Simple Summary
Since the approval of immune checkpoint inhibitors for solid tumors, concerns have been raised about the role of the microbiota on immunotherapy success and the potential negative impact of several drugs on oncological response and survival. In this review, we analyzed the existing data regarding such negative but also positive effect of many drugs on immunotherapy results. Most deleterious drugs concerning immunotherapy efficacy are corticosteroids, antibiotics and proton pump inhibitors, but preclinical as well as clinical studies have been conducted on other molecules such as metformin, statins, aspirin or beta blockers. The aim of this review is to elaborate a practical overview of current scientific data to help clinicians make critical treatment decisions by taking into account the totality of their patients’ comedications.
Abstract
Immune checkpoint inhibitors (ICIs) have been a major breakthrough in solid oncology over the past decade. The immune system and the gut microbiota are involved in their complex mechanisms of action. However, drug interactions have been suspected of disrupting the fine equilibrium necessary for optimal ICI efficacy. Thus, clinicians are facing a great deal of sometimes contradictory information on comedications with ICIs and must at times oppose conflicting objectives between oncological response and comorbidities or complications. We compiled in this review published data on the role of the microbiota in ICI efficacy and the impact of comedications. We found mostly concordant results on detrimental action of concurrent corticosteroids, antibiotics, and proton pump inhibitors. The timeframe seems to be an important variable each time to preserve an initial immune priming at ICIs initiation. Other molecules have been associated with improved or impaired ICIs outcomes in pre-clinical models with discordant conclusions in retrospective clinical studies. We gathered the results of the main studies concerning metformin, aspirin, and non-steroidal anti-inflammatory drugs, beta blockers, renin-angiotensin-aldosterone system inhibitors, opioids, and statins. In conclusion, one should always assess the necessity of concomitant treatment according to evidence-based recommendations and discuss the possibility of postponing ICI initiation or switching strategies to preserve the critical window.
1. Introduction
The advent of immune checkpoint inhibitors (ICIs) in the 2010s has revolutionized cancer therapy. These molecules act very differently from previous oncological treatments and have become a standard of care for many cancers in metastatic or neoadjuvant/adjuvant settings (e.g., melanoma or lung carcinoma) [1,2]. Their mechanism of action is based on blocking the recognition of the lymphocyte ligand/receptor checkpoint pair, which activates and stimulates the immune system against tumor cells [3]. The main targets of these treatments for solid tumors are the programmed cell death protein 1 (PD-1), its ligand (PD-L1), and the cytotoxic T-lymphocyte-associated protein 4 (CTLA-4). However, not all patients benefit from the efficacy of these molecules. Primary resistance is often observed, as well as secondary resistance after an initial response. Elucidating some of the underlying mechanisms of resistance could help clinicians optimize treatment strategies. Because of the inherently pro-inflammatory therapeutic effect of ICIs, many classes of drugs that might impact the immune system may decrease their efficacy, most notably corticosteroids [4].
More recently, the important role of microbiota, mainly though not only intestinal, has been demonstrated on the antitumor activity of ICIs. As a result, it has been suggested that other therapeutic families known to induce dysbiosis, such as antibiotics or proton pump inhibitors, might reduce the effectiveness of ICIs [5,6]. In addition, other molecules have been associated in vitro and in animal models with increased or decreased efficacy of ICIs through other inflammatory or metabolic pathways, but it was not straightforward to transpose these results for clinical practice, and they need to be confirmed.
The main objective of this review is to draw a state of the art of the microbiota’s role in the efficacy of ICIs and to gather various studies that looked for an impact, positive or negative, on oncological outcomes under ICI treatment of the main therapeutic classes that might interact. We have focused on the three most commonly suggested drug families: corticosteroids, antibiotics, and proton pump inhibitors; and then we identified existing data for the other relevant molecules: metformin, aspirin and nonsteroidal anti-inflammatory drugs, beta blockers, renin-angiotensin-aldosterone system antagonists, opioids, and statins.
2. Methodology of Literature Search and Selection
This review analyzes the existing data of the literature published between 2007 and 2023 related to the microbiota, its treatment-induced perturbations, and the impact of the microbiota and several comedications on ICI efficacy to give a broad overview on this increasingly important topic in clinical practice. In this regard, the authors searched well-known databases (PubMed, Cochrane, Google Scholar), using key words or combinations of them (i.e., immunotherapy; immune checkpoint inhibitors; immune checkpoint blockade; microbiota; immune system; corticosteroids; antibiotics; proton pump inhibitors; metformin; aspirin; non-steroidal anti-inflammatory drugs; beta blockers; renin-angiotensin-aldosterone system antagonists; angiotensin converting enzyme inhibitors; angiotensin-receptor blocker; opioids; statins). Most cited preclinical studies were selected, along with those providing striking results. Likewise, the most important meta-analyses were selected, from which retrospective studies were extracted. Those exploring only one drug and/or examining interesting patient subgroups were preferred. As a result, 143 references were cited as supporting the statements in this work.
3. The Microbiota and the Immune System
3.1. Microbiota: Definition and Composition
The microbiota is the collection of all the microorganisms that occupy a given environment, whereas the microbiome is defined as the set of all the genomic elements of a specific microbiota. The human microbiota living in and on human organisms is composed of thousands of species belonging to different kingdoms: bacteria, archaea, protozoa, fungi, animals, and viruses [7,8]. Dominant bacterial phyla include Firmicutes (30–50%), Bacteroidetes (20–40%), and Actinobacteria (3–10%). At the genus level, Bacteroides is the most abundant by far (up to almost 20%), followed by Faecalibacterium and Bifidobacterium [8]. The microbiota plays a fundamental role in the physiological functioning of the human body: among other things, it is involved in digestion, immune system development, and specific enzyme or vitamin synthesis. This is why the microbiome is sometimes considered as a second genome [7].
3.2. Relation with the Immune System
The role of gut microbiota on human host inflammation has been mostly studied in the context of inflammatory bowel diseases (IBD), where significant alterations in composition have been shown in affected patients compared to control samples [9]. A review by Pavel et al. reported the specifically increased and decreased bacterial genera in IBD patients and their consequences on mucosal injuries. They point out as well the beneficial potential of probiotics in the management of these diseases, particularly in combination. Bifidobacterium and Lactobacillus seem to be the most interesting strains in these pathologies. Results are encouraging with prebiotics and more variable with fecal transplantation [10,11]. Differences in gut flora composition have also been associated with pro-inflammatory status in relation to obesity, with the onset of allergies at school age, and with a high-risk human leukocyte antigen (HLA) genotype for celiac disease in children [12,13,14].
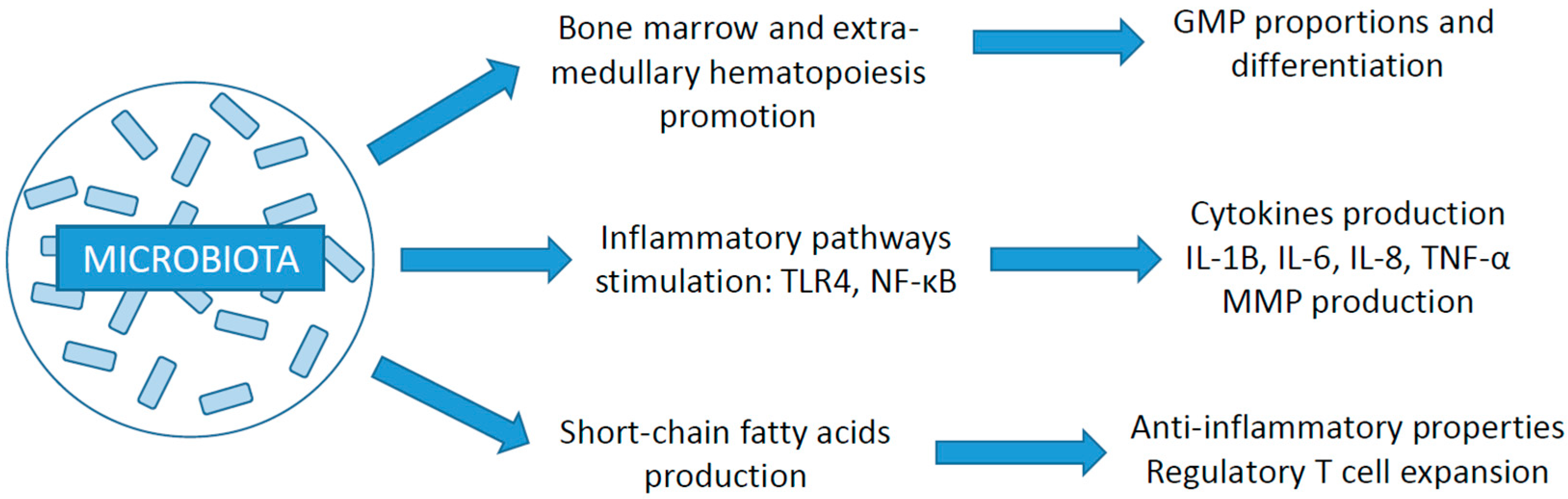
As illustrated in Figure 1, the microbiota’s important role in immune regulation involves, among other things, secreting of cytokines (e.g., interleukins, tumor-necrosis factor (TNF)-α) or matrix metalloproteinases, maintaining homeostasis, or producing T cells [15,16]. Its action has also been demonstrated in stimulating medullary and extra-medullary hematopoiesis for the development of certain components of the immune system, such as myeloid cell derivatives through granulocyte and/or monocyte progenitors differentiation [17].
Figure 1.
Schematic diagram summarizing the relation between the microbiota and the immune system (GMP: granulocyte and/or monocyte progenitor; TLR4: Toll-like receptor 4; NF-κB: nuclear factor kappa B; IL: interleukin; TNF: tumor necrosis factor; MMP: matrix metalloproteinases) [15,16,17].
3.3. Impact of Gut Microbiota on Cancer Development and ICI Efficacy
Changes in the gut microbiota have been associated with the development of cancer, as well as with immunotherapy response. First of all, dysbiosis could alter the gut mucosa, lead to chronic inflammation, and eventually promote colorectal cancer. Tabowei et al. noted in their review the predominant association of Fusobacterium genus with colorectal cancer and its depletion in healthy individuals [18]. Dysbiosis-associated microbes are thought to activate various immune pathways, including nuclear factor kappa B (NF-κB) dependent signaling, release of inflammatory mediators such as interleukins, or interaction with monocytes, promoting carcinogenesis in the mucosa epithelium [18]. Likewise, oral microbiota alterations leading to chronic periodontal inflammation have been associated with permanent genetic alterations in epithelial cells and eventually carcinoma development. Some of the suspected germs have been associated with inflammatory cytokines or TNF-α production, apoptosis inhibition, or promotion of cell proliferation. These oral pathogens have also been associated with colorectal and pancreatic cancer [19].
On the other hand, the influence of gut microbiota on cancer immunotherapy likely lies in its role in fine-tuning the immune status and in its possible activation against tumor cells under the action of ICIs [5]. It is thought to reduce Treg levels and promote CD8+ T cell activation and CD4+ T cell differentiation [20]. Two major studies in mice gave evidence of this strong interaction. First, the efficacy of anti-CTLA-4 was suppressed in antibiotic-treated and germ-free mice before being recovered through fecal transplantation from anti-CTLA-4-responding patients. It was discovered that these patients’ stools contained larger amounts of specific Bacteroides species. The same results were obtained through feeding the mice directly with Bacteroides isolates [21]. In addition, distinct preexisting microbiota have been associated with differences in spontaneous melanoma growth, which disappeared after fecal transplantation or cohousing the mice. Sequencing identified Bifidobacterium as a pivotal bacterial genus in cancer control, and oral supplementation with Bifidobacterium enhanced the efficacy of anti-PD-1 treatment [22]. In both cases, ICIs activity improvement is probably due to microbiome-induced maturation of dendritic cells and T cells’ priming and accumulation [21,22].
Other preclinical studies showed the benefit of probiotics on ICI efficiency in mice, notably through T cell induction [23]. Hibberd et al. reported probiotics-induced changes in gut microbiota composition in patients with colorectal cancer. These changes included higher levels of butyrate-producing bacteria, which are associated with a better response to immunotherapy [20,24]. Furthermore, a Japanese retrospective study suggests that probiotic supplementation by Clostridium butyricum could have a positive impact on progression-free survival and overall survival in patients with lung cancer receiving ICIs [25]. Finally, prospective trials are also currently recruiting to assess the benefit of fecal transplantation on response rates to ICIs; for example, the TACITO randomized controlled trial in patients with renal cell cancer (NCT04758507).
3.4. Focus on Akkermansia Muciniphila
Routy et al. found significant differences in baseline fecal microbiota sequencing between patients with non-small cell lung carcinoma (NSCLC) or renal cell carcinoma (RCC) exhibiting long progression-free survival (PFS) under ICI (more than 6 months) or not. While further analyzing the stools’ characteristics of responders versus non-responders, they showed the overrepresentation of distinct bacterial taxa such as Akkermansia and isolated the species that was most significantly associated with a good response, Akkermansia muciniphila (p = 0.004). This anaerobe is one of the most abundant bacteria in the ileum microbiota. Its presence was identified in 69% and 58% of patients presenting partial response and stable disease, respectively, and 34% of those who progressed or died. The higher prevalence of this bacterium was then confirmed in a validation cohort. Responders’ stools conveyed sensitivity to PD-1 blockade after fecal transplantation to germ-free mice when non-responders’ did not [26].
The same group published a subsequent study to prospectively confirm the predictive nature of stool A. muciniphila on the response to ICIs (Derosa et al. [27]). In a multicentric cohort of 338 patients with NSCLC, baseline fecal A. muciniphila was associated with a better overall response rate (ORR: 28% vs. 18%, p = 0.04) and longer overall survival (OS) (18.8 months vs. 15.4 months, p = 0.03), independently of PD-L1 tumor proportion score (TPS), Eastern Cooperative Oncology Group Performance Status (ECOG-PS), or antibiotics therapy. The results were even more striking among the 86 patients receiving an ICI alone in first line with 41% ORR vs. 19% (p = 0.03) and 59% of long survivors (over 12 months) vs. 35% (p = 0.04). Interestingly, further stratification of patients according to their A. muciniphila levels (absent, low, high) revealed an association between previous antibiotic exposure and A. muciniphila overabundance, both correlated with decreased survival, suggesting that the importance of A. muciniphila needs a preserved microbial equilibrium. Finally, the team set up a prospective interventional phase 1/2 trial at Gustave Roussy Cancer Hospital to evaluate the contribution of A. muciniphila oral supplementation on the efficacy of ICI treatment for advanced NSCLC and RCC (CSET 3502, EV-2101, no NCT ID). Modulating the composition of the microbiota seems indeed to be a means of optimizing immune checkpoint blockade treatments [25,28].
The importance of A. muciniphila as a key gut bacterium has been evidenced in mice and humans aside from cancer therapy. Its lower abundance has also been associated with numerous diseases such as obesity, diabetes, or liver steatosis [29]. The favorable action of what is now considered as a “next-generation beneficial microbe” on metabolic diseases interestingly concerns the live bacterium as well as pasteurized A. muciniphila or some of its constituent parts (e.g., membrane protein or extracellular vesicles) [30]. However, the complex implications of this key bacterium and its derived products on the host’s metabolism and its perturbations is beginning to be understood and will be the focus of many further studies.
3.5. Role of Other Organ-Specific Microbiomes
In addition to the major role of the gut flora, studies have investigated the impact of other microbiota on the effectiveness of ICIs. Two organs in particular, the lungs and the bladder (until recently presumed sterile when healthy), could host a flora with a decisive role on the efficacy of ICIs.
New generation sequencing (NGS) or 16S ribosomal RNA sequencing of various sputum samples, bronchoalveolar lavage, or lung tissue have led to the detection of many bacterial species belonging to specific taxa such as Prevotella, Streptococcus, or Veillonella. Even though around 90% of identified DNA likely comes from nonviable or dead microorganisms, some studies discovered culturable bacteria in lung samplings [31]. Changes in this microbiota in childhood have been associated with several lung diseases like asthma, and other changes can occur under inhaled corticosteroid treatments [32]. This may play an important role as well in carcinogenesis, and it has been suggested that patients with lung cancer present decreased diversity and higher rates of dysbiosis-associated bacterial genera like Granulicatella or Abiotrophia. Dysbiosis also seems to be associated with decreased immune modulation, especially through γδ T cells, and subsequently with loss of cancer control. Although it seems conceivable that the impact of antibiotics on the loss of efficacy of ICIs may also involve the lung flora in addition to the gut microbiota, no specific studies have been conducted to date [31].
The same sequencing techniques applied to healthy individuals’ culture-negative urine samples isolated numerous bacteria—noticeable taxa were Lactobacillus, Corynebacterium, or Streptococcus—overturning the older dogma of Louis Pasteur and affirming the existence of the urinary microbiota. Similarities in urinary bacterial flora have been reported in patients with prostate cancer, which differed from healthy controls—without differences of gut microbiota. This contributes to the hypothesis of an etiopathogenic role of the urinary dysbiosis in carcinogenesis, the involvement of chronic infection and inflammation being already well-known with schistosomiasis. It has also been suggested that as well as the inflammation caused by tobacco or other carcinogenic agents, urinary dysbiosis could be associated with high tumor mutational burden, and could therefore increase susceptibility to immunotherapy. However, the real impact of this newly identified microbiota and its actions on the efficacy of ICIs has not been formally studied yet [33].
The potential role of oral microbiota on head and neck squamous cell carcinoma (HNSCC) incidence and management has also been studied [34]. Hayes et al. showed an association between greater oral abundance of commensal Corynebacterium and Kingella spp. and a decreased risk of HNSCC occurrence in a nested case-control study [35]. However, regarding ICI efficacy, Ferris et al. found no significant impact of oral microbiota diversity on nivolumab (anti-PD-1) response in 85 patients with HNSCC from the CheckMate 141 trial [36].
3.6. Treatment-Induced Microbiome Changes
Unlike the genome inherited from the parents, the microbiome involves a complex ecosystem that is unstable and can be significantly altered throughout life, especially by age, diet, disease, or drugs. The interaction between gut flora and medications is intricate and bidirectional: drugs can alter the microbiome composition, but gut microorganisms also influence the host response to the drug through what is referred to as pharmacomicrobiomics [20].
One major recent discovery involves the impact of many non-antibiotic drugs on microbiota composition, and thus on the health condition of the host, notably its immune status. Some of these drugs are widely used, such as proton pump inhibitors, metformin, or statins, while others are used more specifically in oncology, such as corticosteroids, opioids, or laxatives [5]. Major studies have reported drug-induced changes in microbiome constitution using large population-based cohorts in the Netherlands [37], the UK [38], or Belgium [39]. Up to 19 commonly used drugs, including additional medications to those mentioned before, from other families such as beta blockers, aspirin, or angiotensin-converting enzyme inhibitors, have been shown to impact microbiome diversity, increasing or decreasing specific bacterial species [5]. Because many patients are taking multiple medications, some studies have examined the additional effect of polypharmacy [40,41].
4. Corticosteroids
Due to their strong immune modulating properties, including cytokine release alteration and T cell activation, migration, and differentiation inhibition [42], corticosteroids are widely used for the treatment of inflammatory and autoimmune diseases. However, they are also broadly used in oncology, prescribed from short to long courses of treatment, in small or large doses, to treat many cancer-related symptoms: pain, nausea, dyspnea, occlusion, cerebral or meningeal symptoms, etc. Related adverse events of such medications are well known and entail infections, including opportunistic infections like pneumocystis, osteoporosis, diabetes, glaucoma, cataracts, or skin alteration [43].
4.1. Impact of Immunosuppression on Cancer Development and Microbiota Composition
Complex interactions between the immune system and cancer development have been studied through observations in patients with primary or acquired immunodeficiencies (e.g., organ transplant). The concept of cancer immunosurveillance involves, notably, interferon production and T cells promotion. Newly produced cancer cells are physiologically identified and killed by natural killer cells and cytotoxic T cells, and if tumor cell proliferation escapes immune monitoring, cancer growth remains immunologically restricted. However, both phases can be altered in immunosuppressed patients [44]. Chronic use of glucocorticoids has been associated with the occurrence of cancers such as lymphomas or sarcomas, especially Kaposi’s sarcoma in transplant and non-transplant clinical settings [45,46].
Immunosuppression-induced dysbiosis has been mostly studied in solid organ transplant recipients with limited outcomes and biases involving the complex interactions between pre-transplant diseases (e.g., cirrhosis) and the gut microbiota. The main results were reduced Enterobacteriaceae and increased Lachnospiraceae and Ruminococcaceae after liver transplant and higher abundance of Bacteroidetes in patients without diarrhea after kidney transplant [47]. Moreover, immunosuppressive drugs, including prednisone, have also been associated with decreased Bacteroidetes and increased Firmicutes in mice [48]. Both acute and chronic dexamethasone treatments have been associated in mice and rats with shifts in gut microbiota [49] and increased levels of Bifidobacterium and Lactobacillus, and it is remarkable to note that the anti-inflammatory action is passed on after fecal transplantation from a treated individual to one with a genetic susceptibility for IBD [50]. Likewise, the use of inhaled or systemic corticosteroids for asthma, chronic obstructive pulmonary disease (COPD), or chronic rhinitis has been associated with changes in diversity, composition, and/or burden of the respiratory microbiome [32]. However, the impact of glucocorticoids on ICI treatment response involves, more likely, direct immune modulation, rather than microbiome-induced [42].
4.2. Effect on ICI Treatment Efficacy
Patients receiving systemic glucocorticoids over 10 mg of prednisone equivalent were usually excluded from ICIs clinical trials because this dose is considered immunosuppressive. However, numerous real-world studies analyzed the impact of such medication at baseline or during ICI treatment and showed a significant decrease in PFS and OS in patients on glucocorticoids [51,52]. Ricciuti et al. conducted a retrospective study to measure the indication-related impact of steroid therapy, which appears to be more detrimental on survival if initiated for palliative care (e.g., fatigue, pain, brain edema) than to treat non-cancer-related diseases (e.g., COPD flare, auto-immune disease), even at high doses [53]. Table 1 and Table 2 present the results of studies (mostly retrospective, except for Hendriks et al.) and systematic reviews and meta-analyses, respectively, on this subject, providing subgroup analyses on the indications of steroid treatment. The same differences were observed between palliative care indications or brain metastases subgroups, and between non-cancer-related indications or immune-related adverse events (irAEs) management. The deleterious impact on survival could therefore be linked to the preexisting poor prognosis of the patients needing steroids for palliative reasons or brain metastases rather than to the action of steroids themselves [42]. However, even among patients with baseline brain metastases, the observed deleterious effect of corticosteroids could reflect the pejorative nature of symptomatic cerebral lesions. On the contrary, association of irAEs with better overall prognosis has often been reported and could compensate for possible harmful effects of glucocorticoid prescription.

Table 1.
Studies analyzing the impact of baseline or concomitant corticosteroids with ICI treatment on response rate and survival [51,52,53,54,55,56,57,58,59].

Table 2.
Systematic reviews and meta-analyses on the impact of corticosteroids with ICI treatment on survival [42,60,61].
These findings suggest reassuring data for clinicians about the possibility of initiating corticosteroids even at high dosage for irAE management, but could lead to delay immunotherapy or reconsider other treatment options like chemotherapy for patients requiring high dose palliative steroids if no withdrawal is possible before initiation.
5. Antibiotics
Early on, antibiotics were suspected in dysbiosis-induced variations of immune response because of their strong impact on the composition, diversity, and burden of gut microbiota. Due to their long-term influence on metabolic pathways, even after early-age short treatments, they have been associated with various chronic diseases in mice and in humans, such as asthma or obesity [62,63]. The increasing evidence of the potentially detrimental effect of antibiotics on immunotherapy results has led to the exclusion of patients who received recent antibiotic therapy from clinical trials or to the requirement of antibiotic wash-out periods.
5.1. Antibiotic-Induced Perturbations of the Microbiota
Among the many classes of antibiotics, not all have the same impact on the intestinal flora. The differential action on the families of bacteria will disturb the balance and diversity of this complex microenvironment for a long time, and in doing so, uncouple the mutualistic host-microbiota relationship. While nearly full recovery is often obtained after four weeks, several studies have shown that the consequences of an antibiotic treatment can be observed in the long term on the composition of the microbiota. Most durable perturbations occur with antibiotics having broad activity on anaerobes, like clindamycin [64]. Jakobsson et al. explored throat and fecal microbiota after clarithromycin and metronidazole treatment. While the flora of control individuals showed relative long-term stability, treated patients showed profound changes in the microbiota within a week of treatment, and alterations were still noticeable up to four years later. These changes could affect the bacterial composition (e.g., Actinobacteria decrease), but also the latent presence of resistance genes selected earlier (e.g., erm(B) coding for macrolide resistance) [65]. Besides the flora’s composition and selection of potential resistances, the complex alterations involve interactions between bacterial species themselves and favorable biochemical conditions for pathogenic species’ proliferation. Moreover, if antibiotics induce broadly human-conserved microbiota alterations, some of their consequences include unpredictable host-specific responses leading to so-called “ecological surprises” [64].
Antibiotics have also been associated with the development of colorectal cancer (CRC). Simin et al. conducted a large meta-analysis including more than 4 million individuals and over 73,000 CRC. Higher risk of CRC was associated with antibiotics, particularly for broad-spectrum antibiotics. The causality is not clearly established, and could involve DNA-damage (e.g., quinolones), treatment-induced dysbiosis, or pathogenic colonization promoting the production of DNA-damaging toxins [24,66]. These metabolites include notably bacterial-derived genotoxins (e.g., BFT from Bacteroides fragilis or colibactin from Enterobacteriaceae) and bacterial virulence factors (e.g., FadA from Fusobacterium nucleatum) that have been found to activate cancer-promoting signaling pathways or cause DNA damages [67].
5.2. Impact of Antibiotics on ICI Response according to Histology
Many retrospective studies have analyzed the effect of antibiotics on response rate and survival among patients receiving ICIs, and the results of some of them are compiled in Table 3. Antibiotics seem to alter progression-free and overall survival regardless of the histology of cancer. Routy et al. found decreased OS in patients with NSCLC, confirmed in NSCLC validation cohort, and decreased PFS in patients with renal cell cancer and urothelial cancer [26]. These results were confirmed in the same team’s prospective NSCLC cohort: exposure to antibiotics was associated with poorer survival in both groups exhibiting fecal Akkermansia muciniphila or not [27].

Table 3.
Studies analyzing the impact of baseline and/or concomitant antibiotics on response rate and survival with ICI and/or chemotherapy or targeted therapy [26,68,69,70,71,72].
5.3. Specificities under Immunotherapy versus Chemotherapy
Cortellini et al. added a second cohort in their retrospective study of patients treated with chemotherapy alone. Interestingly, the use of antibiotics has no impact on chemotherapy efficacy [71]. Although patients in the immunotherapy arm were significantly older and more frequently with an ECOG-PS ≥ 2, these results suggest a real impact of antibiotics on specific immune response rather than a bias towards survival due to initially poorer prognosis of patients needing such treatments. Cortellini et al. published another international retrospective study to estimate the effect of antibiotics on response and survival in patients with NSCLC treated with a first-line chemo-immunotherapy combination [72]. No association was found with this treatment modality, even among patients with a high TPS score of 50% or more. Among the antibiotic therapies preceding antitumor treatment, the modality of administration (intravenous or oral) or duration (≥ or <7 days) did not show any significant impact either.
5.4. Importance of the Antibiotic Treatment Modality: Timing and Duration
Table 4 summarizes some systematic reviews and meta-analyses on the subject, including subgroup analyses on histology and/or chronology of antibiotics and ICI treatment. If no major differences seem to emerge from the type of cancer, the numerous studies highlight one discernible point on the timing of antibiotic therapy in relation with the initiation of treatment with ICI. There is apparently a window of maximum deleterious effect, approximately between the month before and the month after the beginning of immunotherapy. The importance of this pivotal period probably reflects the lasting impact of dysbiosis-induced immune “priming” perturbation [73].

Table 4.
Systematic reviews and meta-analyses on the impact of antibiotics with ICI treatment on response rate and survival [74,75,76,77].
Moreover, Tinsley et al. included subgroup analyses in their retrospective study on single versus cumulative antibiotic therapies [70]. Results show a significant decrease in survival only with cumulative treatments defined as concurrent or successive antibiotics for more than seven days. Once again, it is likely that the patients in need for these treatments were in a more severe condition, which could explain the results, regardless of the possible impact on the response to ICI.
5.5. Importance of the Antibiotic Treatment Modality: Molecule and Spectrum
Antibiotics are a very large family of molecules, presenting different pharmacokinetics, pharmacodynamics, and activity spectra. In vitro studies showed maximal impact on microbiota with antibiotics having a strong activity on anaerobes (e.g., macrolides). Some studies have been able to differentiate the action of antibiotics on the results of immunotherapy according to their class. Ahmed et al. showed no impact on response rate with narrow Gram-positive spectrum antibiotics (vancomycin, daptomycin, linezolid), whereas broad spectrum antibiotics (e.g., β–lactams, quinolones, cyclines) affected both response rate and PFS [78]. Chalabi et al. examined the difference in OS between chemotherapy and atezolizumab (anti-PD-L1) for several antibiotic classes without showing any significantly impairing class for ICIs survival [79]. Because amoxicillin (AMX) is a widely used penicillin, alone or in association with clavulanic acid (AMC), it is interesting to note that Gaucher et al. found no difference in OS between patients treated with AMX versus AMC, nor between those treated with AMX or AMC versus other antibiotics [6].
However, Medik et al. presented interesting outcomes in mice treated with anti-CTLA-4 ICI and metronidazole. The antibiotic-induced shift in microbiome composition was associated with a favorable immune microenvironment and more complete tumor regression [80]. Using antibiotics to modulate the immune response through bacterial changes could represent an attractive way to improve the action of ICIs [81]. This has been explored with oral vancomycin in liver tumors: its action on bile acid metabolism has been associated with chemokine ligand CXCL16 expression. Monge et al. are conducting a Phase 2 single-arm trial of nivolumab with oral vancomycin and tadalafil, a phosphodiesterase inhibitor, in hepatocellular carcinoma (HCC) and liver-dominant metastatic digestive cancers (NCT03785210) [82].
6. Proton Pump Inhibitors
Proton pump inhibitors (PPIs) are very commonly used to treat peptic ulcers or gastroesophageal reflux disease or to prevent digestive complications due to non-steroidal anti-inflammatory drugs. Because of their low level of toxicities, they are often over-prescribed: up to 70% of PPIs prescriptions may be unnecessary and not grounded on evidence-based recommendations. Moreover, initial indication is rarely re-evaluated, leading to unjustified chronic use [5]. Since their arrival on the market in 1989, they have been suspected in association with numerous adverse events such as hypomagnesemia, vitamin B12 deficiency, bone fracture, or Clostridioides difficile infection [83]. Because oncology patients in particular often present previous comorbidities, inherent frailty, and potentially ulcer-inducing comedications, they are quite frequently treated with PPIs.
6.1. PPI-Induced Alterations of the Microbiota
Increased gastric pH caused by acid secretion blockade can lead to downstream disturbances in the equilibrium of gut flora, but PPIs can also generate pH-unrelated effects. Indeed, they are associated with hormonal disturbances (e.g., hypergastrinemia, hyperparathyroidism) and alterations in nutrient absorption [84]. Several studies and large population-based cohorts led to evidence of profound alteration in microbiota composition and diversity under PPI treatment [5,37]. These perturbations involve decreased gut commensal bacteria (e.g., Ruminococcacae, Bifidobacteriaceae) to the benefit of oral cavity microorganisms (e.g., Rothia dentocariosa, Rothia mucilaginosa, Actinomyces spp.) [5,85].
PPIs also induce favorable conditions for colonization by enteric pathogens leading in PPI-users-to-odds-ratio of 1.5 to 1.8 for C. difficile and 2 to 4 for other germs such as Campylobacter or Salmonella [86]. This pathogen spread might be promoted by alterations in colonic colonization resistance patterns, such as increased Lactobacillus spp. and decreased Bacteroidetes [84]. Similar alterations in bacterial orders have been found in PPI use-discordant monozygotic twins from the TwinsUK cohort, and with small interventional study [85]. Finally, PPIs are also associated with a 3-fold increase in risk of small intestinal bacterial overgrowth (SIBO), involving species like Escherichia coli, Enterococcus spp., or Klebsiella pneumoniae [84].
If gut flora perturbations contribute to the negative impact of PPIs on ICI survival, retuning the microbiota could be a means to restore ICI efficacy. Indeed, Tomita et al. reported significantly better OS and PFS in a small retrospective study among PPI-using patients with NSCLC treated with ICIs when receiving oral supplementation with Clostridium butyricum (OS: HR 0.42 [95% CI: 0.19, 0.92] p = 0.03; PFS: HR 0.52 [0.29, 0.94] p = 0.03). The oral supplementation was also associated in patients’ stools with decreased oral pathogens (e.g., Atopobium, Streptococcus) as well as increased gut bacteria Bifidobacterium spp., which has been associated with ICI efficacy in previous studies [87].
6.2. Impact on ICI Efficacy
Apart from their activity on the gastrointestinal microbiome, PPIs are thought to directly alter the inflammatory response, especially by decreasing the secretion of adhesion molecules by inflammatory cells and by inhibiting cytokines production [73]. Results of studies of PPIs’ impact on response and survival under ICI treatment are heterogeneous, as illustrated in Table 5. First studies looking for a detrimental impact of PPIs on ICI efficacy were post hoc analyses from pooled phase 2 and 3 randomized controlled trials. Pooled patients in atezolizumab arms presented significantly decreased OS and PFS when receiving prior or concomitant PPI, whereas survival in chemotherapy arms was not altered [79,88]. Subsequent large-scale retrospective studies are also discordant. Stokes et al. found no impact of PPIs on survival in more than 3500 ICI-treated veterans with NSCLC [89], while Baek et al. studied nearly 3000 patients with NSCLC receiving ICIs from the South Korean national health system and evidenced a significant decrease in OS due to PPI use [90]. Moreover, they evidenced stronger pejorative effect in “new PPI users”, defined as patients having initiated PPIs after a washout period of at least 180 days, suggesting a more deleterious action when the first PPI intake in a naive organism is closer to the initiation of ICI.

Table 5.
Studies analyzing the impact of proton pump inhibitors on response rate and survival with ICI and/or chemotherapy treatment [79,88,89,90,91].
6.3. Differences in Histology
Large meta-analyses have also led to divergent results as shown in Table 6. Subgroup analyses yielded some surprising results, like an inconsistently favorable effect of PPI use on survival in patients with melanoma. The two meta-analyses use the same retrospective studies, including the results of Failing et al. on 159 patients with melanoma at Mayo Clinic, whose results found a trend in this direction, although not significant [92]. All the meta-analyses seem to agree on decreased survival in patients with NSCLC [93,94,95,96], whereas no significant impact has been shown in patients with RCC, based on a pool of more than 400 patients [95].

Table 6.
Systematic reviews and meta-analyses on the impact of proton pump inhibitors on ICI treatment survival [93,94,95,96].
6.4. Importance of Timing
As well as with antibiotics, many studies reported in Table 1 evidenced a critical window associated with more negative results. This period involves about 30 days before and after the start of immunotherapy. Subgroup analyses investigating the effect of PPIs after initiation of ICI treatment do not evidence significant decreased survival [94,95]. Thus, the importance of a preserved gut microbiota during initial immune priming can once more be hypothesized.
7. Other Medications according to Pathway Alterations
7.1. Metabolism and Hypoxia Lowering: Metformin
Metformin is a widely prescribed blood glucose-lowering treatment and standard of care for type 2 diabetes. It amplifies insulin sensitivity and inhibits liver gluconeogenesis. Its complex mechanism of action is not entirely understood and is thought to involve the gut microbiota: interventional studies showed gut flora alteration in healthy volunteers receiving metformin. Interestingly, fecal transplantation from metformin-treated individuals induced lower blood glucose levels in germ-free mice [5,97]. Metformin especially favors the abundance of Akkermansia muciniphila, which independently enhances glucose tolerance in mice [98].
Its action on the mitochondrial metabolism chain also impacts the immune system by decreasing immune exhaustion and stimulating IL-10 secretion and CD8+ T-cells promotion, as well as cancer cells by diminishing intratumoral hypoxia [73,97,99]. Metformin also interacts with the PD-1/PD-L1 checkpoint pair: the degradation of membrane PD-L1 after metformin treatment has been evidenced in breast tumor mice models and confirmed in breast cancer samples of metformin-treated patients [100]. In vitro and animal experiments showed increased CD8+ T cell infiltration and enhanced efficacy of PD-1 inhibitor pembrolizumab in lung cancer when associated with metformin [101]. Moreover, intratumoral hypoxia has been associated with decreased efficacy of PD-1 blockade in murine models. That barrier to immunotherapy could be reduced by metformin-induced diminution of oxygen consumption in tumor cells, allowing for higher infiltration by T cells and better tumor response [102].
However, the objective impact of metformin on ICI efficacy in clinical practice has not been formally proven thus far. Afzal et al. evidenced longer OS and PFS in a small retrospective cohort of ICI-treated patients with metastatic melanoma receiving concomitant metformin (22/55 patients) without reaching statistical significance (OS: 46.7 m vs. 28 m, HR 0.40 [95% CI: 0.12, 1.35] p = 0.12; PFS: 19.8 m vs. 5 m, HR 0.55 [0.24, 1.24] p = 0.15) [103]. The same team published similar trends with patients with NSCLC: non-significant improvement in OS and PFS was found with concomitant metformin (21/50 patients; OS: 11.5 m vs. 7.6 m, HR 0.8 [95% CI: 0.39, 1.63] p = 0.5; PFS: 3 m vs. 4 m, HR 0.86 [0.47, 1.6] p = 0.6) [104]. Recently, Yang et al. found analogous results in a bigger cohort of 466 NSCLC patients. Eighty-nine patients (19%) received metformin from at least 8 weeks before ICI initiation. The study showed significantly higher ORR (24.7% vs. 14.8%, p = 0.025) and PFS (5.1 m vs. 2.8 m, HR 0.69 [95% CI: 0.52, 0.93] p = 0.013) without a difference in OS [105].
Phase 1 and 2 trials are currently open to prospectively assess a positive effect of concurrent metformin on anti-PD-1 and anti-PD-L1 treatment for different types of cancer: melanoma (NCT04114136), NSCLC (NCT03048500), or microsatellite stable (MSS) colorectal cancer (NCT03800602) [97,106,107].
7.2. Local Inflammation: Aspirin and Nonsteroidal Anti-Inflammatory Drugs
Aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs) act as more or less selective inhibitors of cyclooxygenases (COX1/COX2). These enzymes are involved in prostaglandins synthesis, including prostaglandin E2, which has been associated with tumor cell survival, growth, and invasion [108,109]. Moreover, in vivo studies showed the role of COX2 in ICIs resistance, notably by decreasing the infiltration of immune cells in the tumor environment. Pi et al. showed experimental reverse of pembrolizumab resistance in mice when combined with aspirin or NSAID celecoxib [109]. The benefit of aspirin on the response to ICIs could also involve its antiplatelet action: Riesenberg et al. showed improved anti-PD-1 response in vivo with aspirin and another antiplatelet agent, clopidogrel: tempering platelet activation could generate beneficial immune remodeling in the tumor microenvironment [110].
Once again, the transposition of these promising findings to patients has not yet yielded satisfactory results. Different studies specifically examined the impact of aspirin and/or NSAIDs on response and survival on ICIs [111,112,113]. The results, although not statistically significant, all support a deleterious association. However, the prescription of NSAIDs in oncology patients may be a significant bias due to their use for cancer pain and could reveal more active, aggressive, or rapidly progressing disease that would necessarily impair survival. In some studies, looking for several drugs’ impact on ICI survival that isolated low-dose aspirin from NSAIDs prescription, a favorable effect has been evidenced with aspirin. Cortellini et al. showed higher ORR (OR 1.47 [95% CI: 1.04, 2.08] p = 0.03) and longer PFS (HR 0.79 [0.64, 0.98] p = 0.03) in a 1012-patient retrospective study [114]. Zhang et al. compiled five studies with specific low dose aspirin subgroups in their meta-analysis and evidenced longer PFS (HR 0.84 [0.72, 0.98] p = 0.02) with no impact on OS [115].
7.3. Stress and Neuro-Oncology: Beta Blockers
The role of the β-adrenergic receptor has been recently highlighted in the tumor microenvironment, as well as its potential influence on cancer growth, invasion, and metastatic spreading [116,117]. The β-adrenergic receptor blockers, or beta blockers, are widely used treatments for hypertension, coronary heart disease, or arrhythmia. Because of the negative impact of stress-induced adrenergic signaling on the immune system, beta blockers have been thought to positively impact ICI efficacy. They have been reported to decrease tumor neoangiogenesis and to improve anti-CTLA-4 activity in mice models [118]. Kokolus et al. showed significantly higher OS in patients with metastatic melanoma receiving ICIs and/or interleukin 2 with concomitant beta blockers, and confirmed the results in a preclinical murine model [119]. Mellgard et al. found better disease control (ORR: OR 2.79 [1.54, 5.03] p = 0.001) with no impact on survival in a 339-patient cohort [120]. Similar results have been shown in other retrospective studies and meta-analyses [114,117]. Oh et al. evidenced beta blocker-associated longer PFS (HR 0.58 [0.36, 0.93]) without benefit on OS in a small retrospective study of 109 patients with NSCLC [121].
Finally, a phase 1 study by Gandhi et al. established a treatment dosing of 30 mg propranolol twice a day combined with pembrolizumab with satisfactory safety in melanoma [122]. Phase 2 trials are currently recruiting in order to test this potential positive association in triple negative breast cancer (NCT05741164), urothelial carcinoma (NCT04848519), or melanoma (NCT03384836). Again, biases on tumor response and survival are possible with beta blockers, even if they appear less obvious than with other molecules.
7.4. Microenvironment Remodeling and Immune Modulation
7.4.1. Renin-Angiotensin-Aldosterone System Inhibitors
The renin-angiotensin-aldosterone system (RAAS) is a key target for hypertension treatment. It is also thought to enable cancer cell growth and proliferation through its interaction with the tumor microenvironment, especially cancer-associated fibroblasts (CAFs). Angiotensin-receptor blockers (ARB) have been shown to reprogram CAFs to an immunosupportive state and to diminish T cell inhibition and immunosuppressive factor expression (e.g., interleukins 6 and 10) [123,124,125]. Moreover, RAAS inhibitors’ action on the tumor microenvironment involves blood vessel decompression and therefore better tumor perfusion, allowing for hypoxia alleviation and better drug delivery [126]. Chauhan et al. designed a tumor-selective ARB that has been associated with improved tumor T cell activity and increased ICI efficacy in animal models without blood pressure-lowering effects [125].
The results of real-life studies are divergent. Nuzzo et al. showed encouraging results in metastatic RCC with increased OS (HR 0.35 [0.17, 0.70] p = 0.003) and longer time to treatment failure (HR 0.57 [0.36, 0.92] p = 0.02) [127]. Drobni et al. showed higher OS with concurrent RAAS inhibitors in a large retrospective cohort of almost 6000 ICI-treated patients receiving diverse anti-hypertensive medication (HR 0.92 [0.85, 0.99] p = 0.03) [128]. However, Medjebar et al. found an opposite effect in a 178-patient retrospective study, with a decrease in PFS in patients receiving angiotensin-converting enzyme (ACE) inhibitors. Subsequent RNA sequencing of tumor samples suggested an immunosuppressed state in the ACE inhibitors group with a lower rate of M1 macrophages, activated mast cells, NK cells, and memory-activated T cells [129]. Further studies—ideally prospective—are still needed to answer the question and to prove a benefit in clinical practice.
7.4.2. Opioids
Strong analgesia is often needed due to intense cancer pain: opioids are therefore widely used in oncology. Morphine-like analgesics include numerous molecules (e.g., morphine, fentanyl, oxycodone, codeine) that have been thought to stimulate tumor progression and metastasis formation because of overexpressed opioid receptors on cancer cells. Their role has also been shown in impairing the immune system through T cell modulation and in gut flora alterations [130]. Hence, the impact of opioid treatments on ICI efficacy was the focus of several retrospective studies [131,132,133] and meta-analyses [134]. The results seem to be in favor of lower response rates and shorter PFS and OS.
Yet the breadth of difference in response (e.g., in Tanigushi et al. 2.6% vs. 13.5%) [132] or survival (e.g., in Botticelli et al. 3 vs. 19 months of PFS, and 4 vs. 35 months of OS) [133] suggests the existence of strong biases. The necessity of opioid use is indeed likely associated with poorer general condition, aggressive disease, or pejorative metastatic burden, and studies with a higher level of evidence, if possible, will be needed to conclude a real effect.
7.4.3. Statins
Statins are cholesterol-lowering agents commonly used in the primary and secondary prevention of cardiovascular disease. They have been thought to potentially interfere with ICI efficacy due to their immune modulation properties. In preclinical models, statins have been shown to inhibit PD-L1 expression on cancer cells by action on multiple signaling pathways such as RAS, AKT, or ꞵ-catenin. Their activity also involves enhanced T cell activity in tumor microenvironments as well as in draining lymph nodes [135,136,137]. Retrospective studies found improved survival in malignant pleural mesothelioma and NSCLC [138,139], but meta-analyses are discordant. Yongchao Zhang et al. showed longer OS and PFS based on five studies (OS: HR 0.76 [0.63, 0.92] p = 0.005; PFS: HR 0.86 [0.75, 0.99] p = 0.036) [115], while Lei Zhang et al. found no significant association between statin use and OS or PFS based on eight cohorts including 2382 patients [140]. Again, the evidence for a real impact on the efficacy of immunotherapy treatment is limited, and further study is needed.
8. Discussion
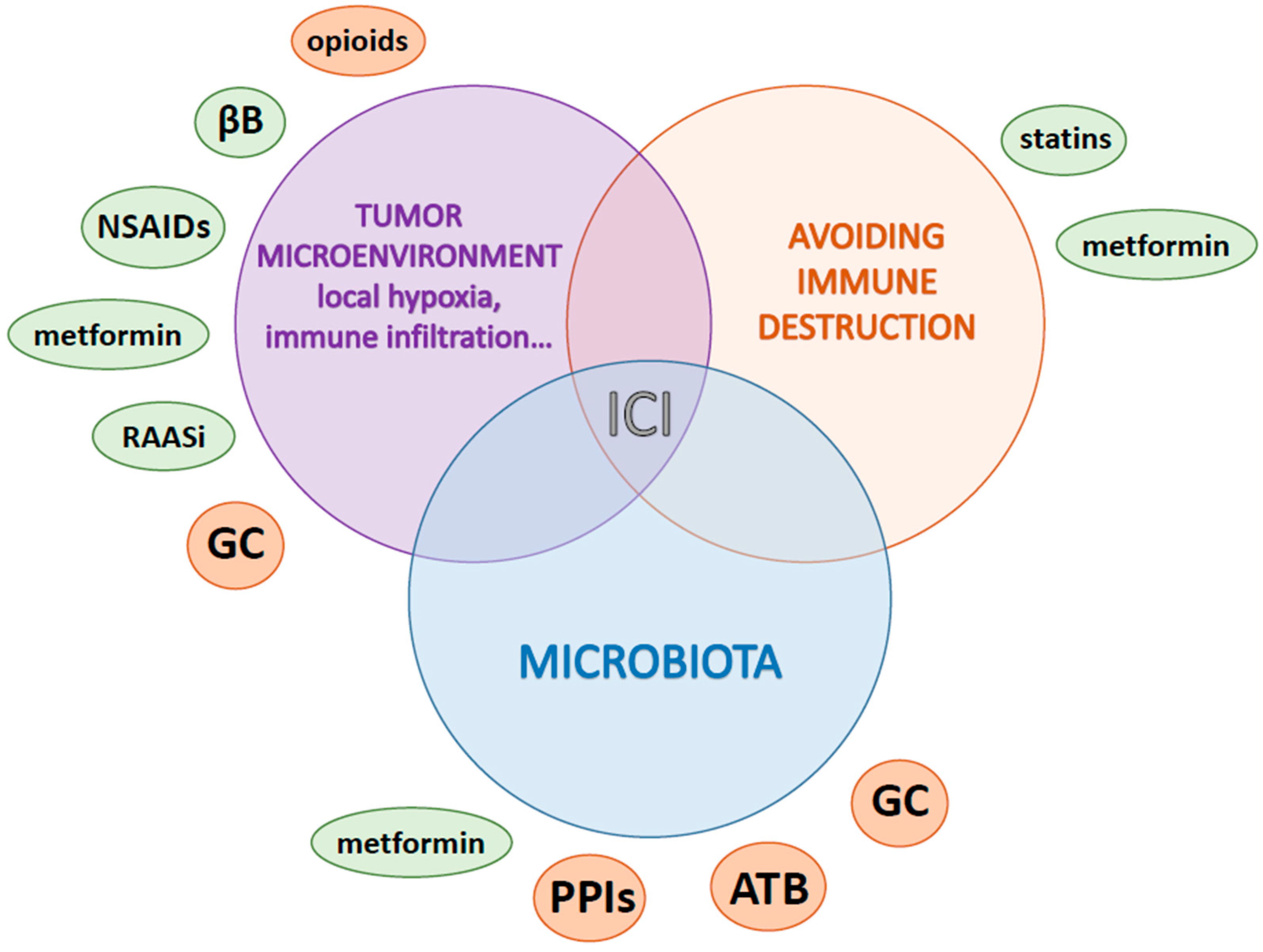
We showed that many studies have explored the potential impact of concurrent use of multiple therapeutics on the outcomes of ICI treatment, from in vitro and animal models to retrospective clinical studies. Described interactions are very diverse and can positively or negatively affect various cancer-promoting mechanisms, as well as several necessary factors for the functioning of ICIs. Figure 2 illustrates these complex linkages and interactions with some of the hallmarks of cancer proposed by Hanahan and Weinberg [141].
Figure 2.
Multiple interactions between drugs, cancer hallmarks and ICI efficacy (red/green: negative/positive impact on ICI efficacy, respectively; ICI: immune checkpoint inhibitor; GC: glucocorticoids; ATB: antibiotics; PPIs: proton pump inhibitors; NSAIDs: non-steroidal anti-inflammatory drugs and aspirin; ꞵB: beta blockers; RAASi: renin-angiotensin-aldosterone system inhibitors).
Positive or negative associations have been evidenced regarding response and survival outcomes, and it seems difficult for the clinician to determine the right therapeutic attitude in the patient’s best interest. Moreover, direct extrapolation of convincing in vitro or animal models’ results is not possible and proper randomized controlled trials cannot always be conducted for such issues. It is therefore necessary to rely on well-conducted retrospective studies and meta-analyses. They are not immune to many biases, in particular on the probability of a more precarious general condition due to comorbidities in patients requiring comedications, which independently affects their prognosis.
The results we gathered seem to show a detrimental association of corticosteroids given for supportive care reasons, as well as antibiotics and PPIs on objective response and survival, especially when used within a window of a few weeks before and/or after the start of ICI therapy. The first results concerning the other comedications (metformin, NSAIDs, beta blockers, RAAS antagonists, opioids, and statins) also call for caution. It should be kept in mind that any new drug introduction may have an unpredictable effect on expected oncologic outcomes and should not be minimized.
Yet, it is not always possible for the clinician to stop the treatments involved because of their often unquestionable necessity. One should however try to manage the timing of treatment as well as possible, even sometimes by delaying the ICI by a few weeks to allow time for the microbiota to recover and to ensure that the immunotherapy has not been initiated in a particularly deleterious period.
One should also ascertain the need to introduce a new concomitant treatment, according to evidence-based recommendations: for instance, avoiding prophylactic antibiotics or unjustified PPIs. Countermeasures like phages or histamine H2-receptor antagonists are suggested by Derosa et al. among other “microbiota-centered interventions” in immuno-oncology (e.g., intermittent fasting, fiber intake, aerobic and anaerobic physical exercise) [28].
If deleterious comedications are required, the possibility to initiate alternative oncological treatments such as chemotherapy or targeted therapy should be discussed. Buti et al. developed and validated a prognostic index based on OS under ICI treatment in patients with baseline comedications which might be helpful. Corticosteroids are assigned 2 points, antibiotics and PPIs 1 point each, generating a 3-risk group stratification that significantly predicted OS, PFS, and ORR in an external validation cohort: score 0 (good prognosis), score 1–2 (intermediate), 3–4 (poor) [142].
Finally, looking to the future of immunotherapy for solid tumors leads to a consideration of new ICI targets (e.g., TIGIT, LAG-3, TIM-3), new combinations [143], and new treatment classes such as vaccines and chimeric antigen receptors T cells (CAR T cells). Questions will arise as to their efficacy in real-life conditions, and studies must be conducted in order to know whether the interactions observed with anti-PD-(L)1 and anti-CTLA-4 will be confirmed with these new strategies.
9. Conclusions
We reported here the complex associations between the microbiota, the immune system, and immunotherapy response, as well as the promising results expected from microbiota adjustments, notably with the key commensal bacterium Akkermansia muciniphila. We gathered data on the negative impact of corticosteroids, antibiotics, and proton pump inhibitors on ICI efficacy, highlighting the critical period surrounding the initiation of immunotherapy and the interesting differences between palliative or non-palliative corticosteroids indications, narrow or broad spectrum antibiotics, and former or new PPIs users. We also gave the preliminary outcomes concerning the positive impact on ICI efficacy of several frequently prescribed medications such as metformin or beta blockers, although these conclusions need to be assessed in prospective trials.
Our review provides a practical tool for the clinician, showing the critical involvement of the microbiota in the efficacy of ICIs and the impact of many usual comedications on the oncological response. These results are intended to help clinicians for overall management of patients receiving immunotherapy, taking into account all the patient’s comedications to support these complex decisions.
Author Contributions
Conceptualization, J.C.-T., Q.D.T. and M.V.; writing—original draft preparation, J.C.-T.; writing—review and editing, Q.D.T. and M.V.; supervision, Q.D.T. and M.V. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
The authors would like to thank Victoria Baena for her careful review of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Carlino, M.S.; Larkin, J.; Long, G.V. Immune Checkpoint Inhibitors in Melanoma. Lancet 2021, 398, 1002–1014. [Google Scholar] [CrossRef]
- Vaddepally, R.K.; Kharel, P.; Pandey, R.; Garje, R.; Chandra, A.B. Review of Indications of FDA-Approved Immune Checkpoint Inhibitors per NCCN Guidelines with the Level of Evidence. Cancers 2020, 12, 738. [Google Scholar] [CrossRef]
- Ai, L.; Xu, A.; Xu, J. Roles of PD-1/PD-L1 Pathway: Signaling, Cancer, and Beyond. In Regulation of Cancer Immune Checkpoints; Xu, J., Ed.; Advances in Experimental Medicine and Biology; Springer: Singapore, 2020; Volume 1248, pp. 33–59. ISBN 9789811532658. [Google Scholar]
- Kalfeist, L.; Galland, L.; Ledys, F.; Ghiringhelli, F.; Limagne, E.; Ladoire, S. Impact of Glucocorticoid Use in Oncology in the Immunotherapy Era. Cells 2022, 11, 770. [Google Scholar] [CrossRef]
- Weersma, R.K.; Zhernakova, A.; Fu, J. Interaction between Drugs and the Gut Microbiome. Gut 2020, 69, 1510–1519. [Google Scholar] [CrossRef]
- Gaucher, L.; Adda, L.; Séjourné, A.; Joachim, C.; Guillaume, C.; Poulet, C.; Liabeuf, S.; Gras-Champel, V.; Masmoudi, K.; Houessinon, A.; et al. Associations between Dysbiosis-Inducing Drugs, Overall Survival and Tumor Response in Patients Treated with Immune Checkpoint Inhibitors. Ther. Adv. Med. Oncol. 2021, 13, 175883592110005. [Google Scholar] [CrossRef]
- D’Argenio, V.; Salvatore, F. The Role of the Gut Microbiome in the Healthy Adult Status. Clin. Chim. Acta 2015, 451, 97–102. [Google Scholar] [CrossRef]
- MetaHIT Consortium (Additional Members); Arumugam, M.; Raes, J.; Pelletier, E.; Le Paslier, D.; Yamada, T.; Mende, D.R.; Fernandes, G.R.; Tap, J.; Bruls, T.; et al. Enterotypes of the Human Gut Microbiome. Nature 2011, 473, 174–180. [Google Scholar] [CrossRef] [PubMed]
- Ni, J.; Wu, G.D.; Albenberg, L.; Tomov, V.T. Gut Microbiota and IBD: Causation or Correlation? Nat. Rev. Gastroenterol. Hepatol. 2017, 14, 573–584. [Google Scholar] [CrossRef]
- Pavel, F.M.; Vesa, C.M.; Gheorghe, G.; Diaconu, C.C.; Stoicescu, M.; Munteanu, M.A.; Babes, E.E.; Tit, D.M.; Toma, M.M.; Bungau, S. Highlighting the Relevance of Gut Microbiota Manipulation in Inflammatory Bowel Disease. Diagnostics 2021, 11, 1090. [Google Scholar] [CrossRef]
- Imdad, A.; Nicholson, M.R.; Tanner-Smith, E.E.; Zackular, J.P.; Gomez-Duarte, O.G.; Beaulieu, D.B.; Acra, S. Fecal Transplantation for Treatment of Inflammatory Bowel Disease. Cochrane Database Syst. Rev. 2018, 2018, CD012774. [Google Scholar] [CrossRef]
- Olivares, M.; Neef, A.; Castillejo, G.; Palma, G.D.; Varea, V.; Capilla, A.; Palau, F.; Nova, E.; Marcos, A.; Polanco, I.; et al. The HLA-DQ2 Genotype Selects for Early Intestinal Microbiota Composition in Infants at High Risk of Developing Coeliac Disease. Gut 2015, 64, 406–417. [Google Scholar] [CrossRef]
- Bisgaard, H.; Li, N.; Bonnelykke, K.; Chawes, B.L.K.; Skov, T.; Paludan-Müller, G.; Stokholm, J.; Smith, B.; Krogfelt, K.A. Reduced Diversity of the Intestinal Microbiota during Infancy Is Associated with Increased Risk of Allergic Disease at School Age. J. Allergy Clin. Immunol. 2011, 128, 646–652.e5. [Google Scholar] [CrossRef] [PubMed]
- Cox, A.J.; West, N.P.; Cripps, A.W. Obesity, Inflammation, and the Gut Microbiota. Lancet Diabetes Endocrinol. 2015, 3, 207–215. [Google Scholar] [CrossRef]
- Schirmer, M.; Smeekens, S.P.; Vlamakis, H.; Jaeger, M.; Oosting, M.; Franzosa, E.A.; ter Horst, R.; Jansen, T.; Jacobs, L.; Bonder, M.J.; et al. Linking the Human Gut Microbiome to Inflammatory Cytokine Production Capacity. Cell 2016, 167, 1125–1136.e8. [Google Scholar] [CrossRef] [PubMed]
- Lambring, C.B.; Siraj, S.; Patel, K.; Sankpal, U.T.; Mathew, S.; Basha, R. Impact of the Microbiome on the Immune System. Crit. Rev. Immunol. 2019, 39, 313–328. [Google Scholar] [CrossRef] [PubMed]
- Khosravi, A.; Yáñez, A.; Price, J.G.; Chow, A.; Merad, M.; Goodridge, H.S.; Mazmanian, S.K. Gut Microbiota Promote Hematopoiesis to Control Bacterial Infection. Cell Host Microbe 2014, 15, 374–381. [Google Scholar] [CrossRef]
- Tabowei, G.; Gaddipati, G.N.; Mukhtar, M.; Alzubaidee, M.J.; Dwarampudi, R.S.; Mathew, S.; Bichenapally, S.; Khachatryan, V.; Muazzam, A.; Hamal, C.; et al. Microbiota Dysbiosis a Cause of Colorectal Cancer or Not? A Systematic Review. Cureus 2022, 14, e30893. [Google Scholar] [CrossRef]
- Tuominen, H.; Rautava, J. Oral Microbiota and Cancer Development. Pathobiology 2021, 88, 116–126. [Google Scholar] [CrossRef]
- Ting, N.L.-N.; Lau, H.C.-H.; Yu, J. Cancer Pharmacomicrobiomics: Targeting Microbiota to Optimise Cancer Therapy Outcomes. Gut 2022, 71, 1412–1425. [Google Scholar] [CrossRef] [PubMed]
- Vétizou, M.; Pitt, J.M.; Daillère, R.; Lepage, P.; Waldschmitt, N.; Flament, C.; Rusakiewicz, S.; Routy, B.; Roberti, M.P.; Duong, C.P.M.; et al. Anticancer Immunotherapy by CTLA-4 Blockade Relies on the Gut Microbiota. Science 2015, 350, 1079–1084. [Google Scholar] [CrossRef]
- Sivan, A.; Corrales, L.; Hubert, N.; Williams, J.B.; Aquino-Michaels, K.; Earley, Z.M.; Benyamin, F.W.; Man Lei, Y.; Jabri, B.; Alegre, M.-L.; et al. Commensal Bifidobacterium Promotes Antitumor Immunity and Facilitates Anti–PD-L1 Efficacy. Science 2015, 350, 1084–1089. [Google Scholar] [CrossRef] [PubMed]
- Tanoue, T.; Morita, S.; Plichta, D.R.; Skelly, A.N.; Suda, W.; Sugiura, Y.; Narushima, S.; Vlamakis, H.; Motoo, I.; Sugita, K.; et al. A Defined Commensal Consortium Elicits CD8 T Cells and Anti-Cancer Immunity. Nature 2019, 565, 600–605. [Google Scholar] [CrossRef]
- Hibberd, A.A.; Lyra, A.; Ouwehand, A.C.; Rolny, P.; Lindegren, H.; Cedgård, L.; Wettergren, Y. Intestinal Microbiota Is Altered in Patients with Colon Cancer and Modified by Probiotic Intervention. BMJ Open Gastroenterol. 2017, 4, e000145. [Google Scholar] [CrossRef] [PubMed]
- Tomita, Y.; Ikeda, T.; Sakata, S.; Saruwatari, K.; Sato, R.; Iyama, S.; Jodai, T.; Akaike, K.; Ishizuka, S.; Saeki, S.; et al. Association of Probiotic Clostridium Butyricum Therapy with Survival and Response to Immune Checkpoint Blockade in Patients with Lung Cancer. Cancer Immunol. Res. 2020, 8, 1236–1242. [Google Scholar] [CrossRef] [PubMed]
- Routy, B.; Le Chatelier, E.; Derosa, L.; Duong, C.P.M.; Alou, M.T.; Daillère, R.; Fluckiger, A.; Messaoudene, M.; Rauber, C.; Roberti, M.P.; et al. Gut Microbiome Influences Efficacy of PD-1–Based Immunotherapy against Epithelial Tumors. Science 2018, 359, 91–97. [Google Scholar] [CrossRef]
- Derosa, L.; Routy, B.; Thomas, A.M.; Iebba, V.; Zalcman, G.; Friard, S.; Mazieres, J.; Audigier-Valette, C.; Moro-Sibilot, D.; Goldwasser, F.; et al. Intestinal Akkermansia Muciniphila Predicts Clinical Response to PD-1 Blockade in Patients with Advanced Non-Small-Cell Lung Cancer. Nat. Med. 2022, 28, 315–324. [Google Scholar] [CrossRef]
- Derosa, L.; Routy, B.; Desilets, A.; Daillère, R.; Terrisse, S.; Kroemer, G.; Zitvogel, L. Microbiota-Centered Interventions: The Next Breakthrough in Immuno-Oncology? Cancer Discov. 2021, 11, 2396–2412. [Google Scholar] [CrossRef] [PubMed]
- Cani, P.D.; Depommier, C.; Derrien, M.; Everard, A.; de Vos, W.M. Akkermansia Muciniphila: Paradigm for next-Generation Beneficial Microorganisms. Nat. Rev. Gastroenterol. Hepatol. 2022, 19, 625–637. [Google Scholar] [CrossRef]
- Yan, J.; Sheng, L.; Li, H. Akkermansia Muciniphila: Is It the Holy Grail for Ameliorating Metabolic Diseases? Gut Microbes 2021, 13, 1984104. [Google Scholar] [CrossRef]
- Ramírez-Labrada, A.G.; Isla, D.; Artal, A.; Arias, M.; Rezusta, A.; Pardo, J.; Gálvez, E.M. The Influence of Lung Microbiota on Lung Carcinogenesis, Immunity, and Immunotherapy. Trends Cancer 2020, 6, 86–97. [Google Scholar] [CrossRef]
- Hartmann, J.E.; Albrich, W.C.; Dmitrijeva, M.; Kahlert, C.R. The Effects of Corticosteroids on the Respiratory Microbiome: A Systematic Review. Front. Med. 2021, 8, 588584. [Google Scholar] [CrossRef] [PubMed]
- Bersanelli, M.; Santoni, M.; Ticinesi, A.; Buti, S. The Urinary Microbiome and Anticancer Immunotherapy: The Potentially Hidden Role of Unculturable Microbes. Target. Oncol. 2019, 14, 247–252. [Google Scholar] [CrossRef] [PubMed]
- Burcher, K.M.; Burcher, J.T.; Inscore, L.; Bloomer, C.H.; Furdui, C.M.; Porosnicu, M. A Review of the Role of Oral Microbiome in the Development, Detection, and Management of Head and Neck Squamous Cell Cancers. Cancers 2022, 14, 4116. [Google Scholar] [CrossRef] [PubMed]
- Hayes, R.B.; Ahn, J.; Fan, X.; Peters, B.A.; Ma, Y.; Yang, L.; Agalliu, I.; Burk, R.D.; Ganly, I.; Purdue, M.P.; et al. Association of Oral Microbiome With Risk for Incident Head and Neck Squamous Cell Cancer. JAMA Oncol. 2018, 4, 358. [Google Scholar] [CrossRef]
- Ferris, R.L.; Blumenschein, G.; Harrington, K.; Fayette, J.; Guigay, J.; Colevas, A.D.; Licitra, L.; Vokes, E.; Gillison, M.; Even, C.; et al. Abstract CT022: Evaluation of Oral Microbiome Profiling as a Response Biomarker in Squamous Cell Carcinoma of the Head and Neck: Analyses from CheckMate 141. Cancer Res. 2017, 77, CT022. [Google Scholar] [CrossRef]
- Bonder, M.J.; Tigchelaar, E.F.; Cai, X.; Trynka, G.; Cenit, M.C.; Hrdlickova, B.; Zhong, H.; Vatanen, T.; Gevers, D.; Wijmenga, C.; et al. The Influence of a Short-Term Gluten-Free Diet on the Human Gut Microbiome. Genome Med. 2016, 8, 45. [Google Scholar] [CrossRef]
- Jackson, M.A.; Verdi, S.; Maxan, M.-E.; Shin, C.M.; Zierer, J.; Bowyer, R.C.E.; Martin, T.; Williams, F.M.K.; Menni, C.; Bell, J.T.; et al. Gut Microbiota Associations with Common Diseases and Prescription Medications in a Population-Based Cohort. Nat. Commun. 2018, 9, 2655. [Google Scholar] [CrossRef]
- Falony, G.; Joossens, M.; Vieira-Silva, S.; Wang, J.; Darzi, Y.; Faust, K.; Kurilshikov, A.; Bonder, M.J.; Valles-Colomer, M.; Vandeputte, D.; et al. Population-Level Analysis of Gut Microbiome Variation. Science 2016, 352, 560–564. [Google Scholar] [CrossRef]
- Ticinesi, A.; Milani, C.; Lauretani, F.; Nouvenne, A.; Mancabelli, L.; Lugli, G.A.; Turroni, F.; Duranti, S.; Mangifesta, M.; Viappiani, A.; et al. Gut Microbiota Composition Is Associated with Polypharmacy in Elderly Hospitalized Patients. Sci. Rep. 2017, 7, 11102. [Google Scholar] [CrossRef]
- Gemikonakli, G.; Mach, J.; Zhang, F.; Bullock, M.; Tran, T.; El-Omar, E.; Hilmer, S.N. Polypharmacy with High Drug Burden Index (DBI) Alters the Gut Microbiome Overriding Aging Effects and Is Reversible with Deprescribing. J. Gerontol. Ser. A 2022, 78, 213–222. [Google Scholar] [CrossRef]
- Petrelli, F.; Signorelli, D.; Ghidini, M.; Ghidini, A.; Pizzutilo, E.G.; Ruggieri, L.; Cabiddu, M.; Borgonovo, K.; Dognini, G.; Brighenti, M.; et al. Association of Steroids Use with Survival in Patients Treated with Immune Checkpoint Inhibitors: A Systematic Review and Meta-Analysis. Cancers 2020, 12, 546. [Google Scholar] [CrossRef] [PubMed]
- Ramamoorthy, S.; Cidlowski, J.A. Corticosteroids. Rheum. Dis. Clin. N. Am. 2016, 42, 15–31. [Google Scholar] [CrossRef] [PubMed]
- Acuna, S.A. Etiology of Increased Cancer Incidence after Solid Organ Transplantation. Transplant. Rev. 2018, 32, 218–224. [Google Scholar] [CrossRef]
- Guba, M.; Graeb, C.; Jauch, K.-W.; Geissler, E.K. Pro- and anti-cancer effects of immunosuppressive agents used in organ transplantation. Transplantation 2004, 77, 1777–1782. [Google Scholar] [CrossRef] [PubMed]
- Walker, S.E.; Anver, M.R.; Schechter, S.L.; Bole, G.G. Prolonged Lifespan and High Incidence of Neoplasms in NZB/NZW Mice Treated with Hydrocortisone Sodium Succinate. Kidney Int. 1978, 14, 151–157. [Google Scholar] [CrossRef]
- Chong, P.P.; Koh, A.Y. The Gut Microbiota in Transplant Patients. Blood Rev. 2020, 39, 100614. [Google Scholar] [CrossRef]
- Tourret, J.; Willing, B.P.; Dion, S.; MacPherson, J.; Denamur, E.; Finlay, B.B. Immunosuppressive Treatment Alters Secretion of Ileal Antimicrobial Peptides and Gut Microbiota, and Favors Subsequent Colonization by Uropathogenic Escherichia coli. Transplantation 2017, 101, 74–82. [Google Scholar] [CrossRef]
- Wu, T.; Yang, L.; Jiang, J.; Ni, Y.; Zhu, J.; Zheng, X.; Wang, Q.; Lu, X.; Fu, Z. Chronic Glucocorticoid Treatment Induced Circadian Clock Disorder Leads to Lipid Metabolism and Gut Microbiota Alterations in Rats. Life Sci. 2018, 192, 173–182. [Google Scholar] [CrossRef]
- Huang, E.Y.; Inoue, T.; Leone, V.A.; Dalal, S.; Touw, K.; Wang, Y.; Musch, M.W.; Theriault, B.; Higuchi, K.; Donovan, S.; et al. Using Corticosteroids to Reshape the Gut Microbiome: Implications for Inflammatory Bowel Diseases. Inflamm. Bowel Dis. 2015, 21, 963–972. [Google Scholar] [CrossRef]
- Arbour, K.C.; Mezquita, L.; Long, N.; Rizvi, H.; Auclin, E.; Ni, A.; Martínez-Bernal, G.; Ferrara, R.; Lai, W.V.; Hendriks, L.E.L.; et al. Impact of Baseline Steroids on Efficacy of Programmed Cell Death-1 and Programmed Death-Ligand 1 Blockade in Patients With Non–Small-Cell Lung Cancer. J. Clin. Oncol. 2018, 36, 2872–2878. [Google Scholar] [CrossRef]
- Scott, S.C.; Pennell, N.A. Early Use of Systemic Corticosteroids in Patients with Advanced NSCLC Treated with Nivolumab. J. Thorac. Oncol. 2018, 13, 1771–1775. [Google Scholar] [CrossRef] [PubMed]
- Ricciuti, B.; Dahlberg, S.E.; Adeni, A.; Sholl, L.M.; Nishino, M.; Awad, M.M. Immune Checkpoint Inhibitor Outcomes for Patients with Non–Small-Cell Lung Cancer Receiving Baseline Corticosteroids for Palliative Versus Nonpalliative Indications. J. Clin. Oncol. 2019, 37, 1927–1934. [Google Scholar] [CrossRef] [PubMed]
- Margolin, K.; Ernstoff, M.S.; Hamid, O.; Lawrence, D.; McDermott, D.; Puzanov, I.; Wolchok, J.D.; Clark, J.I.; Sznol, M.; Logan, T.F.; et al. Ipilimumab in Patients with Melanoma and Brain Metastases: An Open-Label, Phase 2 Trial. Lancet Oncol. 2012, 13, 459–465. [Google Scholar] [CrossRef]
- Chasset, F.; Pages, C.; Biard, L.; Roux, J.; Sidina, I.; Madelaine, I.; Basset-Seguin, N.; Viguier, M.; Madjlessi-EzrA, N.; Schneider, P.; et al. Single-Center Study under a French Temporary Authorization for Use (TAU) Protocol for Ipilimumab in Metastatic Melanoma: Negative Impact of Baseline Corticosteroids. Eur. J. Dermatol. 2015, 25, 36–44. [Google Scholar] [CrossRef]
- Hendriks, L.E.L.; Henon, C.; Auclin, E.; Mezquita, L.; Ferrara, R.; Audigier-Valette, C.; Mazieres, J.; Lefebvre, C.; Rabeau, A.; Le Moulec, S.; et al. Outcome of Patients with Non–Small Cell Lung Cancer and Brain Metastases Treated with Checkpoint Inhibitors. J. Thorac. Oncol. 2019, 14, 1244–1254. [Google Scholar] [CrossRef] [PubMed]
- Pinato, D.J.; Kaseb, A.; Wang, Y.; Saeed, A.; Szafron, D.; Jun, T.; Dharmapuri, S.; Naqash, A.R.; Muzaffar, M.; Navaid, M.; et al. Impact of Corticosteroid Therapy on the Outcomes of Hepatocellular Carcinoma Treated with Immune Checkpoint Inhibitor Therapy. J. Immunother. Cancer 2020, 8, e000726. [Google Scholar] [CrossRef]
- Umehara, K.; Yama, K.; Goto, K.; Wakamoto, A.; Hatsuyama, T.; Honjo, O.; Saikai, T.; Fujita, A.; Sato, H. Effect of Systemic Corticosteroid Therapy on the Efficacy and Safety of Nivolumab in the Treatment of Non-Small-Cell Lung Cancer. Cancer Control 2021, 28, 107327482098579. [Google Scholar] [CrossRef]
- Gaucher, L.; Adda, L.; Séjourné, A.; Joachim, C.; Chaby, G.; Poulet, C.; Liabeuf, S.; Gras-Champel, V.; Masmoudi, K.; Moreira, A.; et al. Impact of the Corticosteroid Indication and Administration Route on Overall Survival and the Tumor Response after Immune Checkpoint Inhibitor Initiation. Ther. Adv. Med. Oncol. 2021, 13, 175883592199665. [Google Scholar] [CrossRef]
- Zhang, H.; Li, X.; Huang, X.; Li, J.; Ma, H.; Zeng, R. Impact of Corticosteroid Use on Outcomes of Non–Small-cell Lung Cancer Patients Treated with Immune Checkpoint Inhibitors: A Systematic Review and Meta-analysis. J. Clin. Pharm. Ther. 2021, 46, 927–935. [Google Scholar] [CrossRef]
- Jessurun, C.A.C.; Hulsbergen, A.F.C.; de Wit, A.E.; Tewarie, I.A.; Snijders, T.J.; Verhoeff, J.J.C.; Phillips, J.G.; Reardon, D.A.; Mekary, R.A.; Broekman, M.L.D. The Combined Use of Steroids and Immune Checkpoint Inhibitors in Brain Metastasis Patients: A Systematic Review and Meta-Analysis. Neuro-Oncology 2021, 23, 1261–1272. [Google Scholar] [CrossRef]
- Korpela, K.; de Vos, W. Antibiotic Use in Childhood Alters the Gut Microbiota and Predisposes to Overweight. Microb. Cell 2016, 3, 296–298. [Google Scholar] [CrossRef] [PubMed]
- Arrieta, M.-C.; Stiemsma, L.T.; Dimitriu, P.A.; Thorson, L.; Russell, S.; Yurist-Doutsch, S.; Kuzeljevic, B.; Gold, M.J.; Britton, H.M.; Lefebvre, D.L.; et al. Early Infancy Microbial and Metabolic Alterations Affect Risk of Childhood Asthma. Sci. Transl. Med. 2015, 7, 307ra152. [Google Scholar] [CrossRef] [PubMed]
- Modi, S.R.; Collins, J.J.; Relman, D.A. Antibiotics and the Gut Microbiota. J. Clin. Investig. 2014, 124, 4212–4218. [Google Scholar] [CrossRef] [PubMed]
- Jakobsson, H.E.; Jernberg, C.; Andersson, A.F.; Sjölund-Karlsson, M.; Jansson, J.K.; Engstrand, L. Short-Term Antibiotic Treatment Has Differing Long-Term Impacts on the Human Throat and Gut Microbiome. PLoS ONE 2010, 5, e9836. [Google Scholar] [CrossRef] [PubMed]
- Simin, J.; Fornes, R.; Liu, Q.; Olsen, R.S.; Callens, S.; Engstrand, L.; Brusselaers, N. Antibiotic Use and Risk of Colorectal Cancer: A Systematic Review and Dose–Response Meta-Analysis. Br. J. Cancer 2020, 123, 1825–1832. [Google Scholar] [CrossRef] [PubMed]
- Gagnière, J. Gut Microbiota Imbalance and Colorectal Cancer. World J. Gastroenterol. 2016, 22, 501. [Google Scholar] [CrossRef]
- Derosa, L.; Hellmann, M.D.; Spaziano, M.; Halpenny, D.; Fidelle, M.; Rizvi, H.; Long, N.; Plodkowski, A.J.; Arbour, K.C.; Chaft, J.E.; et al. Negative Association of Antibiotics on Clinical Activity of Immune Checkpoint Inhibitors in Patients with Advanced Renal Cell and Non-Small-Cell Lung Cancer. Ann. Oncol. 2018, 29, 1437–1444. [Google Scholar] [CrossRef]
- Pinato, D.J.; Howlett, S.; Ottaviani, D.; Urus, H.; Patel, A.; Mineo, T.; Brock, C.; Power, D.; Hatcher, O.; Falconer, A.; et al. Association of Prior Antibiotic Treatment with Survival and Response to Immune Checkpoint Inhibitor Therapy in Patients with Cancer. JAMA Oncol. 2019, 5, 1774. [Google Scholar] [CrossRef]
- Tinsley, N.; Zhou, C.; Tan, G.; Rack, S.; Lorigan, P.; Blackhall, F.; Krebs, M.; Carter, L.; Thistlethwaite, F.; Graham, D.; et al. Cumulative Antibiotic Use Significantly Decreases Efficacy of Checkpoint Inhibitors in Patients with Advanced Cancer. Oncologist 2020, 25, 55–63. [Google Scholar] [CrossRef]
- Cortellini, A.; Di Maio, M.; Nigro, O.; Leonetti, A.; Cortinovis, D.L.; Aerts, J.G.; Guaitoli, G.; Barbieri, F.; Giusti, R.; Ferrara, M.G.; et al. Differential Influence of Antibiotic Therapy and Other Medications on Oncological Outcomes of Patients with Non-Small Cell Lung Cancer Treated with First-Line Pembrolizumab versus Cytotoxic Chemotherapy. J. Immunother. Cancer 2021, 9, e002421. [Google Scholar] [CrossRef]
- Cortellini, A.; Ricciuti, B.; Facchinetti, F.; Alessi, J.V.M.; Venkatraman, D.; Dall’Olio, F.G.; Cravero, P.; Vaz, V.R.; Ottaviani, D.; Majem, M.; et al. Antibiotic-Exposed Patients with Non-Small-Cell Lung Cancer Preserve Efficacy Outcomes Following First-Line Chemo-Immunotherapy. Ann. Oncol. 2021, 32, 1391–1399. [Google Scholar] [CrossRef] [PubMed]
- Hussain, N.; Naeem, M.; Pinato, D.J. Concomitant Medications and Immune Checkpoint Inhibitor Therapy for Cancer: Causation or Association? Hum. Vaccines Immunother. 2021, 17, 55–61. [Google Scholar] [CrossRef]
- Lurienne, L.; Cervesi, J.; Duhalde, L.; de Gunzburg, J.; Andremont, A.; Zalcman, G.; Buffet, R.; Bandinelli, P.-A. NSCLC Immunotherapy Efficacy and Antibiotic Use: A Systematic Review and Meta-Analysis. J. Thorac. Oncol. 2020, 15, 1147–1159. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Xu, X.; Wang, H.; Ge, W.; Cao, D. The Association between Antibiotics Use and Outcome of Cancer Patients Treated with Immune Checkpoint Inhibitors: A Systematic Review and Meta-Analysis. Crit. Rev. Oncol. Hematol. 2020, 149, 102909. [Google Scholar] [CrossRef] [PubMed]
- Wu, Q.; Liu, J.; Wu, S.; Xie, X. The Impact of Antibiotics on Efficacy of Immune Checkpoint Inhibitors in Malignancies: A Study Based on 44 Cohorts. Int. Immunopharmacol. 2021, 92, 107303. [Google Scholar] [CrossRef]
- Luo, Z.; Hao, S.; Li, Y.; Cheng, L.; Zhou, X.; Gunes, E.G.; Liu, S.; Chen, J. The Negative Effect of Antibiotics on RCC Patients with Immunotherapy: A Systematic Review and Meta-Analysis. Front. Immunol. 2022, 13, 1065004. [Google Scholar] [CrossRef]
- Ahmed, J.; Kumar, A.; Parikh, K.; Anwar, A.; Knoll, B.M.; Puccio, C.; Chun, H.; Fanucchi, M.; Lim, S.H. Use of Broad-Spectrum Antibiotics Impacts Outcome in Patients Treated with Immune Checkpoint Inhibitors. OncoImmunology 2018, 7, e1507670. [Google Scholar] [CrossRef]
- Chalabi, M.; Cardona, A.; Nagarkar, D.R.; Dhawahir Scala, A.; Gandara, D.R.; Rittmeyer, A.; Albert, M.L.; Powles, T.; Kok, M.; Herrera, F.G. Efficacy of Chemotherapy and Atezolizumab in Patients with Non-Small-Cell Lung Cancer Receiving Antibiotics and Proton Pump Inhibitors: Pooled Post Hoc Analyses of the OAK and POPLAR Trials. Ann. Oncol. 2020, 31, 525–531. [Google Scholar] [CrossRef]
- Medik, Y.B.; Zhou, Y.; Kahn, L.M.; Patel, B.; Babcock, R.L.; Chrisikos, T.T.; Wan, X.; Dyevoich, A.; Ajami, N.J.; Wargo, J.A.; et al. Outcome of Concurrent Treatment with A-CTLA4 and Metronidazole in Murine Model of Colon Adenocarcinoma. J. Clin. Oncol. 2021, 39, e14566. [Google Scholar] [CrossRef]
- Cortellini, A.; Facchinetti, F.; Derosa, L.; Pinato, D.J. Antibiotic Exposure and Immune Checkpoint Inhibitors in Patients With NSCLC: The Backbone Matters. J. Thorac. Oncol. 2022, 17, 739–741. [Google Scholar] [CrossRef]
- Monge, B.M.C.; Xie, C.; Mabry-Hrones, D.; Wood, B.J.; Steinberg, S.M.; Kleiner, D.E.; Greten, T.F. Phase II Study of Nivolumab (Anti-PD1), Tadalafil, and Oral Vancomycin in Patients with Refractory Primary Hepatocellular Carcinoma or Liver Dominant Metastatic Cancer from Colorectal or Pancreatic Cancers. J. Clin. Oncol. 2020, 38, TPS4656. [Google Scholar] [CrossRef]
- Nehra, A.K.; Alexander, J.A.; Loftus, C.G.; Nehra, V. Proton Pump Inhibitors: Review of Emerging Concerns. Mayo Clin. Proc. 2018, 93, 240–246. [Google Scholar] [CrossRef]
- Freedberg, D.E.; Lebwohl, B.; Abrams, J.A. The Impact of Proton Pump Inhibitors on the Human Gastrointestinal Microbiome. Clin. Lab. Med. 2014, 34, 771–785. [Google Scholar] [CrossRef]
- Jackson, M.A.; Goodrich, J.K.; Maxan, M.-E.; Freedberg, D.E.; Abrams, J.A.; Poole, A.C.; Sutter, J.L.; Welter, D.; Ley, R.E.; Bell, J.T.; et al. Proton Pump Inhibitors Alter the Composition of the Gut Microbiota. Gut 2016, 65, 749–756. [Google Scholar] [CrossRef]
- Leonard, J.; Marshall, J.K.; Moayyedi, P. Systematic Review of the Risk of Enteric Infection in Patients Taking Acid Suppression. Am. J. Gastroenterol. 2007, 102, 2047–2056. [Google Scholar] [CrossRef] [PubMed]
- Tomita, Y.; Goto, Y.; Sakata, S.; Imamura, K.; Minemura, A.; Oka, K.; Hayashi, A.; Jodai, T.; Akaike, K.; Anai, M.; et al. Clostridium Butyricum Therapy Restores the Decreased Efficacy of Immune Checkpoint Blockade in Lung Cancer Patients Receiving Proton Pump Inhibitors. OncoImmunology 2022, 11, 2081010. [Google Scholar] [CrossRef]
- Hopkins, A.M.; Kichenadasse, G.; Karapetis, C.S.; Rowland, A.; Sorich, M.J. Concomitant Proton Pump Inhibitor Use and Survival in Urothelial Carcinoma Treated with Atezolizumab. Clin. Cancer Res. 2020, 26, 5487–5493. [Google Scholar] [CrossRef] [PubMed]
- Stokes, W.A.; Behera, M.; Jiang, R.; Gutman, D.; Giuste, F.; Burns, A.; Sebastian, N.; Ramalingam, S.; Sukhatme, V.; Lowe, M.C.; et al. Association of Proton Pump Inhibitors with Survival in Veterans with Non-Small Cell Lung Cancer Receiving Immunotherapy. J. Clin. Oncol. 2021, 39, e18729. [Google Scholar] [CrossRef]
- Baek, Y.; Kang, E.J.; Hong, S.; Park, S.; Kim, J.H.; Shin, J. Survival Outcomes of Patients with Nonsmall Cell Lung Cancer Concomitantly Receiving Proton Pump Inhibitors and Immune Checkpoint Inhibitors. Int. J. Cancer 2022, 150, 1291–1300. [Google Scholar] [CrossRef]
- Peng, K.; Chen, K.; Teply, B.A.; Yee, G.C.; Farazi, P.A.; Lyden, E.R. Impact of Proton Pump Inhibitor Use on the Effectiveness of Immune Checkpoint Inhibitors in Advanced Cancer Patients. Ann. Pharmacother. 2022, 56, 377–386. [Google Scholar] [CrossRef]
- Failing, J.J.; Finnes, H.D.; Kottschade, L.A.; Allred, J.B.; Markovic, S.N. Effects of Commonly Used Chronic Medications on the Outcomes of Ipilimumab Therapy in Patients with Metastatic Melanoma. Melanoma Res. 2016, 26, 609–615. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Zeng, C.; Yao, J.; Ge, Y.; An, G. The Association between Proton Pump Inhibitors Use and Clinical Outcome of Patients Receiving Immune Checkpoint Inhibitors Therapy. Int. Immunopharmacol. 2020, 88, 106972. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Guo, H.; Mao, H.; Tong, J.; Yang, M.; Yan, X. An Up-To-Date Investigation Into the Correlation Between Proton Pump Inhibitor Use and the Clinical Efficacy of Immune Checkpoint Inhibitors in Advanced Solid Cancers: A Systematic Review and Meta-Analysis. Front. Oncol. 2022, 12, 753234. [Google Scholar] [CrossRef]
- Chen, B.; Yang, C.; Dragomir, M.P.; Chi, D.; Chen, W.; Horst, D.; Calin, G.A.; Li, Q. Association of Proton Pump Inhibitor Use with Survival Outcomes in Cancer Patients Treated with Immune Checkpoint Inhibitors: A Systematic Review and Meta-Analysis. Ther. Adv. Med. Oncol. 2022, 14, 175883592211117. [Google Scholar] [CrossRef] [PubMed]
- Dar, S.; Merza, N.; Rahim, M.; Qatani, A.; Varughese, T.; Mohammad, A.; Masood, F.; Reza, F.; Shucenwan; Almas, T.; et al. Impact of Proton-Pump Inhibitors on the Efficacy of Immune Checkpoint Inhibitors in Non-Small Cell Lung Cancer: A Systematic Review and Meta-Analysis. Ann. Med. Surg. 2022, 78, 103752. [Google Scholar] [CrossRef]
- Verdura, S.; Cuyàs, E.; Martin-Castillo, B.; Menendez, J.A. Metformin as an Archetype Immuno-Metabolic Adjuvant for Cancer Immunotherapy. OncoImmunology 2019, 8, e1633235. [Google Scholar] [CrossRef]
- Shin, N.-R.; Lee, J.-C.; Lee, H.-Y.; Kim, M.-S.; Whon, T.W.; Lee, M.-S.; Bae, J.-W. An Increase in the Akkermansia Spp. Population Induced by Metformin Treatment Improves Glucose Homeostasis in Diet-Induced Obese Mice. Gut 2014, 63, 727–735. [Google Scholar] [CrossRef]
- Munoz, L.E.; Huang, L.; Bommireddy, R.; Sharma, R.; Monterroza, L.; Guin, R.N.; Samaranayake, S.G.; Pack, C.D.; Ramachandiran, S.; Reddy, S.J.C.; et al. Metformin Reduces PD-L1 on Tumor Cells and Enhances the Anti-Tumor Immune Response Generated by Vaccine Immunotherapy. J. Immunother. Cancer 2021, 9, e002614. [Google Scholar] [CrossRef]
- Cha, J.-H.; Yang, W.-H.; Xia, W.; Wei, Y.; Chan, L.-C.; Lim, S.-O.; Li, C.-W.; Kim, T.; Chang, S.-S.; Lee, H.-H.; et al. Metformin Promotes Antitumor Immunity via Endoplasmic-Reticulum-Associated Degradation of PD-L1. Mol. Cell 2018, 71, 606–620.e7. [Google Scholar] [CrossRef]
- Wang, Z.; Lu, C.; Zhang, K.; Lin, C.; Wu, F.; Tang, X.; Wu, D.; Dou, Y.; Han, R.; Wang, Y.; et al. Metformin Combining PD-1 Inhibitor Enhanced Anti-Tumor Efficacy in STK11 Mutant Lung Cancer Through AXIN-1-Dependent Inhibition of STING Ubiquitination. Front. Mol. Biosci. 2022, 9, 780200. [Google Scholar] [CrossRef]
- Scharping, N.E.; Menk, A.V.; Whetstone, R.D.; Zeng, X.; Delgoffe, G.M. Efficacy of PD-1 Blockade Is Potentiated by Metformin-Induced Reduction of Tumor Hypoxia. Cancer Immunol. Res. 2017, 5, 9–16. [Google Scholar] [CrossRef]
- Afzal, M.Z.; Mercado, R.R.; Shirai, K. Efficacy of Metformin in Combination with Immune Checkpoint Inhibitors (Anti-PD-1/Anti-CTLA-4) in Metastatic Malignant Melanoma. J. Immunother. Cancer 2018, 6, 64. [Google Scholar] [CrossRef]
- Afzal, M.Z.; Dragnev, K.; Sarwar, T.; Shirai, K. Clinical Outcomes in Non-Small-Cell Lung Cancer Patients Receiving Concurrent Metformin and Immune Checkpoint Inhibitors. Lung Cancer Manag. 2019, 8, LMT11. [Google Scholar] [CrossRef]
- Yang, J.; Kim, S.H.; Jung, E.H.; Kim, S.; Suh, K.J.; Lee, J.Y.; Kim, J.; Kim, J.W.; Lee, J.; Kim, Y.J.; et al. The Effect of Metformin or Dipeptidyl Peptidase 4 Inhibitors on Clinical Outcomes in Metastatic Non-small Cell Lung Cancer Treated with Immune Checkpoint Inhibitors. Thorac. Cancer 2023, 14, 52–60. [Google Scholar] [CrossRef]
- Liu, W.; Wang, Y.; Luo, J.; Liu, M.; Luo, Z. Pleiotropic Effects of Metformin on the Antitumor Efficiency of Immune Checkpoint Inhibitors. Front. Immunol. 2021, 11, 586760. [Google Scholar] [CrossRef] [PubMed]
- Kubo, T.; Ninomiya, T.; Hotta, K.; Kozuki, T.; Toyooka, S.; Okada, H.; Fujiwara, T.; Udono, H.; Kiura, K. Study Protocol: Phase-Ib Trial of Nivolumab Combined With Metformin for Refractory/Recurrent Solid Tumors. Clin. Lung Cancer 2018, 19, e861–e864. [Google Scholar] [CrossRef]
- Kunzmann, A.T.; Murray, L.J.; Cardwell, C.R.; McShane, C.M.; McMenamin, Ú.C.; Cantwell, M.M. PTGS2 (Cyclooxygenase-2) Expression and Survival among Colorectal Cancer Patients: A Systematic Review. Cancer Epidemiol. Biomark. Prev. 2013, 22, 1490–1497. [Google Scholar] [CrossRef]
- Pi, C.; Jing, P.; Li, B.; Feng, Y.; Xu, L.; Xie, K.; Huang, T.; Xu, X.; Gu, H.; Fang, J. Reversing PD-1 Resistance in B16F10 Cells and Recovering Tumour Immunity Using a COX2 Inhibitor. Cancers 2022, 14, 4134. [Google Scholar] [CrossRef] [PubMed]
- Riesenberg, B.P.; Ansa-Addo, E.A.; Gutierrez, J.; Timmers, C.D.; Liu, B.; Li, Z. Cutting Edge: Targeting Thrombocytes to Rewire Anticancer Immunity in the Tumor Microenvironment and Potentiate Efficacy of PD-1 Blockade. J. Immunol. 2019, 203, 1105–1110. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Kumar, P.; Adashek, J.J.; Skelton, W.P.; Li, J.; Vosoughi, A.; Chahoud, J.; Manley, B.J.; Spiess, P.E. Adding Cyclooxygenase Inhibitors to Immune Checkpoint Inhibitors Did Not Improve Outcomes in Metastatic Renal Cell Carcinoma. Cells 2022, 11, 2505. [Google Scholar] [CrossRef]
- Aiad, M.; Tahir, A.; Fresco, K.; Prenatt, Z.; Ramos-Feliciano, K.; Walia, J.; Stoltzfus, J.; Albandar, H.J. Does the Combined Use of Aspirin and Immunotherapy Result in Better Outcomes in Non-Small Cell Lung Cancer Than Immunotherapy Alone? Cureus 2022, 14, e25891. [Google Scholar] [CrossRef] [PubMed]
- Kanai, O.; Ito, T.; Saito, Z.; Yamamoto, Y.; Fujita, K.; Okamura, M.; Hashimoto, M.; Nakatani, K.; Sawai, S.; Mio, T. Effect of Cyclooxygenase Inhibitor Use on Immunotherapy Efficacy in Non-small Cell Lung Cancer. Thorac. Cancer 2021, 12, 949–957. [Google Scholar] [CrossRef] [PubMed]
- Cortellini, A.; Tucci, M.; Adamo, V.; Stucci, L.S.; Russo, A.; Tanda, E.T.; Spagnolo, F.; Rastelli, F.; Bisonni, R.; Santini, D.; et al. Integrated Analysis of Concomitant Medications and Oncological Outcomes from PD-1/PD-L1 Checkpoint Inhibitors in Clinical Practice. J. Immunother. Cancer 2020, 8, e001361. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Chen, H.; Chen, S.; Li, Z.; Chen, J.; Li, W. The Effect of Concomitant Use of Statins, NSAIDs, Low-Dose Aspirin, Metformin and Beta-Blockers on Outcomes in Patients Receiving Immune Checkpoint Inhibitors: A Systematic Review and Meta-Analysis. OncoImmunology 2021, 10, 1957605. [Google Scholar] [CrossRef]
- Mravec, B.; Horvathova, L.; Hunakova, L. Neurobiology of Cancer: The Role of β-Adrenergic Receptor Signaling in Various Tumor Environments. Int. J. Mol. Sci. 2020, 21, 7958. [Google Scholar] [CrossRef]
- Yan, X.; Liu, P.; Li, D.; Hu, R.; Tao, M.; Zhu, S.; Wu, W.; Yang, M.; Qu, X. Novel Evidence for the Prognostic Impact of β-Blockers in Solid Cancer Patients Receiving Immune Checkpoint Inhibitors. Int. Immunopharmacol. 2022, 113, 109383. [Google Scholar] [CrossRef]
- Fjæstad, K.Y.; Rømer, A.M.A.; Goitea, V.; Johansen, A.Z.; Thorseth, M.-L.; Carretta, M.; Engelholm, L.H.; Grøntved, L.; Junker, N.; Madsen, D.H. Blockade of Beta-Adrenergic Receptors Reduces Cancer Growth and Enhances the Response to Anti-CTLA4 Therapy by Modulating the Tumor Microenvironment. Oncogene 2022, 41, 1364–1375. [Google Scholar] [CrossRef] [PubMed]
- Kokolus, K.M.; Zhang, Y.; Sivik, J.M.; Schmeck, C.; Zhu, J.; Repasky, E.A.; Drabick, J.J.; Schell, T.D. Beta Blocker Use Correlates with Better Overall Survival in Metastatic Melanoma Patients and Improves the Efficacy of Immunotherapies in Mice. OncoImmunology 2018, 7, e1405205. [Google Scholar] [CrossRef] [PubMed]
- Mellgard, G.; Patel, V.G.; Zhong, X.; Joshi, H.; Qin, Q.; Wang, B.; Parikh, A.; Jun, T.; Alerasool, P.; Garcia, P.; et al. Effect of Concurrent Beta-Blocker Use in Patients Receiving Immune Checkpoint Inhibitors for Advanced Solid Tumors. J. Cancer Res. Clin. Oncol. 2022. [Google Scholar] [CrossRef] [PubMed]
- Oh, M.S.; Guzner, A.; Wainwright, D.A.; Mohindra, N.A.; Chae, Y.K.; Behdad, A.; Villaflor, V.M. The Impact of Beta Blockers on Survival Outcomes in Patients With Non–Small-Cell Lung Cancer Treated With Immune Checkpoint Inhibitors. Clin. Lung Cancer 2021, 22, e57–e62. [Google Scholar] [CrossRef]
- Gandhi, S.; Pandey, M.R.; Attwood, K.; Ji, W.; Witkiewicz, A.K.; Knudsen, E.S.; Allen, C.; Tario, J.D.; Wallace, P.K.; Cedeno, C.D.; et al. Phase I Clinical Trial of Combination Propranolol and Pembrolizumab in Locally Advanced and Metastatic Melanoma: Safety, Tolerability, and Preliminary Evidence of Antitumor Activity. Clin. Cancer Res. 2021, 27, 87–95. [Google Scholar] [CrossRef]
- Nakamura, K.; Yaguchi, T.; Ohmura, G.; Kobayashi, A.; Kawamura, N.; Iwata, T.; Kiniwa, Y.; Okuyama, R.; Kawakami, Y. Involvement of Local Renin-Angiotensin System in Immunosuppression of Tumor Microenvironment. Cancer Sci. 2018, 109, 54–64. [Google Scholar] [CrossRef] [PubMed]
- Xie, G.; Cheng, T.; Lin, J.; Zhang, L.; Zheng, J.; Liu, Y.; Xie, G.; Wang, B.; Yuan, Y. Local Angiotensin II Contributes to Tumor Resistance to Checkpoint Immunotherapy. J. Immunother. Cancer 2018, 6, 88. [Google Scholar] [CrossRef]
- Chauhan, V.P.; Chen, I.X.; Tong, R.; Ng, M.R.; Martin, J.D.; Naxerova, K.; Wu, M.W.; Huang, P.; Boucher, Y.; Kohane, D.S.; et al. Reprogramming the Microenvironment with Tumor-Selective Angiotensin Blockers Enhances Cancer Immunotherapy. Proc. Natl. Acad. Sci. USA 2019, 116, 10674–10680. [Google Scholar] [CrossRef] [PubMed]
- Chauhan, V.P.; Martin, J.D.; Liu, H.; Lacorre, D.A.; Jain, S.R.; Kozin, S.V.; Stylianopoulos, T.; Mousa, A.S.; Han, X.; Adstamongkonkul, P.; et al. Angiotensin Inhibition Enhances Drug Delivery and Potentiates Chemotherapy by Decompressing Tumour Blood Vessels. Nat. Commun. 2013, 4, 2516. [Google Scholar] [CrossRef] [PubMed]
- Nuzzo, P.V.; Adib, E.; Weise, N.; Curran, C.; Stewart, T.; Freeman, D.; Nassar, A.H.; Abou Alaiwi, S.; Bakouny, Z.; McGregor, B.A.; et al. Impact of Renin-Angiotensin System Inhibitors on Outcomes in Patients with Metastatic Renal Cell Carcinoma Treated with Immune-Checkpoint Inhibitors. Clin. Genitourin. Cancer 2022, 20, 301–306. [Google Scholar] [CrossRef] [PubMed]
- Drobni, Z.D.; Michielin, O.; Quinaglia, T.; Zlotoff, D.A.; Zubiri, L.; Gilman, H.K.; Supraja, S.; Merkely, B.; Muller, V.; Sullivan, R.J.; et al. Renin–Angiotensin–Aldosterone System Inhibitors and Survival in Patients with Hypertension Treated with Immune Checkpoint Inhibitors. Eur. J. Cancer 2022, 163, 108–118. [Google Scholar] [CrossRef] [PubMed]
- Medjebar, S.; Truntzer, C.; Perrichet, A.; Limagne, E.; Fumet, J.-D.; Richard, C.; Elkrief, A.; Routy, B.; Rébé, C.; Ghiringhelli, F. Angiotensin-Converting Enzyme (ACE) Inhibitor Prescription Affects Non-Small-Cell Lung Cancer (NSCLC) Patients Response to PD-1/PD-L1 Immune Checkpoint Blockers. OncoImmunology 2020, 9, 1836766. [Google Scholar] [CrossRef] [PubMed]
- Prasetya, R.A.; Metselaar-Albers, M.; Engels, F. Concomitant Use of Analgesics and Immune Checkpoint Inhibitors in Non-Small Cell Lung Cancer: A Pharmacodynamics Perspective. Eur. J. Pharmacol. 2021, 906, 174284. [Google Scholar] [CrossRef]
- Yu, X.; Zhao, L.; Song, B. Impact of Opioid Analgesics on the Efficacy of Immune Checkpoint Inhibitors in a Lung Cancer Population. BMC Pulm. Med. 2022, 22, 431. [Google Scholar] [CrossRef]
- Taniguchi, Y.; Tamiya, A.; Matsuda, Y.; Adachi, Y.; Enomoto, T.; Azuma, K.; Kouno, S.; Tokoro, A.; Atagi, S. Opioids Impair Nivolumab Outcomes: A Retrospective Propensity Score Analysis in Non-Small-Cell Lung Cancer. BMJ Support. Palliat. Care 2020. [Google Scholar] [CrossRef] [PubMed]
- Botticelli, A.; Cirillo, A.; Pomati, G.; Cerbelli, B.; Scagnoli, S.; Roberto, M.; Gelibter, A.; Mammone, G.; Calandrella, M.L.; Cerbelli, E.; et al. The Role of Opioids in Cancer Response to Immunotherapy. J. Transl. Med. 2021, 19, 119. [Google Scholar] [CrossRef]
- Mao, Z.; Jia, X.; Jiang, P.; Wang, Q.; Zhang, Y.; Li, Y.; Fu, X.; Jiao, M.; Jiang, L.; Liu, Z.; et al. Effect of Concomitant Use of Analgesics on Prognosis in Patients Treated With Immune Checkpoint Inhibitors: A Systematic Review and Meta-Analysis. Front. Immunol. 2022, 13, 861723. [Google Scholar] [CrossRef] [PubMed]
- Shwe, T.H.; Pothacharoen, P.; Phitak, T.; Wudtiwai, B.; Kongtawelert, P. Atorvastatin Attenuates Programmed Death Ligand-1 (PD-L1) Induction in Human Hepatocellular Carcinoma Cells. Int. J. Mol. Sci. 2021, 22, 8755. [Google Scholar] [CrossRef] [PubMed]
- Choe, E.-J.; Lee, C.-H.; Bae, J.-H.; Park, J.-M.; Park, S.-S.; Baek, M.-C. Atorvastatin Enhances the Efficacy of Immune Checkpoint Therapy and Suppresses the Cellular and Extracellular Vesicle PD-L1. Pharmaceutics 2022, 14, 1660. [Google Scholar] [CrossRef]
- Lim, W.-J.; Lee, M.; Oh, Y.; Fang, X.-Q.; Lee, S.; Lim, C.-H.; Park, J.; Lim, J.-H. Statins Decrease Programmed Death-Ligand 1 (PD-L1) by Inhibiting AKT and β-Catenin Signaling. Cells 2021, 10, 2488. [Google Scholar] [CrossRef] [PubMed]
- Cantini, L.; Pecci, F.; Hurkmans, D.P.; Belderbos, R.A.; Lanese, A.; Copparoni, C.; Aerts, S.; Cornelissen, R.; Dumoulin, D.W.; Fiordoliva, I.; et al. High-Intensity Statins Are Associated with Improved Clinical Activity of PD-1 Inhibitors in Malignant Pleural Mesothelioma and Advanced Non-Small Cell Lung Cancer Patients. Eur. J. Cancer 2021, 144, 41–48. [Google Scholar] [CrossRef]
- Rossi, A.; Filetti, M.; Taurelli Salimbeni, B.; Piras, M.; Rizzo, F.; Giusti, R.; Marchetti, P. Statins and Immunotherapy: Togetherness Makes Strength The Potential Effect of Statins on Immunotherapy for NSCLC. Cancer Rep. 2021, 4, e1368. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Wang, H.; Tian, J.; Sui, L.; Chen, X. Concomitant Statins and the Survival of Patients with Non-Small-Cell Lung Cancer Treated with Immune Checkpoint Inhibitors: A Meta-Analysis. Int. J. Clin. Pract. 2022, 2022, 1–10. [Google Scholar] [CrossRef]
- Hanahan, D. Hallmarks of Cancer: New Dimensions. Cancer Discov. 2022, 12, 31–46. [Google Scholar] [CrossRef]
- Buti, S.; Bersanelli, M.; Perrone, F.; Tiseo, M.; Tucci, M.; Adamo, V.; Stucci, L.S.; Russo, A.; Tanda, E.T.; Spagnolo, F.; et al. Effect of Concomitant Medications with Immune-Modulatory Properties on the Outcomes of Patients with Advanced Cancer Treated with Immune Checkpoint Inhibitors: Development and Validation of a Novel Prognostic Index. Eur. J. Cancer 2021, 142, 18–28. [Google Scholar] [CrossRef] [PubMed]
- Dussart, C.; Decaux-Tramoni, B.; Quesada, S.; Thomas, Q.D.; Benzerouale, O.; Nicolas, E.; Fiteni, F. Combinaisons d’inhibiteurs de points de contrôle immunitaires en oncologie: état de l’art et perspectivesCombination strategies for checkpoint inhibition: Current practices and perspectives. Bull. Cancer, 2023; in press. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).