Revolutionizing Skin Cancer Triage: The Role of Patient-Initiated Teledermoscopy in Remote Diagnosis
Abstract
:Simple Summary
Abstract
1. Introduction
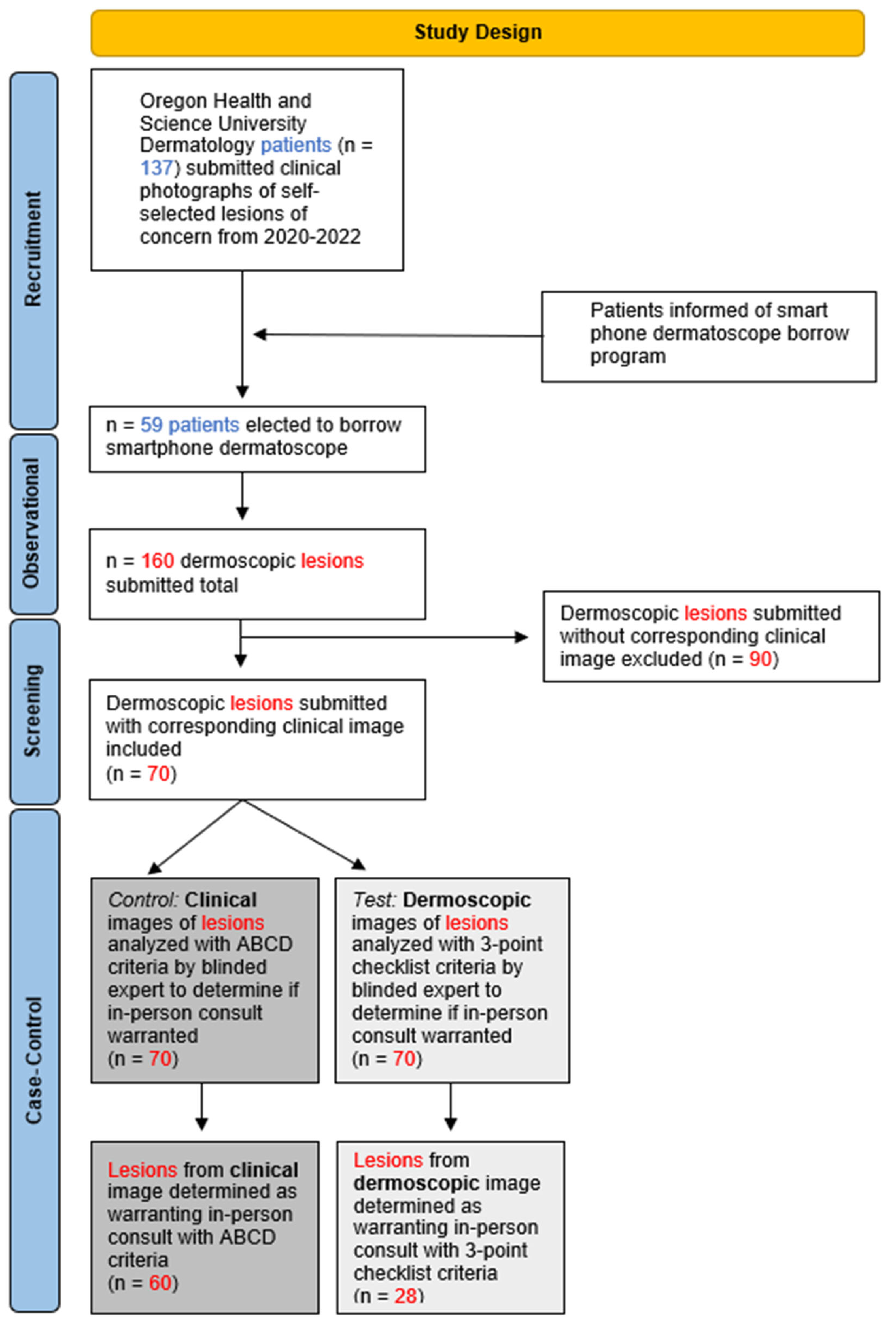
2. Materials and Methods
2.1. Study Design
2.2. Measures and Statistics
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Glazer, A.M.; Rigel, D.S. Analysis of Trends in Geographic Distribution of US Dermatology Workforce Density. JAMA Dermatol. 2017, 153, 472–473. [Google Scholar] [CrossRef]
- Sharma, A.; Jindal, V.; Singla, P.; Goldust, M.; Mhatre, M. Will teledermatology be the silver lining during and after COVID-19? Dermatol. Ther. 2020, 33, e13643. [Google Scholar] [CrossRef]
- Lee, C.; Witkowski, A.; Żychowska, M.; Ludzik, J. The role of mobile teledermoscopy in skin cancer triage and management during the COVID-19 pandemic. Indian J. Dermatol. Venereol. Leprol. 2023, 89, 347–352. [Google Scholar] [CrossRef]
- Phelan, D.L.; Oliveria, S.A.; Christos, P.J.; Dusza, S.W.; Halpern, A.C. Skin self-examination in patients at high risk for melanoma: A pilot study. Oncol. Nurs. Forum. 2003, 30, 1029–1036. [Google Scholar] [CrossRef] [PubMed]
- Dahlén Gyllencreutz, J.; Johansson Backman, E.; Terstappen, K.; Paoli, J. Teledermoscopy images acquired in primary health care and hospital settings—A comparative study of image quality. J. Eur. Acad. Dermatol. Venereol. 2018, 32, 1038–1043. [Google Scholar] [CrossRef]
- Kho, J.; Gillespie, N.; Horsham, C.; Snoswell, C.; Vagenas, D.; Soyer, H.P.; Janda, M. Skin Doctor Consultations Using Mobile Teledermoscopy: Exploring Virtual Care Business Models. Telemed. J. e-Health 2020, 26, 1406–1413. [Google Scholar] [CrossRef] [PubMed]
- Lowe, A.; Atwan, A.; Mills, C. Teledermoscopy as a community based diagnostic test in the era of COVID-19? Clin. Exp. Dermatol. 2021, 46, 173–174. [Google Scholar] [CrossRef]
- Bandic, J.; Kovacevic, S.; Karabeg, R.; Lazarov, A.; Opric, D. Teledermoscopy for Skin Cancer Prevention: A Comparative Study of Clinical and Teledermoscopic Diagnosis. Acta Inform. Med. 2020, 28, 37–41. [Google Scholar] [CrossRef] [PubMed]
- Ferrándiz, L.; Fernández-Orland, A.; Moreno-Ramírez, D. Finding the needle in the haystack is teledermoscopy’s task. J. Eur. Acad. Dermatol. Venereol. 2018, 32, e191–e192. [Google Scholar] [CrossRef]
- Blum, A.; Menzies, M. Home Dermoscopy During the COVID-19 Pandemic. Dermatol. Pract. Concept. 2020, 10, e2020091. [Google Scholar] [CrossRef]
- Manahan, M.N.; Soyer, H.P.; Loescher, L.J.; Horsham, C.; Vagenas, D.; Whiteman, D.C.; Olsen, C.M.; Janda, M. A pilot trial of mobile, patient-performed teledermoscopy. Br. J. Dermatol. 2015, 172, 1072–1080. [Google Scholar] [CrossRef] [PubMed]
- Ferrándiz, L.; Ojeda-Vila, T.; Corrales, A.; Martín-Gutiérrez, F.J.; Ruíz-de-Casas, A.; Galdeano, R.; Álvarez-Torralba, I.; Sánchez-Ibáñez, F.; Domínguez-Toro, J.M.; Encina, F.; et al. Internet-based skin cancer screening using clinical images alone or in conjunction with dermoscopic images: A randomized teledermoscopy trial. J. Am. Acad. Dermatol. 2017, 76, 676–682. [Google Scholar] [CrossRef] [PubMed]
- Barcaui, C.B.; Lima, P.M.O. Application of Teledermoscopy in the Diagnosis of Pigmented Lesions. Int. J. Telemed. Appl. 2018, 2018, 1624073. [Google Scholar] [CrossRef] [PubMed]
- Chuchu, N.; Dinnes, J.; Takwoingi, Y.; Matin, R.N.; Bayliss, S.E.; Davenport, C.; Moreau, J.F.; Bassett, O.; Godfrey, K.; O’Sullivan, C.; et al. Teledermatology for diagnosing skin cancer in adults. Cochrane Database Syst. Rev. 2018, 12, CD013193. [Google Scholar] [CrossRef] [PubMed]
- Uppal, S.K.; Beer, J.; Hadeler, E.; Gitlow, H.; Nouri, K. The clinical utility of teledermoscopy in the era of telemedicine. Dermatol. Ther. 2021, 34, e14766. [Google Scholar] [CrossRef] [PubMed]
- Horsham, C.; Snoswell, C.; Vagenas, D.; Loescher, L.J.; Gillespie, N.; Soyer, H.P.; Janda, M. Is Teledermoscopy Ready to Replace Face-to-Face Examinations for the Early Detection of Skin Cancer? Consumer Views, Technology Acceptance, and Satisfaction with Care. DRM 2020, 236, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Rossi, A.; Marghoob, A. Are patients capable and comfortable using mobile teledermoscopy? Br. J. Dermatol. 2016, 175, 1146. [Google Scholar] [CrossRef] [PubMed]
- Kong, F.; Horsham, C.; Rayner, J.; Simunovic, M.; O’Hara, M.; Soyer, H.P.; Janda, M. Consumer Preferences for Skin Cancer Screening Using Mobile Teledermoscopy: A Qualitative Study. DRM 2020, 236, 97–104. [Google Scholar] [CrossRef]
- Spinks, J.; Janda, M.; Soyer, H.P.; Whitty, J.A. Consumer preferences for teledermoscopy screening to detect melanoma early. J. Telemed. Telecare 2016, 22, 39–46. [Google Scholar] [CrossRef]
- Giavina Bianchi, M.; Santos, A.; Cordioli, E. Dermatologists’ perceptions on the utility and limitations of teledermatology after examining 55,000 lesions. J. Telemed. Telecare 2021, 27, 166–173. [Google Scholar] [CrossRef]
- De Bedout, V.; Williams, N.M.; Muñoz, A.M.; Londoño, A.M.; Munera, M.; Naranjo, N.; Rodriguez, L.M.; Toro, A.M.; Miao, F.; Koru-Sengul, T.; et al. Skin Cancer and Dermoscopy Training for Primary Care Physicians: A Pilot Study. Dermatol. Pract. Concept. 2021, 11, e2021145. [Google Scholar] [CrossRef] [PubMed]
- Van Sinderen, F.; Tensen, E.; van der Heijden, J.P.; Witkamp, L.; Jaspers, M.W.M.; Peute, L.W.P. Is Teledermoscopy Improving General Practitioner Skin Cancer Care? In MEDINFO 2019: Health and Wellbeing e-Networks for All; IOS Press: Amsterdam, The Netherlands, 2019; pp. 1795–1796. [Google Scholar] [CrossRef]
- Börve, A.; Dahlén Gyllencreutz, J.; Terstappen, K.; Johansson Backman, E.; Aldenbratt, A.; Danielsson, M.; Gillstedt, M.; Sandberg, C.; Paoli, J. Smartphone Teledermoscopy Referrals: A Novel Process for Improved Triage of Skin Cancer Patients. Acta Derm. Venerol. 2015, 95, 186–190. [Google Scholar] [CrossRef] [PubMed]
- Gilling, S.; Mortz, C.G.; Vestergaard, T. Patient Satisfaction and Expectations Regarding Mobile Teledermoscopy in General Practice for Diagnosis of Non-melanoma Skin Cancer and Malignant Melanoma. Acta Derm. Venereol. 2020, 100, adv00117. [Google Scholar] [CrossRef] [PubMed]
- Vestergaard, T.; Prasad, S.C.; Schuster, A.; Laurinaviciene, R.; Bygum, A.; Munck, A.; Andersen, M.K. Introducing teledermoscopy of possible skin cancers in general practice in Southern Denmark. Fam. Pract. 2020, 37, 513–518. [Google Scholar] [CrossRef] [PubMed]
- Petrie, T.; Samatham, R.; Witkowski, A.M.; Esteva, A.; Leachman, S.A. Melanoma Early Detection: Big Data, Bigger Picture. J. Investig. Dermatol. 2019, 139, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Sklip®. At-Home Dermoscopy. OHSU. Available online: https://www.ohsu.edu/war-on-melanoma/sklipr-home-dermoscopy#:~:text=OHSU%20is%20excited%20to%20offer,the%20best%20possible%20virtual%20care.&text=The%20Sklip%C2%AE%20is%20a,that%20attaches%20to%20your%20smartphone (accessed on 20 July 2022).
- Sklip At-Home Dermoscopy Guide. Available online: https://www.youtube.com/watch?v=bQLBThh6Uls&t=3s (accessed on 20 July 2022).
- American Academy of Dermatology Ad Hoc Task Force for the ABCDEs of Melanoma; Tsao, H.; Olazagasti, J.M.; Cordoro, K.M.; Brewer, J.D.; Taylor, S.C.; Bordeaux, J.S.; Chren, M.M.; Sober, A.J.; Tegeler, C.; et al. Early detection of melanoma: Reviewing the ABCDEs. J. Am. Acad. Dermatol. 2015, 72, 717–723. [Google Scholar] [CrossRef] [PubMed]
- Friedman, R.J.; Rigel, D.S. The clinical features of malignant melanoma. Dermatol. Clin. 1985, 3, 271–283. [Google Scholar] [CrossRef] [PubMed]
- Abbasi, N.R.; Shaw, H.M.; Rigel, D.S.; Friedman, R.J.; McCarthy, W.H.; Osman, I.; Kopf, A.W.; Polsky, D. Early diagnosis of cutaneous melanoma: Revisiting the ABCD criteria. JAMA 2004, 292, 2771–2776. [Google Scholar] [CrossRef] [PubMed]
- Soyer, H.P.; Argenziano, G.; Zalaudek, I.; Corona, R.; Sera, F.; Talamini, R.; Barbato, F.; Baroni, A.; Cicale, L.; Di Stefani, A.; et al. Three-point checklist of dermoscopy. A new screening method for early detection of melanoma. Dermatology 2004, 208, 27–31. [Google Scholar] [CrossRef]
- AAA. AAA Gas Prices. 2022. Available online: https://gasprices.aaa.com/ (accessed on 20 July 2022).
- U.S. Department of Energy. Alternative Fuels Data Center: Maps and Data. Available online: https://afdc.energy.gov/data (accessed on 20 July 2022).
- State of Oregon: Bureau of Labor and Industries. 2019. Available online: https://www.oregon.gov/BOLI/pages/index.aspx (accessed on 20 July 2022).
- Mehrotra, A. Opportunity costs of ambulatory medical care in the United States. Am. J. Manag. Care 2015, 21, 567–574. [Google Scholar]
- Fazil Jaber, N.; Jerkovic Gulin, S.; Seifert, O. Analysis of Teledermoscopy and Face-to-Face Examination of Atypical Pigmented Lesions: A Cross-Sectional, Retrospective Study. Dermatol. Pract. Concept. 2023, 13, e2023212. [Google Scholar] [CrossRef]
- Fan, W.; Mattson, G.; Twigg, A. Direct-to-Patient Mobile Teledermoscopy: Prospective Observational Study. JMIR Dermatol. 2024, 7, e52400. [Google Scholar] [CrossRef]
- Ingvar, J.; Nielsen, K.; Ingvar, Å. Factors for not performing total body skin examinations in primary care in association with teledermoscopy. BMC Prim. Care 2023, 24, 76. [Google Scholar] [CrossRef]
- Jones, L.K.; Oakley, A. Store-and-Forward Teledermatology for Assessing Skin Cancer in 2023: Literature Review. JMIR Dermatol. 2023, 6, e43395. [Google Scholar] [CrossRef]
- Gellatly, Z.S.; Lagha, I.B.; Ternov, N.K.; Berry, E.; Nelson, K.C.; Seiverling, E.V. The Role of Dermoscopy in Provider-to-Provider Store-and-Forward Dermatology eConsults: A Scoping Review of the Recent Literature. Curr. Dermatol. Rep. 2023, 12, 169–179. [Google Scholar] [CrossRef]
- Argenziano, G.; Puig, S.; Zalaudek, I.; Sera, F.; Corona, R.; Alsina, M.; Barbato, F.; Carrera, C.; Ferrara, G.; Guilabert, A.; et al. Dermoscopy improves accuracy of primary care physicians to triage lesions suggestive of skin cancer. J. Clin. Oncol. 2006, 24, 1877–1882. [Google Scholar] [CrossRef]
| Sample Characteristics | |||||
|---|---|---|---|---|---|
| Total number of participants submitting DDI | n = 59 | ||||
| Participant age (years) | |||||
| Mean | 46 | ||||
| Median | 42 | ||||
| ≥65 years | n = 13 | ||||
| ≤64 years | n = 46 | ||||
| Participant gender identity | |||||
| Male | 27% (n = 16) | ||||
| Female | 73% (n = 43) | ||||
| Participant distance from home to dermatology clinic * (miles) | |||||
| Mean | 22.6 | ||||
| Median | 8.8 | ||||
| Total number of lesions submitted with DDI | n = 160 | ||||
| DDI of individual lesion(s) submitted per participant | |||||
| 1 lesion 2 lesions 3 lesions 4 lesions 5 lesions 6 lesions >10 lesions Mean | n = 35 n = 11 n = 6 n = 1 n = 1 n = 1 n = 4 2.71 | ||||
| Median | 1 | ||||
| Lesions biopsied | 9% (n = 15) | ||||
| Malignant Benign Insufficient tissue for analysis | 20% (n = 3) 67% (n = 10) 13% (n = 2) | ||||
| DDI resulting in in-person consultation ** | 18% (n = 29) | ||||
| Retrospective Case-Control Outcomes | ||
|---|---|---|
| Total number of participants who submitted both DDI and clinical image | n = 46 | |
| Total number of lesions submitted with both DDI and clinical image | n = 70 | |
| Lesions meeting ABCD criteria from clinical image | 86% (n = 60) | |
| Lesions meeting D3PC criteria from DDI | 40% (n = 28) | |
| Opportunity Costs for the Average Patient in Oregon State visiting OHSU Dermatology | |
|---|---|
| Cost of one visit for average patient with Medicare * | 36.72 USD |
| Total gas expenditure per patient ((19.41 × 2) × 3.68)/25.7) | 5.56 USD |
| Average distance from sample population to dermatology clinic ** | 19.41 miles |
| Cost of gas per gallon, average between 2020 and 2022 [33] | 3.68 USD |
| Average miles per gallon for 2020 vehicle [34] | 25.7 miles |
| Total wages lost for time spent (12.75 × 2) | 25.50 USD |
| Minimum wage, Oregon state ‡ [35] | 12.75 USD/hour |
| Average total time spent per medical office visit [36] | 2 h |
| Total opportunity cost estimated on average | $67.78 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Foltz, E.A.; Ludzik, J.; Leachman, S.; Stoos, E.; Greiling, T.; Teske, N.; Clayton, L.; Becker, A.L.; Witkowski, A. Revolutionizing Skin Cancer Triage: The Role of Patient-Initiated Teledermoscopy in Remote Diagnosis. Cancers 2024, 16, 2565. https://doi.org/10.3390/cancers16142565
Foltz EA, Ludzik J, Leachman S, Stoos E, Greiling T, Teske N, Clayton L, Becker AL, Witkowski A. Revolutionizing Skin Cancer Triage: The Role of Patient-Initiated Teledermoscopy in Remote Diagnosis. Cancers. 2024; 16(14):2565. https://doi.org/10.3390/cancers16142565
Chicago/Turabian StyleFoltz, Emilie A., Joanna Ludzik, Sancy Leachman, Elizabeth Stoos, Teri Greiling, Noelle Teske, Lara Clayton, Alyssa L. Becker, and Alexander Witkowski. 2024. "Revolutionizing Skin Cancer Triage: The Role of Patient-Initiated Teledermoscopy in Remote Diagnosis" Cancers 16, no. 14: 2565. https://doi.org/10.3390/cancers16142565
APA StyleFoltz, E. A., Ludzik, J., Leachman, S., Stoos, E., Greiling, T., Teske, N., Clayton, L., Becker, A. L., & Witkowski, A. (2024). Revolutionizing Skin Cancer Triage: The Role of Patient-Initiated Teledermoscopy in Remote Diagnosis. Cancers, 16(14), 2565. https://doi.org/10.3390/cancers16142565





