Development of a Duplex Serological Multiplex Assay for the Simultaneous Detection of Epstein-Barr Virus IgA and IgG Antibodies in Nasopharyngeal Carcinoma Patients
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Material/Study Population
2.2. Serology
2.2.1. Singleplex Assay
2.2.2. Development of a Duplex Assay
2.3. Molecular Tumor Analysis
2.4. Statistical Analysis
3. Results
3.1. Assay Development
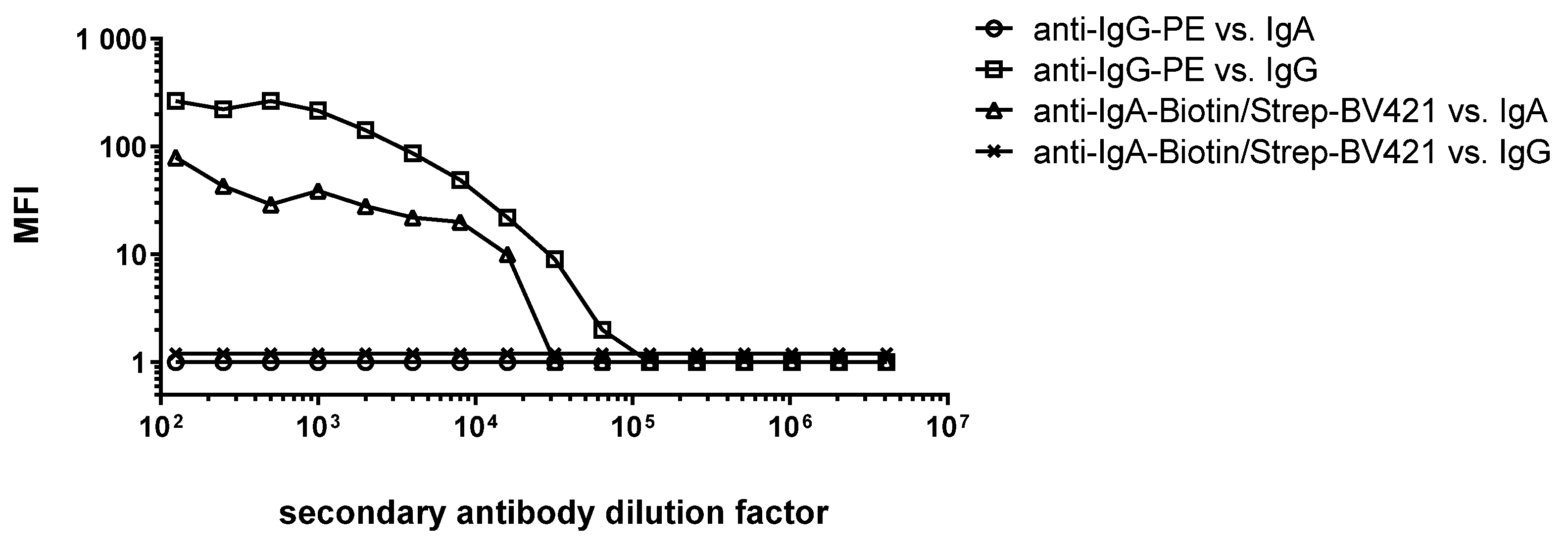
3.1.1. Selection of Antibody-Dye Combinations
3.1.2. Determination of the Optimal Serum Dilution Factor for the Simultaneous Detection of IgA and IgG Antibodies
3.1.3. Duplexing of IgA and IgG Antibodies
3.2. Study Data: Simultaneous Measurement of EBV IgA and IgG Antibodies in NPC Cases and Controls from the Head and Neck 5000 Study
3.2.1. Correlation of IgA and IgG Antibody Responses in Singleplex (Luminex 200) and Duplex (Intelliflex) Assay
3.2.2. Seropositivity by EBER-ISH Status
3.2.3. Performance of the 13-Marker Antibody Risk Stratification Signature
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chang, E.T.; Adami, H.O. The enigmatic epidemiology of nasopharyngeal carcinoma. Cancer Epidemiol. Biomark. Prev. 2006, 15, 1765–1777. [Google Scholar] [CrossRef] [PubMed]
- Ferlay, J.; Soerjomataram, I.; Dikshit, R.; Eser, S.; Mathers, C.; Rebelo, M.; Parkin, D.M.; Forman, D.; Bray, F. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int. J. Cancer 2015, 136, E359–E386. [Google Scholar] [CrossRef] [PubMed]
- Henle, W.; Henle, G.; Ho, H.C.; Burtin, P.; Cachin, Y.; Clifford, P.; de Schryver, A.; de-Thé, G.; Diehl, V.; Klein, G. Antibodies to Epstein-Barr virus in nasopharyngeal carcinoma, other head and neck neoplasms, and control groups. J. Natl. Cancer Inst. 1970, 44, 225–231. [Google Scholar] [PubMed]
- Chien, Y.C.; Chen, J.Y.; Liu, M.Y.; Yang, H.I.; Hsu, M.M.; Chen, C.J.; Yang, C.S. Serologic markers of Epstein-Barr virus infection and nasopharyngeal carcinoma in Taiwanese men. N. Engl. J. Med. 2001, 345, 1877–1882. [Google Scholar] [CrossRef] [PubMed]
- Robinson, M.; Suh, Y.; Paleri, V.; Devlin, D.; Ayaz, B.; Pertl, L.; Thavaraj, S. Oncogenic human papillomavirus-associated nasopharyngeal carcinoma: An observational study of correlation with ethnicity, histological subtype and outcome in a UK population. Infect. Agents Cancer 2013, 8, 30. [Google Scholar] [CrossRef]
- Dogan, S.; Hedberg, M.L.; Ferris, R.L.; Rath, T.J.; Assaad, A.M.; Chiosea, S.I. Human papillomavirus and Epstein–Barr virus in nasopharyngeal carcinoma in a low-incidence population. Head Neck 2014, 36, 511–516. [Google Scholar] [CrossRef]
- Singhi, A.D.; Califano, J.; Westra, W.H. High-risk human papillomavirus in nasopharyngeal carcinoma. Head Neck 2012, 34, 213–218. [Google Scholar] [CrossRef]
- Ruuskanen, M.; Irjala, H.; Minn, H.; Vahlberg, T.; Randen-Brady, R.; Hagström, J.; Syrjänen, S.; Leivo, I. Epstein-Barr virus and human papillomaviruses as favorable prognostic factors in nasopharyngeal carcinoma: A nationwide study in Finland. Head Neck 2019, 41, 349–357. [Google Scholar] [CrossRef]
- Ambinder, R.F.; Mann, R.B. Epstein-Barr-encoded RNA in situ hybridization: Diagnostic applications. Hum. Pathol. 1994, 25, 602–605. [Google Scholar] [CrossRef]
- Simon, J.; Schroeder, L.; Ingarfield, K.; Diehl, S.; Werner, J.; Brenner, N.; Liu, Z.; Pawlita, M.; Pring, M.; Butt, J.; et al. Epstein-Barr virus and human papillomavirus serum antibodies define the viral status of nasopharyngeal carcinoma in a low endemic country. Int. J. Cancer 2020, 147, 461–471. [Google Scholar] [CrossRef]
- Henle, G.; Henle, W. Epstein-barr virus-specific IgA serum antibodies as an outstanding feature of nasopharyngeal carcinoma. Int. J. Cancer 1976, 17, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Lin, T.M.; Yang, C.S.; Chiou, J.F.; Tu, S.M.; Chen, T.Y.; Tu, Y.C.; Lin, P.J.; Kawamura, A., Jr.; Hirayama, T. Antibodies to epstein-barr virus capsid antigen and early antigen in nasopharyngeal carcinoma and comparison groups. Am. J. Epidemiol. 1977, 106, 336–339. [Google Scholar] [CrossRef] [PubMed]
- Lanier, A.P.; Bornkamm, G.W.; Henle, W.; Henle, G.; Bender, T.R.; Talbot, M.L.; Dohan, P.H. Association of Epstein-Barr virus with nasopharyngeal carcinoma in alaskan native patients: Serum antibodies and tissue EBNA and DNA. Int. J. Cancer 1981, 28, 301–305. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Huang, Q.; Liu, W.; Liu, Q.; Jia, W.; Chang, E.; Chen, F.; Liu, Z.; Guo, X.; Mo, H.; et al. Establishment of VCA and EBNA1 IgA-based combination by enzyme-linked immunosorbent assay as preferred screening method for nasopharyngeal carcinoma: A two-stage design with a preliminary performance study and a mass screening in southern China. Int. J. Cancer 2012, 131, 406–416. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Cai, Y. Screening of Nasopharyngeal Carcinoma Pharynx—Diagnosis and Treatmented; IntechOpen: London, UK, 2021. [Google Scholar] [CrossRef]
- Coghill, A.E.; Pfeiffer, R.M.; Proietti, C.; Hsu, W.L.; Chien, Y.C.; Lekieffre, L.; Krause, L.; Teng, A.; Pablo, J.; Yu, K.J.; et al. Identification of a Novel, EBV-Based Antibody Risk Stratification Signature for Early Detection of Nasopharyngeal Carcinoma in Taiwan. Clin. Cancer Res. 2018, 24, 1305–1314. [Google Scholar] [CrossRef] [PubMed]
- Waterboer, T.; Sehr, P.; Michael, K.M.; Franceschi, S.; Nieland, J.D.; Joos, T.O.; Templin, M.F.; Pawlita, M. Multiplex human papillomavirus serology based on in situ-purified glutathione s-transferase fusion proteins. Clin. Chem. 2005, 51, 1845–1853. [Google Scholar] [CrossRef]
- Simon, J.; Liu, Z.; Brenner, N.; Yu, K.J.; Hsu, W.L.; Wang, C.P.; Chien, Y.C.; Coghill, A.E.; Chen, C.J.; Butt, J.; et al. Validation of an Epstein-Barr Virus Antibody Risk Stratification Signature for Nasopharyngeal Carcinoma by Use of Multiplex Serology. J. Clin. Microbiol. 2020, 58, e00077-20. [Google Scholar] [CrossRef]
- Liu, Z.; Yu, K.J.; Coghill, A.E.; Brenner, N.; Cao, S.M.; Chen, C.J.; Chen, Y.; Doolan, D.L.; Hsu, W.L.; Labo, N.; et al. Multilaboratory Assessment of Epstein-Barr Virus Serologic Assays: The Case for Standardization. J. Clin. Microbiol. 2019, 57, e01107-19. [Google Scholar] [CrossRef]
- Ness, A.R.; Waylen, A.; Hurley, K.; Jeffreys, M.; Penfold, C.; Pring, M.; Leary, S.D.; Allmark, C.; Toms, S.; Ring, S.; et al. Recruitment, response rates and characteristics of 5511 people enrolled in a prospective clinical cohort study: Head and neck 5000. Clin. Otolaryngol. 2016, 41, 804–809. [Google Scholar] [CrossRef]
- Brenner, N.; Mentzer, A.J.; Butt, J.; Michel, A.; Prager, K.; Brozy, J.; Weißbrich, B.; Aiello, A.E.; Meier, H.C.S.; Breuer, J.; et al. Validation of Multiplex Serology detecting human herpesviruses 1-5. PLoS ONE 2018, 13, e0209379. [Google Scholar] [CrossRef]
- Waterboer, T.; Sehr, P.; Pawlita, M. Suppression of non-specific binding in serological Luminex assays. J. Immunol. Methods 2006, 309, 200–204. [Google Scholar] [CrossRef] [PubMed]
- Vidarsson, G.; Dekkers, G.; Rispens, T. IgG subclasses and allotypes: From structure to effector functions. Front. Immunol. 2014, 5, 520. [Google Scholar] [CrossRef] [PubMed]
- Macpherson, A.J.; McCoy, K.D.; Johansen, F.E.; Brandtzaeg, P. The immune geography of IgA induction and function. Mucosal Immunol. 2008, 1, 11–22. [Google Scholar] [CrossRef]
- Cameron, A.; Bohrhunter, J.L.; Porterfield, C.A.; Mangat, R.; Karasick, M.H.; Pearson, Z.; Angeloni, S.; Pecora, N.D. Simultaneous Measurement of IgM and IgG Antibodies to SARS-CoV-2 Spike, RBD, and Nucleocapsid Multiplexed in a Single Assay on the xMAP INTELLIFLEX DR-SE Flow Analyzer. Microbiol. Spectr. 2022, 10, e0250721. [Google Scholar] [CrossRef] [PubMed]
- Häring, J.; Hassenstein, M.J.; Becker, M.; Ortmann, J.; Junker, D.; Karch, A.; Berger, K.; Tchitchagua, T.; Leschnik, O.; Harries, M.; et al. Borrelia multiplex: A bead-based multiplex assay for the simultaneous detection of Borrelia specific IgG/IgM class antibodies. BMC Infect. Dis. 2022, 22, 859. [Google Scholar] [CrossRef] [PubMed]
- Lam, W.K.J.; King, A.D.; Miller, J.A.; Liu, Z.; Yu, K.J.; Chua, M.L.K.; Ma, B.B.Y.; Chen, M.Y.; Pinsky, B.A.; Lou, P.J.; et al. Recommendations for Epstein-Barr virus-based screening for nasopharyngeal cancer in high- and intermediate-risk regions. J. Natl. Cancer Inst. 2023, 115, 355–364. [Google Scholar] [CrossRef]
- Robbins, H.A.; Ferreiro-Iglesias, A.; Waterboer, T.; Brenner, N.; Nygard, M.; Bender, N.; Schroeder, L.; Hildesheim, A.; Pawlita, M.; D’Souza, G.; et al. Absolute Risk of Oropharyngeal Cancer After an HPV16-E6 Serology Test and Potential Implications for Screening: Results From the Human Papillomavirus Cancer Cohort Consortium. J. Clin. Oncol. 2022, 40, 3613–3622. [Google Scholar] [CrossRef]
- Van Keer, S.; Willhauck-Fleckenstein, M.; Pattyn, J.; Butt, J.; Tjalma, W.A.A.; Van Ostade, X.; Hens, N.; Van Damme, P.; Waterboer, T.; Vorsters, A. First-void urine as a non-invasive liquid biopsy source to detect vaccine-induced human papillomavirus antibodies originating from cervicovaginal secretions. J. Clin. Virol. 2019, 117, 11–18. [Google Scholar] [CrossRef]



| Product | Manufacturer | Product Number |
|---|---|---|
| Directly labeled antibodies | ||
| goat anti-human IgA-PE | Dianova | 109-115-011 |
| goat anti-human IgG-PE | Dianova | 109-115-098 |
| goat anti-human IgA-DyLight405 | Dianova | 109-475-011 |
| goat anti-human IgG-DyLight405 | Dianova | 109-475-098 |
| Biotinylated antibodies | ||
| biotinylated goat anti-human IgG | Dianova | 109-065-098 |
| biotinylated goat anti-human IgA | Dianova | 109-065-011 |
| Biotinylated mouse anti-tag from KT3 hybridoma supernatant [17] | ||
| goat anti-mouse-Cy3 | Dianova | 115-165-146 |
| Dyes | ||
| BV421 Streptavidin Horizon | BD Biosciences | 563259 |
| Streptavidin-R-Phycoerythrin | Moss | SAPE-001 |
| Streptavidin Super Bright 436 Conjugate | eBioscience | 62-4317-82 |
| Antigen | Cut-Off | Sensitivity | Specificity | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Singleplex | BV-Duplex | SB-Duplex | Singleplex | BV-Duplex | SB-Duplex | Singleplex | BV-Duplex | SB-Duplex | |
| BGLF2 IgG | 241 | 251 | 271 | 96.6 | 100 | 100 | 91.7 | 91.7 | 91.7 |
| LF2 IgG | 30 * | 30 * | 31 | 96.6 | 96.6 | 96.6 | 100 | 100 | 100 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schieber, J.; Pring, M.; Ness, A.; Liu, Z.; Hsu, W.-L.; Brenner, N.; Butt, J.; Waterboer, T.; Simon, J. Development of a Duplex Serological Multiplex Assay for the Simultaneous Detection of Epstein-Barr Virus IgA and IgG Antibodies in Nasopharyngeal Carcinoma Patients. Cancers 2023, 15, 2578. https://doi.org/10.3390/cancers15092578
Schieber J, Pring M, Ness A, Liu Z, Hsu W-L, Brenner N, Butt J, Waterboer T, Simon J. Development of a Duplex Serological Multiplex Assay for the Simultaneous Detection of Epstein-Barr Virus IgA and IgG Antibodies in Nasopharyngeal Carcinoma Patients. Cancers. 2023; 15(9):2578. https://doi.org/10.3390/cancers15092578
Chicago/Turabian StyleSchieber, Jennifer, Miranda Pring, Andy Ness, Zhiwei Liu, Wan-Lun Hsu, Nicole Brenner, Julia Butt, Tim Waterboer, and Julia Simon. 2023. "Development of a Duplex Serological Multiplex Assay for the Simultaneous Detection of Epstein-Barr Virus IgA and IgG Antibodies in Nasopharyngeal Carcinoma Patients" Cancers 15, no. 9: 2578. https://doi.org/10.3390/cancers15092578
APA StyleSchieber, J., Pring, M., Ness, A., Liu, Z., Hsu, W.-L., Brenner, N., Butt, J., Waterboer, T., & Simon, J. (2023). Development of a Duplex Serological Multiplex Assay for the Simultaneous Detection of Epstein-Barr Virus IgA and IgG Antibodies in Nasopharyngeal Carcinoma Patients. Cancers, 15(9), 2578. https://doi.org/10.3390/cancers15092578






