Thermosensitive Liposomes for Gemcitabine Delivery to Pancreatic Ductal Adenocarcinoma
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Carboxyfluorescein Thermosensitive Liposome Manufacturing and Release
2.3. Gemcitabine-Loaded Thermosensitive Liposome Manufacturing and Release
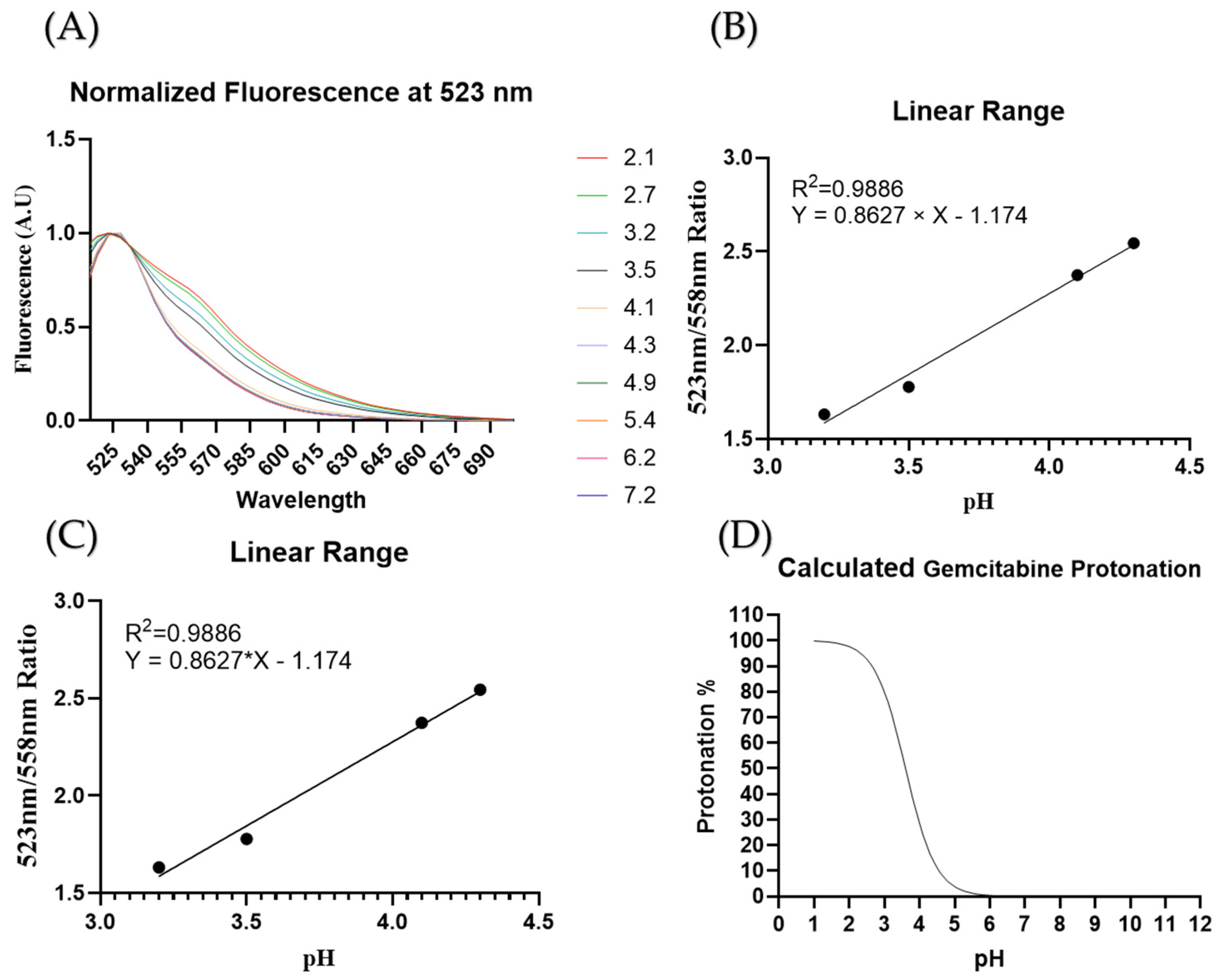
2.4. Intraliposomal pH Measurements
2.5. Cell Culture
2.6. Cell Hyperthermia Treatment
2.7. Statistical Analysis
3. Results
3.1. Liposome Characterization
3.2. Liposome Stability
3.3. Encapsulation Efficiency
3.4. In Vitro Viability Studies
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Orth, M.; Metzger, P.; Gerum, S.; Mayerle, J.; Schneider, G.; Belka, C.; Schnurr, M.; Lauber, K. Pancreatic Ductal Adenocarcinoma: Biological Hallmarks, Current Status, and Future Perspectives of Combined Modality Treatment Approaches. Radiat. Oncol. 2019, 14, 141. [Google Scholar] [CrossRef]
- Angstadt, S.; Zhu, Q.; Jaffee, E.M.; Robinson, D.N.; Anders, R.A. Pancreatic Ductal Adenocarcinoma Cortical Mechanics and Clinical Implications. Front. Oncol. 2022, 12, 809179. [Google Scholar] [CrossRef]
- Placido, D.; Yuan, B.; Hjaltelin, J.X.; Zheng, C.; Haue, A.D.; Chmura, P.J.; Yuan, C.; Kim, J.; Umeton, R.; Antell, G.; et al. A Deep Learning Algorithm to Predict Risk of Pancreatic Cancer from Disease Trajectories. Nat. Med. 2023, 29, 1113–1122. [Google Scholar] [CrossRef] [PubMed]
- Bakasa, W.; Viriri, S. Pancreatic Cancer Survival Prediction: A Survey of the State-of-the-Art. Comput. Math. Methods Med. 2021, 2021, 1188414. [Google Scholar] [CrossRef]
- Freelove, R.; Walling, A.D. Pancreatic Cancer: Diagnosis and Management. Am. Fam. Physician 2006, 73, 485–492. [Google Scholar]
- Zhang, L.; Sanagapalli, S.; Stoita, A. Challenges in Diagnosis of Pancreatic Cancer. World J. Gastroenterol. 2018, 24, 2047–2060. [Google Scholar] [CrossRef]
- Barreto, S.G.; Shukla, P.J.; Shrikhande, S.V. Tumors of the Pancreatic Body and Tail. World J. Oncol. 2010, 1, 52–65. [Google Scholar] [CrossRef] [PubMed]
- Wei, K.; Hackert, T. Surgical Treatment of Pancreatic Ductal Adenocarcinoma. Cancers 2021, 13, 1971. [Google Scholar] [CrossRef] [PubMed]
- Sarantis, P.; Koustas, E.; Papadimitropoulou, A.; Papavassiliou, A.G.; Karamouzis, M.V. Pancreatic Ductal Adenocarcinoma: Treatment Hurdles, Tumor Microenvironment and Immunotherapy. World J. Gastrointest. Oncol. 2020, 12, 173–181. [Google Scholar] [CrossRef]
- Regine, W.F.; Winter, K.A.; Abrams, R.A.; Safran, H.; Hoffman, J.P.; Konski, A.; Benson, A.B.; Macdonald, J.S.; Kudrimoti, M.R.; Fromm, M.L.; et al. Fluorouracil vs Gemcitabine Chemotherapy before and after Fluorouracil-Based Chemoradiation Following Resection of Pancreatic Adenocarcinoma: A Randomized Controlled Trial. JAMA 2008, 299, 1019–1026. [Google Scholar] [CrossRef]
- Brunner, M.; Wu, Z.; Krautz, C.; Pilarsky, C.; Grützmann, R.; Weber, G.F. Current Clinical Strategies of Pancreatic Cancer Treatment and Open Molecular Questions. Int. J. Mol. Sci. 2019, 20, 4543. [Google Scholar] [CrossRef] [PubMed]
- Ciccolini, J.; Serdjebi, C.; Peters, G.J.; Giovannetti, E. Pharmacokinetics and Pharmacogenetics of Gemcitabine as a Mainstay in Adult and Pediatric Oncology: An EORTC-PAMM Perspective. Cancer Chemother. Pharmacol. 2016, 78, 1–12. [Google Scholar] [CrossRef]
- Cai, H.; Wang, R.; Guo, X.; Song, M.; Yan, F.; Ji, B.; Liu, Y. Combining Gemcitabine-Loaded Macrophage-like Nanoparticles and Erlotinib for Pancreatic Cancer Therapy. Mol. Pharm. 2021, 18, 2495–2506. [Google Scholar] [CrossRef]
- Chen, Y. Development of a Novel Ionic Liquid Based Microemulsion System for Gemcitabine Hydrochloride and in Vitro Evaluation in Human Cervical Cancer HeLa Cells. Indian. J. Pharm. Educ. Res. 2021, 55, 685–691. [Google Scholar] [CrossRef]
- Tucci, S.T.; Kheirolomoom, A.; Ingham, E.S.; Mahakian, L.M.; Tam, S.M.; Foiret, J.; Hubbard, N.E.; Borowsky, A.D.; Baikoghli, M.; Cheng, R.H.; et al. Tumor-Specific Delivery of Gemcitabine with Activatable Liposomes. J. Control. Release Off. J. Control. Release Soc. 2019, 309, 277–288. [Google Scholar] [CrossRef] [PubMed]
- Nurgali, K.; Jagoe, R.T.; Abalo, R. Editorial: Adverse Effects of Cancer Chemotherapy: Anything New to Improve Tolerance and Reduce Sequelae? Front. Pharmacol. 2018, 9, 245. [Google Scholar] [CrossRef]
- Wei, X.; Shamrakov, D.; Nudelman, S.; Peretz-Damari, S.; Nativ-Roth, E.; Regev, O.; Barenholz, Y. Cardinal Role of Intraliposome Doxorubicin-Sulfate Nanorod Crystal in Doxil Properties and Performance. ACS Omega 2018, 3, 2508–2517. [Google Scholar] [CrossRef] [PubMed]
- Sivadasan, D.; Sultan, M.H.; Madkhali, O.A.; Alsabei, S.H.; Alessa, A.A. Stealth Liposomes (PEGylated) Containing an Anticancer Drug Camptothecin: In Vitro Characterization and In Vivo Pharmacokinetic and Tissue Distribution Study. Molecules 2022, 27, 1086. [Google Scholar] [CrossRef]
- Storm, G.; Woodle, M.C. Long Circulating Liposome Therapeutics: From Concept to Clinical Reality. In Long Circulating Liposomes: Old Drugs, New Therapeutics; Woodle, M.C., Storm, G., Eds.; Springer: Berlin/Heidelberg, Germany, 1998; pp. 3–16. [Google Scholar] [CrossRef]
- Lombardo, D.; Kiselev, M.A. Methods of Liposomes Preparation: Formation and Control Factors of Versatile Nanocarriers for Biomedical and Nanomedicine Application. Pharmaceutics 2022, 14, 543. [Google Scholar] [CrossRef]
- Hassan, T.; Jinho, P.; Hytham, H.G.; Masters, A.R.; Abdel-Aleem, J.A.; Abdelrahman, S.I.; Abdelrahman, A.A.; Lyle, L.T.; Yeo, Y. Development of Liposomal Gemcitabine with High Drug Loading Capacity. Mol. Pharm. 2019, 16, 2858–2871. [Google Scholar] [CrossRef]
- Li, M.; Jiang, S.; Simon, J.; Paßlick, D.; Frey, M.-L.; Wagner, M.; Mailänder, V.; Crespy, D.; Landfester, K. Brush Conformation of Polyethylene Glycol Determines the Stealth Effect of Nanocarriers in the Low Protein Adsorption Regime. Nano Lett. 2021, 21, 1591–1598. [Google Scholar] [CrossRef] [PubMed]
- Amoozgar, Z.; Yeo, Y. Recent Advances in Stealth Coating of Nanoparticle Drug Delivery Systems. WIREs Nanomed. Nanobiotechnology 2012, 4, 219–233. [Google Scholar] [CrossRef]
- Wu, J. The Enhanced Permeability and Retention (EPR) Effect: The Significance of the Concept and Methods to Enhance Its Application. J. Pers. Med. 2021, 11, 771. [Google Scholar] [CrossRef] [PubMed]
- Maeda, H.; Nakamura, H.; Fang, J. The EPR Effect for Macromolecular Drug Delivery to Solid Tumors: Improvement of Tumor Uptake, Lowering of Systemic Toxicity, and Distinct Tumor Imaging in Vivo. Adv. Drug Deliv. Rev. 2013, 65, 71–79. [Google Scholar] [CrossRef]
- Torchilin, V. Tumor Delivery of Macromolecular Drugs Based on the EPR Effect. Adv. Drug Deliv. Rev. 2011, 63, 131–135. [Google Scholar] [CrossRef]
- Miao, L.; Lin, C.M.; Huang, L. Stromal Barriers and Strategies for the Delivery of Nanomedicine to Desmoplastic Tumors. J. Control. Release Off. J. Control. Release Soc. 2015, 219, 192–204. [Google Scholar] [CrossRef] [PubMed]
- Chintamaneni, P.K.; Pindiprolu, S.K.S.S.; Swain, S.S.; Karri, V.V.S.R.; Nesamony, J.; Chelliah, S.; Bhaskaran, M. Conquering Chemoresistance in Pancreatic Cancer: Exploring Novel Drug Therapies and Delivery Approaches amidst Desmoplasia and Hypoxia. Cancer Lett. 2024, 588, 216782. [Google Scholar] [CrossRef]
- Seynhaeve, A.L.B.; Amin, M.; Haemmerich, D.; van Rhoon, G.C.; ten Hagen, T.L.M. Hyperthermia and Smart Drug Delivery Systems for Solid Tumor Therapy. Adv. Drug Deliv. Rev. 2020, 163–164, 125–144. [Google Scholar] [CrossRef] [PubMed]
- Jin, Y.; Liang, X.; An, Y.; Dai, Z. Microwave-Triggered Smart Drug Release from Liposomes Co-Encapsulating Doxorubicin and Salt for Local Combined Hyperthermia and Chemotherapy of Cancer. Bioconjug. Chem. 2016, 27, 2931–2942. [Google Scholar] [CrossRef]
- Fleige, E.; Quadir, M.A.; Haag, R. Stimuli-Responsive Polymeric Nanocarriers for the Controlled Transport of Active Compounds: Concepts and Applications. Adv. Drug Deliv. Rev. 2012, 64, 866–884. [Google Scholar] [CrossRef]
- Kong, G.; Braun, R.D.; Dewhirst, M.W. Characterization of the Effect of Hyperthermia on Nanoparticle Extravasation from Tumor Vasculature. Cancer Res. 2001, 61, 3027–3032. [Google Scholar] [PubMed]
- Vaupel, P.; Piazena, H.; Notter, M.; Thomsen, A.R.; Grosu, A.-L.; Scholkmann, F.; Pockley, A.G.; Multhoff, G. From Localized Mild Hyperthermia to Improved Tumor Oxygenation: Physiological Mechanisms Critically Involved in Oncologic Thermo-Radio-Immunotherapy. Cancers 2023, 15, 1394. [Google Scholar] [CrossRef]
- Shevtsov, M.; Multhoff, G. Heat Shock Protein–Peptide and HSP-Based Immunotherapies for the Treatment of Cancer. Front. Immunol. 2016, 7, 171. [Google Scholar] [CrossRef] [PubMed]
- Deng, Z.-S.; Liu, J. Chemothermal Therapy for Localized Heating and Ablation of Tumor. J. Healthc. Eng. 2013, 4, 409–425. [Google Scholar] [CrossRef]
- Gabizon, A.A.; Shmeeda, H.; Zalipsky, S. Pros and Cons of the Liposome Platform in Cancer Drug Targeting. J. Liposome Res. 2006, 16, 175–183. [Google Scholar] [CrossRef]
- Gupta, S.; De Mel, J.U.; Schneider, G.J. Dynamics of Liposomes in the Fluid Phase. Curr. Opin. Colloid. Interface Sci. 2019, 42, 121–136. [Google Scholar] [CrossRef]
- Keller, D.; Larsen, N.B.; Møller, I.M.; Mouritsen, O.G. Decoupled Phase Transitions and Grain-Boundary Melting in Supported Phospholipid Bilayers. Phys. Rev. Lett. 2005, 94, 025701. [Google Scholar] [CrossRef]
- Lu, T.; ten Hagen, T.L.M. Inhomogeneous Crystal Grain Formation in DPPC-DSPC Based Thermosensitive Liposomes Determines Content Release Kinetics. J. Control. Release 2017, 247, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Motamarry, A.; Wolfe, A.M.; Ramajayam, K.K.; Pattanaik, S.; Benton, T.; Peterson, Y.; Faridi, P.; Prakash, P.; Twombley, K.; Haemmerich, D. Extracorporeal Removal of Thermosensitive Liposomal Doxorubicin from Systemic Circulation after Tumor Delivery to Reduce Toxicities. Cancers 2022, 14, 1322. [Google Scholar] [CrossRef] [PubMed]
- DiCiccio, J.E.; Steinberg, B.E. Lysosomal pH and Analysis of the Counter Ion Pathways That Support Acidification. J. Gen. Physiol. 2011, 137, 385–390. [Google Scholar] [CrossRef]
- Chamani, F.; Pyle, M.M.; Shrestha, T.B.; Sebek, J.; Bossmann, S.H.; Basel, M.T.; Sheth, R.A.; Prakash, P. In Vitro Measurement and Mathematical Modeling of Thermally-Induced Injury in Pancreatic Cancer Cells. Cancers 2023, 15, 655. [Google Scholar] [CrossRef] [PubMed]
- Kaasgaard, T.; Leidy, C.; Crowe, J.H.; Mouritsen, O.G.; Jørgensen, K. Temperature-Controlled Structure and Kinetics of Ripple Phases in One- and Two-Component Supported Lipid Bilayers. Biophys. J. 2003, 85, 350–360. [Google Scholar] [CrossRef] [PubMed]
- Tataranni, T.; Agriesti, F.; Ruggieri, V.; Mazzoccoli, C.; Simeon, V.; Laurenzana, I.; Scrima, R.; Pazienza, V.; Capitanio, N.; Piccoli, C. Rewiring Carbohydrate Catabolism Differentially Affects Survival of Pancreatic Cancer Cell Lines with Diverse Metabolic Profiles. Oncotarget 2017, 8, 41265–41281. [Google Scholar] [CrossRef] [PubMed]
- Michalopoulou, E.; Auciello, F.R.; Bulusu, V.; Strachan, D.; Campbell, A.D.; Tait-Mulder, J.; Karim, S.A.; Morton, J.P.; Sansom, O.J.; Kamphorst, J.J. Macropinocytosis Renders a Subset of Pancreatic Tumor Cells Resistant to mTOR Inhibition. Cell Rep. 2020, 30, 2729–2742.e4. [Google Scholar] [CrossRef]
- Katsuta, E.; Qi, Q.; Peng, X.; Hochwald, S.N.; Yan, L.; Takabe, K. Pancreatic Adenocarcinomas with Mature Blood Vessels Have Better Overall Survival. Sci. Rep. 2019, 9, 1310. [Google Scholar] [CrossRef]

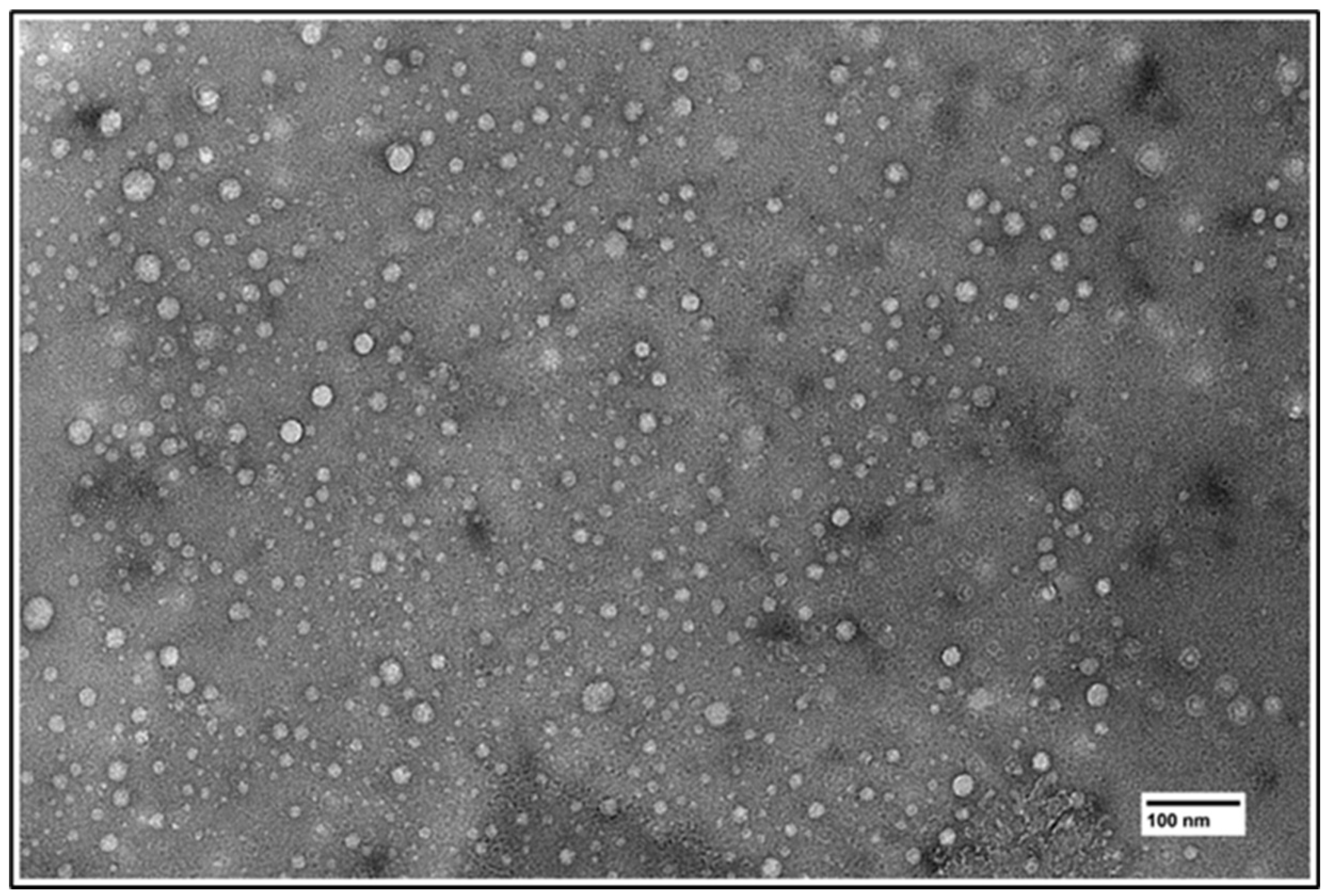



| DPPC Content | Size (nm) | PDI | Z-Potential (mV) |
|---|---|---|---|
| 65% | 125.7 ± 2.5 | 0.058 ± 0.010 | −1.89 |
| 70% | 123.3 ± 3.1 | 0.092 ± 0.022 | −2.31 |
| 75% | 119.1 ± 3.6 | 0.040 ± 0.009 | −2.17 |
| 80% | 114.7 ± 3.5 | 0.083 ± 0.013 | −1.82 |
| 85% | 124.8 ± 3.4 | 0.049 ± 0.027 | −2.24 |
| 90% | 124.8 ± 3.2 | 0.052 ± 0.024 | −1.97 |
| Pre-Column | Post-Column | |
|---|---|---|
| 523/558 | 1.5 | 2.3 |
| Calculated pH | 3.2 | 4.2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aparicio-Lopez, C.B.; Timmerman, S.; Lorino, G.; Rogers, T.; Pyle, M.; Shrestha, T.B.; Basel, M.T. Thermosensitive Liposomes for Gemcitabine Delivery to Pancreatic Ductal Adenocarcinoma. Cancers 2024, 16, 3048. https://doi.org/10.3390/cancers16173048
Aparicio-Lopez CB, Timmerman S, Lorino G, Rogers T, Pyle M, Shrestha TB, Basel MT. Thermosensitive Liposomes for Gemcitabine Delivery to Pancreatic Ductal Adenocarcinoma. Cancers. 2024; 16(17):3048. https://doi.org/10.3390/cancers16173048
Chicago/Turabian StyleAparicio-Lopez, Cesar B., Sarah Timmerman, Gabriella Lorino, Tatiana Rogers, Marla Pyle, Tej B. Shrestha, and Matthew T. Basel. 2024. "Thermosensitive Liposomes for Gemcitabine Delivery to Pancreatic Ductal Adenocarcinoma" Cancers 16, no. 17: 3048. https://doi.org/10.3390/cancers16173048






