Abbreviated MRI for Comprehensive Regional Lymph Node Staging during Pre-Operative Breast MRI
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Inclusion and Exclusion Criteria
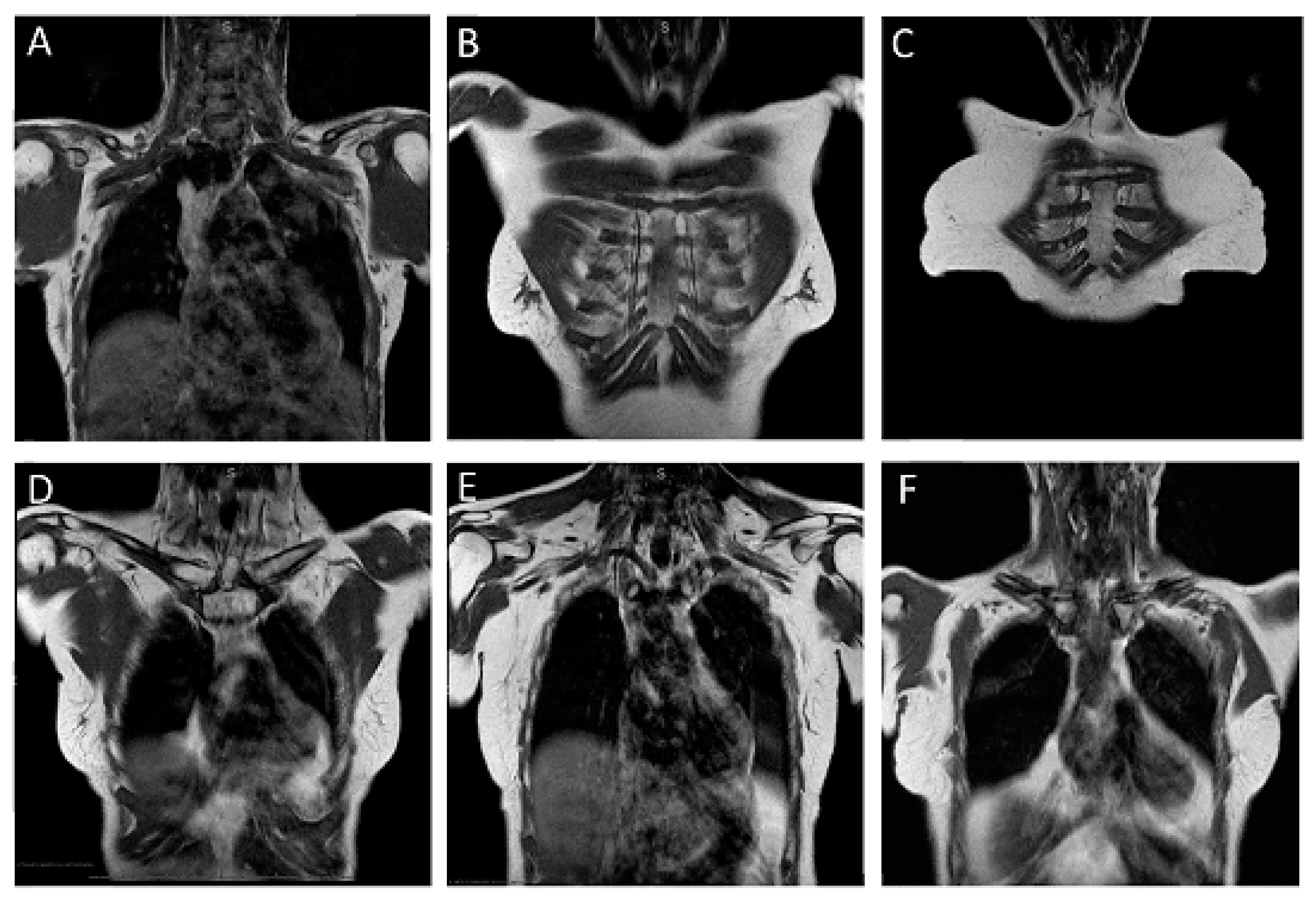
2.2. MR Imaging Protocol
2.3. MRI Evaluation of Lymph Node Status
2.4. Validation of Lymph Node Diagnoses
2.5. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Edge, S.B.; Compton, C.C. The American Joint Committee on Cancer: The 7th edition of the AJCC cancer staging manual and the future of TNM. Ann. Surg. Oncol. 2010, 17, 1471–1474. [Google Scholar] [CrossRef]
- Carlson, R.W.; Allred, D.C.; Anderson, B.O.; Burstein, H.J.; Carter, W.B.; Edge, S.B.; Erban, J.K.; Farrar, W.B.; Goldstein, L.J.; Gradishar, W.J.; et al. Breast cancer. Clinical practice guidelines in oncology. J. Natl. Compr. Cancer Netw. 2009, 7, 122–192. [Google Scholar] [CrossRef] [PubMed]
- Rao, R.; Euhus, D.; Mayo, H.G.; Balch, C. Axillary node interventions in breast cancer: A systematic review. JAMA 2013, 310, 1385–1394. [Google Scholar] [CrossRef] [PubMed]
- Ivens, D.; Hoe, A.L.; Podd, T.J.; Hamilton, C.R.; Taylor, I.; Royle, G.T. Assessment of morbidity from complete axillary dissection. Br. J. Cancer 1992, 66, 136–138. [Google Scholar] [CrossRef] [Green Version]
- Yeoh, E.K.; Denham, J.W.; Davies, S.A.; Spittle, M.F. Primary breast cancer. Complications of axillary management. Acta Radiol. Oncol. 1986, 25, 105–108. [Google Scholar] [CrossRef] [Green Version]
- Giuliano, A.E.; Hunt, K.K.; Ballman, K.V.; Beitsch, P.D.; Whitworth, P.W.; Blumencranz, P.W.; Leitch, A.M.; Saha, S.; McCall, L.M.; Morrow, M. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: A randomized clinical trial. JAMA 2011, 305, 569–575. [Google Scholar] [CrossRef] [Green Version]
- Giuliano, A.E.; Ballman, K.V.; McCall, L.; Beitsch, P.D.; Brennan, M.B.; Kelemen, P.R.; Ollila, D.W.; Hansen, N.M.; Whitworth, P.W.; Blumencranz, P.W.; et al. Effect of Axillary Dissection vs No Axillary Dissection on 10-Year Overall Survival Among Women With Invasive Breast Cancer and Sentinel Node Metastasis: The ACOSOG Z0011 (Alliance) Randomized Clinical Trial. JAMA 2017, 318, 918–926. [Google Scholar] [CrossRef] [Green Version]
- Gao, W.; Lu, S.; Zeng, Y.; Chen, X.; Shen, K. Axilla lymph node dissection can be safely omitted in patients with 1-2 positive sentinel nodes receiving mastectomy: A large multi-institutional study and a systemic meta-analysis. Breast Cancer Res. Treat. 2022, 196, 129–141. [Google Scholar] [CrossRef]
- Donker, M.; van Tienhoven, G.; Straver, M.E.; Meijnen, P.; van de Velde, C.J.; Mansel, R.E.; Cataliotti, L.; Westenberg, A.H.; Klinkenbijl, J.H.; Orzalesi, L.; et al. Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer (EORTC 10981-22023 AMAROS): A randomised, multicentre, open-label, phase 3 non-inferiority trial. Lancet Oncol. 2014, 15, 1303–1310. [Google Scholar] [CrossRef] [Green Version]
- Yun, S.J.; Sohn, Y.M.; Seo, M. Risk Factors for False-Negative and False-Positive Results of Magnetic Resonance Computer-Aided Evaluation in Axillary Lymph Node Staging. J. Comput. Assist. Tomogr. 2016, 40, 928–936. [Google Scholar] [CrossRef] [PubMed]
- Chai, R.; Ma, H.; Xu, M.; Arefan, D.; Cui, X.; Liu, Y.; Zhang, L.; Wu, S.; Xu, K. Differentiating axillary lymph node metastasis in invasive breast cancer patients: A comparison of radiomic signatures from multiparametric breast MR sequences. J. Magn. Reson. Imaging 2019, 50, 1125–1132. [Google Scholar] [CrossRef]
- Baltzer, P.A.; Dietzel, M.; Burmeister, H.P.; Zoubi, R.; Gajda, M.; Camara, O.; Kaiser, W.A. Application of MR mammography beyond local staging: Is there a potential to accurately assess axillary lymph nodes? evaluation of an extended protocol in an initial prospective study. Am. J. Roentgenol. 2011, 196, W641–W647. [Google Scholar] [CrossRef]
- van der Ent, F.W.; Kengen, R.A.; van der Pol, H.A.; Povel, J.A.; Stroeken, H.J.; Hoofwijk, A.G. Halsted revisited: Internal mammary sentinel lymph node biopsy in breast cancer. Ann. Surg. 2001, 234, 79–84. [Google Scholar] [CrossRef]
- Kuhl, C.K.; Strobel, K.; Bieling, H.; Leutner, C.; Schild, H.H.; Schrading, S. Supplemental Breast MR Imaging Screening of Women with Average Risk of Breast Cancer. Radiology 2017, 283, 361–370. [Google Scholar] [CrossRef] [Green Version]
- Brierley, J.D.; Gospodarowicz, M.K.; Wittekind, C. TNM Classification of Malignant Tumours; John Wiley & Sons: New York, NY, USA, 2017. [Google Scholar]
- Coates, A.S.; Winer, E.P.; Goldhirsch, A.; Gelber, R.D.; Gnant, M.; Piccart-Gebhart, M.; Thürlimann, B.; Senn, H.-J.; Members, P.; André, F. Tailoring therapies—Improving the management of early breast cancer: St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2015. Ann. Oncol. 2015, 26, 1533–1546. [Google Scholar] [CrossRef]
- Kreienberg, R.; Albert, U.; Follmann, M.; Kopp, I.; Kühn, T.; Wöckel, A. Interdisziplinäre S3-Leitlinie für die Diagnostik, Therapie und Nachsorge des Mammakarzinoms. Senol.-Z. Mammadiagnostik Ther. 2013, 10, 164–192. [Google Scholar] [CrossRef]
- Giuliano, A.E.; Kirgan, D.M.; Guenther, J.M.; Morton, D.L. Lymphatic mapping and sentinel lymphadenectomy for breast cancer. Ann. Surg. 1994, 220, 391–398; discussion 398–401. [Google Scholar] [CrossRef] [PubMed]
- Lyman, G.H.; Somerfield, M.R.; Bosserman, L.D.; Perkins, C.L.; Weaver, D.L.; Giuliano, A.E. Sentinel Lymph Node Biopsy for Patients With Early-Stage Breast Cancer: American Society of Clinical Oncology Clinical Practice Guideline Update. J. Clin. Oncol. 2017, 35, 561–564. [Google Scholar] [CrossRef] [Green Version]
- Humphrey, K.L.; Saksena, M.A.; Freer, P.E.; Smith, B.L.; Rafferty, E.A. To do or not to do: Axillary nodal evaluation after ACOSOG Z0011 Trial. Radiographics 2014, 34, 1807–1816. [Google Scholar] [CrossRef] [PubMed]
- Gera, R.; Kasem, A.; Mokbel, K. Can Complete Axillary Node Dissection Be Safely Omitted in Patients with Early Breast Cancer When the Sentinel Node Biopsy Is Positive for Malignancy? An Update for Clinical Practice. In Vivo 2018, 32, 1301–1307. [Google Scholar] [CrossRef] [Green Version]
- Cardoso, F.; Harbeck, N.; Fallowfield, L.; Kyriakides, S.; Senkus, E. Locally recurrent or metastatic breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2012, 23 (Suppl. S7), vii11–vii19. [Google Scholar] [CrossRef] [PubMed]
- Houssami, N.; Diepstraten, S.C.; Cody, H.S., III; Turner, R.M.; Sever, A.R. Clinical utility of ultrasound-needle biopsy for preoperative staging of the axilla in invasive breast cancer. Anticancer Res. 2014, 34, 1087–1097. [Google Scholar] [PubMed]
- Alvarez, S.; Añorbe, E.; Alcorta, P.; López, F.; Alonso, I.; Cortés, J. Role of sonography in the diagnosis of axillary lymph node metastases in breast cancer: A systematic review. Am. J. Roentgenol. 2006, 186, 1342–1348. [Google Scholar] [CrossRef] [Green Version]
- Marino, M.A.; Avendano, D.; Zapata, P.; Riedl, C.C.; Pinker, K. Lymph Node Imaging in Patients with Primary Breast Cancer: Concurrent Diagnostic Tools. Oncologist 2020, 25, e231–e242. [Google Scholar] [CrossRef] [Green Version]
- Scaranelo, A.M.; Eiada, R.; Jacks, L.M.; Kulkarni, S.R.; Crystal, P. Accuracy of unenhanced MR imaging in the detection of axillary lymph node metastasis: Study of reproducibility and reliability. Radiology 2012, 262, 425–434. [Google Scholar] [CrossRef] [Green Version]
- van Nijnatten, T.J.A.; Ploumen, E.H.; Schipper, R.J.; Goorts, B.; Andriessen, E.H.; Vanwetswinkel, S.; Schavemaker, M.; Nelemans, P.; de Vries, B.; Beets-Tan, R.G.H.; et al. Routine use of standard breast MRI compared to axillary ultrasound for differentiating between no, limited and advanced axillary nodal disease in newly diagnosed breast cancer patients. Eur. J. Radiol. 2016, 85, 2288–2294. [Google Scholar] [CrossRef]
- Schiaffino, S.; Pinker, K.; Magni, V.; Cozzi, A.; Athanasiou, A.; Baltzer, P.A.T.; Camps Herrero, J.; Clauser, P.; Fallenberg, E.M.; Forrai, G.; et al. Axillary lymphadenopathy at the time of COVID-19 vaccination: Ten recommendations from the European Society of Breast Imaging (EUSOBI). Insights Imaging 2021, 12, 119. [Google Scholar] [CrossRef] [PubMed]



| Characteristic | Women with No or Non-Significant LNM (pN0 or pN1) (n = 368) | Women with Significant LNM (≥pN2) (n = 46) | All Women (n = 414) | |
|---|---|---|---|---|
| Demographic features | ||||
| Age | mean ± SD, years | 59.5 ± 11.1 | 59.6 ± 11.1 | 59.5 ± 11.1 |
| Menopausal status | ||||
| Premenopausal | 92 (25.0) | 16 (3.5) | 108 (26.1) | |
| Postmenopausal | 276 (75.0) | 30 (6.5) | 306 (73.9) | |
| Familial risk | ||||
| Average | 236 (64.1) | 28 (60.9) | 264 (63.8) | |
| Moderate | 72 (19.6) | 8 (17.4) | 80 (19.3) | |
| High | 45 (12.2) | 5 (10.9) | 50 (12.1) | |
| n/a | 15 (4.1) | 5 (10.9) | 20 (4.8) | |
| Characteristics of the newly diagnosed breast cancer | ||||
| Histologic subtype | ||||
| NST | 246 (66.8) | 34 (73.9) | 280 (67.6) | |
| Invasive lobular | 93 (25.3) | 12 (26.1) | 105 (25.4) | |
| Other | 29 (8.0) | - | 29 (7) | |
| Molecular subtype | ||||
| Luminal A | 172 (46.7) | 15 (32.6) | 187 (45.2) | |
| Luminal B | 96 (26.0) | 12 (26.1) | 108 (26.1) | |
| Her2 type | 79 (21.5) | 16 (34.8) | 95 (22.9) | |
| Triple negative | 20 (5.4) | 4 (8.7) | 24 (5.8) | |
| n/a | 3 (0.8) | - | 3 (0.7) | |
| Nuclear grade | ||||
| Low | 45 (12.2) | 1 (2.2) | 46 (11.1) | |
| Intermediate | 245 (66.6) | 27 (58.7) | 272 (65.7) | |
| High | 78 (21.2) | 18 (39.1) | 96 (23.2) | |
| Stage information | ||||
| T-stage | ||||
| T1 | 228 (61.2) | 14 (30.4) | 244 (58.9) | |
| T2 | 111 (30.2) | 15 (32.6) | 126 (30.4) | |
| T3 | 26 (7.1) | 12 (26.1) | 38 (9.2) | |
| T4 | 3 (0.8) | 3 (0.7) | 6 (1.5) | |
| Final N-stage | ||||
| pN0 | 282 (76.6) | - | 282 (68.1) | |
| pN1 | 86 (23.4) | - | 86 (20.8) | |
| pN2 | - | 28 (60.9) | 28 (6.8) | |
| pN3 | - | 18 (3.9) | 18 (4.4) | |
| Significant Nodal Disease Absent | Significant Nodal Disease Present | Total | ||
|---|---|---|---|---|
| pN0 | pN1 | pN2 or Higher | ||
| MRI positive | 3 | 38 | 42 | 83 |
| MRI negative | 279 | 48 | 4 | 331 |
| Total | 282 | 86 | 46 | 414 |
| Test Accuracy Measurements | Diagnosis of Any Nodal Disease (Final Stage >pN0) | Diagnosis of Significant Nodal Disease (Final Stage ≥N2) |
|---|---|---|
| TP (No.) | 80 | 42 |
| FP (No.) | 3 | 41 |
| FN (No.) | 52 | 4 |
| TN (No.) | 279 | 327 |
| Sensitivity | 80/132 (60.6%; 95% CI: 51.7–69.0) | 42/46 (91.3%; 95% CI: 79.2–97.6) |
| Specificity | 279/282 (98.9%; 95% CI: 96.9–99.8) | 327/368 (88.7%; 95% CI: 85.2–91.9) |
| NPV (%) | 279/331 (84.2%; 95% CI: 81.3–86.9) | 327/331 (98.8%; 95% CI: 97.0–99.5) |
| PPV (%) | 80/83 (96.4%; 95% CI: 89.6–98.8) | 42/83 (50.6%; 95% CI: 43.1–58.1) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bode, M.; Schrading, S.; Masoumi, A.; Morscheid, S.; Schacht, S.; Dirrichs, T.; Gaisa, N.; Stickeler, E.; Kuhl, C.K. Abbreviated MRI for Comprehensive Regional Lymph Node Staging during Pre-Operative Breast MRI. Cancers 2023, 15, 1859. https://doi.org/10.3390/cancers15061859
Bode M, Schrading S, Masoumi A, Morscheid S, Schacht S, Dirrichs T, Gaisa N, Stickeler E, Kuhl CK. Abbreviated MRI for Comprehensive Regional Lymph Node Staging during Pre-Operative Breast MRI. Cancers. 2023; 15(6):1859. https://doi.org/10.3390/cancers15061859
Chicago/Turabian StyleBode, Maike, Simone Schrading, Arghavan Masoumi, Stephanie Morscheid, Sabine Schacht, Timm Dirrichs, Nadine Gaisa, Elmar Stickeler, and Christiane K. Kuhl. 2023. "Abbreviated MRI for Comprehensive Regional Lymph Node Staging during Pre-Operative Breast MRI" Cancers 15, no. 6: 1859. https://doi.org/10.3390/cancers15061859






