Early Disturbance of Lymphatic Transport as a Risk Factor for the Development of Breast-Cancer-Related Lymphedema
Abstract
Simple Summary
Abstract
1. Introduction
2. Methodology
2.1. Trial Design
2.2. Participants
2.3. Data Collection
2.4. Development of Clinical BCRL
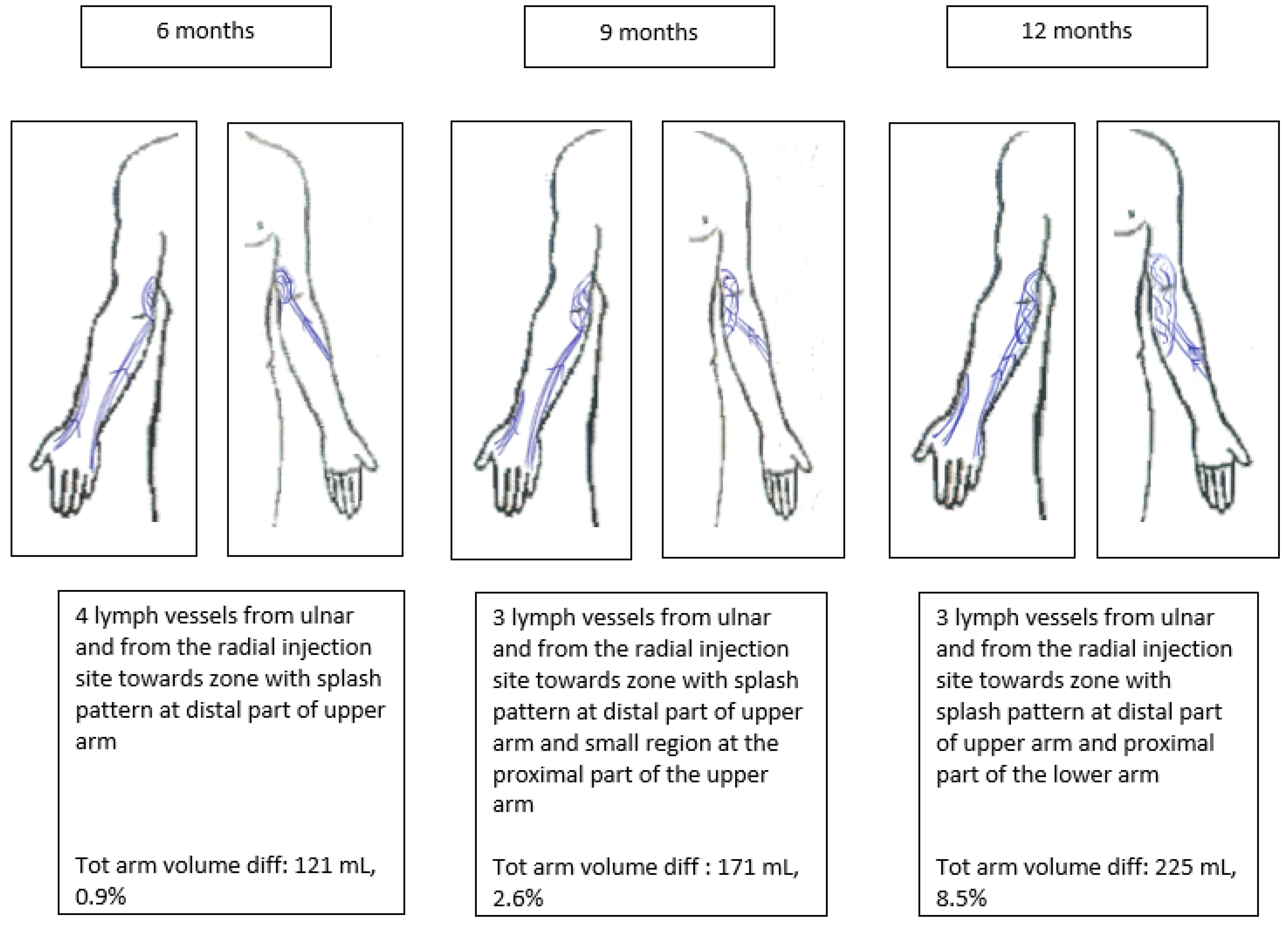
2.5. Lymphatic-Transport-Related Variable
2.6. Demographic and General Health-Related Variables
2.7. Breast-Cancer- and Treatment-Related Variables
2.8. Statistical Methods
3. Results
3.1. Description of Participants
3.2. Lymphatic-Transport-Related Variable
3.3. Demographic and General Health-Related Variables
3.4. Breast-Cancer- and Treatment-Related Variables
3.5. Multivariate Analysis
4. Discussion
4.1. Lymphatic-Transport-Related Variable Associated with BCRL
4.2. Demographic and General Health-Related Variables Associated with Clinical BCRL
4.3. Breast-Cancer- and Treatment-Related Variables Associated with Clinical BCRL
4.4. Strenghts and Limitations
4.5. Clinical Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- The diagnosis and treatment of peripheral lymphedema: 2020 Consensus Document of the International Society of Lymphology. Lymphology 2020, 53, 3–19.
- DiSipio, T.; Rye, S.; Newman, B.; Hayes, S. Incidence of unilateral arm lymphoedema after breast cancer: A systematic review and meta-analysis. Lancet Oncol. 2013, 14, 500–515. [Google Scholar] [CrossRef] [PubMed]
- Markkula, S.P.; Leung, N.; Allen, V.B.; Furniss, D. Surgical interventions for the prevention or treatment of lymphoedema after breast cancer treatment. Cochrane Database Syst. Rev. 2019, 2019, CD011433. [Google Scholar] [CrossRef] [PubMed]
- Ciudad, P.; Escandón, J.M.; Bustos, V.P.; Manrique, O.J.; Kaciulyte, J. Primary Prevention of Cancer-Related Lymphedema Using Preventive Lymphatic Surgery: Systematic Review and Meta-analysis. Indian J. Plast. Surg. 2022, 55, 18–25. [Google Scholar] [CrossRef]
- Devoogdt, N.; Christiaens, M.R.; Geraerts, I.; Truijen, S.; Smeets, A.; Leunen, K.; Neven, P.; Van Kampen, M. Abstract S5-3: Is Manual Lymph Drainage Applied after Axillary Lymph Node Dissection for Breast Cancer Effective To Prevent Arm Lymphoedema? A Randomised Controlled Trial. Cancer Res. 2010, 70, S5-3. [Google Scholar] [CrossRef]
- Shah, C.; Arthur, D.W.; Wazer, D.; Khan, A.; Ridner, S.; Vicini, F. The impact of early detection and intervention of breast cancer-related lymphedema: A systematic review. Cancer Med. 2016, 5, 1154–1162. [Google Scholar] [CrossRef] [PubMed]
- Gencay Can, A.; Eksioglu, E.; Cakci, F.A. Early Detection and Treatment of Subclinical Lymphedema in Patients with Breast Cancer. Lymphat. Res. Biol. 2019, 17, 368–373. [Google Scholar] [CrossRef]
- Stout, N.L.; Pfalzer, L.; Levy, E.; McGarvey, C.; Gerber, L.; Springer, B.; Soballe, P. Five year preliminary outcomes of a prospective surveillance model to reduce upper extremity morbidity related to breast cancer treatment. Cancer Res. 2011, 71, P4-12. [Google Scholar] [CrossRef]
- Soran, A.; Ozmen, T.; McGuire, K.P.; Diego, E.J.; McAuliffe, P.F.; Bonaventura, M.; Ahrendt, G.M.; Degore, L.; Johnson, R. The importance of detection of subclinical lymphedema for the prevention of breast cancer-related clinical lymphedema after axillary lymph node dissection; A prospective observational study. Lymphat. Res. Biol. 2014, 12, 289–294. [Google Scholar] [CrossRef]
- De Vrieze, T.; Gebruers, N.; Nevelsteen, I.; De Groef, A.; Tjalma, W.A.A.; Thomis, S.; Dams, L.; Van der Gucht, E.; Penen, F.; Devoogdt, N. Reliability of the MoistureMeterD Compact Device and the Pitting Test to Evaluate Local Tissue Water in Subjects with Breast Cancer-Related Lymphedema. Lymphat. Res. Biol. 2020, 18, 116–128. [Google Scholar] [CrossRef]
- Yamamoto, T.; Yamamoto, N.; Doi, K.; Oshima, A.; Yoshimatsu, H.; Todokoro, T.; Ogata, F.; Mihara, M.; Narushima, M.; Iida, T.; et al. Indocyanine green-enhanced lymphography for upper extremity lymphedema: A novel severity staging system using dermal backflow patterns. Plast. Reconstr. Surg. 2011, 128, 941–947. [Google Scholar] [CrossRef] [PubMed]
- Akita, S.; Nakamura, R.; Yamamoto, N.; Tokumoto, H.; Ishigaki, T.; Yamaji, Y.; Sasahara, Y.; Kubota, Y.; Mitsukawa, N.; Satoh, K. Early Detection of Lymphatic Disorder and Treatment for Lymphedema following Breast Cancer. Plast. Reconstr. Surg. 2016, 138, 192e–202e. [Google Scholar] [CrossRef]
- Ahmed. Randomized controlled trial of weight training and lymphedema in breast cancer survivors (vol 24, pg 2765, 2006). J. Clin. Oncol. 2006, 24, 3716. [Google Scholar] [CrossRef]
- Meeske, K.A.; Sullivan-Halley, J.; Smith, A.W.; McTiernan, A.; Baumgartner, K.B.; Harlan, L.C.; Bernstein, L. Risk factors for arm lymphedema following breast cancer diagnosis in Black women and White women. Breast Cancer Res. Treat. 2009, 113, 383–391. [Google Scholar] [CrossRef] [PubMed]
- Shahpar, H.; Atieh, A.; Maryam, A.; Fatemeh, H.S.; Massoome, N.; Mandana, E.; Masud, Y.; Hamid Reza, M.; Mohammad Esmaeil, A. Risk factors of lymph edema in breast cancer patients. Int. J. Breast Cancer 2013, 2013, 641818. [Google Scholar] [CrossRef]
- Gillespie, T.C.; Sayegh, H.E.; Brunelle, C.L.; Daniell, K.M.; Taghian, A.G. Breast cancer-related lymphedema: Risk factors, precautionary measures, and treatments. Gland Surg. 2018, 7, 379–403. [Google Scholar] [CrossRef]
- Das, N.; Baumgartner, R.; Riley, E.; Pinkston, C.; Yang, D.; Baumgartner, K. Treatment-related risk factors for arm lymphedema among long-term breast cancer survivors. J. Cancer Surviv. 2015, 9, 422–430. [Google Scholar] [CrossRef]
- Lopez Penha, T.R.; Van Roozendaal, L.M.; Smidt, M.L.; Boersma, L.J.; Von Meyenfeldt, M.F.; Voogd, A.C.; Heuts, E.M. The changing role of axillary treatment in breast cancer: Who will remain at risk for developing arm morbidity in the future? Breast 2015, 24, 543–547. [Google Scholar] [CrossRef]
- Tsai, R.J.; Dennis, L.K.; Lynch, C.F.; Snetselaar, L.G.; Zamba, G.K.D.; Scott-Conner, C. The risk of developing arm lymphedema among breast cancer survivors: A meta-analysis of treatment factors. Ann. Surg. Oncol. 2009, 16, 1959–1972. [Google Scholar] [CrossRef]
- Thomis, S.; Devoogdt, N.; Bechter-Hugl, B.; Nevelsteen, I.; Neven, P.; Fourneau, I. Impact of a compression garment, on top of the usual care, in patients with breast cancer with early disturbance of the lymphatic transport: Protocol of a randomised controlled trial. BMJ Open 2020, 10, e042018. [Google Scholar] [CrossRef]
- Devoogdt, N.; Lemkens, H.; Geraerts, I.; Van Nuland, J.; Flour, M.; Coremans, T.; Christiaens, M.R.; Van Kampen, M. A new device to measure upper limb circumferences: Validity and reliability. Int. Angiol. 2010, 29, 401–407. [Google Scholar] [PubMed]
- Taylor, R.; Jayasinghe, U.W.; Koelmeyer, L.; Ung, O.; Boyages, J. Reliability and validity of arm volume measurements for assessment of lymphedema. Phys. Ther. 2006, 86, 205–214. [Google Scholar] [CrossRef]
- Damstra, R.J.; Glazenburg, E.J.; Hop, W.C.J. Validation of the inverse water volumetry method: A new gold standard for arm volume measurements. Breast Cancer Res. Treat. 2006, 99, 267–273. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed]
- Thomis, S.; Devoogdt, N.; De Vrieze, T.; Bechter-Hugl, B.; Heroes, A.K.; Fourneau, I. Relation Between Early Disturbance of lymphatic transport Visualized With Lymphofluoroscopy and Other Clinical Assessment Methods in Patients With Breast Cancer. Clin. Breast Cancer 2022, 22, e37–e47. [Google Scholar] [CrossRef]
- Jørgensen, M.G.; Toyserkani, N.M.; Hansen, F.C.G.; Thomsen, J.B.; Sørensen, J.A. Prospective Validation of Indocyanine Green Lymphangiography Staging of Breast Cancer-Related Lymphedema. Cancers 2021, 13, 1540. [Google Scholar] [CrossRef]
- Akita, S.; Mitsukawa, N.; Rikihisa, N.; Kubota, Y.; Omori, N.; Mitsuhashi, A.; Tate, S.; Shozu, M.; Satoh, K. Early diagnosis and risk factors for lymphedema following lymph node dissection for gynecologic cancer. Plast. Reconstr. Surg. 2013, 131, 283–290. [Google Scholar] [CrossRef]
- Liu, M.; Liu, S.; Zhao, Q.; Cui, Y.; Chen, J.; Wang, S. Using the Indocyanine Green (ICG) Lymphography to Screen Breast Cancer Patients at High Risk for Lymphedema. Diagnostics 2022, 12, 983. [Google Scholar] [CrossRef] [PubMed]
- Aldrich, M.B.; Rasmussen, J.C.; DeSnyder, S.M.; Woodward, W.A.; Chan, W.; Sevick-Muraca, E.M.; Mittendorf, E.A.; Smith, B.D.; Stauder, M.C.; Strom, E.A.; et al. Prediction of breast cancer-related lymphedema by dermal backflow detected with near-infrared fluorescence lymphatic imaging. Breast Cancer Res. Treat. 2022, 195, 33–41. [Google Scholar] [CrossRef]
- Mihara, M.; Hara, H.; Araki, J.; Kikuchi, K.; Narushima, M.; Yamamoto, T.; Iida, T.; Yoshimatsu, H.; Murai, N.; Mitsui, K.; et al. Indocyanine Green (ICG) lymphography is superior to lymphoscintigraphy for diagnostic imaging of early lymphedema of the upper limbs. PLoS ONE 2012, 7, e38182. [Google Scholar] [CrossRef]
- Akita, S.; Mitsukawa, N.; Kazama, T.; Kuriyama, M.; Kubota, Y.; Omori, N.; Koizumi, T.; Kosaka, K.; Uno, T.; Satoh, K. Comparison of lymphoscintigraphy and indocyanine green lymphography for the diagnosis of extremity lymphoedema. J. Plast. Reconstr. Aesthetic Surg. JPRAS 2013, 66, 792–798. [Google Scholar] [CrossRef] [PubMed]
- Dean, L.T.; Kumar, A.; Kim, T.; Herling, M.; Brown, J.C.; Zhang, Z.; Evangelisti, M.; Hackley, R.; Kim, J.; Cheville, A.; et al. Race or Resource? BMI, Race, and Other Social Factors as Risk Factors for Interlimb Differences among Overweight Breast Cancer Survivors with Lymphedema. J. Obes. 2016, 2016, 8241710. [Google Scholar] [CrossRef] [PubMed]
- Swaroop, M.N.; Ferguson, C.M.; Horick, N.K.; Skolny, M.N.; Miller, C.L.; Jammallo, L.S.; Brunelle, C.L.; O’Toole, J.A.; Isakoff, S.J.; Specht, M.C.; et al. Impact of adjuvant taxane-based chemotherapy on the development of breast cancer-related lymphedema: Results from a large prospective cohort. Breast Cancer Res. Treat. 2015, 151, 393–403. [Google Scholar] [CrossRef]
- Ugur, S.; Arici, C.; Yaprak, M.; Mesci, A.; Arici, G.A.; Dolay, K.; Ozmen, V. Risk factors of breast cancer-related lymphedema. Lymphat. Res. Biol. 2013, 11, 72–75. [Google Scholar] [CrossRef] [PubMed]
- Showalter, S.L.; Brown, J.C.; Cheville, A.L.; Fisher, C.S.; Sataloff, D.; Schmitz, K.H. Lifestyle risk factors associated with arm swelling among women with breast cancer. Ann. Surg. Oncol. 2013, 20, 842–849. [Google Scholar] [CrossRef]
- Ozaslan, C.; Kuru, B. Lymphedema after treatment of breast cancer. Am. J. Surg. 2004, 187, 69–72. [Google Scholar] [CrossRef] [PubMed]
- Haddad, P.; Farzin, M.; Amouzegar-Hashemi, F.; Kalaghchi, B.; Babazadeh, S.; Mirzaei, H.R.; Mousavizadeh, A.; Harirchi, I.; Rafat, J. A multicentre cross-sectional study of arm lymphedema four or more years after breast cancer treatment in Iranian patients. Breast Cancer 2010, 17, 281–285. [Google Scholar] [CrossRef] [PubMed]
- Lane, K.N.; Dolan, L.B.; Worsley, D.; McKenzie, D.C. Upper extremity lymphatic function at rest and during exercise in breast cancer survivors with and without lymphedema compared with healthy controls. J. Appl. Physiol. 2007, 103, 917–925. [Google Scholar] [CrossRef] [PubMed]
- Baumann, F.T.; Reike, A.; Hallek, M.; Wiskemann, J.; Reimer, V. Does Exercise Have a Preventive Effect on Secondary Lymphedema in Breast Cancer Patients Following Local Treatment?—A Systematic Review. Breast Care 2018, 13, 380–385. [Google Scholar] [CrossRef]
- Kwan, M.L.; Darbinian, J.; Schmitz, K.H.; Citron, R.; Partee, P.; Kutner, S.E.; Kushi, L.H. Risk factors for lymphedema in a prospective breast cancer survivorship study: The Pathways Study. Arch. Surg. 2010, 145, 1055–1063. [Google Scholar] [CrossRef]
- Paskett, E.D.; Herndon, J.E., 2nd; Day, J.M.; Stark, N.N.; Winer, E.P.; Grubbs, S.S.; Pavy, M.D.; Shapiro, C.L.; List, M.A.; Hensley, M.L.; et al. Applying a conceptual model for examining health-related quality of life in long-term breast cancer survivors: CALGB study 79804. Psychooncology 2008, 17, 1108–1120. [Google Scholar] [CrossRef] [PubMed]
- Kilbreath, S.L.; Refshauge, K.M.; Ward, L.C.; Kastanias, K.; Yee, J.; Koelmeyer, L.A.; Beith, J.M.; French, J.R.; Ung, O.A.; Black, D. Factors affecting the preoperative and postoperative extracellular fluid in the arm on the side of breast cancer: A cohort study. Lymphat. Res. Biol. 2013, 11, 66–71. [Google Scholar] [CrossRef]
- Khanna, S.; Gupta, A.K.; Cherian, A.J.; Yadav, B.; Jacob, P.M. Post Mastectomy Lymphedemaa Prospective Study of Incidence and Risk Factors. Indian J. Surg. 2019, 81, 16–22. [Google Scholar] [CrossRef]
- Monleon, S.; Murta-Nascimento, C.; Bascuas, I.; Macià, F.; Duarte, E.; Belmonte, R. Lymphedema predictor factors after breast cancer surgery: A survival analysis. Lymphat. Res. Biol. 2015, 13, 268–274. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, C.M.; Swaroop, M.N.; Horick, N.; Skolny, M.N.; Miller, C.L.; Jammallo, L.S.; Brunelle, C.; O’Toole, J.A.; Salama, L.; Specht, M.C.; et al. Impact of ipsilateral blood draws, injections, blood pressure measurements, and air travel on the risk of lymphedema for patients treated for breast cancer. J. Clin. Oncol. 2016, 34, 691–698. [Google Scholar] [CrossRef] [PubMed]
- Ben Salah, H.; Bahri, M.; Jbali, B.; Guermazi, M.; Frikha, M.; Daoud, J. Upper limb lymphedema after breast cancer treatment. Cancer/Radiotherapie 2012, 16, 123–127. [Google Scholar] [CrossRef] [PubMed]
- De Luca, A.; Tripodi, D.; Frusone, F.; Leonardi, B.; Cerbelli, B.; Botticelli, A.; Vergine, M.; D’Andrea, V.; Pironi, D.; Sorrenti, S.; et al. Retrospective Evaluation of the Effectiveness of a Synthetic Glue and a Fibrin-Based Sealant for the Prevention of Seroma Following Axillary Dissection in Breast Cancer Patients. Front. Oncol. 2020, 10, 1061. [Google Scholar] [CrossRef]
- Kwan, W.; Jackson, J.; Weir, L.M.; Dingee, C.; McGregor, G.; Olivotto, I.A. Chronic arm morbidity after curative breast cancer treatment: Prevalence and impact on quality of life. J. Clin. Oncol. 2002, 20, 4242–4248. [Google Scholar] [CrossRef]
- Ashikaga, T.; Krag, D.N.; Land, S.R.; Julian, T.B.; Anderson, S.J.; Brown, A.M.; Skelly, J.M.; Harlow, S.P.; Weaver, D.L.; Mamounas, E.P.; et al. Morbidity results from the NSABP B-32 trial comparing sentinel lymph node dissection versus axillary dissection. J. Surg. Oncol. 2010, 102, 111–118. [Google Scholar] [CrossRef]
- Donker, M.; van Tienhoven, G.; Straver, M.E.; Meijnen, P.; van de Velde, C.J.H.; Mansel, R.E.; Cataliotti, L.; Westenberg, A.H.; Klinkenbijl, J.H.G.; Orzalesi, L.; et al. Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer (EORTC 10981-22023 AMAROS): A randomised, multicentre, open-label, phase 3 non-inferiority trial. Lancet Oncol. 2014, 15, 1303–1310. [Google Scholar] [CrossRef]
- Fontaine, C.; Adriaenssens, N.; Vanparijs, H.; Voordeckers, M.; Jean-François, F.; De Coster, L.; Schallier, D.; Vanhoeij, M.; Verfaillie, G.; Lamote, J.; et al. A prospective analysis of the incidence of breast cancer related lymphedema of the arm after surgery and axillary lymph node dissection in early breast cancer patients treated with concomitant irradiation and anthracyclines followed by paclitaxel. Eur. J. Lymphology Relat. Probl. 2011, 22, 20–24. [Google Scholar]
- Cariati, M.; Bains, S.; Grootendorst, M.; Suyoi, A.; Peters, M.; Mortimer, P.; Ellis, P.; Harries, M.; Van Hemelrijck, M.; Purushotham, A. Adjuvant taxanes play a key role in the development of upper limb breast cancer-related lymphoedema. Eur. J. Surg. Oncol. 2015, 41, S18. [Google Scholar] [CrossRef]
- Aoishi, Y.; Oura, S.; Nishiguchi, H.; Hirai, Y.; Miyasaka, M.; Kawaji, M.; Shima, A.; Nishimura, Y. Risk factors for breast cancer-related lymphedema: Correlation with docetaxel administration. Breast Cancer 2020, 27, 929–937. [Google Scholar] [CrossRef] [PubMed]
- Gross, J.P.; Sachdev, S.; Helenowski, I.B.; Lipps, D.; Hayes, J.P.; Donnelly, E.D.; Strauss, J.B. Radiation Therapy Field Design and Lymphedema Risk After Regional Nodal Irradiation for Breast Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2018, 102, 71–78. [Google Scholar] [CrossRef]
- Kibar, S.; Dalyan Aras, M.; Ünsal Delialioğlu, S.; Köseoğlu, B.F. A cross-sectional study examining the risk factors associated with lymphedema and its prevalence in breast cancer patients after level 3 axillary lymph node dissection. Turkiye Fiziksel Tip ve Rehabilitasyon Dergisi 2015, 61, 36–44. [Google Scholar] [CrossRef]
| Variable | Without Clinical BCRL after 3 Years | With Clinical BCRL after 3 Years | p-Value |
|---|---|---|---|
| Demographic and general health-related variables | |||
| N = 71 | N = 47 | ||
| Age | 54.6 (±11.8) * | 56.9 (±12.7) * | 0.394 |
| BMI | 25.7 (±4.9) * | 26.2 (±4.9) * | 0.451 |
| Surgery on dominant side | |||
| No | 34 (47.89%) | 24 (51.06%) | 0.851 |
| Yes | 37 (52.11%) | 23 (48.94%) | |
| Diabetes | |||
| No | 68 (95.77%) | 45 (95.74%) | 1.000 |
| Yes | 3 (4.23%) | 2 (4.26%) | |
| Hypothyroidism | |||
| No | 68 (95.77%) | 40 (85.11%) | 0.087 |
| Yes | 3 (4.23%) | 7 (14.89%) | |
| Hyperthyroidism | |||
| No | 68 (95.77%) | 46 (97.87%) | 1.000 |
| Yes | 3 (4.23%) | 1 (2.13%) | |
| Arterial hypertension | |||
| No | 57 (80.28%) | 36 (76.60%) | 0.651 |
| Yes | 14 (19.72%) | 11 (23.40%) | |
| Chronic heart failure | |||
| No | 70 (98.59%) | 46 (97.87%) | 1.000 |
| Yes | 1 (1.41%) | 1 (2.13%) | |
| Chronic renal failure | |||
| No | 71 (100%) | 46 (97.87%) | 0.398 |
| Yes | 0 (0%) | 1 (2.13%) | |
| Previous injury/infection | |||
| No | 65 (91.55%) | 43 (91.49%) | 1.000 |
| Yes | 6 (8.45%) | 4 (8.54%) | |
| N = 69 | N = 44 | ||
| Physical activity score | |||
| Low | 7 (10.14%) | 6 (13.64%) | 0.630 |
| Moderate | 29 (42.03%) | 21 (47.73%) | |
| High | 33 (47.83%) | 17 (38.64%) | |
| Breast-cancer- and treatment-related variables | |||
| N = 71 | N = 47 | ||
| Type of cancer | |||
| Ductal | 58 (81.69%) | 37 (78.72%) | 0.586 |
| Lobular | 8 (11.27%) | 8 (17.02%) | |
| Other | 5 (7.04%) | 2 (4.26%) | |
| Tumor stage | |||
| Tis | 2 (2.82%) | 0 (0%) | 0.002 |
| T1 | 30 (42.25%) | 10 (21.28%) | |
| T2 | 31 (43.66%) | 18 (38.30%) | |
| T3 | 6 (8.45%) | 11 (23.40%) | |
| T4 | 2 (2.82%) | 8 (17.02%) | |
| Type of surgery | |||
| Mastectomy | 40 (56.34%) | 43 (91.49.84%) | <0.001 |
| Breast-conserving surgery | 31 (43.66%) | 4 (8.51%) | |
| Extent of LN dissection | |||
| SLNB | 45 (63.38%) | 3 (6.38%) | <0.001 |
| ALND | 26 (36.62%) | 44 (93.62%) | |
| Number of removed LNs | 8.68 (±10.351) * | 18.45 (±8.235) * | <0.001 |
| Number of positive LNs | 0.85 (±2.494) * | 3.26 (±3.26) * | <0.001 |
| Postsurgical complications | |||
| No | 35 (49.30%) | 10 (21.28%) | 0.003 |
| Yes | 36 (50.70%) | 37 (78.72%) | |
| RT axilla | |||
| No | 69 (97.18%) | 41 (87.23%) | 0.058 |
| Yes | 2 (2.82%) | 6 (12.77%) | |
| Taxanes | |||
| No | 45 (63.38%) | 12 (25.53%) | <0.001 |
| Yes | 26 (36.62%) | 35 (74.47%) | |
| Tamoxifen | |||
| No | 56 (78.87%) | 38 (80.85%) | 1.000 |
| Yes | 15 (21.13%) | 9 (19.15%) | |
| AI | |||
| No | 25 (35.21%) | 12 (25.53%) | 0.314 |
| Yes | 46 (64.79%) | 35 (74.47%) | |
| Patients with Clinical BCRL N = 42 | Patients without Clinical BCRL N = 70 | |||||
|---|---|---|---|---|---|---|
| Without Early Disturbance | With Early Disturbance | p-Value | Without Early Disturbance | With Early Disturbance | p-Value | |
| N = 25 | N = 17 | N = 46 | N = 24 | |||
| Total volume Median (range) | 2632 mL (1477;4548) | 2537 mL (1821;3892) | 0.898 | 2554 mL (1641;3952) | 2490 mL (1709;3695) | 0.590 |
| Absolute volume difference sum Median (range) | 175 mL (−52.87;420) | 152 mL (19.94;500) | 1.000 | −28 mL (−250;163) | −43 mL (−231;197) | 0.758 |
| Relative volume difference percentage Median (range) | 7.61% (−1.77;18.78) | 6.34% (0.90;23.38) | 0.778 | −0.86% (−10,91;6.62) | −1.69% (−9.11;8.56) | 0.806 |
| Variable | HR (95% CI) | p-Value | Number of Patients |
|---|---|---|---|
| Early disturbance lymphofluoroscopy versus no early disturbance lymphofluoroscopy | 2.808 (1.362;5.791) | 0.0052 | 112 |
| Demographic and general health-related variables | |||
| Age, continuous | 1.017 (0.992;1.042) | 0.1838 | 118 |
| BMI, continuous | 1.028 (0.970;1.089) | 0.3509 | 118 |
| Treatment on dominant side versus non-dominant side | 0.895 (0.505;1.586) | 0.7033 | 118 |
| Hypertension versus no hypertension | 1.219 (0.620;2.395) | 0.5658 | 118 |
| Diabetes versus no diabetes | 1.327 (0.321;5.490) | 0.6964 | 118 |
| Hypothyroidism versus no hypothyroidism | 2.070 (0.926;4.626) | 0.0762 | 118 |
| Hyperthyroidism versus no hyperthyroidism | 0.503 (0.069;3.649) | 0.4967 | 118 |
| Chronic heart failure versus no chronic heart failure | 1.277 (0.176;9.282) | 0.8091 | 118 |
| Chronic renal failure versus no chronic renal failure | 2.432 (0.334;17.703) | 0.3801 | 118 |
| Previous injury/infection versus no previous injury/infection | 1.113 (0.399;3.103) | 0.8374 | 118 |
| Physical activity score, continuous | 0.768 (0.496;1.191) | 0.2385 | 113 |
| Breast-cancer- and treatment-related variables | |||
| Type of cancer | 0.4767 | 118 | |
| Tumor stage | 1.745 (1.317;2.313) | 0.0001 | 118 |
| BCS versus ME | 0.186 (0.067;0.519) | 0.0013 | 118 |
| Number of removed LNs, continuous | 1.055 (1.030;1.080) | <0.0001 | 118 |
| Number positive LNs, continuous | 1.121 (1.060;1.186) | <0.0001 | 118 |
| Postsurgical complications versus no postsurgical complications | 2.590 (1.286;5.213) | 0.0077 | 118 |
| RT axilla versus no RT axilla | 2.715 (1.149;6.416) | 0.0228 | 118 |
| Taxanes versus no taxanes | 3.220(1.669;6.210) | 0.0005 | 118 |
| Tamoxifen versus no tamoxifen | 0.874 (0.422;1.807) | 0.7160 | 118 |
| AI versus no AI | 1.400 (0.726;2.697) | 0.3152 | 118 |
| ALND versus SLNB | 15.127 (4.684;48.830) | <0.0001 | 118 |
| Variable | Test | HR (95% CI) | p-Value | Number of Patients |
|---|---|---|---|---|
| ALND | ALND vs. SLNB | 19.958 (6.108;65.217) | <0.0001 | 118 |
| Age | +1 year | 1.038 (1.015;1.062) | 0.0011 | 118 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thomis, S.; Devoogdt, N.; Bechter-Hugl, B.; Fourneau, I. Early Disturbance of Lymphatic Transport as a Risk Factor for the Development of Breast-Cancer-Related Lymphedema. Cancers 2023, 15, 1774. https://doi.org/10.3390/cancers15061774
Thomis S, Devoogdt N, Bechter-Hugl B, Fourneau I. Early Disturbance of Lymphatic Transport as a Risk Factor for the Development of Breast-Cancer-Related Lymphedema. Cancers. 2023; 15(6):1774. https://doi.org/10.3390/cancers15061774
Chicago/Turabian StyleThomis, Sarah, Nele Devoogdt, Beate Bechter-Hugl, and Inge Fourneau. 2023. "Early Disturbance of Lymphatic Transport as a Risk Factor for the Development of Breast-Cancer-Related Lymphedema" Cancers 15, no. 6: 1774. https://doi.org/10.3390/cancers15061774
APA StyleThomis, S., Devoogdt, N., Bechter-Hugl, B., & Fourneau, I. (2023). Early Disturbance of Lymphatic Transport as a Risk Factor for the Development of Breast-Cancer-Related Lymphedema. Cancers, 15(6), 1774. https://doi.org/10.3390/cancers15061774








