Lck Function and Modulation: Immune Cytotoxic Response and Tumor Treatment More Than a Simple Event
Abstract
:Simple Summary
Abstract
1. Introduction
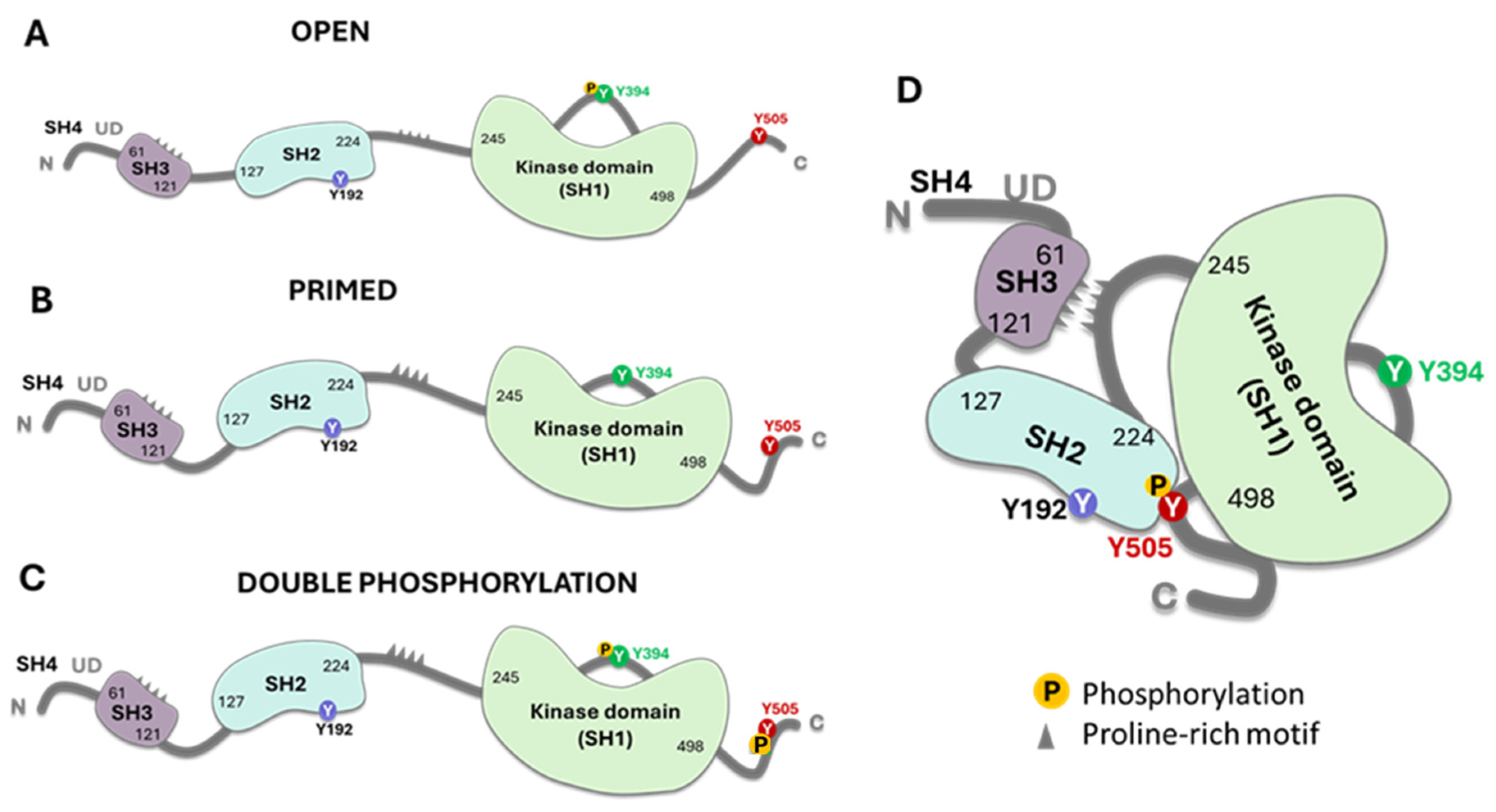
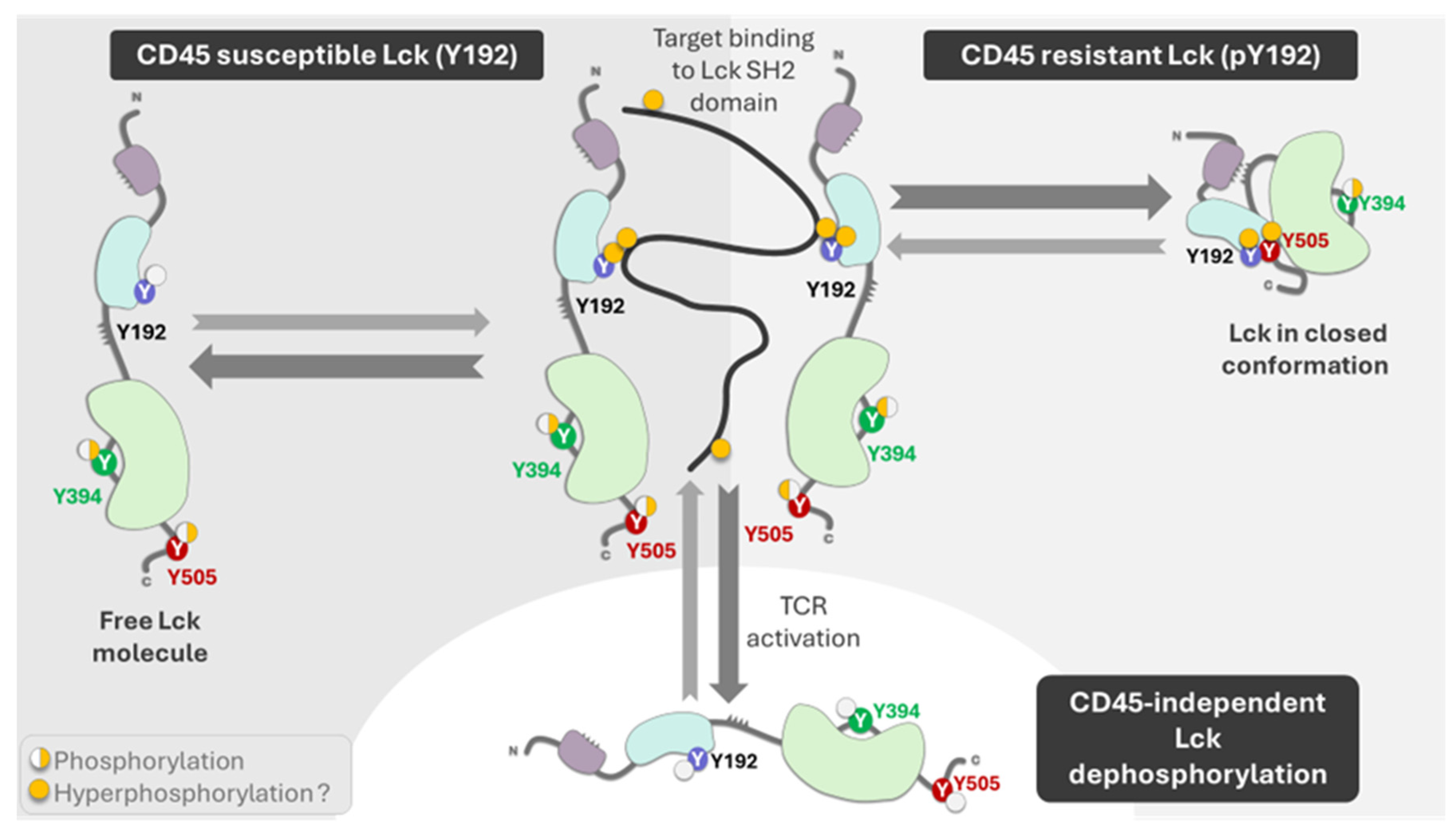
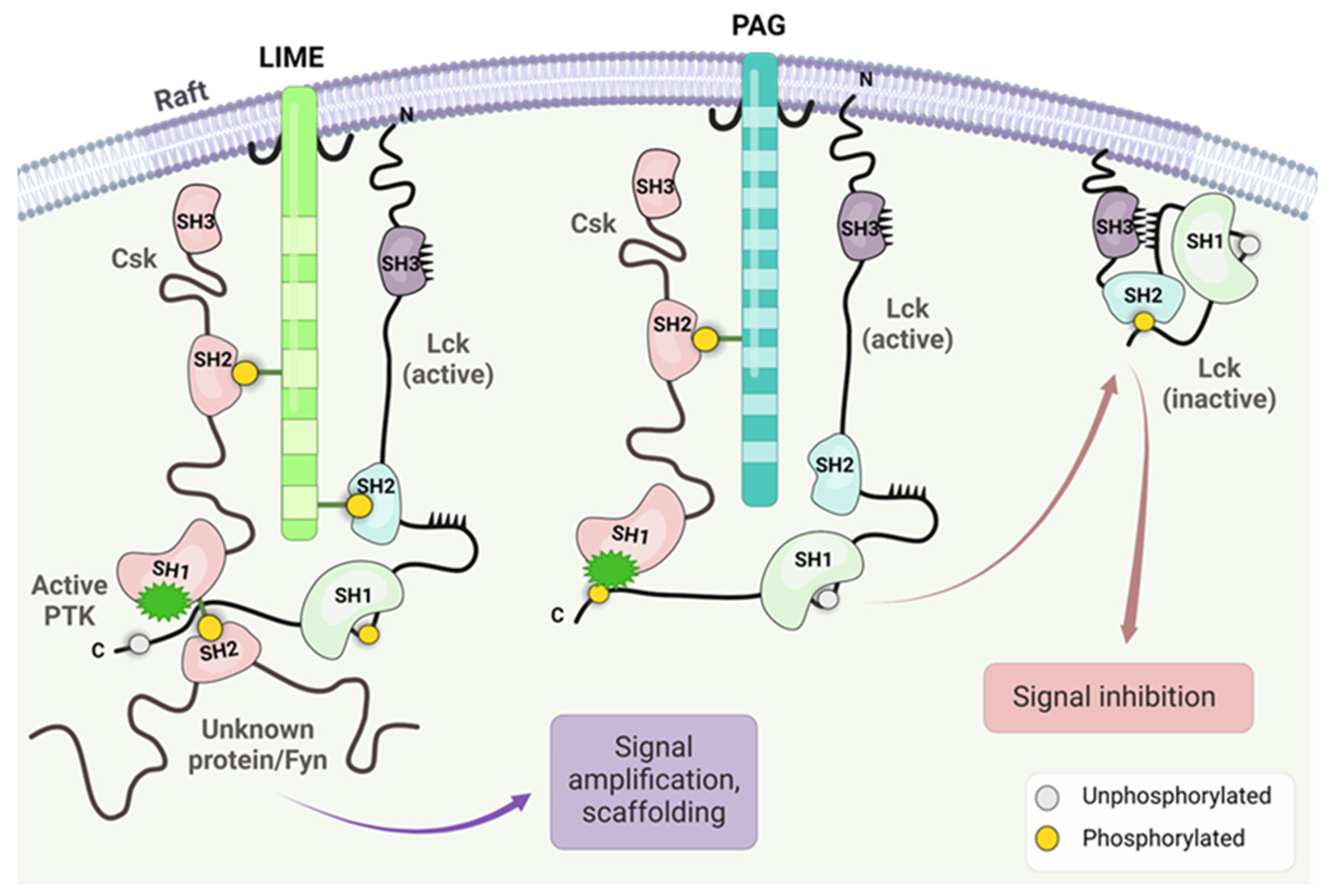
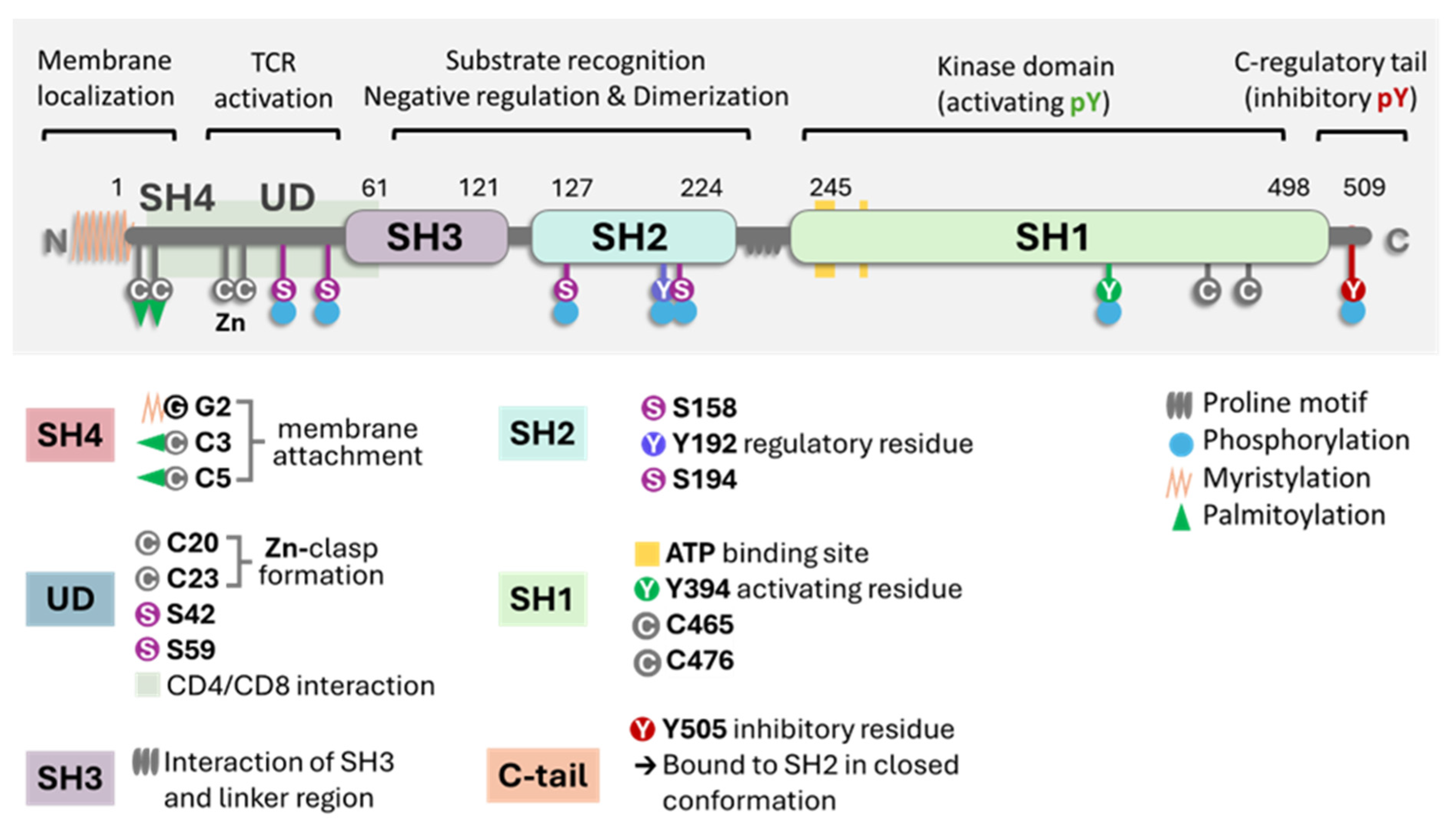
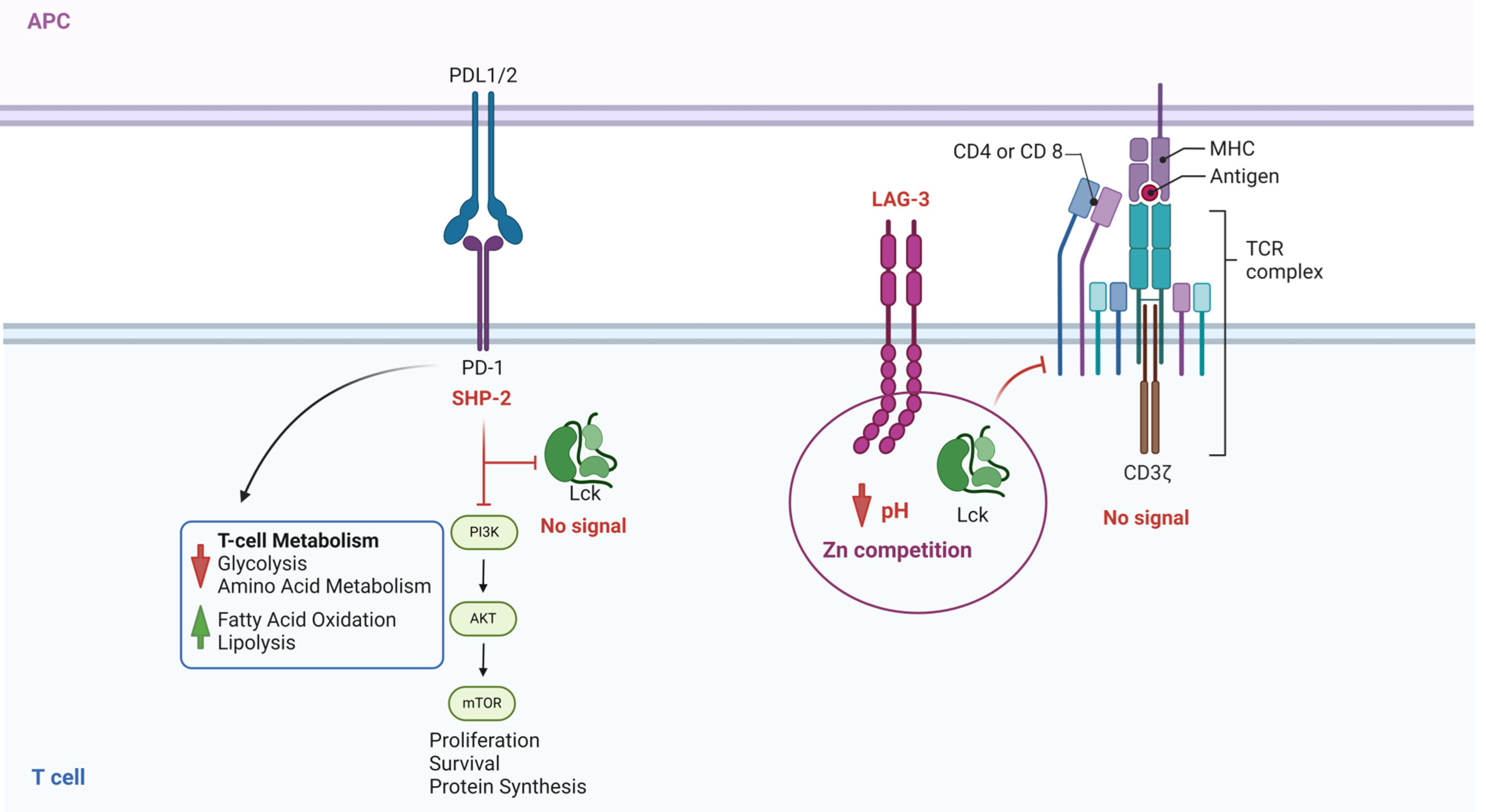
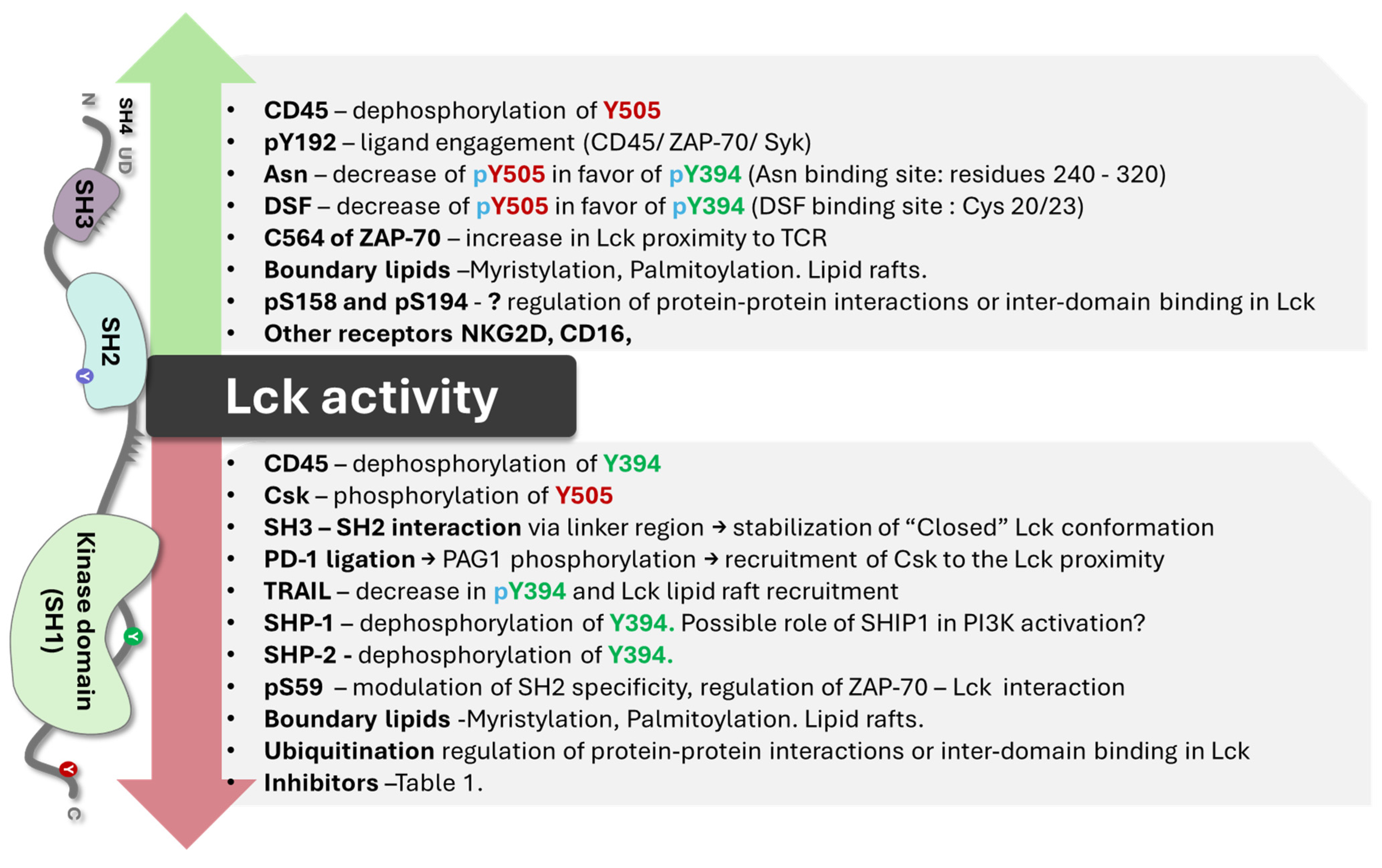
2. Key Biochemical Elements of Enzyme Activity

3. CAR T Cells and Lck Signaling
4. Lck Genetic Analysis
5. Pharmacological Modulation of Lck Activity
6. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- P06239·LCK_Human. Available online: https://www.uniprot.org/uniprotkb/P06239/entry (accessed on 9 June 2024).
- Serfas, M.S.; Tyner, A.L. BRK, SRM, FRK, and SRC42A form a distinct family of intracellular SRC-Like tyrosine kinases. Oncol. Res. Featur. Preclin. Clin. Cancer Ther. 2003, 13, 409–419. [Google Scholar] [CrossRef] [PubMed]
- Parsons, S.J.; Parsons, J.T. Src family kinases, key regulators of signal transduction. Oncogene 2004, 23, 7906–7909. [Google Scholar] [CrossRef] [PubMed]
- Palacios, E.H.; Weiss, A. Function of the Src-family kinases, Lck and Fyn, in T-cell development and activation. Oncogene 2004, 23, 7990–8000. [Google Scholar] [CrossRef] [PubMed]
- Levin, S.E.; Weiss, A. Non-Receptor Tyrosine Kinases in T Cell Antigen Receptor Function. In Handbook of Cell Signaling, 2nd ed.; Bradshaw, R.A., Dennis, E.A., Eds.; Chapter 68; Academic Press: Cambridge, MA, USA, 2009; pp. 507–516. [Google Scholar] [CrossRef]
- Clarke, C.N.; Lee, M.S.; Wei, W.; Manyam, G.; Jiang, Z.-Q.; Lu, Y.; Morris, J.; Broom, B.; Menter, D.; Vilar-Sanchez, E.; et al. Proteomic Features of Colorectal Cancer Identify Tumor Subtypes Independent of Oncogenic Mutations and Independently Predict Relapse-Free Survival. Ann. Surg. Oncol. 2017, 24, 4051–4058. [Google Scholar] [CrossRef] [PubMed]
- Janikowska, G.; Janikowski, T.; Pyka-Pająk, A.; Mazurek, U.; Janikowski, M.; Gonciarz, M.; Lorenc, Z. Potential Biomarkers for the Early Diagnosis of Colorectal Adenocarcinoma—Transcriptomic Analysis of Four Clinical Stages. Cancer Biomark. 2018, 22, 89–99. [Google Scholar] [CrossRef] [PubMed]
- Bommhardt, U.; Schraven, B.; Simeoni, L. Beyond TCR Signaling: Emerging Functions of Lck in Cancer and Immunotherapy. Int. J. Mol. Sci. 2019, 20, 3500. [Google Scholar] [CrossRef] [PubMed]
- Chakraborty, G.; Rangaswami, H.; Jain, S.; Kundu, G.C. Hypoxia Regulates Cross-talk between Syk and Lck Leading to Breast Cancer Progression and Angiogenesis. J. Biol. Chem. 2006, 281, 11322–11331. [Google Scholar] [CrossRef] [PubMed]
- Köster, A.; Landgraf, S.; Leipold, A.; Sachse, R.; Gebhart, E.; Tulusan, A.H.; Rónay, G.; Schmidt, C.; Dingermann, T. Expression of Oncogenes in Human Breast Cancer Specimens. Anticancer Res. 1991, 11, 193–201. [Google Scholar] [PubMed]
- Rupniewska, E.; Roy, R.; Mauri, F.A.; Liu, X.; Kaliszczak, M.; Bellezza, G.; Cagini, L.; Barbareschi, M.; Ferrero, S.; Tommasi, A.M.; et al. Targeting Autophagy Sensitises Lung Cancer Cells to Src Family Kinase Inhibitors. Oncotarget 2018, 9, 27346–27362. [Google Scholar] [CrossRef]
- Sugihara, T.; Werneburg, N.W.; Hernandez, M.C.; Yang, L.; Kabashima, A.; Hirsova, P.; Yohanathan, L.; Sosa, C.; Truty, M.J.; Vasmatzis, G.; et al. YAP Tyrosine Phosphorylation and Nuclear Localization in Cholangiocarcinoma Cells Are Regulated by LCK and Independent of LATS Activity. Mol. Cancer Res. 2018, 16, 1556–1567. [Google Scholar] [CrossRef] [PubMed]
- Zepecki, J.P.; Snyder, K.M.; Moreno, M.M.; Fajardo, E.; Fiser, A.; Ness, J.; Sarkar, A.; Toms, S.A.; Tapinos, N. Regulation of Human Glioma Cell Migration, Tumor Growth, and Stemness Gene Expression Using a Lck Targeted Inhibitor. Oncogene 2018, 38, 1734–1750. [Google Scholar] [CrossRef] [PubMed]
- The Cancer Genome Atlas Network. Genomic Classification of Cutaneous Melanoma. Cell 2015, 161, 1681–1696. [Google Scholar] [CrossRef] [PubMed]
- Creeden, J.F.; Alganem, K.; Imami, A.S.; Henkel, N.D.; Brunicardi, F.C.; Liu, S.-H.; Shukla, R.; Tomar, T.; Naji, F.; McCullumsmith, R.E. Emerging Kinase Therapeutic Targets in Pancreatic Ductal Adenocarcinoma and Pancreatic Cancer Desmoplasia. Int. J. Mol. Sci. 2020, 21, 8823. [Google Scholar] [CrossRef] [PubMed]
- Filipp, D.; Ballek, O.; Manning, J. Lck, Membrane Microdomains, and TCR Triggering Machinery: Defining the New Rules of Engagement. Front. Immunol. 2012, 3, 23330. [Google Scholar] [CrossRef] [PubMed]
- Shah, K.; Al-Haidari, A.; Sun, J.; Kazi, J.U. T cell receptor (TCR) signaling in health and disease. Signal Transduct. Target. Ther. 2021, 6, 412. [Google Scholar] [CrossRef] [PubMed]
- Porciello, N.; Cipria, D.; Masi, G.; Lanz, A.-L.; Milanetti, E.; Grottesi, A.; Howie, D.; Cobbold, S.P.; Schermelleh, L.; He, H.-T.; et al. Role of the membrane anchor in the regulation of Lck activity. J. Biol. Chem. 2022, 298, 102663. [Google Scholar] [CrossRef] [PubMed]
- Kocyła, A.M.; Czogalla, A.; Wessels, I.; Rink, L.; Krężel, A. A combined biochemical and cellular approach reveals Zn2+-dependent hetero- and homodimeric CD4 and Lck assemblies in T cells. Structure 2024, 32, 292–303.e7. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Li, Y.; Wu, L. Protein S-palmitoylation modification: Implications in tumor and tumor immune microenvironment. Front. Immunol. 2024, 15, 1337478. [Google Scholar] [CrossRef] [PubMed]
- Gauthaman, A.; Jacob, R.; Pasupati, S.; Rajadurai, A.; Doss, C.G.P.; Moorthy, A. Novel peptide—Based inhibitor for targeted inhibition of T cell function. J. Cell Commun. Signal. 2021, 16, 349–359. [Google Scholar] [CrossRef] [PubMed]
- Tate, E.W.; Soday, L.; de la Lastra, A.L.; Wang, M.; Lin, H. Protein lipidation in cancer: Mechanisms, dysregulation and emerging drug targets. Nat. Rev. Cancer 2024, 24, 240–260. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.; Bai, Y.; Xiong, Y.; Zhang, J.; Chen, S.; Zheng, X.; Meng, X.; Li, L.; Wang, J.; Xu, C.; et al. Potentiating the antitumour response of CD8+ T cells by modulating cholesterol metabolism. Nature 2016, 531, 651–655. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Bi, E.; Lu, Y.; Su, P.; Huang, C.; Liu, L.; Wang, Q.; Yang, M.; Kalady, M.F.; Qian, J.; et al. Cholesterol Induces CD8+ T Cell Exhaustion in the Tumor Microenvironment. Cell Metab. 2019, 30, 143–156.e5. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Cao, Y.; Shen, L.; Xiao, T.; Cao, R.; Wei, S.; Tang, M.; Du, L.; Wu, H.; Wu, B.; et al. Regulation of PD-L1 through direct binding of cholesterol to CRAC motifs. Sci. Adv. 2022, 8, eabq4722. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.; Zhang, X.; Chen, X.; Aramsangtienchai, P.; Tong, Z.; Lin, H. Protein Lipidation: Occurrence, Mechanisms, Biological Functions, and Enabling Technologies. Chem. Rev. 2018, 118, 919–988. [Google Scholar] [CrossRef] [PubMed]
- Sitaram, P.; Uyemura, B.; Malarkannan, S.; Riese, M.J. Beyond the Cell Surface: Targeting Intracellular Negative Regulators to Enhance T cell Anti-Tumor Activity. Int. J. Mol. Sci. 2019, 20, 5821. [Google Scholar] [CrossRef] [PubMed]
- Sheng, R.; Jung, D.-J.; Silkov, A.; Kim, H.; Singaram, I.; Wang, Z.-G.; Xin, Y.; Kim, E.; Park, M.-J.; Thiagarajan-Rosenkranz, P.; et al. Lipids Regulate Lck Protein Activity through Their Interactions with the Lck Src Homology 2 Domain. J. Biol. Chem. 2016, 291, 17639–17650. [Google Scholar] [CrossRef] [PubMed]
- Kabouridis, P.S.; Janzen, J.; Magee, A.L.; Ley, S.C. Cholesterol depletion disrupts lipid rafts and modulates the activity of multiple signaling pathways in T lymphocytes. Eur. J. Immunol. 2000, 30, 954–963. [Google Scholar] [CrossRef] [PubMed]
- Tripathi, S.; Gupta, E.; Galande, S. Statins as anti-tumor agents: A paradigm for repurposed drugs. Cancer Rep. 2024, 7, e2078. [Google Scholar] [CrossRef] [PubMed]
- Chamani, S.; Kooshkaki, O.; Moossavi, M.; Rastegar, M.; Soflaei, S.S.; McCloskey, A.P.; Banach, M.; Sahebkar, A. The effects of statins on the function and differentiation of blood cells. Arch. Med. Sci. 2022, 19, 1314–1326. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, D.J.; Haslam, A.; Prasad, V. Cardiovascular/anti-inflammatory drugs repurposed for treating or preventing cancer: A systematic review and meta-analysis of randomized trials. Cancer Med. 2024, 13, e7049. [Google Scholar] [CrossRef] [PubMed]
- Mariuzza, R.A.; Shahid, S.; Karade, S.S. The immune checkpoint receptor LAG3: Structure, function, and target for cancer immunotherapy. J. Biol. Chem. 2024, 300, 107241. [Google Scholar] [CrossRef] [PubMed]
- Nika, K.; Soldani, C.; Salek, M.; Paster, W.; Gray, A.; Etzensperger, R.; Fugger, L.; Polzella, P.; Cerundolo, V.; Dushek, O.; et al. Constitutively active Lck kinase in T cells drives antigen receptor signal transduction. Immunity 2010, 32, 766–777. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Aguilar, L.M.; Vico-Barranco, I.; Arbulo-Echevarria, M.M.; Aguado, E. A Story of Kinases and Adaptors: The Role of Lck, ZAP-70 and LAT in Switch Panel Governing T-Cell Development and Activation. Biology 2023, 12, 1163. [Google Scholar] [CrossRef] [PubMed]
- Bozso, S.J.; Kang, J.J.H.; Nagendran, J. The role of competing mechanisms on Lck regulation. Immunol. Res. 2020, 68, 289–295. [Google Scholar] [CrossRef] [PubMed]
- Kesavan, K.P.; Isaacson, C.C.; Ashendel, C.L.; Geahlen, R.L.; Harrison, M.L. Characterization of the in vivo sites of serine phosphorylation on Lck identifying serine 59 as a site of mitotic phosphorylation. J. Biol. Chem. 2002, 277, 14666–14673. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Li, G.; Li, L.; Li, D.; Dong, Z.; Jiang, P. Asparagine enhances LCK signalling to potentiate CD8+ T-cell activation and anti-tumour responses. Nat. Cell Biol. 2021, 23, 75–86. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Zhu, T.; Miao, N.; Qu, Y.; Wang, Z.; Chao, Y.; Wang, J.; Wu, W.; Xu, X.; Xu, C.; et al. Disulfiram bolsters T-cell anti-tumor immunity through direct activation of LCK-mediated TCR signaling. EMBO J. 2022, 41, e110636. [Google Scholar] [CrossRef] [PubMed]
- Rheinländer, A.; Schraven, B.; Bommhardt, U. CD45 in human physiology and clinical medicine. Immunol. Lett. 2018, 196, 22–32. [Google Scholar] [CrossRef] [PubMed]
- Inderberg, E.M.; Mensali, N.; Oksvold, M.P.; Fallang, L.-E.; Fåne, A.; Skorstad, G.; Stenvik, G.-E.; Progida, C.; Bakke, O.; Kvalheim, G.; et al. Human c-SRC kinase (CSK) overexpression makes T cells dummy. Cancer Immunol. Immunother. 2017, 67, 525–536. [Google Scholar] [CrossRef]
- Zhu, S.; Wang, H.; Ranjan, K.; Zhang, D. Regulation, targets and functions of CSK. Front. Cell Dev. Biol. 2023, 11, 1206539. [Google Scholar] [CrossRef] [PubMed]
- Hui, E.; Vale, R.D. In vitro membrane reconstitution of the T-cell receptor proximal signaling network. Nat. Struct. Mol. Biol. 2014, 21, 133–142. [Google Scholar] [CrossRef] [PubMed]
- Kästle, M.; Merten, C.; Hartig, R.; Kaehne, T.; Liaunardy-Jopeace, A.; Woessner, N.M.; Schamel, W.W.; James, J.; Minguet, S.; Simeoni, L.; et al. Tyrosine 192 within the SH2 domain of the Src-protein tyrosine kinase p56Lck regulates T-cell activation independently of Lck/CD45 interactions. Cell Commun. Signal. 2020, 18, 183. [Google Scholar] [CrossRef] [PubMed]
- Courtney, A.H.; Amacher, J.F.; Kadlecek, T.A.; Mollenauer, M.N.; Au-Yeung, B.B.; Kuriyan, J.; Weiss, A. A Phosphosite within the SH2 Domain of Lck Regulates Its Activation by CD45. Mol. Cell 2017, 67, 498–511.e6. [Google Scholar] [CrossRef] [PubMed]
- Kästle, M.; Merten, C.; Hartig, R.; Plaza-Sirvent, C.; Schmitz, I.; Bommhardt, U.; Schraven, B.; Simeoni, L. Y192 within the SH2 Domain of Lck Regulates TCR Signaling Downstream of PLC-γ1 and Thymic Selection. Int. J. Mol. Sci. 2022, 23, 7271. [Google Scholar] [CrossRef] [PubMed]
- Prakaash, D.; Fagnen, C.; Cook, G.P.; Acuto, O.; Kalli, A.C. Molecular dynamics simulations reveal membrane lipid interactions of the full-length lymphocyte specific kinase (Lck). Sci. Rep. 2022, 12, 21121. [Google Scholar] [CrossRef] [PubMed]
- Brian, B.F.; Sjaastad, F.V.; Freedman, T.S. SH3-domain mutations selectively disrupt Csk homodimerization or PTPN22 binding. Sci. Rep. 2022, 12, 5875. [Google Scholar] [CrossRef]
- Okada, M. Regulation of the Src Family Kinases by Csk. Int. J. Biol. Sci. 2012, 8, 1385–1397. [Google Scholar] [CrossRef] [PubMed]
- Hur, E.M.; Son, M.; Lee, O.-H.; Choi, Y.B.; Park, C.; Lee, H.; Yun, Y. LIME, a novel transmembrane adaptor protein, associates with p56lck and mediates T cell activation. J. Exp. Med. 2003, 198, 1463–1473. [Google Scholar] [CrossRef] [PubMed]
- Ventimiglia, L.N.; Alonso, M.A. The role of membrane rafts in Lck transport, regulation and signalling in T-cells. Biochem. J. 2013, 454, 169–179. [Google Scholar] [CrossRef] [PubMed]
- Strazza, M.; Azoulay-Alfaguter, I.; Peled, M.; Adam, K.; Mor, A. Transmembrane adaptor protein PAG is a mediator of PD-1 inhibitory signaling in human T cells. Commun. Biol. 2021, 4, 672. [Google Scholar] [CrossRef] [PubMed]
- Borowicz, P.; Sundvold, V.; Chan, H.; Abrahamsen, G.; Kjelstrup, H.; Nyman, T.A.; Spurkland, A. Tyr192 Regulates Lymphocyte-Specific Tyrosine Kinase Activity in T Cells. J. Immunol. 2021, 207, 1128–1137. [Google Scholar] [CrossRef]
- Schultz, A.; Schnurra, M.; El-Bizri, A.; Woessner, N.M.; Hartmann, S.; Hartig, R.; Minguet, S.; Schraven, B.; Simeoni, L. A Cysteine Residue within the Kinase Domain of Zap70 Regulates Lck Activity and Proximal TCR Signaling. Cells 2022, 11, 2723. [Google Scholar] [CrossRef] [PubMed]
- Feng, S.; Cheng, X.; Zhang, L.; Lu, X.; Chaudhary, S.; Teng, R.; Frederickson, C.; Champion, M.M.; Zhao, R.; Cheng, L.; et al. Myeloid-derived suppressor cells inhibit T cell activation through nitrating LCK in mouse cancers. Proc. Natl. Acad. Sci. USA 2018, 115, 10094–10099. [Google Scholar] [CrossRef] [PubMed]
- Mohanasundaram, K.A.; Haworth, N.L.; Grover, M.P.; Crowley, T.M.; Goscinski, A.; Wouters, M.A. Potential role of glutathione in evolution of thiol-based redox signaling sites in proteins. Front. Pharmacol. 2015, 6, 1. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, K.; Hori, T.; Yodoi, J. Alternative binding of p56lck and phosphatidylinositol 3-kinase in T cells by sulfhydryl oxidation: Implication of aberrant signaling due to oxidative stress in T lymphocytes. Mol. Immunol. 1996, 33, 855–865. [Google Scholar] [CrossRef] [PubMed]
- Lasser, S.A.; Kurt, F.G.O.; Arkhypov, I.; Utikal, J.; Umansky, V. Myeloid-derived suppressor cells in cancer and cancer therapy. Nat. Rev. Clin. Oncol. 2024, 21, 147–164. [Google Scholar] [CrossRef] [PubMed]
- Rudd, C.E. How the Discovery of the CD4/CD8-p56lck Complexes Changed Immunology and Immunotherapy. Front. Cell Dev. Biol. 2021, 9, 626095. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.; Ye, L. Bound to be perfect: Lck and T cell co-receptors. Nat. Immunol. 2023, 24, 5–7. [Google Scholar] [CrossRef] [PubMed]
- Horkova, V.; Drobek, A.; Mueller, D.; Gubser, C.; Niederlova, V.; Wyss, L.; King, C.G.; Zehn, D.; Stepanek, O. Dynamics of the Coreceptor-LCK Interactions during T Cell Development Shape the Self-Reactivity of Peripheral CD4 and CD8 T Cells. Cell Rep. 2020, 30, 1504–1514.e7. [Google Scholar] [CrossRef]
- Qin, Z.; Hou, P.; Lin, H.; Chen, M.; Wang, R.; Xu, T. Inhibition of Lck/Fyn kinase activity promotes the differentiation of induced Treg cells through AKT/mTOR pathway. Int. Immunopharmacol. 2024, 134, 112237. [Google Scholar] [CrossRef] [PubMed]
- Le Page, A.; Dupuis, G.; Larbi, A.; Witkowski, J.M.; Fülöp, T. Signal transduction changes in CD4 + and CD8 + T cell subpopulations with aging. Exp. Gerontol. 2018, 105, 128–139. [Google Scholar] [CrossRef]
- Tedeschi, V.; Paldino, G.; Kunkl, M.; Paroli, M.; Sorrentino, R.; Tuosto, L.; Fiorillo, M.T. CD8+ T Cell Senescence: Lights and Shadows in Viral Infections, Autoimmune Disorders and Cancer. Int. J. Mol. Sci. 2022, 23, 3374. [Google Scholar] [CrossRef] [PubMed]
- Braga, F.A.V.; Hertoghs, K.M.L.; van Lier, R.A.; van Gisbergen, K.P.J.M. Molecular characterization of HCMV-specific immune responses: Parallels between CD8+ T cells, CD4+ T cells, and NK cells. Eur. J. Immunol. 2015, 45, 2433–2445. [Google Scholar] [CrossRef]
- Esensten, J.H.; Helou, Y.A.; Chopra, G.; Weiss, A.; Bluestone, J.A. CD28 Costimulation: From Mechanism to Therapy. Immunity 2016, 44, 973–988. [Google Scholar] [CrossRef] [PubMed]
- Paprckova, D.; Niederlova, V.; Moudra, A.; Drobek, A.; Pribikova, M.; Janusova, S.; Schober, K.; Neuwirth, A.; Michalik, J.; Huranova, M.; et al. Self-reactivity of CD8 T-cell clones determines their differentiation status rather than their responsiveness in infections. Front. Immunol. 2022, 13, 1009198. [Google Scholar] [CrossRef] [PubMed]
- Kwon, J.; Devadas, S.; Williams, M. T Cell Receptor-Stimulated Generation of Hydrogen Peroxide Inhibits MEK-ERK Activation and Lck Serine Phosphorylation. Free. Radic. Biol. Med. 2003, 35, 406–417. [Google Scholar] [CrossRef] [PubMed]
- Franklin, R.A.; Atherfold, P.A.; McCubrey, J.A. Calcium-Induced ERK Activation in Human T Lymphocytes Occurs via P56(Lck) and CaM-Kinase. Mol. Immunol. 2000, 37, 675–683. [Google Scholar] [CrossRef]
- Rodriguez-Rodriguez, C.; González-Mancha, N.; Ochoa-Echeverría, A.; Mérida, I. Sorting Nexin 27-dependent regulation of Lck and CD4 tunes the initial stages of T-cell activation. J. Leukoc. Biol. 2024, qiae086, advance online publication. [Google Scholar] [CrossRef]
- Trefny, M.P.; Kirchhammer, N.; der Maur, P.A.; Natoli, M.; Schmid, D.; Germann, M.; Rodriguez, L.F.; Herzig, P.; Lötscher, J.; Akrami, M.; et al. Deletion of SNX9 alleviates CD8 T cell exhaustion for effective cellular cancer immunotherapy. Nat. Commun. 2023, 14, 86. [Google Scholar] [CrossRef] [PubMed]
- Overduin, M.; Bhat, R. Recognition and remodeling of endosomal zones by sorting nexins. Biochim. Biophys. Acta (BBA)-Biomembr. 2024, 1866, 184305. [Google Scholar] [CrossRef] [PubMed]
- Rao, N.; Miyake, S.; Reddi, A.L.; Douillard, P.; Ghosh, A.K.; Dodge, I.L.; Zhou, P.; Fernandes, N.D.; Band, H. Negative regulation of Lck by Cbl ubiquitin ligase. Proc. Natl. Acad. Sci. USA 2002, 99, 3794–3799. [Google Scholar] [CrossRef] [PubMed]
- Kashiwakura, J.I.; Oritani, K.; Matsuda, T. The Functional Properties and Physiological Roles of Signal-Transducing Adaptor Protein-2 in the Pathogenesis of Inflammatory and Immune Disorders. Biomedicines 2022, 10, 3079. [Google Scholar] [CrossRef] [PubMed]
- Shao, Y.; Elly, C.; Liu, Y. Negative regulation of Rap1 activation by the Cbl E3 ubiquitin ligase. EMBO Rep. 2003, 4, 425–431. [Google Scholar] [CrossRef] [PubMed]
- Jeon, M.-S.; Atfield, A.; Venuprasad, K.; Krawczyk, C.; Sarao, R.; Elly, C.; Yang, C.; Arya, S.; Bachmaier, K.; Su, L.; et al. Essential role of the E3 ubiquitin ligase Cbl-b in T cell anergy induction. Immunity 2004, 21, 167–177. [Google Scholar] [CrossRef] [PubMed]
- Matalon, O.; Fried, S.; Ben-Shmuel, A.; Pauker, M.H.; Joseph, N.; Keizer, D.; Piterburg, M.; Barda-Saad, M. Dephosphorylation of the adaptor LAT and phospholipase C-γ by SHP-1 inhibits natural killer cell cytotoxicity. Sci Signal. 2016, 9, ra54. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.; Strasser, A.; Green, D.R.; Latz, E.; Mantovani, A.; Melino, G. Legacy of the discovery of the T-cell receptor: 40 years of shaping basic immunology and translational work to develop novel therapies. Cell Mol. Immunol. 2024, 21, 790–797. [Google Scholar] [CrossRef] [PubMed]
- Augustin, R.C.; Bao, R.; Luke, J.J. Targeting Cbl-b in cancer immunotherapy. J. Immunother. Cancer 2023, 11, e006007. [Google Scholar] [CrossRef] [PubMed]
- Yu; Cooper, J. C.; Shi, M.; Chueh, F.-Y.; Venkitachalam, S.; Yu, C.-L. Enforced SOCS1 and SOCS3 expression attenuates Lck-mediated cellular transformation. Int. J. Oncol. 2010, 36, 1201–1208. [Google Scholar] [CrossRef]
- Shih, Y.-C.; Chen, H.-F.; Wu, C.-Y.; Ciou, Y.-R.; Wang, C.-W.; Chuang, H.-C.; Tan, T.-H. The phosphatase DUSP22 inhibits UBR2-mediated K63-ubiquitination and activation of Lck downstream of TCR signalling. Nat. Commun. 2024, 15, 532. [Google Scholar] [CrossRef] [PubMed]
- Jury, E.C.; Kabouridis, P.S.; Abba, A.; Mageed, R.A.; Isenberg, D.A. Increased ubiquitination and reduced expression of LCK in T lymphocytes from patients with systemic lupus erythematosus. Arthritis Rheum. 2003, 48, 1343–1354. [Google Scholar] [CrossRef]
- Huang, L.; Zhu, P.; Xia, P.; Fan, Z. WASH has a critical role in NK cell cytotoxicity through Lck-mediated phosphorylation. Cell Death Dis. 2016, 7, e2301. [Google Scholar] [CrossRef] [PubMed]
- Moore, E.K.; Strazza, M.; Mor, A. Combination Approaches to Target PD-1 Signaling in Cancer. Front. Immunol. 2022, 13, 927265. [Google Scholar] [CrossRef]
- Chiang, G.G.; Sefton, B.M. Specific Dephosphorylation of the Lck Tyrosine Protein Kinase at Tyr-394 by the SHP-1 Protein-tyrosine Phosphatase. J. Biol. Chem. 2001, 276, 23173–23178. [Google Scholar] [CrossRef] [PubMed]
- Baldanzi, G. Immune Checkpoint Receptors Signaling in T Cells. Int. J. Mol. Sci. 2022, 23, 3529. [Google Scholar] [CrossRef]
- Celis-Gutierrez, J.; Blattmann, P.; Zhai, Y.; Jarmuzynski, N.; Ruminski, K.; Grégoire, C.; Ounoughene, Y.; Fiore, F.; Aebersold, R.; Roncagalli, R.; et al. Quantitative interactomics in primary T cells provides a rationale for concomitant PD-1 and BTLA coinhibitor blockade in cancer immunotherapy. Cell Rep. 2019, 27, 3315–3330.e7. [Google Scholar] [CrossRef]
- Li, K.; Yuan, Z.; Lyu, J.; Ahn, E.; Davis, S.J.; Ahmed, R.; Zhu, C. PD-1 suppresses TCR-CD8 cooperativity during T-cell antigen recognition. Nat. Commun. 2021, 12, 2746. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; He, S.; Long, J.; Wang, Y.; Jiang, X.; Chen, M.; Wang, J. Emerging therapeutic frontiers in cancer: Insights into posttranslational modifications of PD-1/PD-L1 and regulatory pathways. Exp. Hematol. Oncol. 2024, 13, 46. [Google Scholar] [CrossRef] [PubMed]
- Chyuan, I.-T.; Liao, H.-J.; Tan, T.-H.; Chuang, H.-C.; Chu, Y.-C.; Pan, M.-H.; Wu, C.-S.; Chu, C.-L.; Sheu, B.-C.; Hsu, P.-N. Association of TRAIL receptor with phosphatase SHP-1 enables repressing T cell receptor signaling and T cell activation through inactivating Lck. J. Biomed. Sci. 2024, 31, 33. [Google Scholar] [CrossRef]
- Lai, T.-C.; Fang, C.-Y.; Jan, Y.-H.; Hsieh, H.-L.; Yang, Y.-F.; Liu, C.-Y.; Chang, P.M.-H.; Hsiao, M. Kinase shRNA screening reveals that TAOK3 enhances microtubule-targeted drug resistance of breast cancer cells via the NF-κB signaling pathway. Cell Commun. Signal. 2020, 18, 164. [Google Scholar] [CrossRef] [PubMed]
- Poirier, A.; Ormonde, J.V.S.; Aubry, I.; Abidin, B.M.; Feng, C.-H.; Martinez-Cordova, Z.; Hincapie, A.M.; Wu, C.; Pérez-Quintero, L.A.; Wang, C.-L.; et al. The induction of SHP-1 degradation by TAOK3 ensures the responsiveness of T cells to TCR stimulation. Sci. Signal. 2024, 17, eadg4422. [Google Scholar] [CrossRef] [PubMed]
- Graydon, C.G.; Mohideen, S.; Fowke, K.R. LAG3’s Enigmatic Mechanism of Action. Front. Immunol. 2021, 11, 615317. [Google Scholar] [CrossRef] [PubMed]
- Guy, C.; Mitrea, D.M.; Chou, P.-C.; Temirov, J.; Vignali, K.M.; Liu, X.; Zhang, H.; Kriwacki, R.; Bruchez, M.P.; Watkins, S.C.; et al. LAG3 associates with TCR–CD3 complexes and suppresses signaling by driving co-receptor–Lck dissociation. Nat. Immunol. 2022, 23, 757–767. [Google Scholar] [CrossRef] [PubMed]
- Luke, J.J.; Luke, J.J.; Patel, M.R.; Patel, M.R.; Blumenschein, G.R.; Blumenschein, G.R.; Hamilton, E.; Hamilton, E.; Chmielowski, B.; Chmielowski, B.; et al. The PD-1- and LAG-3-targeting bispecific molecule tebotelimab in solid tumors and hematologic cancers: A phase 1 trial. Nat. Med. 2023, 29, 2814–2824. [Google Scholar] [CrossRef] [PubMed]
- Binder, C.; Cvetkovski, F.; Sellberg, F.; Berg, S.; Visbal, H.P.; Sachs, D.H.; Berglund, E.; Berglund, D. CD2 Immunobiology. Front. Immunol. 2020, 11, 1090. [Google Scholar] [CrossRef] [PubMed]
- Nunes, R.J.; Castro, M.A.A.; Gonçalves, C.M.; Bamberger, M.; Pereira, C.F.; Bismuth, G.; Carmo, A.M. Protein Interactions between CD2 and Lck Are Required for the Lipid Raft Distribution of CD2. J. Immunol. 2008, 180, 988–997. [Google Scholar] [CrossRef]
- Burgueño-Bucio, E.; Mier-Aguilar, C.A.; Soldevila, G. The multiple faces of CD5. J. Leukoc. Biol. 2019, 105, 891–904. [Google Scholar] [CrossRef] [PubMed]
- Baaten, B.J.; Li, C.-R.; Bradley, L.M. Multifaceted regulation of T cells by CD44. Commun. Integr. Biol. 2010, 3, 508–512. [Google Scholar] [CrossRef] [PubMed]
- Senbanjo, L.T.; Chellaiah, M.A. CD44: A Multifunctional Cell Surface Adhesion Receptor Is a Regulator of Progression and Metastasis of Cancer Cells. Front. Cell Dev. Biol. 2017, 5, 18. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Zhao, S.; Karnad, A.; Freeman, J.W. The biology and role of CD44 in cancer progression: Therapeutic implications. J. Hematol. Oncol. 2018, 11, 64. [Google Scholar] [CrossRef] [PubMed]
- Duan, H.; Jing, L.; Jiang, X.; Ma, Y.; Wang, D.; Xiang, J.; Chen, X.; Wu, Z.; Yan, H.; Jia, J.; et al. CD146 bound to LCK promotes T cell receptor signaling and antitumor immune responses in mice. J. Clin. Investig. 2021, 131, e148568. [Google Scholar] [CrossRef] [PubMed]
- Raychaudhuri, S.K.; Abria, C.; Raychaudhuri, S.P. Phenotype and pathological significance of MCAM+ (CD146+) T cell subset in psoriatic arthritis. Mol. Biol. Rep. 2021, 48, 6787–6796. [Google Scholar] [CrossRef] [PubMed]
- Al-Harbi, N.O.; Ahmad, S.F.; Almutairi, M.; Alanazi, A.Z.; Ibrahim, K.E.; Alqarni, S.A.; Alqahtani, F.; Alhazzani, K.; Alharbi, M.; Alasmari, F.; et al. Lck signaling inhibition causes improvement in clinical features of psoriatic inflammation through reduction in inflammatory cytokines in CD4+ T cells in imiquimod mouse model. Cell. Immunol. 2022, 376, 104531. [Google Scholar] [CrossRef]
- McArdel, S.L.; Terhorst, C.; Sharpe, A.H. Roles of CD48 in regulating immunity and tolerance. Clin. Immunol. 2016, 164, 10–20. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Lu, Y.; Zhong, M.-C.; Qian, J.; Li, R.; Davidson, D.; Tang, Z.; Zhu, K.; Argenty, J.; de Peredo, A.G.; et al. Cis interactions between CD2 and its ligands on T cells are required for T cell activation. Sci. Immunol. 2022, 7, eabn6373. [Google Scholar] [CrossRef] [PubMed]
- Bharti, R.; Dey, G.; Lin, F.; Lathia, J.; Reizes, O. CD55 in cancer: Complementing functions in a non-canonical manner. Cancer Lett. 2022, 551, 215935. [Google Scholar] [CrossRef] [PubMed]
- Saygin, C.; Wiechert, A.; Rao, V.S.; Alluri, R.; Connor, E.; Thiagarajan, P.S.; Hale, J.S.; Li, Y.; Chumakova, A.; Jarrar, A.; et al. CD55 regulates self-renewal and cisplatin resistance in endometrioid tumors. J. Exp. Med. 2017, 214, 2715–2732. [Google Scholar] [CrossRef] [PubMed]
- Giustiniani, J.; Bensussan, A.; Marie-Cardine, A. Identification and characterization of a transmembrane isoform of CD160 (CD160-TM), a unique activating receptor selectively expressed upon human NK cell activation. J. Immunol. 2009, 182, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Oumeslakht, L.; Aziz, A.-I.; Bensussan, A.; Ben Mkaddem, S. CD160 receptor in CLL: Current state and future avenues. Front. Immunol. 2022, 13, 1028013. [Google Scholar] [CrossRef] [PubMed]
- Zhan, F.; He, L.; Yu, Y.; Chen, Q.; Guo, Y.; Wang, L. A multimodal radiomic machine learning approach to predict the LCK expression and clinical prognosis in high-grade serous ovarian cancer. Sci. Rep. 2023, 13, 16397. [Google Scholar] [CrossRef]
- Wang, F.; Zheng, A.; Zhang, D.; Zou, T.; Xiao, M.; Chen, J.; Wen, B.; Wen, Q.; Wu, X.; Li, M.; et al. Molecular profiling of core immune-escape genes highlights LCK as an immune-related prognostic biomarker in melanoma. Front. Immunol. 2022, 13, 1024931. [Google Scholar] [CrossRef] [PubMed]
- Weiße, J.; Rosemann, J.; Müller, L.; Kappler, M.; Eckert, A.W.; Glaß, M.; Misiak, D.; Hüttelmaier, S.; Ballhausen, W.G.; Hatzfeld, M.; et al. Identification of lymphocyte cell-specific protein-tyrosine kinase (LCK) as a driver for invasion and migration of oral cancer by tumor heterogeneity exploitation. Mol. Cancer 2021, 20, 88. [Google Scholar] [CrossRef] [PubMed]
- Vahedi, S.; Chueh, F.-Y.; Dutta, S.; Chandran, B.; Yu, C.-L. Nuclear lymphocyte-specific protein tyrosine kinase and its interaction with CR6-interacting factor 1 promote the survival of human leukemic T cells. Oncol. Rep. 2015, 34, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Dey, G.; Bharti, R.; Braley, C.; Alluri, R.; Esakov, E.; Crean-Tate, K.; McCrae, K.; Joehlin-Price, A.; Rose, P.G.; Lathia, J.; et al. LCK facilitates DNA damage repair by stabilizing RAD51 and BRCA1 in the nucleus of chemoresistant ovarian cancer. J. Ovarian Res. 2023, 16, 122. [Google Scholar] [CrossRef] [PubMed]
- Kumari, G.; Singhal, P.; Suryaraja, R.; Mahalingam, S. Functional Interaction of the Ras Effector RASSF5 with the Tyrosine Kinase Lck: Critical Role in Nucleocytoplasmic Transport and Cell Cycle Regulation. J. Mol. Biol. 2010, 397, 89–109. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Li, H.; Zhang, C.; Chen, Q.; Liu, Z.; Zhang, J.; Luo, P.; Wei, T. Unlocking the potential of T-cell metabolism reprogramming: Advancing single-cell approaches for precision immunotherapy in tumour immunity. Clin. Transl. Med. 2024, 14, e1620. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Wu, Y.-J.; Hu, X.-X.; Wei, W. New insights into the Lck-NF-κB signaling pathway. Front. Cell Dev. Biol. 2023, 11, 1120747. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Li, S.; Liu, Q.; Wang, Z.; Li, S.; Liu, L.; Zhao, W.; Wang, K.; Zhang, R.; Wang, L.; et al. The LCK-14-3-3ζ-TRPM8 axis regulates TRPM8 function/assembly and promotes pancreatic cancer malignancy. Cell Death Dis. 2022, 13, 524. [Google Scholar] [CrossRef] [PubMed]
- Honikel, M.M.; Olejniczak, S.H. Co-Stimulatory Receptor Signaling in CAR-T Cells. Biomolecules 2022, 12, 1303. [Google Scholar] [CrossRef] [PubMed]
- Curio, S.; Jonsson, G.; Marinović, S. A summary of current NKG2D-based CAR clinical trials. Immunother. Adv. 2021, 1, ltab018. [Google Scholar] [CrossRef] [PubMed]
- Czaplicka, A.; Lachota, M.; Pączek, L.; Zagożdżon, R.; Kaleta, B. Chimeric Antigen Receptor T Cell Therapy for Pancreatic Cancer: A Review of Current Evidence. Cells 2024, 13, 101. [Google Scholar] [CrossRef] [PubMed]
- Deng, Y.; Kumar, A.; Xie, K.; Schaaf, K.; Scifo, E.; Morsy, S.; Li, T.; Ehninger, A.; Bano, D.; Ehninger, D. Targeting senescent cells with NKG2D-CAR T cells. Cell Death Discov. 2024, 10, 217. [Google Scholar] [CrossRef] [PubMed]
- Acharya, S.; Basar, R.; Daher, M.; Rafei, H.; Li, P.; Uprety, N.; Ensley, E.; Shanley, M.; Kumar, B.; Banerjee, P.P.; et al. CD28 costimulation augments CAR signaling in NK cells via the LCK/CD3Z/ZAP70 signaling axis. Cancer Discov. 2024, 1–22. [Google Scholar] [CrossRef]
- Wu, L.; Brzostek, J.; Vale, P.D.S.; Wei, Q.; Koh, C.K.; Ong, J.X.H.; Wu, L.-Z.; Tan, J.C.; Chua, Y.L.; Yap, J.; et al. CD28-CAR-T cell activation through FYN kinase signaling rather than LCK enhances therapeutic performance. Cell Rep. Med. 2023, 4, 100917. [Google Scholar] [CrossRef]
- Zhang, J.; Zhang, J.; Jiang, Z.; Jiang, Z.; Zhang, X.; Zhang, X.; Yang, Z.; Yang, Z.; Wang, J.; Wang, J.; et al. THEMIS is a substrate and allosteric activator of SHP1, playing dual roles during T cell development. Nat. Struct. Mol. Biol. 2024, 31, 54–67. [Google Scholar] [CrossRef] [PubMed]
- Goldsmith, M.A.; Weiss, A. Isolation and characterization of a T-lymphocyte somatic mutant with altered signal transduction by the antigen receptor. Proc. Natl. Acad. Sci. USA 1987, 84, 6879–6883. [Google Scholar] [CrossRef]
- Oh-Hori, N.; Koga, Y.; Yoshida, H.; Morita, M.; Kimura, G.; Nomoto, K. Human T-cell leukemia virus type-I-infected T-cell lines scarcely produce p56lck, whether or not they express lck mRNA. Int. J. Cancer 1990, 46, 315–319. [Google Scholar] [CrossRef] [PubMed]
- Hauck, F.; Randriamampita, C.; Martin, E.; Gerart, S.; Lambert, N.; Lim, A.; Soulier, J.; Maciorowski, Z.; Touzot, F.; Moshous, D.; et al. Primary T-Cell Immunodeficiency with Immunodysregulation Caused by Autosomal Recessive LCK Deficiency. J. Allergy Clin. Immunol. 2012, 130, 1144–1152.e11. [Google Scholar] [CrossRef] [PubMed]
- Lanz, A.-L.; Erdem, S.; Ozcan, A.; Ceylaner, G.; Cansever, M.; Ceylaner, S.; Conca, R.; Magg, T.; Acuto, O.; Latour, S.; et al. A Novel Biallelic LCK Variant Resulting in Profound T-Cell Immune Deficiency and Review of the Literature. J. Clin. Immunol. 2023, 44, 1. [Google Scholar] [CrossRef] [PubMed]
- Lui, V.G.; Hoenig, M.; Cabrera-Martinez, B.; Baxter, R.M.; Garcia-Perez, J.E.; Bailey, O.; Acharya, A.; Lundquist, K.; Capera, J.; Matusewicz, P.; et al. A partial human LCK defect causes a T cell immunodeficiency with intestinal inflammation. J. Exp. Med. 2023, 221, e20230927. [Google Scholar] [CrossRef] [PubMed]
- Guérin, A.; Moncada-Vélez, M.; Jackson, K.; Ogishi, M.; Rosain, J.; Mancini, M.; Langlais, D.; Nunez, A.; Webster, S.; Goyette, J.; et al. Helper T cell immunity in humans with inherited CD4 deficiency. J. Exp. Med. 2024, 221, e20231044. [Google Scholar] [CrossRef] [PubMed]
- Hulme, J.S.; Barratt, B.J.; Twells, R.C.; Cooper, J.D.; Lowe, C.E.; Howson, J.M.; Lam, A.C.; Smink, L.J.; Savage, D.A.; Undlien, D.E.; et al. Association Analysis of the Lymphocyte-Specific Protein Tyrosine Kinase (LCK) Gene in Type 1 Diabetes. Diabetes 2004, 53, 2479–2482. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Q.; Wang, J.; Zhang, L.; Bian, W.; Lin, M.; Xu, X.; Zhou, X. LCK Rs10914542-G Allele Associates with Type 1 Diabetes in Children via T Cell Hyporesponsiveness. Pediatr. Res. 2019, 86, 311–315. [Google Scholar] [CrossRef] [PubMed]
- Han, M.; Li, Y.; Guo, Y.; Zhu, W.; Jiang, J. Integrative and Comprehensive Pan-Cancer Analysis of Lymphocyte-Specific Protein Tyrosine Kinase in Human Tumors. Int. J. Mol. Sci. 2022, 23, 13998. [Google Scholar] [CrossRef] [PubMed]
- Bai, F.; Jin, Y.; Zhang, P.; Chen, H.; Fu, Y.; Zhang, M.; Weng, Z.; Wu, K. Bioinformatic profiling of prognosis-related genes in the breast cancer immune microenvironment. Aging 2019, 11, 9328–9347. [Google Scholar] [CrossRef] [PubMed]
- Elkamhawy, A.; Ali, E.M.H.; Lee, K. New horizons in drug discovery of lymphocyte-specific protein tyrosine kinase (Lck) inhibitors: A decade review (2011–2021) focussing on structure–activity relationship (SAR) and docking insights. J. Enzym. Inhib. Med. Chem. 2021, 36, 1572–1600. [Google Scholar] [CrossRef]
- Roskoski, R. Properties of FDA-approved small molecule protein kinase inhibitors: A 2024 update. Pharmacol. Res. 2024, 200, 107059. [Google Scholar] [CrossRef] [PubMed]
- Musumeci, F.; Schenone, S. Unlocking Potential and Limits of Kinase Inhibitors: The Highway to Enhanced Cancer Targeted Therapy. Pharmaceutics 2024, 16, 625. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Zhang, K.; Tan, J.; Fan, Z.; Fu, Y.; Li, X.; Liu, B.; Wang, G. Design, synthesis, and pharmacological evaluation of novel benzothiazole derivatives targeting LCK in acute lymphoblastic leukemia. Bioorg. Chem. 2024, 144, 107–180. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.C.; Ouwehand, I.; Giannini, A.L.; Thomas, N.S.; Dibb, N.J.; Bijlmakers, M.J. Lck Is a Key Target of Imatinib and Dasatinib in T-Cell Activation. Leukemia 2010, 24, 896–900. [Google Scholar] [CrossRef] [PubMed]
- Dasatinib. Available online: https://go.drugbank.com/drugs/DB01254 (accessed on 13 July 2024).
- Cheng, Y.; Ji, C.; Xu, J.; Chen, R.; Guo, Y.; Bian, Q.; Shen, Z.; Zhang, B. LCK-SafeScreen-Model: An Advanced Ensemble Machine Learning Approach for Estimating the Binding Affinity between Compounds and LCK Target. Molecules 2023, 28, 7382. [Google Scholar] [CrossRef] [PubMed]
- Schindler, C.G.; Armbrust, T.; Gunawan, B.; Langer, C.; Füzesi, L.; Ramadori, G. Gastrointestinal stromal tumor (GIST)—Single center experience of prolonged treatment with imatinib. Z. Gastroenterol. 2005, 43, 267–273. [Google Scholar] [CrossRef] [PubMed]
- Schlemmer, M.; Bauer, S.; Schütte, R.; Hartmann, J.; Bokemeyer, C.; Hosius, C.; Reichardt, P. Activity and side effects of imatinib in patients with gastrointestinal stromal tumors: Data from a German multicenter trial. Eur. J. Med. Res. 2011, 16, 206–212. [Google Scholar] [CrossRef] [PubMed]
- Lam, T.J.R.; Udonwa, S.A.; Masuda, Y.; Yeo, M.H.X.; Ras, M.F.b.H.; Goh, B.K.P. A systematic review and meta-analysis of neoadjuvant imatinib use in locally advanced and metastatic gastrointestinal stromal tumors. World J. Surg. 2024, 48, 1681–1691. [Google Scholar] [CrossRef] [PubMed]
- Karim, N.A.; Ullah, A.; Wang, H.; Shoukier, M.; Pulliam, S.; Khaled, A.; Patel, N.; Morris, J.C. A Phase I Study of the Non-Receptor Kinase Inhibitor Bosutinib in Combination with Pemetrexed in Patients with Selected Metastatic Solid Tumors. Curr. Oncol. 2022, 29, 9461–9473. [Google Scholar] [CrossRef] [PubMed]
- Deplanque, G.; Demarchi, M.; Hebbar, M.; Flynn, P.; Melichar, B.; Atkins, J.; Nowara, E.; Moyé, L.; Piquemal, D.; Ritter, D.; et al. A randomized, placebo-controlled phase III trial of masitinib plus gemcitabine in the treatment of advanced pancreatic cancer. Ann. Oncol. 2015, 26, 1194–1200. [Google Scholar] [CrossRef] [PubMed]
- Adenis, A.; Blay, J.-Y.; Bui-Nguyen, B.; Bouché, O.; Bertucci, F.; Isambert, N.; Bompas, E.; Chaigneau, L.; Domont, J.; Ray-Coquard, I.; et al. Masitinib in advanced gastrointestinal stromal tumor (GIST) after failure of imatinib: A randomized controlled open-label trial. Ann. Oncol. 2014, 25, 1762–1769. [Google Scholar] [CrossRef] [PubMed]
- Le Cesne, A.; Blay, J.-Y.; Bui, B.N.; Bouché, O.; Adenis, A.; Domont, J.; Cioffi, A.; Ray-Coquard, I.; Lassau, N.; Bonvalot, S.; et al. Phase II study of oral masitinib mesilate in imatinib-naïve patients with locally advanced or metastatic gastro-intestinal stromal tumour (GIST). Eur. J. Cancer 2010, 46, 1344–1351. [Google Scholar] [CrossRef] [PubMed]
- Larkin, J.; Marais, R.; Porta, N.; de Castro, D.G.; Parsons, L.; Messiou, C.; Stamp, G.; Thompson, L.; Edmonds, K.; Sarker, S.; et al. Nilotinib in KIT-driven advanced melanoma: Results from the phase II single-arm NICAM trial. Cell Rep. Med. 2024, 5, 101435. [Google Scholar] [CrossRef] [PubMed]
- Mishra, R. Oral tumor heterogeneity, its implications for patient monitoring and designing anti-cancer strategies. Pathol.-Res. Pract. 2024, 253, 154953. [Google Scholar] [CrossRef] [PubMed]
- Barnwal, A.; Das, S.; Bhattacharyya, J. Repurposing Ponatinib as a PD-L1 Inhibitor Revealed by Drug Repurposing Screening and Validation by In Vitro and In Vivo Experiments. ACS Pharmacol. Transl. Sci. 2023, 6, 281–289. [Google Scholar] [CrossRef]
- Li, L.; Cui, Y.; Shen, J.; Dobson, H.; Sun, G. Evidence for activated Lck protein tyrosine kinase as the driver of proliferation in acute myeloid leukemia cell, CTV-1. Leuk. Res. 2019, 78, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Frumento, D.; Grossi, G.; Falesiedi, M.; Musumeci, F.; Carbone, A.; Schenone, S. Small Molecule Tyrosine Kinase Inhibitors (TKIs) for Glioblastoma Treatment. Int. J. Mol. Sci. 2024, 25, 1398. [Google Scholar] [CrossRef] [PubMed]
- Harada, D.; Isozaki, H.; Kozuki, T.; Yokoyama, T.; Yoshioka, H.; Bessho, A.; Hosokawa, S.; Takata, I.; Takigawa, N.; Hotta, K.; et al. Crizotinib for recurring non-small-cell lung cancer with EML4-ALK fusion genes previously treated with alectinib: A phase II trial. Thorac. Cancer 2021, 12, 643–649. [Google Scholar] [CrossRef] [PubMed]
- Camidge, D.R.; Bang, Y.-J.; Kwak, E.L.; Iafrate, A.J.; Varella-Garcia, M.; Fox, S.B.; Riely, G.J.; Solomon, B.; Ou, S.-H.I.; Kim, D.-W.; et al. Activity and safety of crizotinib in patients with ALK-positive non-small-cell lung cancer: Updated results from a phase 1 study. Lancet Oncol. 2012, 13, 1011–1019. [Google Scholar] [CrossRef] [PubMed]
- Cruz, B.D.; Barbosa, M.M.; Torres, L.L.; Azevedo, P.S.; Silva, V.E.A.; Godman, B.; Alvares-Teodoro, J. Crizotinib Versus Conventional Chemotherapy in First-Line Treatment for ALK-Positive Non-Small Cell Lung Cancer: A Systematic Review and Meta-Analysis. Oncol. Ther. 2021, 9, 505–524. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, A.; Nishikawa, H.; Noguchi, S.; Sugiyama, D.; Morikawa, H.; Takeuchi, Y.; Ha, D.; Shigeta, N.; Kitawaki, T.; Maeda, Y.; et al. Tyrosine kinase inhibitor imatinib augments tumor immunity by depleting effector regulatory T cells. J. Exp. Med. 2019, 217, e20191009. [Google Scholar] [CrossRef]
- Burchat, A.; Borhani, D.W.; Calderwood, D.J.; Hirst, G.C.; Li, B.; Stachlewitz, R.F. Discovery of A-770041, a src-family selective orally active lck inhibitor that prevents organ allograft rejection. Bioorganic Med. Chem. Lett. 2006, 16, 118–122. [Google Scholar] [CrossRef] [PubMed]
- Singh, P.K.; Kashyap, A.; Silakari, O. Exploration of the therapeutic aspects of Lck: A kinase target in inflammatory mediated pathological conditions. Biomed. Pharmacother. 2018, 108, 1565–1571. [Google Scholar] [CrossRef] [PubMed]
- Kagawa, K.; Sato, S.; Koyama, K.; Imakura, T.; Murakami, K.; Yamashita, Y.; Naito, N.; Ogawa, H.; Kawano, H.; Nishioka, Y. The lymphocyte-specific protein tyrosine kinase-specific inhibitor A-770041 attenuates lung fibrosis via the suppression of TGF-β production in regulatory T-cells. PLoS ONE 2022, 17, e0275987. [Google Scholar] [CrossRef] [PubMed]
- Alqarni, S.A.; Bineid, A.; Ahmad, S.F.; Al-Harbi, N.O.; Alqahtani, F.; Ibrahim, K.E.; Ali, N.; Nadeem, A. Blockade of Tyrosine Kinase, LCK Leads to Reduction in Airway Inflammation through Regulation of Pulmonary Th2/Treg Balance and Oxidative Stress in Cockroach Extract-Induced Mouse Model of Allergic Asthma. Metabolites 2022, 12, 793. [Google Scholar] [CrossRef] [PubMed]
- Carter, N.M.; Pomerantz, J.L. Calcineurin inhibitors target Lck activation in graft-versus-host disease. J. Clin. Investig. 2021, 131, e149934. [Google Scholar] [CrossRef] [PubMed]
- Srour, M.; Alsuliman, T.; Labreuche, J.; Bulabois, C.-E.; Chevallier, P.; Daguindau, E.; Forcade, E.; François, S.; Guillerm, G.; Coiteux, V.; et al. Nilotinib efficacy and safety as salvage treatment following imatinib intolerance and/or inefficacy in steroid refractory chronic graft-versus-host-disease (SR-cGVHD): A prospective, multicenter, phase II study on behalf of the Francophone Society of Bone Marrow Transplantation and Cellular Therapy (SFGM-TC). Bone Marrow Transplant. 2023, 58, 401–406. [Google Scholar] [CrossRef]
- Olivieri, A.; Mancini, G.; Olivieri, J.; Busilacchi, E.M.; Cimminiello, M.; Pascale, S.P.; Nuccorini, R.; Patriarca, F.; Corradini, P.; Bacigalupo, A.; et al. Nilotinib in steroid-refractory cGVHD: Prospective parallel evaluation of response, according to NIH criteria and exploratory response criteria (GITMO criteria). Bone Marrow Transplant. 2020, 55, 2077–2086. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.-T.; Hsueh, P.-R.; Wu, S.-J.; Yao, M.; Ko, B.-S.; Li, C.-C.; Hsu, C.-A.; Tang, J.-L.; Tien, H.-F. Repurposing Nilotinib for Cytomegalovirus Infection Prophylaxis after Allogeneic Hematopoietic Stem Cell Transplantation: A Single-Arm, Phase II Trial. Biol. Blood Marrow Transplant. 2018, 24, 2310–2315. [Google Scholar] [CrossRef] [PubMed]
- Martin, M.W.; Newcomb, J.; Nunes, J.J.; McGowan, D.C.; Armistead, D.M.; Boucher, C.; Buchanan, J.L.; Buckner, W.; Chai, L.; Elbaum, D.; et al. Novel 2-aminopyrimidine carbamates as potent and orally active inhibitors of Lck: Synthesis, SAR, and in vivo antiinflammatory activity. J. Med. Chem. 2006, 49, 4981–4991. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Yao, H.; Ma, Z.; Hu, X. Investigating small molecule compounds targeting psoriasis based on cMAP database and molecular dynamics simulation. Ski. Res. Technol. 2023, 29, e13301. [Google Scholar] [CrossRef] [PubMed]


| Inhibitor | Structure | Site of Binding | Initial Proposed Target | References |
|---|---|---|---|---|
| Saracatinib | 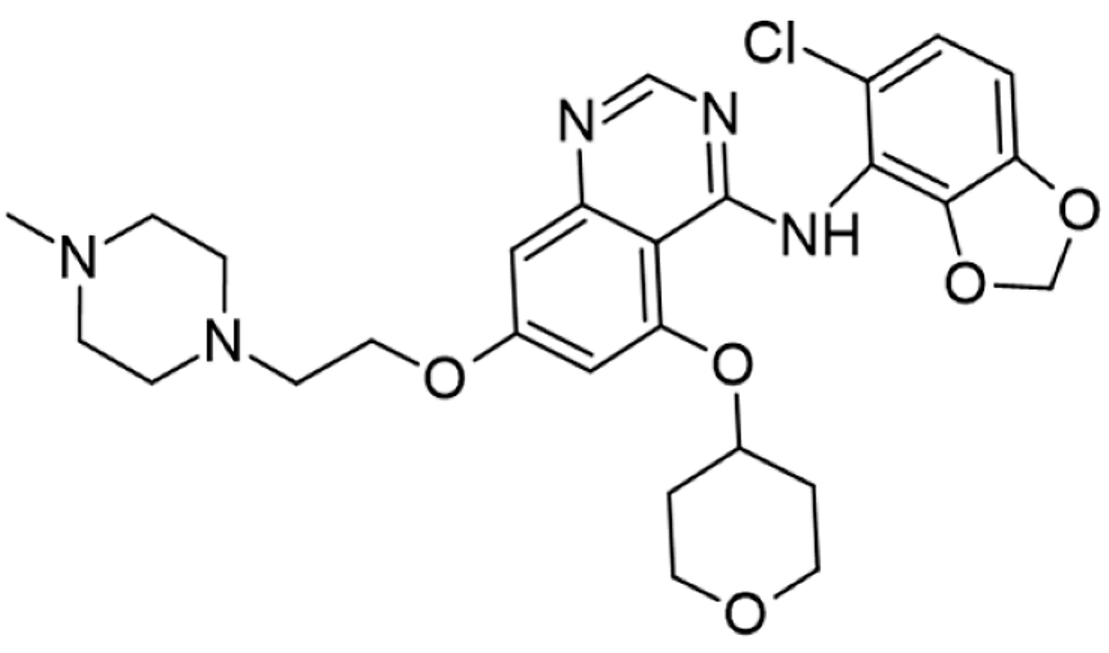 | ATP-binding site | Selective Scr inhibitor | [137,138,139] |
| Dasatinib | 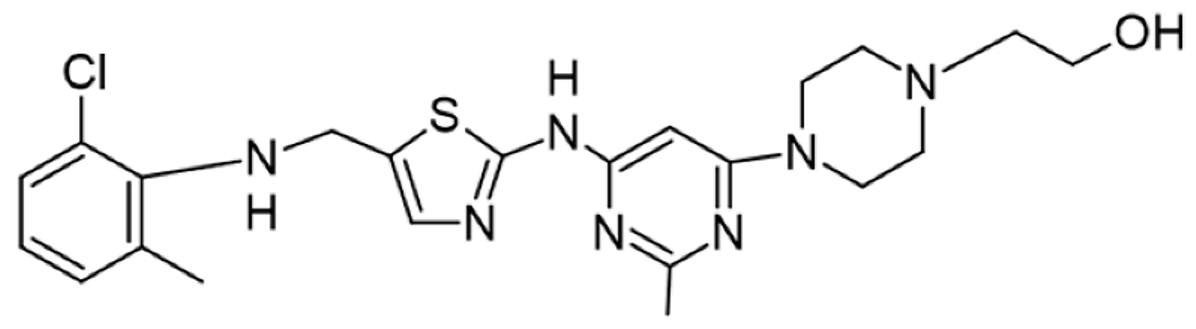 | Tyr-394 | ABL kinase domain | [137,138,139,141] |
| Imatinib |  | ATP-binding site | Pan tyrosine kinase inhibitor | [137,138,141] |
| Bosutinib | 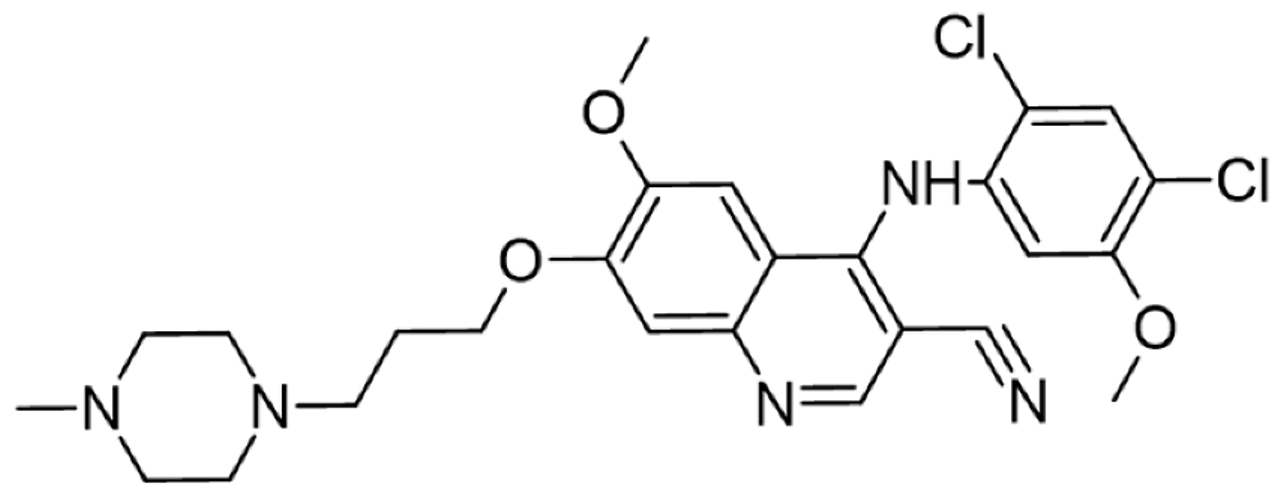 | ATP-binding site | BCR-ABL inhibitor | [13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,147] |
| Ponatinib |  | ATP-binding site | ABL kinase inactive site | [137,138] |
| Masitinib | 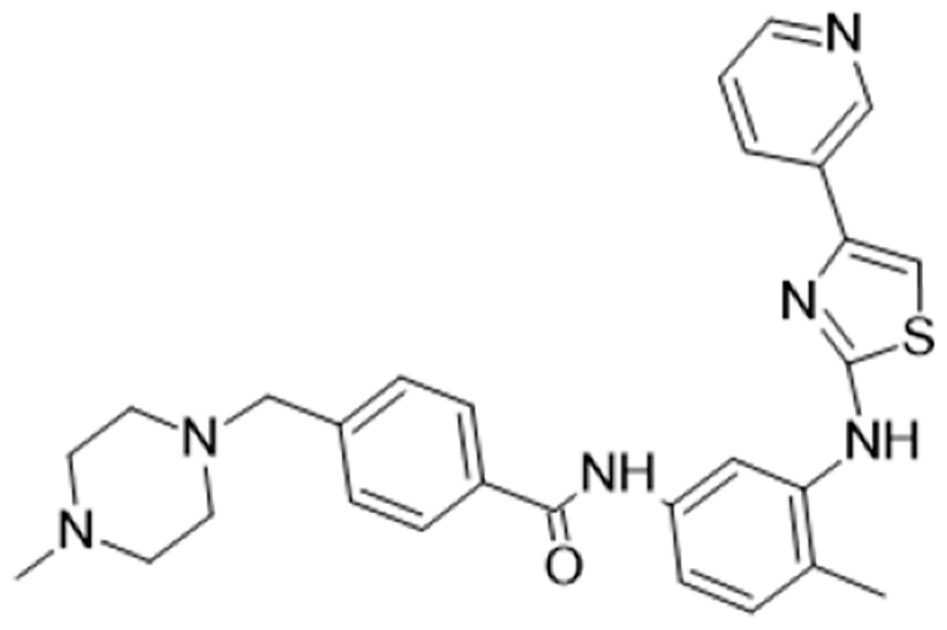 | ATP-binding site | Binds to stem cell factor receptor c-KitR, | [137,138,148] |
| Ceritinib | 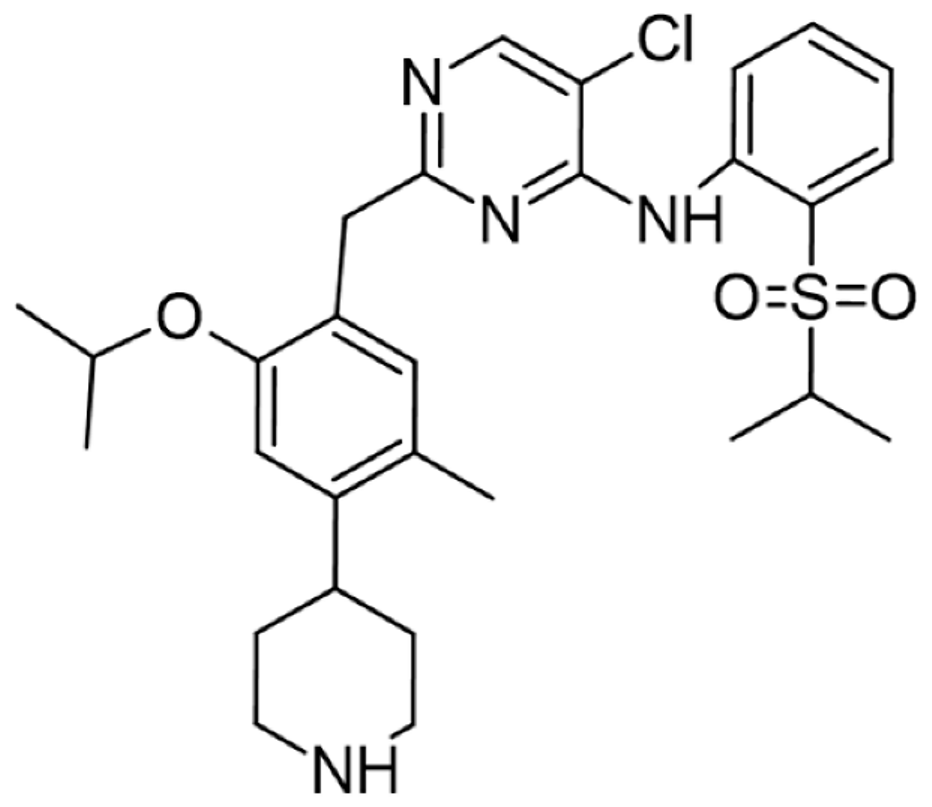 | ATP-binding pocket | Autophosphorylation of ALK | [137,138] |
| Crizotinib |  | ATP-binding pocket | ALK and c-Met kinase inhibitor | [139,140] |
| Nilotinib | 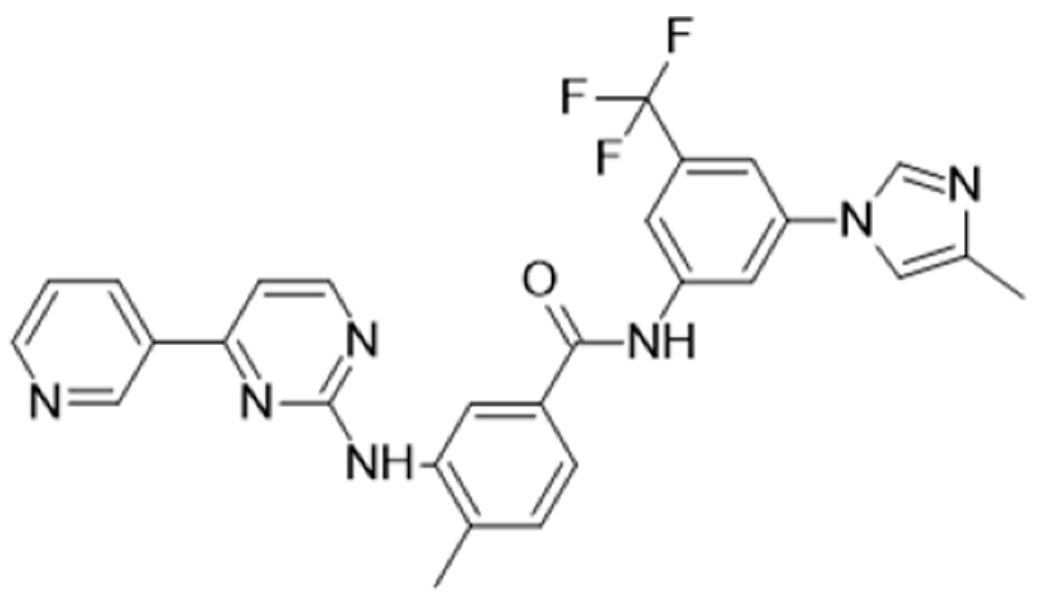 | Kinase domain | Chronic myelogenous leukemia | [137,138,139] |
| A-770041 | 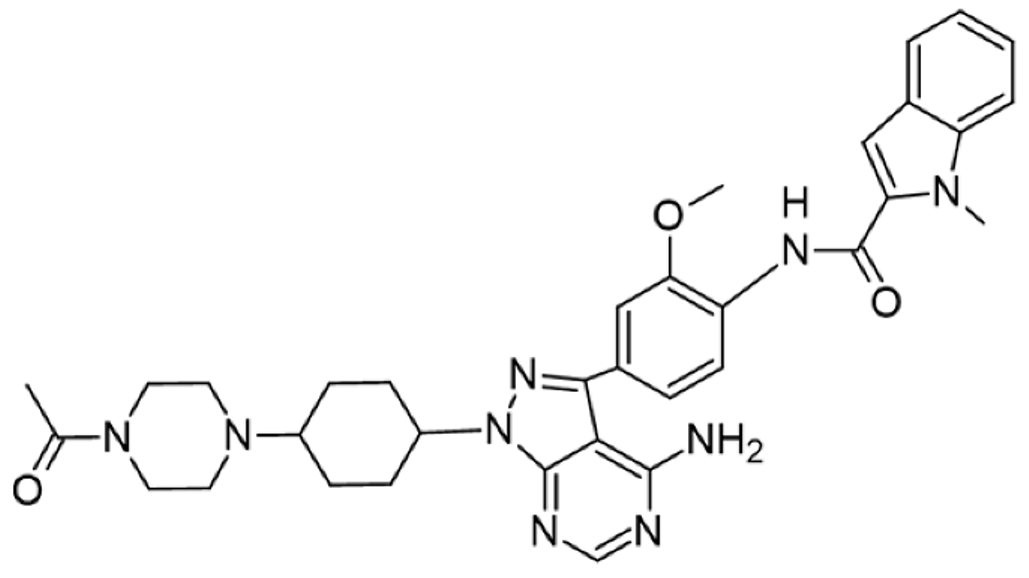 | ATP-binding site | Specific Lck inhibitor | [160] |
| WH-4-23 | 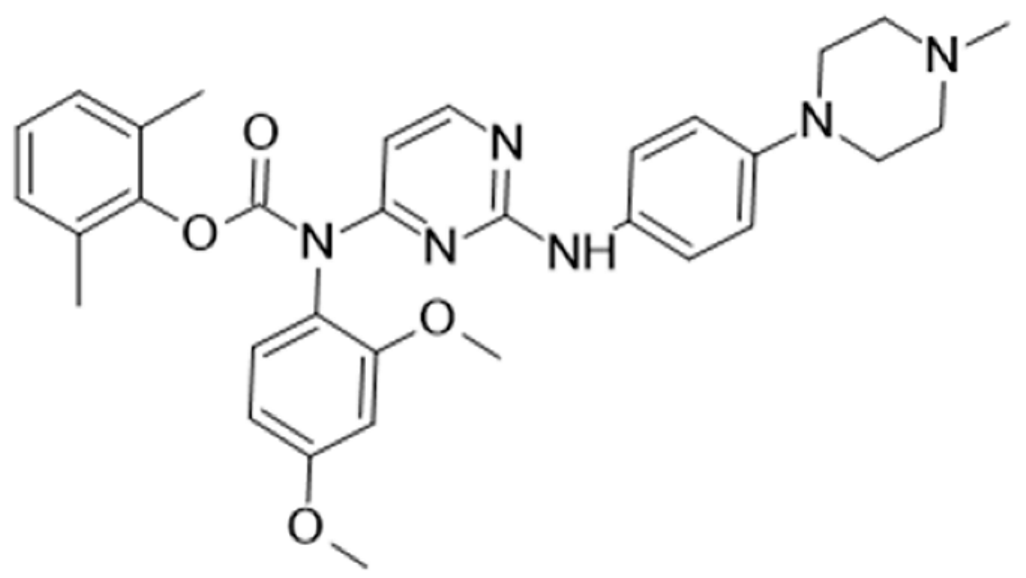 | Most probably ATP-binding site | Pan tyrosine kinase inhibitor | [168] |
| Tirbanibulin | 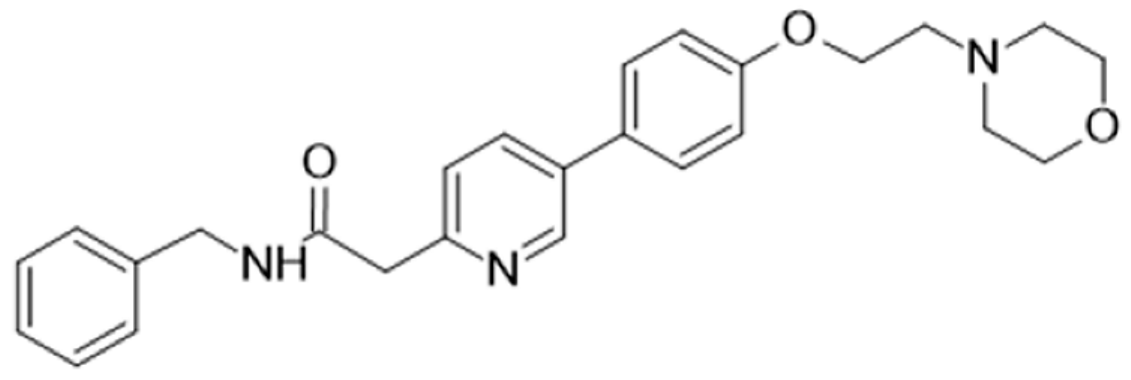 | Peptide substrate binding site | Scr inhibtor. | [169] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Sanctis, J.B.; Garmendia, J.V.; Duchová, H.; Valentini, V.; Puskasu, A.; Kubíčková, A.; Hajdúch, M. Lck Function and Modulation: Immune Cytotoxic Response and Tumor Treatment More Than a Simple Event. Cancers 2024, 16, 2630. https://doi.org/10.3390/cancers16152630
De Sanctis JB, Garmendia JV, Duchová H, Valentini V, Puskasu A, Kubíčková A, Hajdúch M. Lck Function and Modulation: Immune Cytotoxic Response and Tumor Treatment More Than a Simple Event. Cancers. 2024; 16(15):2630. https://doi.org/10.3390/cancers16152630
Chicago/Turabian StyleDe Sanctis, Juan Bautista, Jenny Valentina Garmendia, Hana Duchová, Viktor Valentini, Alex Puskasu, Agáta Kubíčková, and Marián Hajdúch. 2024. "Lck Function and Modulation: Immune Cytotoxic Response and Tumor Treatment More Than a Simple Event" Cancers 16, no. 15: 2630. https://doi.org/10.3390/cancers16152630
APA StyleDe Sanctis, J. B., Garmendia, J. V., Duchová, H., Valentini, V., Puskasu, A., Kubíčková, A., & Hajdúch, M. (2024). Lck Function and Modulation: Immune Cytotoxic Response and Tumor Treatment More Than a Simple Event. Cancers, 16(15), 2630. https://doi.org/10.3390/cancers16152630







