Fertility-Sparing Treatment and Assisted Reproductive Technology in Patients with Endometrial Carcinoma and Endometrial Hyperplasia: Pregnancy Outcomes after Embryo Transfer
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Subjects
2.3. Variables and Statistical Analysis
2.4. Embryo Cryopreservation and Warming
2.5. Embryo Transfer
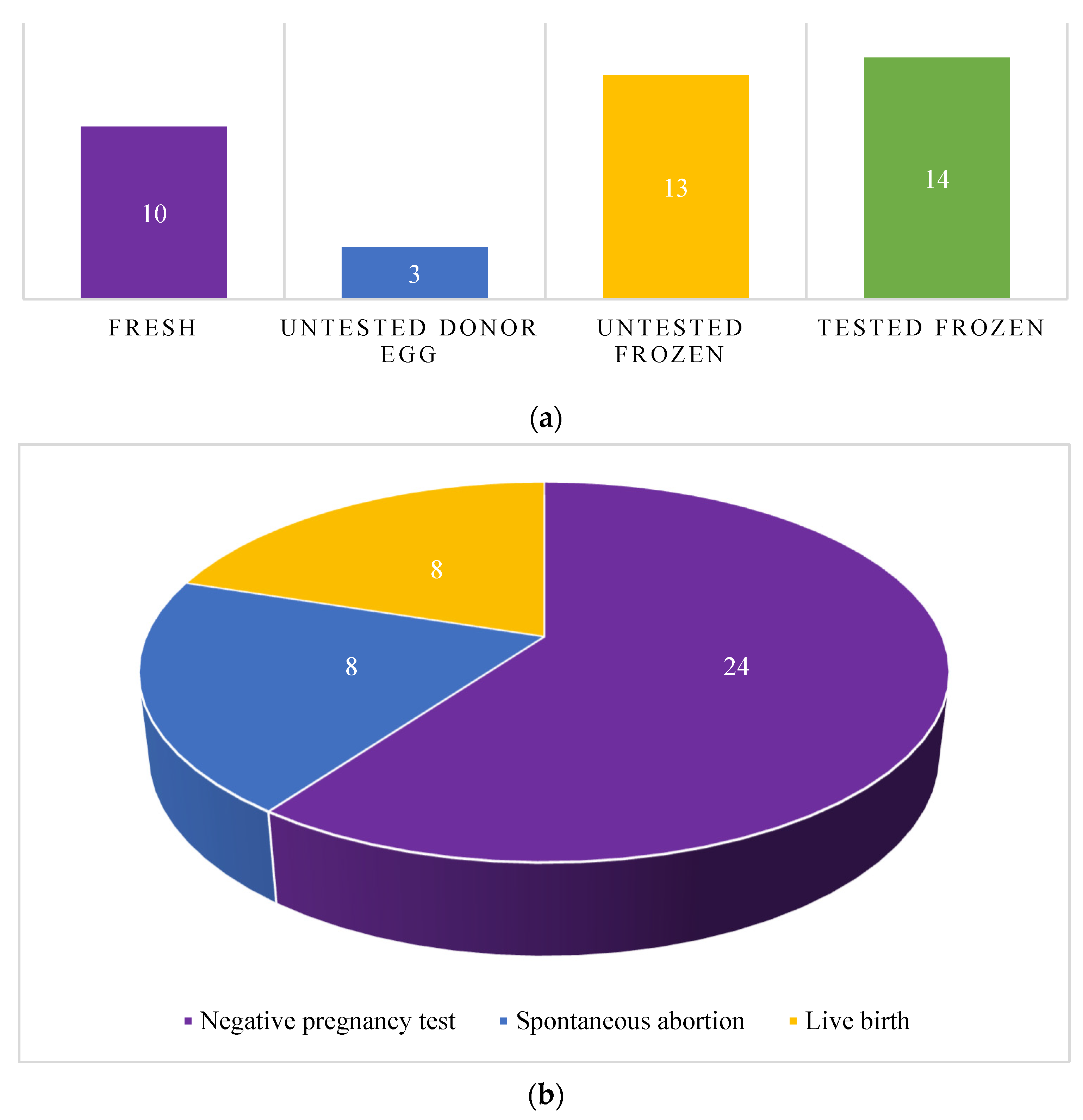
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef]
- Mutter, G.L. Endometrial intraepithelial neoplasia (EIN): Will it bring order to chaos? The Endometrial Collaborative Group. Gynecol. Oncol. 2000, 76, 287–290. [Google Scholar] [CrossRef]
- Epidemiology of Endometrial Cancer Consortium (E2C2). Available online: https://epi.grants.cancer.gov/eecc/ (accessed on 14 September 2021).
- Reed, S.D.; Newton, K.M.; Clinton, W.L.; Epplein, M.; Garcia, R.; Allison, K.; Voigt, L.F.; Weiss, N.S. Incidence of endometrial hyperplasia. Am. J. Obstet. Gynecol. 2009, 200, 678.e1–678.e6. [Google Scholar] [CrossRef]
- Travaglino, A.; Raffone, A.; Saccone, G.; Mascolo, M.; Guida, M.; Mollo, A.; Insabato, L.; Zullo, F. Congruence Between 1994 WHO Classification of Endometrial Hyperplasia and Endometrial Intraepithelial Neoplasia System. Am. J. Clin. Pathol. 2020, 153, 40–48. [Google Scholar] [CrossRef]
- Soliman, P.T.; Oh, J.C.; Schmeler, K.M.; Sun, C.C.; Slomovitz, B.M.; Gershenson, D.M.; Burke, T.W.; Lu, K.H. Risk Factors for Young Premenopausal Women With Endometrial Cancer. Obstet. Gynecol. 2005, 105, 575–580. [Google Scholar] [CrossRef]
- Mathews, T.J.; Hamilton, B.E. Mean Age of Mothers is on the Rise: United States, 2000–2014. NCHS Data Brief 2016, 232, 1–8. [Google Scholar]
- Tian, Y.; Liu, Y.; Wang, G.; Lv, Y.; Zhang, J.; Bai, X.; Zhang, H.; Song, X. Endometrial hyperplasia in infertile women undergoing IVF/ICSI: A retrospective cross-sectional study. J. Gynecol. Obstet. Hum. Reprod. 2020, 49, 101780. [Google Scholar] [CrossRef] [PubMed]
- Quinn, M.A.; Kneale, B.J.; Fortune, D.W. Endometrial carcinoma in premenopausal women: A clinicopathological study. Gynecol. Oncol. 1985, 20, 298–306. [Google Scholar] [CrossRef] [PubMed]
- Yamazawa, K.; Seki, K.; Matsui, H.; Kihara, M.; Sekiya, S. Prognostic factors in young women with endometrial carcinoma: A report of 20 cases and review of literature. Int. J. Gynecol. Cancer 2000, 10, 212–222. [Google Scholar] [CrossRef] [PubMed]
- Gitsch, G.; Hanzal, E.; Jensen, D.; Hacker, N.F. Endometrial cancer in premenopausal women 45 years and younger. Obstet. Gynecol. 1995, 85, 504–508. [Google Scholar] [CrossRef]
- Abu Hashim, H.; Ghayaty, E.; El Rakhawy, M. Levonorgestrel-releasing intrauterine system vs oral progestins for non-atypical endometrial hyperplasia: A systematic review and metaanalysis of randomized trials. Am. J. Obstet. Gynecol. 2015, 213, 469–478. [Google Scholar] [CrossRef]
- Randall, T.C.; Kurman, R.J. Progestin treatment of atypical hyperplasia and well-differentiated carcinoma of the endometrium in women under age 40. Obstet. Gynecol. 1997, 90, 434–440. [Google Scholar] [CrossRef] [PubMed]
- Montz, F.J.; Bristow, R.E.; Bovicelli, A.; Tomacruz, R.; Kurman, R.J. Intrauterine progesterone treatment of early endometrial cancer. Am. J. Obstet. Gynecol. 2002, 186, 651–657. [Google Scholar] [CrossRef] [PubMed]
- Gallos, I.D.; Yap, J.; Rajkhowa, M.; Luesley, D.M.; Coomarasamy, A.; Gupta, J.K. Regression, relapse, and live birth rates with fertility-sparing therapy for endometrial cancer and atypical complex endometrial hyperplasia: A systematic review and metaanalysis. Am. J. Obstet. Gynecol. 2012, 207, 266.e1–266.e12. [Google Scholar] [CrossRef] [PubMed]
- Kurman, R.J.; Kaminski, P.F.; Norris, H.J. The behavior of endometrial hyperplasia. A long-term study of “untreated” hyperplasia in 170 patients. Cancer 1985, 56, 403–412. [Google Scholar] [CrossRef]
- Giampaolino, P.; Di Spiezio Sardo, A.; Mollo, A.; Raffone, A.; Travaglino, A.; Boccellino, A.; Zizolfi, B.; Insabato, L.; Zullo, F.; De Placido, G.; et al. Hysteroscopic Endometrial Focal Resection followed by Levonorgestrel Intrauterine Device Insertion as a Fertility-Sparing Treatment of Atypical Endometrial Hyperplasia and Early Endometrial Cancer: A Retrospective Study. J. Minim. Invasive Gynecol. 2019, 26, 648–656. [Google Scholar] [CrossRef]
- Rodolakis, A.; Biliatis, I.; Morice, P.; Reed, N.; Mangler, M.; Kesic, V.; Denschlag, D. European Society of Gynecological Oncology Task Force for Fertility Preservation: Clinical Recommendations for Fertility-Sparing Management in Young Endometrial Cancer Patients. Int. J. Gynecol. Cancer 2015, 25, 1258–1265. [Google Scholar] [CrossRef]
- Elizur, S.E.; Beiner, M.E.; Korach, J.; Weiser, A.; Ben-Baruch, G.; Dor, J. Outcome of in vitro fertilization treatment in infertile women conservatively treated for endometrial adenocarcinoma. Fertil. Steril. 2007, 88, 1562–1567. [Google Scholar] [CrossRef] [PubMed]
- Han, A.R.; Kwon, Y.S.; Kim, D.Y.; Kim, J.H.; Kim, Y.M.; Kim, Y.T.; Nam, J.H. Pregnancy outcomes using assisted reproductive technology after fertility-preserving therapy in patients with endometrial adenocarcinoma or atypical complex hyperplasia. Int. J. Gynecol. Cancer 2009, 19, 147–151. [Google Scholar] [CrossRef]
- Kim, M.J.; Choe, S.A.; Kim, M.K.; Yun, B.S.; Seong, S.J.; Kim, Y.S. Outcomes of in vitro fertilization cycles following fertility-sparing treatment in stage IA endometrial cancer. Arch. Gynecol. Obstet. 2019, 300, 975–980. [Google Scholar] [CrossRef]
- Li, M.; Song, J.L.; Zhao, Y.; Wu, S.L.; Liu, H.B.; Tang, R.; Yan, L. Fertility outcomes in infertile women with complex hyperplasia or complex atypical hyperplasia who received progestin therapy and in vitro fertilization. J. Zhejiang Univ. Sci. B 2017, 18, 1022–1025. [Google Scholar] [CrossRef]
- Park, J.Y.; Seong, S.J.; Kim, T.J.; Kim, J.W.; Kim, S.M.; Bae, D.S.; Nam, J.H. Pregnancy outcomes after fertility-sparing management in young women with early endometrial cancer. Obstet. Gynecol. 2013, 121, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Pinto, A.B.; Gopal, M.; Herzog, T.J.; Pfeifer, J.D.; Williams, D.B. Successful in vitro fertilization pregnancy after conservative management of endometrial cancer. Fertil. Steril. 2001, 76, 826–829. [Google Scholar] [CrossRef] [PubMed]
- Piura, B. Two successful pregnancies after in vitro fertilization and embryo transfer in a patient with endometrial atypical hyperplasia bordering on adenocarcinoma treated conservatively with high-dose progesterone. Gynecol. Obstet. Investig. 2006, 61, 21–23. [Google Scholar] [CrossRef]
- Paulson, R.J.; Sauer, M.V.; Lobo, R.A. Pregnancy after in vitro fertilization in a patient with stage I endometrial carcinoma treated with progestins. Fertil. Steril. 1990, 54, 735–736. [Google Scholar] [CrossRef] [PubMed]
- Bian, J.; Shao, H.; Liu, H.; Li, H.; Fang, L.; Xing, C.; Wang, L.; Tao, M. Efficacy of the Levonorgestrel-Releasing Intrauterine System on IVF-ET Outcomes in PCOS With Simple Endometrial Hyperplasia. Reprod. Sci. 2015, 22, 758–766. [Google Scholar] [CrossRef] [PubMed]
- Inoue, O.; Hamatani, T.; Susumu, N.; Yamagami, W.; Ogawa, S.; Takemoto, T.; Hirasawa, A.; Banno, K.; Kuji, N.; Tanaka, M.; et al. Factors affecting pregnancy outcomes in young women treated with fertility-preserving therapy for well-differentiated endometrial cancer or atypical endometrial hyperplasia. Reprod. Biol. Endocrinol. 2016, 14, 2. [Google Scholar] [CrossRef]
- Guidance on the limits to the number of embryos to transfer: A committee opinion. Fertil. Steril. 2017, 107, 901–903. [CrossRef]
- Yang, B.Y.; Gulinazi, Y.; Du, Y.; Ning, C.C.; Cheng, Y.L.; Shan, W.W.; Luo, X.Z.; Zhang, H.W.; Zhu, Q.; Ma, F.H.; et al. Metformin plus megestrol acetate compared with megestrol acetate alone as fertility-sparing treatment in patients with atypical endometrial hyperplasia and well-differentiated endometrial cancer: A randomised controlled trial. BJOG 2020, 127, 848–857. [Google Scholar] [CrossRef]
- Mitsuhashi, A.; Habu, Y.; Kobayashi, T.; Kawarai, Y.; Ishikawa, H.; Usui, H.; Shozu, M. Long-term outcomes of progestin plus metformin as a fertility-sparing treatment for atypical endometrial hyperplasia and endometrial cancer patients. J. Gynecol. Oncol. 2019, 30, e90. [Google Scholar] [CrossRef]
- Mitsuhashi, A.; Shozu, M. New therapeutic approaches for the fertility-sparing treatment of endometrial cancer. J. Obstet. Gynaecol. Res. 2020, 46, 215–222. [Google Scholar] [CrossRef] [PubMed]

| EMCA/EH | EMCA | EH | |
|---|---|---|---|
| Patients (n) | 14 | 3 | 11 |
| Median age at diagnosis in years | 34 (27–37) | 34 (31.5–35.5) | 34 (29–38.5) |
| Median age at retrieval in years | 34 (30.75–36.25) | 36 (33–38) | 34 (31–36) |
| Median age at first transfer in years | 36 (31.25–39.5) | 36 (33–38) | 36 (31.5–39) |
| Median BMI | 27.88 (20.37–30.9) | 35.1 (30.55–36.55) | 25.37 (20.12–28.89) |
| Nulliparity (n) | 10 | 3 | 7 |
| Number of patients using PGT-A (n) | 6 | 2 | 4 |
| Median number of embryo transfer cycles | 2.5 (2–3) | 2 (1.5–3) | 3 (3–3.5) |
| Patient ID | Diagnosis | Age at Diagnosis (years) | Age at Retrieval (years) | Age at First Transfer (years) | BMI | Gravidity/Parity | PGT-A | Risk Factors | Treatment | Total Number of ET Cycles | Pregnancy Outcome | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LB | SAB | NPT | |||||||||||
| 1 | Endometrial hyperplasia | 30 | 31 | 31 | 32.06 | 0/0 | No | PCOS | Megestrol acetate | 2 | 1 | 1 | - |
| 2 | Endometrial hyperplasia | 44 | Donor egg | 48 | 19.7 | 0/0 | No | Oligo-ovulation | Progesterone | 1 | 1 | - | - |
| 3 | Endometrial hyperplasia | 40 | Donor egg | 44 | 30.9 | 0/0 | No | PCOS, obesity | NA | 2 | 2 | - | - |
| 4 | Complex hyperplasia without atypia | 35 | 37 | 37 | 20 | 0/0 | No | NA | Norethindrone, megestrol acetate | 9 | - | 1 | 8 |
| 5 | Complex atypical hyperplasia | 28 | 28 | 28 | 29.1 | 0/0 | Yes | Oligo-ovulation | Megestrol acetate | 3 | - | - | 3 |
| 6 | Complex atypical hyperplasia | 34 | 34 | 34 | 20.03 | 0/0 | No | PCOS | Megestrol acetate | 4 | 1 | - | 3 |
| 7 | Simple and complex endometrial hyperplasia without atypia confined to polyp | 37 | 38 | 38 | 22.85 | 1/0010 | Yes | PCOS | Polypectomy | 2 | 1 | 1 | - |
| 8 | Endometrial hyperplasia | 27 | 32 | 32 | 20.37 | 0/0 | Yes | PCOS | Norethindrone | 1 | 1 | - | - |
| 9 | Endometrial hyperplasia with atypia | 28 | 30 | 30 | 28.24 | 4/0040 | No | PCOS | Levonorgestrel IUD | 3 | - | 2 | 1 |
| 10 | Endometrial hyperplasia | 40 | 34 | 40 | NA | 3/2012 | No | PCOS | Progesterone | 1 | - | - | 1 |
| 11 | Endometrial hyperplasia | 31 | 36 | 36 | 27.88 | 2/0020 | Yes | PCOS | Progesterone | 2 | 1 | - | 1 |
| 12 | Endometrial adenocarcinoma, endometrioid type, FIGO grade I | 34 | 36 | 36 | 38 | 0/0 | Yes | PCOS, obesity | Megestrol acetate, levonorgestrel IUD | 3 | - | - | 3 |
| 13 | Endometrial hyperplasia with a focus on adenocarcinoma | 37 | 40 | 40 | 26 | 0/0 | No | NA | Megestrol acetate | 3 | - | 1 | 2 |
| 14 | Endometrial adenocarcinoma, endometrioid type, FIGO grade I | 29 | 30 | 30 | 35.1 | 0/0 | Yes | PCOS, obesity | Megestrol acetate | 4 | - | 2 | 2 |
| Patient ID | PGT-A Type | Embryos Transferred (n) | Live Birth | Expected Outcome |
|---|---|---|---|---|
| 5 | NGS | 1 | No | 0.617 |
| 5 | NGS | 1 | No | 0.617 |
| 5 | NGS | 1 | No | 0.617 |
| 7 | NGS | 1 | Yes | 0.617 |
| 8 | NGS | 1 | Yes | 0.617 |
| 11 | NGS | 1 | No | 0.617 |
| 11 | NGS | 1 | Yes | 0.617 |
| 12 | aCGH | 1 | No | 0.532 |
| 12 | aCGH | 1 | No | 0.532 |
| 12 | aCGH | 1 | No | 0.532 |
| 14 | aCGH | 2 | No | 0.781 |
| 14 | aCGH | 2 | No | 0.781 |
| 14 | aCGH | 2 | No | 0.781 |
| 14 | aCGH | 1 | No | 0.532 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Friedlander, H.; Blakemore, J.K.; McCulloh, D.H.; Fino, M.E. Fertility-Sparing Treatment and Assisted Reproductive Technology in Patients with Endometrial Carcinoma and Endometrial Hyperplasia: Pregnancy Outcomes after Embryo Transfer. Cancers 2023, 15, 2123. https://doi.org/10.3390/cancers15072123
Friedlander H, Blakemore JK, McCulloh DH, Fino ME. Fertility-Sparing Treatment and Assisted Reproductive Technology in Patients with Endometrial Carcinoma and Endometrial Hyperplasia: Pregnancy Outcomes after Embryo Transfer. Cancers. 2023; 15(7):2123. https://doi.org/10.3390/cancers15072123
Chicago/Turabian StyleFriedlander, Hilary, Jennifer K. Blakemore, David H. McCulloh, and M. Elizabeth Fino. 2023. "Fertility-Sparing Treatment and Assisted Reproductive Technology in Patients with Endometrial Carcinoma and Endometrial Hyperplasia: Pregnancy Outcomes after Embryo Transfer" Cancers 15, no. 7: 2123. https://doi.org/10.3390/cancers15072123
APA StyleFriedlander, H., Blakemore, J. K., McCulloh, D. H., & Fino, M. E. (2023). Fertility-Sparing Treatment and Assisted Reproductive Technology in Patients with Endometrial Carcinoma and Endometrial Hyperplasia: Pregnancy Outcomes after Embryo Transfer. Cancers, 15(7), 2123. https://doi.org/10.3390/cancers15072123









