LC-MS/MS Based Volatile Organic Compound Biomarkers Analysis for Early Detection of Lung Cancer
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Study Participants
2.3. Breath Sample Processing and Analysis
2.4. Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) Analysis
2.5. Quality Control
2.6. 16S rRNA
2.7. Statistical Analysis
3. Results
3.1. Effect of Ambient Air
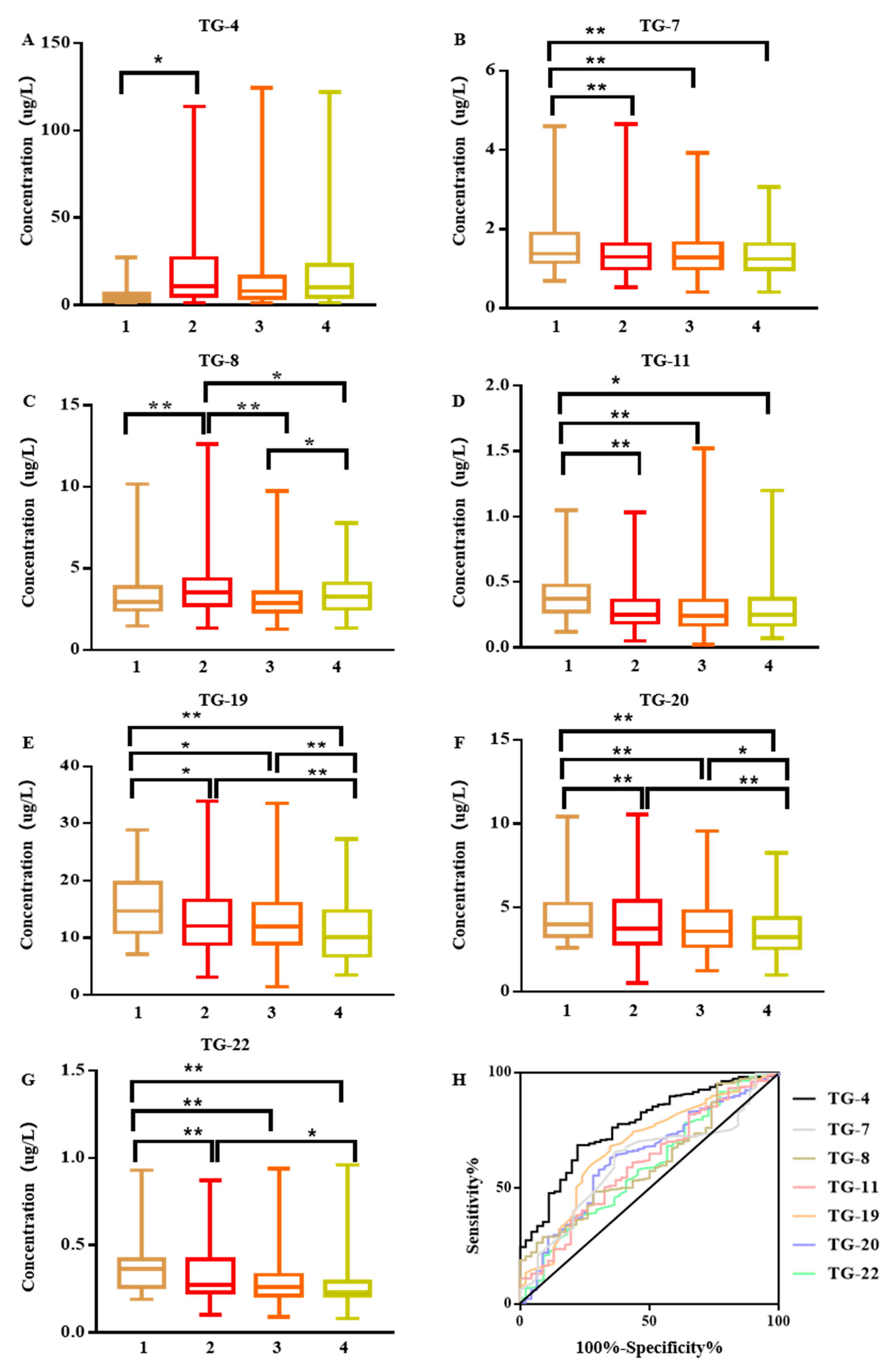
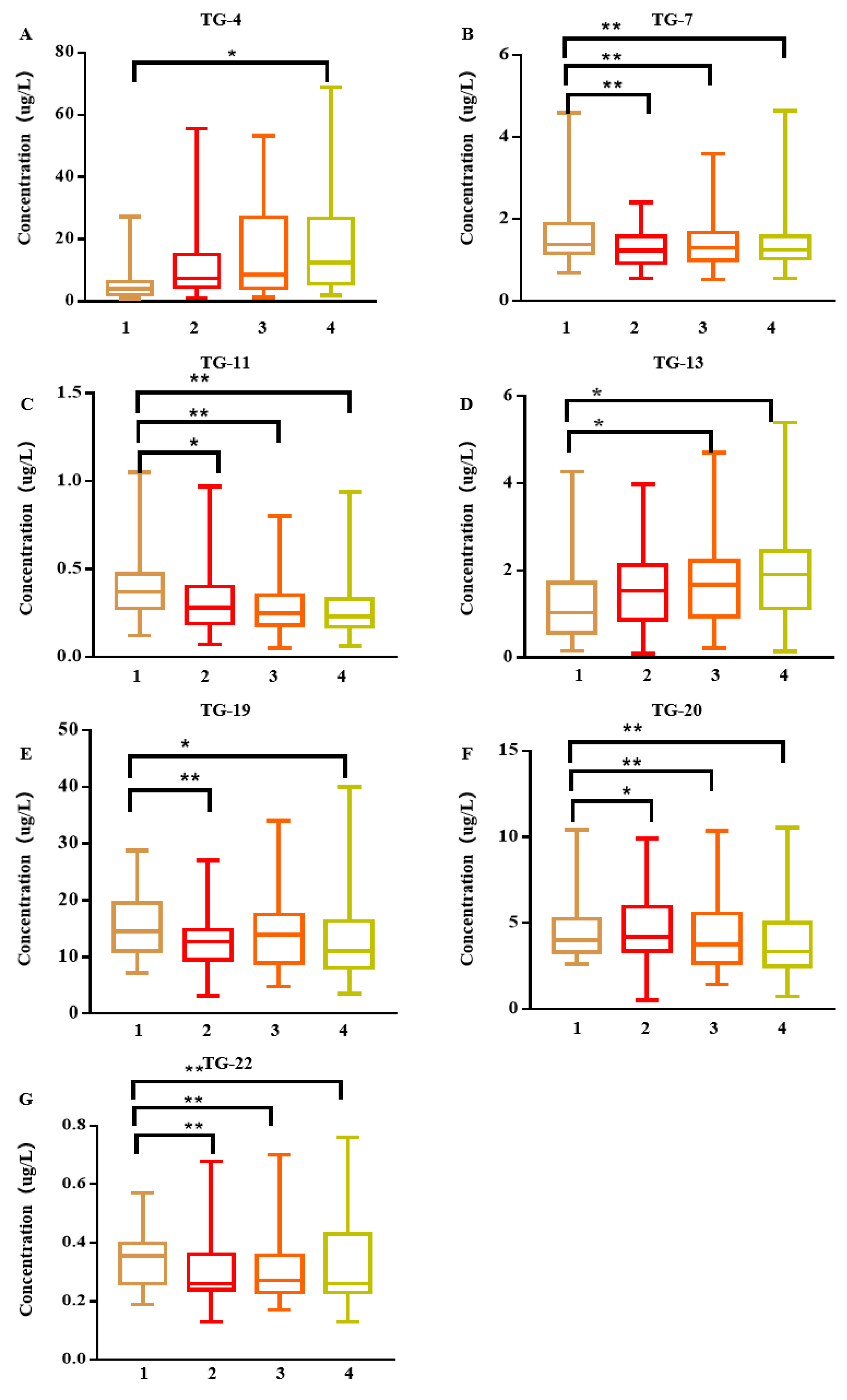
3.2. Carbonyl VOCs in Exhaled Breath of Early Lung Cancer Patients
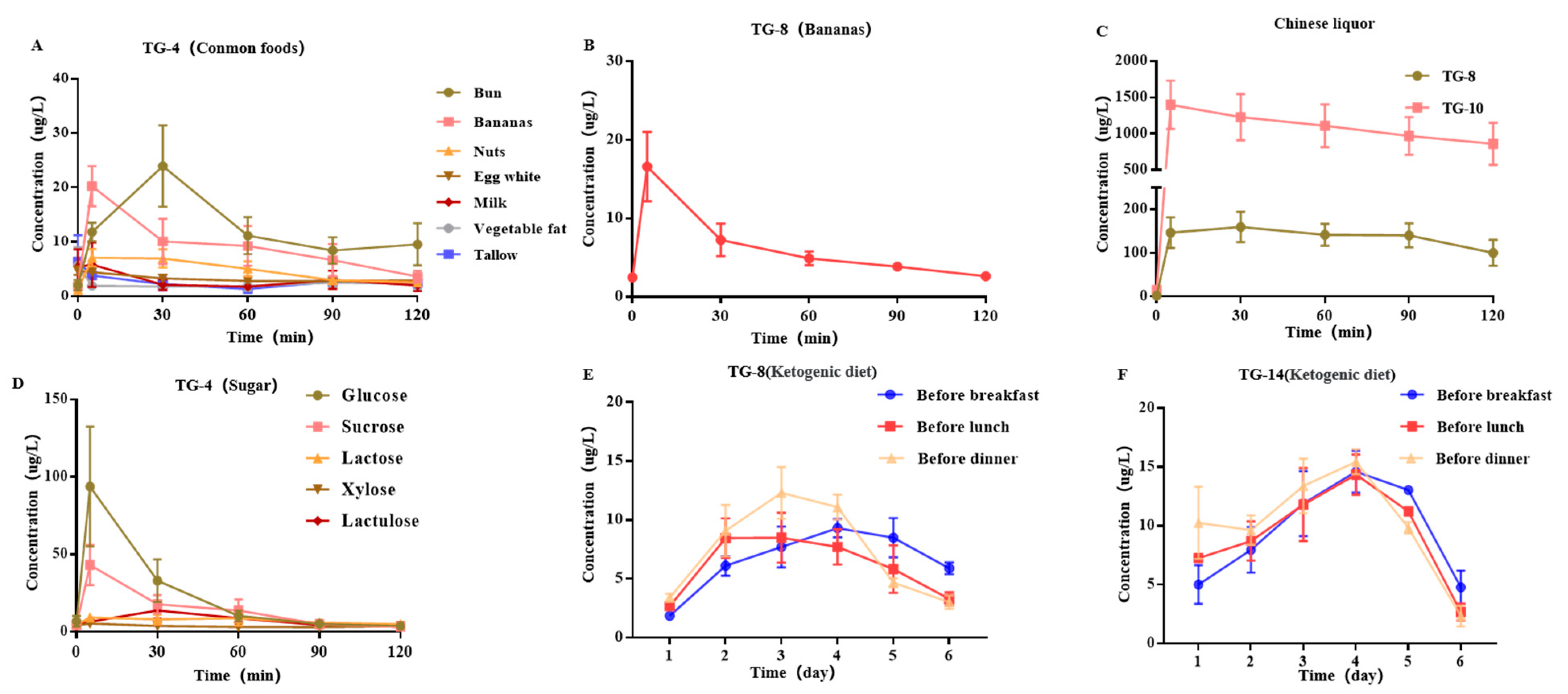
3.3. Effects of Diet on Exhaled Breath Carbonyl VOCs
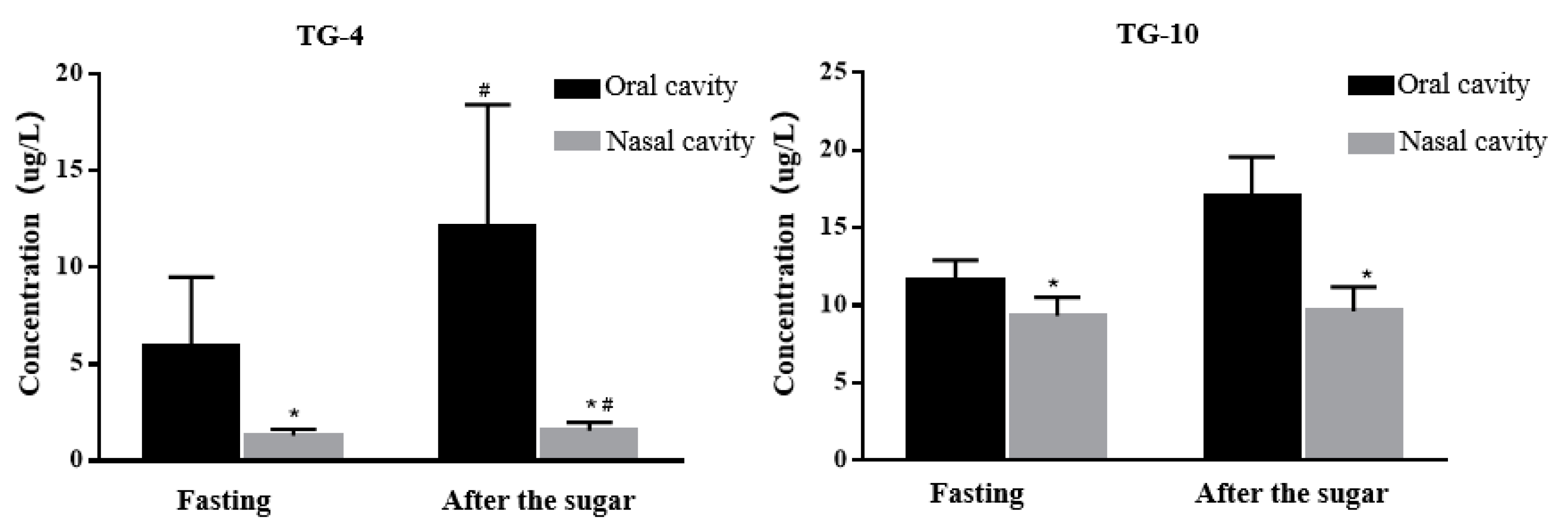
3.4. Influence of Exhalation Mode on Exhalation Collection
3.5. Mouth Glucose Metabolism
3.6. 16S rRNA Detection
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AIS | Adenocarcinoma in situ |
| APCI | Atmospheric pressure chemical ionization |
| AUC | Area under the curve |
| DNPH | 2,4-Dinitrophenylhydrazine |
| ESI | Electrospray ionization |
| GC-MS | Gas chromatography mass spectrometry |
| GC-TOGMS | Gas chromatography time of flight mass spectrometry |
| GI | Glycemic index |
| GNP | Gold nanoparticles |
| HPLC | High-performance liquid chromatography |
| HS-PTV-MS | Headspace temperature programmed vaporization mass spectrometer |
| IAC | Invasive adenocarcinoma |
| LC-MS | Liquid chromatography–mass spectrometry |
| LC-MS/MS | Liquid chromatography and tandem mass spectrometry |
| LD-CT | Low dose computed tomography |
| LOD | Limit of detection |
| LOQ | Limit of quantification |
| LSD-t | Least significant difference test |
| MIA | Minimally invasive adenocarcinoma |
| MRM | Multiple reaction monitoring |
| MS | Mass spectrometry |
| PTFE | Polyfluortetraethylene |
| R | Correlation coefficient |
| ROC | Receiver operating characteristic |
| RSD | Relative standard deviation |
| S/N | Signal-to-noise ratio |
| SPE | Solid-phase extraction |
| VOC | Volatile organic compound |
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2019. CA Cancer J. Clin. 2019, 69, 7–34. [Google Scholar] [CrossRef] [PubMed]
- Henley, S.J.; Ward, E.M.; Scott, S.; Ma, J.; Anderson, R.N.; Firth, A.U.; Thomas, C.C.; Islami, F.; Weir, H.K.; Lewis, D.R.; et al. Annual report to the nation on the status of cancer, part I: National cancer statistics. Cancer 2020, 126, 2225–2249. [Google Scholar] [CrossRef] [PubMed]
- Tanoue, L.T.; Tanner, N.T.; Gould, M.K.; Silvestri, G.A. Lung cancer screening. Am. J. Respir. Crit. Care Med. 2015, 191, 19–33. [Google Scholar] [CrossRef]
- Karachaliou, N.; Sosa, A.E.; Rosell, R. Annual or biennial lung cancer CT screening? J. Thorac. Dis. 2016, 8, 2424–2426. [Google Scholar] [CrossRef] [PubMed]
- Farnum, A.; Parnas, M.; Hoque Apu, E.; Cox, E.; Lefevre, N.; Contag, C.H.; Saha, D. Harnessing insect olfactory neural circuits for detecting and discriminating human cancers. Biosens. Bioelectron. 2023, 219, 114814. [Google Scholar] [CrossRef]
- Saidi, T.; Moufid, M.; de Jesus Beleño-Saenz, K.; Welearegay, T.G.; El Bari, N.; Jaimes-Mogollon, A.L.; Ionescu, R.; Bourkadi, J.E.; Benamor, J.; El Ftouh, M.; et al. Non-invasive prediction of lung cancer histological types through exhaled breath analysis by UV-irradiated electronic nose and GC/QTOF/MS. Sens. Actuators B Chem. 2020, 311, 127932. [Google Scholar] [CrossRef]
- Wang, C.; Dong, R.; Wang, X.; Lian, A.; Chi, C.; Ke, C.; Guo, L.; Liu, S.; Zhao, W.; Xu, G.; et al. Exhaled volatile organic compounds as lung cancer biomarkers during one-lung ventilation. Sci. Rep. 2014, 4, 7312. [Google Scholar] [CrossRef] [PubMed]
- Gordon, S.M.; Szldon, J.P.; Krotoszynski, B.K.; Gibbons, R.D.; O’Neill, H.J. Volatile Organic Compounds in Exhaled Air from Patients with Lung Cancer. Clin. Chem. 1985, 318, 1278–1282. [Google Scholar] [CrossRef]
- Amann, A.; Costello, B.D.L.; Miekisch, W.; Schubert, J.; Buszewski, B.; Pleil, J.; Ratcliffe, N.; Risby, T. The human volatilome: Volatile organic compounds (VOCs) in exhaled breath, skin emanations, urine, feces and saliva. J. Breath Res. 2014, 8, 034001. [Google Scholar] [CrossRef] [PubMed]
- Markar, S.R.; Wiggins, T.; Antonowicz, S.; Chin, S.T.; Romano, A.; Nikolic, K.; Evans, B.; Cunningham, D.; Mughal, M.; Lagergren, J.; et al. Assessment of a noninvasive exhaled breath test for the diagnosis of oesophagogastric cancer. JAMA Oncol. 2018, 4, 970–976. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Skallevold, H.E.; Vallenari, E.M.; Sapkota, D. Salivary Biomarkers in Lung Cancer. Mediators Inflamm. 2021, 2021, 6019791. [Google Scholar] [CrossRef] [PubMed]
- Sholl, L.M. Biomarkers of response to checkpoint inhibitors beyond PD-L1 in lung cancer. Mod. Pathol. 2022, 35, 66–74. [Google Scholar] [CrossRef] [PubMed]
- Otálora-Otálora, B.A.; Osuna-Garzón, D.A.; Carvajal-Parra, M.S.; Cañas, A.; Montecino, M.; López-Kleine, L.; Rojas, A. Identifying General Tumor and Specific Lung Cancer Biomarkers by Transcriptomic Analysis. Biology 2022, 11, 1082. [Google Scholar] [CrossRef] [PubMed]
- Montes, A.G.; Molins López-Rodó, L.; Ramón Rodríguez, I.; Dequigiovanni, G.S.; Nolas Segarra, V.; Sicart, R.M.M.; Hernández Ferrández, J.; José Fibla Alfara, J.; García-Navarro, Á.A. Lung cancer diagnosis by trained dogs. Eur. J. Cardiothorac. Surg. 2017, 52, 1206–1210. [Google Scholar] [CrossRef]
- De Vries, R.; Muller, M.; Van Der Noort, V.; Theelen, W.S.M.E.; Schouten, R.D.; Hummelink, K.; Muller, S.H.; Wolf-Lansdorf, M.; Dagelet, J.W.F.; Monkhorst, K.; et al. Prediction of response to anti-PD-1 therapy in patients with non-small-cell lung cancer by electronic nose analysis of exhaled breath. Ann. Oncol. 2019, 30, 1660–1666. [Google Scholar] [CrossRef] [PubMed]
- Buszewski, B.; Ulanowska, A.; Kowalkowski, T.; Cieliski, K. Investigation of lung cancer biomarkers by hyphenated separation techniques and chemometrics. Clin. Chem. Lab. Med. 2012, 50, 573–581. [Google Scholar] [CrossRef]
- Fu, X.-A.; Li, M.; Knipp, R.J.; Nantz, M.H.; Bousamra, M. Noninvasive detection of lung cancer using exhaled breath. Cancer Med. 2014, 3, 174–181. [Google Scholar] [CrossRef]
- Hanna, G.B.; Boshier, P.R.; Markar, S.R.; Romano, A. Accuracy and Methodologic Challenges of Volatile Organic Compound-Based Exhaled Breath Tests for Cancer Diagnosis: A Systematic Review and Meta-analysis. JAMA Oncol. 2019, 5, e182815. [Google Scholar] [CrossRef]
- Ismail, B.B.; Pu, Y.; Guo, M.; Ma, X.; Liu, D. LC-MS/QTOF identification of phytochemicals and the effects of solvents on phenolic constituents and antioxidant activity of baobab (Adansonia digitata) fruit pulp. Food Chem. 2019, 277, 279–288. [Google Scholar] [CrossRef]
- Williams, M.D.; Reeves, R.; Resar, L.S.; Hill, H.H. Metabolomics of colorectal cancer: Past and current analytical platforms. Anal. Bioanal. Chem. 2013, 405, 5013–5030. [Google Scholar] [CrossRef]
- Weitzel, K.-M. Bond-Dissociation Energies of Cations—Pushing the limits to quantum state resolution. Mass Spectrum. Res. 2011, 30, 221–235. [Google Scholar] [CrossRef] [PubMed]
- Walker, V.; Mills, G.A. Urine 4-heptanone: A β-oxidation product of 2-ethylhexanoic acid from plasticisers. Clin. Chim. Acta 2001, 306, 51–61. [Google Scholar] [CrossRef] [PubMed]
- Horváth, I.; Lázár, Z.; Gyulai, N.; Kollai, M.; Losonczy, G. Exhaled biomarkers in lung cancer. Eur. Respir. J. 2009, 34, 261–275. [Google Scholar] [CrossRef] [PubMed]
- Song, G.; Qin, T.; Liu, H.; Xu, G.B.; Pan, Y.Y.; Xiong, F.X.; Gu, K.S.; Sun, G.P.; Chen, Z.D. Quantitative breath analysis of volatile organic compounds of lung cancer patients. Lung Cancer 2010, 67, 227–231. [Google Scholar] [CrossRef]
- Rudnicka, J.; Walczak, M.; Kowalkowski, T.; Jezierski, T.; Buszewski, B. Determination of volatile organic compounds as potential markers of lung cancer by gas chromatography-mass spectrometry versus trained dogs. Sens. Actuators B Chem. 2014, 202, 615–621. [Google Scholar] [CrossRef]
- Phillips, M.; Cataneo, R.N.; Cummin, A.R.C.; Gagliardi, A.J.; Gleeson, K.; Greenberg, J.; Maxfield, R.A.; Rom, W.N. Detection of lung cancer with volatile markers in the breath. Chest 2003, 123, 2115–2123. [Google Scholar] [CrossRef]
- Peled, N.; Barash, O.; Tisch, U.; Ionescu, R.; Broza, Y.Y.; Ilouze, M.; Mattei, J.; Bunn, P.A.; Hirsch, F.R.; Haick, H. Volatile fingerprints of cancer specific genetic mutations. Nanomed. Nanotechnol. Biol. Med. 2013, 9, 758–766. [Google Scholar] [CrossRef]
- Pérez Antón, A.; Ramos, Á.G.; del Nogal Sánchez, M.; Pavón, J.L.P.; Cordero, B.M.; Pozas, Á.P.C. Headspace-programmed temperature vaporization-mass spectrometry for the rapid determination of possible volatile biomarkers of lung cancer in urine. Anal. Bioanal. Chem. 2016, 408, 5239–5246. [Google Scholar] [CrossRef]
- Hanai, Y.; Shimono, K.; Oka, H.; Baba, Y.; Yamazaki, K.; Beauchamp, G.K. Analysis of volatile organic compounds released from human lung cancer cells and from the urine of tumor-bearing mice. Cancer Cell Int. 2012, 12, 7. [Google Scholar] [CrossRef]
- Pérez Antón, A.; del Nogal Sánchez, M.; Crisolino Pozas, A.Á.P.; Pérez, J.L.P.; Cordero, B.M. Headspace-programmed temperature vaporizer-mass spectrometry and pattern recognition techniques for the analysis of volatiles in saliva samples. Talanta 2016, 160, 21–27. [Google Scholar] [CrossRef]
- Rocco, R.; Incalzi, R.A.; Pennazza, G.; Santonico, M.; Pedone, C.; Bartoli, I.R.; Vernile, C.; Mangiameli, G.; La Rocca, A.; De Luca, G.; et al. BIONOTE e-nose technology may reduce false positives in lung cancer screening programmes. Eur. J. Cardio Thoracic Surg. 2016, 49, 1112–1117. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Yang, D.; Brock, G.; Knipp, R.J.; Bousamra, M.; Nantz, M.H.; Fu, X.-A. Breath carbonyl compounds as biomarkers of lung cancer. Lung Cancer 2015, 90, 92–97. [Google Scholar] [CrossRef] [PubMed]
- Knipp, R.J.; Li, M.; Fu, X.A.; Nantz, M.H. A versatile probe for chemoselective capture and analysis of carbonyl compounds in exhaled breath. Anal. Methods 2015, 7, 6027–6033. [Google Scholar] [CrossRef]
- Horváth, I.; Barnes, P.J.; Loukides, S.; Sterk, P.J.; Högman, M.; Olin, A.C.; Amann, A.; Antus, B.; Baraldi, E.; Bikov, A.; et al. A european respiratory society technical standard: Exhaled biomarkers in lung disease. Eur. Respir. J. 2017, 49, 1600965. [Google Scholar] [CrossRef]
- Martin, A.N.; Farquar, G.R.; Jones, A.D.; Frank, M. Human breath analysis: Methods for sample collection and reduction of localized background effects. Anal. Bioanal. Chem. 2010, 396, 739–750. [Google Scholar] [CrossRef]
- Risby, T.H. Critical issues for breath analysis. J. Breath Res. 2008, 2, 030302. [Google Scholar] [CrossRef]
- Slingers, G.; Goossens, R.; Janssens, H.; Spruyt, M.; Goelen, E.; Vanden, E.M.; Raes, M.; Koppen, G. Real-time selected ion flow tube mass spectrometry to assess short- and long-term variability in oral and nasal breath. J. Breath Res. 2020, 14, 036006. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Zou, X.; Wang, H.; Lu, Y.; Shen, C.; Chu, Y. Standardization study of expiratory conditions for on-line breath testing by proton transfer reaction mass spectrometry. Anal. Biochem. 2019, 581, 113344. [Google Scholar] [CrossRef] [PubMed]
- Kischkel, S.; Miekisch, W.; Patricia, F.; Schubert, J.K. Breath analysis during one-lung ventilation in cancer patients. Eur. Respir. J. 2012, 40, 706–713. [Google Scholar] [CrossRef]
- Capuano, R.; Santonico, M.; Pennazza, G.; Ghezzi, S.; Martinelli, E.; Roscioni, C.; Lucantoni, G.; Galluccio, G.; Paolesse, R.; Di Natale, C.; et al. The lung cancer breath signature: A comparative analysis of exhaled breath and air sampled from inside the lungs. Sci. Rep. 2015, 5, 16491. [Google Scholar] [CrossRef] [Green Version]
- Krilaviciute, A.; Leja, M.; Kopp-Schneider, A.; Barash, O.; Khatib, S.; Ama, H.; Broza, Y.Y.; Polaka, I.; Parshutin, S.; Rudule, A.; et al. Associations of diet and lifestyle factors with common volatile organic compounds in exhaled breath of average-risk individuals. J. Breath Res. 2019, 13, 026006. [Google Scholar] [CrossRef]
- Zou, X.; Wang, H.; Ge, D.; Lu, Y.; Xia, L.; Huang, C.; Shen, X.; Chu, Y. On-line monitoring human breath acetone during exercise and diet by proton transfer reaction mass spectrometry. Future Sci. 2018, 11, 33–40. [Google Scholar] [CrossRef]
- Vishinkin, R.; Haick, H. Nanoscale Sensor Technologies for Disease Detection via Volatolomics. Small 2015, 11, 6142–6164. [Google Scholar] [CrossRef]
- Yang, T.; Rao, Z.; Zhang, X.; Xu, M.; Xu, Z.; Yang, S.T. Metabolic engineering strategies for acetoin and 2,3-butanediol production: Advances and prospects. Crit. Rev. Biotechnol. 2017, 37, 990–1005. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Z.; Lu, J.R. Strategies for enhancing fermentative production of acetoin: A review. Biotechnol. Adv. 2014, 32, 492–503. [Google Scholar] [CrossRef]
- Sun, J.A.; Zhang, L.Y.; Rao, B.; Shen, Y.L.; Wei, D.Z. Enhanced acetoin production by Serratia marcescens H32 with expression of a water-forming NADH oxidase. Bioresour. Technol. 2012, 119, 94–98. [Google Scholar] [CrossRef] [PubMed]
- Yan, X.; Yang, M.; Liu, J.; Gao, R.; Hu, J.; Li, J.; Zhang, L.; Shi, Y.; Guo, H.; Cheng, J.; et al. Discovery and validation of potential bacterial biomarkers for lung cancer. Am. J. Cancer Res. 2015, 5, 3111–3122. [Google Scholar]
- Zhang, W.; Luo, J.; Dong, X.; Zhao, S.; Hao, Y.; Peng, C.; Shi, H.; Zhou, Y.; Shan, L.; Sun, Q.; et al. Salivary microbial dysbiosis is associated with systemic inflammatory markers and predicted oral metabolites in non-small cell lung cancer patients. J. Cancer. 2019, 10, 1651–1662. [Google Scholar] [CrossRef]
- Poli, D.; Goldoni, M.; Corradi, M.; Acampa, O.; Carbognani, P.; Internullo, E.; Casalini, A.; Mutti, A. Determination of aldehydes in exhaled breath of patients with lung cancer by means of on-fiber-derivatisation SPME-GC/MS. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2010, 878, 2643–2651. [Google Scholar] [CrossRef] [PubMed]

| Lung Cancer Patients (n = 291) | Healthy Controls (n = 95) | Χ2/t | p Value | |
|---|---|---|---|---|
| Mean age (years) | 60 (19–89) | 50 (23–81) | 6.917 | 0.000 |
| Proportion (man) | 116 (40%) | 27 (29%) | 4.02 | 0.044 |
| Smoking behavior | 0.793 | 0.370 | ||
| Active | 19 (7%) | 6 (7%) | ||
| Former | 22 (7%) | 4 (4%) | ||
| Never | 250 (86%) | 85 (89%) | ||
| Histologic classification | ||||
| Adenocarcinoma | 251 (86%) | |||
| Squamous carcinoma | 11 (4%) | |||
| Others | 29 (10%) |
| Positive Correlation | Negative Correlation |
|---|---|
| Phylum: Spirochetes, Intertrophic bacteria, Pericarpium, Verruca microflora | Phylum: Proteobacteria |
| Class: Some spirochetes, Mutual nutrient bacteria, Flexible membrane bacteria, Verruca microbe | Class: Saccharibacteria |
| Order: Spirochetes, Ynergistales, Mycoplasmas, Microflora | Order: Saccharibacteria |
| Family: Streptococcus, Spirochetes | Family: Saccharibacteria |
| Genus: Streptococcus, Treponema Pallidum | Genus: Digestive streptococcus, Actinomycetes, Saccharibacteria |
| Species: Streptococcus pharyngitis, Porphyrin monomonas dental medulla, Lactobacillus mucous, Alloscardovia_omnicolens | Species: TM7 animal phylum oral clone DR034 |
| Study | Method | VOCs | Sensitivity | Specificity | References |
|---|---|---|---|---|---|
| Anton et al. | HS-PTV-MS | 2-butanone | 40% | 100% | [23] |
| Hanai et al. | GC-TOFMS | 2-Pentanone | 85% | 70% | [24] |
| G. Song et al. | GC-MS | 3-Hydroxy-2-butanone | 93% | 92.7% | [19] |
| J. Rudnicka et al. | GC-MS | Acetone | 74% | 73% | [20] |
| M. Phillips et al. | GC-MS | Pentane | 89.6% | 82.9% | [21] |
| N. Peled et al. | GNP sensor | Toluene | 70% | 100% | [22] |
| Mingxiao Li et al. | FT-ICR-MS | 2-butanone | 97% | 84% | [32] |
| Ralph J. Knipp | FT-ICR-MS and GC-MS | Hydroxyl acetaldehyde and 3-hydroxy-2-butanone | 94.2 ± 2.5% | - | [33] |
| This study | LC-MS/MS | 3-Hydroxy-2-butanone | 96% | 73% | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sani, S.N.; Zhou, W.; Ismail, B.B.; Zhang, Y.; Chen, Z.; Zhang, B.; Bao, C.; Zhang, H.; Wang, X. LC-MS/MS Based Volatile Organic Compound Biomarkers Analysis for Early Detection of Lung Cancer. Cancers 2023, 15, 1186. https://doi.org/10.3390/cancers15041186
Sani SN, Zhou W, Ismail BB, Zhang Y, Chen Z, Zhang B, Bao C, Zhang H, Wang X. LC-MS/MS Based Volatile Organic Compound Biomarkers Analysis for Early Detection of Lung Cancer. Cancers. 2023; 15(4):1186. https://doi.org/10.3390/cancers15041186
Chicago/Turabian StyleSani, Shuaibu Nazifi, Wei Zhou, Balarabe B. Ismail, Yongkui Zhang, Zhijun Chen, Binjie Zhang, Changqian Bao, Houde Zhang, and Xiaozhi Wang. 2023. "LC-MS/MS Based Volatile Organic Compound Biomarkers Analysis for Early Detection of Lung Cancer" Cancers 15, no. 4: 1186. https://doi.org/10.3390/cancers15041186
APA StyleSani, S. N., Zhou, W., Ismail, B. B., Zhang, Y., Chen, Z., Zhang, B., Bao, C., Zhang, H., & Wang, X. (2023). LC-MS/MS Based Volatile Organic Compound Biomarkers Analysis for Early Detection of Lung Cancer. Cancers, 15(4), 1186. https://doi.org/10.3390/cancers15041186









