova, M.; Sabado, C.; Wulff, B.; Stegert, M.; et al. Ceritinib in paediatric patients with anaplastic lymphoma kinase-positive malignancies: An open-label, multicentre, phase 1, dose-escalation and dose-expansion study. Lancet Oncol. 2021, 22, 1764–1776. [Google Scholar] [CrossRef]
- Nishio, M.; Murakami, H.; Horiike, A.; Takahashi, T.; Hirai, F.; Suenaga, N.; Tajima, T.; Tokushige, K.; Ishii, M.; Boral, A.; et al. Phase I study of ceritinib (LDK378) in Japanese patients with advanced, anaplastic lymphoma kinase-rearranged non-small-cell lung cancer or other tumors. J. Thorac. Oncol. 2015, 10, 1058–1066. [Google Scholar] [CrossRef]
- Tan, D.S.; Geater, S.; Yu, C.-J.; Tsai, C.-M.; Hsia, T.-C.; Chen, J.; Lin, M.-C.; Lu, Y.; Sriuranpong, V.; Yang, C.-T.; et al. Ceritinib efficacy and safety in treatment-naive Asian patients with advanced ALK-rearranged NSCLC: An ASCEND-4 subgroup analysis. JTO Clin. Res. Rep. 2021, 2, 100131. [Google Scholar] [CrossRef]
- Camidge, D.R.; Kim, H.R.; Ahn, M.-J.; Yang, J.C.; Han, J.-Y.; Hochmair, M.J.; Lee, K.H.; Delmonte, A.; Campelo, M.R.G.; Kim, D.-W.; et al. Brigatinib versus crizotinib in ALK inhibitor–naive advanced ALK-positive NSCLC: Final results of phase 3 ALTA-1L trial. J. Thorac. Oncol. 2021, 16, 2091–2108. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, H.; Teraoka, S.; Goto, Y.; Kumagai, T.; Nishio, M.; Sugawara, S.; Oizumi, S.; Matsumura, M.; Okura, M.; Peltz, G.; et al. First-line lorlatinib versus crizotinib in ALK-positive NSCLC: Japanese subgroup analysis of CROWN. JTO Clin. Res. Rep. 2023, 4, 100471. [Google Scholar] [CrossRef] [PubMed]
- Demetri, G.D.; De Braud, F.; Drilon, A.; Siena, S.; Patel, M.R.; Cho, B.C.; Liu, S.V.; Ahn, M.J.; Chiu, C.H.; Lin, J.J.; et al. Updated integrated analysis of the efficacy and safety of entrectinib in patients with NTRK fusion-positive solid tumors. Clin. Cancer Res. 2022, 28, 1302–1312. [Google Scholar] [CrossRef]
- Drilon, A.; Chiu, C.-H.; Fan, Y.; Cho, B.C.; Lu, S.; Ahn, M.-J.; Krebs, M.G.; Liu, S.V.; John, T.; Otterson, G.A.; et al. Long-term efficacy and safety of entrectinib in ROS1 fusion–positive NSCLC. JTO Clin. Res. Rep. 2022, 3, 100332. [Google Scholar] [CrossRef]
- Desai, A.V.; Robinson, G.W.; Gauvain, K.; Basu, E.M.; Macy, M.E.; Maese, L.; Whipple, N.S.; Sabnis, A.J.; Foster, J.H.; Shus-terman, S.; et al. Entrectinib in children and young adults with solid or primary CNS tumors harboring NTRK, ROS1, or ALK aberrations (STARTRK-NG). Neuro Oncol. 2022, 24, 1776–1789. [Google Scholar] [CrossRef]
- Ma, Y.; Zhao, H.; Xue, J.; Liu, L.; Yang, N.; Zhang, Y.; Yang, H.; Hong, S.; Xiong, Y.; Zhang, Z.; et al. First-in-human phase I study of TQ-B3139 (CT-711) in advanced non-small cell lung cancer patients with ALK and ROS1 rearrangements. Eur. J. Cancer 2022, 173, 238–249. [Google Scholar] [CrossRef] [PubMed]
- Gursoy, P.; Çakar, B.; Nart, D.; Göker, E. Predictive role of neutropenia under crizotinib treatment in ALK-rearranged nonsmall cell lung cancer patients: A single-institution retrospective analysis. Indian J. Cancer 2022, 59, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Osugi, J.; Owada, Y.; Yamaura, T.; Muto, S.; Okabe, N.; Matsumura, Y.; Higuchi, M.; Suzuki, H.; Gotoh, M. Successful man-agement of crizotinib-induced neutropenia in a patient with anaplastic lymphoma kinase-positive non-small cell lung cancer: A case report. Case Rep. Oncol. 2016, 9, 51–55. [Google Scholar] [CrossRef]
- Toyota, Y.; Sakugawa, M.; Bessho, A.; Horiuchi, T.; Hosokawa, S.; Watanabe, Y. Therapeutic use of low-dose corticosteroids to treat neutropenia resulting from crizotinib administration in a patient with anaplastic lymphoma kinase gene transloca-tion-positive lung cancer. Haigan Jpn. J. Lung Cancer 2014, 54, 78–83. [Google Scholar] [CrossRef]
- Chen, X.; Zhou, J.Y.; Zhao, J.; Chen, J.J.; Ma, S.N.; Zhou, J.Y. Crizotinib overcomes hepatocyte growth factor-mediated re-sistance to gefitinib in EGFR-mutant non-small-cell lung cancer cells. Anticancer Drugs 2013, 24, 1039–1046. [Google Scholar] [CrossRef] [PubMed]
- Xiong, S.; Dong, L.; Cheng, L. Neutrophils in cancer carcinogenesis and metastasis. J. Hematol. Oncol. 2021, 14, 173. [Google Scholar] [CrossRef] [PubMed]
- Coussens, L.M.; Werb, Z. Inflammation and cancer. Nature 2002, 420, 860–867. [Google Scholar] [CrossRef] [PubMed]
- Ozyurek, B.A.; Ozdemirel, T.S.; Ozden, S.B.; Erdogan, Y.; Kaplan, B.; Kaplan, T. Prognostic value of the neutrophil to lymphocyte ratio (NLR) in lung cancer cases. Asian Pac. J. Cancer Prev. 2017, 18, 1417–1421. [Google Scholar] [CrossRef]
- Zeng, L.; Kang, R.; Zhu, S.; Wang, X.; Cao, L.; Wang, H.; Billiar, T.R.; Jiang, J.; Tang, D. ALK is a therapeutic target for lethal sepsis. Sci. Transl. Med. 2017, 9, eaan5689. [Google Scholar] [CrossRef]
- Nielsen, S.R.; Strøbech, J.E.; Horton, E.R.; Jackstadt, R.; Laitala, A.; Bravo, M.C.; Maltese, G.; Jensen, A.R.D.; Reuten, R.; Rafaeva, M.; et al. Suppression of tumor-associated neutrophils by lorlatinib attenuates pancreatic cancer growth and improves treatment with immune checkpoint blockade. Nat. Commun. 2021, 12, 3414. [Google Scholar] [CrossRef]
- Li, J.; Smithgall, T.E. Fibroblast transformation by Fps/Fes tyrosine kinases requires Ras, Rac, and Cdc42 and induces extra-cellular signal-regulated and c-Jun N-terminal kinase activation. J. Biol. Chem. 1998, 273, 13828–13834. [Google Scholar] [CrossRef]
- Österlund, P.; Soveri, L.-M.; Isoniemi, H.; Poussa, T.; Alanko, T.; Bono, P. Hypertension and overall survival in metastatic colorectal cancer patients treated with bevacizumab-containing chemotherapy. Br. J. Cancer 2011, 104, 599–604. [Google Scholar] [CrossRef]
- Wu, R.R.; Lindenberg, P.A.; Slack, R.; Noone, A.-M.; Marshall, J.L.; He, A.R. Evaluation of hypertension as a marker of bevacizumab efficacy. J. Gastrointest. Cancer 2009, 40, 101–108. [Google Scholar] [CrossRef]
- Liu, Y.; Zhou, L.; Chen, Y.; Liao, B.; Ye, D.; Wang, K.; Li, H. Hypertension as a prognostic factor in metastatic renal cell car-cinoma treated with tyrosine kinase inhibitors: A systematic review and meta-analysis. BMC Urol. 2019, 19, 49. [Google Scholar] [CrossRef]
- Groenland, S.L.; Geel, D.R.; Janssen, J.M.; de Vries, N.; Rosing, H.; Beijnen, J.H.; Burgers, J.A.; Smit, E.F.; Huitema, A.D.; Steeghs, N. Exposure–response analyses of anaplastic lymphoma kinase inhibitors crizotinib and alectinib in non-small cell lung cancer patients. Clin. Pharmacol. Ther. 2020, 109, 394–402. [Google Scholar] [CrossRef] [PubMed]
| Ref. | Study Design | Population Treated with ALK Inhibitors | Cancer Type | Lines of Treatment before Metastatic Disease | Treatment and Dose | Region | Neutropenia All Grade n (%) | Neutropenia G3–4 n (%) |
|---|---|---|---|---|---|---|---|---|
| [19] | Phase 1, single-arm, multicentre | Adults n = 149 | ALK-positive lung cancer | 16% of patients had no previous treatment regimen Other patients had 1–4 or more previous lines of treatment | Crizotinib 250 mg twice per day | USA, Australia, and South Korea | NR | 9 (25) |
| [20] | Phase 1, open-label, expansion cohort, multicentre | Adults n = 53 | ROS1-rearranged lung cancer | 13% of patients had no previous treatment 65% of patients had 1–2 previous lines of treatment 23% of patients had 3 or more previous lines of treatment | Crizotinib 250 mg twice per day | International | 8 (15) | 5 (9) |
| [21] | Phase 1b, open-label, single-arm, multicentre | Adults n = 44 | ALK-positive tumours (excluding lung cancer) | 16% of patients had no prior systemic therapy Other patients had 1 or more prior lines of treatment | Crizotinib 250 mg twice per day | International | 14 (32) | 10 (23) |
| [22] | Phase 1, open-label, multicentre | Children n = 65 | ALK-positive solid tumours, lymphomas, CNS tumours | Refractory to therapy | Dose escalationcrizotinib 100, 130, 165, 215, 280, and 365 mg/m2 twice per day | USA | 21 (32) | 10 (15) |
| [23] | Phase 2, multicentre, single-arm | Adults n = 1069 | ALK-positive lung cancer | 25% of patients had 1 prior line of systemic therapy 74% had 2 or more prior lines of treatment | Crizotinib 250 mg twice per day | International | 226 (21) | 137 (13) |
| [24] | Phase 2, multicentre, nonrandomized, open-label | Adults n = 34 | MET alterations clear cell sarcoma | 26% had previous systemic therapy | Crizotinib 250 mg twice per day | Europe | 6 (18) | 2 (6) |
| [25] | Phase 2, multicentre, single-agent, open-label | Adults n = 48 | Rearrangement of TFE3 alveolar soft part sarcoma | 48% had received systemic therapy | Crizotinib 250 mg twice per day | Europe | 8 (17) | 2 (4) |
| [26] | Phase 2, single-arm, multicentre | Adults n = 127 | ROS1-rearranged lung cancer | 19% of patients had no prior therapy 42% had 1 prior line of therapy 39% had 2 or more prior lines of therapy | Crizotinib 250 mg twice per day | East Asia | 43 (34) | 15 (12) |
| [27] | Phase 2, multicentre, single-arm | Adults n = 20 | Inflammatory myofibroblastic tumours | 40% of patients had prior systemic therapy | Crizotinib 250 mg twice per day | Europe | 4 (20) | 2 (10) |
| [28] | Phase 2, multicentre, single-arm | Adults n = 34 | ROS1-rearranged lung cancer | 21% of patients had no prior therapy Other patients had 1 or more prior lines of therapy | Crizotinib 250 mg twice per day | Europe | 11 (32) | 3 (9) |
| [29] | Phase 2, open-label, randomized | Adults n = 152 | Papillary renal cell carcinoma | 7% of patients had prior systemic therapy | Crizotinib 250 mg twice per day | USA and Canada | 1 (3) | 0 (0) |
| [5] | Phase 3, randomized, open-label, multicentre | Adults n = 171 | ALK-positive lung cancer | No prior therapy | Crizotinib 250 mg twice per day | International | 42 (25) | 26 (15) |
| [30] | Phase 3, randomized, open-label, multicentre | Adults n = 104 | ALK-positive lung cancer | No prior therapy | Crizotinib 250 mg twice per day | East Asia | 43 (41) | 17 (16) |
| [31] | Prospective, multicentre study | Adults n = 11 | ALK-positive anaplastic large T-cell lymphoma | Previous chemotherapy | Crizotinib 250 mg twice per day | Europe and North America | 2 (18) | 0 (0) |
| [32] | Retrospective, monocentric | Adults n = 27 | ALK-positive anaplastic large T-cell lymphoma Lymphoma | 2 median previous lines (range 1–6) | Crizotinib 250 mg twice per day | Europe | 10 (37) | 8 (30) |
| [33] | Retrospective, national cohort | Adults n = 90 | c-MET and ROS1-positive lung cancer | Between 1–7 previous lines of systemic therapy | Crizotinib 250 mg twice per day | France | 21 (23) | 9 (10) |
| [34] | Retrospective, monocentre | Adults n = 35 | ROS1-rearranged lung cancer | 49% of patients had 1 previous line of therapy 31% of patients had 2 previous lines of therapy 20% of patients had 3 or more previous lines of therapy | Crizotinib 250 mg twice per day | China | 5 (14) | 1 (3) |
| [35] | Retrospective, monocentre | Adults n = 7 | ALK-positive lung cancer | No prior therapy | Crizotinib 250 mg twice per day | China | 1 (14) | 0 (0) |
| [36] | Chart review, retrospective study | Adults n = 38 | ALK-positive lung cancer | 55% had prior chemotherapy | Crizotinib 250 mg twice per day | Kuwait and Saudi Arabia | 6 (16) | 0 (0) |
| [37] | Retrospective, single-centre | Adults n = 104 | ALK-positive lung cancer | 61% of patients had no prior therapy Other patients had 1 or more prior lines of therapy | Crizotinib 250 mg twice per day | China | 20 (19) | 3 (3) |
| [38] | Retrospective, multicentre | Adults n = 2028 | ALK-positive lung cancer | 28% of patients had no prior lines of therapy Other patients had 1 or more prior lines of therapy | Crizotinib 250 mg twice per day | Japan | 278 (14) | 183 (9) |
| [39] | Retrospective, multicentre | Adults n = 91 | ALK-positive lung cancer | 44% of patients had no prior chemotherapy | Crizotinib 250 mg twice per day | Spain | 8 (9) | 4 (4) |
| [40] | Phase 1/2, multicentre, open-label | Adults n = 28 | RET-rearranged lung cancer | 21% of patients had 1 prior line of chemotherapy 79% had 2 or more prior lines of chemotherapy | Alectinib 450 mg twice per day | Japan | 1 (4) | 1 (4) |
| [41] | Phase 1/2, single-arm, open-label | Adults n = 47 | ALK-positive lung cancer | 13% of patients had no prior therapy 57% had 1 or 2 prior lines of therapy 30% had 3 or more prior lines of therapy | Dose escalation Alectinib 300 mg, 460 mg, 600 mg, 760 mg, 900 mg twice per day | USA | 3 (6) | 2 (4) |
| [42] | Phase 1/2, single-arm, open-label | Adults n = 58 | ALK-positive lung cancer | 2% of patients had no prior therapy Other patients had 1 or more prior lines of therapy | Dose escalation Alectinib 20 to 300 mg twice daily | Japan | 15 (26) | 4 (7) |
| [43] | Phase 2, multicentre | Adults n = 18 | ALK-positive lung cancer with poor performance status | 72% had no previous systemic therapy 28% had chemotherapy, crizotinib or both | Alectinib 300 mg twice per day | Japan | 3 (17) | 0 (0) |
| [44] | Phase 2, open-label, multicentre | Children and Adults n = 10 | ALK-positive anaplastic large T-cell lymphoma | 1 or 2 previous lines of systemic therapy | Alectinib 600 mg twice per day | Japan | 2 (20) | 2 (20) |
| [13] | Phase 2, multicentre, single-agent, open-label | Adults n = 87 | ALK-positive lung cancer, crizotinib-resistant | 74% of patients had previous chemotherapy | Alectinib 600 mg twice per day | USA and Canada | 4 (5) | 1 (1) |
| [4] | Phase 3, multicentre, randomized, open-label | Adults n = 70 | ALK-positive lung cancer, crizotinib pretreated | 2 prior lines of systemic therapy | Alectinib 600 mg twice per day | Europe and Asia | 2 (3) | 0 (0) |
| [45] | Phase 3, multicentre, randomized, open-label | Adults n = 303 | ALK-positive lung cancer | No prior therapy | Alectinib 600 mg twice per day or Crizotinib 250 mg twice per day | NR | Alectinib: 0 (0) vs. Crizotinib: 8 (5) | |
| [17] | Phase 3, multicentre, randomized, open-label | Adults n = 207 | ALK-positive lung cancer | 64% of patients had no prior systemic therapy Other patients had 1 line of systemic therapy | Alectinib 600 mg twice per day or Crizotinib 250 mg twice per day | Japan | Alectinib: 3 (3) vs. Crizotinib: 19 (18) | Alectinib: 2 (2) vs. Crizotinib: 14 (14) |
| [46] | Phase 3, randomized, open-label, multicentre | Adults n = 187 | ALK-positive lung cancer | No prior therapy | Alectinib 600 mg twice per day or Crizotinib 250 mg twice per day | China, South Korea, Thailand | Alectinib: 4 (3) vs. Crizotinib: 12 (19) | Alectinib: 0 (0) vs. Crizotinib: 7 (11) |
| [47] | Retrospective, multicentre | Adults n = 1221 | ALK-positive lung cancer | 18% of patients had no prior therapy 81% had 1 or more prior lines of therapy | Alectinib 300 mg twice daily | Japan | 93 (8) | 14 (1) |
| [48] | Phase 1, open-label | Adults n = 246 | ALK-positive lung cancer | 19% of patients had no previous treatment regimen Other patients had 1–4 or more previous lines of treatment | Ceritinib 750 mg in dose escalation | Europe and North America and Asia-Pacific | NR | 4 (2) |
| [49] | Phase 1, multicentre, open-label | Children n = 83 | ALK-positive malignancies | 55% of patients had 1–2 previous lines of therapy 25% of patients had 3 or more previous lines of therapy | Ceritinib dose escalation 500 mg/m2, 510 mg/m2 | International | 9 (11) | 6 (7) |
| [50] | Phase 1, multicentre, open-label | Adults n = 20 | ALK-positive lung cancer and inflammatory myofibroblastic tumours | 80% had prior ALK therapy | Dose escalationCeritinib 300 mg, 450 mg, 600 mg, and 750 mg per day | Japan | 4 (20) | 0 (0) |
| [51] | Phase 3, multicentre, randomized, open-label | Adults n = 76 | ALK-positive lung cancer | All patients had no prior therapy | Ceritinib 750 mg per day | Asia | 8 (10) | 2 (3) |
| [6] | Phase 3, randomized, controlled, open-label | Adults n = 115 | ALK-positive lung cancer | All patients had crizotinib and 1 or 2 lines of chemotherapy | Ceritinib 750 mg per day | International | 4 (3) | 1 (2) |
| [18] | Phase 3, randomized, open-label, multicentre | Adults n = 189 | ALK-positive lung cancer | No prior therapy | Ceritinib 750 mg per day | International | 9 (5) | 1 (1) |
| [10] | Phase 3, randomized, open-label, multicentre | Adults n = 11 | ALK-positive lung cancer | All patients had 1 prior line of chemotherapy | Ceritinib 750 mg per day | Japan | 1 (9) | 0 (0) |
| [52] | Phase 3, multicentre, randomized, open-label | Adults n = 275 | ALK-positive lung cancer | No prior therapy | Brigatinib 180 mg per day or Crizotinib 250 mg twice per day | International | Brigatinib: 3 (2) vs. Crizotinib: 13 (10) | Brigatinib: 3 (2) vs. Crizotinib: 11 (8) |
| [14] | Phase 3, randomized, open-label, multicentre | Adults n = 296 | ALK-positive lung cancer | No prior therapy | Lorlatinib 100 mg per day or Crizotinib 250 mg twice per day | International | Lorlatinib: 10 (7) vs. Crizotinib: 21 (15) | Lorlatinib: 1 (1) vs. Crizotinib: 12 (8) |
| [53] | Phase 3, randomized, open-label, multicentre | Adults n = 25 | ALK-positive lung cancer | No prior therapy | Lorlatinib 100 mg per day or Crizotinib 250 mg twice per day | Japan | Lorlatinib: 0 (0) vs. Crizotinib: 4 (18) | Lorlatinib: 0 (0) vs. Crizotinib: 3 (14) |
| [54] | Phase 1 and phase 2, single-arm, multicentre | Adults n = 193 | NTRK tumours | 73% of patients had prior chemotherapy | Entrectinib 600 mg/day | International | 11 (6) | 4 (2) |
| [55] | Phase 1 and phase 2, single-arm, multicentre | Adults n = 224 | ROS1-positive lung cancer | 63% of patients had prior systemic therapy | Entrectinib 600 mg/day | International | 10 (4) | 5 (2) |
| [56] | Phase 1/2, single-arm, multicentre | Children n = 43 | ALK, ROS1, NTRK solid tumours or primary CNS tumours | 77% of patients had prior chemotherapy | Dose escalationEntrectinib 250, 400, 550, 750 mg/m2 | North America, Europe, North Korea | 4 (9) | 3 (7) |
| [57] | Phase 1, dose escalation | Adults n = 63 | ALK- and ROS1- rearranged lung cancer | 25% of patients had prior ALK-TKI treatment 48% of patients had chemotherapy | TQ-B3139 50–800 mg | China | 8 (13) | 0 (0) |
| Ref. | Study Design | Population | Cancer Type | Treatment and Dose | Febrile Neutropenia (%) |
|---|---|---|---|---|---|
| [22] | Phase 1, open-label, multicentre | Children n = 79 | ALK-positive solid tumours, lymphomas, CNS tumours | Dose escalation crizotinib 100, 130, 165, 215, 280, and 365 mg/m2 twice per day | 10 |
| [23] | Phase 2, multicentre, single-arm | Adults n = 1069 | ALK-positive lung cancer | Crizotinib 250 mg twice per day | 3 |
| [25] | Phase 2, multicentre, single-agent, open-label | Adults n = 45 | TFE3-rearranged alveolar soft part sarcoma | Crizotinib 250 mg twice per day | 2 |
| [44] | Phase 2, open-label, multicentre | Children and Adults n = 10 | ALK-positive anaplastic large T-cell lymphoma | Alectinib 600 mg twice per day | 10 |
| [48] | Phase 1, open-label | Adults n = 255 | ALK-positive lung cancer | Ceritinib 750 mg in dose escalation | <1 |
| [6] | Phase 3, randomized, controlled, open-label | Adults n = 231 | ALK-positive lung cancer | Ceritinib 750 mg per day | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moinard-Butot, F.; Nannini, S.; Fischbach, C.; Abdallahoui, S.; Demarchi, M.; Petit, T.; Bender, L.; Schott, R. Anaplastic Lymphoma Kinase Inhibitor-Induced Neutropenia: A Systematic Review. Cancers 2023, 15, 4940. https://doi.org/10.3390/cancers15204940
Moinard-Butot F, Nannini S, Fischbach C, Abdallahoui S, Demarchi M, Petit T, Bender L, Schott R. Anaplastic Lymphoma Kinase Inhibitor-Induced Neutropenia: A Systematic Review. Cancers. 2023; 15(20):4940. https://doi.org/10.3390/cancers15204940
Chicago/Turabian StyleMoinard-Butot, Fabien, Simon Nannini, Cathie Fischbach, Safa Abdallahoui, Martin Demarchi, Thierry Petit, Laura Bender, and Roland Schott. 2023. "Anaplastic Lymphoma Kinase Inhibitor-Induced Neutropenia: A Systematic Review" Cancers 15, no. 20: 4940. https://doi.org/10.3390/cancers15204940
APA StyleMoinard-Butot, F., Nannini, S., Fischbach, C., Abdallahoui, S., Demarchi, M., Petit, T., Bender, L., & Schott, R. (2023). Anaplastic Lymphoma Kinase Inhibitor-Induced Neutropenia: A Systematic Review. Cancers, 15(20), 4940. https://doi.org/10.3390/cancers15204940





