Treatment Optimization in Linac-Based SBRT for Localized Prostate Cancer: A Single-Arc versus Dual-Arc Plan Comparison
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
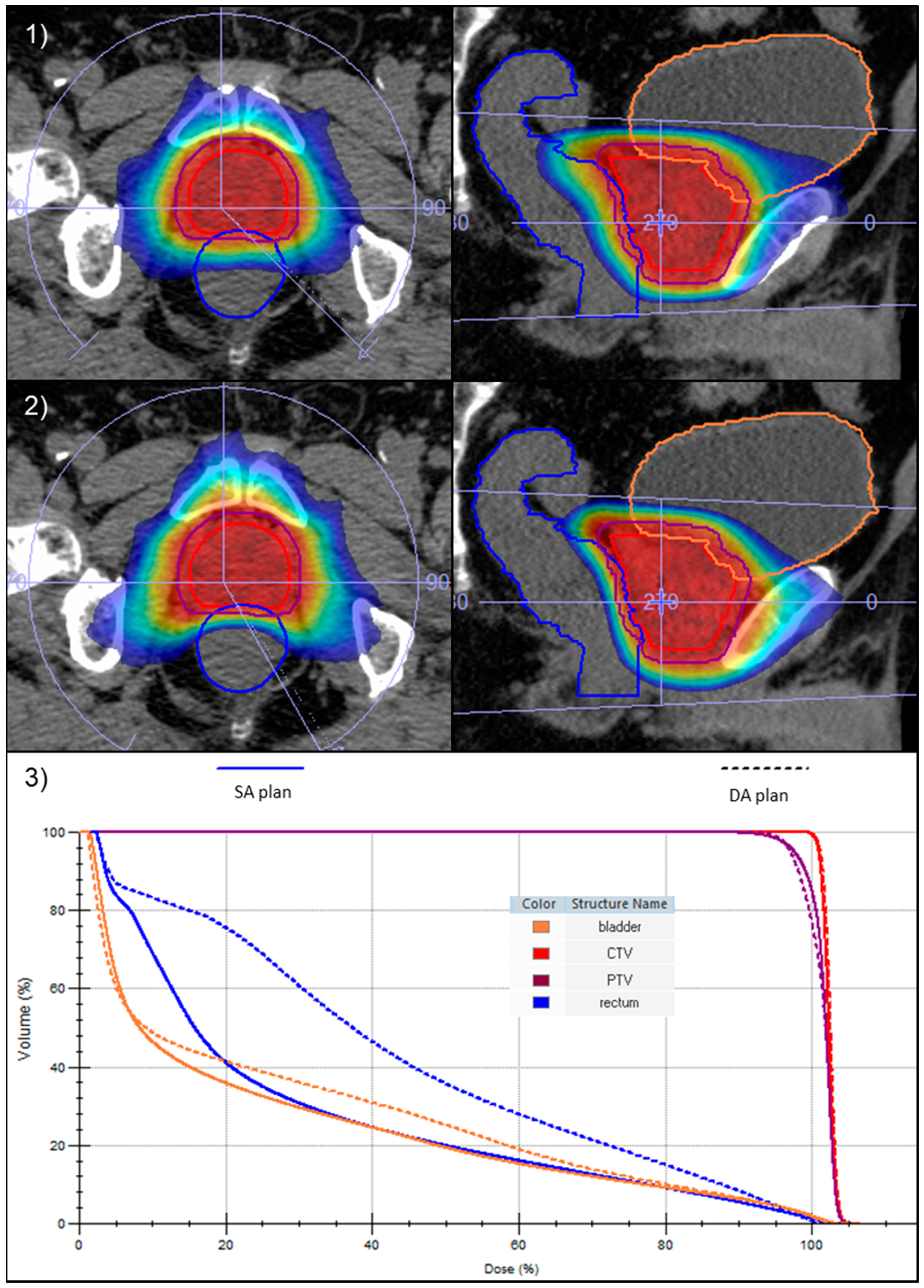
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Arcangeli, S.; Scorsetti, M.; Alongi, F. Will SBRT replace conventional radiotherapy in patients with low-intermediate risk prostate cancer? A review. Crit. Rev. Oncol. Hematol. 2012, 84, 101–108. [Google Scholar] [CrossRef]
- Morgan, S.C.; Hoffman, K.; Loblaw, D.A.; Buyyounouski, M.K.; Patton, C.; Barocas, D.; Bentzen, S.; Chang, M.; Efstathiou, J.; Greany, P.; et al. Hypofractionated Radiation Therapy for Localized Prostate Cancer: Executive Summary of an ASTRO, ASCO, and AUA Evidence-Based Guideline. Pract. Radiat. Oncol. 2018, 8, 354–360. [Google Scholar] [CrossRef] [PubMed]
- Vogelius, I.R.; Bentzen, S.M. Diminishing Returns from Ultrahypofractionated Radiation Therapy for Prostate Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2020, 107, 299–304. [Google Scholar] [CrossRef] [PubMed]
- King, C.R.; Freeman, D.; Kaplan, I.; Fuller, D.; Bolzicco, G.; Collins, S.; Meier, R.; Wang, J.; Kupelian, P.; Steinberg, M.; et al. Stereotactic body radiotherapy for localized prostate cancer: Pooled analysis from a multi-institutional consortium of prospective phase II trials. Radiother. Oncol. 2013, 109, 217–221. [Google Scholar] [CrossRef] [PubMed]
- Katz, A.J.; Kang, J. Stereotactic body radiotherapy as treatment for organ confined low- and intermediate-risk prostate carcinoma, a 7-year study. Front. Oncol. 2014, 4, 240. [Google Scholar] [CrossRef]
- Alayed, Y.; Cheung, P.; Pang, G.; Mamedov, A.; D’Alimonte, L.; Deabreu, A.; Commisso, K.; Commisso, A.; Zhang, L.; Quon, H.C.; et al. Dose escalation for prostate stereotactic ablative radiotherapy (SABR): Late outcomes from two prospective clinical trials. Radiother. Oncol. 2018, 127, 213–218. [Google Scholar] [CrossRef]
- Kishan, A.U.; Dang, A.; Katz, A.J.; Mantz, C.A.; Collins, S.P.; Aghdam, N.; Chu, F.I.; Kaplan, I.D.; Appelbaum, L.; Fuller, D.B.; et al. Long-term Outcomes of Stereotactic Body Radiotherapy for Low-Risk and Intermediate-Risk Prostate Cancer. JAMA Netw. Open 2019, 2, e188006. [Google Scholar] [CrossRef]
- Jackson, W.C.; Silva, J.; Hartman, H.E.; Dess, R.T.; Kishan, A.U.; Beeler, W.H.; Gharzai, L.A.; Jaworski, E.M.; Mehra, R.; Hearn, J.W.D.; et al. Stereotactic Body Radiation Therapy for Localized Prostate Cancer: A Systematic Review and Meta-Analysis of Over 6000 Patients Treated on Prospective Studies. Int. J. Radiat. Oncol. Biol. Phys. 2019, 104, 778–789. [Google Scholar] [CrossRef]
- Widmark, A.; Gunnlaugsson, A.; Beckman, L.; Thellenberg-Karlsson, C.; Hoyer, M.; Lagerlund, M.; Kindblom, J.; Ginman, C.; Johansson, B.; Björnlinger, K.; et al. Ultra-hypofractionated versus conventionally fractionated radiotherapy for prostate cancer: 5-year outcomes of the HYPO-RT-PC randomised, non-inferiority, phase 3 trial. Lancet 2019, 394, 385–395. [Google Scholar] [CrossRef]
- Fransson, P.; Nilsson, P.; Gunnlaugsson, A.; Beckman, L.; Tavelin, B.; Norman, D.; Thellenberg-Karlsson, C.; Hoyer, M.; Lagerlund, M.; Kindblom, J.; et al. Ultra-hypofractionated versus conventionally fractionated radiotherapy for prostate cancer (HYPO-RT-PC): Patient-reported quality-of-life outcomes of a randomised, controlled, non-inferiority, phase 3 trial. Lancet Oncol. 2021, 22, 235–245. [Google Scholar] [CrossRef]
- Brand, D.H.; Tree, A.C.; Ostler, P.; van der Voet, H.; Loblaw, A.; Chu, W.; Ford, D.; Tolan, S.; Jain, S.; Martin, A.; et al. Intensity-modulated fractionated radiotherapy versus stereotactic body radiotherapy for prostate cancer (PACE-B): Acute toxicity findings from an international, randomised, open-label, phase 3, non-inferiority trial. Lancet Oncol. 2019, 20, 1531–1543. [Google Scholar] [CrossRef] [PubMed]
- Tree, A.C.; Ostler, P.; van der Voet, H.; Chu, W.; Loblaw, A.; Ford, D.; Tolan, S.; Jain, S.; Martin, A.; Staffurth, J.; et al. Intensity-modulated radiotherapy versus stereotactic body radiotherapy for prostate cancer (PACE-B): 2-year toxicity results from an open-label, randomised, phase 3, non-inferiority trial. Lancet Oncol. 2022, 23, 1308–1320. [Google Scholar] [CrossRef] [PubMed]
- Kishan, A.U.; Ma, T.M.; Lamb, J.M.; Casado, M.; Wilhalme, H.; Low, D.A.; Sheng, K.; Sharma, S.; Nickols, N.G.; Pham, J.; et al. Magnetic Resonance Imaging-Guided vs Computed Tomography-Guided Stereotactic Body Radiotherapy for Prostate Cancer: The MIRAGE Randomized Clinical Trial. JAMA Oncol. 2023, 9, 365–373. [Google Scholar] [CrossRef] [PubMed]
- Langen, K.M.; Jones, D.T. Organ motion and its management. Int. J. Radiat. Oncol. Biol. Phys. 2001, 50, 265–278. [Google Scholar] [CrossRef] [PubMed]
- Kron, T.; Thomas, J.; Fox, C.; Thompson, A.; Owen, R.; Herschtal, A.; Haworth, A.; Tai, K.H.; Foroudi, F. Intra-fraction prostate displacement in radiotherapy estimated from pre- and post-treatment imaging of patients with implanted fiducial markers. Radiother. Oncol. 2010, 95, 191–197. [Google Scholar] [CrossRef]
- Ballhausen, H.; Li, M.; Hegemann, N.S.; Ganswindt, U.; Belka, C. Intra-fraction motion of the prostate is a random walk. Phys. Med. Biol. 2015, 60, 549–563. [Google Scholar] [CrossRef]
- Legge, K.; Nguyen, D.; Ng, J.A.; Wilton, L.; Richardson, M.; Booth, J.; Keall, P.; O’Connor, D.J.; Greer, P.; Martin, J. Real-time intrafraction prostate motion during linac based stereotactic radiotherapy with rectal displacement. J. Appl. Clin. Med. Phys. 2017, 18, 130–136. [Google Scholar] [CrossRef]
- Gorovets, D.; Burleson, S.; Jacobs, L.; Ravindranath, B.; Tierney, K.; Kollmeier, M.; McBride, S.; Happersett, L.; Hunt, M.; Zelefsky, M. Prostate SBRT With Intrafraction Motion Management Using a Novel Linear Accelerator-Based MV-kV Imaging Method. Pract. Radiat. Oncol. 2020, 10, e388–e396. [Google Scholar] [CrossRef]
- Panizza, D.; Faccenda, V.; Lucchini, R.; Daniotti, M.C.; Trivellato, S.; Caricato, P.; Pisoni, V.; De Ponti, E.; Arcangeli, S. Intrafraction Prostate Motion Management During Dose-Escalated Linac-Based Stereotactic Body Radiation Therapy. Front. Oncol. 2022, 12, 883725. [Google Scholar] [CrossRef]
- Li, H.S.; Chetty, I.J.; Enke, C.A.; Foster, R.D.; Willoughby, T.R.; Kupellian, P.A.; Solberg, T.D. Dosimetric consequences of intrafraction prostate motion. Int. J. Radiat. Oncol. Biol. Phys. 2008, 71, 801–812. [Google Scholar] [CrossRef]
- Langen, K.M.; Lu, W.; Ngwa, W.; Willoughby, T.R.; Chauhan, B.; Meeks, S.L.; Kupelian, P.A.; Olivera, G. Correlation between dosimetric effect and intrafraction motion during prostate treatments delivered with helical tomotherapy. Phys. Med. Biol. 2008, 53, 7073–7086. [Google Scholar] [CrossRef]
- Adamson, J.; Wu, Q.; Yan, D. Dosimetric effect of intrafraction motion and residual setup error for hypofractionated prostate intensity-modulated radiotherapy with online cone beam computed tomography image guidance. Int. J. Radiat. Oncol. Biol. Phys. 2011, 80, 453–461. [Google Scholar] [CrossRef] [PubMed]
- van de Water, S.; Valli, L.; Aluwini, S.; Lanconelli, N.; Heijmen, B.; Hoogeman, M. Intrafraction prostate translations and rotations during hypofractionated robotic radiation surgery: Dosimetric impact of correction strategies and margins. Int. J. Radiat. Oncol. Biol. Phys. 2014, 88, 1154–1160. [Google Scholar] [CrossRef] [PubMed]
- Azcona, J.D.; Xing, L.; Chen, X.; Bush, K.; Li, R. Assessing the dosimetric impact of real-time prostate motion during volumetric modulated arc therapy. Int. J. Radiat. Oncol. Biol. Phys. 2014, 88, 1167–1174. [Google Scholar] [CrossRef] [PubMed]
- Vanhanen, A.; Poulsen, P.; Kapanen, M. Dosimetric effect of intrafraction motion and different localization strategies in prostate SBRT. Phys. Med. 2020, 75, 58–68. [Google Scholar] [CrossRef]
- Faccenda, V.; Panizza, D.; Daniotti, M.C.; Pellegrini, R.; Trivellato, S.; Caricato, P.; Lucchini, R.; De Ponti, E.; Arcangeli, S. Dosimetric Impact of Intrafraction Prostate Motion and Interfraction Anatomical Changes in Dose-Escalated Linac-Based SBRT. Cancers 2023, 15, 1153. [Google Scholar] [CrossRef] [PubMed]
- McNeice, J.M.; Sanilkumar, N.; Alexander, S.E.; Talbot, J.; Tree, A.C.; McNair, H.A. Prostate stereotactic body radiotherapy: Quantifying intra-fraction motion and calculating margins using the new BIR geometric uncertainties in daily online IGRT recommendations. Br. J. Radiol. 2023, 96, 20220852. [Google Scholar] [CrossRef]
- Benedek, H.; Lerner, M.; Nilsson, P.; Knöös, T.; Gunnlaugsson, A.; Ceberg, C. The effect of prostate motion during hypofractionated radiotherapy can be reduced by using flattening filter free beams. Phys. Imaging Radiat. Oncol. 2018, 6, 66–70. [Google Scholar] [CrossRef]
- Zelefsky, M.J.; Kollmeier, M.; McBride, S.; Varghese, M.; Mychalczak, B.; Gewanter, R.; Garg, M.K.; Happersett, L.; Goldman, D.A.; Pei, I.; et al. Five-Year Outcomes of a Phase 1 Dose-Escalation Study Using Stereotactic Body Radiosurgery for Patients With Low-Risk and Intermediate-Risk Prostate Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2019, 104, 42–49. [Google Scholar] [CrossRef]
- Lukka, H.R.; Deshmukh, S.; Bruner, D.W.; Bahary, J.P.; Lawton, C.A.F.; Efstathiou, J.A.; Kudchadker, R.J.; Ponsky, L.E.; Seaward, S.A.; Dayes, I.S.; et al. Five-Year Patient-Reported Outcomes in NRG Oncology RTOG 0938, Evaluating Two Ultrahypofractionated Regimens for Prostate Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2023, 116, 770–778. [Google Scholar] [CrossRef]
- Ghadjar, P.; Zelefsky, M.J.; Spratt, D.E.; Munck af Rosenschöld, P.; Oh, J.H.; Hunt, M.; Kollmeier, M.; Happersett, L.; Yorke, E.; Deasy, J.O.; et al. Impact of dose to the bladder trigone on long-term urinary function after high-dose intensity modulated radiation therapy for localized prostate cancer. Int. J. Radiat. Oncol. Biol. Phys. 2014, 88, 339–344. [Google Scholar] [CrossRef] [PubMed]
- Schaake, W.; van der Schaaf, A.; van Dijk, L.V.; Bongaerts, A.H.; van den Bergh, A.C.; Langendijk, J.A. Normal tissue complication probability (NTCP) models for late rectal bleeding, stool frequency and fecal incontinence after radiotherapy in prostate cancer patients. Radiother. Oncol. 2016, 119, 381–387. [Google Scholar] [CrossRef] [PubMed]
- Neilsen, B.K.; Ma, T.M.; Akingbemi, W.O.; Neylon, J.; Casado, M.; Sharma, S.; Sheng, K.; Ruan, D.; Low, D.A.; Yang, Y.; et al. Impact of Interfractional Bladder and Trigone Displacement and Deformation on Radiation Exposure and Subsequent Acute Genitourinary Toxicity: A Post-Hoc Analysis of Patients Treated with MRI-guided Prostate Stereotactic Body Radiotherapy in a Phase III Randomized Trial. Int. J. Radiat. Oncol. Biol. Phys. 2023. [Google Scholar] [CrossRef]
- Kang, S.W.; Chung, J.B.; Kim, J.S.; Kim, I.A.; Eom, K.Y.; Song, C.; Lee, J.W.; Kim, J.Y.; Suh, T.S. Optimal planning strategy among various arc arrangements for prostate stereotactic body radiotherapy with volumetric modulated arc therapy technique. Radiol. Oncol. 2017, 51, 112–120. [Google Scholar] [CrossRef] [PubMed]
- Leeman, J.E.; Chen, Y.H.; Catalano, P.; Bredfeldt, J.; King, M.; Mouw, K.W.; D’Amico, A.V.; Orio, P.; Nguyen, P.L.; Martin, N. Radiation Dose to the Intraprostatic Urethra Correlates Strongly with Urinary Toxicity After Prostate Stereotactic Body Radiation Therapy: A Combined Analysis of 23 Prospective Clinical Trials. Int. J. Radiat. Oncol. Biol. Phys. 2022, 112, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Le Guevelou, J.; Bosetti, D.G.; Castronovo, F.; Angrisani, A.; de Crevoisier, R.; Zilli, T. State of the art and future challenges of urethra-sparing stereotactic body radiotherapy for prostate cancer: A systematic review of literature. World J. Urol. 2023, 41, 3287–3299. [Google Scholar] [CrossRef]
- Guckenberger, M.; Richter, A.; Krieger, T.; Wilbert, J.; Baier, K.; Flentje, M. Is a single arc sufficient in volumetric-modulated arc therapy (VMAT) for complex-shaped target volumes? Radiother. Oncol. 2009, 93, 259–265. [Google Scholar] [CrossRef]
- Varnava, M.; Sumida, I.; Oda, M.; Kurosu, K.; Isohashi, F.; Seo, Y.; Otani, K.; Ogawa, K. Dosimetric comparison between volumetric modulated arc therapy planning techniques for prostate cancer in the presence of intrafractional organ deformation. J. Radiat. Res. 2021, 62, 309–318. [Google Scholar] [CrossRef]
- Nguyen, B.T.; Hornby, C.; Kron, T.; Cramb, J.; Rolfo, A.; Pham, D.; Haworth, A.; Tai, K.H.; Foroudi, F. Optimising the dosimetric quality and efficiency of post-prostatectomy radiotherapy: A planning study comparing the performance of volumetric-modulated arc therapy (VMAT) with an optimised seven-field intensity-modulated radiotherapy (IMRT) technique. J. Med. Imaging Radiat. Oncol. 2012, 56, 211–219. [Google Scholar] [CrossRef]
- Sasaki, M.; Nakaguuchi, Y.; Kamomae, T.; Tsuzuki, A.; Kobuchi, S.; Kuwahara, K.; Ueda, S.; Endo, Y.; Ikushima, H. Analysis of prostate intensity- and volumetric-modulated arc radiation therapy planning quality with PlanIQ™. J. Appl. Clin. Med. Phys. 2021, 22, 132–142. [Google Scholar] [CrossRef]
- Kong, V.; Dang, J.; Wan, V.; Rosewall, T. The dosimetric underpinning of bladder filling criteria for prostate image-guided volumetric modulated arc therapy. Br. J. Radiol. 2023, 96, 20230020. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Kim, D.W.; Joo, J.H.; Ki, Y.; Kim, W.; Park, D.; Nam, J.; Kim, D.H.; Jeon, H. Minimization of Treatment Time Using Partial-Arc Volumetric Modulated Arc Therapy with Bladder Filling Protocol for Prostate Cancer. Prog. Med. Phys. 2022, 33, 101–107. [Google Scholar] [CrossRef]


| 36.25 Gy/5fx | 42.7 Gy/7fx | |
|---|---|---|
| PTV | D95% ≥ 95% | D95% ≥ 95% |
| D1cc < 105% | D1cc < 105% | |
| Rectum | D1cc < 38.06 Gy | D1cc < 44.84 Gy |
| D5% < 36.25 Gy | D5% < 42.7 Gy | |
| D10% < 32.625 Gy | D10% < 38.43 Gy | |
| D20% < 29 Gy | D20% < 34.16 Gy | |
| D50% < 18.1 Gy | D50% < 20.3 Gy | |
| Bladder | D1cc < 38.06 Gy | D1cc < 44.84 Gy |
| D10% < 32.625 Gy | D10% < 37.3 Gy | |
| D40% < 18.1 Gy | D40% < 20.3 Gy | |
| Femoral Heads | D5% < 14.5 Gy | D5% < 16.1 Gy |
| Small Bowel | D0.1cc < 35 Gy | D0.1cc < 40.1 Gy |
| Metrics | DA Plans | SA Plans | Relative Dose Difference | |
|---|---|---|---|---|
| Mean [Range] | Mean [Range] | Mean [Range] | ||
| PTV | D95% | 96.5% [88.1–98.7] | 96.7% [89.6–99.5] | +0.3% [−1.6–2.4] |
| Dmean | 101.1% [99.8–102.5] | 101.4% [100.4–102.2] | +0.3% [−0.4–1.8] | |
| D2% | 103.9% [102.0–105.3] | 104.1% [103.3–104.6] | +0.2% [−0.7–1.7] |
| Metrics | DA Plans | SA Plans | Relative Dose Difference | |
|---|---|---|---|---|
| Mean [Range] | Mean [Range] | Mean [Range] | ||
| Rectum | Dmean | 15.8 Gy [10.4–21.7] | 12.0 Gy [8.7–17.5] | −23.2% [−41.6–−4.3] |
| D1cc | 38.0 Gy [33.1–43.0] | 38.5 Gy [31.2–43.7] | +1.4% [−5.8–8.0] | |
| D5% | 35.9 Gy [30.9–42.1] | 35.6 Gy [26.4–42.1] | −0.9% [−14.5–8.6] | |
| D10% | 32.7 Gy [26.3–40.3] | 30.6 Gy [19.3–39.4] | −6.4% [−26.8–5.0] | |
| D20% | 26.6 Gy [18.1–36.2] | 21.4 Gy [12.5–33.1] | −19.4% [−42.4–−0.5] | |
| D50% | 13.1 Gy [7.0–22.1] | 7.5 Gy [4.0–13.4] | −42.2% [−68.7–−7.7] | |
| Rectum wall | D0.035cc | 39.9 Gy [36.1–43.9] | 40.7 Gy [36.9–44.7] | +2.1% [−0.9–5.6] |
| Rectum mucosa | D0.035cc | 37.3 Gy [33.1–42.6] | 37.8 Gy [31.0–44.0] | +1.5% [−6.4–11.4] |
| Bladder | Dmean | 13.0 Gy [5.0–22.0] | 11.8 Gy [4.7–18.1] | −8.5% [−20.5–2.8] |
| D1cc | 40.1 Gy [36.4–43.8] | 40.1 Gy [36.0–44.1] | 0.0% [−3.4–3.0] | |
| D10% | 33.1 Gy [19.0–41.6] | 31.7 Gy [16.0–39.1] | −4.3% [−19.9–6.3] | |
| D40% | 12.5 Gy [1.1–21.7] | 10.7 Gy [1.3–20.7] | −12.9% [−48.2–37.2] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Panizza, D.; Faccenda, V.; Arcangeli, S.; De Ponti, E. Treatment Optimization in Linac-Based SBRT for Localized Prostate Cancer: A Single-Arc versus Dual-Arc Plan Comparison. Cancers 2024, 16, 13. https://doi.org/10.3390/cancers16010013
Panizza D, Faccenda V, Arcangeli S, De Ponti E. Treatment Optimization in Linac-Based SBRT for Localized Prostate Cancer: A Single-Arc versus Dual-Arc Plan Comparison. Cancers. 2024; 16(1):13. https://doi.org/10.3390/cancers16010013
Chicago/Turabian StylePanizza, Denis, Valeria Faccenda, Stefano Arcangeli, and Elena De Ponti. 2024. "Treatment Optimization in Linac-Based SBRT for Localized Prostate Cancer: A Single-Arc versus Dual-Arc Plan Comparison" Cancers 16, no. 1: 13. https://doi.org/10.3390/cancers16010013
APA StylePanizza, D., Faccenda, V., Arcangeli, S., & De Ponti, E. (2024). Treatment Optimization in Linac-Based SBRT for Localized Prostate Cancer: A Single-Arc versus Dual-Arc Plan Comparison. Cancers, 16(1), 13. https://doi.org/10.3390/cancers16010013








