Risk of Colorectal Cancer among Patients with One or Multiple Metabolic Syndrome Components
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
- Insulin resistance (IR): average fasting glucose ≥100 mg/dL, HbA1c >= 5.7 at any point, receiving drug therapy for hyperglycemia, or type 2 diabetes listed as a billing diagnosis or under the problem list.
- Hypertension (HTN): blood pressure ≥130/85 mm Hg, receiving drug therapy for hypertension, hypertension listed as a billing diagnosis or under the problem list.
- Hypertriglyceridemia (HG): average triglycerides ≥150 mg/dL, receiving drug therapy for hypertriglyceridemia, or hypertriglyceridemia listed as a billing diagnosis or under the problem list.
- Low high-density lipoprotein cholesterol (HDL-C): average HDL-C < 40 mg/dL in men or <50 mg/dL in women, receiving drug therapy for reduced HDL-C, or low HDL-C listed as a billing diagnosis or under the problem list.
- Obesity: average BMI > 30, or obesity listed as a billing diagnosis or under the problem list.
- Demographic variables—current age and gender.
- Body Mass Index (BMI) (in k Lamichhane, g/m2)—Current BMI. We chose BMI because waist circumference was not available in the data.
- Socioeconomic status (SES)—Insurance was used as a proxy for SES, as patient income and education information was unavailable. We accounted for two categories of insurance: Medicaid and Others or unknown, which also included self-pay. Due to a lack of information on different insurance types, we could not further break down the insurance categories.
- Family history of colorectal cancer (CRC)—patients with a family history of CRC were identified using diagnosis codes (ICD9 or ICD10), SNOMED codes, and problem lists.
- Social history (tobacco and alcohol use history)—If the use of any tobacco, including smoking, or alcohol was ever documented during the study period, the patient was said to have a history of tobacco and/or alcohol use. Conversely, if the patient had a documented history of never using tobacco and/or alcohol, they were said to have no history of tobacco and/or alcohol use, respectively.
- Inherited syndromes—whether the patient had a history of familial adenomatous polyposis, hereditary non-polyposis colorectal cancer, Lynch Syndrome, Turcot Syndrome, or Peutz–Jeghers Syndrome.
- History of polyps.
- History of inflammatory bowel disease.
- Presence or absence of insulin resistance, hypertension, low HDL-C, hypertriglyceridemia, and obesity.
- The number of MetS criteria met by the patient.
- Metabolic syndrome (MetS)—patients who met 3 or more of the 5 conditions mentioned above were classified as MetS patients. In contrast, those who did not meet at least 3 criteria were classified as non-MetS patients.
- Presence or absence of colorectal cancer.
- Individual MetS components—IR, low HDL, HTN, and HG.
Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Cancer Society. Cancer Facts & Figures 2020. Atlanta: American Cancer Society. 2020. Available online: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2020/cancer-facts-and-figures-2020.pdf (accessed on 1 April 2021).
- Esposito, K.; Chiodini, P.; Colao, A.; Lenzi, A.; Giugliano, D. Metabolic syndrome and risk of cancer: A systematic review and meta-analysis. Diabetes Care 2012, 35, 2402–2411. [Google Scholar] [CrossRef] [PubMed]
- Ford, E.S. Risks for all-cause mortality, cardiovascular disease, and diabetes associated with the metabolic syndrome: A summary of the evidence. Diabetes Care 2005, 28, 1769–1778. [Google Scholar] [CrossRef]
- Watanabe, S.; Yaginuma, R.; Ikejima, K.; Miyazaki, A. Liver diseases and metabolic syndrome. J. Gastroenterol. 2008, 43, 509–518. [Google Scholar] [CrossRef] [PubMed]
- Raikou, V.D.; Gavriil, S. Metabolic syndrome and chronic renal disease. Diseases 2018, 6, 12. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ritchie, S.A.; Connell, J.M.C. The link between abdominal obesity, metabolic syndrome, and cardiovascular disease. Nutr. Metab. Cardiovasc. Dis. 2007, 17, 319–326. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.A.; Lee, J.H.; Lim, S.Y.; Ha, H.S.; Kwon, H.; Park, Y.; Lee, W.; Kang, M.; Yim, H.; Yoon, K. Metabolic syndrome as a predictor of type 2 diabetes, and its clinical interpretations and usefulness. J. Diabetes Investig. 2013, 4, 334–343. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ahmed, R.L.; Schmitz, K.H.; Anderson, K.E.; Rosamond, W.D.; Folsom, A.R. The metabolic syndrome and risk of incident colorectal cancer. Cancer 2006, 107, 28–36. [Google Scholar] [CrossRef]
- Chen, X.; Liang, H.; Song, Q.; Xu, X.; Cao, D. Insulin promotes progression of colon cancer by upregulation of ACAT1. Lipids Health Dis. 2018, 17, 122. [Google Scholar] [CrossRef] [PubMed]
- Harlid, S.; Myte, R.; Van Guelpen, B. The metabolic syndrome, inflammation, and colorectal cancer risk: An evaluation of large panels of plasma protein markers using repeated, prediagnostic samples. Mediat. Inflamm. 2017, 2017, 4803156. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Stocks, T.; Lukanova, A.; Bjorge, T.; Ulmer, H.; Manjer, J.; Almquist, M.; Concin, H.; Engeland, A.; Hallmans, G.; Nagel, G.; et al. Metabolic factors and the risk of colorectal cancer in 580,000 men and women in the metabolic syndrome and cancer project (Me-Can). Cancer 2011, 117, 2398–2407. [Google Scholar] [CrossRef]
- Tsilidis, K.K.; Brancati, F.L.; Pollak, M.N.; Rifai, N.; Clipp, S.L.; Hoffman-Bolton, J.; Helzlsouer, K.J.; Platz, E.A. Metabolic syndrome components and colorectal adenoma in the CLUE II cohort. Cancer Causes Control 2010, 21, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Aleksandrova, K.; Boeing, H.; Jenab, M.; Bueno-De-Mesquita, H.B.; Jansen, E.; van Duijnhoven, F.J.; Fedirko, V.; Rinaldi, S.; Romieu, I.; Riboli, E.; et al. Metabolic syndrome and risks of colon and rectal cancer: The European prospective investigation into cancer and nutrition study. Cancer Prev. Res. 2011, 4, 1873–1883. [Google Scholar] [CrossRef] [PubMed]
- Trabulo, D.; Ribeiro, S.; Martins, C.; Teixeira, C.; Cardoso, C.; Mangualde, J.; Freire, R.; Gamito, É.; Alves, A.L.; Augusto, F.; et al. Metabolic syndrome and colorectal neoplasms: An ominous association. World J. Gastroenterol. 2015, 21, 5320–5327. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.S.; Hsu, H.S.; Li, C.I.; Jan, C.-I.; Li, T.-C.; Lin, W.-Y.; Lin, T.; Chen, Y.-C.; Lee, C.-C.; Lin, C.-C. Central obesity and atherogenic dyslipidemia in metabolic syndrome are associated with increased risk for colorectal adenoma in a Chinese population. BMC Gastroenterol. 2010, 10, 51. [Google Scholar] [CrossRef]
- Murphy, T.K.; Calle, E.E.; Rodriguez, C.; Kahn, H.S.; Thun, M.J. Body mass index and colon cancer mortality in a large prospective study. Am. J. Epidemiol. 2000, 152, 847–854. [Google Scholar] [CrossRef]
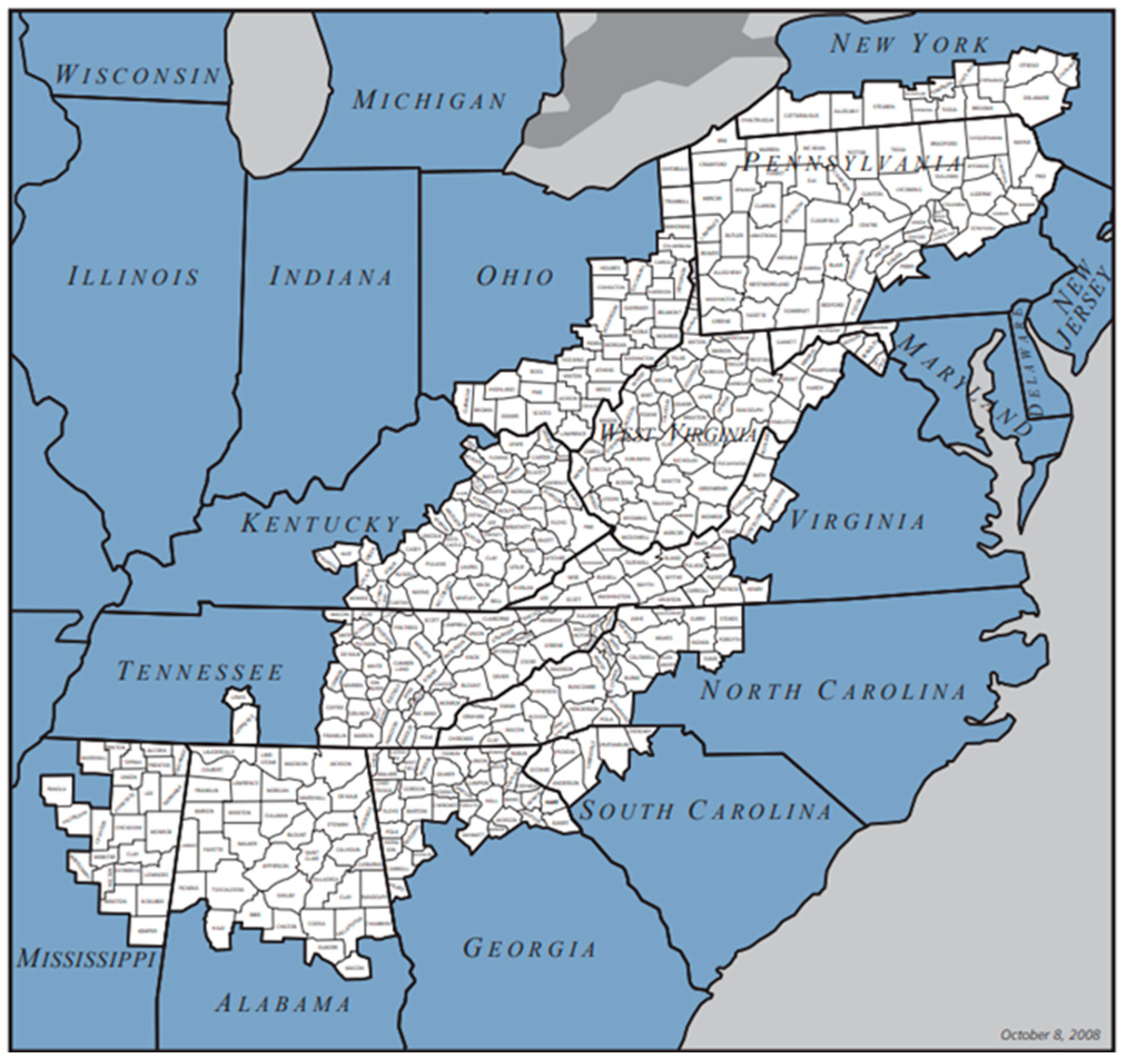
- Wilson, R.J.; Ryerson, A.B.; Singh, S.D.; King, J.B. Cancer incidence in Appalachia, 2004–2011. Cancer Epidemiol. Biomark. Prev. 2016, 25, 250–258. [Google Scholar] [CrossRef] [PubMed]
- Pollard, K.; Jacobsen, L.A. American Community Survey. Appalachian Regional Commission; 2014. The Appalachian Region: A Data Overview from the 2008–2012. Available online: https://www.arc.gov/wp-content/uploads/2020/06/DataOverviewfrom2008-2012ACS.pdf (accessed on 14 April 2020).
- Coughlin, S.S.; Thompson, T.D. Colorectal cancer screening practices among men and women in rural and non-rural areas of the United States, 1999. J. Rural Health 2004, 20, 118–124. [Google Scholar] [CrossRef]
- Dignan, M.; Shelton, B.; Slone, S.A.; Tolle, C.; Mohammad, S.; Schoenberg, N.; Pearce, K.; Van Meter, E.; Ely, G. Effectiveness of a primary care practice intervention for increasing colorectal cancer screening in Appalachian Kentucky. Prev. Med. 2014, 58, 70–74. [Google Scholar] [CrossRef] [PubMed]
- Map of Appalachian Counties. Appalachian Regional Commission. Available online: https://www.arc.gov/about-the-appalachian-region/ (accessed on 16 April 2020).
- Colorectal Cancer Risk Factors. American Cancer Society. Available online: https://www.cancer.org/cancer/colon-rectal-cancer/causes-risks-prevention/risk-factors.html (accessed on 19 April 2020).
- Hannan, L.M.; Jacobs, E.J.; Thun, M.J. The association between cigarette smoking and risk of colorectal cancer in a large prospective cohort from the United States. Cancer Epidemiol. Biomark. Prev. 2009, 18, 3362–3367. [Google Scholar] [CrossRef]
- Johnson, C.M.; Wei, C.; Ensor, J.E.; Smolenski, D.J.; Amos, C.I.; Levin, B.; Berry, D.A. Meta-analyses of colorectal cancer risk factors. Cancer Causes Control. CCC 2013, 24, 1207–1222. [Google Scholar] [CrossRef]
- Muller, A.D.; Sonnenberg, A. Prevention of colorectal cancer by flexible endoscopy and polypectomy. A case-control study of 32,702 veterans. Ann. Intern. Med. 1995, 123, 904–910. [Google Scholar] [CrossRef] [PubMed]
- Stryker, S.J.; Wolff, B.G.; Culp, C.E.; Libbe, S.D.; Ilstrup, D.M.; MacCarty, R.L. Natural history of untreated colonic polyps. Gastroenterology 1987, 93, 1009–1013. [Google Scholar] [CrossRef] [PubMed]
- Amersi, F.; Agustin, M.; Ko, C.Y. Colorectal cancer: Epidemiology, risk factors, and health services. Clin. Colon Rectal Surg. 2005, 18, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, C.S.; Giovannucci, E.L.; Colditz, G.A.; Hunter, D.J.; Speizer, F.E.; Willett, W.C. A prospective study of family history and the risk of colorectal cancer. N. Engl. J. Med. 1994, 331, 1669–1674. [Google Scholar] [CrossRef] [PubMed]
- Smith, R.A.; Von Eschenbach, A.C.; Wender, R.; Levin, B.; Byers, T.; Rothenberger, D.; Brooks, D.; Creasman, W.; Cohen, C.; Runowicz, C.; et al. American Cancer Society guidelines for early cancer detection: Update of early detection guidelines for prostate, colorectal, and endometrial cancers. CA Cancer J. Clin. 2001, 51, 38–75. [Google Scholar] [CrossRef] [PubMed]
- Baek, J.H.; Kim, H.; Kim, K.Y.; Jung, J. Insulin resistance and the risk of diabetes and dysglycemia in Korean general adult population. Diabetes Metab. J. 2018, 42, 296–307. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Giovannucci, E. Insulin and colon cancer. Cancer Causes Control 1995, 6, 164–179. [Google Scholar] [CrossRef]
- Komninou, D.; Ayonote, A.; Richie, J.P.; Rigas, B. Insulin resistance and its contribution to colon carcinogenesis. Exp. Biol. Med. 2003, 228, 396–405. [Google Scholar] [CrossRef] [PubMed]
- Cirillo, F.; Catellani, C.; Sartori, C.; Lazzeroni, P.; Amarri, S.; Street, M.E. Obesity, Insulin resistance, and colorectal cancer: Could miRNA dysregulation play a role? Int. J. Mol. Sci. 2019, 20, 2922. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Farahani, H.; Mahmoudi, T.; Asadi, A.; Nobakht, H.; Dabiri, R.; Hamta, A. Insulin resistance and colorectal cancer risk: The role of elevated plasma resistin levels. J. Gastrointest. Cancer 2020, 51, 478–483. [Google Scholar] [CrossRef]
- Cedó, L.; Reddy, S.T.; Mato, E.; Blanco-Vaca, F.; Escolà-Gil, J.C. HDL and LDL: Potential new players in breast cancer development. J. Clin. Med. 2019, 8, 853. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Murai, T. Cholesterol lowering: Role in cancer prevention and treatment. Biol. Chem. 2015, 396, 1–11. [Google Scholar] [CrossRef]
- McKeown-Eyssen, G. Epidemiology of colorectal cancer revisited: Are serum triglycerides and/or plasma glucose associated with risk. Cancer Epidemiol. Biomark. Prev. 1994, 3, 687–695. [Google Scholar]
- Bruce, W.R.; Wolever, T.M.; Giacca, A. Mechanisms linking diet and colorectal cancer: The possible role of insulin resistance. Nutr. Cancer 2000, 37, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Niho, N.; Takahashi, M.; Shoji, Y.; Takeuchi, Y.; Matsubara, S.; Sugimura, T.; Wakabayashi, K. Dose-dependent suppression of hyperlipidemia and intestinal polyp formation in Min mice by pioglitazone, a PPAR gamma ligand. Cancer Sci. 2003, 94, 960–964. [Google Scholar] [CrossRef] [PubMed]
- Gaard, M.; Tretli, S.; Urdal, P. Blood lipid and lipoprotein levels and the risk of cancer of the colon and rectum. A prospective study of 62,173 Norwegian men and women. Scand. J. Gastroenterol. 1997, 32, 162–168. [Google Scholar] [CrossRef]
- Mannes, G.A.; Maier, A.; Thieme, C.; Wiebecke, B.; Paumgartner, G. Relation between the frequency of colorectal adenoma and the serum cholesterol level. N. Engl. J. Med. 1986, 315, 1634–1638. [Google Scholar] [CrossRef]
- Baena, R.; Salinas, P. Diet and colorectal cancer. Maturitas 2015, 80, 258–264. [Google Scholar] [CrossRef] [PubMed]
- Gill, C.I.R.; Rowland, I.R. Diet and cancer: Accessing the risk. Br. J. Nutr. 2002, 88 (Suppl. S1), S73–S87. [Google Scholar] [CrossRef]
- Abualkhair, W.H.; Zhou, M.; Ahnen, D.; Yu, Q.; Wu, X.-C.; Karlitz, J.J. Trends in incidence of early-onset colorectal cancer in the United States among those approaching screening age. JAMA Netw. Open 2020, 3, e1920407. [Google Scholar] [CrossRef] [PubMed]
- Karanikas, M.; Esebidis, A. Increasing incidence of colon cancer in patients <50 years old: A new entity? Ann. Transl. Med. 2016, 4, 164. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
| Variables | Mean or n | SE or % | |
|---|---|---|---|
| Total Sample | 263,023 | ||
| Age (in yrs.) | 59.9 (median = 61) | 0.03 | |
| BMI (in Kg/m2) | 30.9 | 0.02 | |
| No. of Criteria Met | 3.6 (median = 4) | 0.00 | |
| Colorectal Cancer (CRC) | |||
| Yes | 3474 | 1.3 | |
| No | 259,549 | 98.7 | |
| Gender | |||
| Female | 140,469 | 53.4 | |
| Male | 122,554 | 46.6 | |
| Weight Category | |||
| Obese | 124,456 | 47.9 | |
| Overweight | 77,585 | 29.9 | |
| Others | 57,704 | 22.2 | |
| Age Group | |||
| <50 yrs. | 68,610 | 26.1 | |
| 50–65 yrs | 84,498 | 32.1 | |
| >=65 yrs. | 109,915 | 41.8 | |
| Insurance | |||
| Medicaid or Medicare | 14,964 | 5.7 | |
| Others or unknown | 248,059 | 94.3 | |
| Tobacco Use | |||
| Yes | 128,469 | 48.8 | |
| No | 134,554 | 51.2 | |
| Alcohol Use | |||
| Yes | 31,183 | 11.9 | |
| No | 231,840 | 88.1 | |
| Family History of CRC or Inherited Syndromes | |||
| Yes | 17,617 | 6.7 | |
| No | 245,406 | 93.3 | |
| Inflammatory Bowel Disease | |||
| Yes | 15,485 | 5.9 | |
| No | 247,538 | 94.1 | |
| History of Polyps | |||
| Yes | 21,219 | 8.1 | |
| No | 241,804 | 91.9 | |
| Type II Diabetes | |||
| Yes | 96,162 | 36.6 | |
| No | 166,861 | 63.4 | |
| MetS | |||
| Yes | 211,510 | 80.4 | |
| No | 51,513 | 19.6 | |
| IR | |||
| Yes | 194,400 | 73.9 | |
| No | 68,623 | 26.1 | |
| HDL | |||
| Yes | 212,373 | 80.7 | |
| No | 50,650 | 19.3 | |
| HTN | |||
| Yes | 211,116 | 80.3 | |
| No | 51,907 | 19.7 | |
| TG | |||
| Yes | 204,356 | 77.7 | |
| No | 58,667 | 22.3 | |
| IR and HDL Only | |||
| both IR and HDL but no TG, HTN, or obesity | 1812 | 10.5 | |
| HTN, TG, or obesity but no IR or HDL | 15,495 | 89.5 |
| Components | n | Risk Ratio (RR) | 95% CI | Attributable Risk (per 10,000) |
|---|---|---|---|---|
| MetS | 3092 | 1.97 | (1.77, 2.19) | 72 |
| IR | 2970 | 2.08 | (1.89, 2.29) | 79 |
| HDL | 3068 | 1.8 | (1.63, 2.00) | 64 |
| HTN | 3071 | 1.87 | (1.69, 2.08) | 68 |
| TG | 3008 | 1.85 | (1.68, 2.04) | 68 |
| CI | ||||
|---|---|---|---|---|
| Symptom | RR | LL | UL | p-Value |
| MetS | 1.28 | 1.14 | 1.42 | <0.001 |
| IR | 1.60 | 1.45 | 1.76 | <0.001 |
| HDL | 1.29 | 1.16 | 1.44 | <0.001 |
| HTN | 1.13 | 1.01 | 1.26 | <0.001 |
| TG | 1.17 | 1.06 | 1.30 | <0.001 |
| CI | ||||
|---|---|---|---|---|
| Variables | RR | LL | UL | p-Value |
| IR (Reference = No IR) | 1.55 | 1.40 | 1.71 | <0.0001 |
| HTN (Reference = No HTN) | 1.04 | 0.93 | 1.16 | 0.536 |
| HDL (Reference = No HDL) | 1.24 | 1.08 | 1.42 | 0.002 |
| TG (Reference = No TG) | 0.98 | 0.86 | 1.12 | 0.752 |
| BMI | 1.08 | 1.06 | 1.10 | <0.0001 |
| Gender (Male; Reference = Female) | 1.02 | 0.95 | 1.09 | 0.563 |
| Insurance (Reference = Others) | 1.46 | 1.26 | 1.70 | <0.0001 |
| Age Group 50-65 yrs (Reference = <50 yrs) | 1.93 | 1.69 | 2.21 | <0.0001 |
| Age Group 65 yrs. and above (Reference = <50 yrs) | 3.21 | 2.81 | 3.68 | <0.0001 |
| Smoke (Reference = No History of Smoking) | 1.22 | 1.14 | 1.31 | <0.0001 |
| Alcohol Use (Reference = No Alcohol Use) | 1.32 | 1.20 | 1.45 | <0.0001 |
| History of CRC or Inherited Diseases (Reference = No History of CRC or Inherited Diseases) | 3.64 | 3.31 | 4.01 | <0.0001 |
| History of Inflammatory Bowel Disease (Reference = No History of Inflammatory Bowel Disease) | 1.89 | 1.71 | 2.09 | <0.0001 |
| History of Polyps (Reference = No History of Polyps) | 1.75 | 1.59 | 1.93 | <0.0001 |
| CI | |||||
|---|---|---|---|---|---|
| Symptom | RR | LL | UL | p-Value | ROC-AUC (%) |
| MetS | 1.28 | 1.14 | 1.42 | <0.001 | 72.6 |
| IR+HDL Only | |||||
| Both IR and HDL | 2.65 | 1.68 | 4.20 | <0.001 | 79.5 |
| HTN or TG or Obese but no IR or HDL | Reference | ||||
| Among Individuals <65 yrs. Old | |||||
| IR+HDL | |||||
| Both IR and HDL | 2.39 | 1.35 | 4.23 | <0.001 | 76.9 |
| HTN or TG or Obese but no IR or HDL | Reference | ||||
| Among 65-or-Older Age Group | |||||
| IR+HDL Only | |||||
| Both IR and HDL | 2.67 | 1.25 | 5.69 | <0.001 | 71.1 |
| HTN or TG or Obese but no IR or HDL | Reference | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sundaram, S.; Lamichhane, R.; Cecchetti, A.; Murughiyan, U.; Sundaram, U. Risk of Colorectal Cancer among Patients with One or Multiple Metabolic Syndrome Components. Cancers 2024, 16, 3350. https://doi.org/10.3390/cancers16193350
Sundaram S, Lamichhane R, Cecchetti A, Murughiyan U, Sundaram U. Risk of Colorectal Cancer among Patients with One or Multiple Metabolic Syndrome Components. Cancers. 2024; 16(19):3350. https://doi.org/10.3390/cancers16193350
Chicago/Turabian StyleSundaram, Shanmuga, Rajan Lamichhane, Alfred Cecchetti, Usha Murughiyan, and Uma Sundaram. 2024. "Risk of Colorectal Cancer among Patients with One or Multiple Metabolic Syndrome Components" Cancers 16, no. 19: 3350. https://doi.org/10.3390/cancers16193350
APA StyleSundaram, S., Lamichhane, R., Cecchetti, A., Murughiyan, U., & Sundaram, U. (2024). Risk of Colorectal Cancer among Patients with One or Multiple Metabolic Syndrome Components. Cancers, 16(19), 3350. https://doi.org/10.3390/cancers16193350





