The Evolution of Ki-67 and Breast Carcinoma: Past Observations, Present Directions, and Future Considerations
Abstract
:Simple Summary
Abstract
1. Introduction
2. Ki-67—Past Observations
2.1. The Discovery of Ki-67
2.2. The Development of Ki-67 Immunohistochemistry for Clinical Practice
3. Ki-67—Present Directions
3.1. The Prognostic Value of Ki-67 in Breast Cancer
3.2. Ki-67 in Breast Cancer Molecular Subtypes
3.3. Ki-67 as a Prognostic and Predictive Marker in the Adjuvant Setting
3.4. Ki-67 as a Prognostic and Predictive Marker in the Neoadjuvant Setting
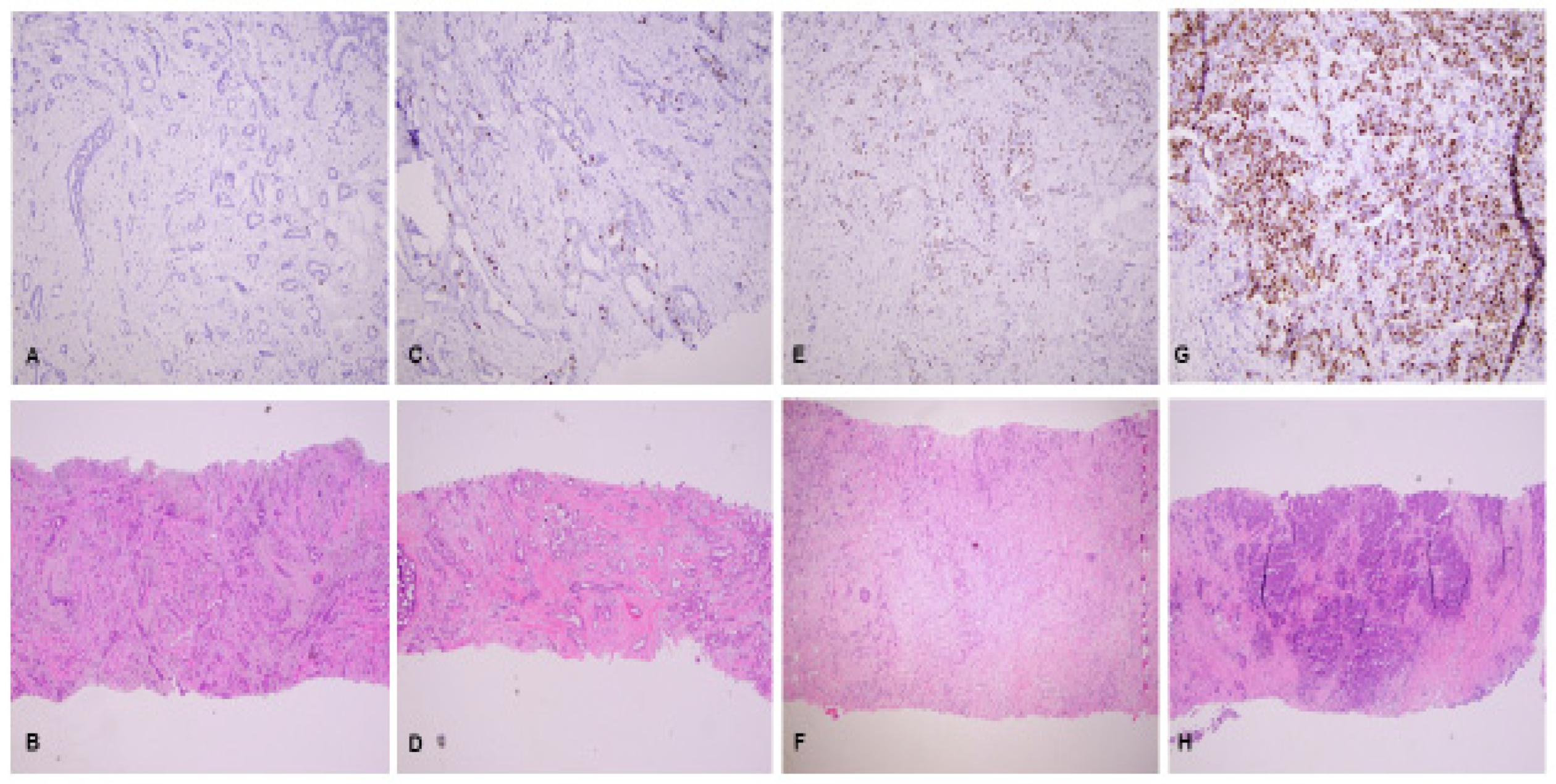
3.5. Recommendations of the International Ki-67 in Breast Cancer Working Group (IKWG)
4. Ki-67—Future Considerations
4.1. Potentially Cost-Effective Alternative to Genomic Profiling Assays
4.2. Potentially Routine Companion Diagnostic Test in Breast Cancer
4.3. Simplified Scoring Algorithms
4.4. Automated Digital Image Analysis
4.5. Potential Alternative/Complementary Assays to Ki-67 Immunohistochemistry
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Penault-Llorca, F.; Radosevic-Robin, N. Ki67 assessment in breast cancer: An update. Pathology 2017, 49, 166–171. [Google Scholar] [CrossRef] [PubMed]
- O Nielsen, T.; Leung, S.C.Y.; Rimm, D.L.; Dodson, A.; Acs, B.; Badve, S.; Denkert, C.; Ellis, M.J.; Fineberg, S.; Flowers, M.; et al. Assessment of Ki67 in Breast Cancer: Updated Recommendations from the International Ki67 in Breast Cancer Working Group. Gynecol. Oncol. 2020, 113, 808–819. [Google Scholar] [CrossRef]
- Tubiana, M.; Pejovic, M.H.; Chavaudra, N.; Contesso, G.; Malaise, E.P. The long-term prognostic significance of the thymidine labelling index in breast cancer. Int. J. Cancer 1984, 33, 441–445. [Google Scholar] [CrossRef] [PubMed]
- Dressler, L.G.; Seamer, L.; A Owens, M.; Clark, G.M.; McGuire, W.L. Evaluation of a modeling system for S-phase estimation in breast cancer by flow cytometry. Cancer Res. 1987, 47, 5294–5302. [Google Scholar] [PubMed]
- Gerdes, J.; Lelle, R.J.; Pickartz, H.; Heidenreich, W.; Schwarting, R.; Kurtsiefer, L.; Stauch, G.; Stein, H. Growth fractions in breast cancers determined in situ with monoclonal antibody Ki-67. J. Clin. Pathol. 1986, 39, 977–980. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paik, S.; Shak, S.; Tang, G.; Kim, C.; Baker, J.; Cronin, M.; Baehner, F.L.; Walker, M.G.; Watson, D.; Park, T.; et al. A Multigene Assay to Predict Recurrence of Tamoxifen-Treated, Node-Negative Breast Cancer. N. Engl. J. Med. 2004, 351, 2817–2826. [Google Scholar] [CrossRef] [Green Version]
- Zerdan, M.B.; Ibrahim, M.; El Nakib, C.; Hajjar, R.; Assi, H.I. Genomic Assays in Node Positive Breast Cancer Patients: A Review. Front. Oncol. 2021, 10, 609100. [Google Scholar] [CrossRef] [PubMed]
- Tian, S.; Roepman, P.; Veer, L.J.V.; Bernards, R.; De Snoo, F.; Glas, A.M. Biological Functions of the Genes in the Mammaprint Breast Cancer Profile Reflect the Hallmarks of Cancer. Biomark. Insights 2010, 5, 129–138. [Google Scholar] [CrossRef] [Green Version]
- Gerdes, J.; Lemke, H.; Baisch, H.; Wacker, H.H.; Schwab, U.; Stein, H. Cell cycle analysis of a cell proliferation-associated human nuclear antigen defined by the monoclonal antibody Ki-67. J. Immunol. 1984, 133, 1710–1715. [Google Scholar] [CrossRef] [PubMed]
- Bullwinkel, J.; Baron-Lühr, B.; Lüdemann, A.; Wohlenberg, C.; Gerdes, J.; Scholzen, T. Ki-67 protein is associated with ribosomal RNA transcription in quiescent and proliferating cells. J. Cell Physiol. 2005, 206, 624–635. [Google Scholar] [CrossRef]
- Yerushalmi, R.; Woods, R.; Ravdin, P.M.; Hayes, M.M.; Gelmon, K.A. Ki67 in breast cancer: Prognostic and predictive potential. Lancet Oncol. 2010, 11, 174–183. [Google Scholar] [CrossRef] [PubMed]
- Urruticoechea, A.; Smith, I.E.; Dowsett, M. Proliferation Marker Ki-67 in Early Breast Cancer. J. Clin. Oncol. 2005, 23, 7212–7220. [Google Scholar] [CrossRef]
- Dowsett, M.; Nielsen, T.O.; A’hern, R.; Bartlett, J.; Coombes, R.C.; Cuzick, J.; Ellis, M.; Henry, N.L.; Hugh, J.C.; Lively, T.; et al. Assessment of Ki67 in breast cancer: Recommendations from the International Ki67 in breast cancer working group. JNCI J. Natl. Cancer Inst. 2011, 103, 1656–1664. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Turner, B.M.; Katerji, H.; Zhang, H.; Hicks, D.G. Biomarker and multigene assay testing in ER positive, HER-2 negative breast carcinomas: An international guidelines-based approach. Hum. Pathol. Rep. 2021, 26, 300574. [Google Scholar] [CrossRef]
- Biganzoli, L.; Calabrese, M.; Conte, B.; Cortesi, L.; Criscitiello, C.; Del Mastro, L.; Fiorentino, A.; Levaggi, A.; Montemurro, F.; Marchio, C.; et al. Breast Neoplasms: Guidelines. Associazione Italiana di Oncologia Medica/Italian Association of Medical Oncology. 2018. Available online: https://www.aiom.it/wp-content/uploads/2018/11/2018_LG_AIOM_Breast_ENversion.pdf (accessed on 23 January 2023).
- Duffy, M.; Harbeck, N.; Nap, M.; Molina, R.; Nicolini, A.; Senkus, E.; Cardoso, F. Clinical use of biomarkers in breast cancer: Updated guidelines from the European Group on Tumor Markers (EGTM). Eur. J. Cancer 2017, 75, 284–298. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- European Society for Medical Oncology (ESMO). Available online: https://www.esmo.org/ (accessed on 23 January 2023).
- Early and Locally Advanced Breast Cancer: Diagnosis and Management; National Institute for Health and Care Excellence (NICE): London, UK, 2018.
- ASCO Hub—American Society of Clinical Oncology. Available online: https://beta.asco.org/ (accessed on 23 January 2023).
- Andre, F.; Ismaila, N.; Henry, N.L.; Somerfield, M.R.; Bast, R.C.; Barlow, W.; Collyar, D.E.; Hammond, M.E.; Kuderer, N.M.; Liu, M.C.; et al. Use of Biomarkers to Guide Decisions on Adjuvant Systemic Therapy for Women with Early-Stage Invasive Breast Cancer: ASCO Clinical Practice Guideline Update—Integration of Results From TAILORx. J. Clin. Oncol. 2019, 37, 1956–1964. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harris, L.N.; Ismaila, N.; McShane, L.M.; Andre, F.; Collyar, D.E.; Gonzalez-Angulo, A.M.; Hammond, E.H.; Kuderer, N.M.; Liu, M.C.; Mennel, R.G.; et al. Use of Biomarkers to Guide Decisions on Adjuvant Systemic Therapy for Women With Early-Stage Invasive Breast Cancer: American Society of Clinical Oncology Clinical Practice Guideline. J. Clin. Oncol. 2016, 34, 1134–1150. [Google Scholar] [CrossRef] [Green Version]
- Krop, I.; Ismaila, N.; Andre, F.; Bast, R.; Barlow, W.; Collyar, D.E.; Hammond, M.E.; Kuderer, N.M.; Liu, M.C.; Mennel, R.G.; et al. Use of Biomarkers to Guide Decisions on Adjuvant Systemic Therapy for Women with Early-Stage Invasive Breast Cancer: American Society of Clinical Oncology Clinical Practice Guideline Focused Update. J. Clin. Oncol. 2017, 35, 2838–2847. [Google Scholar] [CrossRef]
- Gradishar, W.J.; Moran, M.S.; Abraham, J.; Aft, R.; Agnese, D.; Allison, K.H.; Anderson, B.; Burstein, H.J.; Chew, H.; Dang, C.; et al. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines): Breast Cancer. Version 4.2022. National Comprehensive Cancer Network (NCCN), 2022/6/21 2022. Available online: https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf (accessed on 23 January 2023).
- Cardoso, F.; Kyriakides, S.; Ohno, S.; Penault-Llorca, F.; Poortmans, P.; Rubio, I.T.; Zackrisson, S.; Senkus, E. ESMO Guidelines Committee. Early breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2019, 30, 1194–1220, Erratum in 2019, 20, 1674; 2021, 32, 284. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hortobagyi, G.N.; Connolly, J.L.; D’Orsi, C.J.; Edge, S.B.; Mittendorf, E.A.; Rugo, H.S.; Solin, L.J.; Weaver, D.L.; Winchester, D.J.; Giuliano, A. Breast. In AJCC Cancer Staging Manual, 8th ed.; Amin, M.B., Edge, S.B., Greene, F.L., Byrd, D.R., Brookland, R.K., Washington, M.K., Gershenwald, J.E., Compton, C.C., Hess, K.R., Sullivan, D.C., et al., Eds.; American College of Surgeons: Chicago, IL, USA, 2018; pp. 589–636. [Google Scholar]
- Johnston, S.R.D.; Harbeck, N.; Hegg, R.; Toi, M.; Martin, M.; Shao, Z.M.; Zhang, Q.Y.; Rodriguez, J.L.M.; Campone, M.; Hamilton, E.; et al. Abemaciclib Combined with Endocrine Therapy for the Adjuvant Treatment of HR+, HER2−, Node-Positive, High-Risk, Early Breast Cancer (monarchE). J. Clin. Oncol. 2020, 38, 3987–3998. [Google Scholar] [CrossRef]
- Gerdes, J.; Schwab, U.; Lemke, H.; Stein, H. Production of a mouse monoclonal antibody reactive with a human nuclear antigen associated with cell proliferation. Int. J. Cancer 1983, 31, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Scholzen, T.; Gerlach, C.; Cattoretti, G. An insider’s view on how Ki-67, the bright beacon of cell proliferation, became very popular. A tribute to Johannes Gerdes (1950–2016). Histopathology 2018, 73, 191–196. [Google Scholar] [CrossRef] [PubMed]
- Duchrow, M.; Schlüter, C.; Wohlenberg, C.; Flad, H.D.; Gerdes, J. Molecular characterization of the gene locus of the human cell proliferation-associated nuclear protein defined by monoclonal antibody Ki-67. Cell Prolif. 1996, 29, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Endl, E.; Gerdes, J. The Ki-67 Protein: Fascinating Forms and an Unknown Function. Exp. Cell Res. 2000, 257, 231–237. [Google Scholar] [CrossRef] [PubMed]
- Cuylen-Haering, S.; Petrovic, M.; Hernandez-Armendariz, A.; Schneider, M.W.G.; Samwer, M.; Blaukopf, C.; Holt, L.J.; Gerlich, D.W. Chromosome clustering by Ki-67 excludes cytoplasm during nuclear assembly. Nature 2020, 587, 285–290. [Google Scholar] [CrossRef] [PubMed]
- Cuylen, S.; Blaukopf, C.; Politi, A.Z.; Müller-Reichert, T.; Neumann, B.; Poser, I.; Ellenberg, J.; Hyman, A.A.; Gerlich, D.W. Ki-67 acts as a biological surfactant to disperse mitotic chromosomes. Nat. Cell Biol. 2016, 535, 308–312. [Google Scholar] [CrossRef] [Green Version]
- Kreitz, S.; Fackelmayer, F.O.; Gerdes, J.; Knippers, R. The Proliferation-Specific Human Ki-67 Protein Is a Constituent of Compact Chromatin. Exp. Cell Res. 2000, 261, 284–292. [Google Scholar] [CrossRef]
- Schlüter, C.; Duchrow, M.; Wohlenberg, C.; Becker, M.H.; Key, G.; Flad, H.D.; Gerdes, J. The cell proliferation-associated antigen of antibody Ki-67: A very large, ubiquitous nuclear protein with numerous repeated elements, representing a new kind of cell cycle-maintaining proteins. J. Cell Biol. 1993, 123, 513–522. [Google Scholar] [CrossRef]
- Hofmann, K.; Bucher, P. The FHA domain: A putative nuclear signalling domain found in protein kinases and transcription factors. Trends Biochem. Sci. 1995, 20, 347–349. [Google Scholar] [CrossRef]
- Duchrow, M.; Schlüter, C.; Key, G.; Kubbutat, M.H.; Wohlenberg, C.; Flad, H.D.; Gerdes, J. Cell proliferation-associated nuclear antigen defined by antibody Ki-67: A new kind of cell cycle-maintaining proteins. Arch. Immunol. Ther. Exp. 1995, 43, 117–121. [Google Scholar]
- Hall, P.A.; Levison, D.A.; Woods, A.L.; Yu, C.C.-W.; Kellock, D.B.; Watkins, J.A.; Barnes, D.M.; Gillett, C.E.; Camplejohn, R.; Dover, R.; et al. Proliferating cell nuclear antigen (PCNA) immunolocalization in paraffin sections: An index of cell proliferation with evidence of deregulated expression in some, neoplasms. J. Pathol. 1990, 162, 285–294. [Google Scholar] [CrossRef] [PubMed]
- Cattoretti, G.; Becker, M.H.G.; Key, G.; Duchrow, M.; Schlüuter, C.; Galle, J.; Gerdes, J. Monoclonal antibodies against recombinant parts of the Ki-67 antigen (MIB 1 and MIB 3) detect proliferating cells in microwave-processed formalin-fixed paraffin sections. J. Pathol. 1992, 168, 357–363. [Google Scholar] [CrossRef] [PubMed]
- Shi, S.R.; E Key, M.; Kalra, K.L. Antigen retrieval in formalin-fixed, paraffin-embedded tissues: An enhancement method for immunohistochemical staining based on microwave oven heating of tissue sections. J. Histochem. Cytochem. 1991, 39, 741–748. [Google Scholar] [CrossRef] [Green Version]
- Kreipe, H.; Harbeck, N.; Christgen, M. Clinical validity and clinical utility of Ki67 in early breast cancer. Ther. Adv. Med. Oncol. 2022, 14, 17588359221122725. [Google Scholar] [CrossRef]
- Wirapati, P.; Sotiriou, C.; Kunkel, S.; Farmer, P.; Pradervand, S.; Haibe-Kains, B.; Desmedt, C.; Ignatiadis, M.; Sengstag, T.; Schütz, F.; et al. Meta-analysis of gene expression profiles in breast cancer: Toward a unified understanding of breast cancer subtyping and prognosis signatures. Breast Cancer Res. 2008, 10, R65. [Google Scholar] [CrossRef] [PubMed]
- Pathmanathan, N.; Balleine, R.L. Ki67 and proliferation in breast cancer. J. Clin. Pathol. 2013, 66, 512–516. [Google Scholar] [CrossRef]
- Petrelli, F.; Viale, G.; Cabiddu, M.; Barni, S. Prognostic value of different cut-off levels of Ki-67 in breast cancer: A systematic review and meta-analysis of 64,196 patients. Breast Cancer Res. Treat. 2015, 153, 477–491. [Google Scholar] [CrossRef]
- Mirza, A.N.; Mirza, N.Q.; Vlastos, G.; Singletary, S.E. Prognostic Factors in Node-Negative Breast Cancer. Ann. Surg. 2002, 235, 10–26. [Google Scholar] [CrossRef]
- de Azambuja, E.; Cardoso, F.; De Castro, G.; Colozza, M.; Mano, M.S.; Durbecq, V.; Sotiriou, C.; Larsimont, D.; Piccart-Gebhart, M.; Paesmans, M. Ki-67 as prognostic marker in early breast cancer: A meta-analysis of published studies involving 12 155 patients. Br. J. Cancer 2007, 96, 1504–1513. [Google Scholar] [CrossRef] [Green Version]
- Viale, G.; Giobbie-Hurder, A.; Regan, M.M.; Coates, A.S.; Mastropasqua, M.G.; Dell’Orto, P.; Maiorano, E.; MacGrogan, G.; Braye, S.G.; Öhlschlegel, C.; et al. Prognostic and Predictive Value of Centrally Reviewed Ki-67 Labeling Index in Postmenopausal Women With Endocrine-Responsive Breast Cancer: Results From Breast International Group Trial 1-98 Comparing Adjuvant Tamoxifen With Letrozole. J. Clin. Oncol. 2008, 26, 5569–5575. [Google Scholar] [CrossRef]
- Kontzoglou, K.; Palla, V.; Karaolanis, G.; Karaiskos, I.; Alexiou, I.; Pateras, I.; Konstantoudakis, K.; Stamatakos, M. Correlation between Ki67 and Breast Cancer Prognosis. Oncology 2013, 84, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Pathmanathan, N.; Balleine, R.L.; Jayasinghe, U.W.; Bilinski, K.L.; Provan, P.J.; Byth, K.; Bilous, A.M.; Salisbury, E.L.; Boyages, J. The prognostic value of Ki67 in systemically untreated patients with node-negative breast cancer. J. Clin. Pathol. 2014, 67, 222–228. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, F.-Y.; Wu, S.-G.; Zhou, J.; Sun, J.-Y.; Lin, Q.; Lin, H.-X.; Guan, X.-X.; He, Z.-Y. Prognostic Value of Ki-67 in Breast Cancer Patients with Positive Axillary Lymph Nodes: A Retrospective Cohort Study. PLoS ONE 2014, 9, e87264. [Google Scholar] [CrossRef] [PubMed]
- Stuart-Harris, R.; Caldas, C.; Pinder, S.; Pharoah, P. Proliferation markers and survival in early breast cancer: A systematic review and meta-analysis of 85 studies in 32,825 patients. Breast 2008, 17, 323–334. [Google Scholar] [CrossRef]
- Inwald, E.C.; Klinkhammer-Schalke, M.; Hofstädter, F.; Zeman, F.; Koller, M.; Gerstenhauer, M.; Ortmann, O. Ki-67 is a prognostic parameter in breast cancer patients: Results of a large population-based cohort of a cancer registry. Breast Cancer Res. Treat. 2013, 139, 539–552. [Google Scholar] [CrossRef] [Green Version]
- The Cancer Genome Atlas (TCGA) Research Network. Comprehensive molecular portraits of human breast tumours. Nature 2012, 490, 61–70. [Google Scholar] [CrossRef] [Green Version]
- Fan, C.; Oh, D.S.; Wessels, L.; Weigelt, B.; Nuyten, D.S.; Nobel, A.B.; Van’T Veer, L.J.; Perou, C.M. Concordance among Gene-Expression–Based Predictors for Breast Cancer. N. Engl. J. Med. 2006, 355, 560–569. [Google Scholar] [CrossRef] [Green Version]
- Cheang, M.C.U.; Chia, S.K.; Voduc, D.; Gao, D.; Leung, S.; Snider, J.; Watson, M.; Davies, S.; Bernard, P.S.; Parker, J.S.; et al. Ki67 Index, HER2 Status, and Prognosis of Patients with Luminal B Breast Cancer. Gynecol. Oncol. 2009, 101, 736–750. [Google Scholar] [CrossRef] [Green Version]
- Goldhirsch, A.; Wood, W.C.; Coates, A.S.; Gelber, R.D.; Thürlimann, B.; Senn, H.-J.; Panel members. Strategies for subtypes—Dealing with the diversity of breast cancer: Highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann. Oncol. 2011, 22, 1736–1747. [Google Scholar] [CrossRef]
- Goldhirsch, A.; Winer, E.P.; Coates, A.S.; Gelber, R.D.; Piccart-Gebhart, M.; Thürlimann, B.; Senn, H.-J. Personalizing the treatment of women with early breast cancer: Highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2013. Ann. Oncol. 2013, 24, 2206–2223. [Google Scholar] [CrossRef] [PubMed]
- Coates, A.S.; Winer, E.P.; Goldhirsch, A.; Gelber, R.D.; Gnant, M.; Piccart-Gebhart, M.; Thürlimann, B.; Senn, H.-J. Panel Members. Tailoring therapies—Improving the management of early breast cancer: St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2015. Ann. Oncol. 2015, 26, 1533–1546. [Google Scholar] [CrossRef] [PubMed]
- Nishimukai, A.; Yagi, T.; Yanai, A.; Miyagawa, Y.; Enomoto, Y.; Murase, K.; Imamura, M.; Takatsuka, Y.; Sakita, I.; Hatada, T.; et al. High Ki-67 Expression and Low Progesterone Receptor Expression Could Independently Lead to a Worse Prognosis for Postmenopausal Patients with Estrogen Receptor-Positive and HER2-Negative Breast Cancer. Clin. Breast Cancer 2014, 15, 204–211. [Google Scholar] [CrossRef]
- Pata, G.; Guaineri, A.; Bianchi, A.; Amoroso, V.; Pasinetti, N.; Pasini, M. Long-Term Outcomes of Immunohistochemically Defined Subtypes of Breast Cancer Less Than or Equal to 2 cm After Breast-Conserving Surgery. J. Surg. Res. 2019, 236, 288–299. [Google Scholar] [CrossRef] [PubMed]
- Sali, A.P.; Sharma, N.; Verma, A.; Beke, A.; Shet, T.; Patil, A.; Pai, T.; Nair, N.; Parmar, V.; Gupta, S.; et al. Identification of Luminal Subtypes of Breast Carcinoma Using Surrogate Immunohistochemical Markers and Ascertaining Their Prognostic Relevance. Clin. Breast Cancer 2020, 20, 382–389. [Google Scholar] [CrossRef]
- Ono, M.; Tsuda, H.; Yunokawa, M.; Yonemori, K.; Shimizu, C.; Tamura, K.; Kinoshita, T.; Fujiwara, Y. Prognostic impact of Ki-67 labeling indices with 3 different cutoff values, histological grade, and nuclear grade in hormone-receptor-positive, HER2-negative, node-negative invasive breast cancers. Breast Cancer 2013, 22, 141–152. [Google Scholar] [CrossRef]
- Perez-Lopez, M.-E.; Garcia-Gomez, J.; Alves, M.T.; Paradela, A.; García-Mata, J.; García-Caballero, T. Ki-67 is a prognostic marker for hormone receptor positive tumors. Clin. Transl. Oncol. 2016, 18, 996–1002. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Criscitiello, C.; Disalvatore, D.; De Laurentiis, M.; Gelao, L.; Fumagalli, L.; Locatelli, M.; Bagnardi, V.; Rotmensz, N.; Esposito, A.; Minchella, I.; et al. High Ki-67 score is indicative of a greater benefit from adjuvant chemotherapy when added to endocrine therapy in Luminal B HER2 negative and node-positive breast cancer. Breast 2013, 23, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Aman, N.A.; Doukoure, B.; Koffi, K.D.; Koui, B.S.; Traore, Z.C.; Kouyate, M.; Toure, I.; Effi, A.B. Immunohistochemical Evaluation of Ki-67 and Comparison with Clinicopathologic Factors in Breast Carcinomas. Asian Pac. J. Cancer Prev. 2019, 20, 73–79. [Google Scholar] [CrossRef] [Green Version]
- Nahed, A.S.; Shaimaa, M.Y. Ki-67 as a prognostic marker according to breast cancer molecular subtype. Cancer Biol. Med. 2016, 13, 496–504. [Google Scholar] [CrossRef] [Green Version]
- Hashmi, A.A.; Hashmi, K.A.; Irfan, M.; Khan, S.M.; Edhi, M.M.; Ali, J.P.; Hashmi, S.K.; Asif, H.; Faridi, N.; Khan, A. Ki67 index in intrinsic breast cancer subtypes and its association with prognostic parameters. BMC Res. Notes 2019, 12, 605. [Google Scholar] [CrossRef]
- Gadzicki, D.; Schubert, A.; Fischer, C.; Milde, S.; Lehmann, U.; Steinemann, D.; Lück, H.-J.; Kreipe, H.; Schlegelberger, B. Histopathological criteria and selection algorithms for BRCA1 genetic testing. Cancer Genet. Cytogenet. 2009, 189, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Denkert, C.; Loibl, S.; Müller, B.; Eidtmann, H.; Schmitt, W.; Eiermann, W.; Gerber, B.; Tesch, H.; Hilfrich, J.; Huober, J.; et al. Ki67 levels as predictive and prognostic parameters in pretherapeutic breast cancer core biopsies: A translational investigation in the neoadjuvant GeparTrio trial. Ann. Oncol. 2013, 24, 2786–2793. [Google Scholar] [CrossRef]
- Zhang, H.; Katerji, H.; Turner, B.M.; Audeh, W.; Hicks, D.G. HER2-low breast cancers: Incidence, HER2 staining patterns, clinicopathologic features, MammaPrint and BluePrint genomic profiles. Mod. Pathol. 2022, 35, 1075–1082. [Google Scholar] [CrossRef]
- Liang, Q.; Ma, D.; Gao, R.-F.; Yu, K.-D. Effect of Ki-67 Expression Levels and Histological Grade on Breast Cancer Early Relapse in Patients with Different Immunohistochemical-based Subtypes. Sci. Rep. 2020, 10, 7648. [Google Scholar] [CrossRef] [PubMed]
- Tashima, R.; Nishimura, R.; Osako, T.; Nishiyama, Y.; Okumura, Y.; Nakano, M.; Fujisue, M.; Toyozumi, Y.; Arima, N. Evaluation of an Optimal Cut-Off Point for the Ki-67 Index as a Prognostic Factor in Primary Breast Cancer: A Retrospective Study. PLoS ONE 2015, 10, e0119565. [Google Scholar] [CrossRef]
- Davey, M.G.; Hynes, S.O.; Kerin, M.J.; Miller, N.; Lowery, A.J. Ki-67 as a Prognostic Biomarker in Invasive Breast Cancer. Cancers 2021, 13, 4455. [Google Scholar] [CrossRef] [PubMed]
- Zhu, X.; Chen, L.; Huang, B.; Wang, Y.; Ji, L.; Wu, J.; Di, G.; Liu, G.; Yu, K.; Shao, Z.; et al. The prognostic and predictive potential of Ki-67 in triple-negative breast cancer. Sci. Rep. 2020, 10, 225. [Google Scholar] [CrossRef] [Green Version]
- Wu, Q.; Ma, G.; Deng, Y.; Luo, W.; Zhao, Y.; Li, W.; Zhou, Q. Prognostic Value of Ki-67 in Patients with Resected Triple-Negative Breast Cancer: A Meta-Analysis. Front. Oncol. 2019, 9, 1068. [Google Scholar] [CrossRef] [Green Version]
- Aleskandarany, M.; Green, A.R.; A Benhasouna, A.; Barros, F.F.; Neal, K.; Reis-Filho, J.S.; O Ellis, I.; A Rakha, E. Prognostic value of proliferation assay in the luminal, HER2-positive, and triple-negative biologic classes of breast cancer. Breast Cancer Res. 2012, 14, R3. [Google Scholar] [CrossRef] [Green Version]
- Ghebeh, H.; Tulbah, A.; Mohammed, S.; Elkum, N.; Bin Amer, S.M.; Al-Tweigeri, T.; Dermime, S. Expression of B7-H1 in breast cancer patients is strongly associated with high proliferative Ki-67-expressing tumor cells. Int. J. Cancer 2007, 121, 751–758. [Google Scholar] [CrossRef]
- Davey, M.G.; Ryan, J.; Lowery, A.J.; Miller, N.; Kerin, M.J. Clinicopathological and prognostic significance of programmed cell death ligand 1 expression in patients diagnosed with breast cancer: Meta-analysis. Br. J. Surg. 2021, 108, 622–631. [Google Scholar] [CrossRef] [PubMed]
- Muenst, S.; Schaerli, A.R.; Gao, F.; Däster, S.; Trella, E.; Droeser, R.A.; Muraro, M.G.; Zajac, P.; Zanetti, R.; Gillanders, W.E.; et al. Expression of programmed death ligand 1 (PD-L1) is associated with poor prognosis in human breast cancer. Breast Cancer Res. Treat. 2014, 146, 15–24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bae, S.B.; Cho, H.D.; Oh, M.-H.; Lee, J.-H.; Jang, S.-H.; Hong, S.A.; Cho, J.; Kim, S.Y.; Han, S.W.; Lee, J.E.; et al. Expression of Programmed Death Receptor Ligand 1 with High Tumor-Infiltrating Lymphocytes Is Associated with Better Prognosis in Breast Cancer. J. Breast Cancer 2016, 19, 242–251. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Viale, G.; Regan, M.M.; Mastropasqua, M.G.; Maffini, F.; Maiorano, E.; Colleoni, M.; Price, K.N.; Golouh, R.; Perin, T.; Brown, R.W.; et al. Predictive Value of Tumor Ki-67 Expression in Two Randomized Trials of Adjuvant Chemoendocrine Therapy for Node-Negative Breast Cancer. Gynecol. Oncol. 2008, 100, 207–212. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, Y.; Yin, W.; Yan, T.; Du, Y.; Shao, Z.; Lu, J. The clinical significance of Ki-67 as a marker of prognostic value and chemosensitivity prediction in hormone-receptor-positive breast cancer: A meta-analysis of the published literature. Curr. Med. Res. Opin. 2013, 29, 1453–1461. [Google Scholar] [CrossRef]
- Jung, S.-Y.; Han, W.; Lee, J.W.; Ko, E.; Kim, E.; Yu, J.-H.; Moon, H.-G.; Park, I.A.; Oh, D.-Y.; Im, S.-A.; et al. Ki-67 Expression Gives Additional Prognostic Information on St. Gallen 2007 and Adjuvant! Online Risk Categories in Early Breast Cancer. Ann. Surg. Oncol. 2009, 16, 1112–1121. [Google Scholar] [CrossRef] [Green Version]
- Varga, Z.; Li, Q.; Jochum, W.; Perriard, U.; Rau, T.; Tille, J.-C.; Hawle, H.; Klingbiel, D.; Thuerlimann, B.; Ruhstaller, T. Ki-67 assessment in early breast cancer: SAKK28/12 validation study on the IBCSG VIII and IBCSG IX cohort. Sci. Rep. 2019, 9, 13534. [Google Scholar] [CrossRef] [Green Version]
- Amezcua-Gálvez, J.E.; Lopez-Garcia, C.A.; Villarreal-Garza, C.; Lopez-Rivera, V.; Canavati-Marcos, M.; Santuario-Facio, S.; Dono, A.; Monroig-Bosque, P.D.C.; Ortiz-López, R.; Leal-Lopez, A.; et al. Concordance between Ki-67 index in invasive breast cancer and molecular signatures: EndoPredict and MammaPrint. Mol. Clin. Oncol. 2022, 17, 132. [Google Scholar] [CrossRef]
- Erber, R.; Angeloni, M.; Stöhr, R.; Lux, M.P.; Ulbrich-Gebauer, D.; Pelz, E.; Bankfalvi, A.; Schmid, K.W.; Walter, R.F.H.; Vetter, M.; et al. Molecular Subtyping of Invasive Breast Cancer Using a PAM50-Based Multigene Expression Test-Comparison with Molecular-Like Subtyping by Tumor Grade/Immunohistochemistry and Influence on Oncologist’s Decision on Systemic Therapy in a Real-World Setting. Int. J. Mol. Sci. 2022, 23, 8716. [Google Scholar] [CrossRef]
- Cuzick, J.; Dowsett, M.; Pineda, S.; Wale, C.; Salter, J.; Quinn, E.; Zabaglo, L.; Mallon, E.; Green, A.R.; Ellis, I.O.; et al. Prognostic Value of a Combined Estrogen Receptor, Progesterone Receptor, Ki-67, and Human Epidermal Growth Factor Receptor 2 Immunohistochemical Score and Comparison with the Genomic Health Recurrence Score in Early Breast Cancer. J. Clin. Oncol. 2011, 29, 4273–4278. [Google Scholar] [CrossRef] [Green Version]
- Harbeck, N.; Rastogi, P.; Martin, M.; Tolaney, S.; Shao, Z.; Fasching, P.; Huang, C.; Jaliffe, G.; Tryakin, A.; Goetz, M.; et al. Adjuvant abemaciclib combined with endocrine therapy for high-risk early breast cancer: Updated efficacy and Ki-67 analysis from the monarchE study. Ann. Oncol. 2021, 32, 1571–1581. [Google Scholar] [CrossRef] [PubMed]
- Polewski, M.D.; Nielsen, G.B.B.; Gu, Y.; Weaver, A.T.B.; Gegg, G.B.; Tabuena-Frolli, S.B.; Cajaiba, M.; Hanks, D.; Method, M.M.; Press, M.F.M.; et al. A Standardized Investigational Ki-67 Immunohistochemistry Assay Used to Assess High-Risk Early Breast Cancer Patients in the monarchE Phase 3 Clinical Study Identifies a Population with Greater Risk of Disease Recurrence When Treated with Endocrine Therapy Alone. Appl. Immunohistochem. Mol. Morphol. 2022, 30, 237–245. [Google Scholar] [CrossRef] [PubMed]
- Kumaki, N.; Umemura, S.; Tang, X.; Saito, Y.; Suzuki, Y.; Tokuda, Y. Alteration of immunohistochemical biomarkers between pre- and post-chemotherapy: Hormone receptors, HER2 and Ki-67. Breast Cancer 2011, 18, 98–102. [Google Scholar] [CrossRef] [PubMed]
- Avci, N.; Deligonul, A.; Tolunay, S.; Cubukcu, E.; Olmez, O.F.; Ulas, A.; Hartavi, M.; Kurt, E.; Evrensel, T. Neoadjuvant chemotherapy-induced changes in immunohistochemical expression of estrogen receptor, progesterone receptor, HER2, and Ki-67 in patients with breast cancer. J. BUON 2015, 20, 45–49. [Google Scholar] [PubMed]
- Nishimura, R.; Osako, T.; Okumura, Y.; Tashima, R.; Toyozumi, Y.; Arima, N. Changes in the ER, PgR, HER2, p53 and Ki-67 biological markers between primary and recurrent breast cancer: Discordance rates and prognosis. World J. Surg. Oncol. 2011, 9, 131. [Google Scholar] [CrossRef] [Green Version]
- Qin, Q.; Gao, F.; Jiang, W.; Tan, Q.; Mo, Q.; Wei, C. Effect of neoadjuvant chemotherapy on expressions of estrogen receptor, progesterone receptor, human epidermal growth factor receptor 2, and Ki-67 in breast cancer. Chin. Med. J. 2014, 127, 3272–3277. [Google Scholar]
- Li, L.; Han, N.; Wang, X.; Wang, Q.; Tian, J.; Yao, J.; Yuan, L.; Qian, K.; Zou, Q.; Yi, W.; et al. Prognostic values of Ki-67 in neoadjuvant setting for breast cancer: A systematic review and meta-analysis. Futur. Oncol. 2017, 13, 1021–1034. [Google Scholar] [CrossRef]
- Miglietta, L.; Morabito, F.; Provinciali, N.; Canobbio, L.; Meszaros, P.; Naso, C.; Murialdo, R.; Boitano, M.; Salvi, S.; Ferrarini, M. A prognostic model based on combining estrogen receptor expression and Ki-67 value after neoadjuvant chemotherapy predicts clinical outcome in locally advanced breast cancer: Extension and analysis of a previously reported cohort of patients. Eur. J. Surg. Oncol. (EJSO) 2013, 39, 1046–1052. [Google Scholar] [CrossRef]
- Miglietta, L.; Vanella, P.; Canobbio, L.; Naso, C.; Cerisola, N.; Meszaros, P.; Parodi, M.; Morabito, F. Prognostic Value of Estrogen Receptor and Ki-67 Index after Neoadjuvant Chemotherapy in Locally Advanced Breast Cancer Expressing High Levels of Proliferation at Diagnosis. Oncology 2010, 79, 255–261. [Google Scholar] [CrossRef]
- Tan, Q.-X.; Qin, Q.-H.; Yang, W.-P.; Mo, Q.-G.; Wei, C.-Y. Prognostic value of Ki67 expression in HR-negative breast cancer before and after neoadjuvant chemotherapy. Int. J. Clin. Exp. Pathol. 2014, 7, 6862–6870. [Google Scholar]
- Tan, S.; Fu, X.; Xu, S.; Qiu, P.; Lv, Z.; Xu, Y.; Zhang, Q. Quantification of Ki67 Change as a Valid Prognostic Indicator of Luminal B Type Breast Cancer After Neoadjuvant Therapy. Pathol. Oncol. Res. 2021, 27, 1609972. [Google Scholar] [CrossRef] [PubMed]
- Yamazaki, N.; Wada, N.; Yamauchi, C.; Yoneyama, K. High expression of post-treatment Ki-67 status is a risk factor for locoregional recurrence following breast-conserving surgery after neoadjuvant chemotherapy. Eur. J. Surg. Oncol. (EJSO) 2015, 41, 617–624. [Google Scholar] [CrossRef] [PubMed]
- Nishimura, R.; Osako, T.; Okumura, Y.; Hayashi, M.; Arima, N. Clinical significance of Ki-67 in neoadjuvant chemotherapy for primary breast cancer as a predictor for chemosensitivity and for prognosis. Breast Cancer 2009, 17, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Im, Y.H.; Lee, S.H.; Cho, E.Y.; Choi, Y.L.; Ko, Y.H.; Kim, J.H.; Nam, S.J.; Kim, H.J.; Ahn, J.S.; et al. Evaluation of ER and Ki-67 proliferation index as prognostic factors for survival following neoadjuvant chemotherapy with doxorubicin/docetaxel for locally advanced breast cancer. Cancer Chemother. Pharmacol. 2007, 61, 569–577. [Google Scholar] [CrossRef]
- Ács, B.; Zámbó, V.; Vízkeleti, L.; Szász, A.M.; Madaras, L.; Szentmártoni, G.; Tőkés, T.; Molnár, B.; Molnár, I.A.; Vári-Kakas, S.; et al. Ki-67 as a controversial predictive and prognostic marker in breast cancer patients treated with neoadjuvant chemotherapy. Diagn. Pathol. 2017, 12, 20. [Google Scholar] [CrossRef] [Green Version]
- Chen, C.; Zhang, Y.; Huang, Z.; Wu, J.; Huang, W.; Zhang, G. Decrease in the Ki67 index during neoadjuvant chemotherapy predicts favorable relapse-free survival in patients with locally advanced breast cancer. Cancer Biol. Med. 2019, 16, 575–586. [Google Scholar] [CrossRef]
- Matsubara, N.; Mukai, H.; Fujii, S.; Wada, N. Different prognostic significance of Ki-67 change between pre- and post-neoadjuvant chemotherapy in various subtypes of breast cancer. Breast Cancer Res. Treat. 2012, 137, 203–212. [Google Scholar] [CrossRef]
- Chen, R.; Ye, Y.; Yang, C.; Peng, Y.; Zong, B.; Qu, F.; Tang, Z.; Wang, Y.; Su, X.; Li, H.; et al. Assessment of the predictive role of pretreatment Ki-67 and Ki-67 changes in breast cancer patients receiving neoadjuvant chemotherapy according to the molecular classification: A retrospective study of 1010 patients. Breast Cancer Res. Treat. 2018, 170, 35–43. [Google Scholar] [CrossRef] [Green Version]
- Chen, X.; He, C.; Han, D.; Zhou, M.; Wang, Q.; Tian, J.; Li, L.; Xu, F.; Zhou, E.; Yang, K. The predictive value of Ki-67 before neoadjuvant chemotherapy for breast cancer: A systematic review and meta-analysis. Futur. Oncol. 2017, 13, 843–857. [Google Scholar] [CrossRef]
- Choi, S.B.; Park, J.M.; Ahn, J.H.; Go, J.; Kim, J.; Park, H.S.; Kim, S.I.; Park, B.-W.; Park, S. Ki-67 and breast cancer prognosis: Does it matter if Ki-67 level is examined using preoperative biopsy or postoperative specimen? Breast Cancer Res. Treat. 2022, 192, 343–352. [Google Scholar] [CrossRef]
- Boyaci, C.; Sun, W.; Robertson, S.; Acs, B.; Hartman, J. Independent Clinical Validation of the Automated Ki67 Scoring Guideline from the International Ki67 in Breast Cancer Working Group. Biomolecules 2021, 11, 1612. [Google Scholar] [CrossRef] [PubMed]
- Erices-Leclercq, M.; Lubig, S.; Förster, F.; Förster, R.; Baldus, S.; Rudlowski, C.; Schröder, L. Prognostic relevance of Ki67 expression in primary male breast cancer: Determination of cut-off points by different evaluation methods and statistical examinations. J. Cancer Res. Clin. Oncol. 2021, 148, 441–447. [Google Scholar] [CrossRef] [PubMed]
- de Gregorio, A.; Friedl, T.W.P.; Hering, E.; Widschwendter, P.; de Gregorio, N.; Bekes, I.; Janni, W.; Dayan, D.; Huober, J.B. Ki67 as Proliferative Marker in Patients with Early Breast Cancer and Its Association with Clinicopathological Factors. Oncology 2021, 99, 780–789. [Google Scholar] [CrossRef] [PubMed]
- Zhang, A.; Wang, X.; Fan, C.; Mao, X. The Role of Ki67 in Evaluating Neoadjuvant Endocrine Therapy of Hormone Receptor-Positive Breast Cancer. Front. Endocrinol. 2021, 12, 687244. [Google Scholar] [CrossRef] [PubMed]
- Smith, I.; Robertson, J.; Kilburn, L.; Wilcox, M.; Evans, A.; Holcombe, C.; Horgan, K.; Kirwan, C.; Mallon, E.; Sibbering, M.; et al. Long-term outcome and prognostic value of Ki67 after perioperative endocrine therapy in postmenopausal women with hormone-sensitive early breast cancer (POETIC): An open-label, multicentre, parallel-group, randomised, phase 3 trial. Lancet Oncol. 2020, 21, 1443–1454. [Google Scholar] [CrossRef] [PubMed]
- Ellis, M.J.; Suman, V.J.; Hoog, J.; Goncalves, R.; Sanati, S.; Creighton, C.J.; DeSchryver, K.; Crouch, E.; Brink, A.; Watson, M.; et al. Ki67 Proliferation Index as a Tool for Chemotherapy Decisions during and After Neoadjuvant Aromatase Inhibitor Treatment of Breast Cancer: Results From the American College of Surgeons Oncology Group Z1031 Trial (Alliance). J. Clin. Oncol. 2017, 35, 1061–1069. [Google Scholar] [CrossRef] [PubMed]
- Ellis, M.J.; Tao, Y.; Luo, J.; A’Hern, R.; Evans, D.B.; Bhatnagar, A.S.; Ross, H.A.S.; Von Kameke, A.; Miller, W.R.; Smith, I.; et al. Outcome Prediction for Estrogen Receptor-Positive Breast Cancer Based on Postneoadjuvant Endocrine Therapy Tumor Characteristics. J. Natl. Cancer Inst. 2008, 100, 1380–1388. [Google Scholar] [CrossRef] [PubMed]
- Ma, C.X.; Gao, F.; Luo, J.; Northfelt, D.W.; Goetz, M.; Forero, A.; Hoog, J.; Naughton, M.; Ademuyiwa, F.; Suresh, R.; et al. NeoPalAna: Neoadjuvant Palbociclib, a Cyclin-Dependent Kinase 4/6 Inhibitor, and Anastrozole for Clinical Stage 2 or 3 Estrogen Receptor–Positive Breast Cancer. Clin. Cancer Res. 2017, 23, 4055–4065. [Google Scholar] [CrossRef] [Green Version]
- Hurvitz, S.A.; Martin, M.; Press, M.F.; Chan, D.; Fernandez-Abad, M.; Petru, E.; Rostorfer, R.; Guarneri, V.; Huang, C.-S.; Barriga, S.; et al. Potent Cell-Cycle Inhibition and Upregulation of Immune Response with Abemaciclib and Anastrozole in neoMONARCH, Phase II Neoadjuvant Study in HR+/HER2− Breast Cancer. Clin. Cancer Res. 2020, 26, 566–580. [Google Scholar] [CrossRef] [Green Version]
- Johnston, S.; Puhalla, S.; Wheatley, D.; Ring, A.; Barry, P.; Holcombe, C.; Boileau, J.F.; Provencher, L.; Robidoux, A.; Rimawi, M.; et al. Randomized Phase II Study Evaluating Palbociclib in Addition to Letrozole as Neoadjuvant Therapy in Estrogen Receptor–Positive Early Breast Cancer: PALLET Trial. J. Clin. Oncol. 2019, 37, 178–189. [Google Scholar] [CrossRef]
- Arnaout, A.; Robertson, S.; Pond, G.R.; Vieth, R.; Jeong, A.; Hilton, J.; Ramsey, T.; Clemons, M. Randomized window of opportunity trial evaluating high-dose vitamin D in breast cancer patients. Breast Cancer Res. Treat. 2019, 178, 347–356. [Google Scholar] [CrossRef]
- Arnaout, A.; Robertson, S.J.; Pond, G.R.; Lee, H.; Jeong, A.; Ianni, L.; Kroeger, L.; Hilton, J.; Coupland, S.; Gottlieb, C.; et al. A randomized, double-blind, window of opportunity trial evaluating the effects of chloroquine in breast cancer patients. Breast Cancer Res. Treat. 2019, 178, 327–335. [Google Scholar] [CrossRef]
- Robertson, J.F.; Coleman, R.E.; Cheung, K.-L.; Evans, A.; Holcombe, C.; Skene, A.; Rea, D.; Ahmed, S.; Jahan, A.; Horgan, K.; et al. Proliferation and AKT Activity Biomarker Analyses after Capivasertib (AZD5363) Treatment of Patients with ER+ Invasive Breast Cancer (STAKT). Clin. Cancer Res. 2019, 26, 1574–1585. [Google Scholar] [CrossRef]
- Goldstein, L.J.; Perez, R.P.; Yardley, D.; Han, L.K.; Reuben, J.M.; Gao, H.; McCanna, S.; Butler, B.; Ruffini, P.A.; Liu, Y.; et al. A window-of-opportunity trial of the CXCR1/2 inhibitor reparixin in operable HER-2-negative breast cancer. Breast Cancer Res. 2020, 22, 4–9. [Google Scholar] [CrossRef]
- Leary, A.; Evans, A.; Johnston, S.R.; A’Hern, R.; Bliss, J.M.; Sahoo, R.; Detre, S.; Haynes, B.P.; Hills, M.; Harper-Wynne, C.; et al. Antiproliferative Effect of Lapatinib in HER2-Positive and HER2-Negative/HER3-High Breast Cancer: Results of the Presurgical Randomized MAPLE Trial (CRUK E/06/039). Clin. Cancer Res. 2015, 21, 2932–2940. [Google Scholar] [CrossRef] [Green Version]
- von Minckwitz, G.; Schmitt, W.D.; Loibl, S.; Müller, B.M.; Blohmer, J.U.; Sinn, B.V.; Eidtmann, H.; Eiermann, W.; Gerber, B.; Tesch, H.; et al. Ki67 Measured after Neoadjuvant Chemotherapy for Primary Breast Cancer. Clin. Cancer Res. 2013, 19, 4521–4531. [Google Scholar] [CrossRef] [Green Version]
- Jones, R.L.; Salter, J.; A’Hern, R.; Nerurkar, A.; Parton, M.; Reis-Filho, J.S.; Smith, I.E.; Dowsett, M. The prognostic significance of Ki67 before and after neoadjuvant chemotherapy in breast cancer. Breast Cancer Res. Treat. 2008, 116, 53–68. [Google Scholar] [CrossRef]
- Symmans, W.F.; Wei, C.; Gould, R.; Yu, X.; Zhang, Y.; Liu, M.; Walls, A.; Bousamra, A.; Ramineni, M.; Sinn, B.; et al. Long-Term Prognostic Risk after Neoadjuvant Chemotherapy Associated with Residual Cancer Burden and Breast Cancer Subtype. J. Clin. Oncol. 2017, 35, 1049–1060. [Google Scholar] [CrossRef] [Green Version]
- Sheri, A.; Smith, I.E.; Johnston, S.R.; A’Hern, R.; Nerurkar, A.; Jones, R.; Hills, M.; Detre, S.; Pinder, S.E.; Symmans, W.F.; et al. Residual proliferative cancer burden to predict long-term outcome following neoadjuvant chemotherapy. Ann. Oncol. 2014, 26, 75–80. [Google Scholar] [CrossRef]
- Assersohn, L.; Salter, J.; Powles, T.; A’Hern, R.; Makris, A.; Gregory, R.; Chang, J.; Dowsett, M. Studies of the Potential Utility of Ki67 as a Predictive Molecular Marker of Clinical Response in Primary Breast Cancer. Breast Cancer Res. Treat. 2003, 82, 113–123. [Google Scholar] [CrossRef]
- Hofmann, D.; Nitz, U.; Gluz, O.; Kates, R.E.; Schinkoethe, T.; Staib, P.; Harbeck, N. WSG ADAPT—Adjuvant dynamic marker-adjusted personalized therapy trial optimizing risk assessment and therapy response prediction in early breast cancer: Study protocol for a prospective, multi-center, controlled, non-blinded, randomized, investigator initiated phase II/III trial. Trials 2013, 14, 261. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Polley, M.-Y.C.; Leung, S.C.Y.; McShane, L.M.; Gao, D.; Hugh, J.C.; Mastropasqua, M.G.; Viale, G.; Zabaglo, L.A.; Penault-Llorca, F.; Bartlett, J.M.; et al. An International Ki67 Reproducibility Study. Gynecol. Oncol. 2013, 105, 1897–1906. [Google Scholar] [CrossRef] [Green Version]
- Polley, M.-Y.C.; Leung, S.C.Y.; Gao, D.; Mastropasqua, M.G.; A Zabaglo, L.; Bartlett, J.M.S.; McShane, L.M.; A Enos, R.; Badve, S.S.; Bane, A.L.; et al. An international study to increase concordance in Ki67 scoring. Mod. Pathol. 2015, 28, 778–786. [Google Scholar] [CrossRef] [PubMed]
- Leung, S.C.Y.; O Nielsen, T.; Zabaglo, L.; Arun, I.; Badve, S.S.; Bane, A.L.; Bartlett, J.M.S.; Borgquist, S.; Chang, M.C.; Dodson, A.; et al. Analytical validation of a standardized scoring protocol for Ki67: Phase 3 of an international multicenter collaboration. NPJ Breast Cancer 2016, 2, 16014. [Google Scholar] [CrossRef] [Green Version]
- Leung, S.C.Y.; O Nielsen, T.; A Zabaglo, L.; Arun, I.; Badve, S.S.; Bane, A.L.; Bartlett, J.M.S.; Borgquist, S.; Chang, M.C.; Dodson, A.; et al. Analytical validation of a standardised scoring protocol for Ki67 immunohistochemistry on breast cancer excision whole sections: An international multicentre collaboration. Histopathology 2019, 75, 225–235. [Google Scholar] [CrossRef]
- Zabaglo, L.; Salter, J.; Anderson, H.; Quinn, E.; Hills, M.; Detre, S.; A’Hern, R.; Dowsett, M. Comparative validation of the SP6 antibody to Ki67 in breast cancer. J. Clin. Pathol. 2010, 63, 800–804. [Google Scholar] [CrossRef]
- Acs, B.; Leung, S.C.Y.; Kidwell, K.M.; Arun, I.; Augulis, R.; Badve, S.S.; Bai, Y.; Bane, A.L.; Bartlett, J.M.S.; Bayani, J.; et al. Systematically higher Ki67 scores on core biopsy samples compared to corresponding resection specimen in breast cancer: A multi-operator and multi-institutional study. Mod. Pathol. 2022, 35, 1362–1369. [Google Scholar] [CrossRef]
- Allison, K.H.; Hammond, M.E.H.; Dowsett, M.; McKernin, S.E.; Carey, L.A.; Fitzgibbons, P.L.; Hayes, D.F.; Lakhani, S.R.; Chavez-MacGregor, M.; Perlmutter, J.; et al. Estrogen and Progesterone Receptor Testing in Breast Cancer: ASCO/CAP Guideline Update. J. Clin. Oncol. 2020, 38, 1346–1366. [Google Scholar] [CrossRef]
- Wolff, A.C.; Hammond, M.E.H.; Allison, K.H.; Harvey, B.E.; Mangu, P.B.; Bartlett, J.M.S.; Bilous, M.; Ellis, I.O.; Fitzgibbons, P.; Hanna, W.; et al. Human Epidermal Growth Factor Receptor 2 Testing in Breast Cancer: American Society of Clinical Oncology/College of American Pathologists Clinical Practice Guideline Focused Update. J. Clin. Oncol. 2018, 36, 2105–2122. [Google Scholar] [CrossRef] [Green Version]
- Nielsen, T.O.; Leung, S.C.Y.; McShane, L.M.; Dowsett, M.; Hayes, D.F.; The International Ki67 in Breast Cancer Working Group. Response to Zhang and Yang. Gynecol. Oncol. 2021, 113, 1597–1598. [Google Scholar] [CrossRef]
- Hammond, M.E.H.; Hayes, D.F.; Dowsett, M.; Allred, D.C.; Hagerty, K.L.; Badve, S.; Fitzgibbons, P.L.; Francis, G.; Goldstein, N.S.; Hayes, M.; et al. American Society of Clinical Oncology/College of American Pathologists Guideline Recommendations for Immunohistochemical Testing of Estrogen and Progesterone Receptors in Breast Cancer. J. Clin. Oncol. 2010, 28, 2784–2795. [Google Scholar] [CrossRef] [Green Version]
- Hammond, M.E.H.; Hayes, D.F.; Dowsett, M.; Allred, D.C.; Hagerty, K.L.; Badve, S.; Fitzgibbons, P.L.; Francis, G.; Goldstein, N.S.; Hayes, M.; et al. American Society of Clinical Oncology/College of American Pathologists Guideline Recommendations for Immunohistochemical Testing of Estrogen and Progesterone Receptors in Breast Cancer. Arch. Pathol. Lab. Med. 2010, 134, 907–922. [Google Scholar] [CrossRef]
- Wolff, A.C.; Hammond, M.E.H.; Hicks, D.G.; Dowsett, M.; McShane, L.M.; Allison, K.H.; Allred, D.C.; Bartlett, J.M.S.; Bilous, M.; Fitzgibbons, P.; et al. Recommendations for Human Epidermal Growth Factor Receptor 2 Testing in Breast Cancer: American Society of Clinical Oncology/College of American Pathologists Clinical Practice Guideline Update. J. Clin. Oncol. 2013, 31, 3997–4013. [Google Scholar] [CrossRef]
- Wolff, A.C.; Hammond, M.E.H.; Hicks, D.G.; Dowsett, M.; McShane, L.M.; Allison, K.H.; Allred, D.C.; Bartlett, J.M.; Bilous, M.; Fitzgibbons, P.; et al. Recommendations for Human Epidermal Growth Factor Receptor 2 Testing in Breast Cancer: American Society of Clinical Oncology/College of American Pathologists Clinical Practice Guideline Update. Arch. Pathol. Lab. Med. 2013, 138, 241–256. [Google Scholar] [CrossRef] [Green Version]
- Paik, S.; Tang, G.; Shak, S.; Kim, C.; Baker, J.; Kim, W.; Cronin, M.; Baehner, F.L.; Watson, D.; Bryant, J.; et al. Gene Expression and Benefit of Chemotherapy in Women With Node-Negative, Estrogen Receptor–Positive Breast Cancer. J. Clin. Oncol. 2006, 24, 3726–3734. [Google Scholar] [CrossRef]
- Sahebjam, S.; Aloyz, R.; Pilavdzic, D.; Brisson, M.-L.; Ferrario, C.; Bouganim, N.; Cohen, V.; Miller, W.H.; Panasci, L.C. Ki 67 is a major, but not the sole determinant of Oncotype Dx recurrence score. Br. J. Cancer 2011, 105, 1342–1345. [Google Scholar] [CrossRef] [Green Version]
- Williams, D.J.; Cohen, C.; Darrow, M.; Page, A.J.; Chastain, B.; Adams, A.L. Proliferation (Ki-67 and Phosphohistone H3) and Oncotype DX Recurrence Score in Estrogen Receptor-positive Breast Cancer. Appl. Immunohistochem. Mol. Morphol. 2011, 19, 431–436. [Google Scholar] [CrossRef]
- Thakur, S.S.; Li, H.; Chan, A.M.Y.; Tudor, R.; Bigras, G.; Morris, D.; Enwere, E.K.; Yang, H. The use of automated Ki67 analysis to predict Oncotype DX risk-of-recurrence categories in early-stage breast cancer. PLoS ONE 2018, 13, e0188983. [Google Scholar] [CrossRef] [Green Version]
- Patel, R.; Hovstadius, M.; Kier, M.W.; Moshier, E.L.; Zimmerman, B.S.; Cascetta, K.; Jaffer, S.; Sparano, J.A.; Tiersten, A. Correlation of the Ki67 Working Group prognostic risk categories with the Oncotype DX Recurrence Score in early breast cancer. Cancer 2022, 128, 3602–3609. [Google Scholar] [CrossRef]
- Dowsett, M.; Allred, C.; Knox, J.; Quinn, E.; Salter, J.; Wale, C.; Cuzick, J.; Houghton, J.; Williams, N.; Mallon, E.; et al. Relationship Between Quantitative Estrogen and Progesterone Receptor Expression and Human Epidermal Growth Factor Receptor 2 (HER-2) Status With Recurrence in the Arimidex, Tamoxifen, Alone or in Combination Trial. J. Clin. Oncol. 2008, 26, 1059–1065. [Google Scholar] [CrossRef]
- Dowsett, M.; Salter, J.; Zabaglo, L.; Mallon, E.; Howell, A.; Buzdar, A.U.; Forbes, J.; Pineda, S.; Cuzick, J. Predictive algorithms for adjuvant therapy: TransATAC. Steroids 2011, 76, 777–780. [Google Scholar] [CrossRef]
- Barton, S.; Zabaglo, L.; A’Hern, R.; Turner, N.; Ferguson, T.; O’Neill, S.; Hills, M.; Smith, I.; Dowsett, M. Assessment of the contribution of the IHC4+C score to decision making in clinical practice in early breast cancer. Br. J. Cancer 2012, 106, 1760–1765. [Google Scholar] [CrossRef]
- Yeo, B.; Zabaglo, L.; Hills, M.; Dodson, A.; E Smith, I.; Dowsett, M. Clinical utility of the IHC4+C score in oestrogen receptor-positive early breast cancer: A prospective decision impact study. Br. J. Cancer 2015, 113, 390–395. [Google Scholar] [CrossRef]
- Turner, B.M.; Gimenez-Sanders, M.A.; Soukiazian, A.; Breaux, A.C.; Skinner, K.; Shayne, M.; Soukiazian, N.; Ling, M.; Hicks, D.G. Risk stratification of ER-positive breast cancer patients: A multi-institutional validation and outcome study of the Rochester Modified Magee algorithm (RoMMa) and prediction of an Oncotype DX®recurrence score < 26. Cancer Med. 2019, 8, 4176–4188. [Google Scholar] [CrossRef] [Green Version]
- Turner, B.M.; A Skinner, K.; Tang, P.; Jackson, M.C.; Soukiazian, N.; Shayne, M.; Huston, A.; Ling, M.; Hicks, D.G. Use of modified Magee equations and histologic criteria to predict the Oncotype DX recurrence score. Mod. Pathol. 2015, 28, 921–931. [Google Scholar] [CrossRef] [Green Version]
- Bhargava, R.; Clark, B.Z.; Dabbs, D.J. Breast Cancers With Magee Equation Score of Less Than 18, or 18-25 and Mitosis Score of 1, Do Not Require Oncotype DX Testing. Am. J. Clin. Pathol. 2018, 151, 316–323. [Google Scholar] [CrossRef] [Green Version]
- Bhargava, R.; Clark, B.Z.; Carter, G.J.; Brufsky, A.M.; Dabbs, D.J. The healthcare value of the Magee Decision Algorithm™: Use of Magee Equations™ and mitosis score to safely forgo molecular testing in breast cancer. Mod. Pathol. 2020, 33, 1563–1570. [Google Scholar] [CrossRef] [Green Version]
- PMA P210026 FDA Summary of Safety and Effectiveness Data; U.S. Food and Drug Administration: Silver Spring, MD, USA, 2021.
- Han, G.; Schell, M.J.; Reisenbichler, E.S.; Guo, B.; Rimm, D.L. Determination of the number of observers needed to evaluate a subjective test and its application in two PD-L1 studies. Stat. Med. 2021, 41, 1361–1375. [Google Scholar] [CrossRef]
- Reisenbichler, E.S.; Han, G.; Bellizzi, A.; Bossuyt, V.; Brock, J.; Cole, K.; Fadare, O.; Hameed, O.; Hanley, K.; Harrison, B.T.; et al. Prospective multi-institutional evaluation of pathologist assessment of PD-L1 assays for patient selection in triple negative breast cancer. Mod. Pathol. 2020, 33, 1746–1752. [Google Scholar] [CrossRef]
- Dowsett, M.; Nielsen, T.O.; Rimm, D.L.; Hayes, D.F. Ki67 as a Companion Diagnostic: Good or Bad News? J. Clin. Oncol. 2022, 40, 3796–3799. [Google Scholar] [CrossRef]
- Royce, M.; Osgood, C.; Mulkey, F.; Bloomquist, E.; Pierce, W.F.; Roy, A.; Kalavar, S.; Ghosh, S.; Philip, R.; Rizvi, F.; et al. FDA Approval Summary: Abemaciclib With Endocrine Therapy for High-Risk Early Breast Cancer. J. Clin. Oncol. 2022, 40, 1155–1162. [Google Scholar] [CrossRef]
- Tarantino, P.; Burstein, H.J.; Lin, N.U.; Krop, I.E.; Winer, E.P.; Schnitt, S.J.; Hamilton, E.P.; Hurvitz, S.A.; Rugo, H.S.; Curigliano, G.; et al. Should Ki-67 be adopted to select breast cancer patients for treatment with adjuvant abemaciclib? Ann. Oncol. 2021, 33, 234–238. [Google Scholar] [CrossRef] [PubMed]
- I Hida, A.; Bando, K.; Sugita, A.; Maeda, T.; Ueda, N.; Matsukage, S.; Nakanishi, M.; Kito, K.; Miyazaki, T.; Ohtsuki, Y.; et al. Visual assessment of Ki67 using a 5-grade scale (Eye-5) is easy and practical to classify breast cancer subtypes with high reproducibility. J. Clin. Pathol. 2015, 68, 356–361. [Google Scholar] [CrossRef] [PubMed]
- Hida, A.I.; Oshiro, Y.; Inoue, H.; Kawaguchi, H.; Yamashita, N.; Moriya, T. Visual assessment of Ki67 at a glance is an easy method to exclude many luminal-type breast cancers from counting 1000 cells. Breast Cancer 2013, 22, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Han, D.; Yu, Y.; Li, J.; Liu, Y. Artificial intelligence-assisted interpretation of Ki-67 expression and repeatability in breast cancer. Diagn. Pathol. 2022, 17, 20. [Google Scholar] [CrossRef]
- Kadivar, M.; Aram, F. Assessment of Ki67 in Breast Cancer: A Comparison between the Eye-10 Method, Stepwise Counting Strategy, and International System of Ki67 Evaluation. Iran. J. Pathol. 2020, 15, 13–18. [Google Scholar] [CrossRef]
- Mungle, T.; Tewary, S.; Arun, I.; Basak, B.; Agarwal, S.; Ahmed, R.; Chatterjee, S.; Maity, A.K.; Chakraborty, C. Automated characterization and counting of Ki-67 protein for breast cancer prognosis: A quantitative immunohistochemistry approach. Comput. Methods Programs Biomed. 2017, 139, 149–161. [Google Scholar] [CrossRef]
- Klauschen, F.; Wienert, S.; Schmitt, W.D.; Loibl, S.; Gerber, B.; Blohmer, J.-U.; Huober, J.; Rüdiger, T.; Erbstößer, E.; Mehta, K.; et al. Standardized Ki67 Diagnostics Using Automated Scoring—Clinical Validation in the GeparTrio Breast Cancer Study. Clin. Cancer Res. 2015, 21, 3651–3657. [Google Scholar] [CrossRef] [Green Version]
- Tomić, S.; Mrklić, I.; Razumović, J.J.; Jonjić, N.; Šarčević, B.; Blažičević, V.; Jurković, I.; Vrbičić, B.; Šikic, N.L.; Peteh, L.L.; et al. Inter-laboratory comparison of Ki-67 proliferating index detected by visual assessment and automated digital image analysis. Breast Dis. 2019, 38, 73–79. [Google Scholar] [CrossRef]
- Kwon, A.-Y.; Park, H.Y.; Hyeon, J.; Nam, S.J.; Kim, S.W.; Lee, J.E.; Yu, J.-H.; Lee, S.K.; Cho, S.Y.; Cho, E.Y. Practical approaches to automated digital image analysis of Ki-67 labeling index in 997 breast carcinomas and causes of discordance with visual assessment. PLoS ONE 2019, 14, e0212309. [Google Scholar] [CrossRef]
- Arihiro, K.; Oda, M.; Ohara, M.; Kadoya, T.; Osaki, A.; Nishisaka, T.; Shiroma, N.; Kobayashi, Y. Comparison of visual assessment and image analysis in the evaluation of Ki-67 expression and their prognostic significance in immunohistochemically defined luminal breast carcinoma. JPN J. Clin. Oncol. 2016, 46, 1081–1087. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yeo, M.-K.; Kim, H.E.; Kim, S.H.; Chae, B.J.; Song, B.J.; Lee, A. Clinical usefulness of the free web-based image analysis application ImmunoRatio for assessment of Ki-67 labelling index in breast cancer. J. Clin. Pathol. 2017, 70, 715–719. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feng, M.; Deng, Y.; Yang, L.; Jing, Q.; Zhang, Z.; Xu, L.; Wei, X.; Zhou, Y.; Wu, D.; Xiang, F.; et al. Automated quantitative analysis of Ki-67 staining and HE images recognition and registration based on whole tissue sections in breast carcinoma. Diagn. Pathol. 2020, 15, 65. [Google Scholar] [CrossRef] [PubMed]
- Hida, A.I.; Omanovic, D.; Pedersen, L.; Oshiro, Y.; Ogura, T.; Nomura, T.; Kurebayashi, J.; Kanomata, N.; Moriya, T. Automated assessment of Ki-67 in breast cancer: The utility of digital image analysis using virtual triple staining and whole slide imaging. Histopathology 2020, 77, 471–480. [Google Scholar] [CrossRef]
- Finkelman, B.S.; Meindl, A.; LaBoy, C.; Griffin, B.; Narayan, S.; Brancamp, R.; Siziopikou, K.P.; Pincus, J.L.; Jr, L.Z.B. Correlation of manual semi-quantitative and automated quantitative Ki-67 proliferative index with OncotypeDXTM recurrence score in invasive breast carcinoma. Breast Dis. 2022, 41, 55–65. [Google Scholar] [CrossRef]
- Laurinavicius, A.; Plancoulaine, B.; Laurinaviciene, A.; Herlin, P.; Meskauskas, R.; Baltrusaityte, I.; Besusparis, J.; Dasevicius, D.; Elie, N.; Iqbal, Y.; et al. A methodology to ensure and improve accuracy of Ki67 labelling index estimation by automated digital image analysis in breast cancer tissue. Breast Cancer Res. 2014, 16, R35. [Google Scholar] [CrossRef] [Green Version]
- Acs, B.; Pelekanou, V.; Bai, Y.; Martinez-Morilla, S.; Toki, M.; Leung, S.C.Y.; Nielsen, T.O.; Rimm, D.L. Ki67 reproducibility using digital image analysis: An inter-platform and inter-operator study. Lab. Investig. 2020, 99, 107–117. [Google Scholar] [CrossRef]
- Ács, B.; Madaras, L.; Kovács, K.A.; Micsik, T.; Tőkés, A.-M.; Győrffy, B.; Kulka, J.; Szász, A.M. Reproducibility and Prognostic Potential of Ki-67 Proliferation Index when Comparing Digital-Image Analysis with Standard Semi-Quantitative Evaluation in Breast Cancer. Pathol. Oncol. Res. 2017, 24, 115–127. [Google Scholar] [CrossRef]
- Rimm, D.L.; Leung, S.C.Y.; McShane, L.M.; Bai, Y.; Bane, A.L.; Bartlett, J.M.S.; Bayani, J.; Chang, M.C.; Dean, M.; Denkert, C.; et al. An international multicenter study to evaluate reproducibility of automated scoring for assessment of Ki67 in breast cancer. Mod. Pathol. 2019, 32, 59–69. [Google Scholar] [CrossRef]
- Zhong, F.; Bi, R.; Yu, B.; Yang, F.; Yang, W.; Shui, R. A Comparison of Visual Assessment and Automated Digital Image Analysis of Ki67 Labeling Index in Breast Cancer. PLoS ONE 2016, 11, e0150505. [Google Scholar] [CrossRef]
- Arun, I.; Venkatesh, S.; Ahmed, R.; Agrawal, S.K.; Leung, S.C.Y. Reliability of Ki67 visual scoring app compared to eyeball estimate and digital image analysis and its prognostic significance in hormone receptor-positive breast cancer. Apmis 2021, 129, 489–502. [Google Scholar] [CrossRef] [PubMed]
- Cornish, T.C. Clinical Application of Image Analysis in Pathology. Adv. Anat. Pathol. 2020, 27, 227–235. [Google Scholar] [CrossRef] [PubMed]
- Acs, B.; Rimm, D.L. QuPath Protocol for Ki67 IHC Evaluation on Core Biopsy Slides and on Whole Slides. 14 December 2018. Available online: https://www.ki67inbreastcancerwg.org/wp-content/uploads/2022/11/QuPath-protocol-for-Ki67-IHC-evaluation_IWGKBC_ModPath.pdf (accessed on 23 January 2023).
- Sinn, H.-P.; Schneeweiss, A.; Keller, M.; Schlombs, K.; Laible, M.; Seitz, J.; Lakis, S.; Veltrup, E.; Altevogt, P.; Eidt, S.; et al. Comparison of immunohistochemistry with PCR for assessment of ER, PR, and Ki-67 and prediction of pathological complete response in breast cancer. BMC Cancer 2017, 17, 124. [Google Scholar] [CrossRef]
- Wirtz, R.M.; Sihto, H.; Isola, J.; Heikkilä, P.; Kellokumpu-Lehtinen, P.-L.; Auvinen, P.; Turpeenniemi-Hujanen, T.; Jyrkkiö, S.; Lakis, S.; Schlombs, K.; et al. Biological subtyping of early breast cancer: A study comparing RT-qPCR with immunohistochemistry. Breast Cancer Res. Treat. 2016, 157, 437–446. [Google Scholar] [CrossRef] [Green Version]
- Laible, M.; Schlombs, K.; Kaiser, K.; Veltrup, E.; Herlein, S.; Lakis, S.; Stöhr, R.; Eidt, S.; Hartmann, A.; Wirtz, R.M.; et al. Technical validation of an RT-qPCR in vitro diagnostic test system for the determination of breast cancer molecular subtypes by quantification of ERBB2, ESR1, PGR and MKI67 mRNA levels from formalin-fixed paraffin-embedded breast tumor specimens. BMC Cancer 2016, 16, 398. [Google Scholar] [CrossRef] [Green Version]
- Sadeghian, D.; Saffar, H.; Sharif, P.M.; Soleimani, V.; Jahanbin, B. MCM6 versus Ki-67 in diagnosis of luminal molecular subtypes of breast cancers. Diagn. Pathol. 2022, 17, 24. [Google Scholar] [CrossRef]
- Juríková, M.; Danihel, Ľ.; Polák, Š.; Varga, I. Ki67, PCNA, and MCM proteins: Markers of proliferation in the diagnosis of breast cancer. Acta Histochem. 2016, 118, 544–552. [Google Scholar] [CrossRef]
- Al-Keilani, M.S.; Elstaty, R.; Alqudah, M.A. The Prognostic Potential of Neurokinin 1 Receptor in Breast Cancer and Its Relationship with Ki-67 Index. Int. J. Breast Cancer 2022, 2022, 4987912. [Google Scholar] [CrossRef]
- Zarella, M.D.; Heintzelman, R.C.; Popnikolov, N.K.; Garcia, F.U. BCL-2 expression aids in the immunohistochemical prediction of the Oncotype DX breast cancer recurrence score. BMC Clin. Pathol. 2018, 18, 14. [Google Scholar] [CrossRef] [Green Version]
- Mu, K.; Li, L.; Yang, Q.; Yun, H.; Kharaziha, P.; Ye, D.-W.; Auer, G.; Lagercrantz, S.B.; Zetterberg, A. A standardized method for quantifying proliferation by Ki-67 and cyclin A immunohistochemistry in breast cancer. Ann. Diagn. Pathol. 2015, 19, 243–248. [Google Scholar] [CrossRef]
- Tokiniwa, H.; Horiguchi, J.; Takata, D.; Kikuchi, M.; Rokutanda, N.; Nagaoka, R.; Sato, A.; Odawara, H.; Tozuka, K.; Oyama, T.; et al. Topoisomerase II alpha expression and the Ki-67 labeling index correlate with prognostic factors in estrogen receptor-positive and human epidermal growth factor type-2-negative breast cancer. Breast Cancer 2011, 19, 309–314. [Google Scholar] [CrossRef] [PubMed]
- Davey, M.; Davies, M.; Lowery, A.; Miller, N.; Kerin, M. The Role of MicroRNA as Clinical Biomarkers for Breast Cancer Surgery and Treatment. Int. J. Mol. Sci. 2021, 22, 8290. [Google Scholar] [CrossRef] [PubMed]
- Sakurai, M.; Masuda, M.; Miki, Y.; Hirakawa, H.; Suzuki, T.; Sasano, H. Correlation of miRNA Expression Profiling in Surgical Pathology Materials, with Ki-67, HER2, ER and PR in Breast Cancer Patients. Int. J. Biol. Markers 2015, 30, 190–199. [Google Scholar] [CrossRef] [PubMed]
- van den Berg, E.J.; Duarte, R.; Dickens, C.; Joffe, M.; Mohanlal, R.F.M.P. Ki67 Immunohistochemistry Quantification in Breast Carcinoma: A Comparison of Visual Estimation, Counting, and ImmunoRatio. Appl. Immunohistochem. Mol. Morphol. 2020, 29, 105–111. [Google Scholar] [CrossRef]
- Mengel, M.; Von Wasielewski, R.; Wiese, B.; Rüdiger, T.; Müller-Hermelink, H.K.; Kreipe, H. Inter-laboratory and inter-observer reproducibility of immunohistochemical assessment of the Ki-67 labelling index in a large multi-centre trial. J. Pathol. 2002, 198, 292–299. [Google Scholar] [CrossRef]



| Meta- Analysis | Number of Studies | Range of Ki-67 Cutoffs | Range of n | Study Population(s) | Findings |
|---|---|---|---|---|---|
| Mirza et al. [44] | 5 | 1–25% | 212–674 | Node-negative breast cancer | All studies associated with either DFS, OS, or both |
| de Azambuja et al. [45] | 46 | 3.5–34% | 47–863 | Node-negative and -positive breast cancer | Reported overall HR = 1.93 (1.74–2.14) for DFS, and HR = 1.95 (1.70–2.24) for OS, in all patients |
| Stuart-Harris et al. [50] | 43 | 0–28.6% | 100–942 | Node-negative and -positive breast cancer | Reported overall HR = 2.18 (1.92–2.47) for DFS, and HR = 2.09 (1.74–2.52) for OS, in all patients |
| Studies should include a sufficiently large number of participating scorers to represent variability inherent in a broad cross-section of pathology interpretations. |
| Observers performing the scoring in test validation studies need to follow pre-specified training methods and score independently and, in a fashion, blinded to others’ scores. |
| A sufficient number of specimens should be included to have adequate statistical power, and the specimens should represent the entire dynamic range of the assay (in the case of Ki-67 IHC, 0–100%) |
| Although the expected implementation of tests is often categorical, based on one or more cutpoint(s), most tumor biomarkers (including Ki-67) are continuous variables, and data for assessing analytical validity should be captured as such. Doing so will allow for parametric tests that maximize information, and for results to be transposed to alternative cutpoints of clinical relevance. The data distribution for Ki-67 is log-normal, meaning that log transformation is required to satisfy the normal distribution and constant variance assumptions underlying common parametric statistical tests. |
| Studies using biospecimens or linking to prognosis should adhere to Biospecimen Reporting for Improved Study Quality (BRISQ) and Reporting Recommendations for Tumor Marker Prognostic Studies (REMARK) guidelines (including such important features as transparent and detailed reporting of scoring methods so others can apply the system exactly and pre-specified metrics of success, ideally with independent statistical analysis. |
| Specific IKWG Recommendations | Comment | |
|---|---|---|
| Pre-analytic Variables | ||
| Core vs. Excision | Yes | Core biopsies are preferred. Serial analysis of Ki-67 should be performed on the same specimen type. |
| Pre-fixation Delays | Yes | Follow ASCO/CAP guidelines for breast tissue handling [134,135]. Ethanol-fixed or decalcified preparations should not be used. |
| Storage Time | No | Avoid prolonged exposure to air of cut sections on glass slides. |
| Analytic Variables | ||
| Antigen Retrieval | Yes | High-temperature antigen retrieval should be mandatory. |
| Antibody Specificity | No | MIB1 is recognized as the most widely validated antibody. |
| Colorimetric Detection | No | Polymer detection on automated platforms is more sensitive than avidin-biotin systems. |
| Counterstain | Yes | All negative nuclei should be counterstained. |
| QA/QC Control | Yes | QA/QC control should be established and maintained in each laboratory and systematically maintained. Quantitative external quality assessment should be established, and participation should be mandatory. |
| Scoring Interpretation | ||
| Method | Yes | Calculate the percentage of positive invasive carcinoma cells by counting all positive and negative invasive carcinoma cells within the examined region of the slide. Do not consider intensity. |
| Region of Slide | No | A global counting method appears to have higher reproducibility than a hot spot counting method. |
| Digital Imaging | No | Evidence to date suggests that automated scoring is not worse than standardized visual scoring for core-cut biopsies. |
| Data Capture | Yes | Ki-67 data should be captured as a continuous percentage variable, with log transformation for parametric statistical testing. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Finkelman, B.S.; Zhang, H.; Hicks, D.G.; Turner, B.M. The Evolution of Ki-67 and Breast Carcinoma: Past Observations, Present Directions, and Future Considerations. Cancers 2023, 15, 808. https://doi.org/10.3390/cancers15030808
Finkelman BS, Zhang H, Hicks DG, Turner BM. The Evolution of Ki-67 and Breast Carcinoma: Past Observations, Present Directions, and Future Considerations. Cancers. 2023; 15(3):808. https://doi.org/10.3390/cancers15030808
Chicago/Turabian StyleFinkelman, Brian S., Huina Zhang, David G. Hicks, and Bradley M. Turner. 2023. "The Evolution of Ki-67 and Breast Carcinoma: Past Observations, Present Directions, and Future Considerations" Cancers 15, no. 3: 808. https://doi.org/10.3390/cancers15030808
APA StyleFinkelman, B. S., Zhang, H., Hicks, D. G., & Turner, B. M. (2023). The Evolution of Ki-67 and Breast Carcinoma: Past Observations, Present Directions, and Future Considerations. Cancers, 15(3), 808. https://doi.org/10.3390/cancers15030808





