The Role of Whole-Gland and Focal Cryotherapy in Recurrent Prostate Cancer
Abstract
Simple Summary
Abstract
1. Introduction
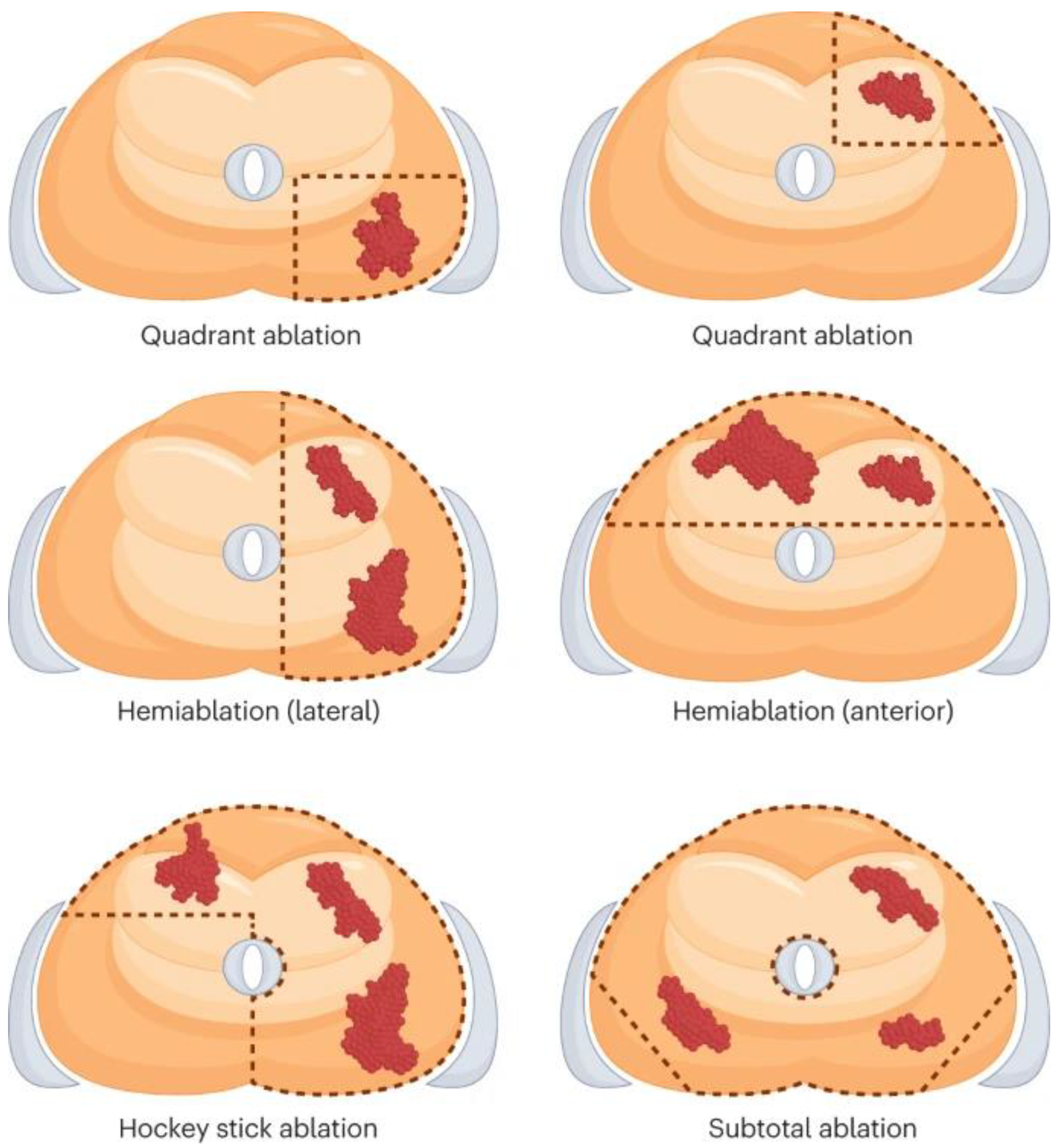
2. Cryoablation Technique
3. Cryotherapy in Various Salvage Settings
3.1. Post-Radiation Therapy Recurrence
- Radiographic Staging at Recurrence
- (i)
- PSMA PET
- (ii)
- Multiparametric MRI
- (iii)
- Combining PSMA PET and Multiparametric MRI
3.2. Use of Cryotherapy Post-Biochemical Recurrence after Radiotherapy
- Whole-gland salvage cryotherapy
- b.
- Focal salvage cryotherapy
| References | Institution | Initial Therapy (No. of Pts) | Risk Categories | Preprocedural PSA (ng/mL), Median (IQR); Use of ADT, n (%) | Mos. Follow-Up | Focal Template; Planned Treatment Margin | Success/ Failure Criteria a | % Post-Ablative Biopsy; % Pos. Biopsy Rate | Urinary Incontinence, n (%); Erectile Function, n (%) |
|---|---|---|---|---|---|---|---|---|---|
| Li et al. (2015) [50] | Cleveland Clinic, OH, USA | RT (91) | NR | 4.8 (0–92.6); 0 (0%) | Median: 15 | NR; NR | BDFS at 1 year: 95.3%, 3 years: 72.4%, 5 years: 46.5% | 15.4%; 28.6% | 5 (5.5); 10 (50) |
| Kongnyuy et al. (2017) [51] | Winthrop University Hospital, Garden City, NY, USA | CR—8 (12.3%) SR—5 (7.7) BT—13 (20.0) PBR—1 (1.5) RT/other—37 (57.0) Unknown—1 (1.5) (n = 65) | NR | 4.0 (0.01–19.0); 13 (20%) | Median: 26.6 | Hemi; NR | BR: 52.3% | 52.3%; 20% | 4 (6.1); 14 (21.5) |
| Tan et al. (2021) [52] | Duke University Medical Center, Durham, NC, USA | NR (11) | NR | 4.99 (2.23–7.86); 0 (0%) | Median: 28 | Focal (n = 6); NR, Hemi (n = 2); NR, Sub-total (n = 3); NR | FFS at 12 months: 100%, 24 months: 80%, and 36 months: 40% | NR; 27.3% | 1 (0.1); NR |
| Tan et al. (2020) [53] | Multiple, USA | RT (72) | NR | 4 (2.7–5.6); 19 (26.4%) | Median: 24.4 | NR; NR | BR: 16 of the 72 patients (22.2%) | 19.2%; 33.3% | 9.3%; 52.6% |
| Ismail et al. (2007) [49] | The Royal Surrey County Hospital and St Luke’s Cancer Centre, Guildford, Surrey, UK | RT (100) | High: 68, Intermediate: 20, Low: 12 | NR; NR | 33.5 | NR; NR | BRFS at 5 years: 73% (low-risk), 45% (intermediate), and 11% (high) | NR; NR | 13, ED: 86 |
| Chang et al. (2015) [54] | The Affiliated Hospital of Nanjing University Medical School, Jiangsu, China | CR (12) | NR | 2.5 (0.18–7.28); 3 (25%) | Median: 33.5 | BRFS: 7 (58.3%) | 16.7; 16.7 | 1 (8.3), impotence: 2 (16.6) | |
| Bomers et al. (2013) [55] | Multiple (the Netherlands) | CR (10) | NR | 3.6 (0.9–8.7); NR | 12 | NR; NR | BRFS at 3 months: 100%; BRFS at 6 months: 70%; BRFS at 12 months: 75% [3/4] | NR; NR | NR; NR |
| de Abreu Castro (2013) [56] | Multiple (USA) | SFC (25), STC (25) | NR | 2.8 (SFC); 3.9 (STC) | 31 months (SFC); 53 months (STC) | NR; NR | BFS at 5 years: 54% (SFC), 86% (STC) | 48% (SFC), 28% (STC); 14.3% [1/7] (STC) | 0% (SFC), 13% (STC); 29% [2/7] (SFC), 0% [0/4] (STC) |
3.3. Post-Focal Ablation Recurrence
4. Comparison of Salvage: Partial vs. Salvage Whole-Gland Cryotherapy
5. Comparison of Salvage Cryotherapy vs. Salvage Radical Prostatectomy
6. Comparison of Salvage Cryotherapy vs. Salvage High-Intensity Focused Ultrasound
7. Limitations
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- American Cancer Society. Cancer Facts & Figures 2024; American Cancer Society: Atlanta, GA, USA, 2024. [Google Scholar]
- Kishan, A.U.; Karnes, R.J.; Romero, T.; Wong, J.K.; Motterle, G.; Tosoian, J.J.; Trock, B.J.; Klein, E.A.; Stish, B.J.; Dess, R.T.; et al. Comparison of Multimodal Therapies and Outcomes Among Patients with High-Risk Prostate Cancer with Adverse Clinicopathologic Features. JAMA Netw. Open 2021, 4, e2115312. [Google Scholar] [CrossRef]
- Chin, J.L.; Lavi, A.; Metcalfe, M.J.; Siddiqui, K.; Dewar, M.; Petros, F.G.; Li, R.; Nogueras González, G.M.; Wang, X.; Nair, S.M.; et al. Long-Term Outcomes of Whole Gland Salvage Cryotherapy for Locally Recurrent Prostate Cancer following Radiation Therapy: A Combined Analysis of Two Centers. J. Urol. 2021, 206, 646–654. [Google Scholar] [CrossRef]
- Zaorsky, N.G.; Calais, J.; Fanti, S.; Tilki, D.; Dorff, T.; Spratt, D.E.; Kishan, A.U. Salvage therapy for prostate cancer after radical prostatectomy. Nat. Rev. Urol. 2021, 18, 643–668. [Google Scholar] [CrossRef]
- Safavy, S.; Jabaji, R.B.; Lu, S.M.; Slezak, J.M.; Cosmatos, H.A.; Williams, S.G.; Finley, D.S. Salvage Cryoablation for Radiorecurrent Prostate Cancer: Initial Experience at a Regional Health Care System. Perm. J. 2019, 23, 18–153. [Google Scholar] [CrossRef]
- Khan, A.; Khan, A.U.; Siref, L.; Feloney, M. Focal cryoablation of the prostate: Primary treatment in 163 patients with localized prostate cancer. Cureus 2023, 15, e37172. [Google Scholar] [CrossRef]
- Tan, W.P.; Wysock, J.S.; Lepor, H. Partial gland cryoablation for prostate cancer—Where are we? Nat. Rev. Urol. 2023, 20, 127–128. [Google Scholar] [CrossRef]
- Sonn, G.A.; Margolis, D.J.; Marks, L.S. Target detection: Magnetic resonance imaging-ultrasound fusion-guided prostate biopsy. Urol. Oncol. 2014, 32, 903–911. [Google Scholar] [CrossRef]
- Valerio, M.; Shah, T.T.; Shah, P.; Mccartan, N.; Emberton, M.; Arya, M.; Ahmed, H.U. Magnetic resonance imaging-transrectal ultrasound fusion focal cryotherapy of the prostate: A prospective development study. Urol. Oncol Semin. Orig. 2017, 35, 150.e1–150.e7. [Google Scholar] [CrossRef]
- Priester, A.; Natarajan, S.; Khoshnoodi, P.; Margolis, D.J.; Raman, S.S.; Reiter, R.E.; Huang, J.; Grundfest, W.; Marks, L.S. Magnetic resonance imaging underestimation of prostate cancer geometry: Use of patient specific molds to correlate images with whole Mount Pathology. J. Urol. 2017, 197, 320–326. [Google Scholar] [CrossRef]
- Littrup, P.J.; Jallad, B.; Vorugu, V.; Littrup, G.; Currier, B.; George, M.; Herring, D. Lethal isotherms of cryoablation in a phantom study: Effects of heat load, probe size, and number. J. Vasc. Interv. Radiol. 2009, 20, 1343–1351. [Google Scholar] [CrossRef]
- Shah, T.T.; Arbel, U.; Foss, S.; Zachman, A.; Rodney, S.; Ahmed, H.U.; Arya, M. Modeling cryotherapy ice ball dimensions and isotherms in a novel gel-based model to determine optimal cryo-needle configurations and settings for potential use in clinical practice. Urology 2016, 91, 234–240. [Google Scholar] [CrossRef]
- de Marini, P.; Cazzato, R.L.; Garnon, J.; Shaygi, B.; Koch, G.; Auloge, P.; Tricard, T.; Lang, H.; Gangi, A. Percutaneous MR-guided prostate cancer cryoablation technical updates and literature review. BJR Open 2019, 1, 20180043. [Google Scholar] [CrossRef]
- Selvaggio, O.; Falagario, U.G.; Bruno, S.M.; Recchia, M.; Sighinolfi, M.C.; Sanguedolce, F.; Milillo, P.; Macarini, L.; Rastinehad, A.R.; Sanchez-Salas, R.; et al. Intraoperative digital analysis of ablation margins (DAAM) by fluorescent confocal microscopy to improve partial prostate gland cryoablation outcomes. Cancers 2021, 13, 4382. [Google Scholar] [CrossRef]
- Chin, Y.F.; Lynn, N. Systematic review of focal and salvage cryotherapy for prostate cancer. Curēus 2022, 14, e26400. [Google Scholar] [CrossRef]
- Agarwal, P.K.; Sadetsky, N.; Konety, B.R.; Resnick, M.I.; Carroll, P.R. Treatment failure after primary and salvage therapy for prostate cancer: Likelihood, patterns of care, and outcomes. Cancer 2008, 112, 307–314. [Google Scholar] [CrossRef]
- Hruby, G.; Eade, T.; Kneebone, A.; Emmett, L.; Guo, L.; Ho, B.; Hsiao, E.; Schembri, G.; Hunter, J.; Kwong, C. Delineating biochemical failure with 68Ga-PSMA-PET following definitive external beam radiation treatment for prostate cancer. Radiother. Oncol. 2017, 122, 99–102. [Google Scholar] [CrossRef]
- Einspieler, I.; Rauscher, I.; Düwel, C.; Krönke, M.; Rischpler, C.; Habl, G.; Dewes, S.; Ott, A.; Wester, H.-J.; Schwaiger, M.; et al. Detection Efficacy of Hybrid 68Ga-PSMA Ligand PET/CT in Prostate Cancer Patients with Biochemical Recurrence after Primary Radiation Therapy Defined by Phoenix Criteria. J. Nucl. Med. 2017, 58, 1081–1087. [Google Scholar] [CrossRef]
- Morris, M.J.; Rowe, S.P.; Gorin, M.A.; Saperstein, L.; Pouliot, F.; Josephson, D.; Wong, J.Y.; Pantel, A.R.; Cho, S.Y.; Gage, K.L.; et al. Diagnostic Performance of 18F-DCFPyL-PET/CT in Men with Biochemically Recurrent Prostate Cancer: Results from the CONDOR Phase III, Multicenter Study. Clin. Cancer Res. 2021, 27, 3674–3682. [Google Scholar] [CrossRef]
- Perera, M.; Papa, N.; Roberts, M.; Williams, M.; Udovicich, C.; Vela, I.; Christidis, D.; Bolton, D.; Hofman, M.S.; Lawrentschuk, N.; et al. Gallium-68 Prostate-specific Membrane Antigen Positron Emission Tomography in Advanced Prostate Cancer-Updated Diagnostic Utility, Sensitivity, Specificity, and Distribution of Prostate-specific Membrane Antigen-avid Lesions: A Systematic Review and Meta-analysis. Eur. Urol. 2020, 77, 403–417. [Google Scholar] [CrossRef]
- Mertan, F.V.; Greer, M.D.; Borofsky, S.; Kabakus, I.M.; Merino, M.J.; Wood, B.J.; Pinto, P.A.; Choyke, P.L.; Turkbey, B. Multiparametric Magnetic Resonance Imaging of Recurrent Prostate Cancer. Top. Magn. Reson. Imaging 2016, 25, 139–147. [Google Scholar] [CrossRef]
- Gaur, S.; Turkbey, B. Prostate MR Imaging for Posttreatment Evaluation and Recurrence. Radiol. Clin. N. Am. 2018, 56, 263–275. [Google Scholar] [CrossRef]
- Barchetti, F.; Panebianco, V. Multiparametric MRI for recurrent prostate cancer post radical prostatectomy and postradiation therapy. Biomed. Res. Int. 2014, 2014, 316272. [Google Scholar] [CrossRef]
- Grant, K.; Lindenberg, M.L.; Shebel, H.; Pang, Y.; Agarwal, H.K.; Bernardo, M.; Kurdziel, K.A.; Turkbey, B.; Choyke, P.L. Functional and molecular imaging of localized and recurrent prostate cancer. Eur. J. Nucl. Med. Mol. Imaging 2013, 40 (Suppl. S1), S48–S59. [Google Scholar] [CrossRef]
- Kim, C.K.; Park, B.K.; Lee, H.M. Prediction of locally recurrent prostate cancer after radiation therapy: Incremental value of 3T diffusion-weighted MRI. J. Magn. Reson. Imaging 2009, 29, 391–397. [Google Scholar] [CrossRef]
- Kim, C.K.; Park, B.K.; Park, W.; Kim, S.S. Prostate MR imaging at 3T using a phased-arrayed coil in predicting locally recurrent prostate cancer after radiation therapy: Preliminary experience. Abdom. Imaging 2010, 35, 246–252. [Google Scholar] [CrossRef]
- Tamada, T.; Sone, T.; Jo, Y.; Hiratsuka, J.; Higaki, A.; Higashi, H.; Ito, K. Locally recurrent prostate cancer after high-dose-rate brachytherapy: The value of diffusion-weighted imaging, dynamic contrast-enhanced MRI, and T2-weighted imaging in localizing tumors. AJR Am. J. Roentgenol. 2011, 197, 408–414. [Google Scholar] [CrossRef]
- Radzina, M.; Tirane, M.; Roznere, L.; Zemniece, L.; Dronka, L.; Kalnina, M.; Mamis, E.; Biederer, J.; Lietuvietis, V.; Freimanis, A.; et al. Accuracy of 68Ga-PSMA-11 PET/CT and multiparametric MRI for the detection of local tumor and lymph node metastases in early biochemical recurrence of prostate cancer. Am. J. Nucl. Med. Mol. Imaging 2020, 10, 106–118. [Google Scholar]
- Satapathy, S.; Singh, H.; Kumar, R.; Mittal, B.R. Diagnostic Accuracy of 68Ga-PSMA PET/CT for Initial Detection in Patients with Suspected Prostate Cancer: A Systematic Review and Meta-Analysis. AJR Am. J. Roentgenol. 2021, 216, 599–607. [Google Scholar] [CrossRef]
- Petersen, L.J.; Zacho, H.D. PSMA PET for primary lymph node staging of intermediate and high-risk prostate cancer: An expedited systematic review. Cancer Imaging Off. Publ. Int. Cancer Imaging Soc. 2020, 20, 10. [Google Scholar] [CrossRef]
- Jannusch, K.; Bruckmann, N.M.; Morawitz, J.; Boschheidgen, M.; Quick, H.H.; Herrmann, K.; Fendler, W.P.; Umutlu, L.; Stuschke, M.; Hadaschik, B.; et al. Recurrent prostate cancer: Combined role for MRI and PSMA-PET in 68Ga-PSMA-11 PET/MRI. Eur. Radiol. 2023, 34, 4789–4800. [Google Scholar] [CrossRef]
- Albisinni, S.; Aoun, F.; Marcelis, Q.; Jungels, C.; Al-Hajj Obeid, W.; Zanaty, M.; Tubaro, A.; Roumeguere, T.; De Nunzio, C. Innovations in imaging modalities for recurrent and metastatic prostate cancer: A systematic review. Minerva Urol. Nefrol. 2018, 70, 347–360. [Google Scholar] [CrossRef]
- Rasing, M.; van Son, M.; Moerland, M.; de Keizer, B.; Wessels, F.; Jonges, T.; van de Pol, S.; Eppinga, W.; Noteboom, J.; Lagendijk, J.; et al. Value of Targeted Biopsies and Combined PSMA PET/CT and mp-MRI Imaging in Locally Recurrent Prostate Cancer after Primary Radiotherapy. Cancers 2022, 14, 781. [Google Scholar] [CrossRef]
- da Silva, R.D.; Kim, F.J. Prostate cancer—Local treatment after radiorecurrence: Salvage cryoablation. Int. Braz. J. Urol. 2018, 44, 435–439. [Google Scholar] [CrossRef]
- Bahn, D.K.; Lee, F.; Badalament, R.; Kumar, A.; Greski, J.; Chernick, M. Targeted cryoablation of the prostate: 7-year outcomes in the primary treatment of prostate cancer. Urology 2002, 60, 3–11. [Google Scholar] [CrossRef]
- Miller, R.J., Jr.; Cohen, J.K.; Shuman, B.; Merlotti, L.A. Percutaneous, transperineal cryosurgery of the prostate as salvage therapy for post radiation recurrence of adenocarcinoma. Cancer 1996, 77, 1510–1514. [Google Scholar] [CrossRef]
- Leibovici, D.; Chiong, E.; Pisters, L.L.; Guo, C.C.; Ward, J.F.; Andino, L.; Prokhorova, I.N.; Troncoso, P. Pathological characteristics of prostate cancer recurrence after radiation therapy: Implications for focal salvage therapy. J. Urol. 2012, 188, 98–102. [Google Scholar] [CrossRef]
- Finley, D.S.; Belldegrun, A.S. Salvage cryotherapy for radiation-recurrent prostate cancer: Outcomes and complications. Curr. Urol. Rep. 2011, 12, 209–215. [Google Scholar] [CrossRef][Green Version]
- Campbell, S.P.; Deivasigamani, S.; Arcot, R.; Adams, E.S.; Orabi, H.; Elshafei, A.; Tan, W.P.; Davis, L.; Wu, Y.; Chang, A.; et al. Salvage Cryoablation for Recurrent Prostate Cancer Following Primary External Beam Radiotherapy or Primary Cryotherapy: A Propensity Score Matched Analysis of Mid-term Oncologic and Functional Outcomes. Clin. Genitourin. Cancer 2023, 21, 555–562. [Google Scholar] [CrossRef]
- Tan, W.P.; Kotamarti, S.; Ayala, A.; Mahle, R.; Chen, E.; Arcot, R.; Chang, A.; Michael, Z.; Seguier, D.; Polascik, T.J. Oncological and functional outcomes for men undergoing salvage whole-gland cryoablation for radiation-resistant prostate cancer. Eur. Urol. Oncol. 2023, 6, 289–294. [Google Scholar] [CrossRef]
- Spiess, P.E.; Levy, D.A.; Mouraviev, V.; Pisters, L.L.; Jones, J.S. Biochemical failure predictors after prostate salvage cryotherapy. BJU Int. 2013, 112, E256–E261. [Google Scholar] [CrossRef]
- Wenske, S.; Quarrier, S.; Katz, A.E. Salvage cryosurgery of the prostate for failure after primary radiotherapy or cryosurgery: Long-term clinical, functional, and oncologic outcomes in a large cohort at a tertiary referral centre. Eur. Urol. 2013, 64, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Lian, H.; Yang, R.; Lin, T.; Wang, W.; Zhang, G.; Guo, H. Salvage cryotherapy with third-generation technology for locally recurrent prostate cancer after radiation therapy. Int. Urol. Nephrol. 2016, 48, 1461–1466. [Google Scholar] [CrossRef] [PubMed]
- Ghafar, M.A.; Johnson, C.W.; De La Taille, A.; Benson, M.C.; Bagiella, E.; Fatal, M.; Olsson, C.A.; Katz, A.E. Salvage cryotherapy using an argon based system for locally recurrent prostate cancer after radiation therapy: The Columbia experience. J. Urol. 2001, 166, 1333–1338. [Google Scholar] [CrossRef] [PubMed]
- Ward, J.F.; Jones, J.S. Focal cryotherapy for localized prostate cancer: A report from the National Cryo on-line database (cold) registry. BJU Int. 2012, 109, 1648–1654. [Google Scholar] [CrossRef] [PubMed]
- Spiess, P.E.; Levy, D.A.; Pisters, L.L.; Mouraviev, V.; Jones, J.S. Outcomes of salvage prostate cryotherapy stratified by pre-treatment PSA: Update from the COLD registry. World J. Urol. 2013, 31, 1321–1325. [Google Scholar] [CrossRef]
- Babaian, R.J.; Donnelly, B.; Bahn, D.; Baust, J.G.; Dineen, M.; Ellis, D.; Katz, A.; Pisters, L.; Rukstalis, D.; Shinohara, K.; et al. Best practice statement on cryosurgery for the treatment of localized prostate cancer. J. Urol. 2008, 180, 1993–2004. [Google Scholar] [CrossRef]
- Izawa, J.I.; Perrotte, P.; Greene, G.F.; Scott, S.; Levy, L.; McGuire, E.; Madsen, L.; von Eschenbach, A.C.; Pisters, L.L. Local tumor control with salvage cryotherapy for locally recurrent prostate cancer after external beam radiotherapy. J. Urol. 2001, 165, 867–870. [Google Scholar] [CrossRef]
- Ismail, M.; Ahmed, S.; Kastner, C.; Davies, J. Salvage cryotherapy for recurrent prostate cancer after radiation failure: A prospective case series of the first 100 patients. BJU Int. 2007, 100, 760–764. [Google Scholar] [CrossRef]
- Li, Y.H.; Elshafei, A.; Agarwal, G.; Ruckle, H.; Powsang, J.; Jones, J.S. Salvage focal prostate cryoablation for locally recurrent prostate cancer after radiotherapy: Initial results from the cryo on-line data registry. Prostate 2015, 75, 1–7. [Google Scholar] [CrossRef]
- Kongnyuy, M.; Berg, C.J.; Kosinski, K.E.; Habibian, D.J.; Schiff, J.T.; Corcoran, A.T.; Katz, A.E. Salvage focal cryosurgery may delay use of androgen deprivation therapy in cryotherapy and radiation recurrent prostate cancer patients. Int. J. Hyperth. 2017, 33, 810–813. [Google Scholar] [CrossRef]
- Tan, W.P.; Chang, A.; Sze, C.; Polascik, T.J. Oncological and functional outcomes of patients undergoing individualized partial gland cryoablation of the prostate: A single-institution experience. J. Endourol. 2021, 35, 1290–1299. [Google Scholar] [CrossRef] [PubMed]
- Tan, W.P.; ElShafei, A.; Aminsharifi, A.; Khalifa, A.O.; Polascik, T.J. Salvage focal cryotherapy offers similar short-term oncologic control and improved urinary function compared with salvage whole gland cryotherapy for radiation-resistant or recurrent prostate cancer. Clin. Genitourin. Cancer 2020, 18, e260–e265. [Google Scholar] [CrossRef] [PubMed]
- Chang, X.; Liu, T.; Zhang, F.; Zhao, X.; Ji, C.; Yang, R.; Gan, W.; Zhang, G.; Li, X.; Guo, H. Salvage cryosurgery for locally recurrent prostate cancer after primary cryotherapy. Int. Urol. Nephrol. 2015, 47, 301–305. [Google Scholar] [CrossRef] [PubMed]
- Bomers, J.G.R.; Yakar, D.; Overduin, C.G.; Sedelaar, J.P.M.; Vergunst, H.; Barentsz, J.O.; de Lange, F.; Fütterer, J.J. MR imaging-guided focal cryoablation in patients with recurrent prostate cancer. Radiology 2013, 268, 451–460. [Google Scholar] [CrossRef] [PubMed]
- de Castro Abreu, A.L.; Bahn, D.; Leslie, S.; Shoji, S.; Silverman, P.; Desai, M.M.; Gill, I.S.; Ukimura, O. Salvage focal and salvage total cryoablation for locally recurrent prostate cancer after primary radiation therapy. BJU Int. 2013, 112, 298–307. [Google Scholar] [CrossRef]
- Kasivisvanathan, V.; Emberton, M.; Ahmed, H.U. Focal therapy for prostate cancer: Rationale and treatment opportunities. Clin. Oncol. 2013, 25, 461–473. [Google Scholar] [CrossRef]
- Aminsharifi, A.; Jibara, G.; Tsivian, E.; Tsivian, M.; Elshafei, A.; Polascik, T.J. Salvage prostate cryoablation for the management of local recurrence after primary cryotherapy: A retrospective analysis of functional and intermediate-term oncological outcomes associated with a second therapeutic freeze. Clin. Genitourin. Cancer 2019, 17, e831–e836. [Google Scholar] [CrossRef]
- Boissier, R.; Sanguedolce, F.; Territo, A.; Gaya, J.; Huguet, J.; Rodriguez-Faba, O.; Regis, F.; Gallioli, A.; Vedovo, F.; Martinez, C. Partial salvage cryoablation of the prostate for local recurrent prostate cancer after primary radiotherapy: Step-by-step technique and outcomes. Urol. Video J. 2020, 7, 100040. [Google Scholar] [CrossRef]
- Perera, M.; Vilaseca, A.; Tin, A.L.; Nguyen, D.P.; Corradi, R.B.; Touijer, A.S.; Martin-Malburet, A.G.; Alvim, R.; Benfante, N.; Sjoberg, D.D.; et al. Morbidity of salvage radical prostatectomy: Limited impact of the minimally invasive approach. World J. Urol. 2022, 40, 1637–1644. [Google Scholar] [CrossRef]
- Pisters, L.L.; Leibovici, D.; Blute, M.; Zincke, H.; Sebo, T.J.; Slezak, J.M.; Izawa, J.; Ward, J.F.; Scott, S.M.; Madsen, L.; et al. Locally recurrent prostate cancer after initial radiation therapy: A comparison of salvage radical prostatectomy versus cryotherapy. J. Urol. 2009, 182, 517–527. [Google Scholar] [CrossRef]
- Vora, A.; Agarwal, V.; Singh, P.; Patel, R.; Rivas, R.; Nething, J.; Muruve, N. Single-institution comparative study on the outcomes of salvage cryotherapy versus salvage robotic prostatectomy for radio-resistant prostate cancer. Prostate Int. 2016, 4, 7–10. [Google Scholar] [CrossRef] [PubMed]
- Friedlander, D.F.; Gu, X.; Prasad, S.M.; Lipsitz, S.R.; Nguyen, P.L.; Trinh, Q.-D.; Sun, M.; Hu, J.C. Population-based Comparative Effectiveness of Salvage Radical Prostatectomy vs Cryotherapy. Urology 2014, 83, 653–657. [Google Scholar] [CrossRef] [PubMed]
- Autran-Gomez, A.M.; Scarpa, R.M.; Chin, J. High-intensity focused ultrasound and cryotherapy as salvage treatment in local radio-recurrent prostate cancer. Urol. Int. 2012, 89, 373–379. [Google Scholar] [CrossRef] [PubMed]
- Uchida, T.; Illing, R.O.; Cathcart, P.J.; Emberton, M. To what extent does the prostate-specific antigen nadir predict subsequent treatment failure after transrectal high-intensity focused ultrasound therapy for presumed localized adenocarcinoma of the prostate? BJU Int. 2006, 98, 537–539. [Google Scholar] [CrossRef] [PubMed]
- Ben Cheikh, A.; Girouin, N.; Ryon-Taponnier, P.; Mège-Lechevallier, F.; Gelet, A.; Chapelon, J.Y.; Lyonnet, D.; Rouvière, O. Détection par IRM des récidives locales du cancer de prostate après traitement par ultrasons focalisés de haute intensité (HIFU) transrectaux: Étude préliminaire [MR detection of local prostate cancer recurrence after transrectal high-intensity focused US treatment: Preliminary results]. J. Radiol. 2008, 89, 571–577. [Google Scholar] [CrossRef]
- Williams, A.K.; Martínez, C.H.; Lu, C.; Ng, C.K.; Pautler, S.E.; Chin, J.L. Disease-free survival following salvage cryotherapy for biopsy-proven radio-recurrent prostate cancer. Eur. Urol. 2011, 60, 405–410. [Google Scholar] [CrossRef]
- Choyke, P.L.; Bouchelouche, K. Prostate specific membrane antigen (PSMA) imaging: The past is prologue. Transl. Androl. Urol. 2019, 8, 283–285. [Google Scholar] [CrossRef]
- Bologna, E.; Ditonno, F.; Licari, L.C.; Franco, A.; Manfredi, C.; Mossack, S.; Pandolfo, S.D.; De Nunzio, C.; Simone, G.; Leonardo, C.; et al. Tissue-Based Genomic Testing in Prostate Cancer: 10-Year Analysis of National Trends on the Use of Prolaris, Decipher, ProMark, and Oncotype DX. Clin. Pract. 2024, 14, 508–520. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Monaco, A.; Sommer, J.; Okpara, C.; Lischalk, J.W.; Haas, J.; Corcoran, A.; Katz, A. Comparative results of focal-cryoablation and stereotactic body radiotherapy in the treatment of unilateral, low-to-intermediate-risk prostate cancer. Int. Urol. Nephrol. 2022, 54, 2529–2535. [Google Scholar] [CrossRef]
- Lewin, R.; Amit, U.; Laufer, M.; Berger, R.; Dotan, Z.; Domachevsky, L.; Davidson, T.; Portnoy, O.; Tsvang, L.; Ben-Ayun, M.; et al. Salvage re-irradiation using stereotactic body radiation therapy for locally recurrent prostate cancer: The impact of castration sensitivity on treatment outcomes. Radiat. Oncol. 2021, 16, 114. [Google Scholar] [CrossRef]

| References | Institution(s) | Prior Treatment (No. of Patients) | Preprocedural PSA (ng/mL), Median (IQR) | Site of Failure | Predictive Factors | PPV |
|---|---|---|---|---|---|---|
| Hruby et al. (2017) [17] | Royal North Shore Hospital, Australia | EBRT (n = 419) | Median (range): 10 (1–145) | Local only: 8 (16.7%) Local and distant: 15 (31.3%) Distant only: 25 (52%) | Gleason scores ≥ 8 (17% vs. 9%, p = 0.011) and initial PSA > 10 ng/mL (16% vs. 8%, p = 0.04) | NR |
| Einspieler et al. (2017) [18] | Multiple (Germany, USA) | EBRT: 77 BT: 41 (n = 118) | >Median: 10.7 (6.9–24.7) | Local only: 43 (40.2%) Local and distant: 25 (23.4%) Distant only: 39 (36.4%) | Increasing PSA and concomitant ADT (SUVmax: p = 0.018 and 0.004; SUVmean: p = 0.025 and 0.007, respectively) | NR |
| Morris et al. (2021) [19] | Multiple (USA) | n = 208 | Median (range): 0.8 (0.2–98.4) | NR | NR | Prostatic region: 75.0–83.3% (range) Pelvic lymph nodes: 67.2–72.7% Extra-pelvic region: 67.3–69.8% |
| MRI | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | AUC (%) |
|---|---|---|---|---|---|
| Kim et al. (2009) [25], Sungkyunkwan University School of Medicine, Republic of Korea | |||||
| T2W | 25 | 92 | 57 | 74 | 61.2 |
| T2W + DWI | 62 | 97 | 91 | 81 | 87.9 |
| Kim et al. (2010) [26], Kangwon National University College of Medicine, Republic of Korea | |||||
| DWI | 49 | 93 | 72 | 84 | 78.2 |
| DCE | 49 | 92 | 67 | 84 | 73.7 |
| DWI + DCE | 59 | 91 | 69 | 87 | 86.3 |
| T2W | 27 | 80 | 32 | 76 | 59.4 |
| Tamada et al. (2011) [27], Kawasaki Medical School, Japan | |||||
| mpMRI | 77 | 92 | 68 | 95 | NR |
| T2W | 27 | 99 | 86 | 87 | NR |
| DCE | 50 | 98 | 85 | 90 | NR |
| DWI | 68 | 95 | 75 | 94 | NR |
| Imaging | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Accuracy (%) |
|---|---|---|---|---|---|
| Radzina et al. (2020) [28], Multiple (Latvia, Germany) | |||||
| PSMA PET (local) | 63.6 | 73.7 | 58.3 | 77.8 | 77.8 |
| mpMRI (local) | 90.9 | 94.7 | 90.9 | 94.7 | 92.3 |
| PSMA PET (LN) | 83.3 | 80.0 | 80 | 100 | 90.6 |
| mpMRI (LN) | 41.7 | 94.4 | 83.3 | 70.8 | 72.0 |
| PSMA PET (bone) | 83.3 | 92.0 | 71.4 | 95.8 | 71.0 |
| mpMRI (bone) | 50.0 | 84.0 | 42.8 | 87.5 | 77.4 |
| Jannusch et al. (2023) [31], Multiple, Germany | |||||
| PSMA PET (local) | 50 | 96 | 50 | 96 | 93 |
| mpMRI (local) | 100 | 100 | 100 | 100 | 100 |
| PSMA PET (LN) | 96 | 97 | 97 | 97 | 97 |
| mpMRI (LN) | 57 | 92 | 81 | 78 | 79 |
| PSMA PET (dLN) | 50 | 100 | 100 | 98 | 98 |
| mpMRI (dLN) | 0 | 100 | - | 97 | 97 |
| PSMA PET (bone) | 100 | 100 | 100 | 100 | 100 |
| mpMRI (bone) | 67 | 98 | 80 | 96 | 95 |
| References | Institution | Initial Therapy (No. of Pts) | Risk Categories | Preprocedural PSA (ng/mL), Median (IQR) | Mos. Follow-Up | Use of ADT, n (%) | Success/Failure Criteria a | % Pos. Biopsy Rate | Urinary Incontinence, n (%); Erectile Function, n (%) |
|---|---|---|---|---|---|---|---|---|---|
| Campbell et al. (2023) [39] | Duke University Medical Center, Durham, NC, USA | ERBT (419) | D’Amico Low: 120 (28.6%), Intermediate: 140 (33.4%), High: 159 (37.9%) | Mean: 7.01 | Median: 72 (60–170) | 142 (33.9%) | Biochemical progression at 2 years: 55 (13.1%), and 5 years: 90 (21.5%) | NR | 67 (16%); 59 (14.1%) |
| Tan et al. (2023) [40] | Duke University Medical Center, Durham, NC, USA | RT (110) | NR | Median: 3.87 (2.48–5.86) | Median: 71 (42.3–116) | 22 (20%) | BRFS at 12 months: 85%, 24 months: 81%, 36 months: 79%, 48 months: 75%, 60 months: 71%, and 72 months: 67% | NR | 9%; NR |
| Spiess et al. (2013) [41] | Department of Genitourinary Oncology, Tampa, FL | NR (132) | D’Amico Low: 18 (14%), Intermediate: 82 (62%), High: 32 (24%) | Mean: 6.2 (4.9–34.2) | Mean (range): 4.0 (0.9–12.7) | 0 (0%) | bPFS at 1 year: 87.8%, 2 years: 72.4%, and 5 years: 45.5% | NR | NR |
| Wenske et al. (2013) [42] | Multiple, USA | EBRT (259), BT (49), CR (20) | NR | Median (range): 8 (0.6–290) | Median (range): 47 (1.6–203.5) | NR | BRFS at 5 years: 63%, 10 years: 37% | NR | 7 (2.1); NR |
| Lian et al. (2016) [43] | Department of Urology, Nanjing University, China | ERBT (4), BT (28) | NR | Median: 7.9 (3.2–17.6) | Median: 63 (38–92) | 5 (15.6%) | BRFS at 5 years: 43.5% | NR | |
| Ghafar et al. (2001) [44] | Department of Urology, Columbia University, New York, USA | EBRT (38) | NR | Mean: 7.5 | Mean (range): 20.7 (3–37) | 38 (100%) | BRFS at 1 year: 86%, at 2 years: 74% | NR | 3 (7.9); NR |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pio, F.; Murdock, A.; Fuller, R.E.; Whalen, M.J. The Role of Whole-Gland and Focal Cryotherapy in Recurrent Prostate Cancer. Cancers 2024, 16, 3225. https://doi.org/10.3390/cancers16183225
Pio F, Murdock A, Fuller RE, Whalen MJ. The Role of Whole-Gland and Focal Cryotherapy in Recurrent Prostate Cancer. Cancers. 2024; 16(18):3225. https://doi.org/10.3390/cancers16183225
Chicago/Turabian StylePio, Faozia, Andeulazia Murdock, Renee E. Fuller, and Michael J. Whalen. 2024. "The Role of Whole-Gland and Focal Cryotherapy in Recurrent Prostate Cancer" Cancers 16, no. 18: 3225. https://doi.org/10.3390/cancers16183225
APA StylePio, F., Murdock, A., Fuller, R. E., & Whalen, M. J. (2024). The Role of Whole-Gland and Focal Cryotherapy in Recurrent Prostate Cancer. Cancers, 16(18), 3225. https://doi.org/10.3390/cancers16183225






