Alternating Gemcitabine/Nab-Paclitaxel (GA) and 5-FU/Leucovorin/Irinotecan (FOLFIRI) as First-Line Treatment for De Novo Metastatic Pancreatic Cancer (MPC): Safety and Effect
Abstract
:Simple Summary
Abstract
1. Introduction
2. Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lippi, G.; Mattiuzzi, C. The global burden of pancreatic cancer. Arch. Med. Sci. 2020, 16, 820–824. [Google Scholar] [CrossRef]
- Rahib, L.; Smith, B.D.; Aizenberg, R.; Rosenzweig, A.B.; Fleshman, J.M.; Matrisian, L.M. Projecting cancer incidence and deaths to 2030: The unex-pected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014, 74, 2913–2921. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. An Update on Cancer Deaths in the United States; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2019. [Google Scholar]
- American Cancer Society. Cancer Facts and Figures 2021; American Cancer Society: Atlanta, GA, USA, 2021. [Google Scholar]
- Lucas, A.L.; Malvezzi, M.; Carioli, G.; Negri, E.; La Vecchia, C.; Boffetta, P.; Bosetti, C. Global Trends in Pancreatic Cancer Mortality From 1980 Through 2013 and Predictions for 2017. Clin. Gastroenterol. Hepatol. 2016, 14, 1452–1462.e4. [Google Scholar] [CrossRef] [PubMed]
- Sohal, D.P.S.; Kennedy, E.B.; Cinar, P.; Conroy, T.; Copur, M.S.; Crane, C.H.; Garrido-Laguna, I.; Lau, M.W.; Johnson, T.; Krishnamurthi, S.; et al. Metastatic Pancreatic Cancer: ASCO Guideline Update. J. Clin. Oncol. 2020, 38, 3217–3230. [Google Scholar] [CrossRef] [PubMed]
- Moore, M.J.; Goldstein, D.; Hamm, J.; Figer, A.; Hecht, J.R.; Gallinger, S.; Au, H.J.; Murawa, P.; Walde, D.; Wolff, R.A.; et al. Erlotinib Plus Gemcitabine Compared with Gemcitabine Alone in Patients with Advanced Pancreatic Cancer: A Phase III Trial of the National Cancer Institute of Canada Clinical Trials Group. J. Clin. Oncol. 2007, 25, 1960–1966. [Google Scholar] [CrossRef] [PubMed]
- Fine, R.L.; Fogelman, D.R.; Schreibman, S.M.; Desai, M.; Sherman, W.; Strauss, J.; Guba, S.; Andrade, R.; Chabot, J. The gemcitabine, docetaxel and capecitabine (GTX) regimen for metastatic pancreatic cancer: A retrospective analysis. Cancer Chemother. Pharmacol. 2008, 61, 167–175. [Google Scholar] [CrossRef]
- Conroy, T.; Desseigne, F.; Ychou, M.; Bouché, O.; Guimbaud, R.; Bécouarn, Y.; Adenis, A.; Raoul, J.-L.; Gourgou-Bourgade, S.; de la Fouchardière, C.; et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N. Engl. J. Med. 2011, 364, 1817–1825. [Google Scholar] [CrossRef] [PubMed]
- Von Hoff, D.D.; Ervin, T.; Arena, F.P.; Chiorean, E.G.; Infante, J.; Moore, M.; Seay, T.; Tjulandin, S.A.; Ma, W.W.; Saleh, M.N.; et al. Increased Survival in Pancreatic Cancer with nab-Paclitaxel plus Gemcitabine. N. Engl. J. Med. 2013, 369, 1691–1703. [Google Scholar] [CrossRef]
- Strickler, J.H.; Satake, H.; George, T.J.; Yaeger, R.; Hollebecque, A.; Garrido-Laguna, I.; Schuler, M.; Burns, T.F.; Coveler, A.L.; Falchook, G.S.; et al. Sotorsib in KRAS p.G12C-mutated advanced pancreatic cancer. N. Engl. J. Med. 2023, 388, 33–43. [Google Scholar] [CrossRef]
- Aung, K.L.; Fischer, S.E.; Denroche, R.E.; Jang, G.-H.; Dodd, A.; Creighton, S.; Southwood, B.; Liang, S.-B.; Chadwick, D.; Zhang, A.; et al. Genomics-driven precision medicine for advanced pan-creatic cancer: Early results from the COMPASS trial. Clin. Cancer Res. 2018, 26, 1344–1354. [Google Scholar] [CrossRef]
- Wainberg, Z.A.; Melisi, D.; Macarulla, T.; Pazo-Cid, R.; Chandana, S.R.; De La Fouchardiere, C.; Dean, A.P.; Kiss, I.; Lee, W.; Goetze, T.O.; et al. NALIRIFOX versus nab-paclitaxel and gemcita-bine in treatment-naïve patients with metastatic pancreatic ductal adenocarcinoma (NAPOLI 3): A randomized, open-label phase 3 trial. Lancet 2023, 402, P1272–P1281. [Google Scholar] [CrossRef] [PubMed]
- Goldie, J.H.; Coldman, A.J. A mathematic model for relating the drug sensitivity of tumors to their spontaneous mutation rate. Cancer Treat. Rep. 1979, 63, 1727–1733. [Google Scholar] [PubMed]
- Goldie, J.H.; Coldman, A.J.; Gudauskas, G.A. Rationale for the use of alternating non-cross-resistant chemotherapy. Cancer Treat. Rep. 1982, 66, 439–449. [Google Scholar] [PubMed]
- Picozzi, V.J.; Leach, J.W.; Seng, J.E.; Anthony, S.P.; Mena, R.; Larson, T.; Borazanci, E.H.; Weiss, G.J.; Lin, S.-L.B.; Jameson, G.S.; et al. Initial gemcitabine/nab-paclitaxel followed by sequential mFOLFI RINOX or alternating mFOLFIRI in metastatic pancreatic cancer: The SEENA-1 study. J. Clin. Oncol. 2017, 35 (Suppl. S4), 359. [Google Scholar] [CrossRef]
- Picozzi, V.J.; Lin, B.S.-L.; Mandelson, M.T. Gemcitabine/nab-paclitaxel alternating with 5-FU/leucovorin/ irinotecan in 1st line metastatic pancreatic cancer. J. Clin. Oncol. 2018, 36 (Suppl. S15), e16218. [Google Scholar] [CrossRef]
- Assenat, E.; De La Fouchardiere, C.; Mollevi, C.; Samalin, E.; Portales, F.; Desseigne, F.; Carenco, C.; Dupuy, M.; Lopez-Martinez, E.; Fiess, C.; et al. Sequential treatment with nab-paclitaxel plus gemcitabine and folfirinox in metastatic pancreatic adenocarcinoma: GABRINOX phase II re-sults. J. Clin. Oncol. 2018, 36 (Suppl. S15), 4109. [Google Scholar] [CrossRef]
- Oken, M.M.; Creech, R.H.; Tormey, D.C.; Horton, J.; Davis, T.E.; McFadden, E.T.; Carbone, P.P. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am. J. Clin. Oncol. 1982, 5, 649–655. [Google Scholar] [CrossRef]
- Poruk, K.E.; Gay, D.Z.; Brown, K.; Mulvihill, J.D.; Boucher, K.M.; Scaife, C.L.; Firpo, M.A.; Mulvihill, S.J. The Clinical Utility of CA 19-9 in Pancreatic Adenocarcinoma: Diagnostic and Prognostic Updates. Curr. Mol. Med. 2013, 13, 340–351. [Google Scholar]
- StataCorp. STATA Statistical Software: Release 17; StatCorp LLC: College Station, TX, USA, 2021. [Google Scholar]
- O’Reilly, E.M.; Melisi, D.; Macarulla, T.; Cid, R.A.P.; Chandana, S.R.; De La Fouchardiere, C.; Dean, A.P.; Kiss, I.; Lee, W.J.; Goetze, T.O.; et al. Liposomal irinotecan + 5-fluorouracil/leucovorin + oxaliplatin (NALIRIFOX) versus nab-paclitaxel + gemcitabine in treatment-naive patients with metastatic pancreatic ductal adenocarcinoma (mPDAC): 12- and 18-month survival rates from the phase 3 NAPOLI 3 trial. J. Clin. Oncol. 2023, 41 (Suppl. S16), 4006. [Google Scholar] [CrossRef]
- Safran, H.; Mantripragada, K.; Perez, K.; Charpentier, K.; Miner, T.; Dipetrillo, T.; Kuritzky, B.; Bishop, K.D.; Apor, E.; Rosati, K. FOLFOX + Nab-paclitaxel for advanced pancreatic cancer: A Brown University oncology research group phase I study. Am. J. Clin. Oncol. 2016, 39, 619–622. [Google Scholar] [CrossRef]
- Sahai, V.; Saif, M.W.; Kalyan, A.; Philip, P.A.; Rocha-Lima, C.M.; Ocean, A.; Ondovik, M.S.; Simeone, D.M.; Banerjee, S.; Bhore, R.; et al. A phase I/II open-label multicenter single-arm study of metronomic 5-fluorouriacil plus nab-paclitaxel, bevacizumab, leucovorin, and oxaliplatin in patients with metastatic pancreatic cancer. J. Pancreat. Cancer 2019, 5, 35–42. [Google Scholar] [CrossRef]
- Giommoni, E.; Maiello, E.; Vaccaro, V.; Rondini, E.; Vivaldi, C.; Tortora, G.; Toppo, L.; Giordano, G.; Latiano, T.P.; Lamperini, C.; et al. Activity and safety of nab-FOLFIRI and nab-FOLFOX as first-line treatment of metastatic pancreatic cancer. J. Clin. Oncol. 2018, 36, 351. [Google Scholar] [CrossRef]
- Joshi, S.S.; Catenacci, D.V.; Karrison, T.G.; Peterson, J.D.; Zalupski, M.M.; Sehdev, A.; Wade, J.; Sadiq, A.; Picozzi, V.J.; Amico, A.; et al. Clinical assessment of 5-fluorouracil/leucovorin, nab-paclitaxel. Clin. Cancer Res. 2020, 26, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Assenat, E.; De La Fouchardiere, C.; Mollevi, C.; Samalin, E.; Portales, F.; Desseigne, F.; Carenco, C.; Dupuy, M.; Lopez-Martinez, E.; Fiess, C.; et al. Gabrinox: A phase I-II of nab-paclitaxel plus gemcitabine followed by FOLFIRINOX in metastatic pancreatic adenocarcinoma. J. Clin. Oncol. 2016, 34, 315688. [Google Scholar] [CrossRef]
- Carrato, A.; Pazo-Cid, R.; Macarulla, T.; Gallego, J.; Jiménez-Fonseca, P.; Rivera, F.; Cano, M.T.; Garrote, M.R.; Pericay, C.; Diaz, I.; et al. Sequential nab-paclitaxel/gemcitabine, followed by modified FOLFOX for first line metastatic pancreatic cancer: The SEQUENCE trial. J. Clin. Oncol. 2022, 40, 4022. [Google Scholar] [CrossRef]
- Macarulla, T.; Pazo-Cid, R.; Guillén-Ponce, C.; López, R.; Vera, R.; Reboredo, M.; Muñoz Martin, A.; Rivera, F.; Díaz Beveridge, R.; La Casta, A.; et al. Phase I/II trial to evaluate the efficacy and safety of nanoparticle albumin-bound paclitaxel in combination with gemcitabine in patients with pancreatic cancer and an ECOG performance status of 2. J. Clin. Oncol. 2019, 37, 230–238. [Google Scholar] [CrossRef]
- Stocken, D.D.; Hassan, A.B.; Altman, D.G.; Billingham, L.J.; Bramhall, S.R.; Johnson, P.J.; Freemantle, N. Modeling prognostic factors in advanced pancreatic cancer. Br. J. Cancer 2008, 99, 883–893. [Google Scholar] [CrossRef]
- Duan, K.; Jang, G.-H.; Grant, R.C.; Wilson, J.M.; Notta, F.; O’kane, G.M.; Knox, J.J.; Gallinger, S.; Fischer, S. The value of GATA6 immunohistochemistry and computer-assisted diagnosis to predict clinical outcome in advanced pancreatic cancer. Sci. Rep. 2021, 11, 14951. [Google Scholar] [CrossRef]
- Baraks, G.; Tseng, R.; Pan, C.-H.; Kasliwal, S.; Leiton, C.V.; Shroyer, K.R.; Escobar-Hoyos, L.F. Dissecting the Oncogenic Roles of Keratin 17 in the Hallmarks of Cancer. Cancer Res. 2021, 82, 1159–1166. [Google Scholar] [CrossRef]
| Demographic and Patient Baseline Characteristics | |
|---|---|
| Characteristic | (N = 108) |
| Age—yr | |
| Median | 68 |
| Range | 35–81 |
| Sex—no. (%) | |
| Male | 42 (39) |
| Female | 66 (61) |
| Alive—no. (%) | 5 (5) |
| Dead—no. (%) | 91 (84) |
| Transferred care | 12 (6) |
| * ECOG performance status score—no. (%) | |
| 0 | 58 (54) |
| 1 | 49 (45) |
| 2 | 1 (1) |
| Site of metastatic disease—no. (%) | |
| Liver | 85 (79) |
| Lung | 14 (13) |
| Peritoneum | 48 (44) |
| Bone | 6 (6) |
| Number of metastatic sites | |
| 1 | 67 (62) |
| 2 | 33 (31) |
| ≥3 | 8 (7) |
| Level of carbohydrate 19-9—U/mL 1 | |
| Median (95% CI) | 4598 (1903–9500) |
| Range | 5–132,000 |
| Biliary obstruction—no. (%) | |
| yes | 43 (40) |
| no | 65 (60) |
| Thrombosis—no. (%) | |
| yes | 23 (21) |
| no | 85 (79) |
| Pain at presentation | |
| yes | 78 (72) |
| no | 30 (28) |
| Common Adverse Events of Grade 3 or Higher | |
|---|---|
| Event | (N = 108) |
| Adverse event leading to death—no. (%) | 0 |
| Grade ≥ 3 hematologic adverse event—no. (%) | |
| Neutropenia | 11 (10.2) |
| Thrombocytopenia | 5 (4.6) |
| Anemia | 10 (9.3) |
| Febrile neutropenia—no. (%) | 2 (1.9) |
| Thromboembolism | 8 (7.4) |
| Peripheral neuropathy | 1 (0.9) |
| Nausea or vomiting | 1 (0.9) |
| Diarrhea | 1 (0.9) |
| Mucositis | 0 |
| Infection | 19 (17.6) |
| Overall Survival, Progression-Free Survival, and Response Rates | |
|---|---|
| All (n = 108) | |
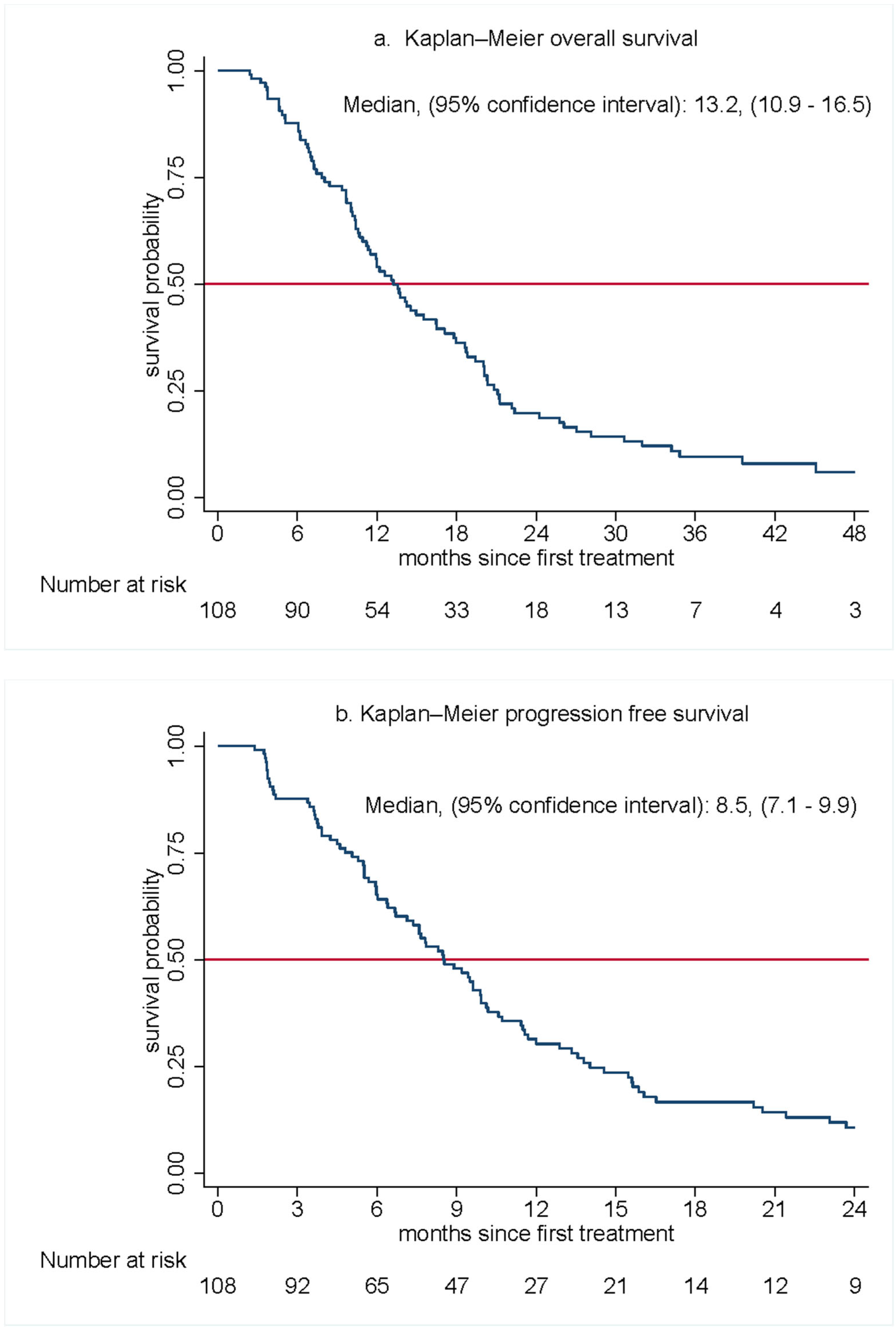
| Overall Survival (months) | |
| Median overall survival—mo (95% CI) | 13.2 (10.9–16.5) |
| 6 mo | 87.7 (79.8–92.7) |
| 12 mo | 54.0 (43.8–63.1) |
| 18 mo | 36.2 (26.8–45.7) |
| 24 mo | 19.8 (12.4–28.3) |
| Progression-Free Survival | |
| Median progression-free survival—mo (95% CI) | 8.5 (7.1–9.9) |
| Progression-Free Survival rate—(95% CI) | |
| 6 mo | 65.2 (55.1–73.6) |
| 12 mo | 30.3 (21.6–39.5) |
| 16-week response * | |
| Partial response | 39 (37.1) |
| Stable disease | 48 (45.7) |
| Progressive disease | 18 (17.1) |
| Disease Control Rate at 16 weeks * | |
| No. (%) | 87 (82.9) |
| 95% CI | 72–87 |
| Treatment Characteristics | |
| Completed 12 cycles of treatment—No. (%) | 42 (38.9) |
| Median OS (95% CI) for completed 12 cycles | 22.2 (20.0–28.1) |
| Did not complete 12 cycles of treatment | 66 (61.1) |
| Median OS (95% CI) for fewer than 12 cycles | 9.7 (7.2–10.4) |
| Median Follow-Up—mo | 20 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schroeder, B.A.; Mandelson, M.T.; Picozzi, V.J. Alternating Gemcitabine/Nab-Paclitaxel (GA) and 5-FU/Leucovorin/Irinotecan (FOLFIRI) as First-Line Treatment for De Novo Metastatic Pancreatic Cancer (MPC): Safety and Effect. Cancers 2023, 15, 5588. https://doi.org/10.3390/cancers15235588
Schroeder BA, Mandelson MT, Picozzi VJ. Alternating Gemcitabine/Nab-Paclitaxel (GA) and 5-FU/Leucovorin/Irinotecan (FOLFIRI) as First-Line Treatment for De Novo Metastatic Pancreatic Cancer (MPC): Safety and Effect. Cancers. 2023; 15(23):5588. https://doi.org/10.3390/cancers15235588
Chicago/Turabian StyleSchroeder, Brett A., Margaret T. Mandelson, and Vincent J. Picozzi. 2023. "Alternating Gemcitabine/Nab-Paclitaxel (GA) and 5-FU/Leucovorin/Irinotecan (FOLFIRI) as First-Line Treatment for De Novo Metastatic Pancreatic Cancer (MPC): Safety and Effect" Cancers 15, no. 23: 5588. https://doi.org/10.3390/cancers15235588





