Therapeutic Advances in Advanced Basal Cell Carcinoma
Abstract
Simple Summary
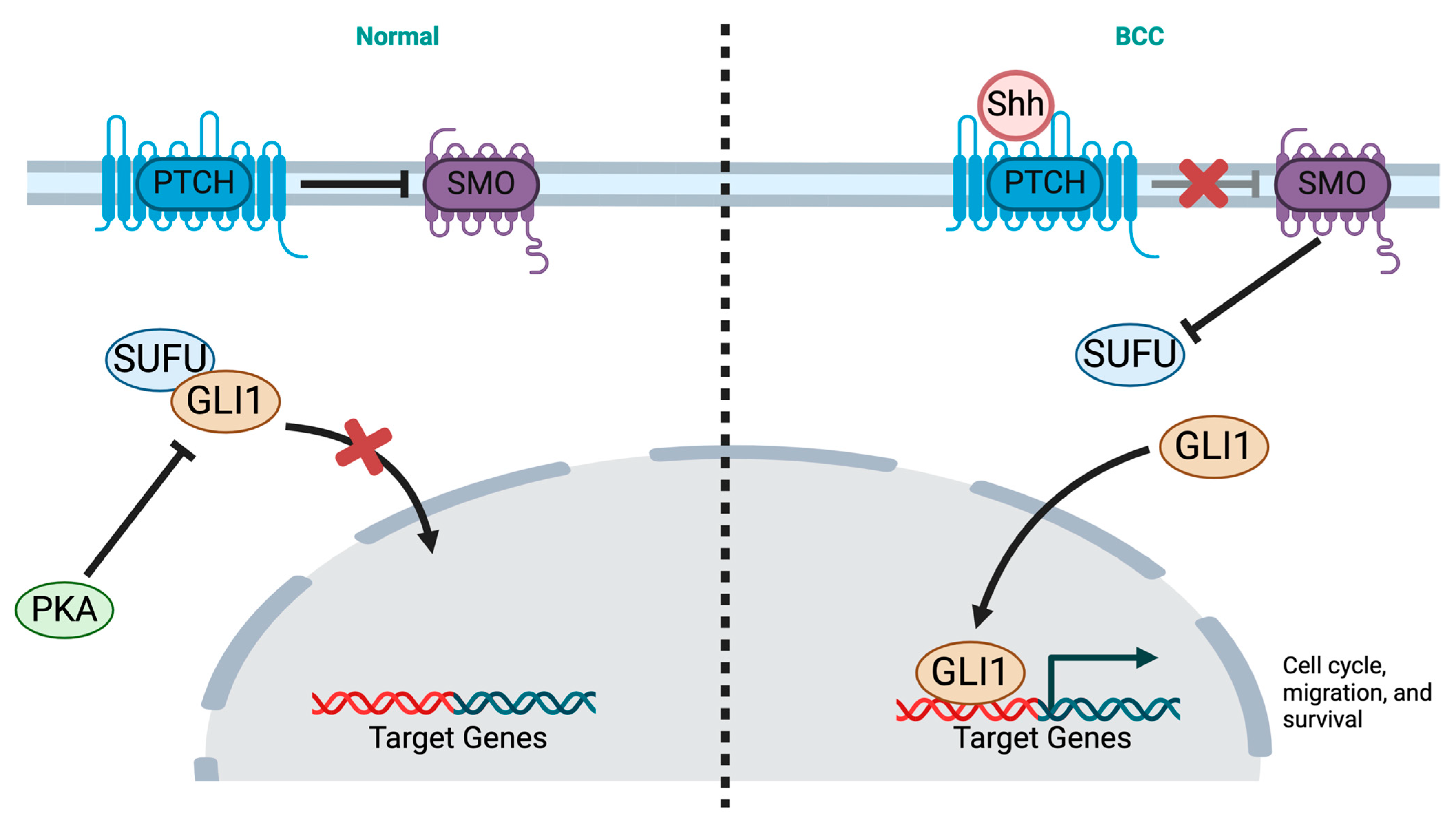
Abstract
1. Introduction
2. Risk Factors and Subtypes
3. Pathogenesis and Genetics
4. Tumor Microenvironment in Advanced BCC
5. Approved Therapies in Advanced BCC
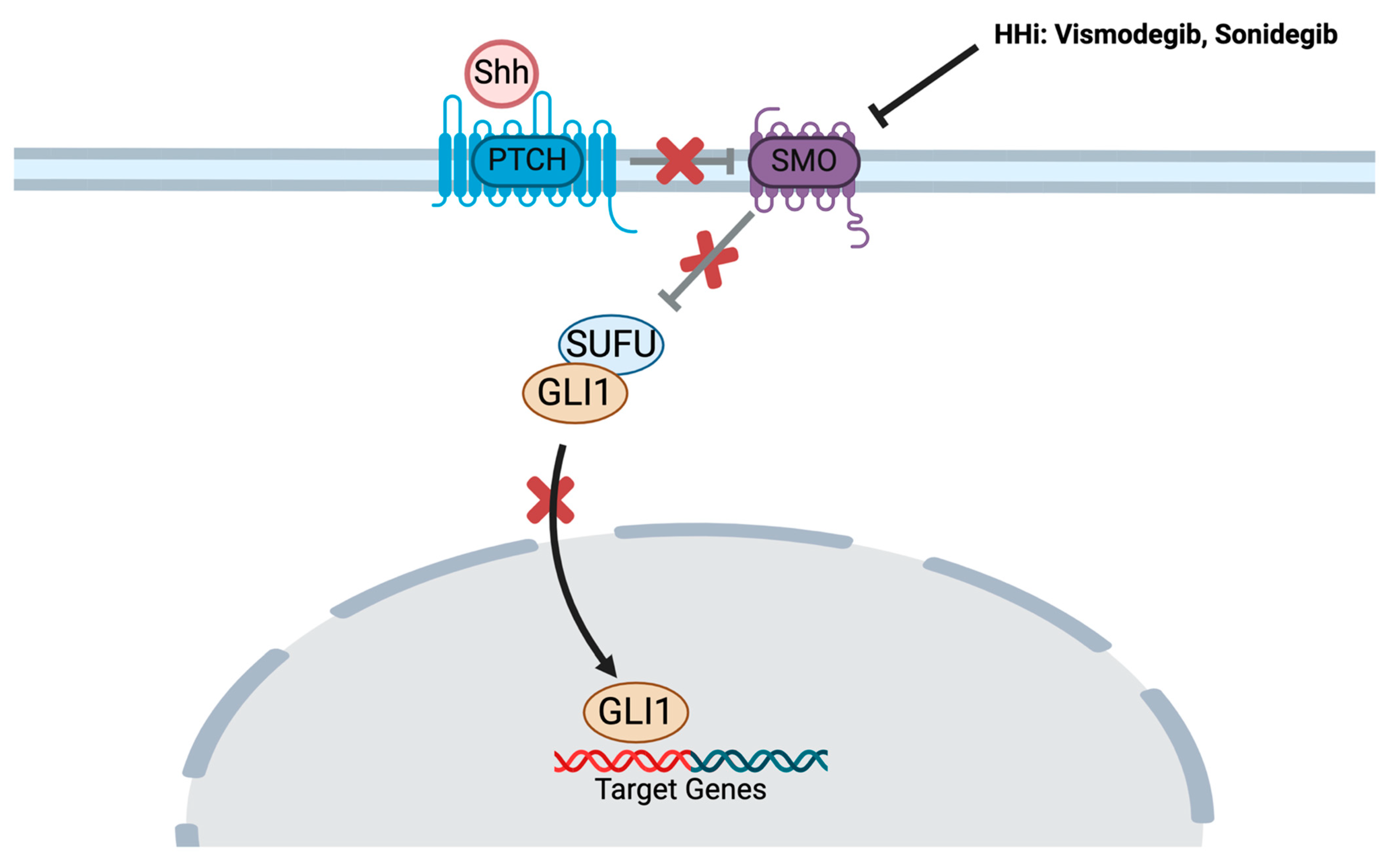
5.1. Hedgehog Pathway Inhibitors
5.1.1. Vismodegib
5.1.2. Sonidegib
5.2. Immune Checkpoint Inhibition
| Trial | NCT | Results | |
|---|---|---|---|
| Vismodegib | ERIVANCE [46,47] | 00833417 | - ORR: 43% (la-BCC), 30% (mBCC) - mPFS: 12.9 months (la-BCC), 9.3 months (mBCC) - mOS: not reached (la-BCC), 33.4 months (mBCC) |
| STEVIE [48] | 01367665 | - ORR: 68.5% (la-BCC), 36.9% (mBCC) - mPFS: 23.2 months (la-BCC), 13.1 months (mBCC) | |
| Sonidegib | BOLT [56,57] | 01327053 | 30-month analysis (200 mg) |
| - ORR: 71.2% (la-BCC), 33% (mBCC) | |||
| - Median DOR: 15.7 months (la-BCC), 18.1 months (mBCC) | |||
| 42-month analysis (200 mg) | |||
| - ORR: 56% (la-BCC), 8% in mBCC | |||
| Cemiplimab | [61,62] | 03132636 | - ORR: 31% - mBCC: ORR 22%, mPFS 10 months, mOS 50 months |
5.2.1. Resistance to Immunotherapy
5.2.2. Predictive Markers for Response to Immunotherapy
6. Ongoing Clinical Trials in Advanced BCC
- Cemiplimab
- Pembrolizumab
- Nivolumab
- Vismodegib
- Novel Intra-Tumoral Therapies
- Other Novel Therapies
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Ju, S.; Fan, W.; Rokohl, A.C.; Guo, Y.; Kakkassery, V.; Heindl, L.M. Genetic factors underlying basal cell carcinoma risk: A narrative review. Front. Oral. Maxillofac. Med. 2023, 5, 20. [Google Scholar] [CrossRef]
- Morgan, F.C.; Ruiz, E.S.; Karia, P.S.; Besaw, R.J.; Neel, V.A.; Schmults, C.D. Brigham and Women’s Hospital tumor classification system for basal cell carcinoma identifies patients with risk of metastasis and death. J. Am. Acad. Dermatol. 2021, 85, 582–587. [Google Scholar] [CrossRef]
- Skin Cancer Foundation-Basal Cell Carcinoma Overview. Available online: https://www.skincancer.org/skin-cancer-information/basal-cell-carcinoma/ (accessed on 31 March 2024).
- Naik, P.P.; Desai, M.B. Basal Cell Carcinoma: A Narrative Review on Contemporary Diagnosis and Management. Oncol. Ther. 2022, 10, 317–335. [Google Scholar] [CrossRef]
- Teng, Y.; Yu, Y.; Li, S.; Huang, Y.; Xu, D.; Tao, X.; Fan, Y. Ultraviolet Radiation and Basal Cell Carcinoma: An Environmental Perspective. Front. Public Health 2021, 9, 666528. [Google Scholar] [CrossRef]
- Christenson, L.J. Incidence of Basal Cell and Squamous Cell Carcinomas in a Population Younger Than 40 Years. JAMA 2005, 294, 681. [Google Scholar] [CrossRef] [PubMed]
- Mohan, S.V.; Chang, A.L.S. Advanced Basal Cell Carcinoma: Epidemiology and Therapeutic Innovations. Curr. Dermatol. Rep. 2014, 3, 40–45. [Google Scholar] [CrossRef]
- Heppt, M.V.; Gebhardt, C.; Hassel, J.C.; Alter, M.; Gutzmer, R.; Leiter, U.; Berking, C. Long-Term Management of Advanced Basal Cell Carcinoma: Current Challenges and Future Perspectives. Cancers 2022, 14, 4547. [Google Scholar] [CrossRef]
- Migden, M.R.; Chang, A.L.S.; Dirix, L.; Stratigos, A.J.; Lear, J.T. Emerging trends in the treatment of advanced basal cell carcinoma. Cancer Treat. Rev. 2018, 64, 1–10. [Google Scholar] [CrossRef]
- Lear, J.T.; Corner, C.; Dziewulski, P.; Fife, K.; Ross, G.L.; Varma, S.; A Harwood, C. Challenges and new horizons in the management of advanced basal cell carcinoma: A UK perspective. Br. J. Cancer 2014, 111, 1476–1481. [Google Scholar] [CrossRef]
- Pour, M.A.E.; Mohebtash, M.; Amin, A.; Khayyat, A.; Khalili-Toosi, A.-R.; Mousavi, S.; Guo, M.; Liu, J. Efficacy of the novel treatments of BCC with bone metastasis. J. Clin. Oncol. 2022, 40 (Suppl. S16), e14547. [Google Scholar] [CrossRef]
- Krakowski, A.C.; Hafeez, F.; Westheim, A.; Pan, E.Y.; Wilson, M. Advanced basal cell carcinoma: What dermatologists need to know about diagnosis. J. Am. Acad. Dermatol. 2022, 86, S1–S13. [Google Scholar] [CrossRef] [PubMed]
- Morgan, F.C.; Ruiz, E.S.; Karia, P.S.; Besaw, R.J.; Neel, V.A.; Schmults, C.D. Factors predictive of recurrence, metastasis, and death from primary basal cell carcinoma 2 cm or larger in diameter. J. Am. Acad. Dermatol. 2020, 83, 832–838. [Google Scholar] [CrossRef] [PubMed]
- Schmults, C.D.; Blitzblau, R.; Aasi, S.Z.; Alam, M.; Amini, A.; Bibee, K.; Bordeaux, J.; Chen, P.-L.; Contreras, C.M.; DiMaio, D.; et al. Basal Cell Skin Cancer, Version 2.2024, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2023, 21, 1181–1203. [Google Scholar] [CrossRef]
- Brash, D.E.; Rudolph, J.A.; Simon, J.A.; Lin, A.; McKenna, G.J.; Baden, H.P.; Halperin, A.J.; Ponten, J. A role for sunlight in skin cancer: UV-induced p53 mutations in squamous cell carcinoma. Proc. Natl. Acad. Sci. USA 1991, 88, 10124–10128. [Google Scholar] [CrossRef]
- Fania, L.; Didona, D.; Morese, R.; Campana, I.; Coco, V.; Di Pietro, F.R.; Ricci, F.; Pallotta, S.; Candi, E.; Abeni, D.; et al. Basal Cell Carcinoma: From Pathophysiology to Novel Therapeutic Approaches. Biomedicines 2020, 8, 449. [Google Scholar] [CrossRef]
- Snaidr, V.A.; Damian, D.L.; Halliday, G.M. Nicotinamide for photoprotection and skin cancer chemoprevention: A review of efficacy and safety. Exp. Dermatol. 2019, 28, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Fania, L.; Mazzanti, C.; Campione, E.; Candi, E.; Abeni, D.; Dellambra, E. Role of Nicotinamide in Genomic Stability and Skin Cancer Chemoprevention. Int. J. Mol. Sci. 2019, 20, 5946. [Google Scholar] [CrossRef]
- López-Otín, C.; Blasco, M.A.; Partridge, L.; Serrano, M.; Kroemer, G. The Hallmarks of Aging. Cell 2013, 153, 1194–1217. [Google Scholar] [CrossRef] [PubMed]
- Cocuz, I.G.; Popelea, M.C.; Niculescu, R.; Manea, A.; Sabău, A.-H.; Tinca, A.-C.; Szoke, A.R.; Budin, C.E.; Stoian, A.; Morariu, S.H.; et al. Pathophysiology, Histopathology, and Differential Diagnostics of Basal Cell Carcinoma and Cutaneous Squamous Cell Carcinoma—An Update from the Pathologist’s Point of View. Int. J. Mol. Sci. 2024, 25, 2220. [Google Scholar] [CrossRef]
- Engström, K.S.; Vahter, M.; Fletcher, T.; Leonardi, G.; Goessler, W.; Gurzau, E.; Koppova, K.; Rudnai, P.; Kumar, R.; Broberg, K. Genetic variation in arsenic (+3 oxidation state) methyltransferase (AS3MT), arsenic metabolism and risk of basal cell carcinoma in a European population. Environ. Mol. Mutagen. 2015, 56, 60–69. [Google Scholar] [CrossRef]
- Marzuka, A.G.; Book, S.E. Basal cell carcinoma: Pathogenesis, epidemiology, clinical features, diagnosis, histopathology, and management. Yale J. Biol. Med. 2015, 88, 167–179. [Google Scholar] [PubMed]
- Euvrard, S.; Kanitakis, J.; Claudy, A. Skin Cancers after Organ Transplantation. N. Engl. J. Med. 2003, 348, 1681–1691. [Google Scholar] [CrossRef] [PubMed]
- Boaventura, P.; Pereira, D.; Mendes, A.; Batista, R.; da Silva, A.F.; Guimarães, I.; Honavar, M.; Teixeira-Gomes, J.; Lopes, J.M.; Máximo, V.; et al. Mitochondrial D310 D-Loop instability and histological subtypes in radiation-induced cutaneous basal cell carcinomas. J. Dermatol. Sci. 2014, 73, 31–39. [Google Scholar] [CrossRef]
- Tampa, M.; Georgescu, S.R.; Mitran, M.I.; Mitran, C.I.; Matei, C.; Caruntu, A.; Scheau, C.; Nicolae, I.; Matei, A.; Caruntu, C.; et al. Current Perspectives on the Role of Matrix Metalloproteinases in the Pathogenesis of Basal Cell Carcinoma. Biomolecules 2021, 11, 903. [Google Scholar] [CrossRef]
- Camela, E.; Anca, P.I.; Lallas, K.; Papageorgiou, C.; Manoli, S.-M.; Gkentsidi, T.; Eftychidou, P.; Liopyris, K.; Sgouros, D.; Apalla, Z.; et al. Dermoscopic Clues of Histopathologically Aggressive Basal Cell Carcinoma Subtypes. Medicina 2023, 59, 349. [Google Scholar] [CrossRef] [PubMed]
- Cameron, M.C.; Lee, E.; Hibler, B.P.; Barker, C.A.; Mori, S.; Cordova, M.; Nehal, K.S.; Rossi, A.M. Basal cell carcinoma. J. Am. Acad. Dermatol. 2019, 80, 303–317. [Google Scholar] [CrossRef]
- Kilgour, J.M.; Jia, J.L.; Sarin, K.Y. Review of the Molecular Genetics of Basal Cell Carcinoma; Inherited Susceptibility, Somatic Mutations, and Targeted Therapeutics. Cancers 2021, 13, 3870. [Google Scholar] [CrossRef]
- Bakshi, A.; Chaudhary, S.C.; Rana, M.; Elmets, C.A.; Athar, M. Basal cell carcinoma pathogenesis and therapy involving hedgehog signaling and beyond. Mol. Carcinog. 2017, 56, 2543–2557. [Google Scholar] [CrossRef]
- PDQ Cancer Genetics Editorial Board. Genetics of Skin. Cancer (PDQ®): Health Professional Version; National Cancer Institute (US): Bethesda, MD, USA, 2002.
- Pellegrini, C.; Maturo, M.; Di Nardo, L.; Ciciarelli, V.; García-Rodrigo, C.G.; Fargnoli, M. Understanding the Molecular Genetics of Basal Cell Carcinoma. Int. J. Mol. Sci. 2017, 18, 2485. [Google Scholar] [CrossRef]
- Altaraihi, M.; Wadt, K.; Ek, J.; Gerdes, A.M.; Ostergaard, E. A healthy individual with a homozygous PTCH2 frameshift variant: Are variants of PTCH2 associated with nevoid basal cell carcinoma syndrome? Hum. Genome Var. 2019, 6, 10. [Google Scholar] [CrossRef]
- Rachakonda, P.S.; Hosen, I.; de Verdier, P.J.; Fallah, M.; Heidenreich, B.; Ryk, C.; Wiklund, N.P.; Steineck, G.; Schadendorf, D.; Hemminki, K.; et al. TERT promoter mutations in bladder cancer affect patient survival and disease recurrence through modification by a common polymorphism. Proc. Natl. Acad. Sci. USA 2013, 110, 17426–17431. [Google Scholar] [CrossRef] [PubMed]
- Denisova, E.; Heidenreich, B.; Nagore, E.; Rachakonda, P.S.; Hosen, I.; Akrap, I.; Traves, V.; García-Casado, Z.; López-Guerrero, J.A.; Requena, C.; et al. Frequent DPH3 promoter mutations in skin cancers. Oncotarget 2015, 6, 35922–35930. [Google Scholar] [CrossRef] [PubMed]
- Bonilla, X.; Parmentier, L.; King, B.; Bezrukov, F.; Kaya, G.; Zoete, V.; Seplyarskiy, V.B.; Sharpe, H.J.; McKee, T.; Letourneau, A.; et al. Genomic analysis identifies new drivers and progression pathways in skin basal cell carcinoma. Nat. Genet. 2016, 48, 398–406. [Google Scholar] [CrossRef]
- Wang, Q.; Shao, X.; Zhang, Y.; Zhu, M.; Wang, F.X.C.; Mu, J.; Li, J.; Yao, H.; Chen, K. Role of tumor microenvironment in cancer progression and therapeutic strategy. Cancer Med. 2023, 12, 11149–11165. [Google Scholar] [CrossRef] [PubMed]
- Lefrançois, P.; Xie, P.; Gunn, S.; Gantchev, J.; Villarreal, A.M.; Sasseville, D.; Litvinov, I.V. In silico analyses of the tumor microenvironment highlight tumoral inflammation, a Th2 cytokine shift and a mesenchymal stem cell-like phenotype in advanced in basal cell carcinomas. J. Cell Commun. Signal 2020, 14, 245–254. [Google Scholar] [CrossRef]
- Chiang, E.; Stafford, H.; Buell, J.; Ramesh, U.; Amit, M.; Nagarajan, P.; Migden, M.; Yaniv, D. Review of the Tumor Microenvironment in Basal and Squamous Cell Carcinoma. Cancers 2023, 15, 2453. [Google Scholar] [CrossRef] [PubMed]
- Ressler, J.M.; Zila, N.; Korosec, A.; Yu, J.; Silmbrod, R.; Bachmayr, V.; Tittes, J.; Strobl, J.; Lichtenberger, B.M.; Hoeller, C.; et al. Myofibroblast stroma differentiation in infiltrative basal cell carcinoma is accompanied by regulatory T-cells. J. Cutan. Pathol. 2023, 50, 544–551. [Google Scholar] [CrossRef]
- Kaporis, H.G.; Guttman-Yassky, E.; Lowes, M.A.; Haider, A.S.; Fuentes-Duculan, J.; Darabi, K.; Whynot-Ertelt, J.; Khatcherian, A.; Cardinale, I.; Novitskaya, I.; et al. Human Basal Cell Carcinoma Is Associated with Foxp3+ T cells in a Th2 Dominant Microenvironment. J. Investig. Dermatol. 2007, 127, 2391–2398. [Google Scholar] [CrossRef] [PubMed]
- Lefrançois, P.; Xie, P.; Gunn, S.; Villarreal, A.M.; Gantchev, J.; Sasseville, D. 16110 In silico analyses of the tumor microenvironment in basal cell carcinoma highlight the importance of TH2 cytokine profile, tumor-associated macrophages, and acquisition of mesenchymal stem cell-like phenotype in advanced and treatment-resistant tumors. J. Am. Acad. Dermatol. 2020, 83, AB54. [Google Scholar] [CrossRef]
- Deutsch, J.S.; Lai, J.; Schenk, K.M.; Soni, A.; Will, E.M.; Engle, L.L.; Xu, H.; Ogurtsova, A.; Madan, V.; Chong, J.K.; et al. Immune microenvironment of basal cell carcinoma and tumor regression following combined PD-1/LAG-3 blockade. J. Immunother. Cancer 2023, 11, e007463. [Google Scholar] [CrossRef]
- Fecher, L.A. Systemic Therapy for Inoperable and Metastatic Basal Cell Cancer. Curr. Treat. Options Oncol. 2013, 14, 237–248. [Google Scholar] [CrossRef] [PubMed]
- Axelson, M.; Liu, K.; Jiang, X.; He, K.; Wang, J.; Zhao, H.; Kufrin, D.; Palmby, T.; Dong, Z.; Russell, A.M.; et al. U.S. Food and Drug Administration Approval: Vismodegib for Recurrent, Locally Advanced, or Metastatic Basal Cell Carcinoma. Clin. Cancer Res. 2013, 19, 2289–2293. [Google Scholar] [CrossRef] [PubMed]
- Aditya, S.; Rattan, A. Vismodegib: A smoothened inhibitor for the treatment of advanced basal cell carcinoma. Indian. Dermatol. Online J. 2013, 4, 365. [Google Scholar] [CrossRef] [PubMed]
- Sekulic, A.; Migden, M.R.; Oro, A.E.; Dirix, L.; Lewis, K.D.; Hainsworth, J.D.; Solomon, J.A.; Yoo, S.; Arron, S.T.; Friedlander, P.A.; et al. Efficacy and Safety of Vismodegib in Advanced Basal-Cell Carcinoma. N. Engl. J. Med. 2012, 366, 2171–2179. [Google Scholar] [CrossRef]
- Sekulic, A.; Migden, M.R.; Basset-Seguin, N.; Garbe, C.; Gesierich, A.; Lao, C.D.; Miller, C.; Mortier, L.; Murrell, D.F.; Hamid, O.; et al. Long-term safety and efficacy of vismodegib in patients with advanced basal cell carcinoma: Final update of the pivotal ERIVANCE BCC study. BMC Cancer 2017, 17, 332. [Google Scholar] [CrossRef]
- Basset-Séguin, N.; Hauschild, A.; Kunstfeld, R.; Grob, J.; Dréno, B.; Mortier, L.; Ascierto, P.; Licitra, L.; Dutriaux, C.; Thomas, L.; et al. Vismodegib in patients with advanced basal cell carcinoma: Primary analysis of STEVIE, an international, open-label trial. Eur. J. Cancer 2017, 86, 334–348. [Google Scholar] [CrossRef]
- Gershoni, A.; Tiosano, A.; Ben Ishai, M.; Barayev, E.; Ben Simon, G.J.; Yassur, I. Vismodegib improves quality of life in patients with periocular locally advanced basal cell carcinoma: Subgroup analysis, STEVIE trial. Eye 2022, 36, 407–413. [Google Scholar] [CrossRef]
- Gutzmer, R.; Schulze, H.; Hauschild, A.; Leiter, U.; Meier, F.; Haferkamp, S.; Ulrich, C.; Wahl, R.; Berking, C.; Herbst, R.; et al. Effectiveness, safety and utilization of vismodegib in locally advanced basal cell carcinoma under real-world conditions in Germany–The non-interventional study NIELS. J. Eur. Acad. Dermatol. Venereol. 2021, 35, 1678–1685. [Google Scholar] [CrossRef] [PubMed]
- Słowińska, M.; Dudzisz-Śledź, M.; Sobczuk, P.; Łasińska, I.; Pietruszka, A.; Cybulska-Stopa, B.; Kowalczyk, A.; Świtaj, T.; Czarnecka, I.; Koseła-Paterczyk, H.; et al. Analysis of efficacy and safety of vismodegib therapy in patients with advanced basal cell carcinoma–real world multicenter cohort study. J. Eur. Acad. Dermatol. Venereol. 2022, 36, 1219–1228. [Google Scholar] [CrossRef] [PubMed]
- Bertrand, N.; Guerreschi, P.; Basset-Seguin, N.; Saiag, P.; Dupuy, A.; Dalac-Rat, S.; Dziwniel, V.; Depoortère, C.; Duhamel, A.; Mortier, L. Vismodegib in neoadjuvant treatment of locally advanced basal cell carcinoma: First results of a multicenter, open-label, phase 2 trial (VISMONEO study). EClinicalMedicine 2021, 35, 100844. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, N.M.; Cho, J. Hedgehog Pathway Inhibitors as Targeted Cancer Therapy and Strategies to Overcome Drug Resistance. Int. J. Mol. Sci. 2022, 23, 1733. [Google Scholar] [CrossRef] [PubMed]
- FDA Approves Sonidegib for Some Patients with Advanced Basal Cell Carcinoma. Available online: https://www.cancer.gov/news-events/cancer-currents-blog/2015/sonidegib-bcc (accessed on 31 March 2024).
- Migden, M.R.; Guminski, A.; Gutzmer, R.; Dirix, L.; Lewis, K.D.; Combemale, P.; Herd, R.M.; Kudchadkar, R.; Trefzer, U.; Gogov, S.; et al. Treatment with two different doses of sonidegib in patients with locally advanced or metastatic basal cell carcinoma (BOLT): A multicentre, randomised, double-blind phase 2 trial. Lancet Oncol. 2015, 16, 716–728. [Google Scholar] [CrossRef]
- Lear, J.T.; Migden, M.R.; Lewis, K.D.; Chang, A.L.S.; Guminski, A.; Gutzmer, R.; Dirix, L.; Combemale, P.; Stratigos, A.; Plummer, R.; et al. Long-term efficacy and safety of sonidegib in patients with locally advanced and metastatic basal cell carcinoma: 30-month analysis of the randomized phase 2 BOLT study. J. Eur. Acad. Dermatol. Venereol. 2018, 32, 372–381. [Google Scholar] [CrossRef] [PubMed]
- Dummer, R.; Guminksi, A.; Gutzmer, R.; Lear, J.; Lewis, K.; Chang, A.; Combemale, P.; Dirix, L.; Kaatz, M.; Kudchadkar, R.; et al. Long-term efficacy and safety of sonidegib in patients with advanced basal cell carcinoma: 42-month analysis of the phase II randomized, double-blind BOLT study. Br. J. Dermatol. 2020, 182, 1369–1378. [Google Scholar] [CrossRef] [PubMed]
- Mohan, S.V.; Chang, A.L.S. Management of Cutaneous and Extracutaneous Side Effects of Smoothened Inhibitor Therapy for Advanced Basal Cell Carcinoma. Clin. Cancer Res. 2015, 21, 2677–2683. [Google Scholar] [CrossRef]
- Shalhout, S.Z.; Emerick, K.S.; Kaufman, H.L.; Miller, D.M. Immunotherapy for Non-melanoma Skin Cancer. Curr. Oncol. Rep. 2021, 23, 125. [Google Scholar] [CrossRef]
- FDA Approves Cemiplimab-Rwlc for Locally Advanced and Metastatic Basal Cell Carcinoma. Available online: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-cemiplimab-rwlc-locally-advanced-and-metastatic-basal-cell-carcinoma (accessed on 4 April 2024).
- Stratigos, A.J.; Sekulic, A.; Peris, K.; Bechter, O.; Prey, S.; Kaatz, M.; Lewis, K.D.; Basset-Seguin, N.; Chang, A.L.S.; Dalle, S.; et al. Cemiplimab in locally advanced basal cell carcinoma after hedgehog inhibitor therapy: An open-label, multi-centre, single-arm, phase 2 trial. Lancet Oncol. 2021, 22, 848–857. [Google Scholar] [CrossRef]
- Lewis, K.; Peris, K.; Sekulic, A.; Stratigos, A.; Dunn, L.; Eroglu, Z.; Chang, A.; Migden, M.; Yoo, S.-Y.; Mohan, K.; et al. Final analysis of phase II results with cemiplimab in metastatic basal cell carcinoma after hedgehog pathway inhibitors. Ann. Oncol. 2024, 35, 221–228. [Google Scholar] [CrossRef]
- Chang, A.L.S.; Tran, D.C.; Cannon, J.G.; Li, S.; Jeng, M.; Patel, R.; Van der Bokke, L.; Pague, A.; Brotherton, R.; Rieger, K.E.; et al. Pembrolizumab for advanced basal cell carcinoma: An investigator-initiated, proof-of-concept study. J. Am. Acad. Dermatol. 2019, 80, 564–566. [Google Scholar] [CrossRef]
- Véron, M.; Chevret, S.; Grob, J.-J.; Beylot-Barry, M.; Saiag, P.; Fléchon, A.; You, B.; Maubec, E.; Jouary, T.; Toulemonde, E.; et al. Safety and efficacy of nivolumab, an anti-PD1 immunotherapy, in patients with advanced basal cell carcinoma, after failure or intolerance to sonic Hedgehog inhibitors: UNICANCER AcSé NIVOLUMAB trial. Eur. J. Cancer 2022, 177, 103–111. [Google Scholar] [CrossRef]
- Schenk, K.; Deutsch, J.; Schollenberger, M.D.; Sharfman, W.; Brothers, P.; Pons, A.; Scott, J.; Bibee, K.; Taube, J.; Topalian, S.; et al. 820P Nivolumab (NIVO) +/- relatlimab (RELA) or ipilimumab (IPI) for patients (pts) with advanced treatment-naïve or -refractory basal cell carcinoma (BCC). Ann. Oncol. 2022, 33, S922–S923. [Google Scholar] [CrossRef]
- Walter, A.; Barysch, M.J.; Behnke, S.; Dziunycz, P.; Schmid, B.; Ritter, E.; Gnjatic, S.; Kristiansen, G.; Moch, H.; Knuth, A.; et al. Cancer-Testis Antigens and Immunosurveillance in Human Cutaneous Squamous Cell and Basal Cell Carcinomas. Clin. Cancer Res. 2010, 16, 3562–3570. [Google Scholar] [CrossRef]
- Sabbatino, F.; Marra, A.; Liguori, L.; Scognamiglio, G.; Fusciello, C.; Botti, G.; Ferrone, S.; Pepe, S. Resistance to anti-PD-1-based immunotherapy in basal cell carcinoma: A case report and review of the literature. J. Immunother. Cancer 2018, 6, 126. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F. Molecular Mechanisms of IFN-γ to Up-Regulate MHC Class I Antigen Processing and Presentation. Int. Rev. Immunol. 2009, 28, 239–260. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Shi, L.Z.; Zhao, H.; Chen, J.; Xiong, L.; He, Q.; Chen, T.; Roszik, J.; Bernatchez, C.; Woodman, S.E.; et al. Loss of IFN-γ Pathway Genes in Tumor Cells as a Mechanism of Resistance to Anti-CTLA-4 Therapy. Cell 2016, 167, 397–404.e9. [Google Scholar] [CrossRef]
- Benci, J.L.; Xu, B.; Qiu, Y.; Wu, T.J.; Dada, H.; Twyman-Saint Victor, C.; Cucolo, L.; Lee, D.S.M.; Pauken, K.E.; Huang, A.C.; et al. Tumor Interferon Signaling Regulates a Multigenic Resistance Program to Immune Checkpoint Blockade. Cell 2016, 167, 1540–1554.e12. [Google Scholar] [CrossRef]
- Dollinger, E.; Bergman, D.; Zhou, P.; Atwood, S.X.; Nie, Q. Divergent Resistance Mechanisms to Immunotherapy Explain Responses in Different Skin Cancers. Cancers 2020, 12, 2946. [Google Scholar] [CrossRef] [PubMed]
- Zelin, E.; Maronese, C.A.; Dri, A.; Toffoli, L.; Di Meo, N.; Nazzaro, G.; Zalaudek, I. Identifying Candidates for Immunotherapy among Patients with Non-Melanoma Skin Cancer: A Review of the Potential Predictors of Response. J. Clin. Med. 2022, 11, 3364. [Google Scholar] [CrossRef]
- Gambichler, T.; Skrygan, M.; Kaczmarczyk, J.M.; Hyun, J.; Tomi, N.S.; Sommer, A.; Bechara, F.G.; Boms, S.; Brockmeyer, N.H.; Altmeyer, P.; et al. Increased expression of TGF-beta/Smad proteins in basal cell carcinoma. Eur. J. Med. Res. 2007, 12, 509–514. [Google Scholar]
- Hall, E.T.; Fernandez-Lopez, E.; Silk, A.W.; Dummer, R.; Bhatia, S. Immunologic Characteristics of Nonmelanoma Skin Cancers: Implications for Immunotherapy. In American Society of Clinical Oncology Educational Book; American Society of Clinical Oncology Educational Book: Alexandria, VA, USA, 2020; pp. 398–407. [Google Scholar] [CrossRef]
- Stratigos, A.; Sekulic, A.; Peris, K.; Bechter, O.; Kaatz, M.; Lewis, K.; Basset-Segiun, N.; Chang, A.L.; Dalle, S.; Orland, A.F.; et al. Primary Analysis of Phase 2 Results for Cemiplimab in Patients (pts) with Locally Advanced Basal Cell Carcinoma (laBCC) who Progress on or are Intolerant to Hedgehog Inhibitors (HHIs). SKIN J. Cutan. Med. 2021, 5, s4. [Google Scholar] [CrossRef]
- Migden, M.R.; Luke, J.J.; Chai-Ho, W.; Kheterpal, M.; Wise-Draper, T.M.; Poklepovic, A.S.; Bolotin, D.; Verschraegen, C.F.; Collichio, F.A.; Tang, J.; et al. An open-label, multicenter, phase 1b/2 study of RP1, a first-in-class, enhanced potency oncolytic virus in solid organ transplant recipients with advanced cutaneous malignancies (ARTACUS). J. Clin. Oncol. 2022, 40 (Suppl. S16), TPS9597. [Google Scholar] [CrossRef]
- McCormick, D.; Eroglu, Z.; Cowey, C.L. 32283 A phase I study of CX-4945 administered orally twice daily to patients with advanced basal cell carcinoma. J. Am. Acad. Dermatol. 2022, 87, AB10. [Google Scholar] [CrossRef]
- Eroglu, Z.; Cowey, C.L.; Soong, J.; McCormick, D.; Fan, P.; Chen, J.; Elgendy, M.; Jang, S.; Chang, A.L.S. A phase I study of CX-4945 administered orally twice daily to patients with advanced basal cell carcinoma. J. Clin. Oncol. 2020, 38 (Suppl. S15), TPS10080. [Google Scholar] [CrossRef]
- Pinato, D.; Plummer, R.; Gutierrez, M.; Yachnin, J.; Schiza, A.; Hojgaard, M.; Smeland, K.; Edenfield, W.; Prenen, H.; Ny, L.; et al. 622 A phase 1 study exploring the safety and tolerability of the small-molecule PD-L1 inhibitor, INCB099318, in patients with select advanced solid tumors. In Regular and Young Investigator Award Abstracts; BMJ Publishing Group Ltd.: London, UK, 2022; p. A653. [Google Scholar] [CrossRef]
- Silk, A.W.; LeBoeuf, N.R.; Rabinowits, G.; Puzanov, I.; Burgess, M.A.; Devata, S.; Moore, D.; Goydos, J.S.; Chen, H.X.; Kaufman, H.; et al. A phase II study of talimogene laherparepvec followed by talimogene laherparepvec + nivolumab in refractory T cell and NK cell lymphomas, cutaneous squamous cell carcinoma, Merkel cell carcinoma, and other rare skin tumors (NCI #10057). J. Clin. Oncol. 2018, 36 (Suppl. S5), TPS219. [Google Scholar] [CrossRef]
| NCT | Study Title | Phase | Intervention | Status |
|---|---|---|---|---|
| 04679480 | A Prospective, Open, Single-arm, Single Center, Phase II Trial to Assess the Efficacy of Anti-PD1 Antibody in Combination with Pulsed Hedgehog Inhibitor in Advanced Basal Cell Carcinoma | II |
| Recruiting |
| 03521830 | Nivolumab Alone or Plus Relatlimab or Ipilimumab for Patients with Locally Advanced Unresectable or Metastatic Basal Cell Carcinoma | II |
| Recruiting [65] |
| 05651828 | Adaptive Therapy of Vismodegib in Advanced Basal Cell Carcinoma | I |
| Recruiting |
| 05929664 | Neoadjuvant REGN2810 (Cemiplimab) in Cutaneous Basal Cell Carcinoma of the Head and Neck | II |
| Recruiting |
| 04806646 | A Phase II, Open-label Study Improving Compliance and Time of Treatment After Obtaining Complete Response Through a Tailored Schedule of Sonidegib in Locally Advanced Basal Cell Carcinomas (BCC)-the SONIBEC Trial | II |
| Recruiting |
| 05561634 | Evaluation of Radiotherapy After Complete Response to Sonic Hedgehog Pathway Inhibitors in Patients with Locally Advanced Basal Cell Carcinoma: A Prospective Multicenter Study | II |
| Not yet recruiting |
| 04349436 | An Open-Label, Multicenter, Phase 1B/2 Study of RP1 in Solid Organ and Hematopoietic Cell Transplant Recipients with Advanced Cutaneous Malignancies | IB/II |
| Recruiting [76] |
| 04916002 | A Multicenter, Open-label, Phase 2 Study of Intratumoral Vidutolimod (CMP-001) in Combination with Intravenous Cemiplimab in Subjects with Selected Types of Advanced or Metastatic Cancer | II |
| Recruiting |
| 05970497 | A Phase 1, Open-Label, Multi-Center, Dose Escalation and Expansion Study of KB707 in Subjects with Locally Advanced or Metastatic Solid Tumor Malignancies | I |
| Recruiting |
| 05859074 | A First-In-Human Phase I, Open Label, Safety and Tolerability Study of Escalating Multiple Doses of Intratumoral MQ710, a Multi-Transgene Expressing Modified Vaccinia Virus Ankara-Based Virotherapy, Alone and in Combination with the Systemic Checkpoint Inhibitor Pembrolizumab in Solid Tumors | I |
| Recruiting |
| 05086692 | A Phase 1/2 Open Label, Dose Escalation and Expansion Study of MDNA11, IL-2 Superkine, Administered Alone or in Combination with Immune Checkpoint Inhibitor in Patients with Advanced Solid Tumors | I/II |
| Recruiting |
| 05592626 | A Phase 1/2, First-in-Human, Open-Label, Dose Escalation and Expansion Study of STAR0602, a Selective T Cell Receptor (TCR) Targeting, Bifunctional Antibody-fusion Molecule, in Subjects with Unresectable, Locally Advanced, or Metastatic Solid Tumors That Are Antigen-rich (START-001) | I/II |
| Recruiting |
| 03897036 | A Phase I, Multi-Center, Open-Label, Treatment Duration Increment, Expansion, Safety, and Pharmacodynamic Study of CX-4945 Administered Orally Twice Daily to Patients with Advanced Basal Cell Carcinoma | I |
| Not recruiting [77,78] |
| 04323202 | A Phase 1B, Single Arm Study of Neoadjuvant-Adjuvant Pembrolizumab in Resectable Advanced Basal Cell Carcinoma of the Head and Neck to Assess for Pathologic Responses in the Tumor Microenvironment | I |
| Not recruiting |
| 04272034 | A Phase 1 Study Exploring the Safety, Tolerability, Pharmacokinetics, and Pharmacodynamics of INCB099318 in Participants with Select Advanced Solid Tumors | I |
| Not recruiting [79] |
| 02978625 | A Phase II Study of Talimogene Laherparepvec Followed by Talimogene Laherparepvec + Nivolumab in Refractory T Cell and NK Cell Lymphomas, Cutaneous Squamous Cell Carcinoma, Merkel Cell Carcinoma, and Other Rare Skin Tumors | II |
| Not recruiting [80] |
| 03775525 | A Phase I/Ib, Multicenter, Open-label, Dose-Escalation, Safety, Pharmacodynamic and Pharmacokinetic Study of GZ17-6.02 Monotherapy and in Combination with Capecitabine, Given Orally on a Daily Schedule in Patients with Advanced Solid Tumors or Lymphoma | I |
| Not recruiting |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alkassis, S.; Shatta, M.; Wong, D.J. Therapeutic Advances in Advanced Basal Cell Carcinoma. Cancers 2024, 16, 3075. https://doi.org/10.3390/cancers16173075
Alkassis S, Shatta M, Wong DJ. Therapeutic Advances in Advanced Basal Cell Carcinoma. Cancers. 2024; 16(17):3075. https://doi.org/10.3390/cancers16173075
Chicago/Turabian StyleAlkassis, Samer, Maya Shatta, and Deborah J. Wong. 2024. "Therapeutic Advances in Advanced Basal Cell Carcinoma" Cancers 16, no. 17: 3075. https://doi.org/10.3390/cancers16173075
APA StyleAlkassis, S., Shatta, M., & Wong, D. J. (2024). Therapeutic Advances in Advanced Basal Cell Carcinoma. Cancers, 16(17), 3075. https://doi.org/10.3390/cancers16173075







