CA-125 Early Dynamics to Predict Overall Survival in Women with Newly Diagnosed Advanced Ovarian Cancer Based on Meta-Analysis Data
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
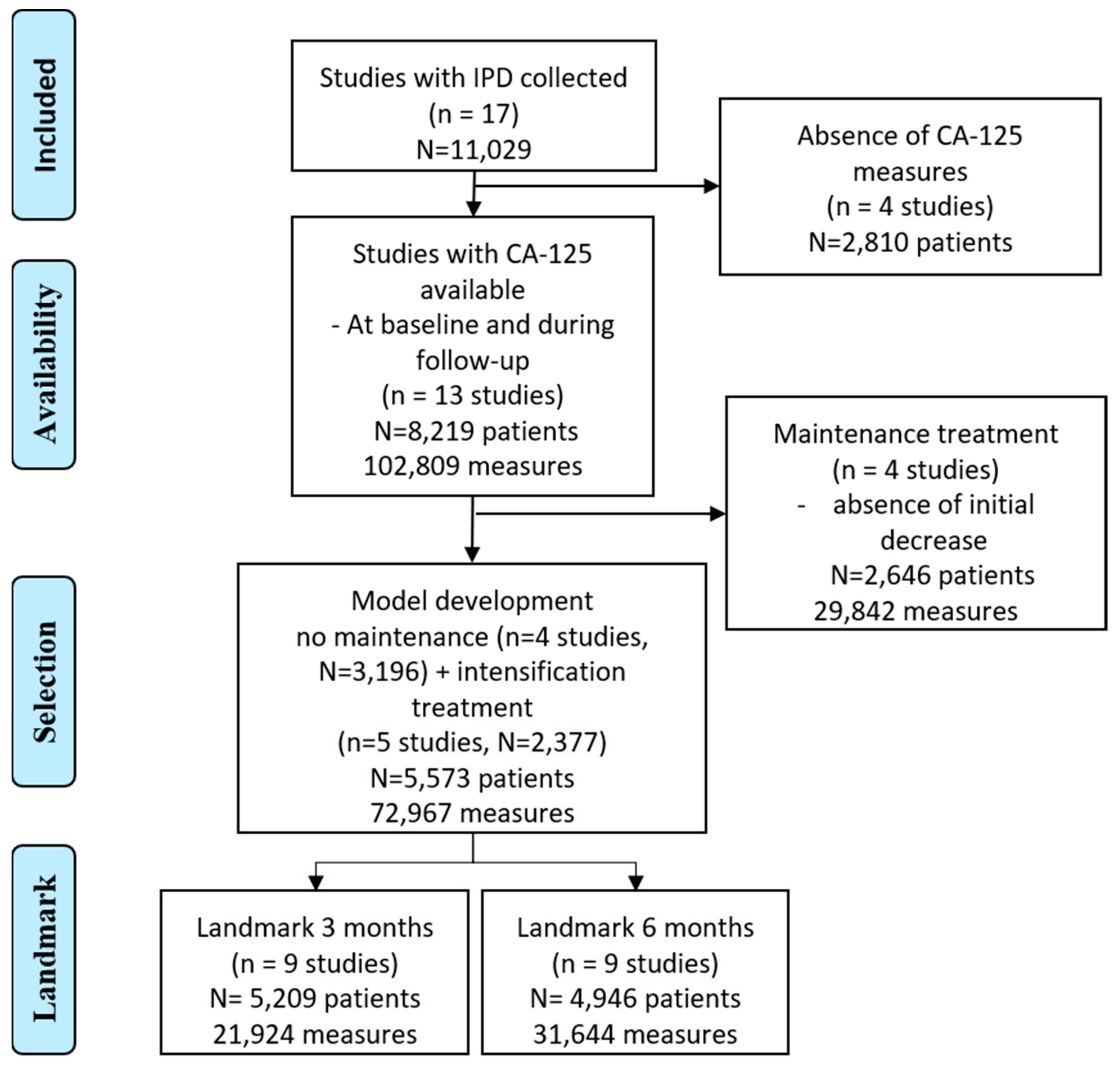
2.1. Study Population
2.2. Outcomes
2.3. Statistical Methods
2.4. Evaluation of the Predictive Performance of the CA-125 Summaries
3. Results
3.1. Study Selection and Characteristics
3.2. Endpoint and Landmark Timeframe
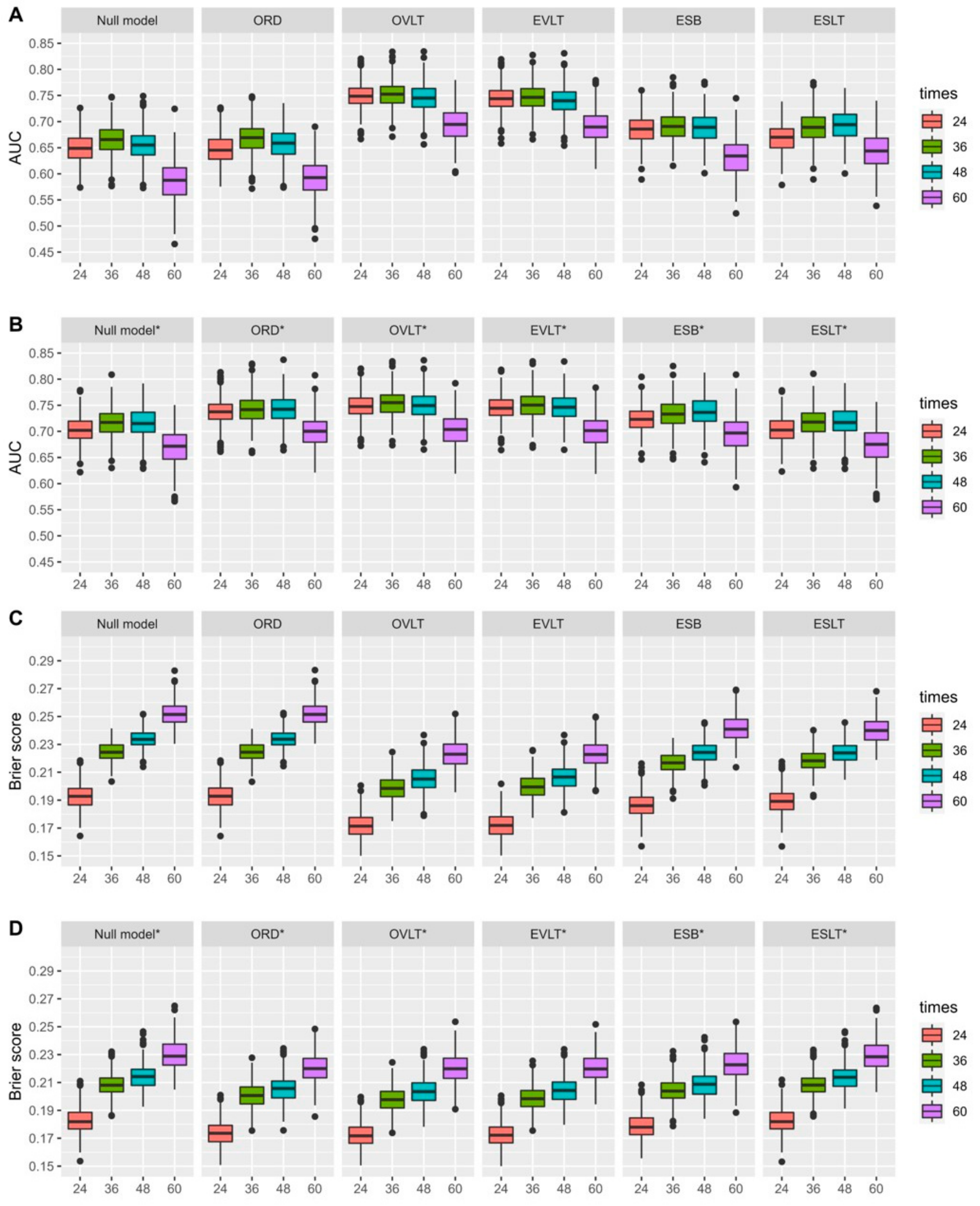
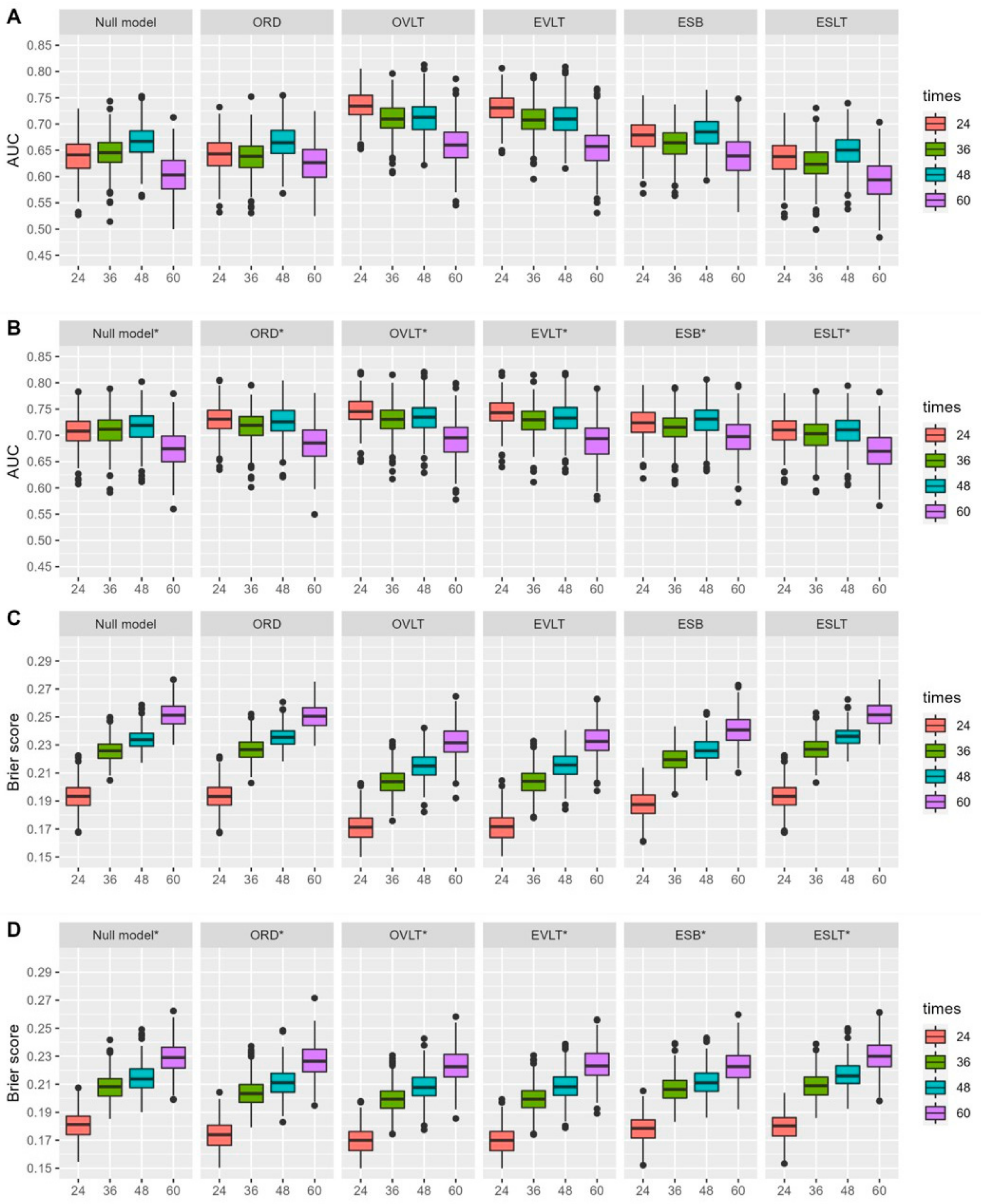
3.3. Performance of CA-125 Summaries
3.3.1. Landmark at 3 Months
3.3.2. Landmark at 6 Months
3.3.3. CA-125 Summary Performance for Subgroups of Patients Based on Characteristics
3.3.4. Sensitivity Analysis and Predictive Values of the CA-125 Normal Range
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Doherty, J.A.; Peres, L.C.; Wang, C.; Way, P.; Greene, C.S.; Schildkraut, J.M. Challenges and Opportunities in Studying the Epidemiology of Ovarian Cancer Subtypes. Curr. Epidemiol. Rep. 2017, 4, 211–220. [Google Scholar] [CrossRef]
- Ray-Coquard, I.; Pautier, P.; Pignata, S.; Pérol, D.; González-Martín, A.; Berger, R.; Fujiwara, K.; Vergote, I.; Colombo, N.; Mäenpää, J.; et al. Olaparib plus Bevacizumab as First-Line Maintenance in Ovarian Cancer. N. Engl. J. Med. 2019, 381, 2416–2428. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, S.; Moore, K.; Colombo, N.; Scambia, G.; Kim, B.; Oaknin, A.; Friedlander, M.; Lisyanskaya, A.; Floquet, A.; Leary, A.; et al. Maintenance olaparib for patients with newly diagnosed advanced ovarian cancer and a BRCA mutation (SOLO1/GOG 3004): 5-year follow-up of a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2021, 22, 1721–1731. [Google Scholar] [CrossRef]
- Grimm, C.; Cropet, C.; Ray-Coquard, I. Maintenance olaparib plus bevacizumab (bev) after platinum-based chemotherapy plus bev in patients (pts) with newly diagnosed advanced high-grade ovarian cancer (HGOC): Efficacy by timing of surgery and residual tumor status in the Phase III PAOLA-1 trial. Gynecol. Oncol. 2020, 159, 19. [Google Scholar] [CrossRef]
- González-Martín, A.; Pothuri, B.; Vergote, I.; Christensen, R.D.; Graybill, W.; Mirza, M.; McCormick, C.; Lorusso, D.; Hoskins, P.; Freyer, G.; et al. Niraparib in Patients with Newly Diagnosed Advanced Ovarian Cancer. N. Engl. J. Med. 2019, 381, 2391–2402. [Google Scholar] [CrossRef] [PubMed]
- Taylor, P.T.; Haverstick, D.M.; Rustin, G.J.S. Re: New guidelines to evaluate the response to treatment in solid tumors (ovarian cancer) (multiple letters). J. Natl. Cancer Inst. 2005, 97, 151–152. [Google Scholar] [CrossRef] [PubMed]
- Rustin, G.J.S.; Van Der Burg, M.E.L.; Griffin, C.L.; Guthrie, D.; Lamont, A.; Jayson, G.C.; Kristensen, G.; Mediola, C.; Coens, C.; Qian, W.; et al. Early versus delayed treatment of relapsed ovarian cancer (MRC OV05/EORTC 55955): A randomised trial. Lancet 2010, 376, 1155–1163. [Google Scholar] [CrossRef]
- Rustin, G.J.S. Follow-up with CA125 after primary therapy of advanced ovarian cancer has major implications for treatment outcome and trial performances and should not be routinely performed. Ann. Oncol. 2011, 22 (Suppl. S8), 45–48. [Google Scholar] [CrossRef]
- Esselen, K.M.; Cronin, A.; Bixel, K.; Bookman, M.; Burger, R.; Cohn, D.; Meyer, L.; Matulonis, U.; Niland, J.; Sun, C.; et al. Use of CA-125 tests and computed tomographic scans for surveillance in ovarian cancer. JAMA Oncol. 2016, 2, 1427–1433. [Google Scholar] [CrossRef]
- Markman, M.; Federico, M.; Liu, P.Y.; Hannigan, E.; Alberts, D. Significance of early changes in the serum CA-125 antigen level on overall survival in advanced ovarian cancer. Gynecol. Oncol. 2006, 103, 195–198. [Google Scholar] [CrossRef] [PubMed]
- Skaznik-Wikiel, M.E.; Sukumvanich, P.; Beriwal, S.; Zorn, K.K.; Kelley, J.L.; Richard, S.D.; Krivak, T.C. Possible use of CA-125 level normalization after the third chemotherapy cycle in deciding on chemotherapy regimen in patients with epithelial ovarian cancer. Int. J. Gynecol. Cancer 2011, 21, 1013–1017. [Google Scholar] [CrossRef]
- You, B.; Colomban, O.; Heywood, M.; Lee, C.; Davy, M.; Reed, N.; Pignata, S.; Varsellona, N.; Emons, G.; Rehman, K.; et al. The strong prognostic value of KELIM, a model-based parameter from CA 125 kinetics in ovarian cancer: Data from CALYPSO trial (a GINECO-GCIG study). Gynecol. Oncol. 2013, 130, 289–294. [Google Scholar] [CrossRef] [PubMed]
- Colloca, G.; Venturino, A.; Governato, I. CA125-related tumor cell kinetics variables after chemotherapy in advanced ovarian cancer: A systematic review. Clin. Transl. Oncol. 2016, 18, 813–824. [Google Scholar] [CrossRef]
- Liao, Y.C.; Ou, Y.C.; Wu, C.H.; Fu, H.C.; Tsai, C.C.; Lin, H. CA125 normalization within 60 days as an independent prognostic factor for patients with advanced epithelial ovarian cancer. Cancer Biomark. 2021, 32, 559–567. [Google Scholar] [CrossRef] [PubMed]
- Overall, J.E.; Tonidandel, S.; Starbuck, R.R. Last-observation-carried-forward (LOCF) and tests for difference in mean rates of change in controlled repeated measurements designs with dropouts. Soc. Sci. Res. 2009, 38, 492–503. [Google Scholar] [CrossRef]
- Prentice, R.L. Covariate measurement errors and parameter estimation in a failure time regression model. Biometrika 1982, 69, 331. [Google Scholar] [CrossRef]
- Proust-Lima, C.; Taylor, J.M.G. Development and validation of a dynamic prognostic tool for prostate cancer recurrence using repeated measures of posttreatment PSA: A joint modeling approach. Biostatistics 2009, 10, 535–549. [Google Scholar] [CrossRef]
- Colomban, O.; Tod, M.; Leary, A.; Ray-Coquard, I.; Lortholary, A.; Hardy-Bessard, A.C.; Pfisterer, J.; Bois, A.D.; Kurzeder, C.; Burges, A.; et al. Early Modeled Longitudinal CA-125 Kinetics and Survival of Ovarian Cancer Patients: A GINECO AGO MRC CTU Study. Clin. Cancer Res. 2019, 25, 5342–5350. [Google Scholar] [CrossRef]
- You, B.; Freyer, G.; Gonzalez-Martin, A.; Lheureux, S.; McNeish, I.; Penson, R.T.; Pignata, S.; Pujade-Lauraine, E. The role of the tumor primary chemosensitivity relative to the success of the medical-surgical management in patients with advanced ovarian carcinomas. Cancer Treat. Rev. 2021, 100, 102294. [Google Scholar] [CrossRef] [PubMed]
- Lauby, A.; Colomban, O.; Corbaux, P.; Peron, J.; Wagensveld, L.V.; Gertych, W.; Bakrin, N.; Descargues, P.; Lopez, J.; Kepenekian, V.; et al. The Increasing Prognostic and Predictive Roles of the Tumor Primary Chemosensitivity Assessed by CA-125 Elimination Rate Constant K (KELIM) in Ovarian Cancer: A Narrative Review. Cancers 2022, 14, 98. [Google Scholar] [CrossRef]
- Carrot, A.; Elaidi, R.T.; Colomban, O.; Maillet, D.; Tod, M.; You, B.; Oudard, S. Modeled Early Longitudinal PSA Kinetics Prognostic Value in Rising PSA Prostate Cancer Patients after Local Therapy Treated with ADT +/− Docetaxel. Cancers 2022, 14, 815. [Google Scholar] [CrossRef] [PubMed]
- Bartl, T.; Karacs, J.; Kreuzinger, C.; Pfaffinger, S.; Kendler, J.; Ciocsirescu, C.; Wolf, A.; Reinthaller, A.; Meyer, E.; Brandstetter, M.; et al. Tumor growth rate estimates are independently predictive of therapy response and survival in recurrent high-grade serous ovarian cancer patients. Cancers 2021, 13, 1076. [Google Scholar] [CrossRef] [PubMed]
- Van Houwelingen, H.C. Dynamic prediction by landmarking in event history analysis. Scand. J. Stat. 2007, 34, 70–85. [Google Scholar] [CrossRef]
- Ferrer, L.; Putter, H.; Proust-Lima, C. Individual dynamic predictions using landmarking and joint modelling: Validation of estimators and robustness assessment. Stat. Methods Med. Res. 2018, 28, 3649–3666. [Google Scholar] [CrossRef]
- Heagerty, P.J.; Lumley, T.; Pepe, M.S. Time-dependent ROC curves for censored survival data and a diagnostic marker. Biometrics 2000, 56, 337–344. [Google Scholar] [CrossRef]
- Gerds, T.A.; Schumacher, M. Consistent estimation of the expected brier score in general survival models with right-censored event times. Biom. J. 2006, 48, 1029–1040. [Google Scholar] [CrossRef]
- Blanche, P.; Proust-Lima, C.; Loubère, L.; Berr, C.; Dartigues, J.F.; Jacqmin-Gadda, H. Quantifying and comparing dynamic predictive accuracy of joint models for longitudinal marker and time-to-event in presence of censoring and competing risks. Biometrics 2015, 71, 102–113. [Google Scholar] [CrossRef]
- Gerds, T.A.; Cai, T.; Schumacher, M. The performance of risk prediction models. Biom. J. 2008, 50, 457–479. [Google Scholar] [CrossRef]
- Debray, T.P.A.; Riley, R.D.; Rovers, M.M.; Reitsma, J.B.; Moons, K.G.M. Individual Participant Data (IPD) Meta-analyses of Diagnostic and Prognostic Modeling Studies: Guidance on Their Use. PLoS Med. 2015, 12, e1001886. [Google Scholar] [CrossRef]
- Stock, S.J.E.; Horne, M.R.; Bruijn, M.; White, H.; Boyd, K.A.; Heggie, R.; Wotherspoon, L.; Aucott, L.S.; Morris, R.; Dorling, J.; et al. Development and validation of a risk prediction model of preterm birth for women with preterm labour symptoms (the QUIDS study): A prospective cohort study and individual participant data meta-analysis. PLoS Med. 2021, 18, e1003686. [Google Scholar] [CrossRef]
- Paoletti, X.; Lewsley, L.A.; Daniele, G.; Cook, A.; Yanaihara, N.; Tinker, A.; Kristensen, G.; Ottevanger, P.B.; Aravantinos, G.; Miller, A.; et al. Assessment of Progression-Free Survival as a Surrogate End Point of Overall Survival in First-Line Treatment of Ovarian Cancer: A Systematic Review and Meta-analysis. JAMA Netw. Open 2020, 3, e1918939. [Google Scholar] [CrossRef] [PubMed]
- Verbeke, G.; Molenberghs, G. Linear Mixed Models for Longitudinal Data; Springer: New York, NY, USA, 2009; Available online: https://books.google.fr/books?id=jmPkX4VU7h0C (accessed on 28 April 2009).
- Perperoglou, A.; Sauerbrei, W.; Abrahamowicz, M.; Schmid, M. A review of spline function procedures in R. BMC Med. Res. Methodol. 2019, 19, 46. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.T.; Williamson, P.R.; Marson, A.G. Investigating heterogeneity in an individual patient data meta-analysis of time to event outcomes. Stat. Med. 2005, 24, 1307–1319. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.T.; Williamson, P.R.; Marson, A.G. An overview of methods and empirical comparison of aggregate data and individual patient data results for investigating heterogeneity in meta-analysis of time-to-event outcomes. J. Eval. Clin. Pract. 2005, 11, 468–478. [Google Scholar] [CrossRef] [PubMed]
- Blanche, P.; Dartigues, J.F.; Jacqmin-Gadda, H. Review and comparison of ROC curve estimators for a time-dependent outcome with marker-dependent censoring. Biom. J. 2013, 55, 687–704. [Google Scholar] [CrossRef]
- Gerds, T.A.; Scheike, T.H.; Andersen, P.K. Absolute risk regression for competing risks: Interpretation, link functions, and prediction. Stat. Med. 2012, 31, 3921–3930. [Google Scholar] [CrossRef]
- Kim, S.I.; Lee, M.; Kim, H.S.; Chung, H.H.; Kim, J.-W.; Park, N.H.; Song, Y.S. Effect of BRCA mutational status on survival outcome in advanced-stage high-grade serous ovarian cancer. J. Ovarian Res. 2019, 12, 40. [Google Scholar] [CrossRef]
- Giampaolino, P.; Foreste, V.; Della Corte, L.; Di Filippo, C.; Iorio, G.; Bifulco, G. Role of biomarkers for early detection of ovarian cancer recurrence. Gland. Surg. 2020, 9, 1102–1111. [Google Scholar] [CrossRef]
- Stewart, L.A.; Clarke, M.; Rovers, M.; Riley, R.D.; Simmonds, M.; Stewart, G.; Tierney, J.F. Preferred reporting items for a systematic review and meta-analysis of individual participant data: The PRISMA-IPD statement. JAMA J. Am. Med. Assoc. 2015, 313, 1657–1665. [Google Scholar] [CrossRef]

| Trial Name | Number of pts | Number of CA-125 Measures | Median Survival | |
|---|---|---|---|---|
| Intensification therapy | total | 2377 | 21,978 | 3.87 (3.6; 4.11) |
| MITO-7 | 529 | 1429 | NR | |
| GINECO-2007 | 109 | 634 | 2.63 (2.25; 3.39) | |
| TURBO-2014 | 253 | 3421 | 3.74 (3.23; 4.30) | |
| JGOG-3016 | 557 | 3475 | 6.72 (5.30; NA) | |
| SCOTROC-4 | 929 | 14,019 | 2.75 (2.54; 2.97) | |
| No maintenance | total | 3196 | 49,989 | 4.33 (4.08; 4.66) |
| JGOG-3017 | 632 | 9403 | NR | |
| NSGO-2012 | 774 | 9904 | 3.60 (3.21; 3.98) | |
| SCOTROC-1 | 1052 | 12,582 | 2.86 (2.73; NA) | |
| CCTG-OV.16 | 737 | 18,100 | 3.84 (3.49; 4.28) | |
| Total | 5573 | 72,967 | 4.11 (3.94; 4.33) | |
| Trials | FIGO | Residual Disease | |||||||
|---|---|---|---|---|---|---|---|---|---|
| I | II | III | IV | . | <1 cm | ≥1 cm | NA | . | |
| MITO-7 | 41 (8.9%) | 42 (9.1%) | 273 (59.2%) | 105 (22.8%) | NA | NA | |||
| GINECO-2007 | 0 | 0 | 78 (80.4%) | 19 (19.6%) | 1 | 14 (14.4%) | 83 (85.6%) | 1 | |
| TURBO | 0 | 19 (7.9%) | 156 (65%) | 65 (27.1%) | 173 (72.7% | 63 (26.5%)) | 2 (0.8%) | 2 | |
| JGOG-3016 | 0 | 102 (18.6%) | 364 (66.5%) | 81 (14.8%) | 258 (47.2%) | 275 (50.3%) | 14 (2.6%) | ||
| SCOTROC-4 | 118 (13.9%) | 75 (8.8%) | 549 (64.6%) | 108 (12.7%) | 300 (35.3%) | 550 (64.7%) | |||
| JGOG-3017 | 395 (66.1%) | 69 (11.5%) | 112 (18.7%) | 22 (3.7%) | 548 (91.6%) | 48 (8%) | 2 (0.3%) | ||
| NSGO-2012 | 0 | 94 (12.7%) | 533 (71.8%) | 115 (15.5%) | 317 (42.7%) | 425 (57.3%) | |||
| SCOTROC-1 | 70 (7.2%) | 127 (13%) | 645 (65.9%) | 137 (14%) | 332 (33.9%) | 647 (66.1%) | |||
| CCTG-OV.16 | 0 | 65 (9.4%) | 468 (67.4%) | 161 (23.2%) | 325 (57%) | 238 (41.8%) | 7 (1.2%) | 124 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karamouza, E.; Glasspool, R.M.; Kelly, C.; Lewsley, L.-A.; Carty, K.; Kristensen, G.B.; Ethier, J.-L.; Kagimura, T.; Yanaihara, N.; Cecere, S.C.; et al. CA-125 Early Dynamics to Predict Overall Survival in Women with Newly Diagnosed Advanced Ovarian Cancer Based on Meta-Analysis Data. Cancers 2023, 15, 1823. https://doi.org/10.3390/cancers15061823
Karamouza E, Glasspool RM, Kelly C, Lewsley L-A, Carty K, Kristensen GB, Ethier J-L, Kagimura T, Yanaihara N, Cecere SC, et al. CA-125 Early Dynamics to Predict Overall Survival in Women with Newly Diagnosed Advanced Ovarian Cancer Based on Meta-Analysis Data. Cancers. 2023; 15(6):1823. https://doi.org/10.3390/cancers15061823
Chicago/Turabian StyleKaramouza, Eleni, Rosalind M. Glasspool, Caroline Kelly, Liz-Anne Lewsley, Karen Carty, Gunnar B. Kristensen, Josee-Lyne Ethier, Tatsuo Kagimura, Nozomu Yanaihara, Sabrina Chiara Cecere, and et al. 2023. "CA-125 Early Dynamics to Predict Overall Survival in Women with Newly Diagnosed Advanced Ovarian Cancer Based on Meta-Analysis Data" Cancers 15, no. 6: 1823. https://doi.org/10.3390/cancers15061823
APA StyleKaramouza, E., Glasspool, R. M., Kelly, C., Lewsley, L.-A., Carty, K., Kristensen, G. B., Ethier, J.-L., Kagimura, T., Yanaihara, N., Cecere, S. C., You, B., Boere, I. A., Pujade-Lauraine, E., Ray-Coquard, I., Proust-Lima, C., & Paoletti, X. (2023). CA-125 Early Dynamics to Predict Overall Survival in Women with Newly Diagnosed Advanced Ovarian Cancer Based on Meta-Analysis Data. Cancers, 15(6), 1823. https://doi.org/10.3390/cancers15061823







