Efficacy of Different Bacillus of Calmette-Guérin (BCG) Strains on Recurrence Rates among Intermediate/High-Risk Non-Muscle Invasive Bladder Cancers (NMIBCs): Single-Arm Study Systematic Review, Cumulative and Network Meta-Analysis
Abstract
:Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Evidence Acquisition
2.2. Selection of the Studies and Criteria of Inclusion
2.3. Assessment of Quality for Studies Included and Statistical Analysis
3. Results
3.1. Search Results
3.2. Characteristics of The Populations, Study Design, and Location
3.3. BCG-Specific Characteristics: Stains, Schedule, and Dose
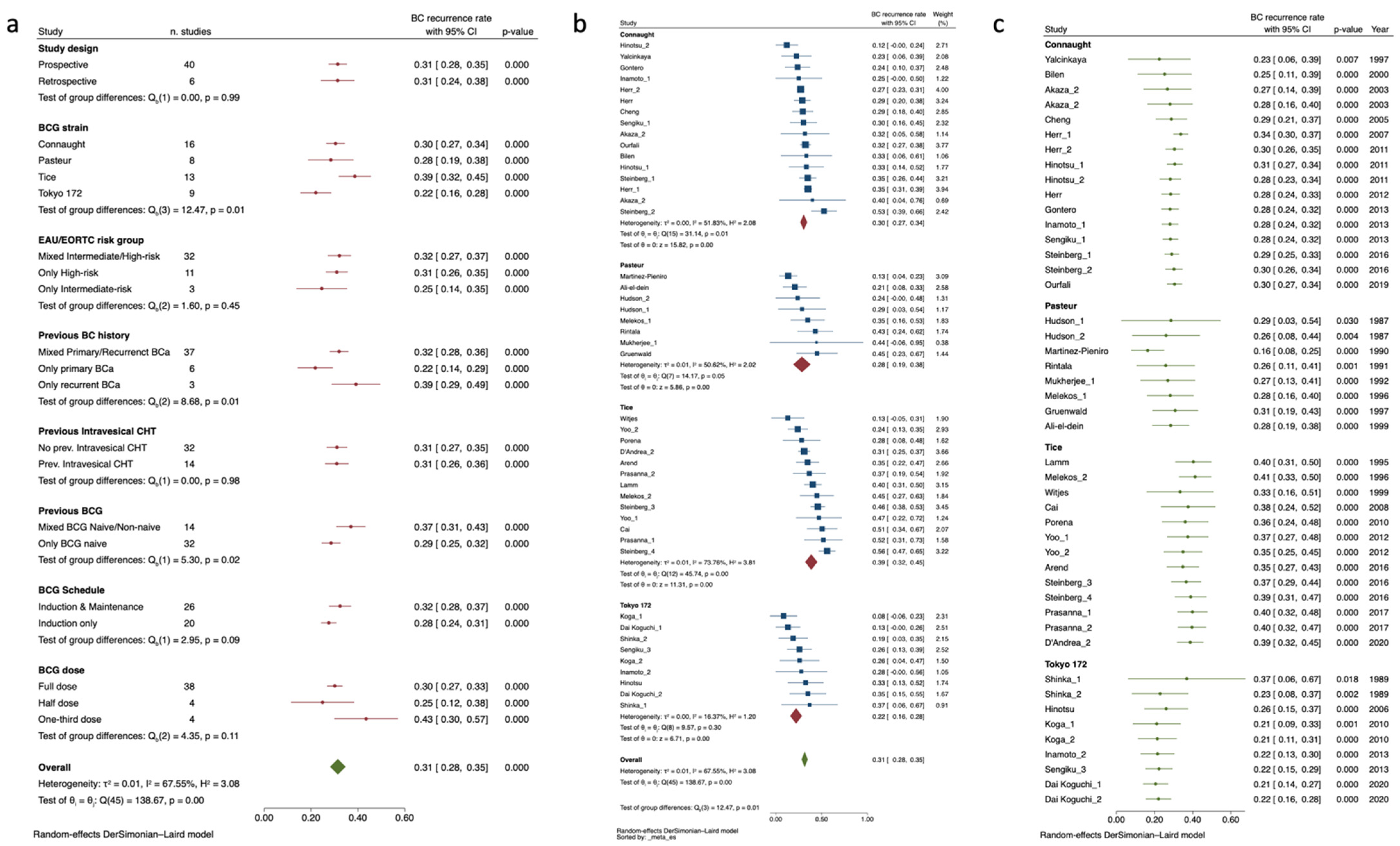
3.3.1. BC Recurrence Rate Meta-Analysis
3.3.2. BC Recurrence Rate by ≤3-y RFS Endpoints and BCG Strain
3.3.3. BC Recurrence Rate for >3-y RFS Endpoint and BCG Strain
3.3.4. Evidence Structure of Network Meta-Analysis for BCG Strain Comparison
3.3.5. Network Meta-Analysis for Risk of BC Recurrence among Intravesical BCG Strains
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Babjuk, M.; Burger, M.; Capoun, O.; Cohen, D.; Compérat, E.M.; Escrig, J.L.D.; Gontero, P.; Liedberg, F.; Masson-Lecomte, A.; Mostafid, A.H.; et al. European Association of Urology Guidelines on Non–muscle-invasive Bladder Cancer (Ta, T1, and Carcinoma in Situ). Eur. Urol. 2021, 81, 75–94. [Google Scholar] [CrossRef]
- Lamm, D.L.; Blumenstein, B.A.; Crissman, J.D.; Montie, J.E.; Gottesman, J.E.; Lowe, B.A.; Sarosdy, M.F.; Bohl, R.D.; Grossman, H.B.; Beck, T.M.; et al. Maintenance bacillus calmette-guerin immunotherapy for recurrent ta, t1 and carcinoma in situ transitional cell carcinoma of the bladder: A randomized southwest oncology group study. J. Urol. 2000, 163, 1124–1129. [Google Scholar] [CrossRef] [PubMed]
- Oddens, J.; Brausi, M.; Sylvester, R.; Bono, A.; van de Beek, C.; van Andel, G.; Gontero, P.; Hoeltl, W.; Turkeri, L.; Marreaud, S.; et al. Final Results of an EORTC-GU Cancers Group Randomized Study of Maintenance Bacillus Calmette-Guérin in Intermediate- and High-risk Ta, T1 Papillary Carcinoma of the Urinary Bladder: One-third Dose Versus Full Dose and 1 Year Versus 3 Years of Maintenance. Eur. Urol. 2013, 63, 462–472. [Google Scholar] [CrossRef] [PubMed]
- Gan, C.; Mostafid, H.; Khan, M.S.; Lewis, D.J. BCG immunotherapy for bladder cancer—The effects of substrain differences. Nat. Rev. Urol. 2013, 10, 580–588, Erratum in Nat. Rev. Urol. 2015, 12, 360. [Google Scholar] [CrossRef] [PubMed]
- Ritz, N.; Hanekom, W.A.; Robins-Browne, R.; Britton, W.J.; Curtis, N. Influence of BCG vaccine strain on the immune response and protection against tuberculosis. FEMS Microbiol. Rev. 2008, 32, 821–841. [Google Scholar] [CrossRef] [PubMed]
- Babjuk, M.; Burger, M.; Compérat, E.; Palou Redorta, J.; van Rhijn, B.; Rouprêt, M.; Shariat, S.; Sylvester, R.; Zigeuner, R.; Gontero, P.; et al. Statement Concerning the Shortage of BCG Vaccine from the EAU Guidelines Panel on Non-Muscle-IInvasive Bladder Cancer. Available online: https://d56bochluxqnz.cloudfront.net/documents/guideline-appendices/non-muscle-invasive-bladder-cancer/Updated-statement-concerning-the-shortage-of-BCG-vaccine-NMIBC-Panel-2018.pdf (accessed on 13 January 2023).
- Angulo, J.C.; Álvarez-Ossorio, J.L.; Domínguez-Escrig, J.L.; Moyano, J.L.; Sousa, A.; Fernández, J.M.; Gómez-Veiga, F.; Unda, M.; Carballido, J.; Carrero, V.; et al. Hyperthermic Mitomycin C in Intermediate-risk Non–muscle-invasive Bladder Cancer: Results of the HIVEC-1 Trial. Eur. Urol. Oncol. 2022, 6, 58–66. [Google Scholar] [CrossRef] [PubMed]
- Carrion, D.; Pradere, B.; Soria, F.; del Giudice, F.; Moschini, M. Editorial commentary on: “Reduced vs full-dose BCG therapy in bladder cancer: A systematic review and meta-analysis”. Actas Urol. Esp. 2022, 47, S2173–S5786. [Google Scholar] [CrossRef]
- Boehm, B.E.; Cornell, J.E.; Wang, H.; Mukherjee, N.; Oppenheimer, J.S.; Svatek, R.S. Efficacy of bacillus Calmette-Guérin Strains for Treatment of Nonmuscle Invasive Bladder Cancer: A Systematic Review and Network Meta-Analysis. J. Urol. 2017, 198, 503–510. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef] [Green Version]
- National Heart, Lung, and Blood Institute (NHLBI). Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 23 February 2022).
- Higgins, J.P.T.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Duval, S.; Tweedie, R. Trim and Fill: A Simple Funnel-Plot-Based Method of Testing and Adjusting for Publication Bias in Meta-Analysis. Biometrics 2000, 56, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Huang, Z.; Liu, H.; Wang, Y.; Zhang, C.; Xu, T. Determining optimal maintenance schedules for adjuvant intravesical bacillus Calmette–Guerin immunotherapy in non-muscle-invasive bladder cancer: A systematic review and network meta-analysis. Curr. Med. Res. Opin. 2017, 33, 1379–1387. [Google Scholar] [CrossRef] [PubMed]
- Busetto, G.; Del Giudice, F.; De Berardinis, E.; Sperduti, I.; Ferro, M.; Maggi, M.; Gross, M.; Sciarra, A.; Eisenberg, M. A systematic review and meta-analysis of clinical trials implementing aromatase inhibitors to treat male infertility. Asian J. Androl. 2020, 22, 360–367. [Google Scholar] [CrossRef] [PubMed]
- Del Del Giudice, F.; Pecoraro, M.; Vargas, H.A.; Cipollari, S.; De Berardinis, E.; Bicchetti, M.; Chung, B.I.; Catalano, C.; Narumi, Y.; Catto, J.W.F.; et al. Systematic Review and Meta-Analysis of Vesical Imaging-Reporting and Data System (VI-RADS) Inter-Observer Reliability: An Added Value for Muscle Invasive Bladder Cancer Detection. Cancers 2020, 12, 2994. [Google Scholar] [CrossRef]
- Del Giudice, F.; Kasman, A.M.; De Berardinis, E.; Busetto, G.M.; Belladelli, F.; Eisenberg, M.L. Association between male infertility and male-specific malignancies: Systematic review and meta-analysis of population-based retrospective cohort studies. Fertil. Steril. 2020, 114, 984–996. [Google Scholar] [CrossRef]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Lu, G.; Ades, A.E. Combination of direct and indirect evidence in mixed treatment comparisons. Stat. Med. 2004, 23, 3105–3124. [Google Scholar] [CrossRef]
- Salanti, G.; Ades, A.E.; Ioannidis, J.P. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: An overview and tutorial. J. Clin. Epidemiol. 2011, 64, 163–171. [Google Scholar] [CrossRef]
- Spiegelhalter, D.J.; Best, N.G.; Carlin, B.P.; Van Der Linde, A. Bayesian measures of model complexity and fit. J. R. Stat. Soc. Ser. B (Stat. Methodol.) 2002, 64, 583–639. [Google Scholar] [CrossRef] [Green Version]
- Song, F.; Altman, D.G.; Glenny, A.-M.; Deeks, J.J. Validity of indirect comparison for estimating efficacy of competing interventions: Empirical evidence from published meta-analyses. BMJ 2003, 326, 472. [Google Scholar] [CrossRef] [Green Version]
- Agrawal, M.S.; Agrawal, M.; Bansal, S.; Agarwal, M.; Lavania, P.; Goyal, J. The Safety and Efficacy of Different Doses of Bacillus Calmette Guérin in Superficial Bladder Transitional Cell Carcinoma. Urology 2007, 70, 1075–1078. [Google Scholar] [CrossRef] [PubMed]
- Ali-El-Dein, B.; Nabeeh, A.; Ismail, E.-H.; Ghoneim, M.A. Sequential bacillus calmette-guerin and epirubicin versus bacillus calmette-guerin alone for superficial bladder tumors: A randomized prospective study. J. Urol. 1999, 162, 339–342. [Google Scholar] [CrossRef] [PubMed]
- Arends, T.J.; Nativ, O.; Maffezzini, M.; de Cobelli, O.; Canepa, G.; Verweij, F.; Moskovitz, B.; van der Heijden, A.G.; Witjes, J.A. Results of a Randomised Controlled Trial Comparing Intravesical Chemohyperthermia with Mitomycin C Versus Bacillus Calmette-Guérin for Adjuvant Treatment of Patients with Intermediate- and High-risk Non–Muscle-invasive Bladder Cancer. Eur. Urol. 2016, 69, 1046–1052. [Google Scholar] [CrossRef] [PubMed]
- Bilen, C.Y.; Özen, H.; Aki, F.T.; Aygün, C.; Ekici, S.; Kendi, S. Clinical experience with BCG alone versus BCG plus epirubicin. Int. J. Urol. 2000, 7, 206–209. [Google Scholar] [CrossRef] [PubMed]
- Brosman, S.A.; Brosman, S.A. Experience with Bacillus Calmette-Guerin in Patients with Superficial Bladder Carcinoma. J. Urol. 1982, 128, 27–30. [Google Scholar] [CrossRef]
- Cai, T.; Nesi, G.; Tinacci, G.; Zini, E.; Mondaini, N.; Boddi, V.; Mazzoli, S.; Bartoletti, R. Can Early Single Dose Instillation of Epirubicin Improve Bacillus Calmette-Guerin Efficacy in Patients With Nonmuscle Invasive High Risk Bladder Cancer? Results From a Prospective, Randomized, Double-Blind Controlled Study. J. Urol. 2008, 180, 110–115. [Google Scholar] [CrossRef]
- Cheng, C.W.; Chan, S.F.P.; Chan, L.W.; Chan, C.K.; Ng, C.F.; Cheung, H.Y.; Chan, S.Y.E.; Wong, W.S.; Lai, F.M.-M.; To, K.F.; et al. Twelve-year follow up of a randomized prospective trial comparing bacillus Calmette-Guerin and epirubicin as adjuvant therapy in superficial bladder cancer. Int. J. Urol. 2005, 12, 449–455. [Google Scholar] [CrossRef]
- D’Andrea, D.; Soria, F.; Abufaraj, M.; Pones, M.; Gontero, P.; Machado, A.T.; Waksman, R.; Enikeev, D.V.; Glybochko, P.V.; Adonias, S.P.; et al. Comparative Effectiveness of Intravesical BCG-Tice and BCG-Moreau in Patients with Non–muscle-invasive Bladder Cancer. Clin. Genitourin. Cancer 2019, 18, 20–25.e2. [Google Scholar] [CrossRef] [Green Version]
- Koguchi, D.; Matsumoto, K.; Hirayama, T.; Moroo, S.; Kobayashi, M.; Katsumata, H.; Ikeda, M.; Iwamura, M. Impact of maintenance therapy using a half dose of the bacillus Calmette–Guérin Tokyo strain on recurrence of intermediate and high-risk nonmuscle invasive bladder cancer: A retrospective single-center study. BMC Urol. 2020, 20, 194. [Google Scholar] [CrossRef]
- Del Giudice, F.; Busetto, G.M.; Gross, M.S.; Maggi, M.; Sciarra, A.; Salciccia, S.; Ferro, M.; Sperduti, I.; Flammia, S.; Canale, V.; et al. Efficacy of three BCG strains (Connaught, TICE and RIVM) with or without secondary resection (re-TUR) for intermediate/high-risk non-muscle-invasive bladder cancers: Results from a retrospective single-institution cohort analysis. J. Cancer Res. Clin. Oncol. 2021, 147, 3073–3080. [Google Scholar] [CrossRef]
- Del Giudice, F.; Flammia, R.S.; Chung, B.I.; Moschini, M.; Pradere, B.; Mari, A.; Soria, F.; Albisinni, S.; Krajewski, W.; Szydełko, T.; et al. Compared Efficacy of Adjuvant Intravesical BCG-TICE vs. BCG-RIVM for High-Risk Non-Muscle Invasive Bladder Cancer (NMIBC): A Propensity Score Matched Analysis. Cancers 2022, 14, 887. [Google Scholar] [CrossRef] [PubMed]
- De Reijke, T.M.; Kurth, K.H.; Sylvester, R.J.; Hall, R.R.; Brausi, M.; Van De Beek, K.; Landsoght, K.E.J.; Carpentier, P.; European Organization for the Research and Treatment of Cancer-Genito-Urinary Group. Bacillus calmette-guerin versus epirubicin for primary, secondary or concurrent carcinoma in situ of the bladder: Results of a european organization for the research and treatment of cancer—Genito-urinary group phase iii trial (30906). J. Urol. 2005, 173, 405–409. [Google Scholar] [CrossRef] [PubMed]
- Di Lorenzo, G.; Perdonà, S.; Damiano, R.; Faiella, A.; Cantiello, F.; Pignata, S.; Ascierto, P.; Simeone, E.; De Sio, M.; Autorino, R. Gemcitabine versus bacille Calmette-Guérin after initial bacille Calmette-Guérin failure in non-muscle-invasive bladder cancer. Cancer 2010, 116, 1893–1900. [Google Scholar] [CrossRef] [PubMed]
- Di Stasi, S.M.; Giannantoni, A.; Giurioli, A.; Valenti, M.; Zampa, G.; Storti, L.; Attisani, F.; De Carolis, A.; Capelli, G.; Vespasiani, G.; et al. Sequential BCG and electromotive mitomycin versus BCG alone for high-risk superficial bladder cancer: A randomised controlled trial. Lancet Oncol. 2006, 7, 43–51. [Google Scholar] [CrossRef] [Green Version]
- Farah, N.B.; Ghanem, R.; Amr, M. Treatment efficacy and tolerability of intravesical Bacillus Calmette-Guerin (BCG)—RIVM strain: Induction and maintenance protocol in high grade and recurrent low grade non-muscle invasive bladder cancer (NMIBC). BMC Urol. 2014, 14, 11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Friedrich, M.G.; Pichlmeier, U.; Schwaibold, H.; Conrad, S.; Huland, H. Long-Term Intravesical Adjuvant Chemotherapy Further Reduces Recurrence Rate Compared with Short-Term Intravesical Chemotherapy and Short-Term Therapy with Bacillus Calmette-Guérin (BCG) in Patients with Non–Muscle-Invasive Bladder Carcinoma. Eur. Urol. 2007, 52, 1123–1130. [Google Scholar] [CrossRef] [PubMed]
- Gontero, P.; Oderda, M.; Mehnert, A.; Gurioli, A.; Marson, F.; Lucca, I.; Rink, M.; Schmid, M.; Kluth, L.A.; Pappagallo, G.; et al. The Impact of Intravesical Gemcitabine and 1/3 Dose Bacillus Calmette-Guérin Instillation Therapy on the Quality of Life in Patients with Nonmuscle Invasive Bladder Cancer: Results of a Prospective, Randomized, Phase II Trial. J. Urol. 2013, 190, 857–862. [Google Scholar] [CrossRef]
- Gruenwald, I.E.; Stein, A.; Rashcovitsky, R.; Shifroni, G.; Lurie, A. A 12 versus 6-week course of bacillus Calmette-Guerin prophylaxis for the treatment of high risk superficial bladder cancer. J. Urol. 1997, 157, 487–491. [Google Scholar] [CrossRef]
- Hemdan, T.; Johansson, R.; Jahnson, S.; Hellström, P.; Tasdemir, I.; Malmström, P.-U.; Members of the Urothelial Cancer Group of the Nordic Association of Urology. 5-Year Outcome of a Randomized Prospective Study Comparing bacillus Calmette-Guérin with Epirubicin and Interferon-α2b in Patients with T1 Bladder Cancer. J. Urol. 2014, 191, 1244–1249. [Google Scholar] [CrossRef]
- Herr, H.W. Intravesical Bacillus Calmette-Guérin Outcomes in Patients With Bladder Cancer and Asymptomatic Bacteriuria. J. Urol. 2012, 187, 435–437. [Google Scholar] [CrossRef]
- Herr, H.W.; Dalbagni, G.; Donat, S.M. Bacillus Calmette-Guérin Without Maintenance Therapy for High-Risk Non–Muscle-Invasive Bladder Cancer. Eur. Urol. 2011, 60, 32–36. [Google Scholar] [CrossRef] [PubMed]
- Herr, H.W. Age and Outcome of Superficial Bladder Cancer Treated with Bacille Calmette-Guérin Therapy. Urology 2007, 70, 65–68. [Google Scholar] [CrossRef] [PubMed]
- Hinotsu, S.; Akaza, H.; Naito, S.; Ozono, S.; Sumiyoshi, Y.; Noguchi, S.; Yamaguchi, A.; Nagamori, S.; Terai, A.; Nasu, Y.; et al. Maintenance therapy with bacillus Calmette-Guérin Connaught strain clearly prolongs recurrence-free survival following transurethral resection of bladder tumour for non-muscle-invasive bladder cancer. BJU Int. 2010, 108, 187–195. [Google Scholar] [CrossRef]
- Hinotsu, S.; Akaza, H.; Isaka, S.; Kanetake, H.; Kubota, Y.; Kuroda, M.; Shinohara, N.; Shinka, T.; Tachibana, M.; Naito, S.; et al. Sustained prophylactic effect of intravesical bacille Calmette-Guérin for superficial bladder cancer: A smoothed hazard analysis in a randomized prospective study. Urology 2006, 67, 545–549. [Google Scholar] [CrossRef] [PubMed]
- Hudson, M.A.; Ratliff, T.L.; Gillen, D.P.; Haaff, E.O.; Dresner, S.M.; Catalona, W.J. Single Course Versus Maintenance Bacillus Calmette-Guerin Therapy for Superficial Bladder Tumors: A Prospective, Randomized Trial. J. Urol. 1987, 138, 295–298. [Google Scholar] [CrossRef]
- Ibrahiem, E.-H.I.; Ghoneim, M.A.; Nigam, V.; Brailovsky, C.; Elhilali, M.M. Prophylactic Maltose Tetrapalmitate and Bacillus Calmette-Guerin Immunotherapy of Recurrent Superficial Bladder Tumors: Preliminary Report. J. Urol. 1988, 140, 498–500. [Google Scholar] [CrossRef] [PubMed]
- Inamoto, T.; Ubai, T.; Nishida, T.; Fujisue, Y.; Katsuoka, Y.; Azuma, H. Comparable effect with minimal morbidity of low-dose Tokyo 172 strain compared with regular dose Connaught strain as an intravesical bacillus Calmette-Guérin prophylaxis in nonmuscle invasive bladder cancer: Results of a randomized prospective comparison. Urol. Ann. 2013, 5, 7–12. [Google Scholar] [CrossRef]
- Järvinen, R.; Kaasinen, E.; Sankila, A.; Rintala, E.; FinnBladder Group. Long-term Efficacy of Maintenance Bacillus Calmette-Guérin versus Maintenance Mitomycin C Instillation Therapy in Frequently Recurrent TaT1 Tumours without Carcinoma In Situ: A Subgroup Analysis of the Prospective, Randomised FinnBladder I Study with a 20-Year Follow-up. Eur. Urol. 2009, 56, 260–265. [Google Scholar] [CrossRef]
- Kamat, M.; Kulkarni, J.; Tongaonkar, H.; Dalal, A. Intravesical Bacillus Calmette-Guerin For Superficial Bladder Cancer: Experience With Danish 1331 Strain. J. Urol. 1994, 152, 1424–1428. [Google Scholar] [CrossRef]
- Koga, H.; Ozono, S.; Tsushima, T.; Tomita, K.; Horiguchi, Y.; Usami, M.; Hirao, Y.; Akaza, H.; Naito, S. BCG Tokyo Strain Study Group Maintenance intravesical bacillus Calmette-Guérin instillation for Ta, T1 cancer and carcinoma in situ of the bladder: Randomized controlled trial by the BCG Tokyo Strain Study Group. Int. J. Urol. 2010, 17, 759–766. [Google Scholar] [CrossRef]
- Lamm, D.L.; Blumenstein, B.A.; Crawford, E.D.; Crissman, J.D.; Lowe, B.A.; Smith, J.A.; Sarosdy, M.F.; Schellhammer, P.F.; Sagalowsky, A.I.; Messing, E.M.; et al. Randomized intergroup comparison of bacillus calmette-guerin immunotherapy and mitomycin C chemotherapy prophylaxis in superficial transitional cell carcinoma of the bladder a southwest oncology group study. Urol. Oncol. Semin. Orig. Investig. 1995, 1, 119–126. [Google Scholar] [CrossRef]
- Martínez-Piñeiro, J.; Flores, N.; Isorna, S.; Solsona, E.; Sebastián, J.; Pertusa, C.; Rioja, L.; Vela, R.; Camacho, J.; Nogueira, J.; et al. Long-term follow-up of a randomized prospective trial comparing a standard 81 mg dose of intravesical bacille Calmette-Guérin with a reduced dose of 27 mg in superficial bladder cancer. BJU Int. 2002, 89, 671–680. [Google Scholar] [CrossRef] [PubMed]
- Piñeiro, J.A.M.; León, J.J.; Piñeiro, L.M.; Fiter, L.; Mosteiro, J.A.; Navarro, J.; Matres, M.J.G.; Cárcamo, P. Bacillus Calmette-Guerin Versus Doxorubicin Versus Thiotepa: A Randomized Prospective Study in 202 Patients with Superficial Bladder Cancer. J. Urol. 1990, 143, 502–506. [Google Scholar] [CrossRef] [PubMed]
- Marttila, T.; Järvinen, R.; Liukkonen, T.; Rintala, E.; Boström, P.; Seppänen, M.; Tammela, T.; Hellström, P.; Aaltomaa, S.; Leskinen, M.; et al. Intravesical Bacillus Calmette-Guérin Versus Combination of Epirubicin and Interferon-α2a in Reducing Recurrence of Non–Muscle-invasive Bladder Carcinoma: FinnBladder-6 Study. Eur. Urol. 2016, 70, 341–347. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Melekos, M.D.; Zarakovitis, I.; Dandinis, K.; Fokaefs, E.; Chionis, H.; Dauaher, H.; Barbalias, G. BCG versus epirubicin in the prophylaxis of multiple superficial bladder tumours: Results of a prospective randomized study using modified treatment schemes. Int. Urol. Nephrol. 1996, 28, 499–509. [Google Scholar] [CrossRef]
- Mukherjee, A.; Persad, R.; Smith, P.J.B. Intravesical BCG Treatment for Superficial Bladder Cancer: Long-term Results using Two Different Strains of BCG. BJU Int. 1992, 69, 147–150. [Google Scholar] [CrossRef]
- Nowak, Ł.; Krajewski, W.; Moschini, M.; Chorbińska, J.; Poletajew, S.; Tukiendorf, A.; Muilwijk, T.; Joniau, S.; Tafuri, A.; Antonelli, A.; et al. Assessment of the oncological outcomes of three different bacillus Calmette–Guérin strains in patients with high-grade T1 non-muscle-invasive bladder cancer. Arab. J. Urol. 2021, 19, 78–85. [Google Scholar] [CrossRef]
- Ojea, A.; Nogueira, J.L.; Solsona, E.; Flores, N.; Gómez, J.M.F.; Molina, J.R.; Chantada, V.; Camacho, J.E.; Piñeiro, L.M.; Rodríguez, R.H.; et al. A Multicentre, Randomised Prospective Trial Comparing Three Intravesical Adjuvant Therapies for Intermediate-Risk Superficial Bladder Cancer: Low-Dose Bacillus Calmette-Guerin (27 mg) versus Very Low-Dose Bacillus Calmette-Guerin (13.5 mg) versus Mitomycin C. Eur. Urol. 2007, 52, 1398–1406. [Google Scholar] [CrossRef]
- Okamura, T.; Akita, H.; Ando, R.; Ikegami, Y.; Naiki, T.; Kawai, N.; Tozawa, K.; Kohri, K. Single monthly bacillus Calmette-Guérin intravesical instillation is effective maintenance therapy to prevent recurrence in Japanese patients with non-muscle-invasive bladder cancer. Int. J. Clin. Oncol. 2011, 17, 477–481. [Google Scholar] [CrossRef]
- Oosterlinck, W.; Kirkali, Z.; Sylvester, R.; da Silva, F.C.; Busch, C.; Algaba, F.; Collette, S.; Bono, A. Sequential Intravesical Chemoimmunotherapy with Mitomycin C and Bacillus Calmette-Guérin and with Bacillus Calmette-Guérin Alone in Patients with Carcinoma in Situ of the Urinary Bladder: Results of an EORTC Genito-Urinary Group Randomized Phase 2 Trial (30993). Eur. Urol. 2011, 59, 438–446. [Google Scholar] [CrossRef]
- Ourfali, S.; Ohannessian, R.; Fassi-Fehri, H.; Pages, A.; Badet, L.; Colombel, M. Recurrence Rate and Cost Consequence of the Shortage of Bacillus Calmette-Guérin Connaught Strain for Bladder Cancer Patients. Eur. Urol. Focus 2019, 7, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Palou, J.; Laguna, P.; Millán-Rodríguez, F.; Hall, R.R.; Salvador-Bayarri, J.; Vicente-Rodríguez, J. Control group and maintenance treatment with bacillus Calmette-Guerin for carcinoma in situ and/or high grade bladder tumors. J. Urol. 2001, 165, 1488. [Google Scholar] [CrossRef] [PubMed]
- Porena, M.; Del Zingaro, M.; Lazzeri, M.; Mearini, L.; Giannantoni, A.; Bini, V.; Costantini, E. Bacillus Calmette-Guérin versus Gemcitabine for Intravesical Therapy in High-Risk Superficial Bladder Cancer: A Randomised Prospective Study. Urol. Int. 2010, 84, 23–27. [Google Scholar] [CrossRef] [PubMed]
- Prasanna, T.; Craft, P.; Balasingam, G.; Haxhimolla, H.; Pranavan, G. Intravesical Gemcitabine versus Intravesical Bacillus Calmette–Guérin for the Treatment of Non-Muscle Invasive Bladder Cancer: An Evaluation of Efficacy and Toxicity. Front. Oncol. 2017, 7, 260. [Google Scholar] [CrossRef] [Green Version]
- Rentsch, C.A.; Birkhäuser, F.D.; Biot, C.; Gsponer, J.R.; Bisiaux, A.; Wetterauer, C.; Lagranderie, M.; Marchal, G.; Orgeur, M.; Bouchier, C.; et al. Bacillus Calmette-Guérin Strain Differences Have an Impact on Clinical Outcome in Bladder Cancer Immunotherapy. Eur. Urol. 2014, 66, 677–688. [Google Scholar] [CrossRef]
- Rintala, E.; Jauhiainen, K.; Alfthan, O.; Hansson, E.; Juusela, H.; Kanerva, K.; Korhonen, H.; Permi, J.; Sotarauta, M.; Vaalasti, T.; et al. Intravesical Chemotherapy (Mitomycin C) versus Immunotherapy (Bacillus Calmette-Guérin) in Superficial Bladder Cancer. Eur. Urol. 1991, 20, 19–25. [Google Scholar] [CrossRef]
- Sekine, H.; Ohya, K.; Kojima, S.-I.; Igarashi, K.; Fukui, I. Equivalent efficacy of mitomycin C plus doxorubicin instillation to bacillus Calmette-Guerin therapy for carcinoma in situ of the bladder. Int. J. Urol. 2001, 8, 483–486. [Google Scholar] [CrossRef] [Green Version]
- Sengiku, A.; Ito, M.; Miyazaki, Y.; Sawazaki, H.; Takahashi, T.; Ogura, K. A Prospective Comparative Study of Intravesical Bacillus Calmette-Guérin Therapy with the Tokyo or Connaught Strain for Nonmuscle Invasive Bladder Cancer. J. Urol. 2013, 190, 50–54. [Google Scholar] [CrossRef]
- Shinka, T.; Matsumoto, M.; Ogura, H.; Hirano, A.; Ohkawa, T. Recurrence of Primary Superficial Bladder Cancer Treated with Prophylactic Intravesical Tokyo 172 Bacillus Calmette-Guerin: A Long-Term Follow-up. Int. J. Urol. 1997, 4, 139–143. [Google Scholar] [CrossRef]
- Shinka, T.; Hirano, A.; Uekado, Y.; Kyoku, I.; Aoshi, H.; Ohkawa, T. Intravesical Bacillus Calmette-Guérin Treatment for Superficial Bladder Tumours. BJU Int. 1989, 63, 610–615. [Google Scholar] [CrossRef]
- Sood, R.; Sharma, H.; Sharma, B.; Parekh, S.; Pujari, P.; Shewale, S. A prospective comparative study to assess the efficacy and tolerability of 2 different doses of intravesical bacillus Calmette-Guerin (BCG) in patients with non–muscle-invasive bladder cancer. Urol. Oncol. Semin. Orig. Investig. 2020, 38, 433–439. [Google Scholar] [CrossRef] [PubMed]
- Steinberg, R.L.; Brooks, N.A.; Thomas, L.J.; Mott, S.L.; O’Donnell, M.A. Bacillus Calmette-Guerin strain may not effect recurrence-free survival when used intravesically with interferon-alpha2b for non–muscle-invasive bladder cancer. Urol. Oncol. Semin. Orig. Investig. 2017, 35, 201–207. [Google Scholar] [CrossRef] [PubMed]
- Sylvester, R.J.; Brausi, M.A.; Kirkels, W.J.; Hoeltl, W.; Da Silva, F.C.; Powell, P.H.; Prescott, S.; Kirkali, Z.; van de Beek, C.; Gorlia, T.; et al. Long-Term Efficacy Results of EORTC Genito-Urinary Group Randomized Phase 3 Study 30911 Comparing Intravesical Instillations of Epirubicin, Bacillus Calmette-Guérin, and Bacillus Calmette-Guérin plus Isoniazid in Patients with Intermediate- and High-Risk Stage Ta T1 Urothelial Carcinoma of the Bladder. Eur. Urol. 2010, 57, 766–773. [Google Scholar] [CrossRef] [Green Version]
- Takashi, M.; Katsuno, S.; Yuba, H.; Ohshima, S.; Wakai, K.; Ohno, Y. Possible factors affecting response to intravesical bacillus Calmette-Guérin (Tokyo 172 Strain) therapy for carcinoma in situ of the bladder: A multivariate analysis. Int. Urol. Nephrol. 1998, 30, 713–722. [Google Scholar] [CrossRef] [PubMed]
- Takashi, M.; Shimoji, T.; Murase, T.; Sakata, T.; Sobajima, T.; Suzuki, Y. Intravesical bacillus Calmette-Guérin (Tokyo 172 strain) therapy for carcinoma in situ of the bladder. Int. Urol. Nephrol. 1997, 29, 557–563. [Google Scholar] [CrossRef]
- Witjes, J.A.; Dalbagni, G.; Karnes, R.J.; Shariat, S.; Joniau, S.; Palou, J.; Serretta, V.; Larré, S.; di Stasi, S.; Colombo, R.; et al. The efficacy of BCG TICE and BCG Connaught in a cohort of 2099 patients with T1G3 non–muscle-invasive bladder cancer. Urol. Oncol. Semin. Orig. Investig. 2016, 34, 484.e19–484.e25. [Google Scholar] [CrossRef] [Green Version]
- Witjes, W.P.; König, M.; Boeminghaus, F.P.; Hall, R.R.; Schulman, C.C.; Zurlo, M.; Fittipaldo, A.; Riggi, M.; Debruyne, F.M. Results of a European Comparative Randomized Study Comparing Oral Bropirimine versus Intravesical BCG Treatment in BCG-Naive Patients with Carcinoma in situ of the Urinary Bladder. Eur. Urol. 1999, 36, 576–581. [Google Scholar] [CrossRef]
- Yalçinkaya, F.; Kamiş, L.; Özteke, O.; Günlüsoy, B.; Yiĝitbasi, O.; Ünal, S. Prospective randomized comparison of intravesical BCG therapy with standard dose versus low doses in superficial bladder cancer. Int. Urol. Nephrol. 1998, 30, 41–44. [Google Scholar] [CrossRef] [PubMed]
- Peyromaure, M.; Guérin, F.; Amsellem-Ouazana, D.; Saighi, D.; Debre, B.; Zerbib, M. Intravesical Bacillus Calmette-Guerin Therapy for Stage T1 Grade 3 Transitional Cell Carcinoma of the Bladder: Recurrence, Progression and Survival in a Study of 57 Patients. J. Urol. 2003, 169, 2110–2112. [Google Scholar] [CrossRef]
- Yoo, K.H.; Lim, T.J.; Chang, S.-G. Monthly intravesical bacillus Calmette-Guérin maintenance therapy for non-muscle-invasive bladder cancer: 10-year experience in a single institute. Exp. Ther. Med. 2011, 3, 221–225. [Google Scholar] [CrossRef] [Green Version]
- Shelley, M.; Kynaston, H.G.; Court, J.B.; Wilt, T.J.; Coles, B.; Burgon, K.; Mason, M.D. A systematic review of intravesical bacillus Calmette-Guérin plus transurethral resection vs transurethral resection alone in Ta and T1 bladder cancer. BJU Int. 2001, 88, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Shelley, M.; Wilt, T.; Court, J.; Coles, B.; Kynaston, H.; Mason, M. Intravesical bacillus Calmette-Guerin is superior to mitomycin C in reducing tumour recurrence in high-risk superficial bladder cancer: A meta-analysis of randomized trials. BJU Int. 2004, 93, 485–490. [Google Scholar] [CrossRef] [PubMed]
- Malmström, P.-U.; Sylvester, R.J.; Crawford, D.E.; Friedrich, M.; Krege, S.; Rintala, E.; Solsona, E.; Di Stasi, S.M.; Witjes, J.A. An Individual Patient Data Meta-Analysis of the Long-Term Outcome of Randomised Studies Comparing Intravesical Mitomycin C versus Bacillus Calmette-Guérin for Non–Muscle-Invasive Bladder Cancer. Eur. Urol. 2009, 56, 247–256. [Google Scholar] [CrossRef] [Green Version]
- Duchek, M.; Johansson, R.; Jahnson, S.; Mestad, O.; Hellström, P.; Hellsten, S.; Malmström, P.-U.; Members of the Urothelial Cancer Group of the Nordic Association of Urology. Bacillus Calmette-Guérin Is Superior to a Combination of Epirubicin and Interferon-α2b in the Intravesical Treatment of Patients with Stage T1 Urinary Bladder Cancer. A Prospective, Randomized, Nordic Study. Eur. Urol. 2010, 57, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Grimm, M.-O.; van der Heijden, A.G.; Colombel, M.; Muilwijk, T.; Martínez-Piñeiro, L.; Babjuk, M.M.; Türkeri, L.N.; Palou, J.; Patel, A.; Bjartell, A.S.; et al. Treatment of High-grade Non–muscle-invasive Bladder Carcinoma by Standard Number and Dose of BCG Instillations Versus Reduced Number and Standard Dose of BCG Instillations: Results of the European Association of Urology Research Foundation Randomised Phase III Clinical Trial “NIMBUS”. Eur. Urol. 2020, 78, 690–698. [Google Scholar] [CrossRef] [PubMed]
- Jiang, S.; Redelman-Sidi, G. BCG in Bladder Cancer Immunotherapy. Cancers 2022, 14, 3073. [Google Scholar] [CrossRef] [PubMed]
- Moon, Y.J.; Cho, K.S.; Jeong, J.Y.; Chung, D.Y.; Kang, D.H.; Jung, H.D.; Lee, J.Y. Effects of intravesical BCG maintenance therapy duration on recurrence rate in high-risk non-muscle invasive bladder cancer (NMIBC): Systematic review and network meta-analysis according to EAU COVID-19 recommendations. PLoS ONE 2022, 17, e0273733. [Google Scholar] [CrossRef] [PubMed]
- Panebianco, V.; Pecoraro, M.; Del Giudice, F.; Takeuchi, M.; Muglia, V.F.; Messina, E.; Cipollari, S.; Giannarini, G.; Catalano, C.; Narumi, Y. VI-RADS for Bladder Cancer: Current Applications and Future Developments. J. Magn. Reson. Imaging 2020, 55, 23–36. [Google Scholar] [CrossRef]
- Panebianco, V.; Del Giudice, F.; Leonardo, C.; Sciarra, A.; Catalano, C.; Catto, J.W. VI-RADS Scoring Criteria for Alternative Risk-adapted Strategies in the Management of Bladder Cancer During the COVID-19 Pandemic. Eur. Urol. 2020, 78, e18–e20. [Google Scholar] [CrossRef]
- Nicolazzo, C.; Busetto, G.M.; Del Giudice, F.; Sperduti, I.; Giannarelli, D.; Gradilone, A.; Gazzaniga, P.; de Berardinis, E.; Raimondi, C. The long-term prognostic value of survivin expressing circulating tumor cells in patients with high-risk non-muscle invasive bladder cancer (NMIBC). J. Cancer Res. Clin. Oncol. 2017, 143, 1971–1976. [Google Scholar] [CrossRef]
- Kamat, A.M.; Sylvester, R.J.; Böhle, A.; Palou, J.; Lamm, D.L.; Brausi, M.; Soloway, M.; Persad, R.; Buckley, R.; Colombel, M.; et al. Definitions, End Points, and Clinical Trial Designs for Non–Muscle-Invasive Bladder Cancer: Recommendations From the International Bladder Cancer Group. J. Clin. Oncol. 2016, 34, 1935–1944. [Google Scholar] [CrossRef] [PubMed]


| Study Author | Year | Study Design | Sample Size (n) | Median Age (yr) | Male Gender (%) | EAU Risk Group | Previous BC History | BCG Strain | BCG Schedule | BCG Dose | Previous BCG | Follow-Up (mo) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Agrawal [23] | 2007 | Prospective | 128 | 64.5 | 71.8 | Only Intermediate | Primary /Recurrent | Danish 1331 | Induction & Maintenance | Full Dose vs. one-third Dose | Naïve | 36 |
| Ali-el-dein [24] | 1999 | Prospective | 58 | 58.5 | 72.4 | Intermediate/ High-risk | Primary /Recurrent | Pasteur | Induction & Maintenance | Full Dose | Naïve | 30 |
| Arend [25] | 2016 | Prospective | 190 | 67.4 | 84.2 | Intermediate/ High-risk | Primary /Recurrent | Tice | Induction & Maintenance | Full Dose | Naïve & Recurrent | 24 |
| Bilen [26] | 2000 | Prospective | 21 | 53 | 95.2 | Only High-risk | Primary /Recurrent | Connaught | Induction only | Full Dose | Naïve | 18 |
| Brosman [27] | 1982 | Prospective | 39 | 63.4 | 73.7 | Intermediate/ High-risk | Recurrent only | Tice | Induction & Maintenance | Full Dose | Recurrent | 24 |
| Cai [28] | 2008 | Prospective | 81 | 69.8 | 86.4 | Only High-risk | Recurrent only | Tice | Induction & Maintenance | Full Dose | Naïve & Recurrent | 15 |
| Cheng [29] | 2005 | Prospective | 102 | 70.1 | 71.5 | Intermediate/ High-risk | Primary /Recurrent | Connaught | Induction & Maintenance | Full Dose | Naïve | 23 |
| D’Andrea [30] | 2020 | Retrospective | 660 | 63 | 89.7 | Intermediate/ High-risk | Primary /Recurrent | Moreau/Tice | Induction & Maintenance | Full Dose | Naïve & Recurrent | 41 |
| Dai Koguchi [31] | 2020 | Retrospective | 78 | 76 | 82.5 | Intermediate/ High-risk | Primary /Recurrent | Tokyo 172 | Induction & Maintenance/ Induction only | Half-dose | Naïve | 35 |
| Del Giudice [32] | 2021 | Retrospective | 422 | 67 | 67.7 | Intermediate/ High-risk | Primary /Recurrent | Connaught/RIVM/Tice | Induction & Maintenance | Full Dose | Naïve | 73 |
| Del Giudice [33] | 2022 | Retrospective | 852 | 68 | 74.4 | Only High-risk | Primary only | Tice/RIVM | Induction & Maintenance | Full Dose | Naïve | 53 |
| Dereijke [34] | 2005 | Prospective | 84 | - | 94 | Only High-risk | Primary /Recurrent | Connaught | Induction only | Full Dose | Naïve & Recurrent | 60 |
| Di Lorenzo [35] | 2010 | Prospective | 40 | 71.4 | 55 | Only High-risk | Recurrent only | Connaught | Induction & Maintenance | Full Dose | Recurrent | 16 |
| Di Stasi [36] | 2006 | Prospective | 105 | 67 | 81.9 | Intermediate/ High-risk | Primary /Recurrent | Connaught | Induction & Maintenance | Full Dose | Naïve | 88 |
| Farah [37] | 2014 | Prospective | 60 | 61.7 | 83.3 | Intermediate/ High-risk | Primary /Recurrent | RIVM | Induction & Maintenance | Full Dose | Naïve | 48 |
| Friedrich [38] | 2007 | Prospective | 163 | 67 | 80.4 | Intermediate/ High-risk | Primary /Recurrent | RIVM | Induction only | Full Dose | Naïve | 36 |
| Gontero [39] | 2013 | Prospective | 120 | 67.5 | - | Only Intermediate | Primary only | Connaught | Induction & Maintenance | One-third Dose | Naïve | 12 |
| Gruenwald [40] | 1997 | Prospective | 40 | 68.5 | 87.5 | Only High-risk | Primary /Recurrent | Pasteur | Induction only | Full Dose | Naïve | 28 |
| Hemdan [41] | 2014 | Prospective | 126 | - | 79.2 | Intermediate. /High-risk | Primary only | Tice | Induction & Maintenance | Full Dose | Naïve | 60 |
| Herr [42] | 2012 | Prospective | 156 | 68 | 67.5 | Only High-risk | Primary /Recurrent | Connaught | Induction only | Full Dose | Naïve | 24 |
| Herr [43] | 2011 | Prospective | 816 | 64 | 73 | Only High-risk | Primary /Recurrent | Connaught | Induction only | Full Dose | Naïve & Recurrent | 24 |
| Herr [44] | 2007 | Prospective | 805 | 65 | 76 | Only High-risk | Recurrent only | Connaught | Induction & Maintenance /Induction only | Full Dose | Naïve & Recurrent | 24 |
| Hinotsu [45] | 2011 | Prospective | 83 | - | 95.2 | Intermediate/ High-risk | Primary /Recurrent | Connaught | Induction & Maintenance /Induction only | Full Dose | Naïve & Recurrent | 24 |
| Hinotsu [46] | 2006 | Prospective | 40 | 64.3 | 78 | Intermediate/ High-risk | Primary /Recurrent | Tokyo 172 | Induction only | Full Dose | Naïve | 36 |
| Hudson [47] | 1987 | Prospective | 42 | 67 | 71.4 | Only Intermediate | Primary only | Pasteur | Induction & Maintenance /Induction only | Full Dose | Naïve | 17 |
| Ibrahiem [48] | 1988 | Prospective | 17 | 55 | 82.3 | Intermediate/ High-risk | Recurrent only | Montreal Armand Frappier | Induction & Maintenance | Full Dose | Naïve & Recurrent | 28 |
| Inamoto [49] | 2013 | Prospective | 38 | 72.5 | 85 | Intermediate/ High-risk | Primary /Recurrent | Connaught/Tokyo 172 | Induction & Maintenance | Full Dose /Half Dose | Naïve & Recurrent | 12 |
| Jarvien [50] | 2009 | Prospective | 44 | 68 | 77.2 | Intermediate/ High-risk | Recurrent only | Pasteur | Induction & Maintenance | Full Dose | Naïve | 60 |
| Kamat [51] | 1994 | Prospective | 95 | 54.1 | 86 | Intermediate/ High-risk | Primary /Recurrent | Danish 1331 | Induction Only | Full Dose | Naïve | 60 |
| Koga [52] | 2010 | Prospective | 51 | 74 | 79 | Intermediate/ High-risk | Primary /Recurrent | Tokyo 172 | Induction & Maintenance /Induction only | Full Dose | Naïve | 29 |
| Lamm [2] | 2000 | Prospective | 384 | 67 | 90.1 | Intermediate/ High-risk | Primary /Recurrent | Connaught | Induction & Maintenance /Induction only | Full Dose | Naïve & Recurrent | 84 |
| Lamm [53] | 1995 | Prospective | 469 | 66.5 | 84 | Intermediate/ High-risk | Primary /Recurrent | Tice | Induction & Maintenance | One-third Dose | Naïve | 30 |
| Martinez-Pieniro [54] | 2002 | Prospective | 500 | - | 89.3 | Intermediate/ High-risk | Primary /Recurrent | Connaught | Induction & Maintenance | Full Dose /one-third Dose | Naïve | 69 |
| Martinez-Pieniro [55] | 1990 | Prospective | 67 | 65 | 82 | Intermediate/ High-risk | Primary /Recurrent | Pasteur | Induction only | Full Dose | Naïve | 36 |
| Marttila [56] | 2016 | Prospective | 115 | 69.5 | 74 | Only Intermediate | Primary /Recurrent | Tice | Induction & Maintenance | Full Dose | Naïve & Recurrent | 90 |
| Melekos [57] | 1996 | Prospective | 46 | 65.4 | 89.1 | Intermediate/ High risk | Primary /Recurrent | Pasteur/Tice | Induction & Maintenance | Full Dose | Naïve & Recurrent | 35 |
| Mukherjee [58] | 1992 | Prospective | 21 | - | - | Intermediate/ High-risk | Primary /Recurrent | Glaxo /Pasteur | Induction only | Full Dose | Naïve & Recurrent | 12 |
| Nowak [59] | 2021 | Retrospective | 590 | 71.1 | 85.3 | Only High Risk | Primary only | Moreau/ RIVM/Tice | Induction & Maintenance | Full Dose | Naïve & Recurrent | 40 |
| Oddens [3] | 2012 | Prospective | 1355 | 69 | 80.7 | Intermediate/ High-risk | Primary /Recurrent | Tice | Induction & Maintenance | Full Dose/ one-third Dose | Naïve | 84 |
| Ojea [60] | 2007 | Prospective | 430 | - | 88 | Only Intermediate | Primary /Recurrent | Connaught | Induction & Maintenance | One-third Dose | Naïve & Recurrent | 57 |
| Okamura [61] | 2011 | Retrospective | 75 | 68 | 88.8 | Intermediate/ High-risk | Primary /Recurrent | Tokyo 172 | Induction & Maintenance/ Induction only | Full Dose | Naïve | 66 |
| Oosterlinck [62] | 2011 | Prospective | 48 | 70 | 81.3 | Intermediate/ High-risk | Primary only | Tice | Induction & Maintenance | Full Dose | Naïve | 56 |
| Ourfali [63] | 2019 | Retrospective | 402 | - | - | Only High-risk | Primary /Recurrent | Connaught | Induction & Maintenance | Full Dose | Naïve | 24 |
| Palou [64] | 2001 | Prospective | 126 | 63 | 95 | Intermediate/ High-risk | Primary /Recurrent | Connaught | Induction & Maintenance /Induction only | Full Dose | Naïve | 78 |
| Peyromaure [81] | 2003 | Retrospective | 57 | 65.4 | - | Intermediate/ High-risk | Primary /Recurrent | Connaught | Induction & Maintenance | Full Dose | Naïve & Recurrent | 48 |
| Porena [65] | 2010 | Prospective | 64 | 68.7 | 87.5 | Only High-risk | Primary only | Tice | Induction & Maintenance | Full Dose | Naïve | 44 |
| Prasanna [66] | 2017 | Retrospective | 103 | 77 | 83 | Intermediate/ High-risk | Primary /Recurrent | Tice | Induction & Maintenance | Full Dose | Naïve & Recurrent | 15 |
| Rentsch [67] | 2014 | Prospective | 131 | 72 | 83.3 | Only High risk | Primary /Recurrent | Connaught/ Tice | Induction only | Full Dose | Naïve & Recurrent | 51.4 |
| Rintala [68] | 1991 | Prospective | 51 | 68 | 76.4 | Intermediate/ High-risk | Primary /Recurrent | Pasteur | Induction only | Full Dose | Naïve | 28 |
| Sekine [69] | 2001 | Prospective | 42 | 72 | 80.9 | Only High-risk | Primary /Recurrent | Tokyo 172 | Induction only | Full Dose | Naïve | 47 |
| Sengiku [70] | 2013 | Prospective | 129 | 70.7 | 76.1 | Intermediate/ High-risk | Primary /Recurrent | Connaught/ Tokyo 172 | Induction only | Full Dose | Naïve | 28 |
| Shinka [71] | 1997 | Prospective | 141 | - | 83 | Intermediate/ High-risk | Primary only | Tokyo 172 | Induction only | Full Dose | Naïve | 60 |
| Shinka [72] | 1989 | Prospective | 56 | 67.8 | - | Only High-risk | Recurrent only | Tokyo 172 | Induction only | Full Dose | Naïve | 20 |
| Sood [73] | 2020 | Prospective | 104 | 58 | 94.1 | Intermediate/ High-risk | Primary only | Sii Onco BCG | Induction & Maintenance | Full Dose | Naïve | 36 |
| Steinberg [74] | 2016 | Prospective | 398 | 70 | 78.4 | Intermediate/ High-risk | Primary /Recurrent | Connaught/ Tice | Induction & Maintenance | Full Dose /one-third Dose | Naïve & Recurrent | 24 |
| Sylvester [75] | 2010 | Prospective | 281 | 66 | NR | Intermediate/ High-risk | Primary /Recurrent | Tice | Induction only | Full Dose | Naïve | 108 |
| Takashi [76] | 1998 | Prospective | 84 | 65.3 | 75 | Only High-risk | Primary /Recurrent | Tokyo 172 | Induction only | Full Dose | Naïve | 56 |
| Takashi [77] | 1997 | Retrospective | 30 | 65.6 | 83.3 | Only High-risk | Primary /Recurrent | Tokyo 172 | Induction only | Full Dose | Naïve | 60 |
| Witjes [78] | 2016 | Retrospective | 2099 | - | 82.8 | Intermediate/ High risk | Primary /Recurrent | Connaught/ Tice | Induction & Maintenance | Full Dose | Naïve & Recurrent | 62.4 |
| Witjes [79] | 1999 | Prospective | 55 | - | 85.7 | Only High-risk | Primary only | Tice | Induction & Maintenance | Full Dose | Naïve | 12.3 |
| Yalcinkaya [80] | 1997 | Prospective | 80 | 55.2 | 55 | Intermediate/ High risk | Primary /Recurrent | Connaught | Induction only | Full Dose | Naïve | 33 |
| Yoo [82] | 2012 | Prospective | 126 | 61.7 | 81.5 | Intermediate/ High risk | Primary /Recurrent | Tice | Induction & Maintenance /Induction only | Full Dose | Naïve | 24 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Del Giudice, F.; Asero, V.; Bologna, E.; Scornajenghi, C.M.; Carino, D.; Dolci, V.; Viscuso, P.; Salciccia, S.; Sciarra, A.; D’Andrea, D.; et al. Efficacy of Different Bacillus of Calmette-Guérin (BCG) Strains on Recurrence Rates among Intermediate/High-Risk Non-Muscle Invasive Bladder Cancers (NMIBCs): Single-Arm Study Systematic Review, Cumulative and Network Meta-Analysis. Cancers 2023, 15, 1937. https://doi.org/10.3390/cancers15071937
Del Giudice F, Asero V, Bologna E, Scornajenghi CM, Carino D, Dolci V, Viscuso P, Salciccia S, Sciarra A, D’Andrea D, et al. Efficacy of Different Bacillus of Calmette-Guérin (BCG) Strains on Recurrence Rates among Intermediate/High-Risk Non-Muscle Invasive Bladder Cancers (NMIBCs): Single-Arm Study Systematic Review, Cumulative and Network Meta-Analysis. Cancers. 2023; 15(7):1937. https://doi.org/10.3390/cancers15071937
Chicago/Turabian StyleDel Giudice, Francesco, Vincenzo Asero, Eugenio Bologna, Carlo Maria Scornajenghi, Dalila Carino, Virginia Dolci, Pietro Viscuso, Stefano Salciccia, Alessandro Sciarra, David D’Andrea, and et al. 2023. "Efficacy of Different Bacillus of Calmette-Guérin (BCG) Strains on Recurrence Rates among Intermediate/High-Risk Non-Muscle Invasive Bladder Cancers (NMIBCs): Single-Arm Study Systematic Review, Cumulative and Network Meta-Analysis" Cancers 15, no. 7: 1937. https://doi.org/10.3390/cancers15071937
APA StyleDel Giudice, F., Asero, V., Bologna, E., Scornajenghi, C. M., Carino, D., Dolci, V., Viscuso, P., Salciccia, S., Sciarra, A., D’Andrea, D., Pradere, B., Moschini, M., Mari, A., Albisinni, S., Krajewski, W., Szydełko, T., Małkiewicz, B., Nowak, Ł., Laukhtina, E., ... De Berardinis, E. (2023). Efficacy of Different Bacillus of Calmette-Guérin (BCG) Strains on Recurrence Rates among Intermediate/High-Risk Non-Muscle Invasive Bladder Cancers (NMIBCs): Single-Arm Study Systematic Review, Cumulative and Network Meta-Analysis. Cancers, 15(7), 1937. https://doi.org/10.3390/cancers15071937















