Digging into the NGS Information from a Large-Scale South European Population with Metastatic/Unresectable Pancreatic Ductal Adenocarcinoma: A Real-World Genomic Depiction
Abstract
:Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Patient Samples
2.2. Tissue Selection and Nucleic Acid Isolation
2.3. Next Generation Sequencing (NGS)—Tumor Mutational Burden (TMB) and Microsatellite Instability (MSI) Analysis
2.4. Classification of Variants
2.5. PD-L1 Expression by Immunohistochemistry
2.6. Statistical Analysis
3. Results
3.1. Characteristics of Study Population
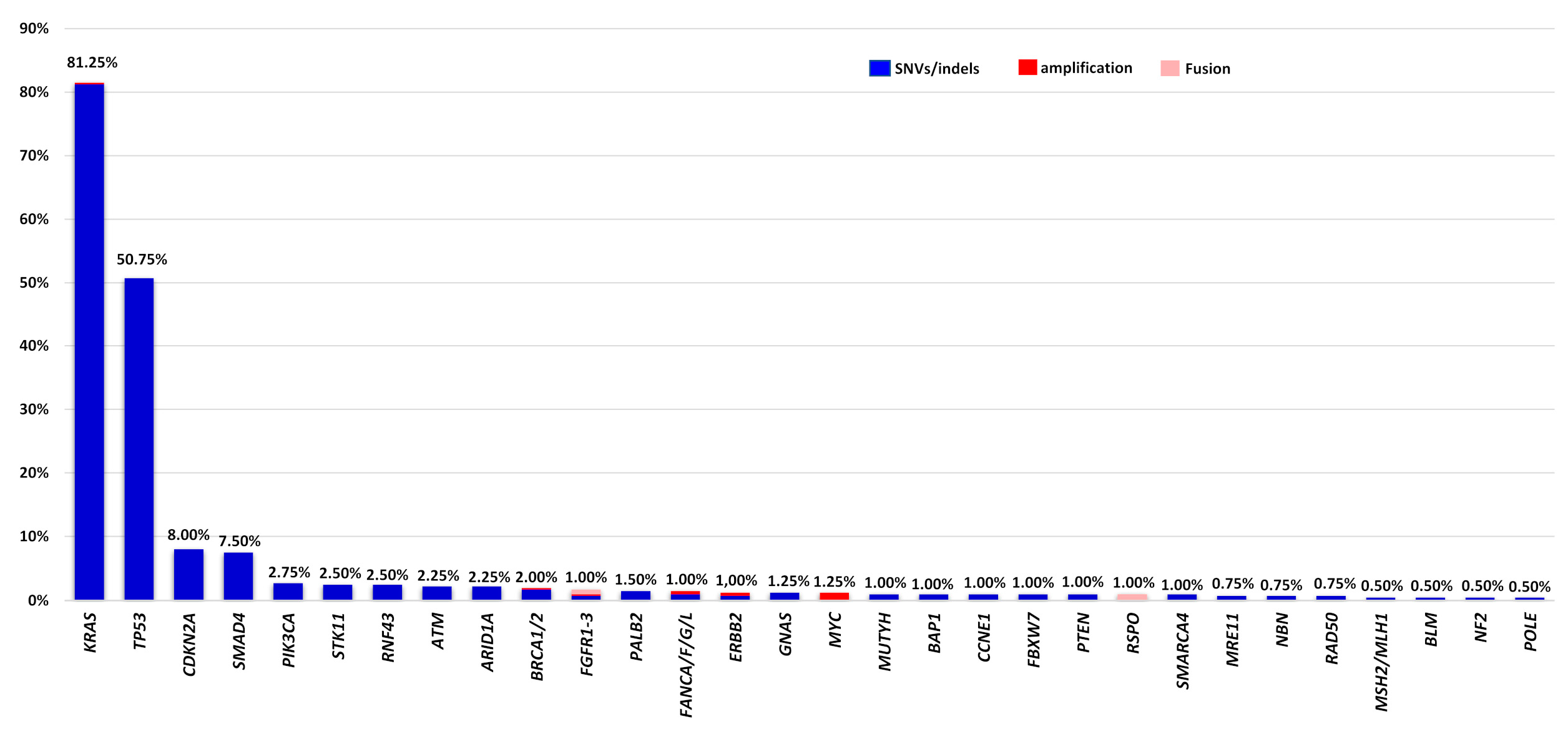
3.2. Genomic Profile of Somatic Alterations in Patients with Metastatic/Unresectable PDAC
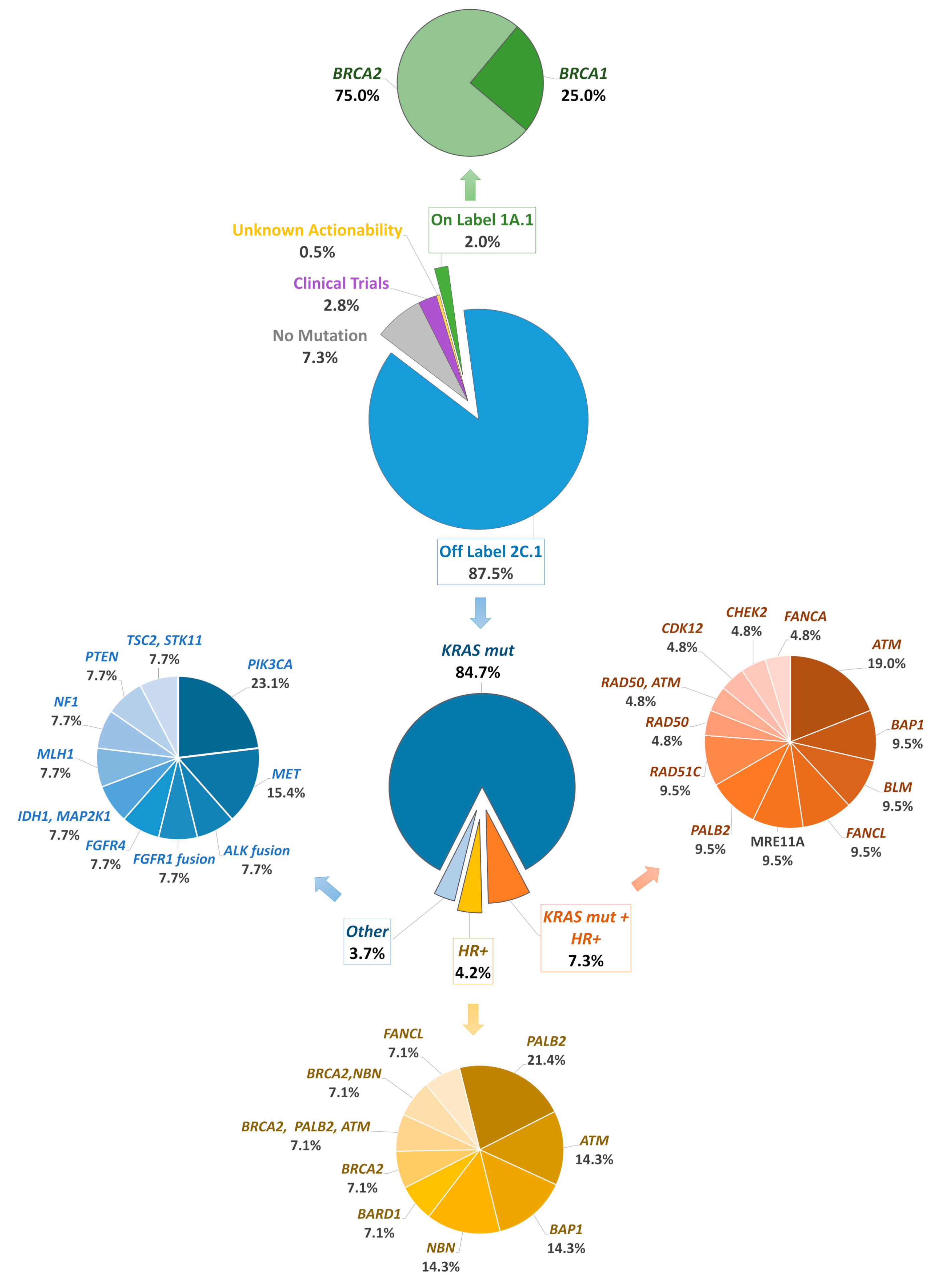
3.3. Distribution of HRR Gene Alterations in Patients with Metastatic/Unresectable PDAC
3.4. Analysis of Immunotherapeutic Biomarkers in PDAC—Incorporation of NGS Information in Clinical Decision
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- 2022-Cancer-Facts-and-Figures. Available online: https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/2023-cancer-facts-figures.html (accessed on 27 May 2023).
- Ghosn, M.; Ibrahim, T.; Assi, T.; El Rassy, E.; Kourie, H.R.; Kattan, J. Dilemma of First Line Regimens in Metastatic Pancreatic Adenocarcinoma. World J. Gastroenterol. 2016, 22, 10124–10130. [Google Scholar] [CrossRef]
- Evan, T.; Wang, V.M.-Y.; Behrens, A. The Roles of Intratumour Heterogeneity in the Biology and Treatment of Pancreatic Ductal Adenocarcinoma. Oncogene 2022, 41, 4686–4695. [Google Scholar] [CrossRef] [PubMed]
- Collisson, E.A.; Bailey, P.; Chang, D.K.; Biankin, A.V. Molecular Subtypes of Pancreatic Cancer. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 207–220. [Google Scholar] [CrossRef]
- Cancer Genome Atlas Research Network. Electronic address: Andrew_aguirre@dfci.harvard.edu; Cancer Genome Atlas Research Network Integrated Genomic Characterization of Pancreatic Ductal Adenocarcinoma. Cancer Cell 2017, 32, 185–203.e13. [Google Scholar] [CrossRef] [PubMed]
- Thompson, E.D.; Roberts, N.J.; Wood, L.D.; Eshleman, J.R.; Goggins, M.G.; Kern, S.E.; Klein, A.P.; Hruban, R.H. The Genetics of Ductal Adenocarcinoma of the Pancreas in the Year 2020: Dramatic Progress, but Far to Go. Mod. Pathol. 2020, 33, 2544–2563. [Google Scholar] [CrossRef] [PubMed]
- Mosele, F.; Remon, J.; Mateo, J.; Westphalen, C.B.; Barlesi, F.; Lolkema, M.P.; Normanno, N.; Scarpa, A.; Robson, M.; Meric-Bernstam, F.; et al. Recommendations for the Use of Next-Generation Sequencing (NGS) for Patients with Metastatic Cancers: A Report from the ESMO Precision Medicine Working Group. Ann. Oncol. 2020, 31, 1491–1505. [Google Scholar] [CrossRef] [PubMed]
- Chakravarty, D.; Johnson, A.; Sklar, J.; Lindeman, N.I.; Moore, K.; Ganesan, S.; Lovly, C.M.; Perlmutter, J.; Gray, S.W.; Hwang, J.; et al. Somatic Genomic Testing in Patients With Metastatic or Advanced Cancer: ASCO Provisional Clinical Opinion. J. Clin. Oncol. 2022, 40, 1231–1258. [Google Scholar] [CrossRef] [PubMed]
- Pishvaian, M.J.; Blais, E.M.; Brody, J.R.; Lyons, E.; DeArbeloa, P.; Hendifar, A.; Mikhail, S.; Chung, V.; Sahai, V.; Sohal, D.P.S.; et al. Overall Survival in Patients with Pancreatic Cancer Receiving Matched Therapies Following Molecular Profiling: A Retrospective Analysis of the Know Your Tumor Registry Trial. Lancet Oncol. 2020, 21, 508–518. [Google Scholar] [CrossRef] [PubMed]
- Biankin, A.V.; Waddell, N.; Kassahn, K.S.; Gingras, M.-C.; Muthuswamy, L.B.; Johns, A.L.; Miller, D.K.; Wilson, P.J.; Patch, A.-M.; Wu, J.; et al. Pancreatic Cancer Genomes Reveal Aberrations in Axon Guidance Pathway Genes. Nature 2012, 491, 399–405. [Google Scholar] [CrossRef]
- Lundy, J.; McKay, O.; Croagh, D.; Ganju, V. Exceptional Response to Olaparib and Pembrolizumab for Pancreatic Adenocarcinoma With Germline BRCA1 Mutation and High Tumor Mutation Burden: Case Report and Literature Review. JCO Precis. Oncol. 2022, 6, e2100437. [Google Scholar] [CrossRef]
- Chantrill, L.A.; Nagrial, A.M.; Watson, C.; Johns, A.L.; Martyn-Smith, M.; Simpson, S.; Mead, S.; Jones, M.D.; Samra, J.S.; Gill, A.J.; et al. Precision Medicine for Advanced Pancreas Cancer: The Individualized Molecular Pancreatic Cancer Therapy (IMPaCT) Trial. Clin. Cancer Res. 2015, 21, 2029–2037. [Google Scholar] [CrossRef]
- Qian, Z.R.; Rubinson, D.A.; Nowak, J.A.; Morales-Oyarvide, V.; Dunne, R.F.; Kozak, M.M.; Welch, M.W.; Brais, L.K.; Da Silva, A.; Li, T.; et al. Association of Alterations in Main Driver Genes with Outcomes of Patients With Resected Pancreatic Ductal Adenocarcinoma. JAMA Oncol. 2018, 4, e173420. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Mao, T.; Zhang, B.; Xu, H.; Cui, J.; Jiao, F.; Chen, D.; Wang, Y.; Hu, J.; Xia, Q.; et al. Characterization of the Genomic Landscape in Large-Scale Chinese Patients with Pancreatic Cancer. EBioMedicine 2022, 77, 103897. [Google Scholar] [CrossRef] [PubMed]
- Hu, H.; Zhu, Y.; Pu, N.; Burkhart, R.A.; Burns, W.; Laheru, D.; Zheng, L.; He, J.; Goggins, M.G.; Yu, J. Association of Germline Variants in Human DNA Damage Repair Genes and Response to Adjuvant Chemotherapy in Resected Pancreatic Ductal Adenocarcinoma. J. Am. Coll. Surg. 2020, 231, 527–535.e14. [Google Scholar] [CrossRef] [PubMed]
- Yadav, S.; Kasi, P.M.; Bamlet, W.R.; Ho, T.P.; Polley, E.C.; Hu, C.; Hart, S.N.; Rabe, K.G.; Boddicker, N.J.; Gnanaolivu, R.D.; et al. Effect of Germline Mutations in Homologous Recombination Repair Genes on Overall Survival of Patients with Pancreatic Adenocarcinoma. Clin. Cancer Res. 2020, 26, 6505–6512. [Google Scholar] [CrossRef] [PubMed]
- Pestana, R.C.; Sen, S.; Hobbs, B.P.; Hong, D.S. Histology-Agnostic Drug Development—Considering Issues beyond the Tissue. Nat. Rev. Clin. Oncol. 2020, 17, 555–568. [Google Scholar] [CrossRef] [PubMed]
- Cocco, E.; Scaltriti, M.; Drilon, A. NTRK Fusion-Positive Cancers and TRK Inhibitor Therapy. Nat. Rev. Clin. Oncol. 2018, 15, 731–747. [Google Scholar] [CrossRef] [PubMed]
- Drilon, A.; Siena, S.; Ou, S.-H.I.; Patel, M.; Ahn, M.J.; Lee, J.; Bauer, T.M.; Farago, A.F.; Wheler, J.J.; Liu, S.V.; et al. Safety and Antitumor Activity of the Multitargeted Pan-TRK, ROS1, and ALK Inhibitor Entrectinib: Combined Results from Two Phase I Trials (ALKA-372-001 and STARTRK-1). Cancer Discov. 2017, 7, 400–409. [Google Scholar] [CrossRef]
- Drilon, A.; Laetsch, T.W.; Kummar, S.; DuBois, S.G.; Lassen, U.N.; Demetri, G.D.; Nathenson, M.; Doebele, R.C.; Farago, A.F.; Pappo, A.S.; et al. Efficacy of Larotrectinib in TRK Fusion-Positive Cancers in Adults and Children. N. Engl. J. Med. 2018, 378, 731–739. [Google Scholar] [CrossRef]
- Arbour, K.C.; Lito, P. Expanding the Arsenal of Clinically Active KRAS G12C Inhibitors. J. Clin. Oncol. 2022, 40, 2609–2611. [Google Scholar] [CrossRef]
- Kazi, A.; Ranjan, A.; Kumar, M.V.V.; Agianian, B.; Garcia Chavez, M.; Vudatha, V.; Wang, R.; Vangipurapu, R.; Chen, L.; Kennedy, P.; et al. Discovery of KRB-456, a KRAS G12D Switch-I/II Allosteric Pocket Binder That Inhibits the Growth of Pancreatic Cancer Patient-Derived Tumors. Cancer Res. Commun. 2023. [Google Scholar] [CrossRef] [PubMed]
- Wattenberg, M.M.; Asch, D.; Yu, S.; O’Dwyer, P.J.; Domchek, S.M.; Nathanson, K.L.; Rosen, M.A.; Beatty, G.L.; Siegelman, E.S.; Reiss, K.A. Platinum Response Characteristics of Patients with Pancreatic Ductal Adenocarcinoma and a Germline BRCA1, BRCA2 or PALB2 Mutation. Br. J. Cancer 2020, 122, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Golan, T.; Hammel, P.; Reni, M.; Van Cutsem, E.; Macarulla, T.; Hall, M.J.; Park, J.-O.; Hochhauser, D.; Arnold, D.; Oh, D.-Y.; et al. Maintenance Olaparib for Germline BRCA-Mutated Metastatic Pancreatic Cancer. N. Engl. J. Med. 2019, 381, 317–327. [Google Scholar] [CrossRef] [PubMed]
- Gouda, M.A.; Nelson, B.E.; Buschhorn, L.; Wahida, A.; Subbiah, V. Tumor-Agnostic Precision Medicine from the AACR GENIE Database: Clinical Implications. Clin. Cancer Res. 2023, 29, 2753–2760. [Google Scholar] [CrossRef] [PubMed]
- Signorelli, D.; Giannatempo, P.; Grazia, G.; Aiello, M.M.; Bertolini, F.; Mirabile, A.; Buti, S.; Vasile, E.; Scotti, V.; Pisapia, P.; et al. Patients Selection for Immunotherapy in Solid Tumors: Overcome the Naïve Vision of a Single Biomarker. Biomed. Res. Int. 2019, 2019, 9056417. [Google Scholar] [CrossRef] [PubMed]
- Marabelle, A.; Fakih, M.; Lopez, J.; Shah, M.; Shapira-Frommer, R.; Nakagawa, K.; Chung, H.C.; Kindler, H.L.; Lopez-Martin, J.A.; Miller, W.H.; et al. Association of Tumour Mutational Burden with Outcomes in Patients with Advanced Solid Tumours Treated with Pembrolizumab: Prospective Biomarker Analysis of the Multicohort, Open-Label, Phase 2 KEYNOTE-158 Study. Lancet Oncol. 2020, 21, 1353–1365. [Google Scholar] [CrossRef] [PubMed]
- Westphalen, C.B.; Fine, A.D.; André, F.; Ganesan, S.; Heinemann, V.; Rouleau, E.; Turnbull, C.; Garcia Palacios, L.; Lopez, J.-A.; Sokol, E.S.; et al. Pan-Cancer Analysis of Homologous Recombination Repair–Associated Gene Alterations and Genome-Wide Loss-of-Heterozygosity Score. Clin. Cancer Res. 2022, 28, 1412–1421. [Google Scholar] [CrossRef]
- Richards, S.; Aziz, N.; Bale, S.; Bick, D.; Das, S.; Gastier-Foster, J.; Grody, W.W.; Hegde, M.; Lyon, E.; Spector, E.; et al. Standards and Guidelines for the Interpretation of Sequence Variants: A Joint Consensus Recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet. Med. 2015, 17, 405–424. [Google Scholar] [CrossRef]
- Marchetti, A.; Barberis, M.; Franco, R.; De Luca, G.; Pace, M.V.; Staibano, S.; Volante, M.; Buttitta, F.; Guerini-Rocco, E.; Righi, L.; et al. Multicenter Comparison of 22C3 PharmDx (Agilent) and SP263 (Ventana) Assays to Test PD-L1 Expression for NSCLC Patients to Be Treated with Immune Checkpoint Inhibitors. J. Thorac. Oncol. 2017, 12, 1654–1663. [Google Scholar] [CrossRef]
- Villaruz, L.C.; Ancevski Hunter, K.; Kurland, B.F.; Abberbock, S.; Herbst, C.; Dacic, S. Comparison of PD-L1 Immunohistochemistry Assays and Response to PD-1/L1 Inhibitors in Advanced Non-Small-Cell Lung Cancer in Clinical Practice. Histopathology 2019, 74, 269–275. [Google Scholar] [CrossRef]
- Sacks, D.; Baxter, B.; Campbell, B.C.V.; Carpenter, J.S.; Cognard, C.; Dippel, D.; Eesa, M.; Fischer, U.; Hausegger, K.; Hirsch, J.A.; et al. Multisociety Consensus Quality Improvement Revised Consensus Statement for Endovascular Therapy of Acute Ischemic Stroke. Int. J. Stroke 2018, 13, 612–632. [Google Scholar] [CrossRef] [PubMed]
- Xie, Z.; Bailey, A.; Kuleshov, M.V.; Clarke, D.J.B.; Evangelista, J.E.; Jenkins, S.L.; Lachmann, A.; Wojciechowicz, M.L.; Kropiwnicki, E.; Jagodnik, K.M.; et al. Gene Set Knowledge Discovery with Enrichr. Curr. Protoc. 2021, 1, e90. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.-X.; Zhao, C.-F.; Chen, W.-B.; Liu, Q.-C.; Li, Q.-W.; Lin, Y.-Y.; Gao, F. Pancreatic Cancer: A Review of Epidemiology, Trend, and Risk Factors. World J. Gastroenterol. 2021, 27, 4298–4321. [Google Scholar] [CrossRef] [PubMed]
- Özdoğan, M.; Papadopoulou, E.; Tsoulos, N.; Tsantikidi, A.; Mariatou, V.-M.; Tsaousis, G.; Kapeni, E.; Bourkoula, E.; Fotiou, D.; Kapetsis, G.; et al. Comprehensive Tumor Molecular Profile Analysis in Clinical Practice. BMC Med. Genom. 2021, 14, 105. [Google Scholar] [CrossRef] [PubMed]
- Dehghani, M.; Rosenblatt, K.P.; Li, L.; Rakhade, M.; Amato, R.J. Validation and Clinical Applications of a Comprehensive Next Generation Sequencing System for Molecular Characterization of Solid Cancer Tissues. Front. Mol. Biosci. 2019, 6, 82. [Google Scholar] [CrossRef] [PubMed]
- Volckmar, A.-L.; Leichsenring, J.; Kirchner, M.; Christopoulos, P.; Neumann, O.; Budczies, J.; Morais de Oliveira, C.M.; Rempel, E.; Buchhalter, I.; Brandt, R.; et al. Combined Targeted DNA and RNA Sequencing of Advanced NSCLC in Routine Molecular Diagnostics: Analysis of the First 3000 Heidelberg Cases. Int. J. Cancer 2019, 145, 649–661. [Google Scholar] [CrossRef]
- Buscail, L.; Bournet, B.; Cordelier, P. Role of Oncogenic KRAS in the Diagnosis, Prognosis and Treatment of Pancreatic Cancer. Nat. Rev. Gastroenterol. Hepatol. 2020, 17, 153–168. [Google Scholar] [CrossRef]
- Singhi, A.D.; George, B.; Greenbowe, J.R.; Chung, J.; Suh, J.; Maitra, A.; Klempner, S.J.; Hendifar, A.; Milind, J.M.; Golan, T.; et al. Real-Time Targeted Genome Profile Analysis of Pancreatic Ductal Adenocarcinomas Identifies Genetic Alterations That Might Be Targeted With Existing Drugs or Used as Biomarkers. Gastroenterology 2019, 156, 2242–2253.e4. [Google Scholar] [CrossRef]
- Bournet, B.; Muscari, F.; Buscail, C.; Assenat, E.; Barthet, M.; Hammel, P.; Selves, J.; Guimbaud, R.; Cordelier, P.; Buscail, L. KRAS G12D Mutation Subtype Is A Prognostic Factor for Advanced Pancreatic Adenocarcinoma. Clin. Transl. Gastroenterol. 2016, 7, e157. [Google Scholar] [CrossRef]
- Pan, M.; Jiang, C.; Zhang, Z.; Achacoso, N.; Alexeeff, S.; Solorzano, A.V.; Tse, P.; Chung, E.; Sundaresan, T.; Suga, J.M.; et al. TP53 Gain-of-Function and Non-Gain-of-Function Mutations Are Associated with Differential Prognosis in Advanced Pancreatic Ductal Adenocarcinoma. JCO Precis. Oncol. 2023, 7, e2200570. [Google Scholar] [CrossRef]
- Cao, L.; Huang, C.; Cui Zhou, D.; Hu, Y.; Lih, T.M.; Savage, S.R.; Krug, K.; Clark, D.J.; Schnaubelt, M.; Chen, L.; et al. Proteogenomic Characterization of Pancreatic Ductal Adenocarcinoma. Cell 2021, 184, 5031–5052.e26. [Google Scholar] [CrossRef] [PubMed]
- Baker, S.J.; Vogelstein, B. P53: A Tumor Suppressor Hiding in Plain Sight. J. Mol. Cell Biol. 2019, 11, 536–538. [Google Scholar] [CrossRef] [PubMed]
- Vousden, K.H.; Prives, C. Blinded by the Light: The Growing Complexity of P53. Cell 2009, 137, 413–431. [Google Scholar] [CrossRef] [PubMed]
- Freed-Pastor, W.A.; Prives, C. Mutant P53: One Name, Many Proteins. Genes Dev. 2012, 26, 1268–1286. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Liu, J.; Xu, D.; Zhang, T.; Hu, W.; Feng, Z. Gain-of-Function Mutant P53 in Cancer Progression and Therapy. J. Mol. Cell Biol. 2020, 12, 674–687. [Google Scholar] [CrossRef] [PubMed]
- Swisher, E.M.; Kwan, T.T.; Oza, A.M.; Tinker, A.V.; Ray-Coquard, I.; Oaknin, A.; Coleman, R.L.; Aghajanian, C.; Konecny, G.E.; O’Malley, D.M.; et al. Molecular and Clinical Determinants of Response and Resistance to Rucaparib for Recurrent Ovarian Cancer Treatment in ARIEL2 (Parts 1 and 2). Nat. Commun. 2021, 12, 2487. [Google Scholar] [CrossRef] [PubMed]
- Terrero, G.; Datta, J.; Dennison, J.; Sussman, D.A.; Lohse, I.; Merchant, N.B.; Hosein, P.J. Ipilimumab/Nivolumab Therapy in Patients With Metastatic Pancreatic or Biliary Cancer With Homologous Recombination Deficiency Pathogenic Germline Variants. JAMA Oncol. 2022, 8, 938–940. [Google Scholar] [CrossRef] [PubMed]
- Lawlor, R.T.; Mattiolo, P.; Mafficini, A.; Hong, S.-M.; Piredda, M.L.; Taormina, S.V.; Malleo, G.; Marchegiani, G.; Pea, A.; Salvia, R.; et al. Tumor Mutational Burden as a Potential Biomarker for Immunotherapy in Pancreatic Cancer: Systematic Review and Still-Open Questions. Cancers 2021, 13, 3119. [Google Scholar] [CrossRef]
- Karamitopoulou, E.; Andreou, A.; Wenning, A.S.; Gloor, B.; Perren, A. High Tumor Mutational Burden (TMB) Identifies a Microsatellite Stable Pancreatic Cancer Subset with Prolonged Survival and Strong Anti-Tumor Immunity. Eur. J. Cancer 2022, 169, 64–73. [Google Scholar] [CrossRef]
- Samstein, R.M.; Lee, C.-H.; Shoushtari, A.N.; Hellmann, M.D.; Shen, R.; Janjigian, Y.Y.; Barron, D.A.; Zehir, A.; Jordan, E.J.; Omuro, A.; et al. Tumor Mutational Load Predicts Survival after Immunotherapy across Multiple Cancer Types. Nat. Genet. 2019, 51, 202–206. [Google Scholar] [CrossRef]
- Imamura, T.; Ashida, R.; Ohshima, K.; Uesaka, K.; Sugiura, T.; Ohgi, K.; Yamada, M.; Otsuka, S.; Hatakeyama, K.; Nagashima, T.; et al. Characterization of Pancreatic Cancer with Ultra-Low Tumor Mutational Burden. Sci. Rep. 2023, 13, 4359. [Google Scholar] [CrossRef] [PubMed]

| Features | No. of Patients | % |
|---|---|---|
| Age | ||
| <60 | 165 | 41.25% |
| ≥60 | 235 | 58.75% |
| Gender | ||
| Male | 226 | 56.50% |
| Female | 174 | 43.50% |
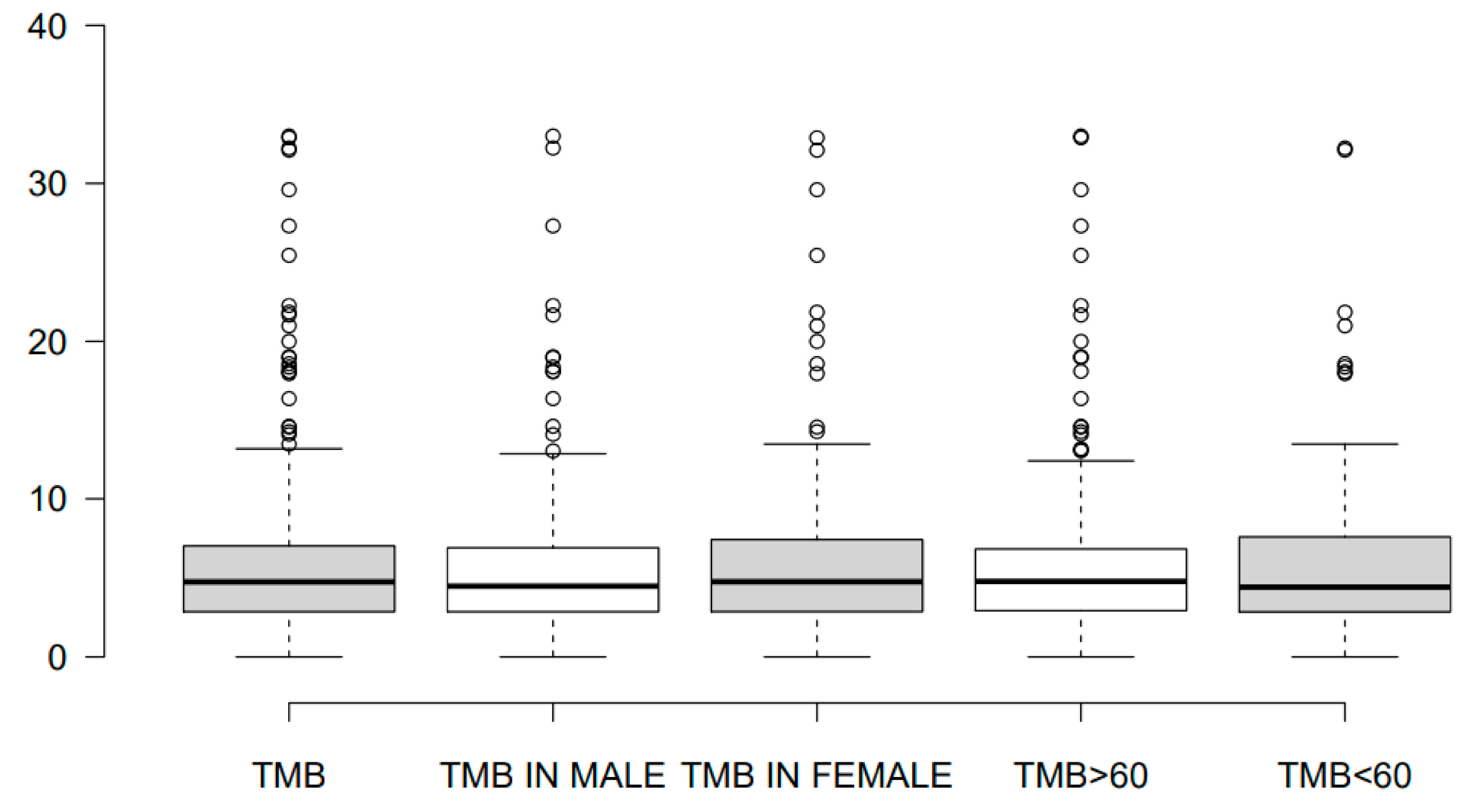
| TMB level | ||
| Median (Range) | 313 | 4.78 (0–45.21) |
| Features | Biomarker | ||||
|---|---|---|---|---|---|
| TMB > 10 muts/MB | KRAS Mutation | TP53 Mutation | HR Gene Positive | %LOH > 16% | |
| Male | 11.18% | 77.43% | 51.72% | 7.25% | 24.05% |
| Female | 14.69% | 86.78% | 48.28% | 2.75% | 15.19% |
| Age < 60 | 13.85% | 77.58% | 43.35% | 4.00% | 20.25% |
| Age > 60 | 12.02% | 84.25% | 56.65% | 6.00% | 18.99% |
| Total | 12.78% (40/313) | 81.50% (326/400) | 50.75% (203/400) | 10.00% (40/400) | 39.24% (31/79) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ziogas, D.C.; Papadopoulou, E.; Gogas, H.; Sakellariou, S.; Felekouras, E.; Theocharopoulos, C.; Stefanou, D.T.; Theochari, M.; Boukovinas, I.; Matthaios, D.; et al. Digging into the NGS Information from a Large-Scale South European Population with Metastatic/Unresectable Pancreatic Ductal Adenocarcinoma: A Real-World Genomic Depiction. Cancers 2024, 16, 2. https://doi.org/10.3390/cancers16010002
Ziogas DC, Papadopoulou E, Gogas H, Sakellariou S, Felekouras E, Theocharopoulos C, Stefanou DT, Theochari M, Boukovinas I, Matthaios D, et al. Digging into the NGS Information from a Large-Scale South European Population with Metastatic/Unresectable Pancreatic Ductal Adenocarcinoma: A Real-World Genomic Depiction. Cancers. 2024; 16(1):2. https://doi.org/10.3390/cancers16010002
Chicago/Turabian StyleZiogas, Dimitrios C., Eirini Papadopoulou, Helen Gogas, Stratigoula Sakellariou, Evangellos Felekouras, Charalampos Theocharopoulos, Dimitra T. Stefanou, Maria Theochari, Ioannis Boukovinas, Dimitris Matthaios, and et al. 2024. "Digging into the NGS Information from a Large-Scale South European Population with Metastatic/Unresectable Pancreatic Ductal Adenocarcinoma: A Real-World Genomic Depiction" Cancers 16, no. 1: 2. https://doi.org/10.3390/cancers16010002
APA StyleZiogas, D. C., Papadopoulou, E., Gogas, H., Sakellariou, S., Felekouras, E., Theocharopoulos, C., Stefanou, D. T., Theochari, M., Boukovinas, I., Matthaios, D., Koumarianou, A., Zairi, E., Liontos, M., Koutsoukos, K., Metaxa-Mariatou, V., Kapetsis, G., Meintani, A., Tsaousis, G. N., & Nasioulas, G. (2024). Digging into the NGS Information from a Large-Scale South European Population with Metastatic/Unresectable Pancreatic Ductal Adenocarcinoma: A Real-World Genomic Depiction. Cancers, 16(1), 2. https://doi.org/10.3390/cancers16010002








