Long-Term Follow-Up of Peritoneal Interposition Flap in Symptomatic Lymphocele Reduction following Robot-Assisted Radical Prostatectomy: Insights from the PIANOFORTE Trial
Abstract
Simple Summary
Abstract
1. Introduction
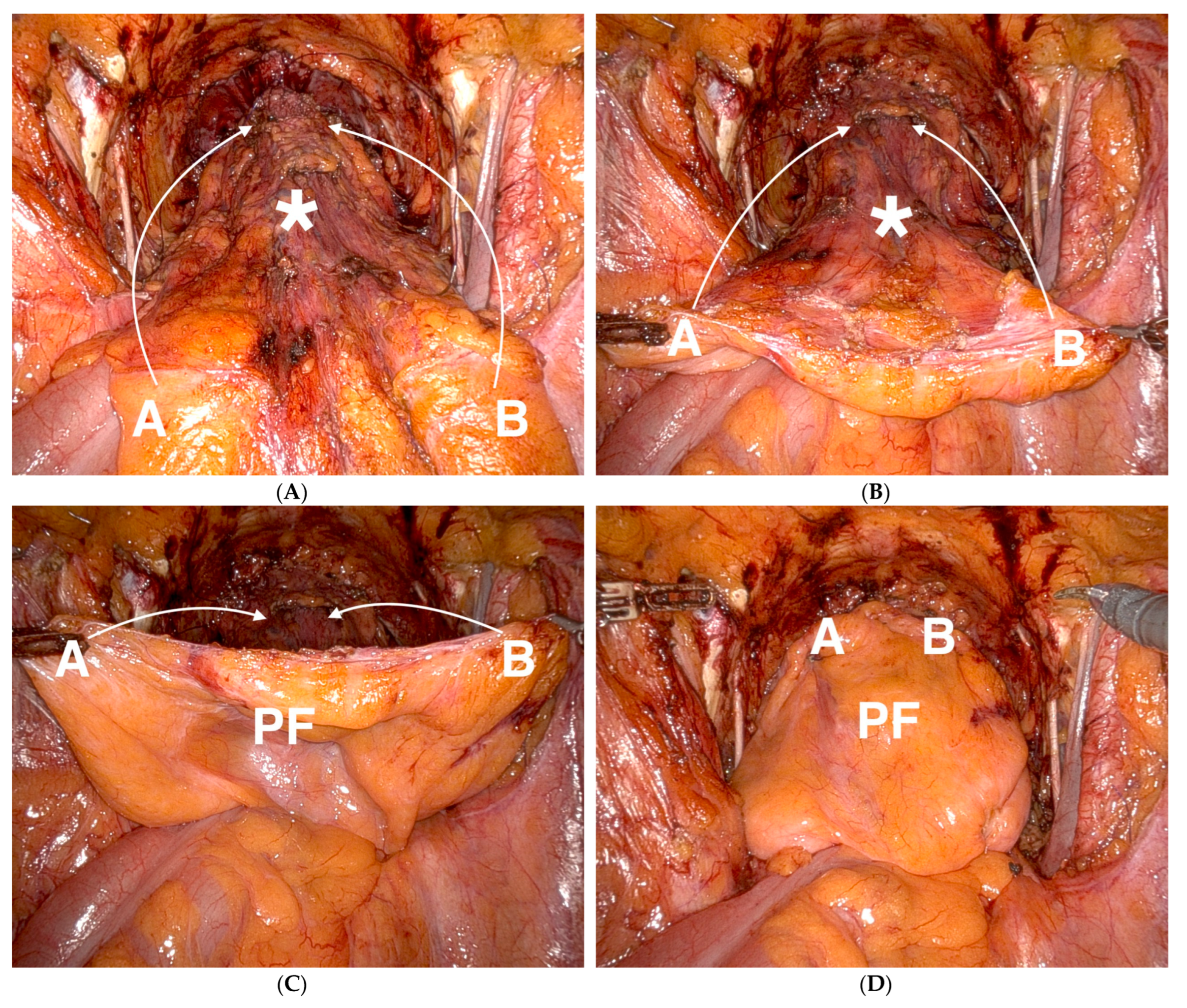
2. Materials and Methods
2.1. Study Population and Follow-Up
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Liss, M.A.; Lusch, A.; Morales, B.; Beheshti, N.; Skarecky, D.; Narula, N.; Osann, K.; Ahlering, T.E. Robot-assisted radical prostatectomy: 5-year oncological and biochemical outcomes. J. Urol. 2012, 188, 2205–2210. [Google Scholar] [CrossRef] [PubMed]
- Dell’Oglio, P.; Mottrie, A.; Mazzone, E. Robot-assisted radical prostatectomy vs. open radical prostatectomy: Latest evidences on perioperative, functional and oncological outcomes. Curr. Opin. Urol. 2020, 30, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Fossati, N.; Willemse, P.M.; Van den Broeck, T.; van den Bergh, R.C.N.; Yuan, C.Y.; Briers, E.; Bellmunt, J.; Bolla, M.; Cornford, P.; De Santis, M.; et al. The Benefits and Harms of Different Extents of Lymph Node Dissection During Radical Prostatectomy for Prostate Cancer: A Systematic Review. Eur. Urol. 2017, 72, 84–109. [Google Scholar] [CrossRef] [PubMed]
- EAU Guidelines. Edn. In Proceedings of the EAU Annual Congress, Milan, Italy, 10–13 March 2023; ISBN 978-94-92671-19-6.
- Ploussard, G.; Briganti, A.; de la Taille, A.; Haese, A.; Heidenreich, A.; Menon, M.; Sulser, T.; Tewari, A.K.; Eastham, J.A. Pelvic lymph node dissection during robot-assisted radical prostatectomy: Efficacy, limitations, and complications-a systematic review of the literature. Eur. Urol. 2014, 65, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Horovitz, D.; Lu, X.; Feng, C.; Messing, E.M.; Joseph, J.V. Rate of Symptomatic Lymphocele Formation After Extraperitoneal vs Transperitoneal Robot-Assisted Radical Prostatectomy and Bilateral Pelvic Lymphadenectomy. J. Endourol. 2017, 31, 1037–1043. [Google Scholar] [CrossRef] [PubMed]
- Sforza, S.; Tellini, R.; Grosso, A.A.; Zaccaro, C.; Viola, L.; Di Maida, F.; Mari, A.; Carini, M.; Minervini, A.; Masieri, L. Can we predict the development of symptomatic lymphocele following robot-assisted radical prostatectomy and lymph node dissection? Results from a tertiary referral Centre. Scand. J. Urol. 2020, 54, 328–333. [Google Scholar] [CrossRef] [PubMed]
- Lebeis, C.; Canes, D.; Sorcini, A.; Moinzadeh, A. Novel Technique Prevents Lymphoceles After Transperitoneal Robotic-assisted Pelvic Lymph Node Dissection: Peritoneal Flap Interposition. Urology 2015, 85, 1505–1509. [Google Scholar] [CrossRef]
- May, M.; Gloger, S.; Wolff, I. Peritoneal Interposition Flap: An Updated Meta-Analysis of Six Randomized Controlled Trials Revealing Consistent Reduction of Symptomatic Lymphoceles Following Robot-Assisted Radical Prostatectomy and Pelvic Lymph Node Dissection. J. Endourol. 2023, 38, 529–530. [Google Scholar] [CrossRef]
- Bründl, J.; Lenart, S.; Stojanoski, G.; Gilfrich, C.; Rosenhammer, B.; Stolzlechner, M.; Ponholzer, A.; Dreissig, C.; Weikert, S.; Burger, M.; et al. Peritoneal Flap in Robot-Assisted Radical Prostatectomy. Dtsch. Arztebl. Int. 2020, 117, 243–250. [Google Scholar] [CrossRef]
- Available online: https://www.drks.de/drks_web/navigate.do?navigationId=trial.HTML&TRIAL_ID=DRKS00011115 (accessed on 3 December 2023).
- Dindo, D.; Demartines, N.; Clavien, P.A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef]
- Wilson, L.C.; Gilling, P.J. Post-prostatectomy urinary incontinence: A review of surgical treatment options. BJU Int. 2011, 107 (Suppl. 3), 7–10. [Google Scholar] [CrossRef] [PubMed]
- Liss, M.A.; Osann, K.; Canvasser, N.; Chu, W.; Chang, A.; Gan, J.; Li, R.; Santos, R.; Skarecky, D.; Finley, D.S.; et al. Continence definition after radical prostatectomy using urinary quality of life: Evaluation of patient reported validated questionnaires. J. Urol. 2010, 183, 1464–1468. [Google Scholar] [CrossRef]
- Schussler, B.; Alloussi, S. [Ingelman-Sundberg classification of stress incontinence]. Gynakol. Rundsch. 1983, 23, 166–174. [Google Scholar] [CrossRef] [PubMed]
- May, M.; Gilfrich, C.; Bründl, J.; Ubrig, B.; Wagner, J.R.; Gloger, S.; Student, V., Jr.; Merseburger, A.S.; Thomas, C.; Brookman-May, S.D.; et al. Impact of Peritoneal Interposition Flap on Patients Undergoing Robot-assisted Radical Prostatectomy and Pelvic Lymph Node Dissection: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Eur. Urol. Focus 2024, 10, 80–89. [Google Scholar] [CrossRef]
- Ditonno, F.; Manfredi, C.; Franco, A.; Veccia, A.; Moro, F.D.; De Nunzio, C.; De Sio, M.; Antonelli, A.; Autorino, R. Impact of peritoneal reconfiguration on lymphocele formation after robot-assisted radical prostatectomy with pelvic lymph node dissection: A systematic review and meta-analysis of randomized controlled trials. Prostate Cancer Prostatic Dis. 2023; ahead of print. [Google Scholar]
- Gloger, S.; Ubrig, B.; Boy, A.; Leyh-Bannurah, S.R.; Siemer, S.; Arndt, M.; Stolzenburg, J.U.; Franz, T.; Oelke, M.; Witt, J.H. Bilateral Peritoneal Flaps Reduce Incidence and Complications of Lymphoceles after Robotic Radical Prostatectomy with Pelvic Lymph Node Dissection-Results of the Prospective Randomized Multicenter Trial ProLy. J. Urol. 2022, 208, 333–340. [Google Scholar] [CrossRef]
- Student, V., Jr.; Tudos, Z.; Studentova, Z.; Cesak, O.; Studentova, H.; Repa, V.; Purova, D.; Student, V. Effect of Peritoneal Fixation (PerFix) on Lymphocele Formation in Robot-assisted Radical Prostatectomy with Pelvic Lymphadenectomy: Results of a Randomized Prospective Trial. Eur. Urol. 2023, 83, 154–162. [Google Scholar] [CrossRef] [PubMed]
- Wagner, J.; McLaughlin, T.; Pinto, K.; Tortora, J.; Gangakhedkar, A.; Staff, I. The Effect of a Peritoneal Iliac Flap on Lymphocele Formation After Robotic Radical Prostatectomy: Results From the PLUS Trial. Urology 2023, 173, 104–110. [Google Scholar] [CrossRef]
- Neuberger, M.; Kowalewski, K.F.; Simon, V.; von Hardenberg, J.; Siegel, F.; Wessels, F.; Worst, T.S.; Michel, M.S.; Westhoff, N.; Kriegmair, M.C.; et al. Peritoneal Flap for Lymphocele Prophylaxis Following Robotic-assisted Radical Prostatectomy with Lymph Node Dissection: The Randomised Controlled Phase 3 PELYCAN Trial. Eur. Urol. Oncol. 2024, 7, 53–62. [Google Scholar] [CrossRef]
- Pose, R.M.; Knipper, S.; Hohenhorst, L.; Beyer, B.; Haese, A.; Heinzer, H.; Salomon, G.; Steuber, T.; Budäus, L.; Tilki, D.; et al. Impact of peritoneal bladder flap on the risk of lymphoceles after robotic radical prostatectomy: Results of a prospective controlled trial. Eur. Urol. Suppl. 2023, 83, S932. [Google Scholar] [CrossRef]
- Gamal, A.; Moschovas, M.C.; Jaber, A.R.; Saikali, S.; Sandri, M.; Patel, E.; Patel, E.; Rogers, T.; Patel, V. Peritoneal Flap Following Lymph Node Dissection in Robotic Radical Prostatectomy: A Novel “Bunching” Technique. Cancers 2024, 16, 1547. [Google Scholar] [CrossRef]
- Khorshidi, F.; Majdalany, B.S.; Peters, G.; Tran, A.N.; Shaikh, J.; Liddell, R.P.; Perez Lozada, J.C.; Kokabi, N.; Nezami, N. Minimally invasive treatment of abdominal lymphocele: A review of contemporary options and how to approach them. Lymphology 2021, 54, 56–67. [Google Scholar] [CrossRef] [PubMed]
- Briganti, A.; Chun, F.K.; Salonia, A.; Suardi, N.; Gallina, A.; Da Pozzo, L.F.; Roscigno, M.; Zanni, G.; Valiquette, L.; Rigatti, P.; et al. Complications and other surgical outcomes associated with extended pelvic lymphadenectomy in men with localized prostate cancer. Eur. Urol. 2006, 50, 1006–1013. [Google Scholar] [CrossRef]
- Naselli, A.; Andreatta, R.; Introini, C.; Fontana, V.; Puppo, P. Predictors of symptomatic lymphocele after lymph node excision and radical prostatectomy. Urology 2010, 75, 630–635. [Google Scholar] [CrossRef] [PubMed]
- Baas, D.J.H.; de Baaij, J.M.S.; Sedelaar, J.P.M.; Hoekstra, R.J.; Vrijhof, H.J.E.J.; Somford, D.M.; van Basten, J.A. Extended pelvic lymph node dissection in robot-assisted radical prostatectomy is an independent risk factor for major complications. J. Robot. Surg. 2024, 18, 140. [Google Scholar] [CrossRef] [PubMed]
- Keskin, M.S.; Argun, Ö.B.; Öbek, C.; Tufek, I.; Tuna, M.B.; Mourmouris, P.; Erdoğan, S.; Kural, A.R. The incidence and sequela of lymphocele formation after robot-assisted extended pelvic lymph node dissection. BJU Int. 2016, 118, 127–131. [Google Scholar] [CrossRef]
- Novara, G.; Ficarra, V.; Mocellin, S.; Ahlering, T.E.; Carroll, P.R.; Graefen, M.; Guazzoni, G.; Menon, M.; Patel, V.R.; Shariat, S.F.; et al. Systematic review and meta-analysis of studies reporting oncologic outcome after robot-assisted radical prostatectomy. Eur. Urol. 2012, 62, 382–404. [Google Scholar] [CrossRef]
| Criteria | Whole Study Group | PIF | No PIF | p |
|---|---|---|---|---|
| Follow-up in months, median (IQR) | 43.0 (41.0–46.0) | 42.0 (40.0–46.0) | 43.0 (41.0–45.00) | 0.758 |
| Patients presenting for long-term FU (% of the original study population) | 176 (75.9%) | 81 (75.0%) | 95 (76.6%) | 0.516 |
| All further values and percentages refer to the above-mentioned number of patients presenting for long-term FU | ||||
| Patients’ age at the time of RARP in years, median (IQR) | 64.5 (58.25–68.0) | 64.0 (58.5–67.5) | 65.0 (58.0–70.0) | 0.454 |
| ISUP grading score in RARP | 0.559 | |||
| 1 | 12 (6.8%) | 7 (8.6%) | 5 (5.3%) | |
| 2 | 94 (53.4%) | 40 (49.4%) | 54 (56.8%) | |
| 3 | 42 (23.9%) | 23 (28.4%) | 19 (20.0% | |
| 4 | 18 (10.2%) | 7 (8.6%) | 11 (11.6%) | |
| 5 | 10 (5.7%) | 4 (4.9%) | 6 (6.3%) | |
| T-Stage in RARP | 0.111 | |||
| pT0 | 1 (0.6%) | 1 (1.2%) | 0 (0%) | |
| pT2a | 15 (8.5%) | 10 (12.3%) | 5 (5.3%) | |
| pT2b | 11 (6.3%) | 6 (7.4%) | 5 (5.3%) | |
| pT2c | 100 (56.8%) | 37 (45.7%) | 63 (66.3%) | |
| pT3a | 26 (14.8%) | 14 (17.3%) | 12 (12.6%) | |
| pT3b | 22 (12.5%) | 13 (16.0%) | 9 (9.5%) | |
| pT4 | 1 (0.6%) | 0 (0%) | 1 (1.1%) | |
| Positive lymph nodes in RARP | 0.550 | |||
| No | 164 (93.2%) | 77 (95.1%) | 87 (91.6%) | |
| Yes | 12 (6.8%) | 4 (4.9%) | 8 (8.4%) | |
| Positive surgical margins in RARP | 0.509 | |||
| No | 152 (86.4%) | 68 (84.0%) | 84 (88.4%) | |
| Yes | 24 (13.6%) | 13 (16.0%) | 11 (11.6%) | |
| Abdominal surgery prior to RARP | 0.622 | |||
| None | 96 (54.5%) | 44 (54.3%) | 52 (54.7%) | |
| Minor | 68 (38.6%) | 33 (40.7%) | 35 (36.8%) | |
| Major (laparotomy) | 12 (6.8%) | 4 (4.9%) | 8 (8.4%) | |
| LC at long-term FU | 0.274 | |||
| 171 (97.2%) | 77 (95.1%) | 94 (98.9%) | |
| 4 (2.3%) | 3 (3.7%) | 1 (1.1%) | |
| 1 (0.6%) | 1 (1.2%) | 0 (0.0%) | |
| Symptoms at long-term FU | 0.626 | |||
| 172 (97.7%) | 80 (98.8%) | 92 (96.8%) | |
| 4 (1.7%) | 1 (1.2%) | 3 (3.2%) | |
| LC between 90 days and long-term FU | 0.576 | |||
| 166 (94.3%) | 75 (92.6%) | 92 (95.8%) | |
| 6 (3.4%) | 4 (4.9%) | 2 (2.1%) | |
| 4 (2.3%) | 2 (2.5%) | 2 (2.1%) | |
| LC therapy between 90 days and long-term FU | 0.999 | |||
| 175 (99.4%) | 81 (100.0%) | 94 (98.9%) | |
| 1 (0.6%) | 0 (0.0%) | 1 (1.1%) | |
| 0.981 | |||
| 113 (64.2%) | 51 (63.0%) | 62 (65.3%) | |
| 54 (30.7%) | 26 (32.1%) | 28 (29.5%) | |
| 7 ( 4.0%) | 3 (3.7%) | 4 (4.2%) | |
| 2 (1.1%) | 1 (1.2%) | 1 (1.1%) | |
| Other complications between 90 days and long-term FU (multiple possible) | 0.481 | |||
| 155 (88.1%) | 74 (91.4%) | 81 (85.3%) | |
| 1 (0.6%) | 0 (0.0%) | 1 (1.1%) | |
| 4 (2.3%) | 2 (2.5%) | 2 (2.1%) | |
| 16 (9.1%) | 5 (6.2%) | 11 (11.6%) | |
| Clavien–Dindo classification of above-mentioned complications: | 0.999 | |||
| 14 (7.9%) | 4 (4.9%) | 10 (10.6%) | |
| 6 (3.4%) | 3 (3.7%) | 3 (3.2%) | |
| Oncologic follow-up | 0.287 | |||
| 135 (76.7%) | 58 (71.6%) | 77 (81.1%) | |
| 21 (11.9%) | 13 (16.0%) | 8 (8.4%) | |
| 1 (0.6%) | 0 (0.0%) | 1 (1.1%) | |
| 18 (10.2%) | 10 (12.3%) | 8 (8.4%) | |
| 1 (0.6%) | 0 (0.0%) | 1 (1.1%) | |
| Reference (Study Name) | Country | Study Period | Study Design | FU (Months) a | sLC Rate d p-Value | FU Extension (Months) | sLC Rate e p-Value |
|---|---|---|---|---|---|---|---|
| Bründl 2020 (PIANOFORTE) [11] | Germany, Austria | 2017 | Multi-centre double-blinded RCT | 3 b | Intervention: 9/108 (8.3%) Control: 12/124 (9.7%) p = 0.721 | 43 c | Intervention: 2/81 (2.5%) Control: 2/95 (2.1%) p = 0.871 |
| Gloger 2022 (ProLy) [19] | Germany | 2018–2020 | Multi-centre double-blinded RCT | 3 b | Intervention: 8/239 (3.3%) Control: 19/236 (8.1%) p = 0.027 | n.a. | n.a. |
| Student 2023 (PerFix) [20] | Czech Republic | 2019–2021 | Single-center single-blinded RCT | 20 c | Intervention: 3/123 (2.4%) Control: 14/122 (11.5%) p = 0.005 | n.a. | n.a. |
| Wagner 2023 (PLUS) [21] | United States of America | 2018–2021 | Single-center assessor-blinded RCT | 3.7 c | Intervention: 1/110 (0.9%) Control: 1/106 (0.9%) p = 0.979 | n.a. | n.a. |
| Neuberger 2023 (PELYCAN) [22] | Germany | 2019–2021 | Single-center double-blinded RCT | 6 b | Intervention: 10/270 (3.7%) Control: 25/274 (9.1%) p = 0.010 | n.a. | n.a. |
| Pose 2023 (Michl-Technique) [23] | Germany | 2017–2019 | Single-center single-blinded RCT | 12 b | Intervention: 38/531 (7.2%) Control: 48/549 (8.7%) p = 0.336 | n.a. | n.a. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goßler, C.; May, M.; Weikert, S.; Lenart, S.; Ponholzer, A.; Dreissig, C.; Stojanoski, G.; Anzinger, I.; Riester, J.; Burger, M.; et al. Long-Term Follow-Up of Peritoneal Interposition Flap in Symptomatic Lymphocele Reduction following Robot-Assisted Radical Prostatectomy: Insights from the PIANOFORTE Trial. Cancers 2024, 16, 1932. https://doi.org/10.3390/cancers16101932
Goßler C, May M, Weikert S, Lenart S, Ponholzer A, Dreissig C, Stojanoski G, Anzinger I, Riester J, Burger M, et al. Long-Term Follow-Up of Peritoneal Interposition Flap in Symptomatic Lymphocele Reduction following Robot-Assisted Radical Prostatectomy: Insights from the PIANOFORTE Trial. Cancers. 2024; 16(10):1932. https://doi.org/10.3390/cancers16101932
Chicago/Turabian StyleGoßler, Christopher, Matthias May, Steffen Weikert, Sebastian Lenart, Anton Ponholzer, Christina Dreissig, Gjoko Stojanoski, Isabel Anzinger, Josef Riester, Maximilian Burger, and et al. 2024. "Long-Term Follow-Up of Peritoneal Interposition Flap in Symptomatic Lymphocele Reduction following Robot-Assisted Radical Prostatectomy: Insights from the PIANOFORTE Trial" Cancers 16, no. 10: 1932. https://doi.org/10.3390/cancers16101932
APA StyleGoßler, C., May, M., Weikert, S., Lenart, S., Ponholzer, A., Dreissig, C., Stojanoski, G., Anzinger, I., Riester, J., Burger, M., Gilfrich, C., Mayr, R., & Bründl, J. (2024). Long-Term Follow-Up of Peritoneal Interposition Flap in Symptomatic Lymphocele Reduction following Robot-Assisted Radical Prostatectomy: Insights from the PIANOFORTE Trial. Cancers, 16(10), 1932. https://doi.org/10.3390/cancers16101932







