Beta Blockers with Statins May Decrease All-Cause Mortality in Patients with Cardiovascular Diseases and Locally Advanced Unresectable Non-Small-Cell Lung Cancer after Chemoradiotherapy
Abstract
Simple Summary
Abstract
1. Introduction
2. Methods
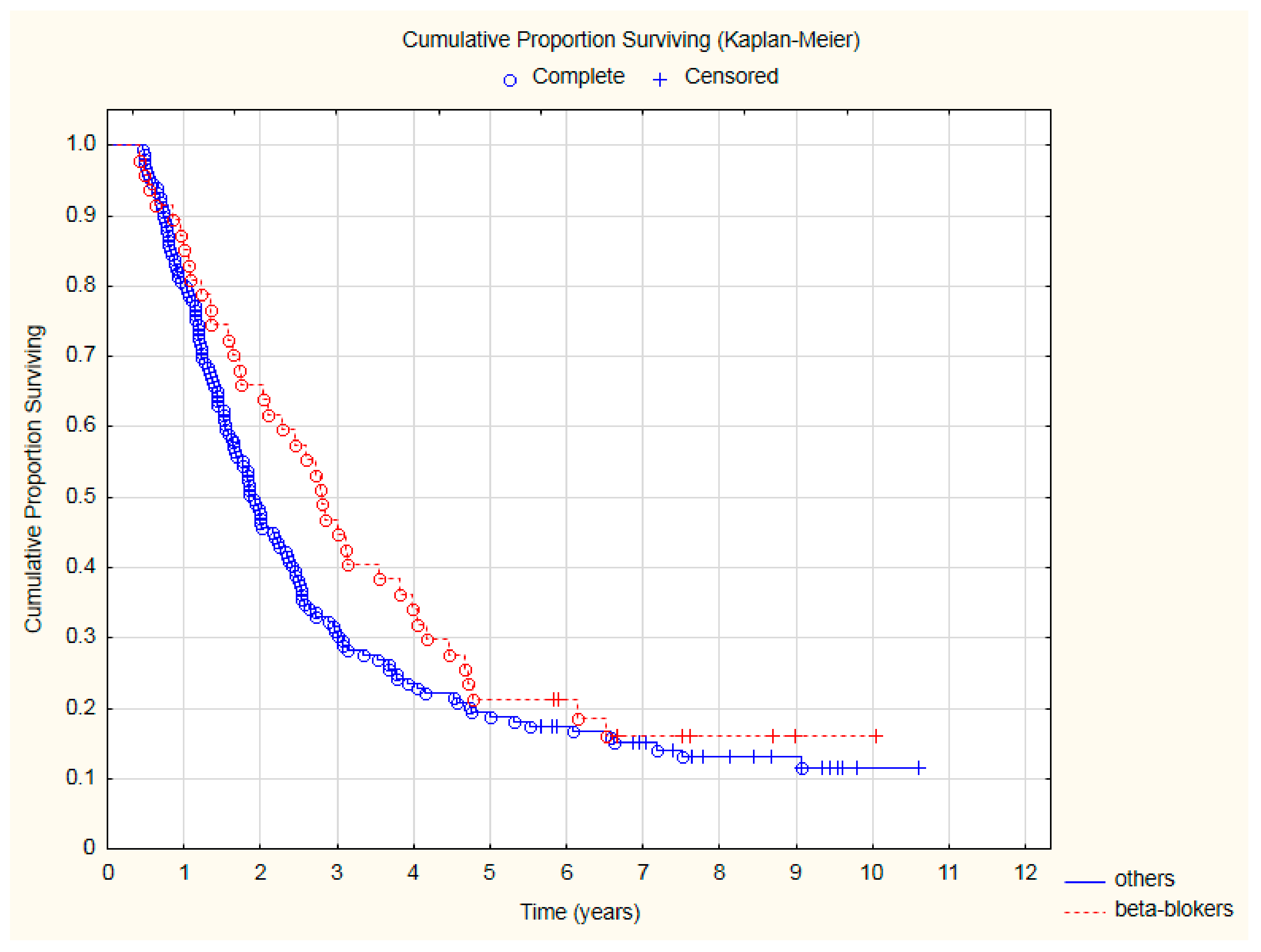
3. Results
- ➢
- arterial hypertension in 79 patients (40.3%),
- ➢
- chronic coronary syndrome in 25 patients (12.8%),
- ➢
- history of arterial thromboembolic events (ATE) in 32 patients (16.3%),
- ➢
- history of venous thromboembolic events (VTE) in 7 patients (3.6%),
- ➢
- atrial fibrillation in 4 patients (2.0%).
4. Discussion
4.1. Why Sequential Treatment?
4.2. Why Beta-Blockers?
4.3. Why Statins?
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- López-Sendón, J.; Álvarez-Ortega, C.; Zamora Auñon, P.; Buño Soto, A.; Lyon, A.R.; Farmakis, D.; Cardinale, D.; Canales Albendea, M.; Feliu Batlle, J.; Rodríguez Rodríguez, I.; et al. Classification, prevalence, and outcomes of anticancer therapy-induced cardiotoxicity: The CARDIOTOX registry. Eur. Heart J. 2020, 41, 1720–1729. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.Y.; Long, J.B.; Hurria, A.; Owusu, C.; Steingart, R.M.; Gross, C.P.; Chen, J. Cardiovascular events, early discontinuation of trastuzumab, and their impact on survival. Breast Cancer Res. Treat. 2014, 146, 411–419. [Google Scholar] [CrossRef] [PubMed]
- Długosz-Danecka, M.; Gruszka, A.M.; Szmit, S.; Olszanecka, A.; Ogórka, T.; Sobociński, M.; Jaroszyński, A.; Krawczyk, K.; Skotnicki, A.B.; Jurczak, W. Primary Cardioprotection Reduces Mortality in Lymphoma Patients with Increased Risk of Anthracycline Cardiotoxicity, Treated by R-CHOP Regimen. Chemotherapy 2018, 63, 238–245. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Eblan, M.J.; Deal, A.M.; Lipner, M.; Zagar, T.M.; Wang, Y.; Mavroidis, P.; Lee, C.B.; Jensen, B.C.; Rosenman, J.G.; et al. Cardiac Toxicity After Radiotherapy for Stage III Non-Small-Cell Lung Cancer: Pooled Analysis of Dose-Escalation Trials Delivering 70 to 90 Gy. J. Clin. Oncol. 2017, 35, 1387–1394. [Google Scholar] [CrossRef]
- Niska, J.R.; Hu, J.; Li, J.; Herman, M.G.; Thorpe, C.S.; Schild, S.E.; Fatyga, M. Using Novel Statistical Techniques to Accurately Determine the Predictive Dose Range in a Study of Overall Survival after Definitive Radiotherapy for Stage III Non-Small Cell Lung Cancer in Association with Heart Dose. J. Cancer Ther. 2021, 12, 505–529. [Google Scholar] [CrossRef]
- Stinchcombe, T.E.; Zhang, Y.; Vokes, E.E.; Schiller, J.H.; Bradley, J.D.; Kelly, K.; Curran, W.J., Jr.; Schild, S.E.; Movsas, B.; Clamon, G.; et al. Pooled Analysis of Individual Patient Data on Concurrent Chemoradiotherapy for Stage III Non-Small-Cell Lung Cancer in Elderly Patients Compared with Younger Patients Who Participated in US National Cancer Institute Cooperative Group Studies. J. Clin. Oncol. 2017, 35, 2885–2892. [Google Scholar] [CrossRef]
- Zaborowska-Szmit, M.; Olszyna-Serementa, M.; Kowalski, D.M.; Szmit, S.; Krzakowski, M. Elderly Patients with Locally Advanced and Unresectable Non-Small-Cell Lung Cancer May Benefit from Sequential Chemoradiotherapy. Cancers 2021, 13, 4534. [Google Scholar] [CrossRef]
- Spigel, D.R.; Faivre-Finn, C.; Gray, J.E.; Vicente, D.; Planchard, D.; Paz-Ares, L.; Vansteenkiste, J.F.; Garassino, M.C.; Hui, R.; Quantin, X.; et al. Five-Year Survival Outcomes from the PACIFIC Trial: Durvalumab After Chemoradiotherapy in Stage III Non-Small-Cell Lung Cancer. J. Clin. Oncol. 2022, 40, 1301–1311. [Google Scholar] [CrossRef]
- Boys, E.; Gao, B.; Hui, R.; da Silva, I.; Hau, E.; Gee, H.; Nagrial, A. Use of durvalumab in stage III non-small-cell lung cancer based on eligibility for the PACIFIC study. Thorac. Cancer 2023. [CrossRef]
- Ramnath, N.; Dilling, T.J.; Harris, L.J.; Kim, A.W.; Michaud, G.C.; Balekian, A.A.; Diekemper, R.; Detterbeck, F.C.; Arenberg, D.A. Treatment of stage III non-small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013, 143 (Suppl. S5), e314S–e340S. [Google Scholar] [CrossRef]
- Eberhardt, W.E.; De Ruysscher, D.; Weder, W.; Le Péchoux, C.; De Leyn, P.; Hoffmann, H.; Westeel, V.; Stahel, R.; Felip, E.; Peters, S.; et al. 2nd ESMO Consensus Conference in Lung Cancer: Locally advanced stage III non-small-cell lung cancer. Ann Oncol. 2015, 26, 1573–1588. [Google Scholar] [CrossRef] [PubMed]
- Park, K.; Vansteenkiste, J.; Lee, K.H.; Pentheroudakis, G.; Zhou, C.; Prabhash, K.; Seto, T.; Voon, P.J.; Tan, D.S.W.; Yang, J.C.H.; et al. Pan-Asian adapted ESMO Clinical Practice Guidelines for the management of patients with locally-advanced unresectable non-small-cell lung cancer: A KSMO-ESMO initiative endorsed by CSCO, ISMPO, JSMO, MOS, SSO and TOS. Ann. Oncol. 2020, 31, 191–201. [Google Scholar] [CrossRef] [PubMed]
- Lyon, A.R.; López-Fernández, T.; Couch, L.S.; Asteggiano, R.; Aznar, M.C.; Bergler-Klein, J.; Boriani, G.; Cardinale, D.; Cordoba, R.; Cosyns, B.; et al. 2022 ESC Guidelines on cardio-oncology developed in collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio-Oncology Society (IC-OS). Eur. Heart J. Cardiovasc. Imaging 2022, 23, e333–e465. [Google Scholar] [CrossRef]
- Zaborowska-Szmit, M.; Krzakowski, M.; Kowalski, D.M.; Szmit, S. Cardiovascular Complications of Systemic Therapy in Non-Small-Cell Lung Cancer. J. Clin. Med. 2020, 9, 1268. [Google Scholar] [CrossRef] [PubMed]
- Curigliano, G.; Cardinale, D.; Suter, T.; Plataniotis, G.; de Azambuja, E.; Sandri, M.T.; Criscitiello, C.; Goldhirsch, A.; Cipolla, C.; Roila, F. Cardiovascular toxicity induced by chemotherapy, targeted agents and radiotherapy: ESMO Clinical Practice Guidelines. Ann. Oncol. 2012, 23 (Suppl. S7), vii155–vii166. [Google Scholar] [CrossRef]
- Curigliano, G.; Lenihan, D.; Fradley, M.; Ganatra, S.; Barac, A.; Blaes, A.; Herrmann, J.; Porter, C.; Lyon, A.R.; Lancellotti, P.; et al. Management of cardiac disease in cancer patients throughout oncological treatment: ESMO consensus recommendations. Ann. Oncol. 2020, 31, 171–190. [Google Scholar] [CrossRef]
- Miller, E.D.; Fisher, J.L.; Haglund, K.E.; Grecula, J.C.; Xu-Welliver, M.; Bertino, E.M.; He, K.; Shields, P.G.; Carbone, D.P.; Williams, T.M.; et al. The Addition of Chemotherapy to Radiation Therapy Improves Survival in Elderly Patients with Stage III Non-Small Cell Lung Cancer. J. Thorac. Oncol. 2018, 13, 426–435. [Google Scholar] [CrossRef]
- Semrau, S.; Klautke, G.; Virchow, J.C.; Kundt, G.; Fietkau, R. Impact of comorbidity and age on the outcome of patients with inoperable NSCLC treated with concurrent chemoradiotherapy. Respir. Med. 2008, 102, 210–218. [Google Scholar] [CrossRef]
- Degens, J.; De Ruysscher, D.; Houben, R.; Kietselaer, B.; Bootsma, G.; Hendriks, L.; Huijbers, E.; Schols, A.; Dingemans, A.C. Are patients with stage III non-small cell lung cancer treated with chemoradiotherapy at risk for cardiac events? Results from a retrospective cohort study. BMJ Open 2020, 10, e036492. [Google Scholar] [CrossRef]
- Dess, R.T.; Sun, Y.; Matuszak, M.M.; Sun, G.; Soni, P.D.; Bazzi, L.; Murthy, V.L.; Hearn, J.W.D.; Kong, F.M.; Kalemkerian, G.P.; et al. Cardiac events after radiation therapy: Combined analysis of prospective multicenter trials for locally advanced non-small-cell lung cancer. J. Clin. Oncol. 2017, 35, 1395–1402. [Google Scholar] [CrossRef]
- Wang, K.; Pearlstein, K.A.; Patchett, N.D.; Deal, A.M.; Mavroidis, P.; Jensen, B.C.; Lipner, M.B.; Zagar, T.M.; Wang, Y.; Lee, C.B.; et al. Heart dosimetric analysis of three types of cardiac toxicity in patients treated on dose-escalation trials for stage III non-small-cell lung cancer. Radiother. Oncol. 2017, 125, 293–300. [Google Scholar] [CrossRef] [PubMed]
- Atkins, K.M.; Rawal, B.; Chaunzwa, T.L.; Lamba, N.; Bitterman, D.S.; Williams, C.L.; Kozono, D.E.; Baldini, E.H.; Chen, A.B.; Nguyen, P.L.; et al. Cardiac radiation dose, cardiac disease, and mortality in patients with lung cancer. J. Am. Coll. Cardiol. 2019, 73, 2976–2987. [Google Scholar] [CrossRef]
- Bradley, J.D.; Paulus, R.; Komaki, R.; Masters, G.; Blumenschein, G.; Schild, S.; Bogart, J.; Hu, C.; Forster, K.; Magliocco, A.; et al. Standard-dose versus high-dose conformal radiotherapy with concurrent and consolidation carboplatin plus paclitaxel with or without cetuximab for patients with stage IIIA or IIIB non-small-cell lung cancer (RTOG 0617): A randomised, two-by-two factorial phase 3 study. Lancet Oncol. 2015, 16, 187–199. [Google Scholar] [PubMed]
- Mitchell, J.D.; Cehic, D.A.; Morgia, M.; Bergom, C.; Toohey, J.; Guerrero, P.A.; Ferencik, M.; Kikuchi, R.; Carver, J.R.; Zaha, V.G.; et al. Cardiovascular Manifestations from Therapeutic Radiation: A Multidisciplinary Expert Consensus Statement From the International Cardio-Oncology Society. JACC CardioOncology 2021, 3, 360–380. [Google Scholar] [CrossRef] [PubMed]
- Ganatra, S.; Chatur, S.; Nohria, A. How to Diagnose and Manage Radiation Cardiotoxicity. JACC CardioOncology 2020, 2, 655–660. [Google Scholar] [CrossRef] [PubMed]
- Mędrek, S.; Szmit, S. Baseline Electrocardiographic and Echocardiographic Assessment May Help Predict Survival in Lung Cancer Patients-A Prospective Cardio-Oncology Study. Cancers 2022, 14, 2010. [Google Scholar] [CrossRef]
- Mędrek, S.; Szmit, S. Are cardiovascular comorbidities always associated with a worse prognosis in patients with lung cancer? Front. Cardiovasc. Med. 2022, 9, 984951. [Google Scholar] [CrossRef]
- He, D.; Hu, J.; Li, Y.; Zeng, X. Preventive use of beta-blockers for anthracycline-induced cardiotoxicity: A network meta-analysis. Front. Cardiovasc. Med. 2022, 9, 968534. [Google Scholar] [CrossRef]
- Zhong, S.; Yu, D.; Zhang, X.; Chen, X.; Yang, S.; Tang, J.; Zhao, J.; Wang, S. β-Blocker use and mortality in cancer patients: Systematic review and meta-analysis of observational studies. Eur. J. Cancer Prev. 2016, 25, 440–448. [Google Scholar] [CrossRef]
- Choi, C.H.; Song, T.; Kim, T.H.; Choi, J.K.; Park, J.Y.; Yoon, A.; Lee, Y.Y.; Kim, T.J.; Bae, D.S.; Lee, J.W.; et al. Meta-analysis of the effects of beta blocker on survival time in cancer patients. J. Cancer Res. Clin. Oncol. 2014, 140, 1179–1188. [Google Scholar] [CrossRef]
- Yap, A.; Lopez-Olivo, M.A.; Dubowitz, J.; Pratt, G.; Hiller, J.; Gottumukkala, V.; Sloan, E.; Riedel, B.; Schier, R. Effect of beta-blockers on cancer recurrence and survival: A meta-analysis of epidemiological and perioperative studies. Br. J. Anaesth. 2018, 121, 45–57. [Google Scholar] [CrossRef]
- Na, Z.; Qiao, X.; Hao, X.; Fan, L.; Xiao, Y.; Shao, Y.; Sun, M.; Feng, Z.; Guo, W.; Li, J.; et al. The effects of beta-blocker use on cancer prognosis: A meta-analysis based on 319,006 patients. OncoTargets Ther. 2018, 11, 4913–4944. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.M.; Liao, Z.X.; Komaki, R.; Welsh, J.W.; O’Reilly, M.S.; Chang, J.Y.; Zhuang, Y.; Levy, L.B.; Lu, C.; Gomez, D.R. Improved survival outcomes with the incidental use of beta-blockers among patients with non-small-cell lung cancer treated with definitive radiation therapy. Ann. Oncol. 2013, 24, 1312–1319. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Liao, Z.; Zhuang, Y.; Liu, Y.; Levy, L.B.; Xu, T.; Yusuf, S.W.; Gomez, D.R. Incidental receipt of cardiac medications and survival outcomes among patients with stage III non-small-cell lung cancer after definitive radiotherapy. Clin. Lung Cancer 2015, 16, 128–136. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.H.; Lee, C.H.; Ko, J.C.; Chang, L.Y.; Lee, M.C.; Zhang, J.F.; Wang, J.Y.; Shih, J.Y.; Yu, C.J. Effect of β-Blocker in Treatment-Naïve Patients with Advanced Lung Adenocarcinoma Receiving First-Generation EGFR-TKIs. Front. Oncol. 2020, 10, 583529. [Google Scholar] [CrossRef] [PubMed]
- Chaudhary, K.R.; Yan, S.X.; Heilbroner, S.P.; Sonett, J.R.; Stoopler, M.B.; Shu, C.; Halmos, B.; Wang, T.J.C.; Hei, T.K.; Cheng, S.K. Effects of β-Adrenergic Antagonists on Chemoradiation Therapy for Locally Advanced Non-Small Cell Lung Cancer. J. Clin. Med. 2019, 8, 575. [Google Scholar] [CrossRef]
- Oh, M.S.; Guzner, A.; Wainwright, D.A.; Mohindra, N.A.; Chae, Y.K.; Behdad, A.; Villaflor, V.M. The Impact of Beta Blockers on Survival Outcomes in Patients with Non-small-cell Lung Cancer Treated with Immune Checkpoint Inhibitors. Clin. Lung Cancer 2021, 22, e57–e62. [Google Scholar] [CrossRef]
- Nissen, M.D.; Sloan, E.K.; Mattarollo, S.R. β-Adrenergic Signaling Impairs Antitumor CD8+ T-cell Responses to B-cell Lymphoma Immunotherapy. Cancer Immunol. Res. 2018, 6, 98–109. [Google Scholar] [CrossRef]
- Amin, F.; Fathi, F.; Reiner, Ž.; Banach, M.; Sahebkar, A. The role of statins in lung cancer. Arch. Med. Sci. 2021, 18, 141–152. [Google Scholar] [CrossRef]
- Cardwell, C.R.; Mc Menamin, Ú.; Hughes, C.M.; Murray, L.J. Statin use and survival from lung cancer: A population-based cohort study. Cancer Epidemiol. Biomarkers Prev. 2015, 24, 833–841. [Google Scholar] [CrossRef]
- Huang, W.Y.; Li, C.H.; Lin, C.L.; Liang, J.A. Long-term statin use in patients with lung cancer and dyslipidemia reduces the risk of death. Oncotarget 2016, 7, 42208–42215. [Google Scholar] [CrossRef] [PubMed]
- Hung, M.S.; Chen, I.C.; Lee, C.P.; Huang, R.J.; Chen, P.C.; Tsai, Y.H.; Yang, Y.H. Statin improves survival in patients with EGFR-TKI lung cancer: A nationwide population-based study. PLoS ONE 2017, 12, e0171137. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.J.; Ezer, N.; Sigel, K.; Mhango, G.; Wisnivesky, J.P. The effect of statins on survival in patients with stage IV lung cancer. Lung Cancer 2016, 99, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Li, X.; Zhang, R.; Xia, Y.; Shao, Z.; Mei, Z. Effects of statin exposure and lung cancer survival: A meta-analysis of observational studies. Pharmacol. Res. 2019, 141, 357–365. [Google Scholar] [CrossRef] [PubMed]
- Xia, D.K.; Hu, Z.G.; Tian, Y.F.; Zeng, F.J. Statin use and prognosis of lung cancer: A systematic review and meta-analysis of observational studies and randomized controlled trials. Drug Des. Devel. Ther. 2019, 13, 405–422. [Google Scholar] [CrossRef]
- Atkins, K.M.; Bitterman, D.S.; Chaunzwa, T.L.; Williams, C.L.; Rahman, R.; Kozono, D.E.; Baldini, E.H.; Aerts, H.J.W.L.; Tamarappoo, B.K.; Hoffmann, U.; et al. Statin Use, Heart Radiation Dose, and Survival in Locally Advanced Lung Cancer. Pract. Radiat. Oncol. 2021, 11, e459–e467. [Google Scholar] [CrossRef]
- Iarrobino, N.A.; Gill, B.S.; Bernard, M.; Klement, R.J.; Werner-Wasik, M.; Champ, C.E. The Impact of Serum Glucose, Anti-Diabetic Agents, and Statin Usage in Non-small Cell Lung Cancer Patients Treated with Definitive Chemoradiation. Front. Oncol. 2018, 8, 281. [Google Scholar] [CrossRef]
- Lam, V.K.; Bentzen, S.M.; Mohindra, P.; Nichols, E.M.; Bhooshan, N.; Vyfhuis, M.; Scilla, K.A.; Feigenberg, S.J.; Edelman, M.J.; Feliciano, J.L. Obesity is associated with long-term improved survival in definitively treated locally advanced non-small cell lung cancer (NSCLC). Lung Cancer 2017, 104, 52–57. [Google Scholar] [CrossRef]
- Omori, M.; Okuma, Y.; Hakozaki, T.; Hosomi, Y. Statins improve survival in patients previously treated with nivolumab for advanced non-small cell lung cancer: An observational study. Mol. Clin. Oncol. 2019, 10, 137–143. [Google Scholar] [CrossRef]
- De Boer, R.A.; Aboumsallem, J.P.; Bracun, V.; Leedy, D.; Cheng, R.; Patel, S.; Rayan, D.; Zaharova, S.; Rymer, J.; Kwan, J.M.; et al. A new classification of cardio-oncology syndromes. Cardiooncology 2021, 7, 24. [Google Scholar] [CrossRef]
- Koelwyn, G.J.; Aboumsallem, J.P.; Moore, K.J.; de Boer, R.A. Reverse cardio-oncology: Exploring the effects of cardiovascular disease on cancer pathogenesis. J. Mol. Cell. Cardiol. 2022, 163, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Mędrek, S.; Szmit, S. Echocardiography-Assessed Changes of Left and Right Ventricular Cardiac Function May Correlate with Progression of Advanced Lung Cancer-A Generating Hypothesis Study. Cancers 2022, 14, 4770. [Google Scholar] [CrossRef] [PubMed]
- Wilk, M.; Waśko-Grabowska, A.; Skoneczna, I.; Szmit, S. Angiotensin System Inhibitors May Improve Outcomes of Patients with Castration-Resistant Prostate Cancer During Abiraterone Acetate Treatment-A Cardio-Oncology Study. Front. Oncol. 2021, 11, 664741. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.; Tai, Z.; Chen, Z.; Zhu, Q.; Bao, L. Clinical applicability of renin-angiotensin system inhibitors in cancer treatment. Am. J. Cancer Res. 2021, 11, 318–336. [Google Scholar]
- Santoro, C.; Capone, V.; Canonico, M.E.; Gargiulo, G.; Esposito, R.; Sanna, G.D.; Parodi, G.; Esposito, G. Single, Dual, and Triple Antithrombotic Therapy in Cancer Patients with Coronary Artery Disease: Searching for Evidence and Personalized Approaches. Semin. Thromb. Hemost. 2021, 47, 950–961. [Google Scholar] [CrossRef] [PubMed]




| All 196 Patients | Presence of CVD | ||||
|---|---|---|---|---|---|
| 101 Patients with CVD | 95 Patients without CVD | Chi-Square p-Value | |||
| Age > 65 years | 52 | 38 (37.62%) | 14 (14.74%) | 0.0003 | |
| Clinical stage IIIA | 94 | 52 (51.49%) | 42 (44.21%) | 0.31 | |
| Weight loss ≥ 10% | 24 | 10 (9.9%) | 14 (14.74%) | 0.3 | |
| Baseline performance status KPS below 100 | 129 | 70 (69.31%) | 59 (62.11%) | 0.29 | |
| Deterioration of performance status at least by 10 points in KPS during CRT | 53 | 23 (22.77%) | 30 (31.58%) | 0.17 | |
| Chemotherapy without cisplatin | 21 | 17 (16.83%) | 4 (4.21%) | 0.009 | |
| Longer time between the end of chemotherapy and start of radiotherapy (defined as >42 days/6 weeks) | 45 | 26 (25.74%) | 19 (20%) | 0.34 | |
| Complications all grades | Pneumotoxicity | 24 | 11 (10.89%) | 13 (13.68%) | 0.55 |
| Nephrotoxicity | 22 | 16 (15.84%) | 6 (6.32%) | 0.03 | |
| Cardiac events | 15 | 12 (11.88%) | 3 (3.16%) | 0.04 | |
| Complications grade 3/4 according to CTCAE | Febrile neutropenia | 8 | 5 (4.95%) | 3 (3.16%) | 0.79 |
| Acute kidney injury | 9 | 7 (6.93%) | 2 (2.11%) | 0.2 | |
| Pneumotoxocity | 5 | 3 (2.97%) | 2 (2.11%) | 0.94 | |
| Cardiac events | 5 | 5 (4.95%) | 0 | 0.08 | |
| Response to CRT according to RECIST | CR | 15 | 8 (7.92%) | 7(7.37%) | 0.82 |
| PR | 123 | 66 (65.35%) | 57 (60%) | ||
| SD | 44 | 20 (19.8%) | 24 (25.26%) | ||
| PD | 14 | 7 (6.93%) | 7 (7.37%) | ||
| Type of cancer disease progression | Local progression | 87 | 48 (47.52%) | 39 (41.05%) | 0.36 |
| Distant metastases | 81 | 38 (37.62%) | 43 (45.26%) | 0.28 | |
| Subsequent chemotherapy | 93 | 47 (46.53%) | 46 (48.42%) | 0.79 | |
| Secondary cancer disease | 9 | 6 (5.94%) | 3 (3.16%) | 0.56 | |
| Without BB (n = 149) | BB (n = 47) | p-Value | ||
|---|---|---|---|---|
| Age > 65 years | 35(23.49%) | 17(36.17%) | 0.09 | |
| Clinical stage IIIA | 68(45.64%) | 26(55.32%) | 0.25 | |
| Weight loss ≥ 10% | 19(12.75%) | 5(10.64%) | 0.70 | |
| Baseline performance status KPS = 100 | 57(38.26%) | 10(21.28%) | 0.03 | |
| Deterioration of performance status at least by 10 points in KPS during CRT | 46(30.87%) | 7(14.89%) | 0.03 | |
| Chemotherapy without cisplatin | 15(10.07%) | 6(12.77%) | 0.60 | |
| Longer time between the end of chemotherapy and start of radiotherapy (defined as >42 days/6 weeks) | 29(19.46%) | 16(34.04%) | 0.04 | |
| Complications all grades | Pneumotoxicity | 21(14.09%) | 3(6.38%) | 0.16 |
| Nephrotoxicity | 15(10.07%) | 7(14.89%) | 0.36 | |
| Cardiac events | 11(7.38%) | 4(8.51%) | 0.80 | |
| Complications grade 3/4 according to CTCAE | Febrile neutropenia | 7(4.70%) | 1(2.13%) | 0.44 |
| Acute kidney injury | 6(4.03%) | 3(6.38%) | 0.50 | |
| Pneumotoxocity | 4(2.68%) | 1(2.13%) | 0.83 | |
| Cardiac events | 3(2.01%) | 2(4.26%) | 0.40 | |
| Response to CRT according to RECIST | CR | 13(8.72%) | 2(4.26%) | 0.31 |
| PR | 92(61.74%) | 31(65.96%) | 0.60 | |
| SD | 32(21.48%) | 12(25.53%) | 0.56 | |
| PD | 12(8.05%) | 2(4.26%) | 0.38 | |
| Type of cancer disease progression | Local progression | 66(44.30%) | 21(44.68%) | 0.96 |
| Distant metastases | 60(40.27%) | 21(44.68%) | 0.59 | |
| Subsequent chemotherapy | 70(46.98%) | 23(48.94%) | 0.81 | |
| Secondary cancer disease | 7(4.70%) | 2(4.26%) | 0.90 | |
| Drugs | All-Cause Mortality | ||||
|---|---|---|---|---|---|
| 1 Year | 2 Year | 3 Year | 4 Year | 5 Year | |
| 36(18.37%) | 96(48.98%) | 129(65.82%) | 145(73.98%) | 157(80.1%) | |
| Beta-blocker (n = 47) | HR = 0.75 95%CI: 0.33–1.71 p = 0.492 | HR = 0.57 95%CI:0.33–0.97 p = 0.039 | HR = 0.63 95%CI:0.41–0.98 p = 0.038 | HR = 0.70 95%CI:0.47–1.04 p = 0.074 | HR = 0.79 95%CI: 0.54–1.14 p = 0.201 |
| Statin (n = 26) | HR = 0.60 95%CI:0.18–1.95 p = 0.392 | HR = 0.54 95%CI:0.26–1.12 p = 0.098 | HR = 0.54 95%CI:0.30–0.98 p = 0.041 | HR = 0.67 95%CI:0.41–1.12 p = 0.126 | HR = 0.78 95%CI:0.49–1.24 p = 0.296 |
| Beta-blocker + statin (n = 16) | HR = 0.67 95%CI:0.16–2.81 p = 0.587 | HR = 0.31 95%CI:0.10–0.98 p = 0.047 | HR = 0.33 95%CI:0.13–0.81 p = 0.015 | HR = 0.45 95%CI:0.22–0.91 p = 0.027 | HR = 0.56 95%CI:0.30–1.04 p = 0.067 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zaborowska-Szmit, M.; Szmit, S.; Olszyna-Serementa, M.; Badurak, P.; Zajda, K.; Janowicz-Żebrowska, A.; Piórek, A.; Knetki-Wróblewska, M.; Jaśkiewicz, P.; Płużański, A.; et al. Beta Blockers with Statins May Decrease All-Cause Mortality in Patients with Cardiovascular Diseases and Locally Advanced Unresectable Non-Small-Cell Lung Cancer after Chemoradiotherapy. Cancers 2023, 15, 1277. https://doi.org/10.3390/cancers15041277
Zaborowska-Szmit M, Szmit S, Olszyna-Serementa M, Badurak P, Zajda K, Janowicz-Żebrowska A, Piórek A, Knetki-Wróblewska M, Jaśkiewicz P, Płużański A, et al. Beta Blockers with Statins May Decrease All-Cause Mortality in Patients with Cardiovascular Diseases and Locally Advanced Unresectable Non-Small-Cell Lung Cancer after Chemoradiotherapy. Cancers. 2023; 15(4):1277. https://doi.org/10.3390/cancers15041277
Chicago/Turabian StyleZaborowska-Szmit, Magdalena, Sebastian Szmit, Marta Olszyna-Serementa, Paweł Badurak, Katarzyna Zajda, Anna Janowicz-Żebrowska, Aleksandra Piórek, Magdalena Knetki-Wróblewska, Piotr Jaśkiewicz, Adam Płużański, and et al. 2023. "Beta Blockers with Statins May Decrease All-Cause Mortality in Patients with Cardiovascular Diseases and Locally Advanced Unresectable Non-Small-Cell Lung Cancer after Chemoradiotherapy" Cancers 15, no. 4: 1277. https://doi.org/10.3390/cancers15041277
APA StyleZaborowska-Szmit, M., Szmit, S., Olszyna-Serementa, M., Badurak, P., Zajda, K., Janowicz-Żebrowska, A., Piórek, A., Knetki-Wróblewska, M., Jaśkiewicz, P., Płużański, A., Krzakowski, M., & Kowalski, D. M. (2023). Beta Blockers with Statins May Decrease All-Cause Mortality in Patients with Cardiovascular Diseases and Locally Advanced Unresectable Non-Small-Cell Lung Cancer after Chemoradiotherapy. Cancers, 15(4), 1277. https://doi.org/10.3390/cancers15041277






