Imaging-Based Disease Assessment and Management Recommendations: Impact of Multidisciplinary Sarcoma Tumor Board
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
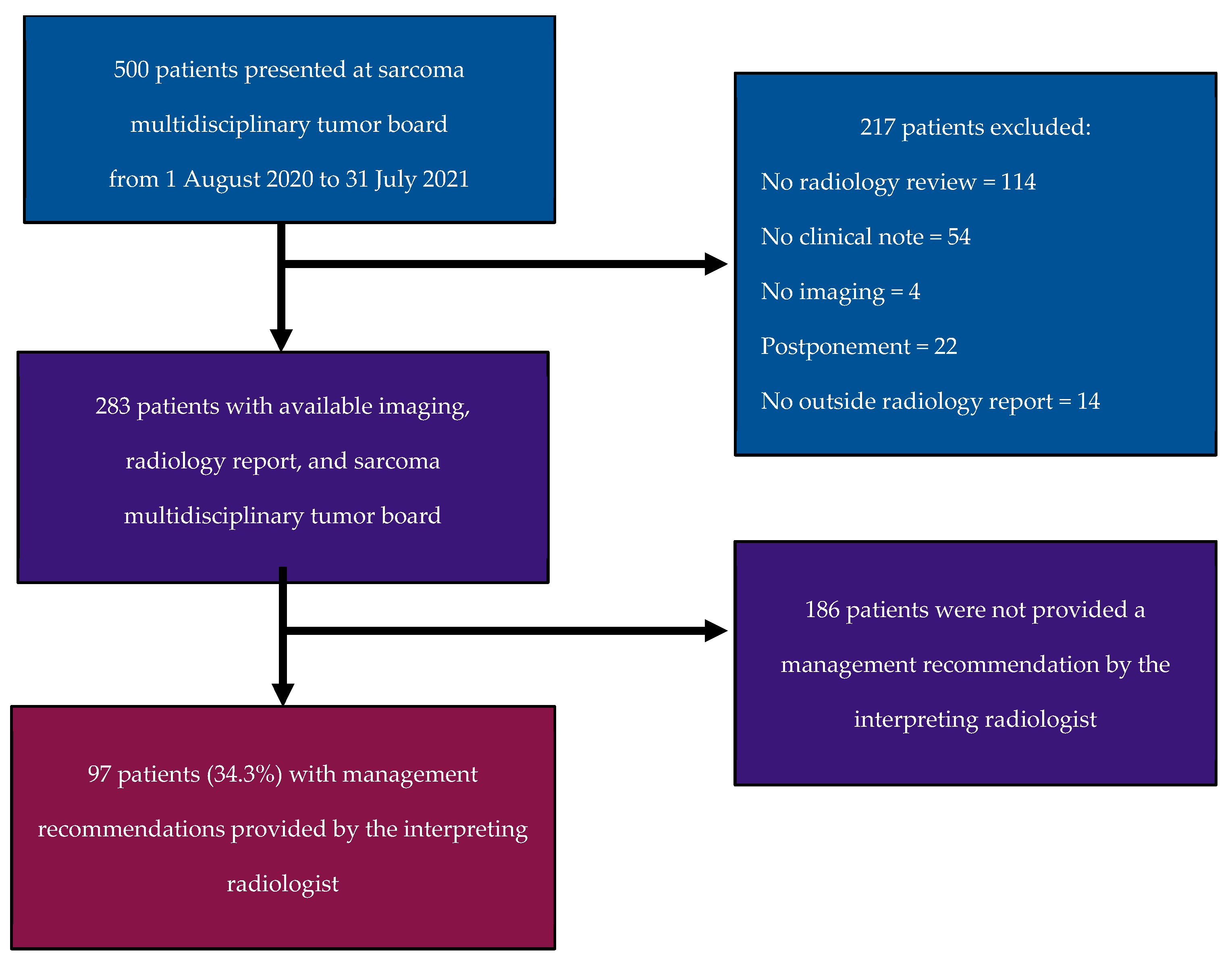
2.1. Study Population
2.2. Data Collection
2.3. Statistical Analysis
3. Results
3.1. Study Population
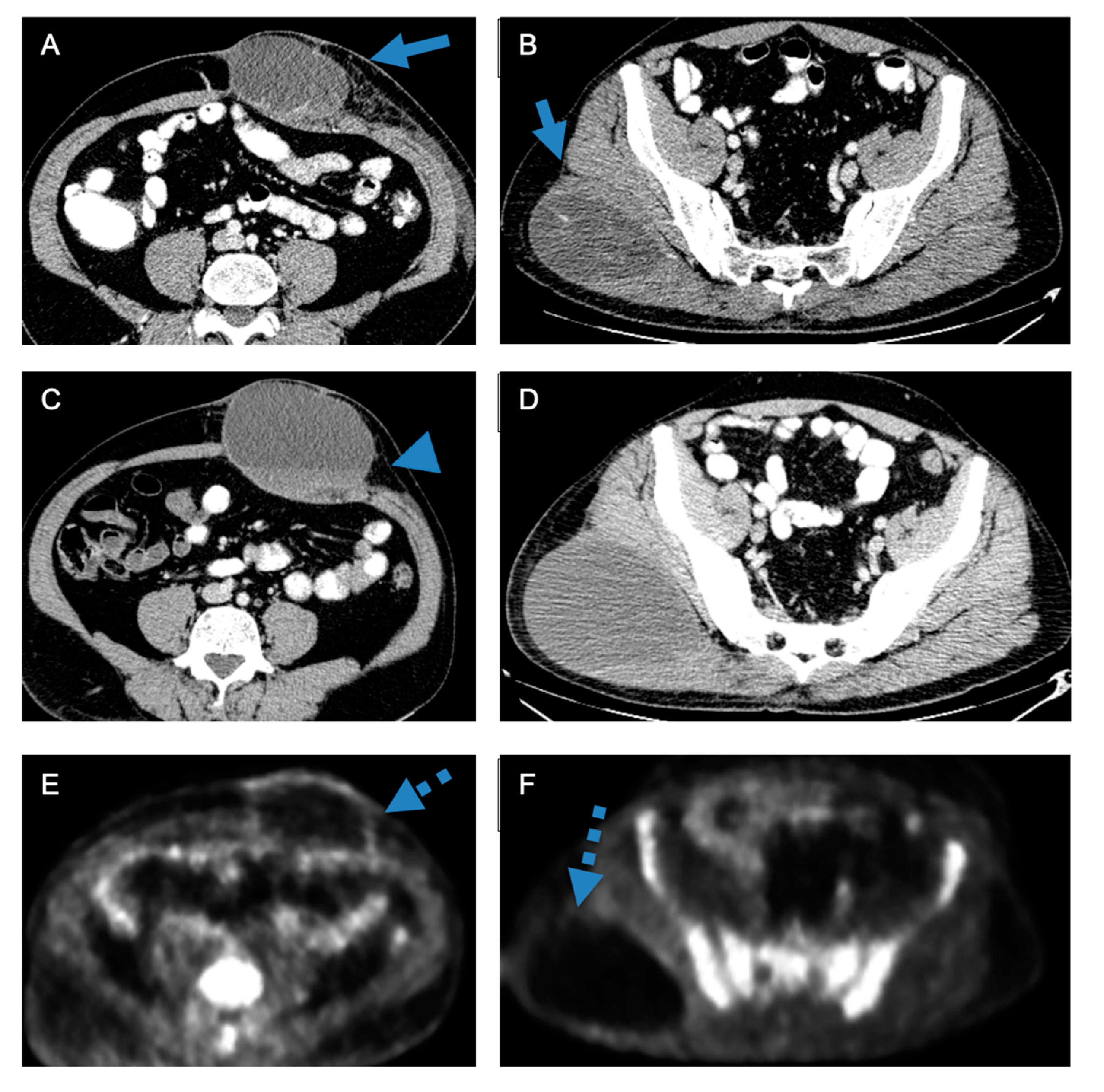
3.2. Disease Assessment
3.3. Radiology Recommendations
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gamboa, A.C.; Gronchi, A.; Cardona, K. Soft-tissue sarcoma in adults: An update on the current state of histiotype-specific management in an era of personalized medicine. CA Cancer J. Clin. 2020, 70, 200–229. [Google Scholar] [CrossRef]
- Siegel, R.L.; Giaquinto, A.N.; Jemal, A. Cancer statistics. CA Cancer J. Clin. 2024, 74, 12–49. [Google Scholar] [CrossRef] [PubMed]
- Key Statistics for Soft Tissue Sarcomas. Available online: https://www.cancer.org/cancer/types/soft-tissue-sarcoma/about/key-statistics.html (accessed on 13 September 2022).
- Blay, J.Y.; Soibinet, P.; Penel, N.; Bompas, E.; Duffaud, F.; Stoeckle, E.; Mir, O.; Adam, J.; Chevreau, C.; Bonvalot, S.; et al. Improved survival using specialized multidisciplinary board in sarcoma patients. Ann. Oncol. 2017, 28, 2852–2859. [Google Scholar] [CrossRef]
- Wilson, R.; Reinke, D.; van Oortmerssen, G.; Gonzato, O.; Ott, G.; Raut, C.P.; Guadagnolo, B.A.; Haas, R.L.M.; Trent, J.; Jones, R.; et al. What Is a Sarcoma ‘Specialist Center’? Multidisciplinary Research Finds an Answer. Cancers 2024, 16, 1857. [Google Scholar] [CrossRef] [PubMed]
- Pan, M.; Yu, J.; Sidhu, M.; Seto, T.; Fang, A. Impact of a Virtual Multidisciplinary Sarcoma Case Conference on Treatment Plan and Survival in a Large Integrated Healthcare System. JCO Oncol. Pract. 2021, 17, e1711–e1718. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, P.D.; Phillips, P.; Hillman, L.; Lucey, M.R.; Lee, F.; Mezrich, J.D.; Said, A. Multidisciplinary Management of Hepatocellular Carcinoma Improves Access to Therapy and Patient Survival. J. Clin. Gastroenterol. 2017, 51, 845–849. [Google Scholar] [CrossRef] [PubMed]
- Levine, R.A.; Chawla, B.; Bergeron, S.; Wasvary, H. Multidisciplinary management of colorectal cancer enhances access to multimodal therapy and compliance with National Comprehensive Cancer Network (NCCN) guidelines. Int. J. Color. Dis. 2012, 27, 1531–1538. [Google Scholar] [CrossRef] [PubMed]
- Quero, G.; Salvatore, L.; Fiorillo, C.; Bagalà, C.; Menghi, R.; Maria, B.; Cina, C.; Laterza, V.; Di Stefano, B.; Maratta, M.G.; et al. The impact of the multidisciplinary tumor board (MDTB) on the management of pancreatic diseases in a tertiary referral center. ESMO Open 2021, 6, 100010. [Google Scholar] [CrossRef] [PubMed]
- Greer, H.O.; Frederick, P.J.; Falls, N.M.; Tapley, E.B.; Samples, K.L.; Kimball, K.J.; Kendrick, J.E.; Conner, M.G.; Novak, L.; Straughn, J.M.J. Impact of a weekly multidisciplinary tumor board conference on the management of women with gynecologic malignancies. Int. J. Gynecol. Cancer 2010, 20, 1321–1325. [Google Scholar]
- Rozenberg, A.; Kenneally, B.E.; Abraham, J.A.; Strogus, K.; Roedl, J.B.; Morrison, W.B.; Zoga, A.C. Clinical Impact of Second-Opinion Musculoskeletal Subspecialty Interpretations During a Multidisciplinary Orthopedic Oncology Conference. J. Am. Coll. Radiol. 2017, 14, 931–936. [Google Scholar] [CrossRef]
- Chung, R.; Rosenkrantz, A.B.; Shanbhogue, K.P. Expert radiologist review at a hepatobiliary multidisciplinary tumor board: Impact on patient management. Abdom. Radiol. N. Y. 2020, 45, 3800–3808. [Google Scholar] [CrossRef]
- Rosenkrantz, A.B.; Duszak, R.; Babb, J.S.; Glover, M.; Kang, S.K. Discrepancy Rates and Clinical Impact of Imaging Secondary Interpretations: A Systematic Review and Meta-Analysis. J. Am. Coll. Radiol. 2018, 15, 1222–1231. [Google Scholar] [CrossRef]
- Jeon, S.K.; Kim, S.H.; Shin, C.I.; Yoo, J.; Park, K.J.; Ryoo, S.B.; Park, J.W.; Kim, T.Y.; Han, S.W.; Lee, D.W.; et al. Role of Dedicated Subspecialized Radiologists in Multidisciplinary Team Discussions on Lower Gastrointestinal Tract Cancers. Korean J. Radiol. 2022, 23, 732–741. [Google Scholar] [CrossRef]
- Mallory, M.A.; Losk, K.; Lin, N.U.; Sagara, Y.; Birdwell, R.L.; Cutone, L.; Camuso, K.; Bunnell, C.; Aydogan, F.; Golshan, M. The Influence of Radiology Image Consultation in the Surgical Management of Breast Cancer Patients. Ann. Surg. Oncol. 2015, 22, 3383–3388. [Google Scholar] [CrossRef]
- Seo, Y.; Min, J.H.; Kim, S.H.; Kim, Y.K.; Kim, H.; Cha, D.I.; Lee, J.H.; Heo, J.S.; Han, I.W.; Shin, S.H.; et al. The role of subspecialized radiologist reviews in preoperative conference for hepato-pancreato-biliary disease. Eur. J. Radiol. 2023, 169, 111183. [Google Scholar] [CrossRef]
- Newman, E.A.; Guest, A.B.; Helvie, M.A.; Roubidoux, M.A.; Chang, A.E.; Kleer, C.G.; Diehl, K.M.; Cimmino, V.M.; Pierce, L.; Hayes, D.; et al. Changes in surgical management resulting from case review at a breast cancer multidisciplinary tumor board. Cancer 2006, 107, 2346–2351. [Google Scholar] [CrossRef]
- Mabotuwana, T.; Hombal, V.; Dalal, S.; Hall, C.S.; Gunn, M. Determining Adherence to Follow-up Imaging Recommendations. J. Am. Coll. Radiol. 2018, 15 Pt A, 422–428. [Google Scholar] [CrossRef]
- White, T.; Aronson, M.D.; Sternberg, S.B.; Shafiq, U.; Berkowitz, S.J.; Benneyan, J.; Phillips, R.S.; Schiff, G.D. Analysis of Radiology Report Recommendation Characteristics and Rate of Recommended Action Performance. JAMA Netw. Open 2022, 5, e2222549. [Google Scholar] [CrossRef]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Medica 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Zhang, J.; Mavros, M.N.; Cosgrove, D.; Hirose, K.; Herman, J.M.; Smallwood-Massey, S.; Kamel, I.; Gurakar, A.; Anders, R.; Cameron, A.; et al. Impact of a single-day multidisciplinary clinic on the management of patients with liver tumours. Curr. Oncol. Tor. Ont. 2013, 20, e123–e131. [Google Scholar] [CrossRef]
- Lamb, B.W.; Green, J.S.A.; Benn, J.; Brown, K.F.; Vincent, C.A.; Sevdalis, N. Improving decision making in multidisciplinary tumor boards: Prospective longitudinal evaluation of a multicomponent intervention for 1421 patients. J. Am. Coll. Surg. 2013, 217, 412–420. [Google Scholar] [CrossRef]
- Campani, C.; Vallot, A.; Ghannouchi, H.; Allaire, M.; Evain, M.; Sultanik, P.; Sidali, S.; Blaise, L.; Thabut, D.; Nahon, P.; et al. Impact of radiological response and pattern of progression in patients with HCC treated by atezolizumab-bevacizumab. Hepatology 2024, 79, 49–60. [Google Scholar] [CrossRef]
- Eisenhauer, E.A.; Therasse, P.; Bogaerts, J.; Schwartz, L.H.; Sargent, D.; Ford, R.; Dancey, J.; Arbuck, S.; Gwyther, S.; Mooney, M.; et al. New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1). Eur. J. Cancer 2009, 45, 228–247. [Google Scholar] [CrossRef]
- Do, R.K.G.; Lefkowitz, R.A.; Hatzoglou, V.; Ma, W.; Juluru, K.; Mayerhoefer, M. Standardized Reporting of Oncologic Response: Making Every Report Count. Radiol. Imaging Cancer 2022, 4, e220042. [Google Scholar] [CrossRef]
- Siegel, M.J.; Ippolito, J.E.; Wahl, R.L.; Siegel, B.A. Discrepant Assessments of Progressive Disease in Clinical Trials between Routine Clinical Reads and Formal RECIST 1.1 Interpretations. Radiol. Imaging Cancer 2023, 5, e230001. [Google Scholar] [CrossRef]
- Briggs, G.M.; Flynn, P.A.; Worthington, M.; Rennie, I.; McKinstry, C.S. The role of specialist neuroradiology second opinion reporting: Is there added value? Clin. Radiol. 2008, 63, 791–795. [Google Scholar] [CrossRef]
- Bruno, M.A.; Walker, E.A.; Abujudeh, H.H. Understanding and Confronting Our Mistakes: The Epidemiology of Error in Radiology and Strategies for Error Reduction. Radiogr. Rev. Publ. Radiol. Soc. N. Am. Inc. 2015, 35, 1668–1676. [Google Scholar] [CrossRef]
- Kane, B.; Luz, S.; O’Briain, D.S.; McDermott, R. Multidisciplinary team meetings and their impact on workflow in radiology and pathology departments. BMC Med. 2007, 5, 15. [Google Scholar] [CrossRef]
- Stratchko, L.M.; Rossebo, A.E.; Kisting, M.A.; Hinshaw, J.L.; Mao, L.; Meyer, C.A.; Robbins, J.B.; Tuite, M.J.; Grist, T.M.; Lee, F.T.J. Unreimbursed Costs of Multidisciplinary Conferences to a Radiology Department: A Prospective Analysis at an Academic Medical Center. J. Am. Coll. Radiol. 2024, 21, 668–675. [Google Scholar] [CrossRef]
- Shenoy-Bhangle, A.S.; Putta, N.; Adondakis, M.; Rawson, J.; Tsai, L.L. Prospective Analysis of Radiology Resource Utilization and Outcomes for Participation in Oncology Multidisciplinary Conferences. Acad. Radiol. 2021, 28, 1219–1224. [Google Scholar] [CrossRef]
- Chau, B.L.; LaGuardia, J.S.; Kim, S.; Zhang, S.C.; Pletcher, E.; Sanford, N.N.; Raldow, A.C.; Singer, L.; Gong, J.; Padda, S.K.; et al. Association of Parental Status and Gender with Burden of Multidisciplinary Tumor Boards Among Oncology Physicians. JAMA Netw. Open 2023, 6, e2340663. [Google Scholar] [CrossRef]
| Imaging Modality |
|
| In-House vs. Outside Interpretation |
|
| Patient’s Clinical Status |
|
| Response Assessment |
|
| Recommendation |
|
| Adherence to Radiologist Recommendation |
|
| Imaging Modality | Computed Tomography (CT): 157 (55.5%) Magnetic Resonance Imaging (MRI): 50 (17.7%) Positron Emitting Tomography (PET/CT): 36 (12.7%) Multiple Imaging Modalities: 40 (14.1%) |
| Patient’s Clinical Status | On Treatment: 175 (61.8%) On Surveillance: 86 (30.4%) Neither/New Diagnosis: 22 (7.8%) |
| In-House vs. Outside Interpretation | In-House Report: 180 (63.6%) Outside Report: 103 (36.4%) |
| Radiologist Disease Assessment | ||||||
|---|---|---|---|---|---|---|
| Multidisciplinary Tumor Board Assessment | CR | SD | PR | PD | Total | |
| CR | 0 | 0 | 0 | 0 | 0 | |
| SD | 0 | 68 | 1 | 21 | 90 | |
| PR | 0 | 2 | 39 | 7 | 48 | |
| PD | 0 | 0 | 3 | 107 | 110 | |
| Total | 0 | 70 | 43 | 135 | 248 | |
| Radiologist Recommendations | |||||||
|---|---|---|---|---|---|---|---|
| Multidisciplinary Tumor Board Recommendations | Bx | SFU | RFU | Tx | Other | Total | |
| Bx | 5 | 12 | 9 | 0 | 7 | 33 | |
| SFU | 2 | 17 | 1 | 0 | 1 | 21 | |
| RFU | 1 | 10 | 14 | 0 | 1 | 26 | |
| Tx | 4 | 6 | 7 | 0 | 0 | 17 | |
| Other | 0 | 0 | 0 | 0 | 0 | 0 | |
| Total | 12 | 45 | 31 | 0 | 9 | 97 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jubane, M.; Rennick, A.C.; Villavicencio, J.J.; Ferreira de Souza, F.; Peters, V.; Jonczak, E.; Bialick, S.; Dhir, A.; Grossman, J.; Trent, J.C.; et al. Imaging-Based Disease Assessment and Management Recommendations: Impact of Multidisciplinary Sarcoma Tumor Board. Cancers 2024, 16, 2674. https://doi.org/10.3390/cancers16152674
Jubane M, Rennick AC, Villavicencio JJ, Ferreira de Souza F, Peters V, Jonczak E, Bialick S, Dhir A, Grossman J, Trent JC, et al. Imaging-Based Disease Assessment and Management Recommendations: Impact of Multidisciplinary Sarcoma Tumor Board. Cancers. 2024; 16(15):2674. https://doi.org/10.3390/cancers16152674
Chicago/Turabian StyleJubane, Maverick, Andrew C. Rennick, Joseph J. Villavicencio, Felipe Ferreira de Souza, Vanessa Peters, Emily Jonczak, Steven Bialick, Aditi Dhir, Julie Grossman, Jonathan C. Trent, and et al. 2024. "Imaging-Based Disease Assessment and Management Recommendations: Impact of Multidisciplinary Sarcoma Tumor Board" Cancers 16, no. 15: 2674. https://doi.org/10.3390/cancers16152674
APA StyleJubane, M., Rennick, A. C., Villavicencio, J. J., Ferreira de Souza, F., Peters, V., Jonczak, E., Bialick, S., Dhir, A., Grossman, J., Trent, J. C., D’Amato, G., Rosenberg, A. E., Hornicek, F. J., Yechieli, R. L., Subhawong, T., & Alessandrino, F. (2024). Imaging-Based Disease Assessment and Management Recommendations: Impact of Multidisciplinary Sarcoma Tumor Board. Cancers, 16(15), 2674. https://doi.org/10.3390/cancers16152674







