Clinical Tools for Rectal Cancer Response Assessment following Neoadjuvant Treatment in the Era of Organ Preservation
Abstract
:Simple Summary
Abstract
1. Introduction
2. Methods
3. Watch and Wait (WW)
4. Why Patient Selection Remains Imperfect
5. Rectal Tumor Response Assessment
6. Biomarkers
7. Digital Rectal Exam
8. Endoscopy
9. Endoscopic Biopsy
10. Local Excision (Full- or Partial-Thickness Local Excision)
11. Imaging
12. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Cui, C.L.; Luo, W.Y.; Cosman, B.C.; Eisenstein, S.; Simpson, D.; Ramamoorthy, S.; Murphy, J.; Lopez, N. Cost Effectiveness of Watch and Wait Versus Resection in Rectal Cancer Patients with Complete Clinical Response to Neoadjuvant Chemoradiation. Ann. Surg. Oncol. 2022, 29, 1894–1907. [Google Scholar] [CrossRef]
- Kennedy, E.; Borowiec, A.; Schmocker, S.; Cho, C.; Brierley, J.; Li, S.; Victor, J.C.; Baxter, N. Patient and physician preferences for nonoperative management for low rectal cancer: Is it a reasonable treatment option? Dis. Colon. Rectum. 2018, 61, 1281–1289. [Google Scholar] [CrossRef]
- Garcia-Aguilar, J.; Patil, S.; Gollub, M.; Kim, J.; Yuval, J.; Thomspon, H.; Verheij, F.; Omer, D.; Lee, M.; Dunne, R.; et al. Organ preservation in patients with rectal adenocarcinoma treatment with total neoadjuvant therapy. J. Clin. Oncol. 2022, 40, 2546–2556. [Google Scholar] [CrossRef]
- Roxburgh, C.S. Organ preservation in rectal cancer: Towards the normal rather than the exception. Br. J. Surg. 2021, 108, 745–747. [Google Scholar] [CrossRef]
- Habr-Gama, A.; Sabbaga, J.; Gama-Rodrigues, J.; Juliao, G.; Proscurshim, I.; Aguilar, P.; Nadalin, W.; Perez, R. Watch and wait approach following extended neoadvjant chemoradiation for distal rectal cancer: Are we getting closer to anal cancer management. Dis. Colon. Rectum. 2013, 56, 1109–1117. [Google Scholar] [CrossRef]
- Akiyoshi, T.; Wang, Z.; Kaneyasu, T.; Gotoh, O.; Tanaka, N.; Amino, S.; Yamamoto, N.; Kawachi, H.; Mukai, T.; Hiyoshi, Y.; et al. Transcriptomic analysis of pretratment tumor biopsy samples, response to neoadjvant chemoradiotherapy, and survival in patients with advanced rectal cancer. JAMA Netw. Open 2023, 6, e2252140. [Google Scholar] [CrossRef]
- Ganesh, K.; Wu, C.; O’Rourke, K.P.; Szeglin, B.C.; Zheng, Y.; Sauvé, C.G.; Adileh, M.; Wasserman, I.; Marco, M.R.; Kim, A.S.; et al. A rectal cancer organoid platform to study individual responses to chemoradiation. Nat. Med. 2019, 10, 1607–1614. [Google Scholar] [CrossRef]
- São Julião, G.P.; Karagkounis, G.; Fernandez, L.M.; Habr-Gama, A.; Vailati, B.B.; Dattani, M.; Kalady, M.F.; Perez, R.O. Conditional Survival in Patients with Rectal Cancer and Complete Clinical Response Managed by Watch and Wait after Chemoradiation: Recurrence Risk Over Time. Ann. Surg. 2020, 272, 138–144. [Google Scholar] [CrossRef]
- Chadi, S.A.; Malcomson, L.; Ensor, J.; Riley, R.D.; Vaccaro, C.A.; Rossi, G.L.; Daniels, I.R.; Smart, N.J.; Osborne, M.E.; Beets, G.L.; et al. Factors affecting local regrowth after watch and wait for patients with a clinical complete response following chemoradiotherapy in rectal cancer (InterCoRe consortium): An individual participant data meta-analysis. Lancet Gastroenterol. Hepatol. 2018, 3, 825–836. [Google Scholar] [CrossRef]
- Fernandez, L.M.; São Julião, G.P.; Figueiredo, N.L.; Beets, G.L.; van der Valk, M.J.M.; Bahadoer, R.R.; Hilling, D.E.; Meershoek-Klein Kranenbarg, E.; Roodvoets, A.G.H.; Renehan, A.G.; et al. Conditional recurrence-free survival of clinical complete responders managed by watch and wait after neoadjuvant chemoradiotherapy for rectal cancer in the International Watch & Wait Database: A retrospective, international, multicentre registry study. Lancet Oncol. 2021, 22, 43–50. [Google Scholar]
- Bettoni, F.; Masotti, C.; Habr-Gama, A.; Correa, B.R.; Gama-Rodrigues, J.; Vianna, M.R.; Vailati, B.B.; São Julião, G.P.; Fernandez, L.M.; Galante, P.A.; et al. Intratumoral Genetic Heterogeneity in Rectal Cancer: Are Single Biopsies representative of the entirety of the tumor? Ann. Surg. 2017, 265, e4–e6. [Google Scholar] [CrossRef]
- Fokas, E.; Ströbel, P.; Fietkau, R.; Ghadimi, M.; Liersch, T.; Grabenbauer, G.G.; Hartmann, A.; Kaufmann, M.; Sauer, R.; Graeven, U.; et al. Tumor Regression Grading after Preoperative Chemoradiotherapy as a Prognostic Factor and Individual-Level Surrogate for Disease-Free Survival in Rectal Cancer. J. Natl. Cancer Inst. 2017, 109, djx095. [Google Scholar] [CrossRef]
- Schrag, D.; Shi, Q.; Weiser, M.R.; Gollub, M.J.; Saltz, L.B.; Musher, B.L.; Goldberg, J.; Al Baghdadi, T.; Goodman, K.A.; McWilliams, R.R.; et al. Preoperative Treatment of Locally Advanced Rectal Cancer. N. Engl. J. Med. 2023, 389, 322–334. [Google Scholar] [CrossRef]
- Conroy, T.; Etienne, P.; Emmanuel Rio, E.; Evesque, L.; Mesgouez-Nebout, N.; Vendrely, V.; Artignan, X.; Bouche, O.; Boileve, A.; Delaye, M.; et al. Total neoadhjvant therapy with mFOLFIRINOX versus preoperative chemoradiation in patients with locally advanced rectal cancer; 7-year results of PRODIGE 23 phase III trial, a UNICANCER GI trial. J. Clin. Oncol. 2023, 41, 702–715. [Google Scholar] [CrossRef]
- Bahadoer, R.R.; Dijkstra, E.A.; van Etten, B.; Marijnen, C.A.M.; Putter, H.; Kranenbarg, E.M.; Roodvoets, A.G.H.; Nagtegaal, I.D.; Beets-Tan, R.G.H.; Blomqvist, L.K.; et al. Short-course radiotherapy followed by chemotherapy before total mesorectal excision (TME) versus preoperative chemoradiotherapy, TME, and optional adjuvant chemotherapy in locally advanced rectal cancer (RAPIDO): A randomised, open-label, phase 3 trial. Lancet Oncol. 2021, 22, 29–42. [Google Scholar] [CrossRef]
- Emile, S.H.; Horesh, N.; Freund, M.R.; Garoufalia, Z.; Gefen, R.; Silva-Alvarenga, E.; Maron, D.J.; DaSilva, G.; Wexner, S.D. Trends in the Characteristics, Treatment, and Outcomes of Rectal Adenocarcinoma in the US From 2004 to 2019: A National Cancer Database Analysis. JAMA Oncol. 2023, 9, 355–364. [Google Scholar] [CrossRef]
- Hudson, E.M.; Noutch, S.; Brown, S.; Adapala, R.; Bach, S.P.; Burnett, C.; Burrage, A.; Gilbert, A.; Hawkins, M.; Howard, D.; et al. A Phase II trial of Higher Radiotherapy Dose In The Eradication of early rectal cancer (APHRODITE): Protocol for a multicentre, open-label randomised controlled trial. BMJ Open 2022, 12, e049119. [Google Scholar] [CrossRef]
- Verheij, F.; Rashid Omer, D.; Williams, H.; Buckley, J.; Lin, S.; Qin, L.; Thompson, H.; Yuval, H.; Gollub, M.; Wu, A.; et al. Sustained organ preservation in patients with rectal cancer treated with total neoadjuvant therapy; long term results of the OPRA trial. J. Clin. Oncol. 2023, 41, 3520. [Google Scholar] [CrossRef]
- Smith, J.J.; Strombom, P.; Chow, O.S.; Roxburgh, C.S.; Lynn, P.; Eaton, A.; Widmar, M.; Ganesh, K.; Yaeger, R.; Cercek, A.; et al. Assessment of a Watch-and-Wait Strategy for Rectal Cancer in Patients with a Complete Response after Neoadjuvant Therapy. JAMA Oncol. 2019, 5, e185896. [Google Scholar] [CrossRef]
- van der Valk, M.J.M.; Hilling, D.E.; Bastiaannet, E.; Meershoek-Klein Kranenbarg, E.; Beets, G.L.; Figueiredo, N.L.; Habr-Gama, A.; Perez, R.O.; Renehan, A.G.; van de Velde, C.J.H. IWWD Consortium. Long-term outcomes of clinical complete responders after neoadjuvant treatment for rectal cancer in the International Watch & Wait Database (IWWD): An international multicentre registry study. Lancet 2018, 391, 2537–2545. [Google Scholar]
- Fernandez, L.M.; São Julião, G.P.; Renehan, A.G.; Beets, G.L.; Papoila, A.L.; Vailati, B.B.; Bahadoer, R.R.; Kranenbarg, E.M.; Roodvoets, A.G.H.; Figueiredo, N.L.; et al. The Risk of Distant Metastases in Patients with Clinical Complete Response Managed by Watch and Wait After Neoadjuvant Therapy for Rectal Cancer: The Influence of Local Regrowth in the International Watch and Wait Database. Dis. Colon. Rectum. 2023, 66, 41–49. [Google Scholar] [CrossRef] [PubMed]
- Beets, G.L. Near-complete response following neoadjuvant therapy in rectal cancer: Wait a bit longer? Br. J. Surg. 2023, 110, 938–939. [Google Scholar] [CrossRef]
- Heald, R.J.; Santiago, I.; Pares, O.; Carvalho, C.; Figueiredo, N. The Perfect Total Mesorectal Excision Obviates the Need for Anything Else in the Management of Most Rectal Cancers. Clin. Colon. Rectal Surg. 2017, 30, 324–332. [Google Scholar]
- Perez, R.O.; Habr-Gama, A.; São Julião, G.P.; Gama-Rodrigues, J.; Sousa, A.H., Jr.; Campos, F.G.; Imperiale, A.R.; Lynn, P.B.; Proscurshim, I.; Nahas, S.C.; et al. Optimal timing for assessment of tumor response to neoadjuvant chemoradiation in patients with rectal cancer: Do all patients benefit from waiting longer than 6 weeks? Int. J. Radiat. Oncol. Biol. Phys. 2012, 84, 1159–1165. [Google Scholar] [CrossRef] [PubMed]
- Stijns, R.C.H.; Leijtens, J.; de Graaf, E.; Bach, S.P.; Beets, G.; Bremers, A.J.A.; Beets-Tan, R.G.H.; de Wilt, J.H.W. Endoscopy and MRI for restaging early rectal cancer after neoadjuvant treatment. Colorectal Dis. 2023, 25, 211–221. [Google Scholar] [CrossRef] [PubMed]
- Maas, M.; Lambregts, D.M.; Nelemans, P.J.; Heijnen, L.A.; Martens, M.H.; Leijtens, J.W.; Sosef, M.; Hulsewé, K.W.; Hoff, C.; Breukink, S.O.; et al. Assessment of Clinical Complete Response After Chemoradiation for Rectal Cancer with Digital Rectal Examination, Endoscopy, and MRI: Selection for Organ-Saving Treatment. Ann. Surg. Oncol. 2015, 22, 3873–3880. [Google Scholar] [CrossRef]
- Smith, J.J.; Chow, O.S.; Gollub, M.J.; Nash, G.M.; Temple, L.K.; Weiser, M.R.; Guillem, J.G.; Paty, P.B.; Avila, K.; Garcia-Aguilar, J.; et al. Organ Preservation in Rectal Adenocarcinoma: A phase II randomized controlled trial evaluating 3-year disease-free survival in patients with locally advanced rectal cancer treated with chemoradiation plus induction or consolidation chemotherapy, and total mesorectal excision or nonoperative management. BMC Cancer 2015, 23, 767. [Google Scholar]
- Thompson, H.; Kim, J.; Yuval, J.; Verheij Patil, S.; Gollub, M.; Wu, A.; Lee, M.; Hezel, A.; Marcet, J.; Cataldo, P.; et al. Survival and organ preservation according to clinical response after total neoadjuvant therapy in locally advanced rectal cancer patients: A secondary analysis from the organ preservation in rectal adenocarcinoma (OPRA) trial. J. Clin. Oncol. 2021, 39, 3509. [Google Scholar] [CrossRef]
- Felder, S.I.; Feuerlein, S.; Parsee, A.; Imanirad, I.; Sanchez, J.; Dessureault, S.; Kim, R.; Hoffe, S.; Frakes, J.; Costello, J. Endoscopic and MRI response evaluation following neoadjuvant treatment for rectal cancer: A pictorial review with matched MRI, endoscopic, and pathologic examples. Abdom Radiol. (N. Y.) 2021, 46, 1783–1804. [Google Scholar] [CrossRef]
- NCCN 4.2023 Version Guidelines. Available online: https://www.nccn.org/guidelines/recently-published-guidelines (accessed on 1 August 2023).
- Temmink, S.J.D.; Peeters, K.C.M.J.; Bahadoer, R.R.; Kranenbarg, E.M.; Roodvoets, A.G.H.; Melenhorst, J.; Burger, J.W.A.; Wolthuis, A.; Renehan, A.G.; Figueiredo, N.L.; et al. Watch and wait after neoadjuvant treatment in rectal cancer: Comparison of outcomes in patients with and without a complete response at first reassessment in the International Watch & Wait Database (IWWD). Br. J. Surg. 2023, 110, 676–684. [Google Scholar]
- Fokas, E.; Appelt, A.; Glynne-Jones, R.; Beets, G.; Perez, R.; Garcia-Aguilar, J.; Rullier, E.; Smith, J.J.; Marijnen, C.; Peters, F.P.; et al. International consensus recommendations on key outcome measures for organ preservation after (chemo)radiotherapy in patients with rectal cancer. Nat. Rev. Clin. Oncol. 2021, 18, 805–816. [Google Scholar] [CrossRef] [PubMed]
- Machado Carvalho, J.V.; Dutoit, V.; Corrò, C.; Koessler, T. Promises and Challenges of Predictive Blood Biomarkers for Locally Advanced Rectal Cancer Treated with Neoadjuvant Chemoradiotherapy. Cells 2023, 12, 413. [Google Scholar] [CrossRef] [PubMed]
- Dayde, D.; Tanaka, I.; Jain, R.; Tai, M.C.; Taguchi, A. Predictive and Prognostic Molecular Biomarkers for Response to Neoadjuvant Chemoradiation in Rectal Cancer. Int. J. Mol. Sci. 2017, 18, 573. [Google Scholar] [CrossRef] [PubMed]
- Guillem, J.G.; Chessin, D.B.; Shia, J.; Moore, H.G.; Mazumdar, M.; Bernard, B.; Paty, P.B.; Saltz, L.; Minsky, B.D.; Weiser, M.R.; et al. Clinical examination following preoperative chemoradiation for rectal cancer is not a reliable surrogate end point. J. Clin. Oncol. 2005, 23, 3475–3479. [Google Scholar] [CrossRef] [PubMed]
- Huh, J.W.; Lee, W.Y.; Park, Y.A.; Cho, Y.B.; Yun, S.H.; Kim, H.C.; Chun, H.K. Intraoperative staging by surgeons in patients with rectal cancer after preoperative chemoradiation: Diagnostic accuracy and prognostic value. J. Cancer Res. Clin. Oncol. 2014, 140, 1221–1227. [Google Scholar] [CrossRef]
- Kahn, H.; Alexander, A.; Rakinic, J.; Nagle, D.; Fry, R. Preoperative staging of irradiated rectal cancers using digital rectal examination, computed tomography, endorectal ultrasound, and magnetic resonance imaging does not accurately predict T0,N0 pathology. Dis. Colon. Rectum. 1997, 40, 140–144. [Google Scholar] [CrossRef]
- Felder, S.I.; Patil, S.; Kennedy, E.; Garcia-Aguilar, J. Endoscopic Feature and Response Reproducibility in Tumor Assessment after Neoadjuvant Therapy for Rectal Adenocarcinoma. Ann. Surg. Oncol. 2021, 28, 5205–5223. [Google Scholar] [CrossRef]
- van der Sande, M.E.; Maas, M.; Melenhorst, J.; Breukink, S.O.; van Leerdam, M.E.; Beets, G.L. Predictive Value of Endoscopic Features for a Complete Response After Chemoradiotherapy for Rectal Cancer. Ann. Surg. 2021, 274, e541–e547. [Google Scholar] [CrossRef]
- Maas, M.; Nelemans, P.J.; Valentini, V.; Das, P.; Rödel, C.; Kuo, L.J.; Calvo, F.A.; García-Aguilar, J.; Glynne-Jones, R.; Haustermans, K.; et al. Long-term outcome in patients with a pathological complete response after chemoradiation for rectal cancer: A pooled analysis of individual patient data. Lancet Oncol. 2010, 11, 835–844. [Google Scholar] [CrossRef]
- Habr-Gama, A.; Perez, R.O.; Wynn, G.; Marks, J.; Kessler, H.; Gama-Rodrigues, J. Complete clinical response after neoadjuvant chemoradiation therapy for distal rectal cancer: Characterization of clinical and endoscopic findings for standardization. Dis. Colon. Rectum. 2010, 53, 1692–1698. [Google Scholar] [CrossRef]
- Safatle-Ribeiro, A.V.; Ribeiro, U., Jr.; Lata, J.; Baba, E.R.; Lenz, L.; da Costa Martins, B.; Kawaguti, F.; Moura, R.N.; Pennacchi, C.; Gusmon, C.; et al. The Role of Probe-Based Confocal Laser Endomicroscopy (pCLE) in the Diagnosis of Sustained Clinical Complete Response Under Watch-and-Wait Strategy After Neoadjuvant Chemoradiotherapy for Locally Advanced Rectal Adenocarcinoma: A Score Validation. J. Gastrointest. Surg. 2023. epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Kimura, C.M.S.; Kawaguti, F.S.; Horvat, N.; Nahas, C.S.R.; Marques, C.F.S.; Pinto, R.A.; de Rezende, D.T.; Segatelli, V.; Safatle-Ribeiro, A.V.; Junior, U.R.; et al. Magnifying chromoendoscopy is a reliable method in the selection of rectal neoplasms for local excision. Tech. Coloproctol. 2023. epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Thompson, H.M.; Kim, J.K.; Jimenez-Rodriguez, R.M.; Garcia-Aguilar, J.; Veeraraghavan, H. Deep Learning-Based Model for Identifying Tumors in Endoscopic Images From Patients With Locally Advanced Rectal Cancer Treated With Total Neoadjuvant Therapy. Dis. Colon. Rectum. 2023, 66, 383–391. [Google Scholar] [CrossRef] [PubMed]
- Smith, F.M.; Chang, K.H.; Sheahan, K.; Hyland, J.; O’Connell, P.R.; Winter, D.C. The surgical significance of residual mucosal abnormalities in rectal cancer following neoadjuvant chemoradiotherapy. Br. J. Surg. 2012, 99, 993–1001. [Google Scholar] [CrossRef] [PubMed]
- Smith, F.M.; Wiland, H.; Mace, A.; Pai, R.K.; Kalady, M.F. Clinical criteria underestimate complete pathological response in rectal cancer treated with neoadjuvant chemoradiotherapy. Dis. Colon. Rectum. 2014, 57, 311–315. [Google Scholar] [CrossRef]
- Habr-Gama, A.; Perez, R.O. The surgical significance of residual mucosal abnormalities in rectal cancer following neoadjuvant chemoradiotherapy. Br. J. Surg. 2012, 99, 1601–1602. [Google Scholar] [CrossRef]
- Custers, P.A.; Geubels, B.M.; Beets, G.L.; Lambregts, D.M.J.; van Leerdam, M.E.; van Triest, B.; Maas, M. Defining near-complete response following (chemo)radiotherapy for rectal cancer: Systematic review. Br. J. Surg. 2022, 110, 43–49. [Google Scholar] [CrossRef]
- Perez, R.O.; Cerdán-Santacruz, C.; São Julião, G.P. Near-complete response following neoadjuvant therapy in rectal cancer: Resect now? Br. J. Surg. 2023, 110, 936–937. [Google Scholar] [CrossRef]
- Duldulao, M.P.; Lee, W.; Streja, L.; Chu, P.; Li, W.; Chen, Z.; Kim, J.; Garcia-Aguilar, J. Distribution of residual cancer cells in the bowel wall after neoadjuvant chemoradiation in patients with rectal cancer. Dis. Colon. Rectum. 2013, 56, 142–149. [Google Scholar] [CrossRef]
- Verrijssen, A.S.; Guillem, J.; Perez, R.; Bujko, K.; Guedj, N.; Habr-Gama, A.; Houben, R.; Goudkade, D.; Melenhorst, J.; Buijsen, J.; et al. Microscopic intramural extension of rectal cancer after neoadjuvant chemoradiation: A meta-analysis based on individual patient data. Radiother. Oncol. 2020, 144, 37–45. [Google Scholar] [CrossRef]
- You, Y.N.; Hardiman, K.M.; Bafford, A.; Poylin, V.; Francone, T.D.; Davis, K.; Paquette, I.M.; Steele, S.R.; Feingold, D.L.; On Behalf of the Clinical Practice Guidelines Committee of the American Society of Colon and Rectal Surgeons. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Management of Rectal Cancer. Dis. Colon. Rectum. 2020, 63, 1191–1222. [Google Scholar] [CrossRef]
- Sprenger, T.; Rothe, H.; Conradi, L.C.; Beissbarth, T.; Kauffels, A.; Kitz, J.; Homayounfar, K.; Wolff, H.; Ströbel, P.; Ghadimi, M.; et al. Stage-Dependent Frequency of Lymph Node Metastases in Patients With Rectal Carcinoma After Preoperative Chemoradiation: Results from the CAO/ARO/AIO-94 Trial and From a Comparative Prospective Evaluation with Extensive Pathological Workup. Dis. Colon. Rectum. 2016, 59, 377–385. [Google Scholar] [CrossRef] [PubMed]
- Perez, R.O.; Habr-Gama, A.; Lynn, P.B.; São Julião, G.P.; Bianchi, R.; Proscurshim, I.; Gama-Rodrigues, J. Transanal endoscopic microsurgery for residual rectal cancer (ypT0-2) following neoadjuvant chemoradiation therapy: Another word of caution. Dis. Colon. Rectum. 2013, 56, 6–13. [Google Scholar] [CrossRef] [PubMed]
- Smith, F.M.; Ahad, A.; Perez, R.O.; Marks, J.; Bujko, K.; Heald, R.J. Local Excision Techniques for Rectal Cancer After Neoadjuvant Chemoradiotherapy: What Are We Doing? Dis. Colon. Rectum. 2017, 60, 228–239. [Google Scholar] [CrossRef] [PubMed]
- Smith, F.M.; Wiland, H.; Mace, A.; Pai, R.K.; Kalady, M.F. Depth and lateral spread of microscopic residual rectal cancer after neoadjuvant chemoradiation: Implications for treatment decisions. Colorectal Dis. 2014, 16, 610–615. [Google Scholar] [CrossRef] [PubMed]
- Hayden, D.M.; Jakate, S.; Pinzon, M.C.; Giusto, D.; Francescatti, A.B.; Brand, M.I.; Saclarides, T.J. Tumor scatter after neoadjuvant therapy for rectal cancer: Are we dealing with an invisible margin? Dis. Colon. Rectum. 2012, 55, 1206–1212. [Google Scholar] [CrossRef]
- Marks, J.H.; Valsdottir, E.B.; DeNittis, A.; Yarandi, S.S.; Newman, D.A.; Nweze, I.; Mohiuddin, M.; Marks, G.J. Transanal endoscopic microsurgery for the treatment of rectal cancer: Comparison of wound complication rates with and without neoadjuvant radiation therapy. Surg. Endosc. 2009, 23, 1081–1087. [Google Scholar] [CrossRef]
- Serra-Aracil, X.; Pericay, C.; Badia-Closa, J.; Golda, T.; Biondo, S.; Hernández, P.; Targarona, E.; Borda-Arrizabalaga, N.; Reina, A.; Delgado, S.; et al. Short-term outcomes of chemoradiotherapy and local excision versus total mesorectal excision in T2-T3ab,N0,M0 rectal cancer: A multicentre randomised, controlled, phase III trial (the TAU-TEM study). Ann. Oncol. 2023, 34, 78–90. [Google Scholar] [CrossRef]
- Hompes, R.; McDonald, R.; Buskens, C.; Lindsey, I.; Armitage, N.; Hill, J.; Scott, A.; Mortensen, N.J.; Cunningham, C.; Association of Coloproctology of Great Britain and Ireland Transanal Endoscopic Microsurgery Collaboration. Completion surgery following transanal endoscopic microsurgery: Assessment of quality and short- and long-term outcome. Colorectal Dis. 2013, 15, e576–e581. [Google Scholar] [CrossRef]
- Serra-Aracil, X.; Galvez Saldaña, A.; Mora-Lopez, L.L.; Montes, N.; Pallisera-Lloveras, A.; Serra-Pla, S.; Pericay, C.; Navarro-Soto, S. Completion Surgery in Unfavorable Rectal Cancer after Transanal Endoscopic Microsurgery: Does It Achieve Satisfactory Sphincter Preservation, Quality of Total Mesorectal Excision Specimen, and Long-term Oncological Outcomes? Dis. Colon. Rectum. 2021, 64, 200–208. [Google Scholar] [CrossRef]
- Morino, M.; Allaix, M.E.; Arolfo, S.; Arezzo, A. Previous transanal endoscopic microsurgery for rectal cancer represents a risk factor for an increased abdominoperineal resection rate. Surg. Endosc. 2013, 27, 3315–3321. [Google Scholar] [CrossRef] [PubMed]
- Rullier, E.; Rouanet, P.; Tuech, J.J.; Valverde, A.; Lelong, B.; Rivoire, M.; Faucheron, J.L.; Jafari, M.; Portier, G.; Meunier, B.; et al. Organ preservation for rectal cancer (GRECCAR 2): A prospective, randomised, open-label, multicentre, phase 3 trial. Lancet 2017, 29, 469–479. [Google Scholar] [CrossRef] [PubMed]
- Habr-Gama, A.; Lynn, P.B.; Jorge, J.M.; São Julião, G.P.; Proscurshim, I.; Gama-Rodrigues, J.; Fernandez, L.M.; Perez, R.O. Impact of Organ-Preserving Strategies on Anorectal Function in Patients with Distal Rectal Cancer Following Neoadjuvant Chemoradiation. Dis. Colon. Rectum. 2016, 59, 264–269. [Google Scholar] [CrossRef]
- Hallam, S.; Messenger, D.E.; Thomas, M.G. A Systematic Review of Local Excision After Neoadjuvant Therapy for Rectal Cancer: Are ypT0 Tumors the Limit? Dis. Colon. Rectum. 2016, 59, 984–997. [Google Scholar] [CrossRef] [PubMed]
- Patel, U.B.; Blomqvist, L.K.; Taylor, F.; George, C.; Guthrie, A.; Bees, N.; Brown, G. MRI after treatment of locally advanced rectal cancer: How to report tumor response—The MERCURY experience. AJR Am. J. Roentgenol. 2012, 199, 486–495. [Google Scholar] [CrossRef] [PubMed]
- Jayaprakasam, V.S.; Alvarez, J.; Omer, D.M.; Gollub, M.J.; Smith, J.J.; Petkovska, I. Watch-and-Wait Approach to Rectal Cancer: The Role of Imaging. Radiology 2023, 307, e221529. [Google Scholar] [CrossRef] [PubMed]
- van der Paardt, M.P.; Zagers, M.B.; Beets-Tan, R.G.; Stoker, J.; Bipat, S. Patients who undergo preoperative chemoradiotherapy for locally advanced rectal cancer restaged by using diagnostic MR imaging: A systematic review and meta-analysis. Radiology 2013, 269, 101–112. [Google Scholar] [CrossRef]
- Hall, W.A.; Li, J.; You, Y.N.; Gollub, M.J.; Grajo, J.R.; Rosen, M.; dePrisco, G.; Yothers, G.; Dorth, J.A.; Rahma, O.E.; et al. Prospective Correlation of Magnetic Resonance Tumor Regression Grade With Pathologic Outcomes in Total Neoadjuvant Therapy for Rectal Adenocarcinoma. J. Clin. Oncol. 2023. epub ahead of print. [Google Scholar] [CrossRef]
- El Khababi, N.; Beets-Tan, R.G.H.; Tissier, R.; Lahaye, M.J.; Maas, M.; Curvo-Semedo, L.; Dresen, R.C.; Nougaret, S.; Beets, G.L.; Lambregts, D.M.J.; et al. Sense and nonsense of yT-staging on MRI after chemoradiotherapy in rectal cancer. Colorectal Dis. 2023. epub ahead of print. [Google Scholar] [CrossRef]
- El Khababi, N.; Beets-Tan, R.G.H.; Tissier, R.; Lahaye, M.J.; Maas, M.; Curvo-Semedo, L.; Dresen, R.C.; Nougaret, S.; Beets, G.L.; Lambregts, D.M.J.; et al. Comparison of MRI response evaluation methods in rectal cancer: A multicentre and multireader validation study. Eur. Radiol. 2023, 33, 4367–4377. [Google Scholar] [CrossRef]
- Haak, H.E.; Maas, M.; Lahaye, M.J.; Boellaard, T.N.; Delli Pizzi, A.; Mihl, C.; van der Zee, D.; Fabris, C.; van der Sande, M.E.; Melenhorst, J.; et al. Selection of Patients for Organ Preservation After Chemoradiotherapy: MRI Identifies Poor Responders Who Can Go Straight to Surgery. Ann. Surg. Oncol. 2020, 27, 2732–2739. [Google Scholar] [CrossRef]
- Crimì, F.; Spolverato, G.; Lacognata, C.; Garieri, M.; Cecchin, D.; Urso, E.D.; Zucchetta, P.; Pucciarelli, S.; Pomerri, F. 18F-FDG PET/MRI for Rectal Cancer TNM Restaging After Preoperative Chemoradiotherapy: Initial Experience. Dis. Colon. Rectum. 2020, 63, 310–318. [Google Scholar] [CrossRef]
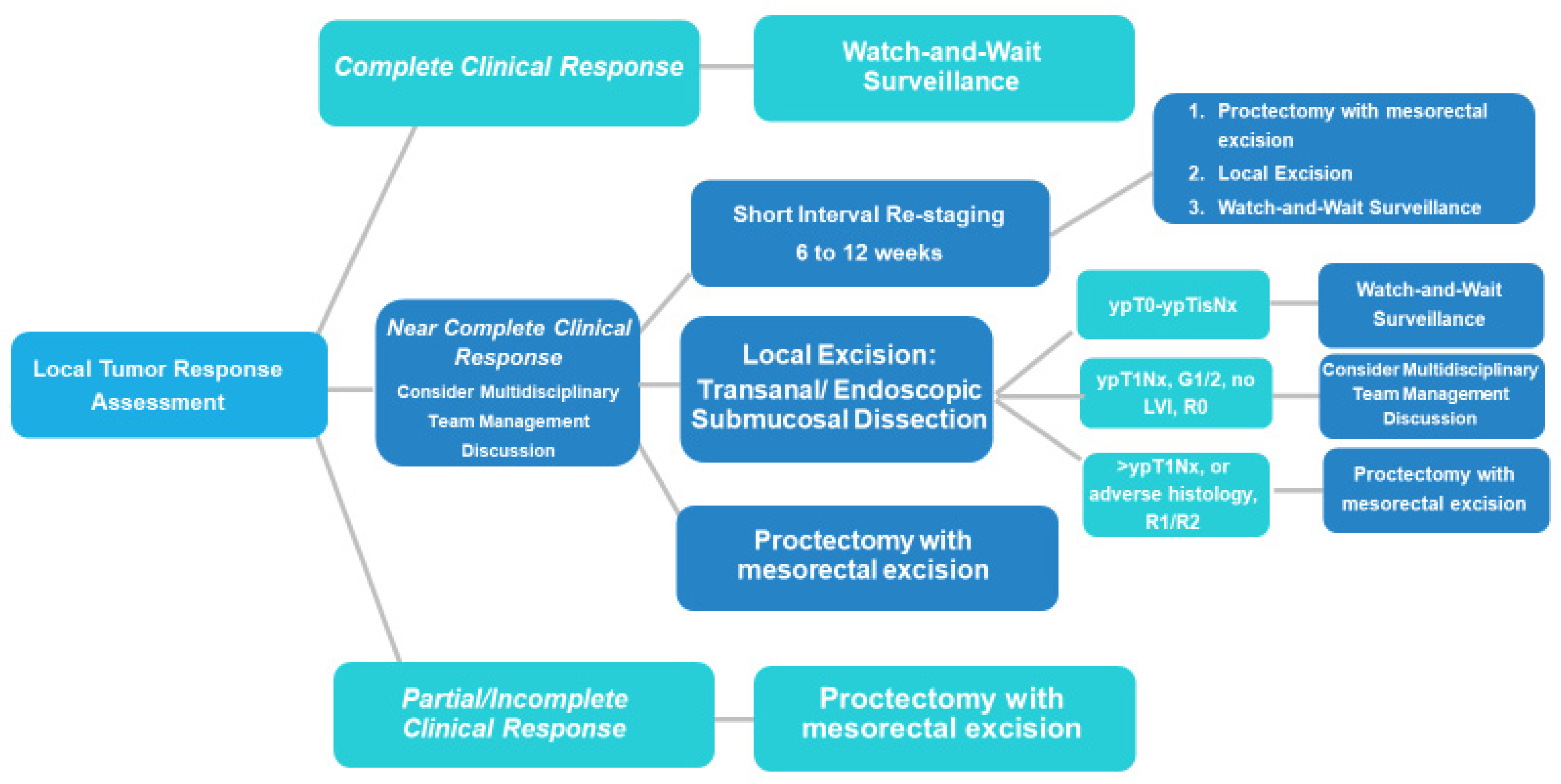
| Complete Clinical Response (cCR) | Near-Complete Clinical Response (nCR) | Incomplete Clinical Response (iCR) | |
|---|---|---|---|
| Endoscopy | Flat white scar Telangiectasia Absence of ulcers and mucosal nodularity | Small mucosal nodules/minor mucosal irregularities Superficial ulceration Mild, persistent erythema of the scar | Visible tumor |
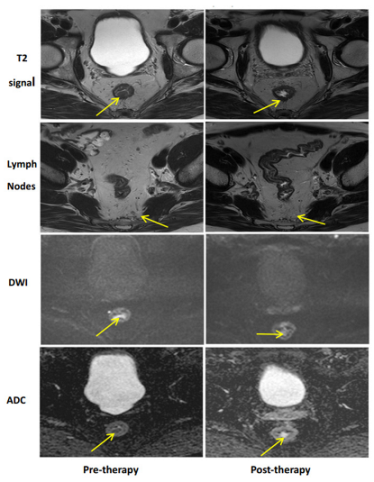
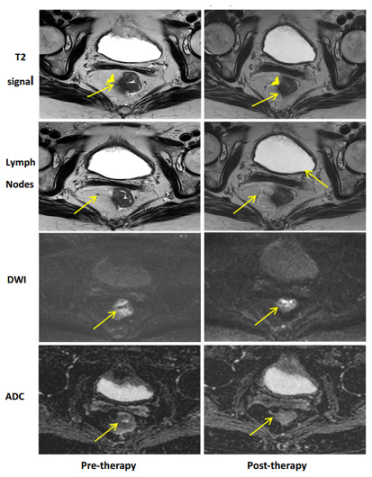
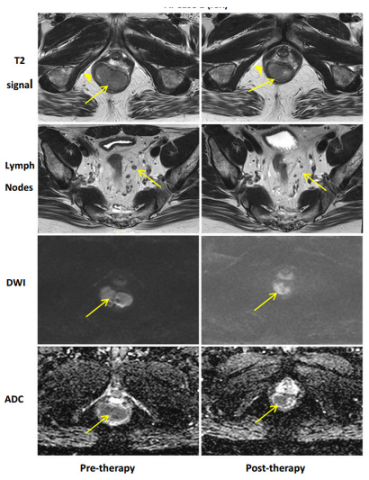
| MRI-T2W | Only a dark T2 signal; no intermediate signal AND No visible lymph nodes | Mostly dark T2 signal, some intermediate signal AND/OR Partial regression of lymph nodes | More intermediate than a dark T2 signal, no T2 scar AND/OR No regression of lymph nodes |
| MRI-DWI | No visible tumor on the B800–B1000 signal AND/OR Lack of or low signal on the ADC map A uniform linear signal in the wall above the tumor is acceptable | Significant regression of the signal on B800–B1000 AND/OR Minimal or low residual signal on the ADC map | Insignificant regression of signal on B800–B1000 AND/OR Obvious low signal on the ADC map |
| Endoscopic Finding | |||
|---|---|---|---|
| Flat, white scar | 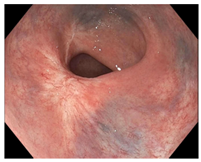 | 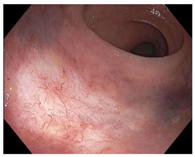 | 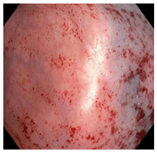 |
| Telangiectasia | 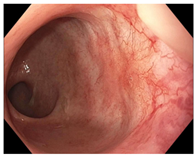 | 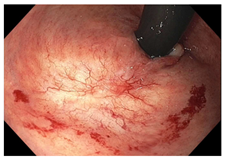 | 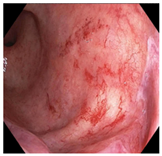 |
| Small mucosal nodules, minor mucosal irregularities |  | 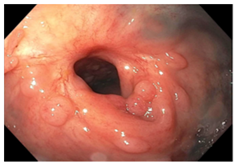 | 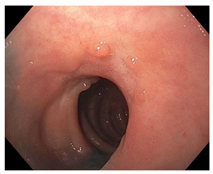 |
| Superficial ulceration |  |  |  |
| Persisting erythema of scar | 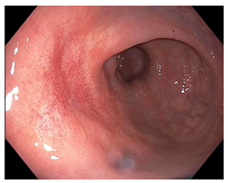 | 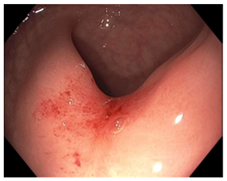 | 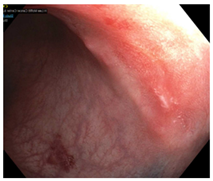 |
| Complete Response | Near-Complete Response | Incomplete Response |
|---|---|---|
 |  |  |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stefanou, A.J.; Dessureault, S.; Sanchez, J.; Felder, S. Clinical Tools for Rectal Cancer Response Assessment following Neoadjuvant Treatment in the Era of Organ Preservation. Cancers 2023, 15, 5535. https://doi.org/10.3390/cancers15235535
Stefanou AJ, Dessureault S, Sanchez J, Felder S. Clinical Tools for Rectal Cancer Response Assessment following Neoadjuvant Treatment in the Era of Organ Preservation. Cancers. 2023; 15(23):5535. https://doi.org/10.3390/cancers15235535
Chicago/Turabian StyleStefanou, Amalia J., Sophie Dessureault, Julian Sanchez, and Seth Felder. 2023. "Clinical Tools for Rectal Cancer Response Assessment following Neoadjuvant Treatment in the Era of Organ Preservation" Cancers 15, no. 23: 5535. https://doi.org/10.3390/cancers15235535
APA StyleStefanou, A. J., Dessureault, S., Sanchez, J., & Felder, S. (2023). Clinical Tools for Rectal Cancer Response Assessment following Neoadjuvant Treatment in the Era of Organ Preservation. Cancers, 15(23), 5535. https://doi.org/10.3390/cancers15235535




