The Role of Biomarkers in Lung Cancer Screening
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. The Need for Meaningful LCS Biomarkers
3.2. Circulating Blood-Based and Serum-Based Biomarkers
3.3. RNA-Based Biomarkers
3.4. miRNA
3.5. Circulating Tumor Cells (CTCs) for LCS
3.6. Breath Biomarkers
3.7. Volatile Organic Compounds (VOCs)
4. Discussion
5. Conclusions
Future Directions
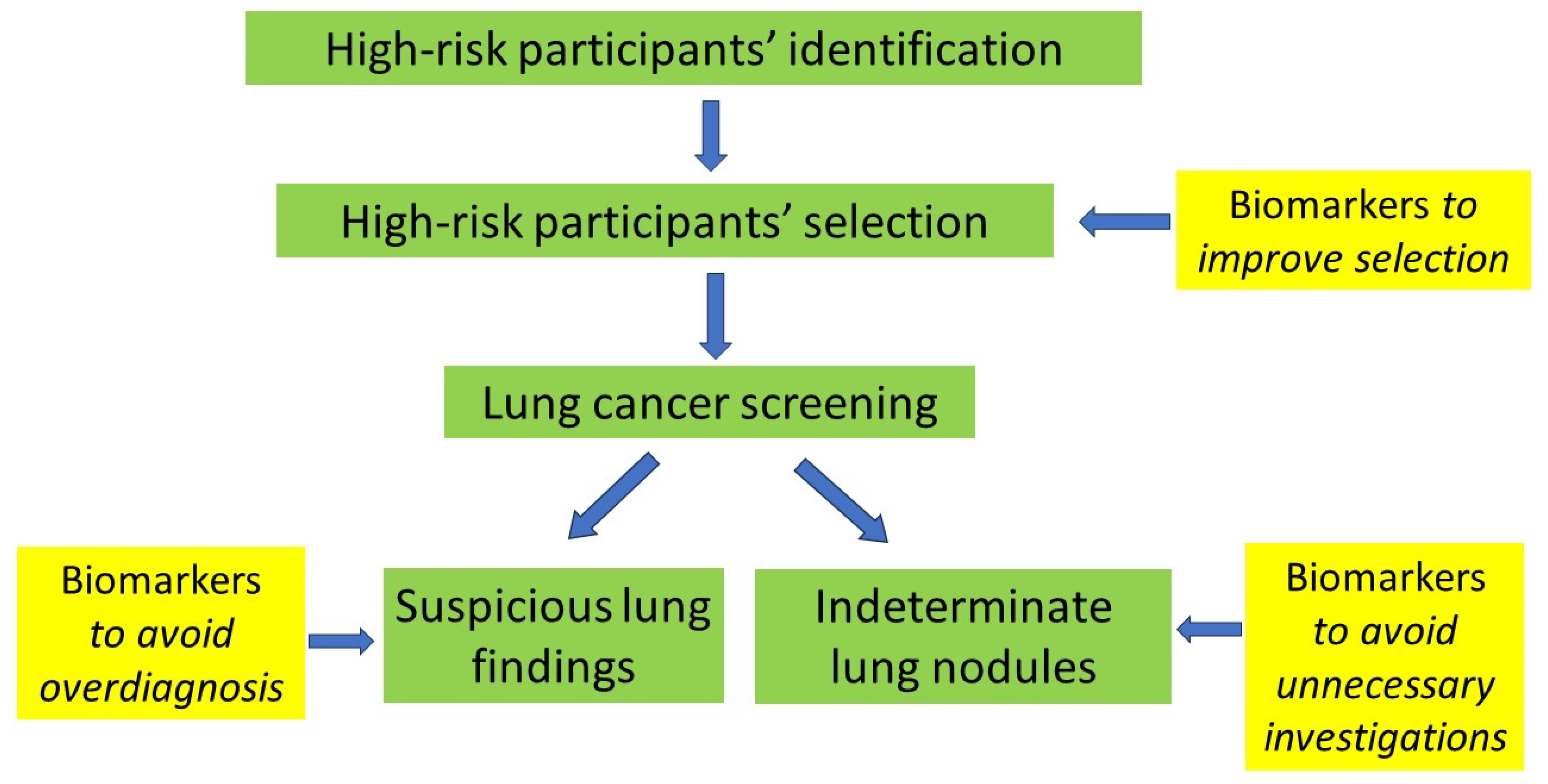
- Optimal participant selection, i.e., identifying high-risk individuals that will, indeed, benefit from LDS. Biomarkers, in this case, will play a complementary role in simple inclusion criteria as well as risk stratification models for LCS.
- The clarification of the status of indeterminate pulmonary nodules to avoid unnecessary follow-up and investigations that will increase the burden on existing resources and participant anxiety.
- The clarification of suspicious lung findings with the view to minimizing or even completely avoiding unnecessary investigations and diminishing overdiagnosis.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2019. CA Cancer J. Clin. 2019, 69, 7–34. [Google Scholar] [CrossRef] [PubMed]
- The National Lung Screening Trial Research Team. Reduced Lung-Cancer Mortality with Low-Dose Computed Tomographic Screening. N. Engl. J. Med. 2011, 365, 395–409. [Google Scholar] [CrossRef] [PubMed]
- De Koning, H.J.; Van Der Aalst, C.M.; De Jong, P.A. Reduced Lung-Cancer Mortality with Volume CT Screening in a Randomized Trial. N. Engl. J. Med. 2020, 382, 503–513. [Google Scholar] [CrossRef] [PubMed]
- Baldwin, D.R.; Callister, M.E.; Crosbie, P.A.; O’Dowd, E.L.; Rintoul, R.C.; Robbins, H.A.; Steele, R.J.C. Biomarkers in lung cancer screening: The importance of study design. Eur. Respir. J. 2021, 57, 2004367. [Google Scholar] [CrossRef]
- Carozzi, F.M.; Bisanzi, S.; Carrozzi, L.; Falaschi, F.; Lopes Pegna, A.; Mascalchi, M.; Picozzi, G.; Peluso, M.; Sani, C.; Greco, L.; et al. ITALUNG Working Group. Multimodal lung cancer screening using the ITALUNG biomarker panel and low dose computed tomography. Results of the ITALUNG biomarker study. Int. J. Cancer 2017, 141, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, F.M.; Mair, F.S.; Anderson, W.; Armory, P.; Briggs, A.; Chew, C.; Dorward, A.; Haughney, J.; Hogarth, F.; Kendrick, D. The Early Diagnosis of Lung Cancer Scotland (ECLS) Team. Earlier diagnosis of lung cancer in a randomised trial of an autoantibody blood test followed by imaging. Eur. Respir. J. 2020, 57, 2000670. [Google Scholar] [CrossRef] [PubMed]
- Larose, T.L.; Meheus, F.; Brennan, P.; Johansson, M.; Robbins, H.A. Assessment of Biomarker Testing for Lung Cancer Screening Eligibility. JAMA Netw. Open 2020, 3, e200409. [Google Scholar] [CrossRef] [PubMed]
- Seijo, L.M.; Peled, N.; Ajona, D.; Boeri, M.; Field, J.K.; Sozzi, G.; Pio, R.; Zulueta, J.J.; Spira, A.; Massion, P.P.; et al. Biomarkers in Lung Cancer Screening: Achievements, Promises, and Challenges. J. Thorac. Oncol. Off. Publ. Int. Assoc. Study Lung Cancer 2019, 14, 343–357. [Google Scholar] [CrossRef]
- Klein, E.A.; Richards, D.; Cohn, A.; Tummala, M.; Lapham, R.; Cosgrove, D.; Chung, G.; Clement, J.; Gao, J.; Hunkapiller, N.; et al. Clinical validation of a targeted methylation-based multi-cancer early detection test using an independent validation set. Ann. Oncol. 2021, 32, 1167–1177. [Google Scholar] [CrossRef]
- Snowsill, T.; Yang, H.; Griffin, E.; Long, L.; Varley-Campbell, J.; Coelho, H.; Robinson, S.; Hyde, C. Low-dose computed tomography for lung cancer screening in high-risk populations: A systematic review and economic evaluation. Health Technol. Assess. 2018, 22, 1–276. [Google Scholar] [CrossRef]
- Trevethan, R. Sensitivity, Specificity, and Predictive Values: Foundations, Pliabilities, and Pitfalls in Research and Practice. Front. Public Health 2017, 5, 307. [Google Scholar] [CrossRef] [PubMed]
- Marmor, H.N.; Zorn, J.T.; Deppen, S.A.; Massion, P.P.; Grogan, E.L. Biomarkers in lung cancer screening: A narrative review. Curr. Chall. Thorac. Surg. 2023, 5, 5. [Google Scholar] [CrossRef] [PubMed]
- Atwater, T.; Massion, P.P. Biomarkers of risk to develop lung cancer in the new screening era. Ann. Transl. Med. 2016, 4, 158. [Google Scholar] [CrossRef]
- Bastani, M.; Toumazis, I.; Hedou’, J.; Leung, A.; Plevritis, S.K. Evaluation of Alternative Diagnostic Follow-up Intervals for Lung Reporting and Data System Criteria on the Effectiveness of Lung Cancer Screening. J. Am. Coll. Radiol. 2021, 18, 1614–1623. [Google Scholar] [CrossRef]
- Bonney, A.; Malouf, R.; Marchal, C.; Manners, K.; Fong, K.M.; Marshall, H.M.; Irving, L.B.; Manser, R. Impact of low-dose computed tomography (LDCT) screening on lung cancer-related mortality. Cochrane Database Syst. Rev. 2022, 8, CD013829. [Google Scholar]
- Rodríguez, M.; Ajona, D.; Seijo, L.M.; Sanz, J.; Valencia, K.; Corral, J.; Mesa-Guzmán, M.; Pío, R.; Calvo, A.; Lozano, M.D.; et al. Molecular biomarkers in early stage lung cancer. Transl. Lung Cancer Res. 2021, 10, 1165–1185. [Google Scholar] [CrossRef]
- Sozzi, G.; Boeri, M. Potential biomarkers for lung cancer screening. Transl. Lung Cancer Res. 2014, 3, 139–148. [Google Scholar]
- Chapman, C.J.; Healey, G.F.; Murray, A.; Boyle, P.; Robertson, C.; Peek, L.J.; Allen, J.; Thorpe, A.J.; Hamilton-Fairley, G.; Parsy-Kowalska, C.B.; et al. EarlyCDT®-Lung test: Improved clinical utility through additional autoantibody assays. Tumour Biol. J. Int. Soc. Oncodevelopmental Biol. Med. 2012, 33, 1319–1326. [Google Scholar] [CrossRef] [PubMed]
- Jett, J.R.; Peek, L.J.; Fredericks, L.; Jewell, W.; Pingleton, W.W.; Robertson, J.F. Audit of the autoantibody test, EarlyCDT®-lung, in 1600 patients: An evaluation of its performance in routine clinical practice. Lung Cancer Amst. Neth. 2014, 83, 51–55. [Google Scholar] [CrossRef]
- Wu, W.Y.-Y.; Haider, Z.; Feng, X.; Heath, A.K.; Tjønneland, A.; Agudo, A.; Masala, G.; Robbins, H.A.; Huerta, J.M.; Guevara, M.; et al. Assessment of the EarlyCDT-Lung test as an early biomarker of lung cancer in ever-smokers: A retrospective nested case-control study in two prospective cohorts. Int. J. Cancer 2023, 152, 2002–2010. [Google Scholar] [CrossRef]
- Borg, M.; Wen, S.W.C.; Nederby, L.; Hansen, T.F.; Jakobsen, A.; Andersen, R.F.; Weinreich, U.M.; Hilberg, O. Performance of the EarlyCDT® Lung test in detection of lung cancer and pulmonary metastases in a high-risk cohort. Lung Cancer Amst. Neth. 2021, 158, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Duarte, A.; Corbett, M.; Melton, H.; Harden, M.; Palmer, S.; Soares, M.; Simmonds, M. EarlyCDT Lung blood test for risk classification of solid pulmonary nodules: Systematic review and economic evaluation. Health Technol. Assess. Winch. Engl. 2022, 26, 1–184. [Google Scholar] [CrossRef] [PubMed]
- Vachani, A.; Pass, H.I.; Rom, W.N.; Midthun, D.E.; Edell, E.S.; Laviolette, M.; Li, X.J.; Fong, P.Y.; Hunsucker, S.W.; Hayward, C.; et al. Validation of a multiprotein plasma classifier to identify benign lung nodules. J. Thorac. Oncol. Off. Publ. Int. Assoc. Study Lung Cancer 2015, 10, 629–637. [Google Scholar] [CrossRef] [PubMed]
- Umu, S.U.; Langseth, H.; Bucher-Johannessen, C.; Fromm, B.; Keller, A.; Meese, E.; Lauritzen, M.; Leithaug, M.; Lyle, R.; Rounge, T.B. A comprehensive profile of circulating RNAs in human serum. RNA Biol. 2018, 15, 242–250. [Google Scholar] [CrossRef] [PubMed]
- Dama, E.; Colangelo, T.; Fina, E.; Cremonesi, M.; Kallikourdis, M.; Veronesi, G.; Bianchi, F. Biomarkers and Lung Cancer Early Detection: State of the Art. Cancers 2021, 13, 3919. [Google Scholar] [CrossRef] [PubMed]
- Montani, F.; Marzi, M.J.; Dezi, F.; Dama, E.; Carletti, R.M.; Bonizzi, G.; Bertolotti, R.; Bellomi, M.; Rampinelli, C.; Maisonneuve, P.; et al. miR-Test: A blood test for lung cancer early detection. J. Natl. Cancer Inst. 2015, 107, djv063. [Google Scholar] [CrossRef] [PubMed]
- Sozzi, G.; Boeri, M.; Rossi, M.; Verri, C.; Suatoni, P.; Bravi, F.; Roz, L.; Conte, D.; Grassi, M.; Sverzellati, N.; et al. Clinical utility of a plasma-based miRNA signature classifier within computed tomography lung cancer screening: A correlative MILD trial study. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2014, 32, 768–773. [Google Scholar] [CrossRef] [PubMed]
- Voigt, W.; Prosch, H.; Silva, M. Clinical Scores, Biomarkers and IT Tools in Lung Cancer Screening-Can an Integrated Approach Overcome Current Challenges? Cancers 2023, 15, 1218. [Google Scholar] [CrossRef] [PubMed]
- Fehlmann, T.; Kahraman, M.; Ludwig, N.; Backes, C.; Galata, V.; Keller, V.; Geffers, L.; Mercaldo, N.; Hornung, D.; Weis, T.; et al. Evaluating the Use of Circulating MicroRNA Profiles for Lung Cancer Detection in Symptomatic Patients. JAMA Oncol. 2020, 6, 714–723. [Google Scholar] [CrossRef]
- Castro-Giner, F.; Aceto, N. Tracking cancer progression: From circulating tumor cells to metastasis. Genome Med. 2020, 12, 31. [Google Scholar] [CrossRef]
- Ilie, M.; Hofman, V.; Long-Mira, E.; Selva, E.; Vignaud, J.M.; Padovani, B.; Mouroux, J.; Marquette, C.H.; Hofman, P. “Sentinel” circulating tumor cells allow early diagnosis of lung cancer in patients with chronic obstructive pulmonary disease. PLoS ONE 2014, 9, e111597. [Google Scholar] [CrossRef] [PubMed]
- Hofman, V.; Bonnetaud, C.; Ilie, M.I.; Vielh, P.; Vignaud, J.M.; Fléjou, J.F.; Lantuejoul, S.; Piaton, E.; Mourad, N.; Butori, C.; et al. Preoperative circulating tumor cell detection using the isolation by size of epithelial tumor cell method for patients with lung cancer is a new prognostic biomarker. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2011, 17, 827–835. [Google Scholar] [CrossRef] [PubMed]
- Marquette, C.-H.; Boutros, J.; Benzaquen, J.; Ferreira, M.; Pastre, J.; Pison, C.; Padovani, B.; Bettayeb, F.; Fallet, V.; Guibert, N.; et al. AIR project Study Group. Circulating tumour cells as a potential biomarker for lung cancer screening: A prospective cohort study. Lancet Respir. Med. 2020, 8, 709–716. [Google Scholar] [CrossRef]
- Roś-Mazurczyk, M.; Wojakowska, A.; Marczak, Ł.; Polański, K.; Pietrowska, M.; Polanska, J.; Dziadziuszko, R.; Jassem, J.; Rzyman, W.; Widlak, P. Panel of serum metabolites discriminates cancer patients and healthy participants of lung cancer screening—A pilot study. Acta Biochim. Pol. 2017, 64, 513–518. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Zhang, P.; Wu, R.; Lu, K.; Zhou, H. Identifying the Best Marker Combination in CEA, CA125, CY211, NSE, and SCC for Lung Cancer Screening by Combining ROC Curve and Logistic Regression Analyses: Is It Feasible? Dis. Markers 2018, 2018, 2082840. [Google Scholar] [CrossRef] [PubMed]
- Kok, V.C.; Yu, C.-C. Cancer-Derived Exosomes: Their Role in Cancer Biology and Biomarker Development. Int. J. Nanomed. 2020, 15, 8019–8036. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.-F.; Wei, S.-N.; Geng, N.; Qin, W.W.; He, X.; Wang, X.H.; Qi, Y.P.; Song, S.; Wang, P. Evaluation of circulating small extracellular vesicle-derived miRNAs as diagnostic biomarkers for differentiating between different pathological types of early lung cancer. Sci. Rep. 2022, 12, 17201. [Google Scholar] [CrossRef] [PubMed]
- Smolarz, M.; Kurczyk, A.; Jelonek, K.; Żyła, J.; Mielańczyk, Ł.; Sitkiewicz, M.; Pietrowska, M.; Polańska, J.; Rzyman, W.; Widłak, P. The Lipid Composition of Serum-Derived Small Extracellular Vesicles in Participants of a Lung Cancer Screening Study. Cancers 2021, 13, 3414. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Liu, H.; Xie, D.; He, Z.; Pi, X. Lung Cancer Screening Based on Type-different Sensor Arrays. Sci. Rep. 2017, 7, 1969. [Google Scholar] [CrossRef]
- Chen, K.; Liu, L.; Nie, B.; Lu, B.; Fu, L.; He, Z.; Li, W.; Pi, X.; Liu, H. Recognizing lung cancer and stages using a self-developed electronic nose system. Comput. Biol. Med. 2021, 131, 104294. [Google Scholar] [CrossRef]
- Covington, J.A.; Marco, S.; Persaud, K.C.; Snyder, D.J. Artificial olfaction in the 21st century. IEEE Sens. J. 2021, 21, 12969–12990. [Google Scholar] [CrossRef]
- Van der Sar, I.G.; Wijbenga, N.; Nakshbandi, G.; Aerts, J.G.J.V.; Manintveld, O.C.; Wijsenbeek, M.S.; Hellemons, M.E.; Moor, C.C. The smell of lung disease: A review of the current status of electronic nose technology. Respir. Res. 2021, 22, 246. [Google Scholar] [CrossRef] [PubMed]
- Meng, S.; Li, Q.; Zhou, Z.; Li, H.; Liu, X.; Pan, S.; Li, M.; Wang, L.; Guo, Y.; Qiu, M.; et al. Assessment of an Exhaled Breath Test Using High-Pressure Photon Ionization Time-of-Flight Mass Spectrometry to Detect Lung Cancer. JAMA Netw. Open 2021, 4, e213486. [Google Scholar] [CrossRef]
- Chen, X.; Muhammad, K.G.; Madeeha, C.; Fu, W.; Xu, L.; Hu, Y.; Liu, J.; Ying, K.; Chen, L.; Yurievna, G.O. Calculated indices of volatile organic compounds (VOCs) in exhalation for lung cancer screening and early detection. Lung Cancer 2021, 154, 197–205. [Google Scholar] [CrossRef]
- Rai, S.N.; Das, S.; Pan, J.; Mishra, D.C.; Fu, X.A. Multigroup prediction in lung cancer patients and comparative controls using signature of volatile organic compounds in breath samples. PLoS ONE 2022, 17, e0277431. [Google Scholar] [CrossRef]
- Tsou, P.H.; Lin, Z.L.; Pan, Y.C.; Yang, H.C.; Chang, C.J.; Liang, S.K.; Wen, Y.F.; Chang, C.H.; Chang, L.Y.; Yu, K.L.; et al. Exploring Volatile Organic Compounds in Breath for High-Accuracy Prediction of Lung Cancer. Cancers 2021, 13, 1431. [Google Scholar] [CrossRef]
- Jia, Z.; Patra, A.; Kutty, V.K.; Venkatesan, T. Critical Review of Volatile Organic Compound Analysis in Breath and In Vitro Cell Culture for Detection of Lung Cancer. Metabolism 2019, 9, 52. [Google Scholar] [CrossRef] [PubMed]
- Hakim, M.; Broza, Y.Y.; Barash, O.; Peled, N.; Phillips, M.; Amann, A.; Haick, H. Volatile Organic Compounds of Lung Cancer and Possible Biochemical Pathways. Chem. Rev. 2012, 112, 5949–5966. [Google Scholar] [CrossRef]
- Ostrin, E.J.; Sidransky, D.; Spira, A.; Hanash, S.M. Biomarkers for Lung Cancer Screening and Detection. Cancer Epidemiol. Biomark. Prev. Publ. Am. Assoc. Cancer Res. Cosponsored Am. Soc. Prev. Oncol. 2020, 29, 2411–2415. [Google Scholar] [CrossRef]
| Sensitivity | Specificity | Positive Predictive Value (PPV) | Negative Predictive Value (NPV) | |
|---|---|---|---|---|
| EarlyCDT Lung | 54.6 (32.2–75.6) | 90.3 (89.6–91.1) | 2.0 (1.0–3.5) | 99.8 (99.7–99.9) |
| Nodify XL2 (Biodesix, Boulder, CO, USA) | 92 | 48 | 26 | 90 |
| MSC algorithm | 87 | 81 | 25 | 99 |
| Serum metabolites (GC/MS) | 100 | 95 | ||
| Tumor markers | ||||
| CEA + CA125 | 75.5 | 79.1 | 74.6 | 79.9 |
| CEA + CY211 | 76.1 | 71.8 | 68.7 | 78.8 |
| E-nose (LDA-Fuzzy 5-NN) | 91.58% [90.01%, 93.15%] | 91.72% [90.35%, 93.09%] | Not mentioned | Not mentioned |
| Volatile organic compounds | 100% | 93% | Not mentioned | Not mentioned |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boutsikou, E.; Hardavella, G.; Fili, E.; Bakiri, A.; Gaitanakis, S.; Kote, A.; Samitas, K.; Gkiozos, I. The Role of Biomarkers in Lung Cancer Screening. Cancers 2024, 16, 1980. https://doi.org/10.3390/cancers16111980
Boutsikou E, Hardavella G, Fili E, Bakiri A, Gaitanakis S, Kote A, Samitas K, Gkiozos I. The Role of Biomarkers in Lung Cancer Screening. Cancers. 2024; 16(11):1980. https://doi.org/10.3390/cancers16111980
Chicago/Turabian StyleBoutsikou, Efimia, Georgia Hardavella, Eleni Fili, Aikaterini Bakiri, Stylianos Gaitanakis, Alexandra Kote, Konstantinos Samitas, and Ioannis Gkiozos. 2024. "The Role of Biomarkers in Lung Cancer Screening" Cancers 16, no. 11: 1980. https://doi.org/10.3390/cancers16111980
APA StyleBoutsikou, E., Hardavella, G., Fili, E., Bakiri, A., Gaitanakis, S., Kote, A., Samitas, K., & Gkiozos, I. (2024). The Role of Biomarkers in Lung Cancer Screening. Cancers, 16(11), 1980. https://doi.org/10.3390/cancers16111980





