Timing of Initiation of Palliative Chemotherapy in Asymptomatic Patients with Metastatic Pancreatic Cancer: An International Expert Survey and Case-Vignette Study
Abstract
:Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Survey and Case-Vignettes
2.3. Data Collection
2.4. Statistical Analysis
3. Results
3.1. Characteristics of Respondents
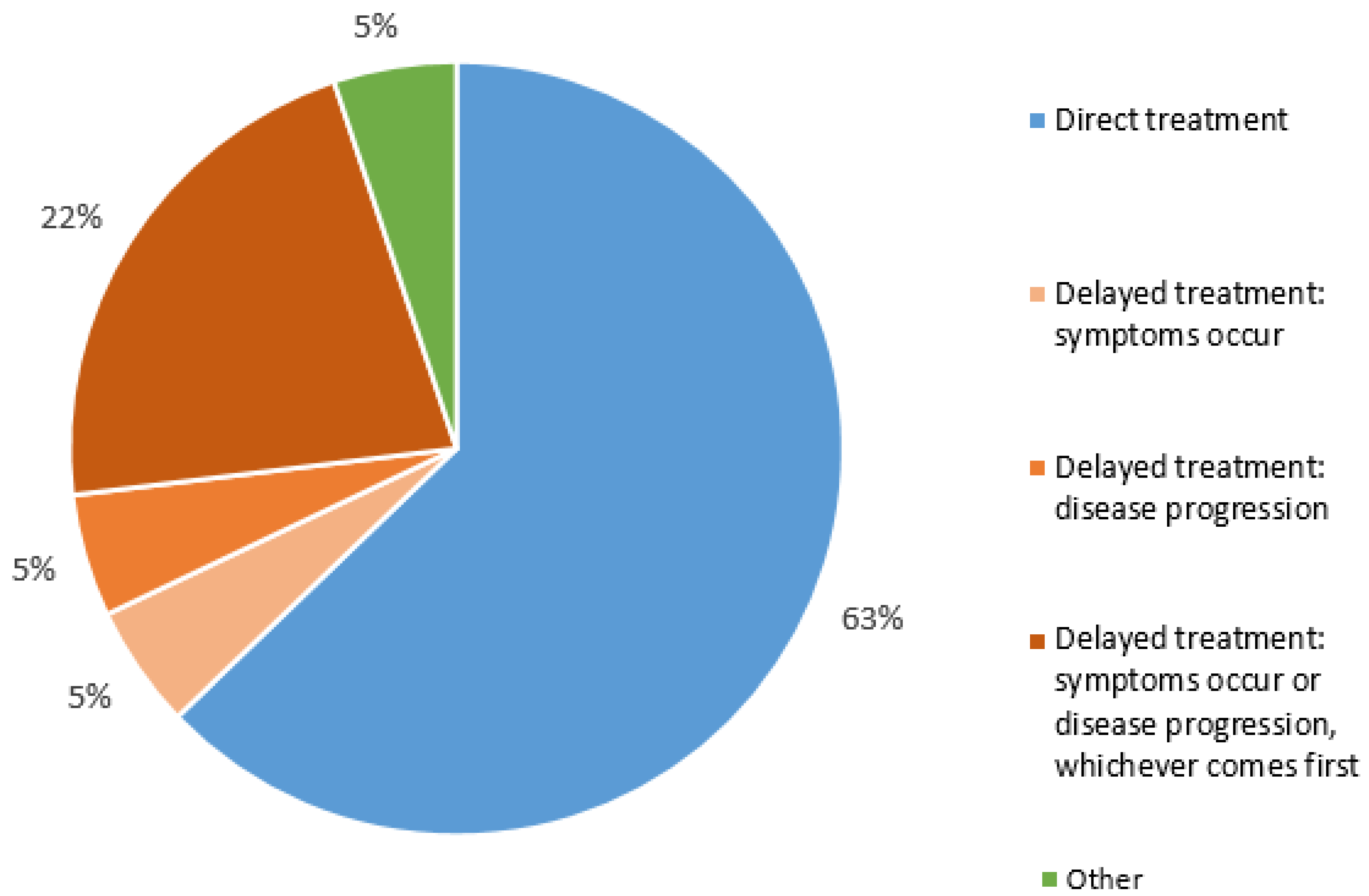
3.2. Perspectives on Timing of Treatment of Asymptomatic Patients with mPDAC
3.3. Case-Vignettes
3.4. Inter-Rater Variability
3.5. Variation in the Timing of Treatment Initiation
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rahib, L.; Smith, B.D.; Aizenberg, R.; Rosenzweig, A.B.; Fleshman, J.M.; Matrisian, L.M. Projecting cancer incidence and deaths to 2030: The unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014, 74, 2913–2921. [Google Scholar] [CrossRef] [PubMed]
- Park, W.; Chawla, A.; O’Reilly, E.M. Pancreatic Cancer: A Review. JAMA 2021, 326, 851–862. [Google Scholar] [CrossRef] [PubMed]
- Conroy, T.; Desseigne, F.; Ychou, M.; Bouché, O.; Guimbaud, R.; Bécouarn, Y.; Adenis, A.; Raoul, J.-L.; Gourgou-Bourgade, S.; de la Fouchardière, C.; et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N. Engl. J. Med. 2011, 364, 1817–1825. [Google Scholar] [CrossRef] [PubMed]
- Von Hoff, D.D.; Ervin, T.; Arena, F.P.; Chiorean, E.G.; Infante, J.; Moore, M.; Seay, T.; Tjulandin, S.A.; Ma, W.W.; Saleh, M.N.; et al. Increased Survival in Pancreatic Cancer with nab-Paclitaxel plus Gemcitabine. N. Engl. J. Med. 2013, 369, 1691–1703. [Google Scholar] [CrossRef]
- Gourgou-Bourgade, S.; Bascoul-Mollevi, C.; Desseigne, F.; Ychou, M.; Bouché, O.; Guimbaud, R.; Bécouarn, Y.; Adenis, A.; Raoul, J.-L.; Boige, V.; et al. Impact of FOLFIRINOX compared with gemcitabine on quality of life in patients with metastatic pancreatic cancer: Results from the PRODIGE 4/ACCORD 11 randomized trial. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2013, 31, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Chiritescu, G.; Dumon, K.; Verslype, C.; Prenen, H.; Houbiers, G.; Peeters, M.; Janssens, J.; Van Daele, D.; Laurent, S.; Arts, J.; et al. Gemcitabine with nab-paclitaxel in patients with locally advanced or metastatic pancreatic ductal adenocarcinoma (PDAC): A quality of life randomized cross-over study (QOLINPAC). Ann. Oncol. 2018, 29 (Suppl. 5), v101. [Google Scholar] [CrossRef]
- Di Gioia, D.; Stieber, P.; Schmidt, G.P.; Nagel, D.; Heinemann, V.; Baur-Melnyk, A. Early detection of metastatic disease in asymptomatic breast cancer patients with whole-body imaging and defined tumor marker increase. Br. J. Cancer 2015, 112, 809–818. [Google Scholar] [CrossRef]
- Chan, H.-P.; Liu, W.-S.; Liou, W.-S.; Hu, C.; Chiu, Y.-L.; Peng, N.-J. Comparison of FDG-PET/CT for Cancer Detection in Populations with Different Risks of Underlying Malignancy. In Vivo 2020, 34, 469–478. [Google Scholar] [CrossRef]
- Tzeng, C.-W.D.; Fleming, J.B.; Lee, J.E.; Wang, X.; Pisters, P.W.T.; Vauthey, J.-N.; Varadhachary, G.; Wolff, R.A.; Katz, M.H.G. Yield of clinical and radiographic surveillance in patients with resected pancreatic adenocarcinoma following multimodal therapy. HPB Off. J. Int. Hepato Pancreato Biliary Assoc. 2012, 14, 365–372. [Google Scholar] [CrossRef]
- Daamen, L.A.; Groot, V.P.; Besselink, M.G.; Bosscha, K.; Busch, O.R.; Cirkel, G.A.; van Dam, R.M.; Festen, S.; Groot Koerkamp, B.; Haj Mohammad, N.; et al. Detection, Treatment, and Survival of Pancreatic Cancer Recurrence in the Netherlands: A Nationwide Analysis. Ann. Surg. 2020, 275, 769–775. [Google Scholar] [CrossRef]
- Tjaden, C.; Michalski, C.W.; Strobel, O.; Giese, N.; Hennche, A.-K.; Büchler, M.W.; Hackert, T. Clinical Impact of Structured Follow-up After Pancreatic Surgery. Pancreas 2016, 45, 895–899. [Google Scholar] [CrossRef] [PubMed]
- Tempero, M.A.; Malafa, M.P.; Al-Hawary, M.; Asbun, H.; Bain, A.; Behrman, S.W.; Benson, A.B.; Binder, E.; Cardin, D.B.; Cha, C.; et al. Pancreatic Adenocarcinoma, Version 2.2017, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2017, 15, 1028–1061. [Google Scholar] [CrossRef] [PubMed]
- Cascinu, S.; Falconi, M.; Valentini, V.; Jelic, S. Pancreatic cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2010, 21 (Suppl. 5), v55–v58. [Google Scholar] [CrossRef] [PubMed]
- Claassen, Y.H.; van der Valk, M.J.; Breugom, A.J.; Frouws, M.A.; Bastiaannet, E.; Liefers, G.-J.; van de Velde, C.J.; Kapiteijn, E. Survival differences with immediate versus delayed chemotherapy for asymptomatic incurable metastatic colorectal cancer. Cochrane Database Syst. Rev. 2018, 11, CD012326. [Google Scholar] [CrossRef] [PubMed]
- Augustinus, S.; Thurairajah, G.; Besselink, M.G.; van Laarhoven, H.W.M.; van Oijen, M.G.H.; Mackay, T.M.; Wilmink, J.W. Delayed Versus Immediate Start of Chemotherapy in Asymptomatic Patients with Advanced Cancer: A Meta-Analysis. Oncologist 2023, 28, 961–968. [Google Scholar] [CrossRef] [PubMed]
- Jooste, V.; Dejardin, O.; Bouvier, V.; Arveux, P.; Maynadie, M.; Launoy, G.; Bouvier, A.-M. Pancreatic cancer: Wait times from presentation to treatment and survival in a population-based study. Int. J. Cancer 2016, 139, 1073–1080. [Google Scholar] [CrossRef] [PubMed]
- Kruger, S.; Schirle, K.; Haas, M.; Crispin, A.; Schirra, J.; Mayerle, J.; D’Haese, J.G.; Kunz, W.G.; Ricke, J.; Ormanns, S.; et al. Prolonged time to treatment initiation in advanced pancreatic cancer patients has no major effect on treatment outcome: A retrospective cohort study controlled for lead time bias and waiting time paradox. J. Cancer Res. Clin. Oncol. 2020, 146, 391–399. [Google Scholar] [CrossRef] [PubMed]
- Pitt, S.C.; Schwartz, T.A.; Chu, D. AAPOR Reporting Guidelines for Survey Studies. JAMA Surg. 2021, 156, 785–786. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- Groot, V.P.; Gemenetzis, G.; Blair, A.B.; Ding, D.; Javed, A.A.; Burkhart, R.A.; Yu, J.; Borel Rinkes, I.H.; Molenaar, I.Q.; Cameron, J.L.; et al. Implications of the Pattern of Disease Recurrence on Survival Following Pancreatectomy for Pancreatic Ductal Adenocarcinoma. Ann. Surg. Oncol. 2018, 25, 2475–2483. [Google Scholar] [CrossRef]
- Lu, F.; Poruk, K.E.; Weiss, M.J. Surgery for oligometastasis of pancreatic cancer. Chin. J. Cancer Res. 2015, 27, 358–367. [Google Scholar] [CrossRef] [PubMed]
- Jung, H.A.; Han, B.R.; Kim, H.Y.; Kim, H.J.; Zang, D.Y.; Jung, J.Y. Treatment and Outcomes of Metastatic Pancreatic Cancer in Elderly Patients. Chemotherapy 2021, 66, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Capanu, M.; Yu, K.H.; Lowery, M.A.; Kelsen, D.P.; O’Reilly, E.M. Treatment, Outcomes, and Clinical Trial Participation in Elderly Patients with Metastatic Pancreas Adenocarcinoma. Clin. Colorectal Cancer 2015, 14, 269–276.e1. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Huang, D.-B.; Zhang, Q.; Guo, C.-X.; Fu, Q.-H.; Zhang, X.-C.; Tang, T.-Y.; Su, W.; Chen, Y.-W.; Chen, W.; et al. The efficacy and toxicity of chemotherapy in the elderly with advanced pancreatic cancer. Pancreatology 2020, 20, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Zijlstra, M.; van der Geest, L.G.M.; van Laarhoven, H.W.M.; Lemmens, V.E.P.P.; van de Poll-Franse, L.V.; Raijmakers, N.J.H. Patient characteristics and treatment considerations in pancreatic cancer: A population based study in the Netherlands. Acta Oncol. 2018, 57, 1185–1191. [Google Scholar] [CrossRef] [PubMed]
- Saade-Lemus, P.; Biller, L.; Bullock, A. Safety and efficacy of combination chemotherapy regimens in older adults with pancreatic ductal adenocarcinoma: A systematic review. J. Gastrointest. Oncol. 2021, 12, 2591–2599. [Google Scholar] [CrossRef] [PubMed]
- Augustinus, S.; Broekman, T.; Creemers, G.-J.; Daamen, L.A.; van Dieren, S.; de Groot, J.-W.B.; Cirkel, G.A.; Homs, M.Y.V.; van Laarhoven, H.W.M.; van Leeuwen, L.; et al. Timing of start of systemic treatment in patients with asymptomatic metastasized pancreatic cancer (TIMEPAN): A protocol of a multicenter prospective patient preference non-randomized trial. Acta Oncol. 2023, 62, 1973–1978. [Google Scholar] [CrossRef]
- de Leede, N.; Bastiaannet, E.; van der Geest, L.; Egan, K.; van de Velde, C.; Balducci, L.; Bonsing, B.; Extermann, M. An international comparison of treatment and short-term overall survival for older patients with pancreatic cancer. J. Geriatr. Oncol. 2019, 10, 584–590. [Google Scholar] [CrossRef]
- Sibeoni, J.; Picard, C.; Orri, M.; Labey, M.; Bousquet, G.; Verneuil, L.; Revah-Levy, A. Patients’ quality of life during active cancer treatment: A qualitative study. BMC Cancer 2018, 18, 951. [Google Scholar] [CrossRef]
| All Respondents (n = 78) | |
|---|---|
| Continent | |
| Asia–Pacific | 12 (15.4%) |
| Europe | 48 (61.5%) |
| USA | 18 (23.1%) |
| Age, mean years (SD) | 51.9 (SD 9.9) |
| Female | 28 (35.9%) |
| Type of hospital | |
| Academic hospital with pancreatic surgery | 53 (67.9%) |
| Academic hospital without pancreatic surgery | 4 (5.1%) |
| Non-academic hospital with pancreatic surgery | 10 (12.8%) |
| Non-academic hospital without pancreatic surgery | 11 (14.1%) |
| Years registered as medical oncologist | |
| 5 years or less | 8 (10.3%) |
| 6–10 years | 11 (14.1%) |
| 11 years or more | 59 (75.6%) |
| Preferred treatment for mPDAC | |
| FOLFIRINOX | 52 (66.7%) |
| Gemcitabine + nab-paclitaxel | 14 (17.9%) |
| Gemcitabine monotherapy | 0 |
| Clinical trials | 12 (15.4%) |
| Number of patients per year with pancreatic cancer | |
| None | 1 (1.3%) |
| Less than 10 patients | 7 (8.9%) |
| 11–20 patients | 15 (19.2%) |
| 21–50 patients | 34 (43.6%) |
| 51–100 patients | 12 (14.3%) |
| >100 patients | 9 (11.5%) |
| Number of patients with asymptomatic pancreatic cancer | |
| None | 6 (7.7%) |
| Less than 10 patients | 43 (55.1%) |
| 11–20 patients | 16 (20.5%) |
| >20 patients | 13 (16.7%) |
| Structured follow-up after resection | |
| Yes | 48 (61.5%) |
| Only within clinical trials | 19 (24.4%) |
| No | 11 (14.1%) |
| Case-Vignettes | Age and Clinical Condition | Disease | Preferred Treatment (n = 78) | Agreement ** | |
|---|---|---|---|---|---|
| Case-vignette 1 | 60 years old No comorbidities | 1 liver metastasis (recurrence) | Immediate | 38 (48.7%) | Slight agreement (K = 0.06) |
| Delayed | 26 (33.3%) | ||||
| Other | 14 (17.9%) | ||||
| Case-vignette 2 | 60 years old No comorbidities | 1 small lung metastasis (recurrence) | Immediate | 23 (29.5%) | Slight agreement (K = 0.11) |
| Delayed | 43 (55.1%) | ||||
| Other | 12 (15.4%) | ||||
| Case-vignette 3 | 60 years old No comorbidities | 6 lung metastases (recurrence) | Immediate | 57 (73.1%) | Fair agreement (K = 0.38) |
| Delayed | 18 (23.1%) | ||||
| Other | 3 (3.8%) | ||||
| Case-vignette 4 | 60 years old No comorbidities | 3 liver + 3 lung metastases (recurrence) | Immediate | 69 (88.5%) | Substantial agreement (K = 0.68) |
| Delayed | 7 (9.0%) | ||||
| Other | 2 (2.6%) | ||||
| Case-vignette 5 | 80 years old No comorbidities | 1 liver metastasis (recurrence) | Immediate | 27 (34.6%) | Slight agreement (K = 0.01) |
| Delayed | 32 (41.0%) | ||||
| Other | 19 (24.4%) | ||||
| Case-vignette 6 | 60 years old Significant comorbidities * | 1 liver metastasis (recurrence) | Immediate | 18 (23.1%) | Slight agreement (K = 0.04) |
| Delayed | 37 (47.4%) | ||||
| Other | 23 (29.5%) | ||||
| Case-vignette 7 | 60 years old No comorbidities | 1 liver metastasis (primary tumor) | Immediate | 56 (71.8%) | Fair agreement (K = 0.33) |
| Delayed | 14 (17.9%) | ||||
| Other | 8 (10.3%) | ||||
| Case-vignette 8 | 60 years old No comorbidities | Progression from 2 to 6 liver metastasis (after 6 weeks delayed) | Immediate | 75 (96.2%) | Perfect agreement (K = 0.85) |
| Delayed | 3 (3.8%) | ||||
| Other | 0 | ||||
| Case-vignette 9 | 60 years old No comorbidities | Progression from 2 liver to 3 liver + 3 lung metastasis (after 6 weeks delayed) | Immediate | 73 (93.6%) | Perfect agreement (K = 0.82) |
| Delayed | 3 (3.8%) | ||||
| Other | 2 (2.6%) | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Augustinus, S.; van Laarhoven, H.W.M.; Cirkel, G.A.; de Groot, J.W.B.; Groot Koerkamp, B.; Macarulla, T.; Melisi, D.; O'Reilly, E.M.; van Santvoort, H.C.; Mackay, T.M.; et al. Timing of Initiation of Palliative Chemotherapy in Asymptomatic Patients with Metastatic Pancreatic Cancer: An International Expert Survey and Case-Vignette Study. Cancers 2023, 15, 5603. https://doi.org/10.3390/cancers15235603
Augustinus S, van Laarhoven HWM, Cirkel GA, de Groot JWB, Groot Koerkamp B, Macarulla T, Melisi D, O'Reilly EM, van Santvoort HC, Mackay TM, et al. Timing of Initiation of Palliative Chemotherapy in Asymptomatic Patients with Metastatic Pancreatic Cancer: An International Expert Survey and Case-Vignette Study. Cancers. 2023; 15(23):5603. https://doi.org/10.3390/cancers15235603
Chicago/Turabian StyleAugustinus, Simone, Hanneke W. M. van Laarhoven, Geert A. Cirkel, Jan Willem B. de Groot, Bas Groot Koerkamp, Teresa Macarulla, Davide Melisi, Eileen M. O'Reilly, Hjalmar C. van Santvoort, Tara M. Mackay, and et al. 2023. "Timing of Initiation of Palliative Chemotherapy in Asymptomatic Patients with Metastatic Pancreatic Cancer: An International Expert Survey and Case-Vignette Study" Cancers 15, no. 23: 5603. https://doi.org/10.3390/cancers15235603
APA StyleAugustinus, S., van Laarhoven, H. W. M., Cirkel, G. A., de Groot, J. W. B., Groot Koerkamp, B., Macarulla, T., Melisi, D., O'Reilly, E. M., van Santvoort, H. C., Mackay, T. M., Besselink, M. G., & Wilmink, J. W., on behalf of the Dutch Pancreatic Cancer Group. (2023). Timing of Initiation of Palliative Chemotherapy in Asymptomatic Patients with Metastatic Pancreatic Cancer: An International Expert Survey and Case-Vignette Study. Cancers, 15(23), 5603. https://doi.org/10.3390/cancers15235603








