The FLARE Score and Circulating Neutrophils in Patients with Cancer and COVID-19 Disease
Abstract
:Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Study Design, Study Population, and Data Collection
2.1.1. Retrospective Clinical Cohort
2.1.2. Prospective Exploratory Cohort
2.1.3. Data Collection
2.2. Endpoints
2.3. Immunophenotyping
2.4. Serum Analyses
2.5. Statistical Analysis
3. Results
3.1. Study Population
3.1.1. Retrospective Clinical Cohort
3.1.2. Prospective Exploratory Cohort
3.2. dNLR in Patients with Cancer and COVID-19 Infection
3.3. Building of the FLARE Score
3.4. The FLARE Score Is Correlated with Early Mortality
3.5. Circulating Neutrophils in Patients with Cancer and COVID-19 Infection
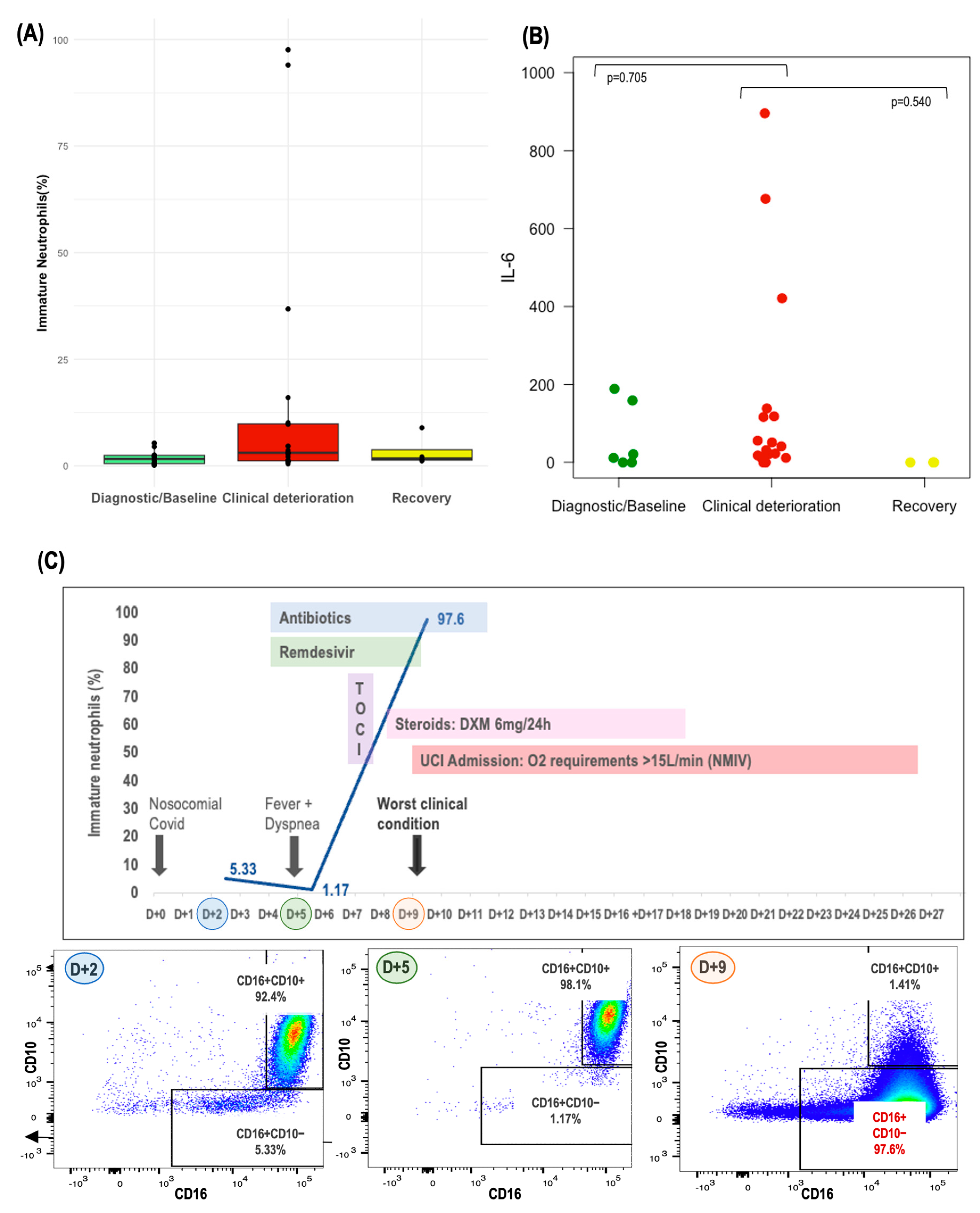
3.6. Circulating Immature Neutrophils in Patients with Cancer and COVID-19 Infection
3.7. Correlation between Circulating Inflammatory Cytokines, Circulating Immature Neutrophils, and Circulating Inflammatory Markers (dNLR) in Patients with Cancer and COVID-19 Infection
3.8. Monitoring of Circulating Neutrophils and IL-6
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pinato, D.J.; Zambelli, A.; Aguilar-Company, J.; Bower, M.; Sng, C.; Salazar, R.; Bertuzzi, A.; Brunet, J.; Mesia, R.; Segui, E.; et al. Clinical portrait of the SARS-CoV-2 epidemic in European cancer patients. Cancer Discov. 2020, 10, 1465–1474. [Google Scholar] [CrossRef] [PubMed]
- Pinato, D.J.; Lee, A.J.X.; Biello, F.; Seguí, E.; Aguilar-Company, J.; Carbó, A.; Bruna, R.; Bower, M.; Rizzo, G.; Benafif, S.; et al. Presenting features and early mortality from SARS-CoV-2 infection in cancer patients during the initial stage of the COVID-19 pandemic in Europe. Cancers 2020, 12, 1841. [Google Scholar] [CrossRef] [PubMed]
- Kuderer, N.M.; Choueiri, T.K.; Shah, D.P.; Shyr, Y.; Rubinstein, S.M.; Rivera, D.R.; Shete, S.; Hsu, C.Y.; Desai, A.; de Lima Lopes, G., Jr.; et al. COVID-19 and Cancer Consortium. Clinical impact of COVID-19 on patients with cancer (CCC19): A cohort study. Lancet 2020, 395, 1907–1918. [Google Scholar] [CrossRef] [PubMed]
- Meizlish, M.L.; Pine, A.B.; Bishai, J.D.; Goshua, G.; Nadelmann, E.R.; Simonov, M.; Chang, C.H.; Zhang, H.; Shallow, M.; Bahel, P.; et al. A neutrophil activation signature predicts critical illness and mortality in COVID-19. Blood Adv. 2021, 5, 1164–1177. [Google Scholar] [CrossRef]
- Schulte-Schrepping, J.; Reusch, N.; Paclik, D.; Baßler, K.; Schlickeiser, S.; Zhang, B.; Krämer, B.; Krammer, T.; Brumhard, S.; Bonaguro, L.; et al. Severe COVID-19 is marked by a dysregulated myeloid cell compartment. Cell 2020, 182, 1419–1440.e23. [Google Scholar] [CrossRef]
- Barnes, B.J.; Adrover, J.M.; Baxter-Stoltzfus, A.; Borczuk, A.; Cools-Lartigue, J.; Crawford, J.M.; Daßler-Plenker, J.; Guerci, P.; Huynh, C.; Knight, J.S.; et al. Targeting potential drivers of COVID-19: Neutrophil extracellular traps. J. Exp. Med. 2020, 217, e20200652. [Google Scholar] [CrossRef]
- Aschenbrenner, A.C.; Mouktaroudi, M.; Krämer, B.; Oestreich, M.; Antonakos, N.; Nuesch-Germano, M.; Gkizeli, K.; Bonaguro, L.; Reusch, N.; Baßler, K.; et al. Disease severity-specific neutrophil signatures in blood transcriptomes stratify COVID-19 patients. Genome Med. 2021, 13, 7. [Google Scholar] [CrossRef]
- Liu, J.; Liu, Y.; Xiang, P.; Pu, L.; Xiong, H.; Li, C.; Zhang, M.; Tan, J.; Xu, Y.; Song, R.; et al. Neutrophil-to-Lymphocyte Ratio Predicts Severe Illness Patients with 2019 Novel Coronavirus in the Early Stage. J. Transl. Med. 2020, 18, 206. [Google Scholar] [CrossRef]
- Hazeldine, J.; Lord, J.M. Neutrophils and COVID-19: Active Participants and Rational Therapeutic Targets. Front. Immunol. 2021, 12, 680134. [Google Scholar] [CrossRef] [PubMed]
- García de Guadiana-Romualdo, L.; Rodríguez Rojas, C.; Morell-García, D.; Andaluz-Ojeda, D.; Rodríguez Mulero, M.D.; Rodríguez-Borja, E.; Ballesteros-Vizoso, A.; Calvo, M.D.; Albert-Botella, L.; Pozo Giráldez, A.; et al. Circulating levels of calprotectin, a signature of neutrophil activation in prediction of severe respiratory failure in COVID-19 patients: A multicenter, prospective study (CalCov study). Inflamm. Res. 2022, 71, 57–67. [Google Scholar] [CrossRef]
- Templeton, A.J.; McNamara, M.G.; Šeruga, B.; Vera-Badillo, F.E.; Aneja, P.; Ocaña, A.; Leibowitz-Amit, R.; Sonpavde, G.; Knox, J.J.; Tran, B.; et al. Prognostic Role of Neutrophil-to-Lymphocyte Ratio in Solid Tumors: A Systematic Review and Meta-Analysis. J. Natl. Cancer Inst. 2014, 106, dju124. [Google Scholar] [CrossRef]
- Mackey, J.B.; Coffelt, S.B.; Carlin, L.M. Neutrophil Maturity in Cancer. Front. Immunol. 2019, 10, 1912. [Google Scholar] [CrossRef] [PubMed]
- Mezquita, L.; Preeshagul, I.; Auclin, E.; Saravia, D.; Hendriks, L.; Rizvi, H.; Park, W.; Nadal, E.; Martin-Romano, P.; Ruffinelli, J.C.; et al. Predicting immunotherapy outcomes under therapy in patients with advanced NSCLC using dNLR and its early dynamics. Eur. J. Cancer 2021, 151, 211–220. [Google Scholar] [CrossRef] [PubMed]
- Dettorre, G.M.; Dolly, S.; Loizidou, A.; Chester, J.; Jackson, A.; Mukherjee, U.; Zambelli, A.; Aguilar-Company, J.; Bower, M.; Sng, C.C.T.; et al. Systemic pro-inflammatory response identifies patients with cancer with adverse outcomes from SARS-CoV-2 infection: The OnCovid Inflammatory Score. J. Immunother. Cancer 2021, 9, e002277. [Google Scholar] [CrossRef] [PubMed]
- Cortellini, A.; Gennari, A.; Pommeret, F.; Patel, G.; Newsom-Davis, T.; Bertuzzi, A.; Viladot, M.; Aguilar-Company, J.; Mirallas, O.; Felip, E.; et al. COVID-19 Sequelae and the Host Proinflammatory Response: An Analysis From the OnCovid Registry. J. Natl. Cancer Inst. 2022, 114, 979–987. [Google Scholar] [CrossRef] [PubMed]
- Mc Millan, D.C. The systemic inflammation-based Glasgow Prognostic Score: A decade of experience in patients with cancer. Cancer Treat. Rev. 2013, 39, 534–540. [Google Scholar] [CrossRef]
- Charrier, M.; Mezquita, L.; Lueza, B.; Dupraz, L.; Planchard, D.; Remon, J.; Caramella, C.; Cassard, L.; Boselli, L.; Reiners, K.S.; et al. Circulating innate immune markers and outcomes in treatment-naïve advanced non-small cell lung cancer patients. Eur. J. Cancer 2019, 108, 88–96. [Google Scholar] [CrossRef]
- Suzuki, R.; Takagi, T.; Hikichi, T.; Konno, N.; Sugimoto, M.; Watanabe, K.O.; Nakamura, J.; Waragai, Y.; Kikuchi, H.; Takasumi, M.; et al. Derived neutrophil/lymphocyte ratio predicts gemcitabine therapy outcome in unresectable pancreatic cancer. Oncol. Lett. 2016, 11, 3441–3445. [Google Scholar] [CrossRef]
- van Kessel, K.E.; de Haan, L.M.; Fransen van de Putte, E.E.; van Rhijn, B.W.; de Wit, R.; van der Heijden, M.S.; Zwarthoff, E.C.; Boormans, J.L. Elevated derived neutrophil-to-lymphocyte ratio corresponds with poor outcomes in patients undergoing pre-operative chemotherapy in muscle-invasive bladder cancer. Bladder Cancer 2016, 2, 351–360. [Google Scholar] [CrossRef]
- Amato, R.J.; Flaherty, A.; Zhang, Y.; Ouyang, F.; Mohlere, V. Clinical prognostic factors associated with outcome in patients with renal cell cancer with prior tyrosine kinase inhibitors or immunotherapy treated with everolimus. Urol. Oncol. 2014, 32, 345–354. [Google Scholar] [CrossRef]
- Silvestre-Roig, C.; Fridlender, Z.G.; Glogauer, M.; Scapini, P. Neutrophil Diversity in Health and Disease. Trends Immunol. 2019, 40, 565–583. [Google Scholar] [CrossRef] [PubMed]
- Arasanz, H.; Bocanegra, A.I.; Morilla, I.; Fernández-Irigoyen, J.; Martínez-Aguillo, M.; Teijeira, L.; Garnica, M.; Blanco, E.; Chocarro, L.; Ausin, K.; et al. Circulating Low Density Neutrophils Are Associated with Resistance to First Line Anti-PD1/PDL1 Immunotherapy in Non-Small Cell Lung Cancer. Cancers 2022, 14, 3846. [Google Scholar] [CrossRef]
- Daix, T.; Guerin, E.; Tavernier, E.; Mercier, E.; Gissot, V.; Hérault, O.; Mira, J.P.; Dumas, F.; Chapuis, N.; Guitton, C.; et al. Multicentric standardized flow cytometry routine assessment of patients with sepsis to predict clinical worsening. Chest 2018, 154, 617–627. [Google Scholar] [CrossRef] [PubMed]
- Coffelt, S.B.; Wellenstein, M.D.; de Visser, K.E. Neutrophils in cancer: Neutral no more. Nat. Rev. Cancer 2016, 16, 431–446. [Google Scholar] [CrossRef]
- Shaul, M.E.; Eyal, O.; Guglietta, S.; Aloni, P.; Zlotnik, A.; Forkosh, E.; Levy, L.; Weber, L.M.; Levin, Y.; Pomerantz, A.; et al. Circulating neutrophil subsets in advanced lung cancer patients exhibit unique immune signature and relate to prognosis. FASEB J. 2020, 34, 4204–4218. [Google Scholar] [CrossRef] [PubMed]
- Rice, C.M.; Lewis, P.; Ponce-Garcia, F.M.; Gibbs, W.; Groves, S.; Cela, D.; Hamilton, F.; Arnold, D.; Hyams, C.; Oliver, E.; et al. Neutrophils in severe COVID-19 are characterized by a hyperactive immature state and maintained CXCR2 expression. Life Sci. Alliance 2023, 6, e202201658. [Google Scholar] [CrossRef] [PubMed]
- Carissimo, G.; Xu, W.; Kwok, I.; Abdad, M.Y.; Chan, Y.H.; Fong, S.W.; Puan, K.J.; Lee, C.Y.; Yeo, N.K.; Amrun, S.N.; et al. Whole blood immunophenotyping uncovers immature neutrophil-to-VD2 T-cell ratio as an early marker for severe COVID-19. Nat. Commun. 2020, 11, 5243. [Google Scholar] [CrossRef] [PubMed]
- Combadière, B.; Adam, L.; Guillou, N.; Quentric, P.; Rosenbaum, P.; Dorgham, K.; Bonduelle, O.; Parizot, C.; Sauce, D.; Mayaux, J.; et al. LOX-1+ immature neutrophils predict severe COVID-19 patients at risk of thrombotic complications. Front. Immunol. 2021, 12, 752612. [Google Scholar] [CrossRef]
- Townsend, L.; Dyer, A.H.; Naughton, A.; Imangaliyev, S.; Dunne, J.; Kiersey, R.; Holden, D.; Mooney, A.; Leavy, D.; Ridge, K.; et al. Severe COVID-19 is characterised by inflammation and immature myeloid cells early in disease progression. Heliyon 2022, 8, e09230. [Google Scholar] [CrossRef]
- Han, H.; Ma, Q.; Li, C.; Liu, R.; Zhao, L.; Wang, W.; Zhang, P.; Liu, X.; Gao, G.; Liu, F.; et al. Profiling serum cytokines in COVID-19 patients reveals IL-6 and IL-10 are disease severity predictors. Emerg. Microbes Infect. 2020, 9, 1123–1130. [Google Scholar] [CrossRef] [PubMed]
- Herold, T.; Jurinovic, V.; Arnreich, C.; Lipworth, B.J.; Hellmuth, J.C.; von Bergwelt-Baildon, M.; Klein, M.; Weinberger, T. Elevated levels of IL-6 and CRP predict the need for mechanical ventilation in COVID-19. J. Allergy Clin. Immunol. 2020, 146, 128–136.e4. [Google Scholar] [CrossRef] [PubMed]
- Giamarellos-Bourboulis, E.J.; Netea, M.G.; Rovina, N.; Akinosoglou, K.; Antoniadou, A.; Antonakos, N.; Damoraki, G.; Gkavogianni, T.; Adami, M.E.; Katsaounou, P.; et al. Complex Immune Dysregulation in COVID-19 Patients with Severe Respiratory Failure. Cell Host Microbe 2020, 27, 992–1000. [Google Scholar] [CrossRef] [PubMed]
- Kumari, N.; Dwarakanath, B.S.; Das, A.; Bhatt, A.N. Role of interleukin-6 in cancer progression and therapeutic resistance. Tumour Biol. 2016, 37, 11553–11572. [Google Scholar] [CrossRef]
- Weber, R.; Groth, C.; Lasser, S.; Arkhypov, I.; Petrova, V.; Altevogt, P.; Utikal, J.; Umansky, V.I. IL-6 as a major regulator of MDSC activity and possible target for cancer immunotherapy. Cell Immunol. 2021, 359, 104254. [Google Scholar] [CrossRef]
- Huseni, M.A.; Wang, L.; Klementowicz, J.E.; Yuen, K.; Breart, B.; Orr, C.; Liu, L.F.; Li, Y.; Gupta, V.; Li, C.; et al. CD8+ T cell-intrinsic IL-6 signaling promotes resistance to anti-PD-L1 immunotherapy. Cell Rep. Med. 2023, 4, 100878. [Google Scholar] [CrossRef] [PubMed]
- RECOVERY Collaborative Group. Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): A randomised, controlled, open-label, platform trial. Lancet 2021, 397, 1637–1645. [Google Scholar]
- The REMAP-CAP Investigators. Interleukin-6 Receptor Antagonists in Critically Ill Patients with COVID-19. N. Engl. J. Med. 2021, 384, 1491–1502. [Google Scholar] [CrossRef]
- Seguí, E.; Auclin, E.; Casadevall, D.; Aguilar-Company, J.; Rodriguez, M.; Epaillard, N.; Tagliamento, M.; Pilotto, S.; López-Castro, R.; Mielgo, X.; et al. Change of circulating pro-inflammatory markers between preCOVID-19 condition and COVID-19 diagnosis predicts early death in cancer patients: The FLARE score. Ann. Oncol. 2020, 31, S1008. [Google Scholar] [CrossRef]
- Seguí, E.; Torres, J.M.; Auclin, E.; Casadevall, D.; Aguilar-Company, J.; Rodríguez, M.; Epaillard, N.; Gavira, J.; Tapia, J.C.; Tagliamento, M.; et al. The FLARE score, circulating neutrophils, and association with COVID-19 outcomes in patients with solid tumors. J. Clin. Oncol. 2022, 40, 2551. [Google Scholar] [CrossRef]



| (A) | |||||
| FLARE T−/I− | FLARE T−/I+ | FLARE T+/I− | FLARE T+/I+ | p-Value | |
| (n = 140) | (n = 136) | (n = 74) | (n = 19) | ||
| Age (median; range) | 68 (39–93) | 69 (41–96) | 69 (37–88) | 69 (43–82) | 0.852 |
| Gender: male | 60 (43%) | 90 (66%) | 41 (55%) | 12 (63%) | 0.001 |
| Current or former smoker | 73 (53%) | 86 (65%) | 44 (62%) | 7 (44%) | --- |
| ECOG PS ≤1 | 111 (80%) | 103 (82%) | 44 (62%) | 14 (78%) | <0.001 |
| Comorbidity | |||||
| Hypertension | 67 (48%) | 60 (44%) | 43 (60%) | 11 (58%) | 0.166 |
| Cardiovascular | 33 (24%) | 24 (18%) | 16 (22%) | 5 (26%) | 0.613 |
| Cancer type | |||||
| Thoracic | 31 (22%) | 40 (30%) | 28 (38%) | 5 (26%) | --- |
| Genitourinary | 15 (11%) | 17 (13%) | 9 (12%) | 3 (16%) | --- |
| Gastrointestinal | 37 (27%) | 33 (25%) | 15 (20%) | 5 (26%) | --- |
| Breast | 30 (22%) | 20 (15%) | 7 (9%) | 3 (16%) | --- |
| Active tumor at diagnosis | 98 (70%) | 103 (75.7%) | 62 (83.8%) | 19 (100%) | 0.005 |
| Advanced stage | 88 (63%) | 94 (69%) | 62 (84%) | 18 (95%) | --- |
| Systemic therapy | 89 (64%) | 83 (61%) | 45 (62%) | 15 (79%) | 0.518 |
| Chemotherapy | 59 (54%) | 47 (55%) | 28 (58%) | 13 (87%) | 0.143 |
| Immunotherapy | 17 (19%) | 12 (14%) | 9 (19%) | 1 (7%) | 0.637 |
| Circulating inflammatory biomarkers prior to COVID-19 diagnosis | |||||
| Platelets (109/L) (median, IQR) | 243 (166.8–292.8) | 223.5 (188–295.25) | 268 (194–423) | 280 (209.5–313.5) | 0.011 |
| LDH (U/L) | 196 (171.5–265) | 202 [167;279] | 239 (183.5–353) | 196 (171.5–265) | 0.025 |
| (median, IQR) | |||||
| Albumin (g/L) | 41 (38–43) | 41 (36–43) | 35.7 (32–39) | 35.4 (30.7–38.5) | 0.001 |
| (median, IQR) | |||||
| COVID-19 symptoms at diagnosis | |||||
| Fever | 97 (69%) | 97 (71%) | 47 (64%) | 13 (68%) | 0.782 |
| Cough | 80 (58%) | 68 (50%) | 39 (53%) | 8 (42%) | 0.494 |
| Dyspnea | 59 (42%) | 64 (47%) | 40 (54%) | 12 (63%) | 0.207 |
| COVID-19 treatment | |||||
| Antibiotics | 99 (73%) | 115 (86%) | 59 (80%) | 16 (89%) | 0.045 |
| Antiviral therapy | 29 (31%) | 37 (38%) | 18 (32%) | 4 (25%) | 0.21 |
| Steroids | 32 (24%) | 27 (21%) | 28 (38%) | 8 (44%) | --- |
| Immunomodulators | 7 (7%) | 12 (13%) | 5 (9%) | 4 (31%) | 0.081 |
| Median hospital stay duration (range) | 18.5 (4–57) | 11.5 (2–44) | 18 (2–73) | 6 (2–23) | 0.177 |
| (B) | |||||
| FLARE T−/I− | FLARE T−/I+ | FLARE T+/I− | FLARE T+/I+ | p-Value | |
| (n = 140) | (n = 136) | (n = 74) | (n = 19) | ||
| Admission to ICU | 7 (8 %) | 11 (14%) | 7 (15%) | 2 (18%) | 0.425 |
| Severe acute respiratory failure | 25 (18%) | 36 (27%) | 18 (24%) | no | 0.275 |
| COVID-19 complications | 67 (54%) | 91 (75%) | 53 (79%) | 14 (88%) | <0.001 |
| 30-day mortality | 29 (23%) | 42 (33%) | 27 (39%) | 13 (68%) | <0.001 |
| FLARE # | Age | Gender | Cancer-Type | Stage | ECOG PS | Days Since Diagnosis | dNLR | Immature Neutrophils (%) | IL-6 | COVID-19 Severity | 30-Day Mortality |
|---|---|---|---|---|---|---|---|---|---|---|---|
| FLARE #1 | 66 | Female | Colorectal | IV | 2 | D + 6 | 2.66 | - | - | Moderate | No |
| FLARE #2 | 60 | Male | Prostate | IV | 1 | D + 10 | 4.63 | - | - | Moderate | No |
| FLARE #3 | 82 | Male | Prostate | IV | 1 | D + 3 | 0.19 | - | - | Moderate | No |
| FLARE #4 | 61 | Male | Bladder | IV | 2 | D + 15 | 10.73 | - | - | Severe | Yes |
| FLARE #5 | 49 | Male | Suprarenal | IV | 0 | D + 3 | 2.31 | 1.03 | 0 | Moderate | No |
| FLARE #6 | 65 | Female | Breast | IV | 1 | D + 2 | 2.59 | 2.72 | 21.93 | Severe | No |
| D + 6 | 2.92 | 3.09 | 41.37 | ||||||||
| FLARE #7 | 66 | Female | Lung | IV | 3 | D + 3 | 18.69 | 1.15 | 22.76 | Severe | Yes |
| FLARE #8 | 59 | Male | Esophagus | IV | 1 | D + 3 | 0.47 | 0.15 | - | As/Mild | No |
| 2.21 | 0.59 | - | |||||||||
| FLARE #9 | 57 | Male | Colorectal | IV | 0 | D + 5 | 0.27 | 4.48 | 21.04 | As/Mild | No |
| FLARE #10 | 77 | Female | Gastric | III | 2 | D + 9 | 6.42 | 0.23 | - | As/Mild | No |
| FLARE #11 | 56 | Female | Breast | IV | 2 | D + 2 | 8.49 | 0.71 | - | Moderate | No |
| D + 9 | 12.4 | 2.14 | - | ||||||||
| D + 16 | 12.53 | 1.4 | 0 | ||||||||
| FLARE #12 | 55 | Female | Colorectal | IV | 1 | D + 1 | 3.21 | 2.19 | 188.85 | As/Mild | No |
| FLARE #13 | 74 | Female | Lung | II | 2 | D + 1 | 1.97 | 2.01 | 0 | As/Mild | No |
| D + 8 | 1.72 | - | - | ||||||||
| FLARE #14 | 61 | Female | Ovarian | IV | 1 | D + 8 | 1.41 | 2.39 | 158.69 | As/Mild | No |
| FLARE #15 | 60 | Male | Bladder | IV | 2 | D + 2 | 7.72 | 5.33 | - | Severe | No |
| D + 5 | 10.88 | 1.17 | 50.4 | ||||||||
| D + 9 | 49.13 | 97.6 | 895.93 | ||||||||
| FLARE #16 | 58 | Male | Head and Neck | III | 1 | D + 3 | 2.74 | 3.64 | 0 | As/Mild | No |
| D + 7 | 2.55 | 8.93 | 00 | ||||||||
| D + 19 | 3.31 | - | - | ||||||||
| FLARE #17 | 73 | Male | Esophagus | IV | 3 | D + 4 | 7.96 | 4.58 | 676.46 | Severe | Yes |
| FLARE #18 | 71 | Male | Thyroid | IV | 1 | D + 4 | 2.61 | 1.42 | 11.43 | Moderate | No |
| FLARE #19 | 54 | Female | Lung | IV | 1 | D + 15 | 2.69 | 0.82 | 0 | Moderate | No |
| D + 46 | 3.28 | 1.12 | - | ||||||||
| FLARE #20 | 77 | Female | Breast | IV | 3 | D + 16 | 2.77 | 9.75 | 116.25 | Severe | No |
| D + 23 | 6.32 | 4.64 | 55.676 | ||||||||
| D + 25 | 6.32 | 3.02 | 138.22 | ||||||||
| FLARE #21 | 72 | Female | Lung | IV | 1 | D + 4 | 1.22 | 94 | 17.83 | Moderate | No |
| FLARE #22 | 55 | Female | Ovarian | IV | 1 | D + 3 | 1.31 | 0.28 | 11.43 | As/Mild | No |
| FLARE #23 | 73 | Female | Head and Neck | III | 3 | D + 8 | 10.52 | 16 | 118.09 | Severe | No |
| D + 10 | 4.64 | 10.1 | 421.18 | ||||||||
| D + 17 | 3.95 | - | - | ||||||||
| FLARE #24 | 50 | Female | Breast | IV | 1 | D + 12 | 2.83 | 1.23 | 0 | As/Mild | No |
| D + 45 | 1.18 | 2.55 | - | ||||||||
| FLARE #25 | 62 | Male | Head and Neck | III | 1 | D + 3 | 12.86 | 36.8 | - | Severe | No |
| D + 10 | 4.11 | 2.08 | 0 | ||||||||
| FLARE #27 | 81 | Male | Lung | IV | 2 | D + 4 | 3.91 | 0.96 | 11.43 | Severe | Yes |
| FLARE #28 | 65 | Female | Renal | IV | 0 | D + 8 | 0.74 | - | - | As/Mild | No |
| FLARE #29 | 72 | Male | Prostate | IV | 2 | D + 2 | 6.59 | 0.46 | 31.07 | Moderate | No |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seguí, E.; Torres, J.M.; Auclin, E.; Casadevall, D.; Peiro Carmona, S.; Aguilar-Company, J.; García de Herreros, M.; Gorría, T.; Laguna, J.C.; Rodríguez, M.; et al. The FLARE Score and Circulating Neutrophils in Patients with Cancer and COVID-19 Disease. Cancers 2024, 16, 2974. https://doi.org/10.3390/cancers16172974
Seguí E, Torres JM, Auclin E, Casadevall D, Peiro Carmona S, Aguilar-Company J, García de Herreros M, Gorría T, Laguna JC, Rodríguez M, et al. The FLARE Score and Circulating Neutrophils in Patients with Cancer and COVID-19 Disease. Cancers. 2024; 16(17):2974. https://doi.org/10.3390/cancers16172974
Chicago/Turabian StyleSeguí, Elia, Juan Manuel Torres, Edouard Auclin, David Casadevall, Sara Peiro Carmona, Juan Aguilar-Company, Marta García de Herreros, Teresa Gorría, Juan Carlos Laguna, Marta Rodríguez, and et al. 2024. "The FLARE Score and Circulating Neutrophils in Patients with Cancer and COVID-19 Disease" Cancers 16, no. 17: 2974. https://doi.org/10.3390/cancers16172974






