Novel Mechanisms and Future Opportunities for the Management of Radiation Necrosis in Patients Treated for Brain Metastases in the Era of Immunotherapy
Abstract
:Simple Summary
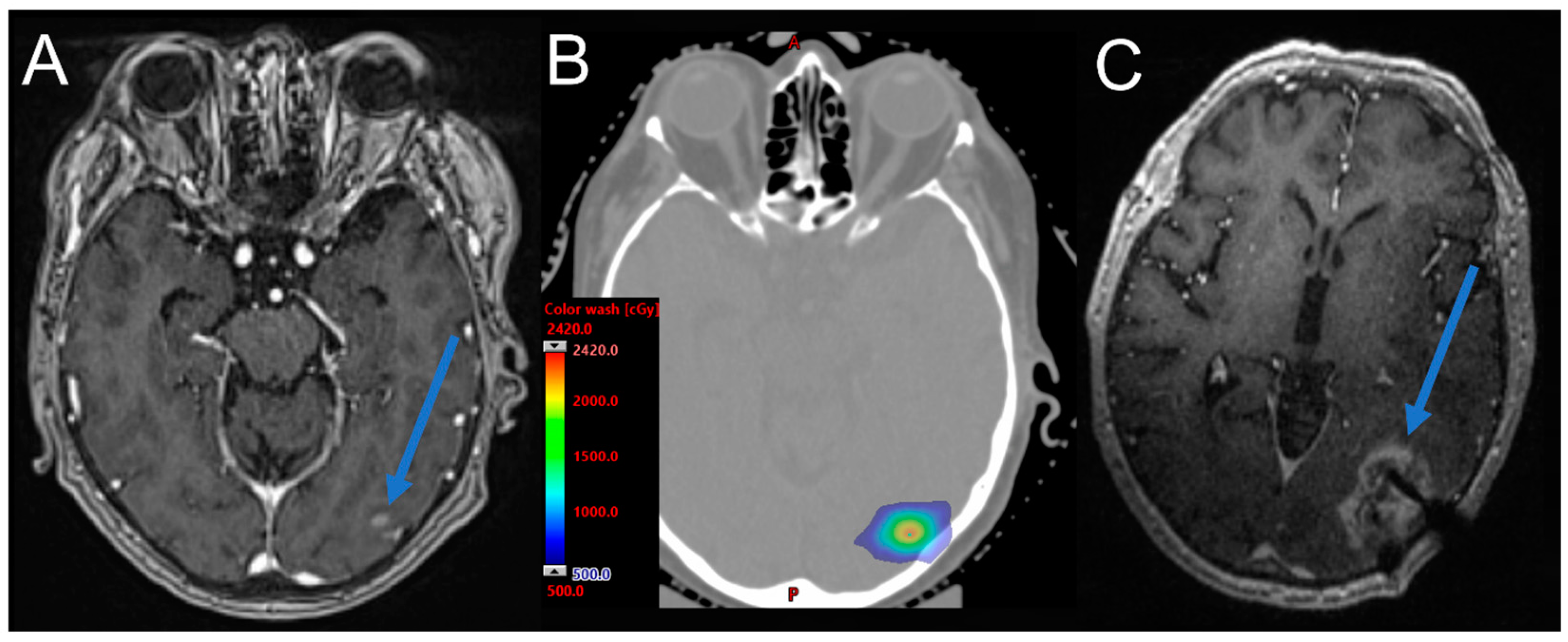
Abstract
1. Introduction
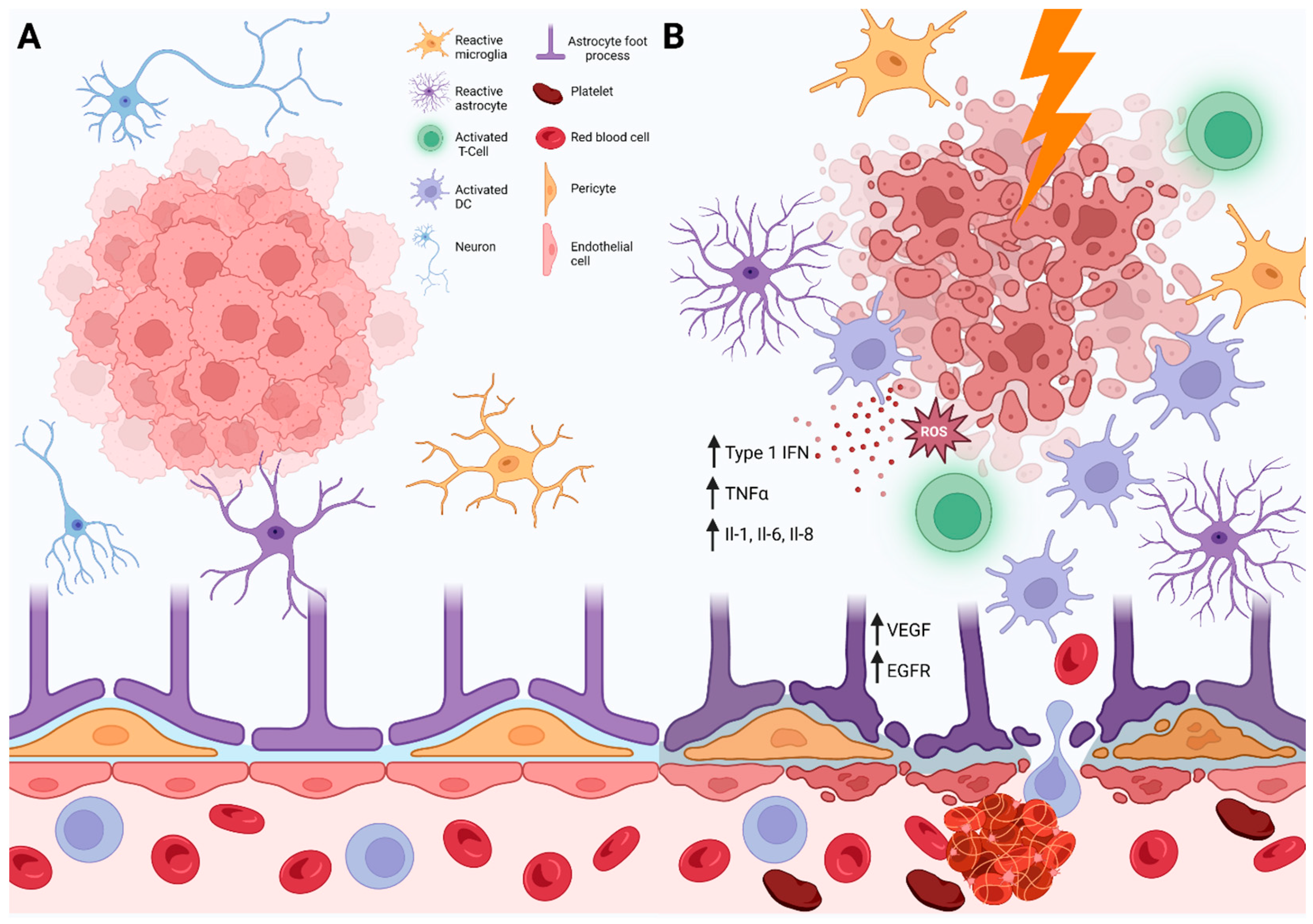
2. Pathophysiology
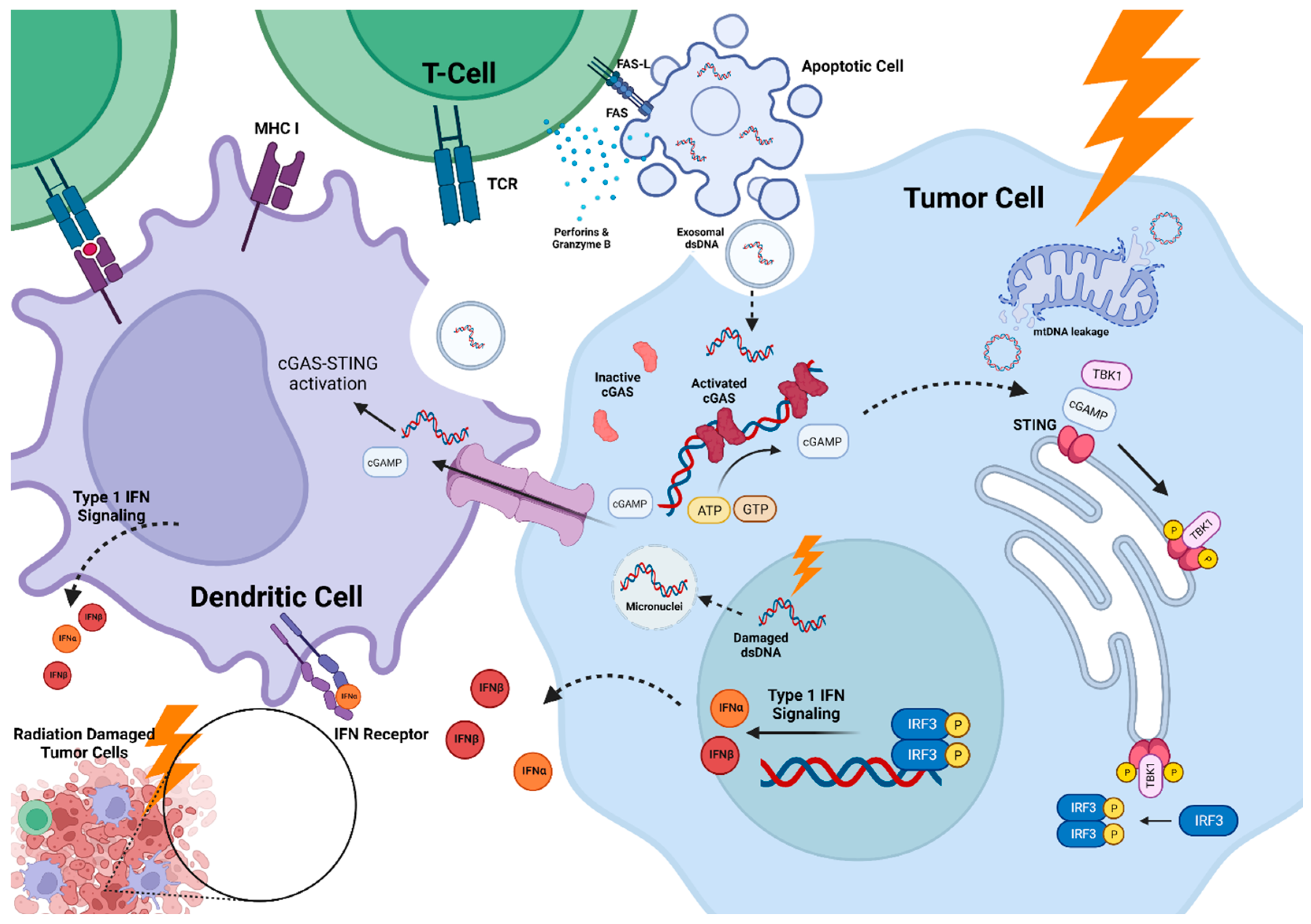
2.1. cGAS-STING Pathway
2.2. Temporal Patterns
3. Diagnostic Evaluation
4. Clinical Significance
5. Risk Factors for Necrosis
5.1. Radiation Therapy Alone
5.2. Reirradiation
5.3. Immunotherapy
5.4. Targeted Therapy
5.5. Chemotherapy
5.6. Proton Therapy
6. Management Options
7. Future Directions
7.1. Dosimetric Strategies
7.2. Novel Imaging Techniques
7.3. Artificial Intelligence
7.4. Circulating Biomarkers
8. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Radiation Alone Studies | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Author | Study Type | Sample Size * | Histology | Radiation | Systemic Therapy | Follow Up (Months) | Overall Necrosis Rate * | Biopsy Rate * | Symptomatic Necrosis Rate * | Necrosis Predictors |
| Miller (2016) | Retrospective | 1939 | NSCLC 43% Melanoma 10% Breast 15% | SRS | Not reported | 12 | 427 (7%) lesions | 30 (7%) lesions | 231 (54%) lesions | GPA score Laterality RCC (HR: 1.78) Tumor diameter (HR:1.29) H-Index (HR: 1.9) |
| Minniti (2016) | Retrospective | 289 | NSCLC 41% Melanoma 14% Breast 17% | SRS/fSRS | None | 29 | SRS: 31 (20%) fSRS: 11 (8%) | 17 (40.5%) | SRS: 13 (42%) fSRS: 4 (36%) | GTV V12 Gy (SRS) V18 Gy (fSRS) |
| Surgery and Radiation Studies | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Author | Study Type | Sample Size * | Histology | Radiation | Resection Rate | Follow Up (Months) | Overall Necrosis Rate * | Biopsy Rate * | Symptomatic Necrosis Rate * | Necrosis Predictors |
| Wernicke (2014) | Prospective | 24 | Lung 67% Melanoma 8% Breast 8% | Cs131 | 100% | 19.3 | 0% | None | None | None |
| Ebner (2015) | Retrospective | 93 (lesions > 3 cm) | NSCLC 48% Melanoma 14% Breast 17% | SRS | 68% | 22 | 10 (11%) | 2 (20%) | 3 (30%) | Not reported |
| Patel (2016) | Retrospective | 180 | NSCLC 40% Melanoma 19% Breast 17% | Pre- vs. Post-op SRS/fSRS | 100% | 11.1 vs. 24.6 | 42 (23%) | 4 (10%) | 24 (57%) | Post-op SRS |
| Prabhu (2017) | Retrospective | 213 | Lung 41% Melanoma 15% Breast 23 | SRS | 72% | 13 | Intact: 7 (12%) Cavities: 24 (16%) | None | Intact: 6 (86%) Cavities: 17 (71%) | Post-op SRS |
| Martinage (2019) | Retrospective | 160 | NSCLC 46% Melanoma 15% Breast 13% | fSRS | 100% | 30.6 | 13 (9%) | None | 2 (15%) | Re-RT |
| Eitz (2020) | Retrospective | 558 | NSCLC 34% Melanoma 15% Breast 17% | fSRS | 100% | 12.3 | 48 (9%) | 9 (19%) | 3 (6%) | Not reported |
| Reirradiation Studies | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Author | Study Type | Sample Size * | Histology | Radiation | Time between Radiation Courses | Systemic Therapy | Follow Up (Months) | Overall Necrosis Rate * | Biopsy Rate * | Symptomatic Necrosis Rate * | Necrosis Predictors |
| Shaw RTOG 9005 (2000) | Prospective | 156 | 36% Primary, 64% Metastases (NSCLC 33% Breast 66%) | SRS | Median: 17 months | None | 36 | 16 (10%) | 16 (100%) | 16 (100%) | Dose Tumor diameter KPS |
| Kowalchuk (2021) | Retrospective | 102 | NSCLC 100% | SRS | Median: 12 months | Not reported | 14 | 25 (20%) | 1 (4%) | 9 (36%) | Dose ≥40 Gy V12 Gy > 9 cm3 |
| Wilcox (2021) | Retrospective | 135 | NSCLC 37% Melanoma 26% Breast 21% | Observation vs. Re-RT (5% SRS, 41% fSRS) | Median: 9.8 months 1 | Not reported | Not reported | 4 (4%) vs. 4 (13%) | Not reported | 1 (25%) vs. 2 (50%) | Re-RT (HR: 3.84) |
| Imber (2022) | Prospective | 24 | Lung 25% Breast 20% | Cs131 | Median: 11.9 months | Not reported | 19.2 | 8 (32%) | None | 4 (50%) | Not reported |
| Sneed (2022) | Retrospective | 124 | Lung 24% Melanoma 21% Breast 43% | Re-SRS | Median: 15.4 months | ICI or TT | 14.5 | 88 (38%) lesions | 6 (7%) lesions | 24 (27%) lesions | Tumor volume Prior WBRT Repeat SRS |
References
- Suh, J.H.; Kotecha, R.; Chao, S.T.; Ahluwalia, M.S.; Sahgal, A.; Chang, E.L. Current Approaches to the Management of Brain Metastases. Nat. Rev. Clin. Oncol. 2020, 17, 279–299. [Google Scholar] [CrossRef] [PubMed]
- Langer, C.J.; Mehta, M.P. Current Management of Brain Metastases, with a Focus on Systemic Options. J. Clin. Oncol. 2005, 23, 6207–6219. [Google Scholar] [CrossRef]
- Borius, P.-Y.; Régis, J.; Carpentier, A.; Kalamarides, M.; Valery, C.A.; Latorzeff, I. Safety of Radiosurgery Concurrent with Systemic Therapy (Chemotherapy, Targeted Therapy, and/or Immunotherapy) in Brain Metastases: A Systematic Review. Cancer Metastasis Rev. 2021, 40, 341–354. [Google Scholar] [CrossRef] [PubMed]
- Moravan, M.J.; Fecci, P.E.; Anders, C.K.; Clarke, J.M.; Salama, A.K.S.; Adamson, J.D.; Floyd, S.R.; Torok, J.A.; Salama, J.K.; Sampson, J.H.; et al. Current Multidisciplinary Management of Brain Metastases. Cancer 2020, 126, 1390–1406. [Google Scholar] [CrossRef]
- Kim, G.J.; Buckley, E.D.; Herndon, J.E.; Allen, K.J.; Dale, T.S.; Adamson, J.D.; Lay, L.; Giles, W.M.; Rodrigues, A.E.; Wang, Z.; et al. Outcomes in Patients with 4 to 10 Brain Metastases Treated with Dose-Adapted Single-Isocenter Multitarget Stereotactic Radiosurgery: A Prospective Study. Adv. Radiat. Oncol. 2021, 6, 100760. [Google Scholar] [CrossRef]
- Shaw, E.; Scott, C.; Souhami, L.; Dinapoli, R.; Kline, R.; Loeffler, J.; Farnan, N. Single Dose Radiosurgical Treatment of Recurrent Previously Irradiated Primary Brain Tumors and Brain Metastases: Final Report of RTOG Protocol 90-05. Int. J. Radiat. Oncol. 2000, 47, 291–298. [Google Scholar] [CrossRef]
- Tonse, R.; Tom, M.C.; Mehta, M.P.; Ahluwalia, M.S.; Kotecha, R. Integration of Systemic Therapy and Stereotactic Radiosurgery for Brain Metastases. Cancers 2021, 13, 3682. [Google Scholar] [CrossRef] [PubMed]
- Milano, M.T.; Grimm, J.; Niemierko, A.; Soltys, S.G.; Moiseenko, V.; Redmond, K.J.; Yorke, E.; Sahgal, A.; Xue, J.; Mahadevan, A.; et al. Single- and Multifraction Stereotactic Radiosurgery Dose/Volume Tolerances of the Brain. Int. J. Radiat. Oncol. 2021, 110, 68–86. [Google Scholar] [CrossRef]
- Li, J.; Ludmir, E.B.; Wang, Y.; Guha-Thakurta, N.; McAleer, M.F.; Settle, S.H.; Yeboa, D.N.; Ghia, A.J.; McGovern, S.L.; Chung, C.; et al. Stereotactic Radiosurgery versus Whole-Brain Radiation Therapy for Patients with 4-15 Brain Metastases: A Phase III Randomized Controlled Trial. Int. J. Radiat. Oncol. 2020, 108, S21–S22. [Google Scholar] [CrossRef]
- Yamamoto, M.; Serizawa, T.; Shuto, T.; Akabane, A.; Higuchi, Y.; Kawagishi, J.; Yamanaka, K.; Sato, Y.; Jokura, H.; Yomo, S.; et al. Stereotactic Radiosurgery for Patients with Multiple Brain Metastases (JLGK0901): A Multi-Institutional Prospective Observational Study. Lancet Oncol. 2014, 15, 387–395. [Google Scholar] [CrossRef]
- Kocher, M.; Soffietti, R.; Abacioglu, U.; Villà, S.; Fauchon, F.; Baumert, B.G.; Fariselli, L.; Tzuk-Shina, T.; Kortmann, R.-D.; Carrie, C.; et al. Adjuvant Whole-Brain Radiotherapy versus Observation after Radiosurgery or Surgical Resection of One to Three Cerebral Metastases: Results of the EORTC 22952-26001 Study. J. Clin. Oncol. 2011, 29, 134–141. [Google Scholar] [CrossRef] [PubMed]
- Chang, E.L.; Wefel, J.S.; Hess, K.R.; Allen, P.K.; Lang, F.F.; Kornguth, D.G.; Arbuckle, R.B.; Swint, J.M.; Shiu, A.S.; Maor, M.H.; et al. Neurocognition in Patients with Brain Metastases Treated with Radiosurgery or Radiosurgery plus Whole-Brain Irradiation: A Randomised Controlled Trial. Lancet Oncol. 2009, 10, 1037–1044. [Google Scholar] [CrossRef] [PubMed]
- Aoyama, H.; Shirato, H.; Tago, M.; Nakagawa, K.; Toyoda, T.; Hatano, K.; Kenjyo, M.; Oya, N.; Hirota, S.; Shioura, H.; et al. Stereotactic Radiosurgery Plus Whole-Brain Radiation Therapy vs. Stereotactic Radiosurgery Alone for Treatment of Brain Metastases. JAMA 2006, 295, 2483. [Google Scholar] [CrossRef]
- Kirkpatrick, J.P.; Laack, N.N.; Halasz, L.M.; Minniti, G.; Chan, M.D. Proton Therapy for Brain Metastases: A Question of Value. Int. J. Radiat. Oncol. 2018, 101, 830–832. [Google Scholar] [CrossRef] [PubMed]
- Winter, S.F.; Loebel, F.; Loeffler, J.; Batchelor, T.T.; Martinez-Lage, M.; Vajkoczy, P.; Dietrich, J. Treatment-Induced Brain Tissue Necrosis: A Clinical Challenge in Neuro-Oncology. Neuro Oncol. 2019, 21, 1118–1130. [Google Scholar] [CrossRef]
- Philchenkov, A. Radiation-Induced Cell Death: Signaling and Pharmacological Modulation. Crit. Rev. Oncog. 2018, 23, 13–37. [Google Scholar] [CrossRef]
- Mackenzie, K.J.; Carroll, P.; Martin, C.-A.; Murina, O.; Fluteau, A.; Simpson, D.J.; Olova, N.; Sutcliffe, H.; Rainger, J.K.; Leitch, A.; et al. CGAS Surveillance of Micronuclei Links Genome Instability to Innate Immunity. Nature 2017, 548, 461–465. [Google Scholar] [CrossRef]
- Harding, S.M.; Benci, J.L.; Irianto, J.; Discher, D.E.; Minn, A.J.; Greenberg, R.A. Mitotic Progression Following DNA Damage Enables Pattern Recognition within Micronuclei. Nature 2017, 548, 466–470. [Google Scholar] [CrossRef]
- Carozza, J.A.; Böhnert, V.; Nguyen, K.C.; Skariah, G.; Shaw, K.E.; Brown, J.A.; Rafat, M.; von Eyben, R.; Graves, E.E.; Glenn, J.S.; et al. Extracellular CGAMP Is a Cancer-Cell-Produced Immunotransmitter Involved in Radiation-Induced Anticancer Immunity. Nat. Cancer 2020, 1, 184–196. [Google Scholar] [CrossRef]
- Glück, S.; Guey, B.; Gulen, M.F.; Wolter, K.; Kang, T.-W.; Schmacke, N.A.; Bridgeman, A.; Rehwinkel, J.; Zender, L.; Ablasser, A. Innate Immune Sensing of Cytosolic Chromatin Fragments through CGAS Promotes Senescence. Nat. Cell Biol. 2017, 19, 1061–1070. [Google Scholar] [CrossRef]
- Han, C.; Liu, Z.; Zhang, Y.; Shen, A.; Dong, C.; Zhang, A.; Moore, C.; Ren, Z.; Lu, C.; Cao, X.; et al. Tumor Cells Suppress Radiation-Induced Immunity by Hijacking Caspase 9 Signaling. Nat. Immunol. 2020, 21, 546–554. [Google Scholar] [CrossRef]
- Fang, C.; Mo, F.; Liu, L.; Du, J.; Luo, M.; Men, K.; Na, F.; Wang, W.; Yang, H.; Wei, X. Oxidized Mitochondrial DNA Sensing by STING Signaling Promotes the Antitumor Effect of an Irradiated Immunogenic Cancer Cell Vaccine. Cell. Mol. Immunol. 2021, 18, 2211–2223. [Google Scholar] [CrossRef] [PubMed]
- Dou, Z.; Ghosh, K.; Vizioli, M.G.; Zhu, J.; Sen, P.; Wangensteen, K.J.; Simithy, J.; Lan, Y.; Lin, Y.; Zhou, Z.; et al. Cytoplasmic Chromatin Triggers Inflammation in Senescence and Cancer. Nature 2017, 550, 402–406. [Google Scholar] [CrossRef] [PubMed]
- Vanpouille-Box, C.; Alard, A.; Aryankalayil, M.J.; Sarfraz, Y.; Diamond, J.M.; Schneider, R.J.; Inghirami, G.; Coleman, C.N.; Formenti, S.C.; Demaria, S. DNA Exonuclease Trex1 Regulates Radiotherapy-Induced Tumour Immunogenicity. Nat. Commun. 2017, 8, 15618. [Google Scholar] [CrossRef] [PubMed]
- Deng, L.; Liang, H.; Xu, M.; Yang, X.; Burnette, B.; Arina, A.; Li, X.-D.; Mauceri, H.; Beckett, M.; Darga, T.; et al. STING-Dependent Cytosolic DNA Sensing Promotes Radiation-Induced Type I Interferon-Dependent Antitumor Immunity in Immunogenic Tumors. Immunity 2014, 41, 843–852. [Google Scholar] [CrossRef] [PubMed]
- Schadt, L.; Sparano, C.; Schweiger, N.A.; Silina, K.; Cecconi, V.; Lucchiari, G.; Yagita, H.; Guggisberg, E.; Saba, S.; Nascakova, Z.; et al. Cancer-Cell-Intrinsic CGAS Expression Mediates Tumor Immunogenicity. Cell Rep. 2019, 29, 1236–1248.e7. [Google Scholar] [CrossRef]
- Härtlova, A.; Erttmann, S.F.; Raffi, F.A.; Schmalz, A.M.; Resch, U.; Anugula, S.; Lienenklaus, S.; Nilsson, L.M.; Kröger, A.; Nilsson, J.A.; et al. DNA Damage Primes the Type I Interferon System via the Cytosolic DNA Sensor STING to Promote Anti-Microbial Innate Immunity. Immunity 2015, 42, 332–343. [Google Scholar] [CrossRef]
- Ishikawa, H.; Barber, G.N. STING Is an Endoplasmic Reticulum Adaptor That Facilitates Innate Immune Signalling. Nature 2008, 455, 674–678. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, H.; Ma, Z.; Barber, G.N. STING Regulates Intracellular DNA-Mediated, Type I Interferon-Dependent Innate Immunity. Nature 2009, 461, 788–792. [Google Scholar] [CrossRef]
- Sun, W.; Li, Y.; Chen, L.; Chen, H.; You, F.; Zhou, X.; Zhou, Y.; Zhai, Z.; Chen, D.; Jiang, Z. ERIS, an Endoplasmic Reticulum IFN Stimulator, Activates Innate Immune Signaling through Dimerization. Proc. Natl. Acad. Sci. USA 2009, 106, 8653–8658. [Google Scholar] [CrossRef]
- Burdette, D.L.; Monroe, K.M.; Sotelo-Troha, K.; Iwig, J.S.; Eckert, B.; Hyodo, M.; Hayakawa, Y.; Vance, R.E. STING Is a Direct Innate Immune Sensor of Cyclic Di-GMP. Nature 2011, 478, 515–518. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Wu, J.; Du, F.; Chen, X.; Chen, Z.J. Cyclic GMP-AMP Synthase Is a Cytosolic DNA Sensor That Activates the Type I Interferon Pathway. Science 2013, 339, 786–791. [Google Scholar] [CrossRef] [PubMed]
- Woo, S.-R.; Fuertes, M.B.; Corrales, L.; Spranger, S.; Furdyna, M.J.; Leung, M.Y.K.; Duggan, R.; Wang, Y.; Barber, G.N.; Fitzgerald, K.A.; et al. STING-Dependent Cytosolic DNA Sensing Mediates Innate Immune Recognition of Immunogenic Tumors. Immunity 2014, 41, 830–842. [Google Scholar] [CrossRef] [PubMed]
- Merad, M.; Sathe, P.; Helft, J.; Miller, J.; Mortha, A. The Dendritic Cell Lineage: Ontogeny and Function of Dendritic Cells and Their Subsets in the Steady State and the Inflamed Setting. Annu. Rev. Immunol. 2013, 31, 563–604. [Google Scholar] [CrossRef]
- Vatner, R.E.; Janssen, E.M. STING, DCs and the Link between Innate and Adaptive Tumor Immunity. Mol. Immunol. 2019, 110, 13–23. [Google Scholar] [CrossRef] [PubMed]
- Hildner, K.; Edelson, B.T.; Purtha, W.E.; Diamond, M.; Matsushita, H.; Kohyama, M.; Calderon, B.; Schraml, B.U.; Unanue, E.R.; Diamond, M.S.; et al. Batf3 Deficiency Reveals a Critical Role for CD8α + Dendritic Cells in Cytotoxic T Cell Immunity. Science 2008, 322, 1097–1100. [Google Scholar] [CrossRef]
- Neefjes, J.; Jongsma, M.L.M.; Paul, P.; Bakke, O. Towards a Systems Understanding of MHC Class I and MHC Class II Antigen Presentation. Nat. Rev. Immunol. 2011, 11, 823–836. [Google Scholar] [CrossRef]
- Andersen, M.H.; Schrama, D.; thor Straten, P.; Becker, J.C. Cytotoxic T Cells. J. Investig. Dermatol. 2006, 126, 32–41. [Google Scholar] [CrossRef]
- Platanias, L.C. Mechanisms of Type-I- and Type-II-Interferon-Mediated Signalling. Nat. Rev. Immunol. 2005, 5, 375–386. [Google Scholar] [CrossRef]
- Zitvogel, L.; Galluzzi, L.; Kepp, O.; Smyth, M.J.; Kroemer, G. Type I Interferons in Anticancer Immunity. Nat. Rev. Immunol. 2015, 15, 405–414. [Google Scholar] [CrossRef]
- Le Bon, A.; Tough, D.F. Links between Innate and Adaptive Immunity via Type I Interferon. Curr. Opin. Immunol. 2002, 14, 432–436. [Google Scholar] [CrossRef] [PubMed]
- Medrano, R.F.V.; Hunger, A.; Mendonça, S.A.; Barbuto, J.A.M.; Strauss, B.E. Immunomodulatory and Antitumor Effects of Type I Interferons and Their Application in Cancer Therapy. Oncotarget 2017, 8, 71249–71284. [Google Scholar] [CrossRef] [PubMed]
- Diamond, M.S.; Kinder, M.; Matsushita, H.; Mashayekhi, M.; Dunn, G.P.; Archambault, J.M.; Lee, H.; Arthur, C.D.; White, J.M.; Kalinke, U.; et al. Type I Interferon Is Selectively Required by Dendritic Cells for Immune Rejection of Tumors. J. Exp. Med. 2011, 208, 1989–2003. [Google Scholar] [CrossRef] [PubMed]
- Fuertes, M.B.; Kacha, A.K.; Kline, J.; Woo, S.-R.; Kranz, D.M.; Murphy, K.M.; Gajewski, T.F. Host Type I IFN Signals Are Required for Antitumor CD8+ T Cell Responses through CD8α+ Dendritic Cells. J. Exp. Med. 2011, 208, 2005–2016. [Google Scholar] [CrossRef] [PubMed]
- Kam, W.W.-Y.; Banati, R.B. Effects of Ionizing Radiation on Mitochondria. Free Radic. Biol. Med. 2013, 65, 607–619. [Google Scholar] [CrossRef]
- White, M.J.; McArthur, K.; Metcalf, D.; Lane, R.M.; Cambier, J.C.; Herold, M.J.; van Delft, M.F.; Bedoui, S.; Lessene, G.; Ritchie, M.E.; et al. Apoptotic Caspases Suppress MtDNA-Induced STING-Mediated Type I IFN Production. Cell 2014, 159, 1549–1562. [Google Scholar] [CrossRef]
- Rongvaux, A.; Jackson, R.; Harman, C.C.D.; Li, T.; West, A.P.; de Zoete, M.R.; Wu, Y.; Yordy, B.; Lakhani, S.A.; Kuan, C.-Y.; et al. Apoptotic Caspases Prevent the Induction of Type I Interferons by Mitochondrial DNA. Cell 2014, 159, 1563–1577. [Google Scholar] [CrossRef]
- Xu, M.M.; Pu, Y.; Han, D.; Shi, Y.; Cao, X.; Liang, H.; Chen, X.; Li, X.-D.; Deng, L.; Chen, Z.J.; et al. Dendritic Cells but Not Macrophages Sense Tumor Mitochondrial DNA for Cross-Priming through Signal Regulatory Protein α Signaling. Immunity 2017, 47, 363–373.e5. [Google Scholar] [CrossRef]
- Deng, L.; Liang, H.; Burnette, B.; Beckett, M.; Darga, T.; Weichselbaum, R.R.; Fu, Y.-X. Irradiation and Anti-PD-L1 Treatment Synergistically Promote Antitumor Immunity in Mice. J. Clin. Investig. 2014, 124, 687–695. [Google Scholar] [CrossRef]
- West, A.P.; Khoury-Hanold, W.; Staron, M.; Tal, M.C.; Pineda, C.M.; Lang, S.M.; Bestwick, M.; Duguay, B.A.; Raimundo, N.; MacDuff, D.A.; et al. Mitochondrial DNA Stress Primes the Antiviral Innate Immune Response. Nature 2015, 520, 553–557. [Google Scholar] [CrossRef]
- Storozynsky, Q.; Hitt, M.M. The Impact of Radiation-Induced DNA Damage on CGAS-STING-Mediated Immune Responses to Cancer. Int. J. Mol. Sci. 2020, 21, 8877. [Google Scholar] [CrossRef]
- Gao, P.; Ascano, M.; Wu, Y.; Barchet, W.; Gaffney, B.L.; Zillinger, T.; Serganov, A.A.; Liu, Y.; Jones, R.A.; Hartmann, G.; et al. Cyclic [G(2′,5′)PA(3′,5′)p] Is the Metazoan Second Messenger Produced by DNA-Activated Cyclic GMP-AMP Synthase. Cell 2013, 153, 1094–1107. [Google Scholar] [CrossRef] [PubMed]
- Gentili, M.; Kowal, J.; Tkach, M.; Satoh, T.; Lahaye, X.; Conrad, C.; Boyron, M.; Lombard, B.; Durand, S.; Kroemer, G.; et al. Transmission of Innate Immune Signaling by Packaging of CGAMP in Viral Particles. Science 2015, 349, 1232–1236. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Shang, G.; Gui, X.; Zhang, X.; Bai, X.; Chen, Z.J. Structural Basis of STING Binding with and Phosphorylation by TBK1. Nature 2019, 567, 394–398. [Google Scholar] [CrossRef]
- Wang, Q.; Liu, X.; Cui, Y.; Tang, Y.; Chen, W.; Li, S.; Yu, H.; Pan, Y.; Wang, C. The E3 Ubiquitin Ligase AMFR and INSIG1 Bridge the Activation of TBK1 Kinase by Modifying the Adaptor STING. Immunity 2014, 41, 919–933. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, Y.; Chen, Z.J. STING Specifies IRF3 Phosphorylation by TBK1 in the Cytosolic DNA Signaling Pathway. Sci. Signal. 2012, 5, ra20. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Cai, X.; Wu, J.; Cong, Q.; Chen, X.; Li, T.; Du, F.; Ren, J.; Wu, Y.-T.; Grishin, N.V.; et al. Phosphorylation of Innate Immune Adaptor Proteins MAVS, STING, and TRIF Induces IRF3 Activation. Science 2015, 347, aaa2630. [Google Scholar] [CrossRef]
- Corrales, L.; Glickman, L.H.; McWhirter, S.M.; Kanne, D.B.; Sivick, K.E.; Katibah, G.E.; Woo, S.-R.; Lemmens, E.; Banda, T.; Leong, J.J.; et al. Direct Activation of STING in the Tumor Microenvironment Leads to Potent and Systemic Tumor Regression and Immunity. Cell Rep. 2015, 11, 1018–1030. [Google Scholar] [CrossRef]
- Honda, K.; Takaoka, A.; Taniguchi, T. Type I Inteferon Gene Induction by the Interferon Regulatory Factor Family of Transcription Factors. Immunity 2006, 25, 349–360. [Google Scholar] [CrossRef]
- Burnette, B.C.; Liang, H.; Lee, Y.; Chlewicki, L.; Khodarev, N.N.; Weichselbaum, R.R.; Fu, Y.-X.; Auh, S.L. The Efficacy of Radiotherapy Relies upon Induction of Type I Interferon–Dependent Innate and Adaptive Immunity. Cancer Res. 2011, 71, 2488–2496. [Google Scholar] [CrossRef]
- Gupta, A.; Probst, H.C.; Vuong, V.; Landshammer, A.; Muth, S.; Yagita, H.; Schwendener, R.; Pruschy, M.; Knuth, A.; van den Broek, M. Radiotherapy Promotes Tumor-Specific Effector CD8+ T Cells via Dendritic Cell Activation. J. Immunol. 2012, 189, 558–566. [Google Scholar] [CrossRef]
- Lim, J.Y.H.; Gerber, S.A.; Murphy, S.P.; Lord, E.M. Type I Interferons Induced by Radiation Therapy Mediate Recruitment and Effector Function of CD8+ T Cells. Cancer Immunol. Immunother. 2014, 63, 259–271. [Google Scholar] [CrossRef]
- Konno, H.; Konno, K.; Barber, G.N. Cyclic Dinucleotides Trigger ULK1 (ATG1) Phosphorylation of STING to Prevent Sustained Innate Immune Signaling. Cell 2013, 155, 688–698. [Google Scholar] [CrossRef]
- Zhong, B.; Zhang, L.; Lei, C.; Li, Y.; Mao, A.-P.; Yang, Y.; Wang, Y.-Y.; Zhang, X.-L.; Shu, H.-B. The Ubiquitin Ligase RNF5 Regulates Antiviral Responses by Mediating Degradation of the Adaptor Protein MITA. Immunity 2009, 30, 397–407. [Google Scholar] [CrossRef] [PubMed]
- Gonugunta, V.K.; Sakai, T.; Pokatayev, V.; Yang, K.; Wu, J.; Dobbs, N.; Yan, N. Trafficking-Mediated STING Degradation Requires Sorting to Acidified Endolysosomes and Can Be Targeted to Enhance Anti-Tumor Response. Cell Rep. 2017, 21, 3234–3242. [Google Scholar] [CrossRef] [PubMed]
- Gao, D.; Li, T.; Li, X.-D.; Chen, X.; Li, Q.-Z.; Wight-Carter, M.; Chen, Z.J. Activation of Cyclic GMP-AMP Synthase by Self-DNA Causes Autoimmune Diseases. Proc. Natl. Acad. Sci. USA 2015, 112, E5699–E5705. [Google Scholar] [CrossRef] [PubMed]
- Motwani, M.; Pesiridis, S.; Fitzgerald, K.A. DNA Sensing by the CGAS–STING Pathway in Health and Disease. Nat. Rev. Genet. 2019, 20, 657–674. [Google Scholar] [CrossRef] [PubMed]
- Pouget, J.-P.; Georgakilas, A.G.; Ravanat, J.-L. Targeted and Off-Target (Bystander and Abscopal) Effects of Radiation Therapy: Redox Mechanisms and Risk/Benefit Analysis. Antioxid. Redox Signal. 2018, 29, 1447–1487. [Google Scholar] [CrossRef]
- Perry, A.; Schmidt, R.E. Cancer Therapy-Associated CNS Neuropathology: An Update and Review of the Literature. Acta Neuropathol. 2006, 111, 197–212. [Google Scholar] [CrossRef]
- Konno, H.; Yamauchi, S.; Berglund, A.; Putney, R.M.; Mulé, J.J.; Barber, G.N. Suppression of STING Signaling through Epigenetic Silencing and Missense Mutation Impedes DNA Damage Mediated Cytokine Production. Oncogene 2018, 37, 2037–2051. [Google Scholar] [CrossRef]
- Berger, G.; Knelson, E.H.; Jimenez-Macias, J.L.; Nowicki, M.O.; Han, S.; Panagioti, E.; Lizotte, P.H.; Adu-Berchie, K.; Stafford, A.; Dimitrakakis, N.; et al. STING Activation Promotes Robust Immune Response and NK Cell–Mediated Tumor Regression in Glioblastoma Models. Proc. Natl. Acad. Sci. USA 2022, 119, e2111003119. [Google Scholar] [CrossRef] [PubMed]
- Boudreau, C.E.; Najem, H.; Ott, M.; Horbinski, C.; Fang, D.; DeRay, C.M.; Levine, J.M.; Curran, M.A.; Heimberger, A.B. Intratumoral Delivery of STING Agonist Results in Clinical Responses in Canine Glioblastoma. Clin. Cancer Res. 2021, 27, 5528–5535. [Google Scholar] [CrossRef] [PubMed]
- Low, J.T.; Chandramohan, V.; Bowie, M.L.; Brown, M.C.; Waitkus, M.S.; Briley, A.; Stevenson, K.; Fuller, R.; Reitman, Z.J.; Muscat, A.M.; et al. Epigenetic STING Silencing Is Developmentally Conserved in Gliomas and Can Be Rescued by Methyltransferase Inhibition. Cancer Cell 2022, 40, 439–440. [Google Scholar] [CrossRef]
- Jost, S.C.; Hope, A.; Kiehl, E.; Perry, A.; Travers, S.; Garbow, J.R. A Novel Murine Model for Localized Radiation Necrosis and Its Characterization Using Advanced Magnetic Resonance Imaging. Int. J. Radiat. Oncol. 2009, 75, 527–533. [Google Scholar] [CrossRef]
- Donabedian, P.L.; Kossatz, S.; Engelbach, J.A.; Jannetti, S.A.; Carney, B.; Young, R.J.; Weber, W.A.; Garbow, J.R.; Reiner, T. Discriminating Radiation Injury from Recurrent Tumor with [18F]PARPi and Amino Acid PET in Mouse Models. EJNMMI Res. 2018, 8, 59. [Google Scholar] [CrossRef]
- Ge, X.; Song, K.-H.; Engelbach, J.A.; Yuan, L.; Gao, F.; Dahiya, S.; Rich, K.M.; Ackerman, J.J.H.; Garbow, J.R. Distinguishing Tumor Admixed in a Radiation Necrosis (RN) Background: 1H and 2H MR with a Novel Mouse Brain-Tumor/RN Model. Front. Oncol. 2022, 12, 885480. [Google Scholar] [CrossRef]
- Passarelli, A.; Mannavola, F.; Stucci, L.S.; Tucci, M.; Silvestris, F. Immune System and Melanoma Biology: A Balance between Immunosurveillance and Immune Escape. Oncotarget 2017, 8, 106132–106142. [Google Scholar] [CrossRef] [PubMed]
- Martin, A.M.; Cagney, D.N.; Catalano, P.J.; Alexander, B.M.; Redig, A.J.; Schoenfeld, J.D.; Aizer, A.A. Immunotherapy and Symptomatic Radiation Necrosis in Patients with Brain Metastases Treated with Stereotactic Radiation. JAMA Oncol. 2018, 4, 1123. [Google Scholar] [CrossRef]
- Vaios, E.; Shenker, R.; Hendrickson, P.; D’Anna, R.; Niedzwiecki, D.; Carpenter, D.; Floyd, W.; Winter, S.; Dietrich, J.; Floyd, S.; et al. MMAP-07 Impact of single and dual immune checkpoint blockade on risk of radiation necrosis among patients with brain metastases treated with stereotactic radiosurgery. Neuro-Oncol. Adv. 2022, 4, i16. [Google Scholar] [CrossRef]
- Spiotto, M.; Fu, Y.-X.; Weichselbaum, R.R. The Intersection of Radiotherapy and Immunotherapy: Mechanisms and Clinical Implications. Sci. Immunol. 2016, 1, eaag1266. [Google Scholar] [CrossRef]
- Van Limbergen, E.J.; De Ruysscher, D.K.; Olivo Pimentel, V.; Marcus, D.; Berbee, M.; Hoeben, A.; Rekers, N.; Theys, J.; Yaromina, A.; Dubois, L.J.; et al. Combining Radiotherapy with Immunotherapy: The Past, the Present and the Future. Br. J. Radiol. 2017, 90, 20170157. [Google Scholar] [CrossRef]
- Weichselbaum, R.R.; Liang, H.; Deng, L.; Fu, Y.-X. Radiotherapy and Immunotherapy: A Beneficial Liaison? Nat. Rev. Clin. Oncol. 2017, 14, 365–379. [Google Scholar] [CrossRef] [PubMed]
- Manda, K.; Glasow, A.; Paape, D.; Hildebrandt, G. Effects of Ionizing Radiation on the Immune System with Special Emphasis on the Interaction of Dendritic and T Cells. Front. Oncol. 2012, 2, 102. [Google Scholar] [CrossRef] [PubMed]
- Kluger, H.M.; Chiang, V.; Mahajan, A.; Zito, C.R.; Sznol, M.; Tran, T.; Weiss, S.A.; Cohen, J.V.; Yu, J.; Hegde, U.; et al. Long-Term Survival of Patients with Melanoma with Active Brain Metastases Treated with Pembrolizumab on a Phase II Trial. J. Clin. Oncol. 2019, 37, 52–60. [Google Scholar] [CrossRef]
- Dequesada, I.M.; Quisling, R.G.; Yachnis, A.; Friedman, W.A. CAN standard magnetic resonance imaging reliably distinguish recurrent tumor from radiation necrosis after radiosurgery for brain metastases? A radiographic-pathological study. Neurosurgery 2008, 63, 898–904. [Google Scholar] [CrossRef] [PubMed]
- Chao, S.T.; Ahluwalia, M.S.; Barnett, G.H.; Stevens, G.H.J.; Murphy, E.S.; Stockham, A.L.; Shiue, K.; Suh, J.H. Challenges with the Diagnosis and Treatment of Cerebral Radiation Necrosis. Int. J. Radiat. Oncol. 2013, 87, 449–457. [Google Scholar] [CrossRef]
- Miller, J.A.; Bennett, E.E.; Xiao, R.; Kotecha, R.; Chao, S.T.; Vogelbaum, M.A.; Barnett, G.H.; Angelov, L.; Murphy, E.S.; Yu, J.S.; et al. Association between Radiation Necrosis and Tumor Biology after Stereotactic Radiosurgery for Brain Metastasis. Int. J. Radiat. Oncol. 2016, 96, 1060–1069. [Google Scholar] [CrossRef]
- Minniti, G.; Scaringi, C.; Paolini, S.; Lanzetta, G.; Romano, A.; Cicone, F.; Osti, M.; Enrici, R.M.; Esposito, V. Single-Fraction versus Multifraction (3 × 9 Gy) Stereotactic Radiosurgery for Large (>2 cm) Brain Metastases: A Comparative Analysis of Local Control and Risk of Radiation-Induced Brain Necrosis. Int. J. Radiat. Oncol. 2016, 95, 1142–1148. [Google Scholar] [CrossRef]
- Siddiqui, Z.A.; Squires, B.S.; Johnson, M.D.; Baschnagel, A.M.; Chen, P.Y.; Krauss, D.J.; Olson, R.E.; Meyer, K.D.; Grills, I.S. Predictors of Radiation Necrosis in Long-Term Survivors after Gamma Knife Stereotactic Radiosurgery for Brain Metastases. Neuro-Oncol. Pract. 2020, 7, 400–408. [Google Scholar] [CrossRef]
- Winter, S.F.; Vaios, E.J.; Muzikansky, A.; Martinez-Lage, M.; Bussière, M.R.; Shih, H.A.; Loeffler, J.; Karschnia, P.; Loebel, F.; Vajkoczy, P.; et al. Defining Treatment-Related Adverse Effects in Patients with Glioma: Distinctive Features of Pseudoprogression and Treatment-Induced Necrosis. Oncologist 2020, 25, e1221–e1232. [Google Scholar] [CrossRef]
- Arbour, K.C.; Mezquita, L.; Long, N.; Rizvi, H.; Auclin, E.; Ni, A.; Martínez-Bernal, G.; Ferrara, R.; Lai, W.V.; Hendriks, L.E.L.; et al. Impact of Baseline Steroids on Efficacy of Programmed Cell Death-1 and Programmed Death-Ligand 1 Blockade in Patients with Non–Small-Cell Lung Cancer. J. Clin. Oncol. 2018, 36, 2872–2878. [Google Scholar] [CrossRef]
- Kotecha, R.; Kim, J.M.; Miller, J.A.; Juloori, A.; Chao, S.T.; Murphy, E.S.; Peereboom, D.M.; Mohammadi, A.M.; Barnett, G.H.; Vogelbaum, M.A.; et al. The Impact of Sequencing PD-1/PD-L1 Inhibitors and Stereotactic Radiosurgery for Patients with Brain Metastasis. Neuro Oncol. 2019, 21, 1060–1068. [Google Scholar] [CrossRef] [PubMed]
- Brown, P.D.; Ballman, K.V.; Cerhan, J.H.; Anderson, S.K.; Carrero, X.W.; Whitton, A.C.; Greenspoon, J.; Parney, I.F.; Laack, N.N.I.; Ashman, J.B.; et al. Postoperative Stereotactic Radiosurgery Compared with Whole Brain Radiotherapy for Resected Metastatic Brain Disease (NCCTG N107C/CEC·3): A Multicentre, Randomised, Controlled, Phase 3 Trial. Lancet Oncol. 2017, 18, 1049–1060. [Google Scholar] [CrossRef]
- Kayama, T.; Sato, S.; Sakurada, K.; Mizusawa, J.; Nishikawa, R.; Narita, Y.; Sumi, M.; Miyakita, Y.; Kumabe, T.; Sonoda, Y.; et al. Effects of Surgery with Salvage Stereotactic Radiosurgery versus Surgery with Whole-Brain Radiation Therapy in Patients with One to Four Brain Metastases (JCOG0504): A Phase III, Noninferiority, Randomized Controlled Trial. J. Clin. Oncol. 2018, 36, 3282–3289. [Google Scholar] [CrossRef]
- Mahajan, A.; Ahmed, S.; McAleer, M.F.; Weinberg, J.S.; Li, J.; Brown, P.; Settle, S.; Prabhu, S.S.; Lang, F.F.; Levine, N.; et al. Post-Operative Stereotactic Radiosurgery versus Observation for Completely Resected Brain Metastases: A Single-Centre, Randomised, Controlled, Phase 3 Trial. Lancet Oncol. 2017, 18, 1040–1048. [Google Scholar] [CrossRef] [PubMed]
- Blonigen, B.J.; Steinmetz, R.D.; Levin, L.; Lamba, M.A.; Warnick, R.E.; Breneman, J.C. Irradiated Volume as a Predictor of Brain Radionecrosis after Linear Accelerator Stereotactic Radiosurgery. Int. J. Radiat. Oncol. 2010, 77, 996–1001. [Google Scholar] [CrossRef]
- Ebner, D.; Rava, P.; Gorovets, D.; Cielo, D.; Hepel, J.T. Stereotactic Radiosurgery for Large Brain Metastases. J. Clin. Neurosci. 2015, 22, 1650–1654. [Google Scholar] [CrossRef]
- Prabhu, R.S.; Press, R.H.; Patel, K.R.; Boselli, D.M.; Symanowski, J.T.; Lankford, S.P.; McCammon, R.J.; Moeller, B.J.; Heinzerling, J.H.; Fasola, C.E.; et al. Single-Fraction Stereotactic Radiosurgery (SRS) Alone versus Surgical Resection and SRS for Large Brain Metastases: A Multi-Institutional Analysis. Int. J. Radiat. Oncol. 2017, 99, 459–467. [Google Scholar] [CrossRef]
- Martinage, G.; Geffrelot, J.; Stefan, D.; Bogart, E.; Rault, E.; Reyns, N.; Emery, E.; Makhloufi-Martinage, S.; Mouttet-Audouard, R.; Basson, L.; et al. Efficacy and Tolerance of Post-Operative Hypo-Fractionated Stereotactic Radiotherapy in a Large Series of Patients with Brain Metastases. Front. Oncol. 2019, 9, 184. [Google Scholar] [CrossRef] [PubMed]
- Eitz, K.A.; Lo, S.S.; Soliman, H.; Sahgal, A.; Theriault, A.; Pinkham, M.B.; Foote, M.C.; Song, A.J.; Shi, W.; Redmond, K.J.; et al. Multi-Institutional Analysis of Prognostic Factors and Outcomes after Hypofractionated Stereotactic Radiotherapy to the Resection Cavity in Patients with Brain Metastases. JAMA Oncol. 2020, 6, 1901. [Google Scholar] [CrossRef]
- Patel, K.R.; Burri, S.H.; Asher, A.L.; Crocker, I.R.; Fraser, R.W.; Zhang, C.; Chen, Z.; Kandula, S.; Zhong, J.; Press, R.H.; et al. Comparing Preoperative with Postoperative Stereotactic Radiosurgery for Resectable Brain Metastases. Neurosurgery 2016, 79, 279–285. [Google Scholar] [CrossRef]
- Li, F.; Tiede, B.; Massagué, J.; Kang, Y. Beyond Tumorigenesis: Cancer Stem Cells in Metastasis. Cell Res. 2007, 17, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Garsa, A.A.; Badiyan, S.N.; DeWees, T.; Simpson, J.R.; Huang, J.; Drzymala, R.E.; Barani, I.J.; Dowling, J.L.; Rich, K.M.; Chicoine, M.R.; et al. Predictors of Individual Tumor Local Control after Stereotactic Radiosurgery for Non-Small Cell Lung Cancer Brain Metastases. Int. J. Radiat. Oncol. 2014, 90, 407–413. [Google Scholar] [CrossRef] [PubMed]
- Kowalchuk, R.O.; Niranjan, A.; Lee, C.; Yang, H.; Liscak, R.; Guseynova, K.; Tripathi, M.; Kumar, N.; Peker, S.; Samanci, Y.; et al. Reirradiation with Stereotactic Radiosurgery after Local or Marginal Recurrence of Brain Metastases from Previous Radiosurgery. Int. J. Radiat. Oncol. 2022, 112, 726–734. [Google Scholar] [CrossRef] [PubMed]
- Sneed, P.K.; Chan, J.W.; Ma, L.; Braunstein, S.E.; Theodosopoulos, P.V.; Fogh, S.E.; Nakamura, J.L.; Boreta, L.; Raleigh, D.R.; Ziemer, B.P.; et al. Adverse Radiation Effect and Freedom from Progression Following Repeat Stereotactic Radiosurgery for Brain Metastases. J. Neurosurg. 2022, 138, 104–112. [Google Scholar] [CrossRef] [PubMed]
- Wilcox, J.A.; Brown, S.; Reiner, A.S.; Young, R.J.; Chen, J.; Bale, T.A.; Rosenblum, M.K.; Newman, W.C.; Brennan, C.W.; Tabar, V.; et al. Salvage Resection of Recurrent Previously Irradiated Brain Metastases: Tumor Control and Radiation Necrosis Dependency on Adjuvant Re-Irradiation. J. Neurooncol. 2021, 155, 277–286. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, S.B.; Gettinger, S.N.; Mahajan, A.; Chiang, A.C.; Herbst, R.S.; Sznol, M.; Tsiouris, A.J.; Cohen, J.; Vortmeyer, A.; Jilaveanu, L.; et al. Pembrolizumab for Patients with Melanoma or Non-Small-Cell Lung Cancer and Untreated Brain Metastases: Early Analysis of a Non-Randomised, Open-Label, Phase 2 Trial. Lancet Oncol. 2016, 17, 976–983. [Google Scholar] [CrossRef]
- Margolin, K.; Ernstoff, M.S.; Hamid, O.; Lawrence, D.; McDermott, D.; Puzanov, I.; Wolchok, J.D.; Clark, J.I.; Sznol, M.; Logan, T.F.; et al. Ipilimumab in Patients with Melanoma and Brain Metastases: An Open-Label, Phase 2 Trial. Lancet Oncol. 2012, 13, 459–465. [Google Scholar] [CrossRef]
- Tawbi, H.A.; Forsyth, P.A.; Hodi, F.S.; Algazi, A.P.; Hamid, O.; Lao, C.D.; Moschos, S.J.; Atkins, M.B.; Lewis, K.; Postow, M.A.; et al. Long-Term Outcomes of Patients with Active Melanoma Brain Metastases Treated with Combination Nivolumab plus Ipilimumab (CheckMate 204): Final Results of an Open-Label, Multicentre, Phase 2 Study. Lancet Oncol. 2021, 22, 1692–1704. [Google Scholar] [CrossRef]
- Long, G.V.; Atkinson, V.G.; Lo, S.; Sandhu, S.K.; Brown, M.; Gonzalez, M.; Guminski, A.; Scolyer, R.A.; Emmett, L.; Menzies, A.M.; et al. Long-Term Outcomes from the Randomized Phase II Study of Nivolumab (Nivo) or Nivo + ipilimumab (Ipi) in Patients (Pts) with Melanoma Brain Metastases (Mets): Anti-PD1 Brain Collaboration (ABC). Ann. Oncol. 2019, 30, v534. [Google Scholar] [CrossRef]
- Fecci, P.E.; Champion, C.D.; Hoj, J.; McKernan, C.M.; Goodwin, C.R.; Kirkpatrick, J.P.; Anders, C.K.; Pendergast, A.M.; Sampson, J.H. The Evolving Modern Management of Brain Metastasis. Clin. Cancer Res. 2019, 25, 6570–6580. [Google Scholar] [CrossRef] [PubMed]
- Lehrer, E.J.; Peterson, J.; Brown, P.D.; Sheehan, J.P.; Quiñones-Hinojosa, A.; Zaorsky, N.G.; Trifiletti, D.M. Treatment of Brain Metastases with Stereotactic Radiosurgery and Immune Checkpoint Inhibitors: An International Meta-Analysis of Individual Patient Data. Radiother. Oncol. 2019, 130, 104–112. [Google Scholar] [CrossRef] [PubMed]
- Colaco, R.J.; Martin, P.; Kluger, H.M.; Yu, J.B.; Chiang, V.L. Does Immunotherapy Increase the Rate of Radiation Necrosis after Radiosurgical Treatment of Brain Metastases? J. Neurosurg. 2016, 125, 17–23. [Google Scholar] [CrossRef]
- Minniti, G.; Anzellini, D.; Reverberi, C.; Cappellini, G.C.A.; Marchetti, L.; Bianciardi, F.; Bozzao, A.; Osti, M.; Gentile, P.C.; Esposito, V. Stereotactic Radiosurgery Combined with Nivolumab or Ipilimumab for Patients with Melanoma Brain Metastases: Evaluation of Brain Control and Toxicity. J. Immunother. Cancer 2019, 7, 102. [Google Scholar] [CrossRef]
- Diao, K.; Bian, S.X.; Routman, D.M.; Yu, C.; Kim, P.E.; Wagle, N.A.; Wong, M.K.; Zada, G.; Chang, E.L. Combination Ipilimumab and Radiosurgery for Brain Metastases: Tumor, Edema, and Adverse Radiation Effects. J. Neurosurg. 2018, 129, 1397–1406. [Google Scholar] [CrossRef] [PubMed]
- Four, S.D.; Janssen, Y.; Michotte, A.; Van Binst, A.-M.; Van den Begin, R.; Duerinck, J.; Neyns, B. Focal Radiation Necrosis of the Brain in Patients with Melanoma Brain Metastases Treated with Pembrolizumab. Cancer Med. 2018, 7, 4870–4879. [Google Scholar] [CrossRef]
- Kowalski, E.S.; Remick, J.S.; Sun, K.; Alexander, G.S.; Khairnar, R.; Morse, E.; Cherng, H.-R.; Berg, L.J.; Poirier, Y.; Lamichhane, N.; et al. Immune Checkpoint Inhibition in Patients Treated with Stereotactic Radiation for Brain Metastases. Radiat. Oncol. 2020, 15, 245. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, S.B.; Schalper, K.A.; Gettinger, S.N.; Mahajan, A.; Herbst, R.S.; Chiang, A.C.; Lilenbaum, R.; Wilson, F.H.; Omay, S.B.; Yu, J.B.; et al. Pembrolizumab for Management of Patients with NSCLC and Brain Metastases: Long-Term Results and Biomarker Analysis from a Non-Randomised, Open-Label, Phase 2 Trial. Lancet Oncol. 2020, 21, 655–663. [Google Scholar] [CrossRef]
- Lehrer, E.J.; Kowalchuk, R.O.; Gurewitz, J.; Bernstein, K.; Kondziolka, D.; Niranjan, A.; Wei, Z.; Lunsford, L.D.; Fakhoury, K.R.; Rusthoven, C.G.; et al. Concurrent Administration of Immune Checkpoint Inhibitors and Single Fraction Stereotactic Radiosurgery in Patients with Non-Small Cell Lung Cancer, Melanoma, and Renal Cell Carcinoma Brain Metastases Is Not Associated with an Increased Risk of Radiation. Int. J. Radiat. Oncol. 2023, in press. [CrossRef]
- Popp, I.; Rau, S.; Hintz, M.; Schneider, J.; Bilger, A.; Fennell, J.T.; Heiland, D.H.; Rothe, T.; Egger, K.; Nieder, C.; et al. Hippocampus-avoidance Whole-brain Radiation Therapy with a Simultaneous Integrated Boost for Multiple Brain Metastases. Cancer 2020, 126, 2694–2703. [Google Scholar] [CrossRef]
- Narayana, A.; Mathew, M.; Tam, M.; Kannan, R.; Madden, K.M.; Golfinos, J.G.; Parker, E.C.; Ott, P.A.; Pavlick, A.C. Vemurafenib and Radiation Therapy in Melanoma Brain Metastases. J. Neurooncol. 2013, 113, 411–416. [Google Scholar] [CrossRef] [PubMed]
- Cho, A.; Untersteiner, H.; Hirschmann, D.; Shaltout, A.; Göbl, P.; Dorfer, C.; Rössler, K.; Marik, W.; Kirchbacher, K.; Kapfhammer, I.; et al. Gamma Knife Radiosurgery for Brain Metastases in Non-Small Cell Lung Cancer Patients Treated with Immunotherapy or Targeted Therapy. Cancers 2020, 12, 3668. [Google Scholar] [CrossRef] [PubMed]
- Parsai, S.; Miller, J.A.; Juloori, A.; Chao, S.T.; Kotecha, R.; Mohammadi, A.M.; Ahluwalia, M.S.; Murphy, E.S.; Barnett, G.H.; Vogelbaum, M.A.; et al. Stereotactic Radiosurgery with Concurrent Lapatinib Is Associated with Improved Local Control for HER2-Positive Breast Cancer Brain Metastases. J. Neurosurg. 2020, 132, 503–511. [Google Scholar] [CrossRef]
- Park, C.; Buckley, E.D.; Van Swearingen, A.E.D.; Giles, W.; Herndon, J.E.; Kirkpatrick, J.P.; Anders, C.K.; Floyd, S.R. Systemic Therapy Type and Timing Effects on Radiation Necrosis Risk in HER2+ Breast Cancer Brain Metastases Patients Treated with Stereotactic Radiosurgery. Front. Oncol. 2022, 12, 854364. [Google Scholar] [CrossRef] [PubMed]
- Burris, H.A.; Hurtig, J. Radiation Recall with Anticancer Agents. Oncologist 2010, 15, 1227–1237. [Google Scholar] [CrossRef]
- Cagney, D.N.; Martin, A.M.; Catalano, P.J.; Reitman, Z.J.; Mezochow, G.A.; Lee, E.Q.; Wen, P.Y.; Weiss, S.E.; Brown, P.D.; Ahluwalia, M.S.; et al. Impact of Pemetrexed on Intracranial Disease Control and Radiation Necrosis in Patients with Brain Metastases from Non-Small Cell Lung Cancer Receiving Stereotactic Radiation. Radiother. Oncol. 2018, 126, 511–518. [Google Scholar] [CrossRef]
- Minniti, G.; Clarke, E.; Lanzetta, G.; Osti, M.F.; Trasimeni, G.; Bozzao, A.; Romano, A.; Enrici, R.M. Stereotactic Radiosurgery for Brain Metastases: Analysis of Outcome and Risk of Brain Radionecrosis. Radiat. Oncol. 2011, 6, 48. [Google Scholar] [CrossRef]
- Sneed, P.K.; Mendez, J.; Vemer-van den Hoek, J.G.M.; Seymour, Z.A.; Ma, L.; Molinaro, A.M.; Fogh, S.E.; Nakamura, J.L.; McDermott, M.W. Adverse Radiation Effect after Stereotactic Radiosurgery for Brain Metastases: Incidence, Time Course, and Risk Factors. J. Neurosurg. 2015, 123, 373–386. [Google Scholar] [CrossRef]
- Kohutek, Z.A.; Yamada, Y.; Chan, T.A.; Brennan, C.W.; Tabar, V.; Gutin, P.H.; Yang, T.J.; Rosenblum, M.K.; Ballangrud, Å.; Young, R.J.; et al. Long-Term Risk of Radionecrosis and Imaging Changes after Stereotactic Radiosurgery for Brain Metastases. J. Neurooncol. 2015, 125, 149–156. [Google Scholar] [CrossRef]
- Di Perri, D.; Tanguy, R.; Malet, C.; Robert, A.; Sunyach, M.-P. Risk of Radiation Necrosis after Hypofractionated Stereotactic Radiotherapy (HFSRT) for Brain Metastases: A Single Center Retrospective Study. J. Neurooncol. 2020, 149, 447–453. [Google Scholar] [CrossRef]
- Atkins, K.M.; Pashtan, I.M.; Bussière, M.R.; Kang, K.H.; Niemierko, A.; Daly, J.E.; Botticello, T.M.; Hurd, M.C.; Chapman, P.H.; Oh, K.; et al. Proton Stereotactic Radiosurgery for Brain Metastases: A Single-Institution Analysis of 370 Patients. Int. J. Radiat. Oncol. 2018, 101, 820–829. [Google Scholar] [CrossRef]
- Song, J.; Aljabab, S.; Abduljabbar, L.; Tseng, Y.D.; Rockhill, J.K.; Fink, J.R.; Chang, L.; Halasz, L.M. Radiation-Induced Brain Injury in Patients with Meningioma Treated with Proton or Photon Therapy. J. Neurooncol. 2021, 153, 169–180. [Google Scholar] [CrossRef] [PubMed]
- Badiyan, S.N.; Ulmer, S.; Ahlhelm, F.J.; Fredh, A.S.M.; Kliebsch, U.; Calaminus, G.; Bolsi, A.; Albertini, F.; Leiser, D.; Timmermann, B.; et al. Clinical and Radiologic Outcomes in Adults and Children Treated with Pencil-Beam Scanning Proton Therapy for Low-Grade Glioma. Int. J. Part. Ther. 2017, 3, 450–460. [Google Scholar] [CrossRef]
- Harrabi, S.B.; von Nettelbladt, B.; Gudden, C.; Adeberg, S.; Seidensaal, K.; Bauer, J.; Bahn, E.; Mairani, A.; Alber, M.; Haberer, T.; et al. Radiation Induced Contrast Enhancement after Proton Beam Therapy in Patients with Low Grade Glioma—How Safe Are Protons? Radiother. Oncol. 2021, 167, 211–218. [Google Scholar] [CrossRef] [PubMed]
- Sher, D.J.; Ringash, J. Quality of Life and Value Considerations in Head and Neck Proton Beam Therapy: The Holy Grail at Last, or the Quest Continues? Int. J. Radiat. Oncol. 2016, 95, 40–42. [Google Scholar] [CrossRef]
- Baumert, B.G.; Lomax, A.J.; Miltchev, V.; Davis, J.B. A Comparison of Dose Distributions of Proton and Photon Beams in Stereotactic Conformal Radiotherapy of Brain Lesions. Int. J. Radiat. Oncol. 2001, 49, 1439–1449. [Google Scholar] [CrossRef] [PubMed]
- Williamson, R.; Kondziolka, D.; Kanaan, H.; Lunsford, L.D.; Flickinger, J.C. Adverse Radiation Effects after Radiosurgery May Benefit from Oral Vitamin E and Pentoxifylline Therapy: A Pilot Study. Stereotact. Funct. Neurosurg. 2008, 86, 359–366. [Google Scholar] [CrossRef]
- Pareek, P.; Samdariya, S.; Sharma, A.; Gupta, N.; Shekhar, S.; Kirubakaran, R. Pentoxifylline and Vitamin E Alone or in Combination for Preventing and Treating Side Effects of Radiation Therapy and Concomitant Chemoradiotherapy. Cochrane Database Syst. Rev. 2016, 2016, CD012117. [Google Scholar] [CrossRef]
- Ohguri, T.; Imada, H.; Kohshi, K.; Kakeda, S.; Ohnari, N.; Morioka, T.; Nakano, K.; Konda, N.; Korogi, Y. Effect of Prophylactic Hyperbaric Oxygen Treatment for Radiation-Induced Brain Injury after Stereotactic Radiosurgery of Brain Metastases. Int. J. Radiat. Oncol. Biol. Phys. 2007, 67, 248–255. [Google Scholar] [CrossRef]
- Wang, X.S.; Ying, H.M.; He, X.Y.; Zhou, Z.R.; Wu, Y.R.; Hu, C.S. Treatment of Cerebral Radiation Necrosis with Nerve Growth Factor: A Prospective, Randomized, Controlled Phase II Study. Radiother. Oncol. 2016, 120, 69–75. [Google Scholar] [CrossRef]
- Vaios, E.J.; Batich, K.A.; Buckley, A.F.; Dunn-Pirio, A.; Patel, M.P.; Kirkpatrick, J.P.; Goudar, R.; Peters, K.B. Resolution of Radiation Necrosis with Bevacizumab Following Radiation Therapy for Primary CNS Lymphoma. Oncotarget 2022, 13, 576–582. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, J.; Kumar, A.J.; Conrad, C.A.; Levin, V.A. Effect of Bevacizumab on Radiation Necrosis of the Brain. Int. J. Radiat. Oncol. Biol. Phys. 2007, 67, 323–326. [Google Scholar] [CrossRef] [PubMed]
- Torcuator, R.; Zuniga, R.; Mohan, Y.S.; Rock, J.; Doyle, T.; Anderson, J.; Gutierrez, J.; Ryu, S.; Jain, R.; Rosenblum, M.; et al. Initial Experience with Bevacizumab Treatment for Biopsy Confirmed Cerebral Radiation Necrosis. J. Neurooncol. 2009, 94, 63–68. [Google Scholar] [CrossRef]
- Levin, V.A.; Bidaut, L.; Hou, P.; Kumar, A.J.; Wefel, J.S.; Bekele, B.N.; Grewal, J.; Prabhu, S.; Loghin, M.; Gilbert, M.R.; et al. Randomized Double-Blind Placebo-Controlled Trial of Bevacizumab Therapy for Radiation Necrosis of the Central Nervous System. Int. J. Radiat. Oncol. Biol. Phys. 2011, 79, 1487–1495. [Google Scholar] [CrossRef] [PubMed]
- Boothe, D.; Young, R.; Yamada, Y.; Prager, A.; Chan, T.; Beal, K. Bevacizumab as a Treatment for Radiation Necrosis of Brain Metastases Post Stereotactic Radiosurgery. Neuro Oncol. 2013, 15, 1257–1263. [Google Scholar] [CrossRef]
- Liao, G.; Khan, M.; Zhao, Z.; Arooj, S.; Yan, M.; Li, X. Bevacizumab Treatment of Radiation-Induced Brain Necrosis: A Systematic Review. Front. Oncol. 2021, 11, 593449. [Google Scholar] [CrossRef]
- Moore, A.; Yust-Katz, S.; Icht, O.; Eliyahou, R.; Gordon, N.; Cohen, A.Y.; Goldstein, I.M.; Peled, N.; Seigal, T.; Amiel, A.; et al. Bevacizumab for Stereotactic Radiosurgery-Induced Radiation Necrosis in Patients with Non-Small Cell Lung Cancer Treated with Immune Check-Point Inhibitors. J. Neurol. Sci. 2021, 427, 117556. [Google Scholar] [CrossRef]
- Newman, W.C.; Goldberg, J.; Guadix, S.W.; Brown, S.; Reiner, A.S.; Panageas, K.; Beal, K.; Brennan, C.W.; Tabar, V.; Young, R.J.; et al. The Effect of Surgery on Radiation Necrosis in Irradiated Brain Metastases: Extent of Resection and Long-Term Clinical and Radiographic Outcomes. J. Neurooncol. 2021, 153, 507–518. [Google Scholar] [CrossRef]
- Vellayappan, B.; Tan, C.L.; Yong, C.; Khor, L.K.; Koh, W.Y.; Yeo, T.T.; Detsky, J.; Lo, S.; Sahgal, A. Diagnosis and Management of Radiation Necrosis in Patients with Brain Metastases. Front. Oncol. 2018, 8, 395. [Google Scholar] [CrossRef]
- Norred, S.E.; Johnson, J.A. Magnetic Resonance-Guided Laser Induced Thermal Therapy for Glioblastoma Multiforme: A Review. Biomed. Res. Int. 2014, 2014, 761312. [Google Scholar] [CrossRef]
- Ahluwalia, M.; Barnett, G.H.; Deng, D.; Tatter, S.B.; Laxton, A.W.; Mohammadi, A.M.; Leuthardt, E.; Chamoun, R.; Judy, K.; Asher, A.; et al. Laser Ablation after Stereotactic Radiosurgery: A Multicenter Prospective Study in Patients with Metastatic Brain Tumors and Radiation Necrosis. J. Neurosurg. 2018, 130, 804–811. [Google Scholar] [CrossRef]
- Sujijantarat, N.; Hong, C.S.; Owusu, K.A.; Elsamadicy, A.A.; Antonios, J.P.; Koo, A.B.; Baehring, J.M.; Chiang, V.L. Laser Interstitial Thermal Therapy (LITT) vs. Bevacizumab for Radiation Necrosis in Previously Irradiated Brain Metastases. J. Neurooncol. 2020, 148, 641–649. [Google Scholar] [CrossRef]
- Hong, C.S.; Deng, D.; Vera, A.; Chiang, V.L. Laser-Interstitial Thermal Therapy Compared to Craniotomy for Treatment of Radiation Necrosis or Recurrent Tumor in Brain Metastases Failing Radiosurgery. J. Neurooncol. 2019, 142, 309–317. [Google Scholar] [CrossRef]
- Hong, C.; Sujijantarat, N.; Chiang, V. MLTI-06. Bevacizumab versus surgical intervention for radiation necrosis in previously irradiated brain metastases. Neuro-Oncol. Adv. 2019, 1, i15. [Google Scholar] [CrossRef]
- Chon, H.; Yoon, K.; Lee, D.; Kwon, D.H.; Cho, Y.H. Single-Fraction versus Hypofractionated Stereotactic Radiosurgery for Medium-Sized Brain Metastases of 2.5 to 3 cm. J. Neurooncol. 2019, 145, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.J.; Choi, K.-S.; Park, E.S.; Cho, Y.H. Single- and Hypofractionated Stereotactic Radiosurgery for Large (>2 cm) Brain Metastases: A Systematic Review. J. Neurooncol. 2021, 154, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, Y.R.; Li, X.A.; el Naqa, I.; Hahn, C.A.; Marks, L.B.; Merchant, T.E.; Dicker, A.P. Radiation Dose–Volume Effects in the Brain. Int. J. Radiat. Oncol. 2010, 76, S20–S27. [Google Scholar] [CrossRef] [PubMed]
- Kirkpatrick, J.P.; Wang, Z.; Sampson, J.H.; McSherry, F.; Herndon, J.E.; Allen, K.J.; Duffy, E.; Hoang, J.K.; Chang, Z.; Yoo, D.S.; et al. Defining the Optimal Planning Target Volume in Image-Guided Stereotactic Radiosurgery of Brain Metastases: Results of a Randomized Trial. Int. J. Radiat. Oncol. 2015, 91, 100–108. [Google Scholar] [CrossRef]
- Sebastian, N.T.; Glenn, C.; Hughes, R.; Raval, R.; Chu, J.; DiCostanzo, D.; Bell, E.H.; Grecula, J.; Arnett, A.; Gondal, H.; et al. Linear Accelerator-Based Radiosurgery Is Associated with Lower Incidence of Radionecrosis Compared with Gamma Knife for Treatment of Multiple Brain Metastases. Radiother. Oncol. 2020, 147, 136–143. [Google Scholar] [CrossRef]
- Xu, J.-L.; Li, Y.-L.; Lian, J.-M.; Dou, S.; Yan, F.-S.; Wu, H.; Shi, D. Distinction between Postoperative Recurrent Glioma and Radiation Injury Using MR Diffusion Tensor Imaging. Neuroradiology 2010, 52, 1193–1199. [Google Scholar] [CrossRef]
- Detsky, J.S.; Keith, J.; Conklin, J.; Symons, S.; Myrehaug, S.; Sahgal, A.; Heyn, C.C.; Soliman, H. Differentiating Radiation Necrosis from Tumor Progression in Brain Metastases Treated with Stereotactic Radiotherapy: Utility of Intravoxel Incoherent Motion Perfusion MRI and Correlation with Histopathology. J. Neurooncol. 2017, 134, 433–441. [Google Scholar] [CrossRef]
- Alexiou, G.A.; Tsiouris, S.; Kyritsis, A.P.; Voulgaris, S.; Argyropoulou, M.I.; Fotopoulos, A.D. Glioma Recurrence versus Radiation Necrosis: Accuracy of Current Imaging Modalities. J. Neurooncol. 2009, 95, 1–11. [Google Scholar] [CrossRef]
- Hu, L.S.; Baxter, L.C.; Smith, K.A.; Feuerstein, B.G.; Karis, J.P.; Eschbacher, J.M.; Coons, S.W.; Nakaji, P.; Yeh, R.F.; Debbins, J.; et al. Relative Cerebral Blood Volume Values to Differentiate High-Grade Glioma Recurrence from Posttreatment Radiation Effect: Direct Correlation between Image-Guided Tissue Histopathology and Localized Dynamic Susceptibility-Weighted Contrast-Enhanced Perfusio. Am. J. Neuroradiol. 2009, 30, 552–558. [Google Scholar] [CrossRef]
- McConathy, J.; Goodman, M.M. Non-Natural Amino Acids for Tumor Imaging Using Positron Emission Tomography and Single Photon Emission Computed Tomography. Cancer Metastasis Rev. 2008, 27, 555–573. [Google Scholar] [CrossRef]
- Cicone, F.; Minniti, G.; Romano, A.; Papa, A.; Scaringi, C.; Tavanti, F.; Bozzao, A.; Maurizi Enrici, R.; Scopinaro, F. Accuracy of F-DOPA PET and Perfusion-MRI for Differentiating Radionecrotic from Progressive Brain Metastases after Radiosurgery. Eur. J. Nucl. Med. Mol. Imaging 2015, 42, 103–111. [Google Scholar] [CrossRef]
- Cicone, F.; Carideo, L.; Scaringi, C.; Romano, A.; Mamede, M.; Papa, A.; Tofani, A.; Cascini, G.L.; Bozzao, A.; Scopinaro, F.; et al. Long-Term Metabolic Evolution of Brain Metastases with Suspected Radiation Necrosis Following Stereotactic Radiosurgery: Longitudinal Assessment by F-DOPA PET. Neuro Oncol. 2021, 23, 1024–1034. [Google Scholar] [CrossRef] [PubMed]
- Yomo, S.; Oguchi, K. Prospective Study of 11C–Methionine PET for Distinguishing between Recurrent Brain Metastases and Radiation Necrosis: Limitations of Diagnostic Accuracy and Long-Term Results of Salvage Treatment. BMC Cancer 2017, 17, 713. [Google Scholar] [CrossRef] [PubMed]
- Kotecha, R.; Chaglassian, A.; Tainer, N.; Teoh, E. TRLS-01. Trial in Progress: A Prospective, Multicenter Phase 2b Study to Establish Image Interpretation Criteria for 18F-Fluciclovine PET in Detecting Recurrent Brain Metastases after Radiation Therapy (PURSUE). Neuro-Oncol. Adv. 2021, 3, iii5. [Google Scholar] [CrossRef]
- Zeng, Q.-S.; Li, C.-F.; Zhang, K.; Liu, H.; Kang, X.-S.; Zhen, J.-H. Multivoxel 3D Proton MR Spectroscopy in the Distinction of Recurrent Glioma from Radiation Injury. J. Neurooncol. 2007, 84, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Peng, L.; Parekh, V.; Huang, P.; Lin, D.D.; Sheikh, K.; Baker, B.; Kirschbaum, T.; Silvestri, F.; Son, J.; Robinson, A.; et al. Distinguishing True Progression from Radionecrosis after Stereotactic Radiation Therapy for Brain Metastases with Machine Learning and Radiomics. Int. J. Radiat. Oncol. Biol. Phys. 2018, 102, 1236–1243. [Google Scholar] [CrossRef]
- Zhang, Z.; Yang, J.; Ho, A.; Jiang, W.; Logan, J.; Wang, X.; Brown, P.D.; McGovern, S.L.; Guha-Thakurta, N.; Ferguson, S.D.; et al. A Predictive Model for Distinguishing Radiation Necrosis from Tumour Progression after Gamma Knife Radiosurgery Based on Radiomic Features from MR Images. Eur. Radiol. 2018, 28, 2255–2263. [Google Scholar] [CrossRef]
- Chen, X.; Parekh, V.S.; Peng, L.; Chan, M.D.; Redmond, K.J.; Soike, M.; McTyre, E.; Lin, D.; Jacobs, M.A.; Kleinberg, L.R. Multiparametric Radiomic Tissue Signature and Machine Learning for Distinguishing Radiation Necrosis from Tumor Progression after Stereotactic Radiosurgery. Neuro-Oncol. Adv. 2021, 3, vdab150. [Google Scholar] [CrossRef]
- Hettal, L.; Stefani, A.; Salleron, J.; Courrech, F.; Behm-Ansmant, I.; Constans, J.M.; Gauchotte, G.; Vogin, G. Radiomics Method for the Differential Diagnosis of Radionecrosis versus Progression after Fractionated Stereotactic Body Radiotherapy for Brain Oligometastasis. Radiat. Res. 2020, 193, 471–480. [Google Scholar] [CrossRef]
- Cho, H.H.; Lee, H.Y.; Kim, E.; Lee, G.; Kim, J.; Kwon, J.; Park, H. Radiomics-Guided Deep Neural Networks Stratify Lung Adenocarcinoma Prognosis from CT Scans. Commun. Biol. 2021, 4, 1286. [Google Scholar] [CrossRef]
- Hosny, A.; Parmar, C.; Quackenbush, J.; Schwartz, L.H.; Aerts, H.J.W.L. Artificial Intelligence in Radiology. Nat. Rev. Cancer 2018, 18, 500–510. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Vaios, E.J.; Carpenter, D.J.; Yang, Z.; Cui, Y.; Lafata, K.; Fecci, P.; Yin, F.F.; Floyd, S.R.; Wang, C. A Radiomics-Integrated Deep Learning Model for Identifying Radionecrosis Following Brain Metastasis Stereotactic Radiosurgery (SRS). Int. J. Radiat. Oncol. 2022, 114, S114. [Google Scholar] [CrossRef]
- Elhalawani, H.; Hammoudeh, L.A.; Cagney, D.N.; Qian, J.M.; Martin, A.; Zgrabik, J.; Meyers, J.; Pataki, K.J.; Martin, K.; Khouj, Y.; et al. Leveraging Serial MRI Radiomics and Machine Learning to Predict Risk of Radiation Necrosis in Patients with Brain Metastases Managed with Stereotactic Radiation and Immunotherapy. Int. J. Radiat. Oncol. 2022, 114, e128. [Google Scholar] [CrossRef]
- Soler, D.C.; Young, A.B.; Cooper, K.D.; Kerstetter-Fogle, A.; Barnholtz-Sloan, J.S.; Gittleman, H.; McCormick, T.S.; Sloan, A.E. The Ratio of HLA-DR and VNN2+ Expression on CD14+ Myeloid Derived Suppressor Cells Can Distinguish Glioblastoma from Radiation Necrosis Patients. J. Neurooncol. 2017, 134, 189–196. [Google Scholar] [CrossRef]
- Koch, C.J.; Lustig, R.A.; Yang, X.-Y.; Jenkins, W.T.; Wolf, R.L.; Martinez-Lage, M.; Desai, A.; Williams, D.; Evans, S.M. Microvesicles as a Biomarker for Tumor Progression versus Treatment Effect in Radiation/Temozolomide-Treated Glioblastoma Patients. Transl. Oncol. 2014, 7, 752–758. [Google Scholar] [CrossRef]
- Barault, L.; Amatu, A.; Siravegna, G.; Ponzetti, A.; Moran, S.; Cassingena, A.; Mussolin, B.; Falcomatà, C.; Binder, A.M.; Cristiano, C.; et al. Discovery of Methylated Circulating DNA Biomarkers for Comprehensive Non-Invasive Monitoring of Treatment Response in Metastatic Colorectal Cancer. Gut 2018, 67, 1995–2005. [Google Scholar] [CrossRef] [PubMed]
- Xu, R.; Wei, W.; Krawczyk, M.; Wang, W.; Luo, H.; Flagg, K.; Yi, S.; Shi, W.; Quan, Q.; Li, K.; et al. Circulating Tumour DNA Methylation Markers for Diagnosis and Prognosis of Hepatocellular Carcinoma. Nat. Mater. 2017, 16, 1155–1161. [Google Scholar] [CrossRef] [PubMed]
- Peter, M.R.; Bilenky, M.; Shi, Y.; Pu, J.; Kamdar, S.; Hansen, A.R.; Fleshner, N.E.; Sridhar, S.S.; Joshua, A.M.; Hirst, M.; et al. A Novel Methylated Cell-Free DNA Marker Panel to Monitor Treatment Response in Metastatic Prostate Cancer. Epigenomics 2022, 14, 811–822. [Google Scholar] [CrossRef]
- Visvanathan, K.; Fackler, M.S.; Zhang, Z.; Lopez-Bujanda, Z.A.; Jeter, S.C.; Sokoll, L.J.; Garrett-Mayer, E.; Cope, L.M.; Umbricht, C.B.; Euhus, D.M.; et al. Monitoring of Serum DNA Methylation as an Early Independent Marker of Response and Survival in Metastatic Breast Cancer: TBCRC 005 Prospective Biomarker Study. J. Clin. Oncol. 2017, 35, 751–758. [Google Scholar] [CrossRef]
- Diehl, F.; Schmidt, K.; Choti, M.A.; Romans, K.; Goodman, S.; Li, M.; Thornton, K.; Agrawal, N.; Sokoll, L.; Szabo, S.A.; et al. Circulating Mutant DNA to Assess Tumor Dynamics. Nat. Med. 2008, 14, 985–990. [Google Scholar] [CrossRef] [PubMed]
- Tie, J.; Cohen, J.D.; Lahouel, K.; Lo, S.N.; Wang, Y.; Kosmider, S.; Wong, R.; Shapiro, J.; Lee, M.; Harris, S.; et al. Circulating Tumor DNA Analysis Guiding Adjuvant Therapy in Stage II Colon Cancer. N. Engl. J. Med. 2022, 386, 2261–2272. [Google Scholar] [CrossRef] [PubMed]
- Sabedot, T.S.; Malta, T.M.; Snyder, J.; Nelson, K.; Wells, M.; DeCarvalho, A.C.; Mukherjee, A.; Chitale, D.A.; Mosella, M.S.; Sokolov, A.; et al. A Serum-Based DNA Methylation Assay Provides Accurate Detection of Glioma. Neuro Oncol. 2021, 23, 1494–1508. [Google Scholar] [CrossRef]
- Wiencke, J.K.; Koestler, D.C.; Salas, L.A.; Wiemels, J.L.; Roy, R.P.; Hansen, H.M.; Rice, T.; McCoy, L.S.; Bracci, P.M.; Molinaro, A.M.; et al. Immunomethylomic Approach to Explore the Blood Neutrophil Lymphocyte Ratio (NLR) in Glioma Survival. Clin. Epigenet. 2017, 9, 10. [Google Scholar] [CrossRef] [PubMed]
| Immunotherapy Studies | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Author | Study Type | Sample Size * | Histology | Radiation | Systemic Therapy | Timing of Immunotherapy | Follow Up (Months) | Any Grade Necrosis Rate * | Biopsy Rate * | Symptomatic Necrosis Rate * | Necrosis Predictors |
| Colaco (2016) | Retrospective | 180 | Lung 39% Melanoma 31% Breast 15% | SRS | ICI only: 18% TT only: 11% CT only: 46% None: 2% | Not reported | 11.7 | 39 (22%) ICI only: 12 (38%) TT only: 5 (25%) CT only: 14 (17%) | 11 (28%) | 18 (46%) | ICI (OR: 2.71) |
| Diao (2018) | Retrospective | 91 | Melanoma 100% | SRS + ICI vs. SRS | 56% Ipilimumab | 25% concurrent (≤4 wks) | 7.4 | SRS alone: 1 (3%) Concurrent: 2 (9%) Delayed: 2 (7%) | 5 (100%) | 5 (100%) | Not reported |
| Martin (2018) | Retrospective | 480 | NSCLC 61% Melanoma 30% | SRS/fSRS + ICI vs. SRS/fSRS | 24% ICI (dual 0%) | Not reported | 23.1 vs. 25.1 | Not reported | Not reported | 23 (20%) vs. 25 (7%) | IO (HR: 2.56) Melanoma (HR: 4.02) |
| Du Four (2018) | Retrospective | 43 | Melanoma 100% | RT + ICI (72% SRS, 19% WBRT) | 100% Pembro (dual 0%) | SRS before Pembro (72%) | 50 | 5 (12%) | 3 (60%) | 5 (100%) | Not reported |
| Kluger (2019) | Prospective | 23 | Melanoma 100% | Prior RT (SRS 52%, WBRT 22%) | 100% Pembro | Not reported | 24 | 7 (30%) | 5 (71%) | Not reported | Not reported |
| Minniti (2019) | Retrospective | 80 | Melanoma 100% | SRS/fSRS + ICI | 56% Ipilimumab 44% Nivolumab (dual 0%) | 100% concurrent (≤1 wk) | 15 | 28 (35%) | 5 (18%) | 12 (43%) | GTV (for symptomatic necrosis) |
| Kowalski (2020) | Retrospective | 179 | NSCLC 70% Melanoma 6% | SRS + ICI vs. SRS | 20% ICI (dual 2%) | 100% concurrent (≤3 months) | 7.7 vs. 10.3 | Not reported | None | 1 (4%) vs. 10 (7%) | Tumor size ≤ 2 cm (HR: 0.24) |
| Goldberg (2020) | Prospective | 42 | NSCLC (100%) | 21 with prior RT (SRS 38%, WBRT 19%) | 100% Pembro | 19% ≤3 months | 8.3 | 3 (14%) | Not reported | 1 (33%) | Not reported |
| Vaios (2022) | Retrospective | 206 | NSCLC 56% Melanoma 44% | SRS/fSRS + ICI vs. SRS/fSRS | 75% ICI (dual 26%) | 49% concurrent (≤4 wks) | 15.3 | Dual: 78 (26%) lesions Single: 87 (14%) No ICI: 39 (13%) | 25 (12%) lesions | Dual: 20 (36%) Single: 17 (17%) SRS alone: 7 (14%) | Melanoma (HR: 2.41) fSRS (HR: 0.27) Concurrent ICI (HR: 6.47) |
| Lehrer (2023) | Retrospective | 657 | NSCLC 57% Melanoma 36% | SRS + ICI | 100% ICI (dual 16%) | 44% concurrent (≤4 wks) | 13.4 | 66 (10%) | 5 (8%) | 45 (68%) | V12Gy (per RPA analysis) |
| Targeted Therapy Studies | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Author | Study Type | Sample Size * | Histology | Radiation | Systemic Therapy | Timing of Targeted Therapy | Follow Up (Months) | Overall Necrosis Rate * | Biopsy Rate * | Symptomatic Necrosis Rate * | Necrosis Predictors |
| Narayana (2013) | Retrospective | 12 | Melanoma 100% (V600 mutant) | RT + TT (58% SRS, 25% WBRT) | 100% vemurafenib | 42% concurrent (during RT) | 12.2 | 1 (8%) | None | 1 (100%) | Not reported |
| Cho (2020) | Retrospective | 379 | NSCLC 100% | SRS +/− ICI/TT | ICI: 18% TT: 15% TT + ICI: 4% | Not reported | 10.7 | 28 (7%) | None | Not reported | Not reported |
| Parsai (2020) | Retrospective | 126 | HER2+ Breast 100% | SRS + TT vs. SRS | 37% lapatinib | 19% concurrent (≤5 d) | 17.1 | 1-year 1% vs. 6% | None | Not reported | Tumor volume |
| Popp (2020) | Prospective | 124 | NSCLC 52% Melanoma 14% Breast 19% | HA-WBRT + SIB vs. WBRT | ICI: 6% TT: 28% | 73% concurrent (during or after RT) | 8.5 vs. 6.3 | HA-WBRT + SIB: 27 (7%) lesions | HA-WBRT + SIB: 2 (7%) lesions | HA-WBRT + SIB: 2 (3%) | Not reported |
| Park (2022) | Retrospective | 46 | HER2+ Breast 100% | SRS/fSRS + TT/Chemo | 100% TT/chemo | 59% concurrent (≤4 wks) | >12 | 28 (61%) | 10 (36%) | Not reported | Multiple HER2-directed agents |
| Chemotherapy Studies | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author | Study Type | Sample Size * | Histology | Radiation | Systemic Therapy | Chemo Agents | Timing of Chemotherapy | Follow Up (Months) | Overall Necrosis Rate * | Biopsy Rate * | Symptomatic Necrosis Rate * | Necrosis Predictors |
| Minniti (2011) | Retrospective | 206 | Lung 51% Melanoma 17% Breast 18% | SRS | 76% Chemo | Not reported | 100% before or after SRS | 9.4 | 75 (24%) lesions | 12 (16%) lesions | 31 (41%) lesions | Tumor volume V10 Gy V12 Gy |
| Sneed (2015) | Retrospective | 435 | Lung 40% Melanoma 14% Breast 31% | SRS | 59% of lesions (ICI: 2% Chemo: 38% TT: 9%) | Gemcitabine, capecitabine, vinca alkaloids, antifolates, taxanes, platinum agents, topoisomerase inhibitors | 100% concurrent (≤1 month) | 9.9 | 118 (5%) lesions | 17 (14%) lesions | 71 (60%) lesions | Prior SRS or WBRT (HR: 3.7) Target volume (HR: 1.1) Taxane (HR: 0.3) Capecitabine/5FU (HR: 2.6) |
| Kohutek (2015) | Retrospective | 160 | NSCLC 43% Melanoma 23% Breast 16% | SRS | 44% Chemo | Not reported | 100% concurrent (≤8 wks) | 17.2 | 70 (26%) lesions | 22 (31%) lesions | 47 (67%) lesions | Tumor diameter (HR: 3.1) |
| Cagney (2018) | Retrospective | 149 | NSCLC 100% | SRS/fSRS + pemetrexed vs. SRS/fSRS + Other Chemo | 100% Chemo | Pemetrexed (70.5%) or Other (26.8%); 91% received alternative platinum doublet | 100% after SRS | 24 vs. 20 | 24% vs. 10% at 1 year | None | Not reported | Pemetrexed (HR: 2.7) |
| Siddiqui (2019) | Retrospective | 198 | Lung 62% Melanoma 4% Breast 21% | SRS | ICI: 1% Chemo: 89% TT: 10% | Not reported | 100% concurrent (≤3 months) | 24 | 55 (8%) lesions | 10 (18%) lesions | 33 (60%) lesions | Tumor volume (HR: 1.1) Female gender (HR: 0.5) |
| Di Perri (2020) | Retrospective | 294 | Lung 56% Melanoma 4% Breast 17% | fSRS | ICI: 7% Chemo: 44% Other: 35% | Not reported | 100% concurrent (≤3 months) | 16.8 | 33 (9.2%) lesions | None | 17 (51.5%) lesions | 27 Gy/3 fx (HR: 3.07) 35 Gy/5 fx (HR: 4.22) ICI (HR: 2.69) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vaios, E.J.; Winter, S.F.; Shih, H.A.; Dietrich, J.; Peters, K.B.; Floyd, S.R.; Kirkpatrick, J.P.; Reitman, Z.J. Novel Mechanisms and Future Opportunities for the Management of Radiation Necrosis in Patients Treated for Brain Metastases in the Era of Immunotherapy. Cancers 2023, 15, 2432. https://doi.org/10.3390/cancers15092432
Vaios EJ, Winter SF, Shih HA, Dietrich J, Peters KB, Floyd SR, Kirkpatrick JP, Reitman ZJ. Novel Mechanisms and Future Opportunities for the Management of Radiation Necrosis in Patients Treated for Brain Metastases in the Era of Immunotherapy. Cancers. 2023; 15(9):2432. https://doi.org/10.3390/cancers15092432
Chicago/Turabian StyleVaios, Eugene J., Sebastian F. Winter, Helen A. Shih, Jorg Dietrich, Katherine B. Peters, Scott R. Floyd, John P. Kirkpatrick, and Zachary J. Reitman. 2023. "Novel Mechanisms and Future Opportunities for the Management of Radiation Necrosis in Patients Treated for Brain Metastases in the Era of Immunotherapy" Cancers 15, no. 9: 2432. https://doi.org/10.3390/cancers15092432
APA StyleVaios, E. J., Winter, S. F., Shih, H. A., Dietrich, J., Peters, K. B., Floyd, S. R., Kirkpatrick, J. P., & Reitman, Z. J. (2023). Novel Mechanisms and Future Opportunities for the Management of Radiation Necrosis in Patients Treated for Brain Metastases in the Era of Immunotherapy. Cancers, 15(9), 2432. https://doi.org/10.3390/cancers15092432






