Simple Summary
One third of all patients with acute myeloid leukaemia (AML) carry a nucleophosmin mutation (NPMmut). This is associated with improved survival and which may be due to the immune response these cells can generate. However the reason is not fully understood. In this review we discuss the ways that patients with an NPM1mut are treated clinically and how preclinical studies are informing best practice for patients with AML NPMmut.
Abstract
Acute myeloid leukemia (AML) is a malignant disease of the blood and bone marrow that is characterized by uncontrolled clonal proliferation of abnormal myeloid progenitor cells. Nucleophosmin 1 (NPM1) gene mutations are the most common genetic abnormality in AML, detectable in blast cells from about one-third of adults with AML. AML NPM1mut is recognized as a separate entity in the World Health Organization classification of AML. Clinical and survival data suggest that patients with this form of AML often have a more favorable prognosis, which may be due to the immunogenicity created by the mutations in the NPM1 protein. Consequently, AML with NPM1mut can be considered an immunogenic subtype of AML. However, the underlying mechanisms of this immunogenicity and associated favorable survival outcomes need to be further investigated. Immune checkpoint molecules, such as the programmed cell death-1 (PD-1) protein and its ligand, PD-L1, play important roles in leukemogenesis through their maintenance of an immunosuppressive tumor microenvironment. Preclinical trials have shown that the use of PD-1/PD-L1 checkpoint inhibitors in solid tumors and lymphoma work best in novel therapy combinations. Patients with AML NPM1mut may be better suited to immunogenic strategies that are based on the inhibition of the PD-1 immune checkpoint pathway than patients without this mutation, suggesting the genetic landscape of patients may also inform best practice for the use of PD-1 inhibitors.
1. Introduction
Nucleophosmin 1 (NPM1.1 or NPM1) is a mainly nucleolar protein that shuttles between nucleoli, nucleoplasm and cytoplasm chaperoning nucleic acids and proteins. It is expressed abundantly in all tissues [1] and plays a crucial role in cell cycle control, centrosome duplication, ribosome maturation and export, and cellular responses to a variety of stress signals. NPM1 is altered by overexpression, chromosomal translocations and mutations in solid and hematological cancers (reviewed in [2]). In hematological malignancies, the NPM1 gene is frequently combined with other genes to generate fusion proteins that retain the oligomerization domain in the N-terminus of NPM1, including NPM1-RARα in a subset of acute promyelocytic leukemia patients [3] and the rare NPM1-MLF1 [4] translocation, which is associated with the progression of myelodysplastic syndrome (MDS) to acute myeloid leukemia (AML).
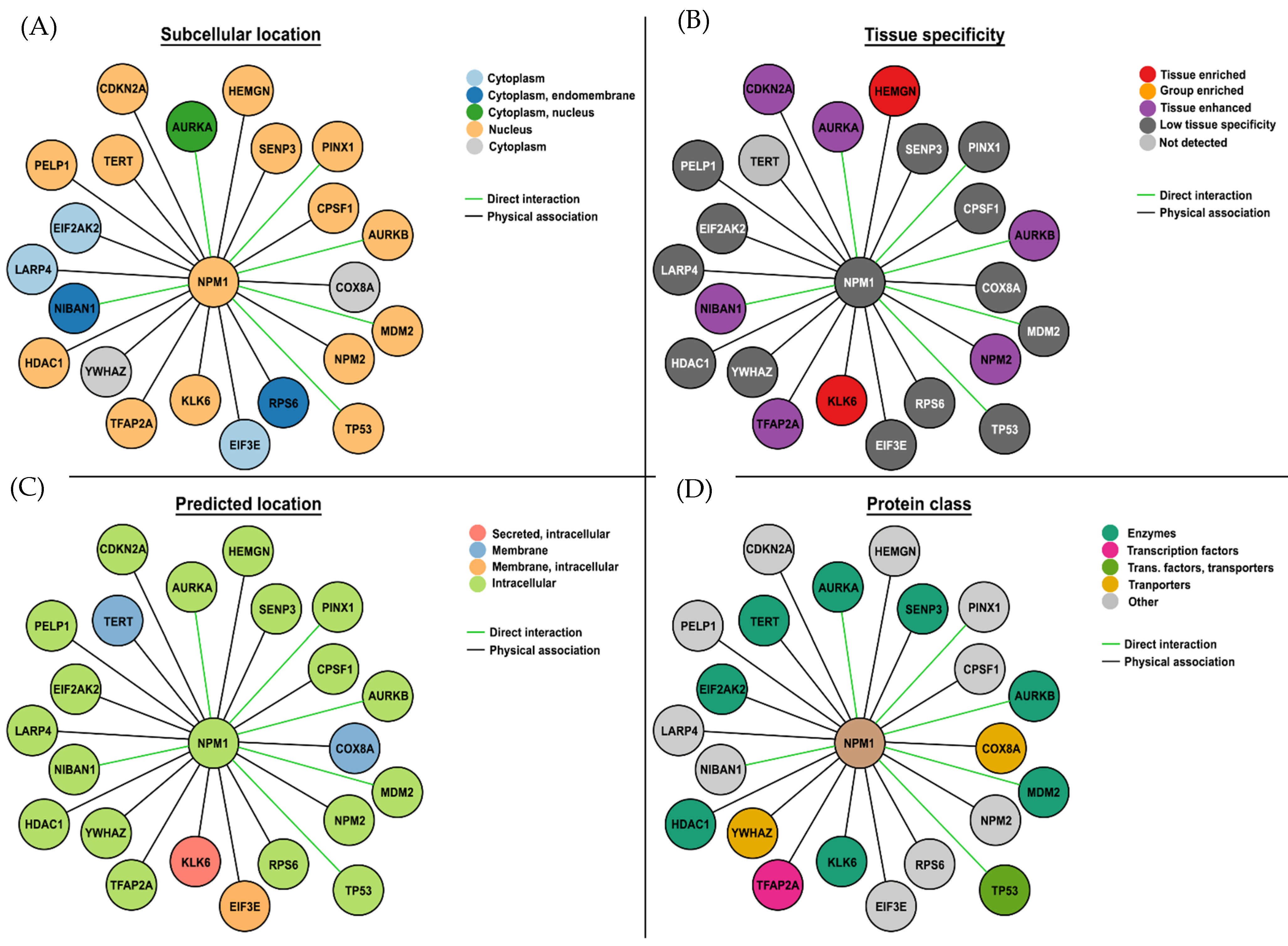
The majority of point mutations in NPM occur in Exon 12 and are named alphabetically. Mutation A, a duplication of TCTG, is the most common [5], followed by Mutations B and D, and each of these point mutations, although different, almost always leads to the same outcome, a frameshift that creates a C-terminus sequence with a disrupted nucleolar localization signal and a third nuclear export sequence. As a consequence, NPM1 no longer predominantly resides in the nucleolus but relocates to the cytoplasm [5,6,7,8], where it is referred to as NPMc+. Accumulation of NPMc+ in the cytoplasm can be detected by immunocytochemistry [9] and qPCR, which allows the monitoring of molecular minimal residual disease (MRD) in patients [10]. NPM1c+ interacts with a number of other proteins (Figure 1), including itself, mostly using its N-terminal domain (reviewed in [11]).
Figure 1.
Direct interactions between wild-type NPM1 (NPM1WT) and proteins. The (A) subcellular localization, (B) tissue specificity, (C) predicted subcellular localization, and (D) protein class are indicated for each protein that NPM1WT interacts with. Data taken from Protein Atlas (https://www.proteinatlas.org/; accessed on 18 June 2024) and drawn in Photoshop. As expected, most interactions are with nuclear proteins, most proteins are expressed in multiple tissues, intracellular locations, and enzymes based on direct interactions and proximity.
Alterations in NPM1 are considered to be a gatekeeper mutation, one of the first hits in the process of leukemogenesis (reviewed in [12]). AML patients with a nucleophosmin-1 mutation (NPM1mut) are recognized as a separate entity by the World Health Organization (WHO) [12,13], since NPM1mut is a founder genetic event that is rare in MDS [14] with distinct genetic, pathological, immunophenotypic, and clinical characteristics (Table 1). In this review, we will discuss AML NPM1mut in the context of immunotherapeutic approaches that have been developed to treat it.

Table 1.
Notable associated features of AML patients with NPM1mut (based on [15,16]).
2. AML NPM1mut and Prognosis
Survival rates for patients with AML are unfortunately still low. The 7 + 3 regimen achieves an estimated 5-year survival rate of 30% to 35% in younger adult patients (age < 60) and 10–15% in older patients (age > 60) [17]. Therefore, exploring new therapeutic options, especially for older patients, is crucial to improve survival rates and address risk factors. NPM1mut are found more commonly in older adult AML patients (over 35 years of age) (Table 1) and correlate with high white cell counts and normal karyotypes [17]. They are present in the M1–M6 subtypes (French American British (FAB) classification of AML), but absent in AML M0 and patients with t(8;21), inv(16), t(15;17), or CCAAT/enhancer-binding protein-α (CEBPA) mutations [15]. Homeobox (HOX) genes (A4, A5, A6, A7, A9, A10, B2, B3, B5, B6) as well as the HOX-related genes, PBX3 and MEIS1, are upregulated in AML NPM1mut samples, while CD34 mRNA levels are low/absent in AML patients with NPM1mut.
There are distinct patterns of co-mutations in NPM1mut patients, and there are gene–gene interactions that are particularly pronounced, causing patterns of co-incidental mutationally defined groups with a favorable, or, conversely, adverse prognosis [18]. The concurrence of NPM1mut is twice as frequent in patients with FLT3-ITD than those with NPM1WT. This may be explained by both being caused by replication slippage errors [19], with the belief that NPM1mut precedes FLT3-ITD [5,20]. FLT3-ITD is associated with poor survival in younger (<60 years) but not in older (60–74 years) AML patients, while NPM1mut is associated with good survival in older but not younger patients, when considering age as well as sex [21]. The European LeukemiaNet (ELN) 2022 results showed that younger patients with NPM1mut, who were FLT3-ITD negative and received high-dose chemotherapy, had a favorable risk classification as an initial risk assignment.
Ostronoff et al. [22] used a different age range and associated this genotype with a comparatively favorable prognostic factor for younger AML patients (55–65 years) but not for older patients (>65 years). Patients with NPM1mut but without a FLT3-ITD translocation often have a favorable prognosis [15], including a better overall survival (OS) rate [23].
Angenendt and colleagues [24] conducted a study on a group of over 2400 AML patients with NPM1mut/FLT3-ITDneg/low, who had varying karyotypes and chromosomal abnormalities. The results showed that in patients with NPM1mut/FLT3-ITDneg/low AML, unfavorable cytogenetics were linked to a lower 5-year OS rate (52.4%, 44.8%, and 19.5% for normal, aberrant intermediate, and adverse karyotypes, respectively). This highlights the significant impact of karyotype abnormalities on the survival outcome of NPM1mut/FLT3-ITDneg/low AML patients. In patients who have adverse-risk cytogenetics, those with NPM1mut have a similarly poor prognosis as those with NPM1WT and should receive treatment accordingly.
Over a long-term follow-up period of 60 months, survival, outcome, and the likelihood of relapse were similar in AML patients with and without NPM1mut, and this is because NPM1mut are significantly associated with normal karyotypes and FLT3-ITD mutations (Table 2). In the group with an intermediate cytogenetic risk without FLT3-ITD but with NPM1mut, patients have a significantly better OS and EFS than patients without NPM1 mutations (p = 0.05) [15].

Table 2.
Definition of AML-NPM1mut risk groups by concurrent clinical, molecular, and cytogenetic indicators.
3. AML NPM1mut Treatment Strategies
According to the ELN guidelines [12], new combination trials in patients eligible for intensive chemotherapy typically involve the incorporation of a new target or agent in combination with standard “7 + 3” chemotherapy. Examples of new targets or agents include ongoing clinical trials involving the FLT3 inhibitor gilteritinib versus midostaurin or the spleen tyrosine kinase (SYK) inhibitor for AML NPM1mut. In a randomized study, treatment with gemtuzumab–ozogamicin (GO) led to a reduction in the relapse probability and greater NPM1mut molecular clearance but with no difference in EFS [35,36].
The NPM1mut protein is a desirable target structure for customized immunotherapy approaches, especially for patients with chronic MRD or AML NPM1mut patients receiving maintenance treatment. In an AML NPM1mut patient in molecular relapse, pre-emptive DLI resulted in poly-specific cytotoxic T-lymphocyte (CTL) responses against multiple leukemia-associated antigens (LAAs), including NPM1 #3 [37]. Jäger et al. [38] examined 64 patients with AML NPM1mut and showed that MRD-negative patients in complete remission (CR) achieve better 2-year progression-free survival (PFS) and 2-year OS compared with patients with MRD-positive patients in CR. They showed that alloHSCT in AML NPM1mut patients depends on the disease burden, relapse type, and response to CT. AlloHSCT transplantation does not seem to benefit NPM1mut/FLT3-ITD-negative patients when used as a first-line treatment; nevertheless, further clinical trials are being conducted, and MRD needs to be considered [38].
AML NPMmut cells are responsive to different cytotoxic agents such as demethylating agents and those that cause BCL-2 inhibition. DiNardo et al. [39] showed that the BCL2 inhibitor, venetoclax, achieved high response rates and durable remissions in older AML patients with NPM1 or IDH2 mutations. Subsequently, Jäger et al. [38] showed, albeit in a small number of patients, that hypomethylating agents combined with venetoclax may be an effective alternative treatment for AML NPM1mut, especially where an isocitrate dehydrogenase (NADP+ 2) IDH2 mutation is present. Effective relapse treatments were offered, with a particular emphasis on the incidence of mild or moderate graft versus host disease (GvHD), which is most likely caused by an immunological graft versus leukemia (GvL) effect.
Forghieri et al. [40] recently wrote about a promising therapeutic approach involving the use of neoantigen-specific T cells, i.e., genetically engineered T cells, such as CAR-T or TCR-transduced T cells directed against NPM1mut peptides presented on HLA. In patients with full-blown leukemia, adoptive or vaccine-based immunotherapies may not be very effective, but these strategies, possibly in combination with immune checkpoint inhibitors (ICIs), may be able to maintain remission or pre-emptively eradicate persistent measurable residual disease (discussed further in Section 5.3). This also applies to patients who are not eligible for alloHSCT.
In summary, the main treatment for AML NPM1mut in younger adults involves standard induction chemotherapy (7+3) with or without FLT3 inhibitors and consolidation rounds using high/medium doses of cytarabine. Allogeneic stem cell transplants may be used in first CR, based on FLT3 gene status and measurable residual disease levels. Recently, several new drugs have been approved for AML NPM1mut, including FLT3 and BCL-2 inhibitors. Multiple studies back the use of GO in the initial treatment of AML NPM1mut [12,41]. Additionally, menin inhibitors constitute a promising new therapy for AML NPM1mut [42].
4. Immunogenic Mutation-Related Targets
Liso et al. [43] demonstrated that mutant NPM1 peptides can be presented in the context of HLA, and showed that AML NPM1mut cells could stimulate anti-leukemic T cell responses. Different CD4+ and CD8+ T cell responses to NPM1mut epitopes have been identified [44], including two HLA-A2-restricted peptides, #1 and #3, which induced distinct T cell responses (33% and 44%, respectively). Compared with healthy individuals, AML NPM1mut patients exhibited significantly higher frequencies of CTL responses against Peptide #3 (p = 0.046). In a survival analysis of 25 patients with AML NPM1mut, Greiner et al. [45] observed that those exhibiting specific CD8+ cytotoxic T cell immune responses against one or two immunogenic peptides had a better OS compared with those without such immune responses (p = 0.004). Schneider et al. [46] isolated a leukemic stem cells (LSC)-enriched population from both NPM1mut and WT patients, and noted that the frequencies of CD34+CD38− cells in AML NPM1mut samples were significantly lower. They found a number of differentially expressed genes of immunological relevance in these populations, including immunoglobulin superfamily member 10 (p = 0.00034), CD96 (p = 0.00052) and IL-12 receptor beta 1 (IL12RB1, p = 0.000834). These markers are involved in immune mechanisms and antigen presentation, highlighting the potential of immune-based therapies that target this subtype of AML patients to be effective.
Kuželová et al. [47] found that in a cohort of 63 AML patients with NPM1mut, compared with 94 patients with NPM1WT, there was a significant decrease in HLA-B*07, B*18, and B*40 expression. There was also a notable OS advantage for AML NPM1mut patients who expressed one of these depleted haplotypes (p = 0.02), suggesting that HLA-B*07, B*18 and B*40 are more effective at generating an anti-leukemia immune response.
Van der Lee et al. [48] identified multiple NPM1mut-derived peptides and demonstrated specific recognition and lysis of AML NPM1mut cells after retroviral transfer to CD8+ and CD4+ T cells. The discovery of common peptide targets in AML NPM1mut patients’ mutations provides an important immunotherapeutic treatment avenue for this subgroup of patients [49].
Among the most prevalent LAAs in AML are Wilms’ tumor antigen 1 (WT-1), Proteinase 3, and receptor for hyaluronan-mediated motility (RHAMM; reviewed in [50]). Cancer-testis antigens, such as helicase antigen (HAGE) and Per ARNT Sim domain containing 1 (PASD1), are expressed less frequently (23% and 35%, respectively) but have disease-specific expression [51,52], with little to no expression in healthy tissues, except in immunologically protected sites. All have been shown to generate antigen-specific CD8+ T cell responses from AML patients [53], and peptide vaccination studies investigating these antigens [54,55,56,57,58] revealed immunological and clinically relevant responses. Greiner et al. [59] examined anti-LAA responses using T cells from NPM1mut and NPM1WT AML patients. The authors showed that the anti-leukemia response was effective against NPM1mut cells when the immunogenic epitope was derived from the mutated region of NPM1 compared with other epitopes/LAA, and these effects were enhanced through the addition of anti-programmed cell death protein 1 (PD-1).
5. Monoclonal Antibody Therapies
The standard treatment for AML has remained largely unchanged during the past few decades, which is the standard “7 + 3” regimen and includes a seven-day infusion of cytarabine and a three-day treatment with an anthracycline. It is commonly used to achieve CR and is particularly successful in patients aged 65 years and under. In recent years, significant advances in our understanding of the pathogenesis of AML, the development of diagnostic assays, and the approval of new treatments has led to updates in the standard care for AML patients.
5.1. αCD33
CD33 is primarily a myeloid differentiation antigen with initial expression at the very early stages of myeloid cells’ development and it is not expressed outside the hematopoietic system or on pluripotent HSCs. FLT3-ITD and NPM1mut were found to have increased expression of CD33 in patients. Both antigens are expressed on proliferative blasts and LSCs and dual targeting of CD33 and CD123 may enhance treatment efficacy for AML [60]. Several approaches, such as monoclonal antibodies and CAR-T cells, have been suggested to target overexpression of CD33 and CD123 on AML blasts. Lintuzumab is a humanized IgG1 against CD33 that has shown only modest activity in clinical trials [61,62,63]. Due to its toxicity in the liver and normal hematopoietic cells, the Phase 3 trial was terminated [64], reflecting the fact that CD33 is largely expressed on myeloid lineage cells, including progenitor cells as well as on neutrophils, natural killer (NK) cells, a subset of B cells, and Kupffer cells in the liver [65].
Due to the short-term effect of αCD33, caused by its rapid internalization when it binds, bivalent antibodies conjugated to toxins have been developed to enhance CD33’s efficacy [64]. In 2017, after a decade of controversy, the Food and Drug Administration (FDA) authorized the use of GO, a humanized monoclonal αCD33 antibody, coupled with the cytotoxic chemical calicheamicin. When GO binds to CD33, it is internalized and calicheamicin is released, triggering DNA double-strand breaks that cause cell death.
Several trials have shown that augmenting the standard treatment with GO has had promising results. It is recommended that GO is added to the first cycle of standard 7+3 induction therapy, especially for CD33-positive AML NPM1mut [12,66,67]. In the randomized AMLSG 09-09 study for NPM1mut patients, CR rates were similar with and without GO, but relapse-free survival was prolonged to a clinically relevant extent in those patients who achieved a CR [68]. The inclusion of GO in intensive chemotherapy for AML NPM1mut patients led to a notable decrease in NPM1mut transcript levels throughout all treatment cycles, explaining this significant reduction in the relapse rates [35,36].
GO has been approved in conjunction with aggressive treatment for newly diagnosed AML patients [69]. GO was initially designed as a monotherapy with a single 9 mg/m2 dose for the first recurrence of CD33+ AML. Later, the dosage was adjusted to 3 mg/m2 on Days 1, 4, and 7 (or possibly only one dose on Day 1) of induction therapy and on Day 1 of consolidation therapy [12]. In the AML-SG study, a randomized trial was conducted to evaluate GO in combination with intensive induction and consolidation therapy in NPM1-mutated AML, as the high CD33 expression in AML with mutated NPM1 provides a rationale for the evaluation of GO in this AML entity. A higher mortality rate was observed in the GO group. More patients over the age of 70 died during induction therapy in the GO group than in the standard group [36].
In another study, the CR recovery rate was 13%, with a median recurrence-free survival of 6.4 months. The most common consequences were Grade 3 and 4 neutropenia (98%), thrombopenia (99%), and a few veno-occlusive disorders (0.9%). In up to 25–35% of patients with newly diagnosed or relapsed/refractory (R/R) AML, GO induced CR or CR with incomplete platelet recovery, especially in AML patients with a favorable prognosis [69]. GO also eliminated MRD in extensively treated individuals with a reduced response [70]. GO enhanced the 5-year OS and significantly reduced relapse rates in AML patients with NPM1mut (p = 0·0028) [71]. However, combining GO with intensive CT for NPM1 AML patients in a randomized AMLSG 09-09 trial (NCT00893399) resulted in a high mortality rate [72]. Patient-administered GO had lower associated relapse rates compared with the standard treatment [72].
5.2. αCD123
Targeting CD123 has been suggested as an AML treatment; however, its efficacy was unsatisfactory, except in AML NPM1mut/or patients with a FLT3-ITD mutation. This is because these patients have an LSC population enriched in CD34+/CD38− cells [73]. Using a naked antibody that targeted CD123 (CSL362) caused lysis of the AML cells that expressed CD123 due to the activation of the innate immune system [74]. However, in a clinical trial of 40 patients with R/R AML, only two patients had a clinical response [74].
Tagraxofusp (SL-401) is a recombinant αCD123 (IL-3 receptor alpha chain) antibody based on the diphtheria toxin. Following its attachment to CD123 and the inhibition of eukaryotic elongation factor 2 (eEF2), tagraxofusp was internalized. In patients with a blastic plasmacytoid dendritic cell neoplasm, a myeloid malignancy with high CD123 expression, SL-401 has led to clinical improvement [75]. To treat CD123-positive AML and MDS, SL-401 has also been used with azacitidine (AZA) or venetoclax/AZA. Three of the four previously untreated MDS patients and eight of the nine AML patients who had not received treatment before achieved CR. It is noteworthy that TP53 mutations were present in three responding MDS patients and two responding AML patients. When paired with venetoclax/AZA in CD123-positive R/R AML, pivekimab sunirine, another αCD123 antibody–drug combination that causes DNA alkylation, produced objective response rates (ORRs) of 51% with promising efficacy [76].
Using a mouse model that targeted both CD33 and CD123 via a bispecific conjugate, LSCs were eliminated through a T-cell-dependent mechanism both in vivo and in vitro [77]. This model suggests that AML NPM1mut is initiated by CD123+ LSCs [77].
5.3. The Immune Checkpoint Inhibitors—Antibodies That Bind Programmed Cell Death-1 (αPD-1) Protein and Its Ligand (αPD-L1)
Checkpoint inhibitors targeting the programmed cell death-1 (PD-1) protein and its ligand (PD-L1), known as the PDx axis, have successfully achieved responses in a number of tumor types, including hematopoietic malignancies (reviewed in [78]). However, responses in AML have shown fewer promising results, perhaps reflecting their lower mutation burden. This may explain why recent ex vivo studies may provide evidence that supports the use of immunogenic strategies for AML NPM1mut in the presence of an ICI.
A systematic review that compared 19 randomized clinical trials involving 11,379 patients with solid tumors including non-small cell lung cancer, renal cell carcinoma, and gastric urothelial carcinoma [79] showed that αPD-1 treatments (such as nivolumab and pembrolizumab) achieved better OS and PFS compared with αPD-L1 therapeutic antibodies, with no significant difference in safety profiles. The reason is thought to be that αPD-1 can bind PD-1 on T cells, blocking the binding of PD-1 to both PD-L1 and PD-L2 ligands on antigen-presenting cells (APC; cancer cells) at the same time. However the PD-L1 antibody can only bind PD-L1, so T cells may still be inhibited by the interaction between PD-1 and PD-L2, even when PD-L1 signaling is blocked (reviewed in [80]). The level of PD-L1 on APCs may affect the response of patients to αPD-L1 treatment, with PD-L1low/negative patients having a compensatory increase in PD-L2 levels, making the difference in the treatment’s efficacy between αPD-1 and αPD-L1 exacerbated.
Expression of CD34/CD38/CD274 surface markers for LPC/LSCs was evaluated in 20/20 NPM1mut/NPM1wt AML patients’ samples via flow cytometry analyses. The LSC fraction showed a higher level of PD-L1 expression than the non-LSC fraction. The influence of αPD-1 antibodies on these antigen-specific immune responses and the formation of stem-like colonies were assessed as well. It is noteworthy that high PD-L1 expression in NPM1mut patients was detected, especially in the leukemic progenitor compartment. This observation further supports the hypothesis that NPM1-directed immune responses might play an important role in tumor cell rejection, which tumor cells try to escape via the expression of PD-L1. The immunogenicity of neoantigens derived from NPM1mut cells with higher PD-L1 expression constitutes promising target structures for individualized immunotherapeutic approaches.
In addition, we have previously shown that CD8+-specific LAA immune responses against Preferentially expressed Antigen in Melanoma (PRAME), WT-1, RHAMM, or NPM1mut expressing LPCs/LSCs from AML patients with mutated or wild-type NPM1 were similar except for their response to NPM1mut epitopes which were only seen in samples from NPM1mut patients (vide supra). We also found that T cell-mediated anti-tumor responses from AML patients were enhanced by the presence of αPD-1 blocking antibodies [59]. Along with the expression of PD-1 on LSCs isolated from NPM1mut patients, this suggests that treatment with αPD-1 antibodies combined with immunotherapeutic vaccine approaches could represent new treatment options for this biologically distinct group of patients [59,81].
The immune-modulating drug lenalidomide is a synthetic compound derived from structural modifications of thalidomide, a drug which was banned in the 1960s because of teratogenicity. Lenalidomide was released to market in 2004 and has been used to treat adults with multiple myeloma, smoldering leukemia, and AML. It has been shown to activate T cells and NKT cells, increase NKT cell numbers, and inhibit the production of pro-inflammatory cytokines such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α by monocytes. It effectively stimulates anti-tumor immunity, including anti-inflammatory, anti-proliferative, pro-apoptotic, and anti-angiogenicity [82]. Lenalidomide has been shown to achieve a 30% response rate as a first-line treatment in older newly diagnosed AML patients with limited treatment options and a poor prognosis [83].
The effects of lenalidomide are distinct from CT, hypomethylating agents, or kinase inhibitors, making lenalidomide an attractive agent for use in AML treatment, including in combination with existing active agents. Combinations of immunotherapeutic approaches are believed to increase antigen-specific immune responses against leukemic cells, including LPC/LSCs. In this study, we used a combination of LAA peptides with ICIs, αPD-1 (nivolumab), and lenalidomide to enhance the killing of LSC/LPCs ex vivo [82]. We used primary cells from AML patients and observed the T cell responses of all patients in vitro. Results using the combination of the ICI αPD-1 and the immune modulatory drug lenalidomide showed enhanced killing of LPCs/LSCs. The effect was greatest against NPM1mut cells when the immunogenic epitope was derived from the mutated region of NPM1 [23]. These studies show that antigen-specific immune responses against leukemic cells as well as LPCs/LSCs are enhanced by combinations of immunotherapeutic approaches, especially when using a combination of LAA peptides, the αPD-1 antibody, and one further immunomodulating drug, providing an interesting opportunity to enhance the outcomes in future clinical studies.
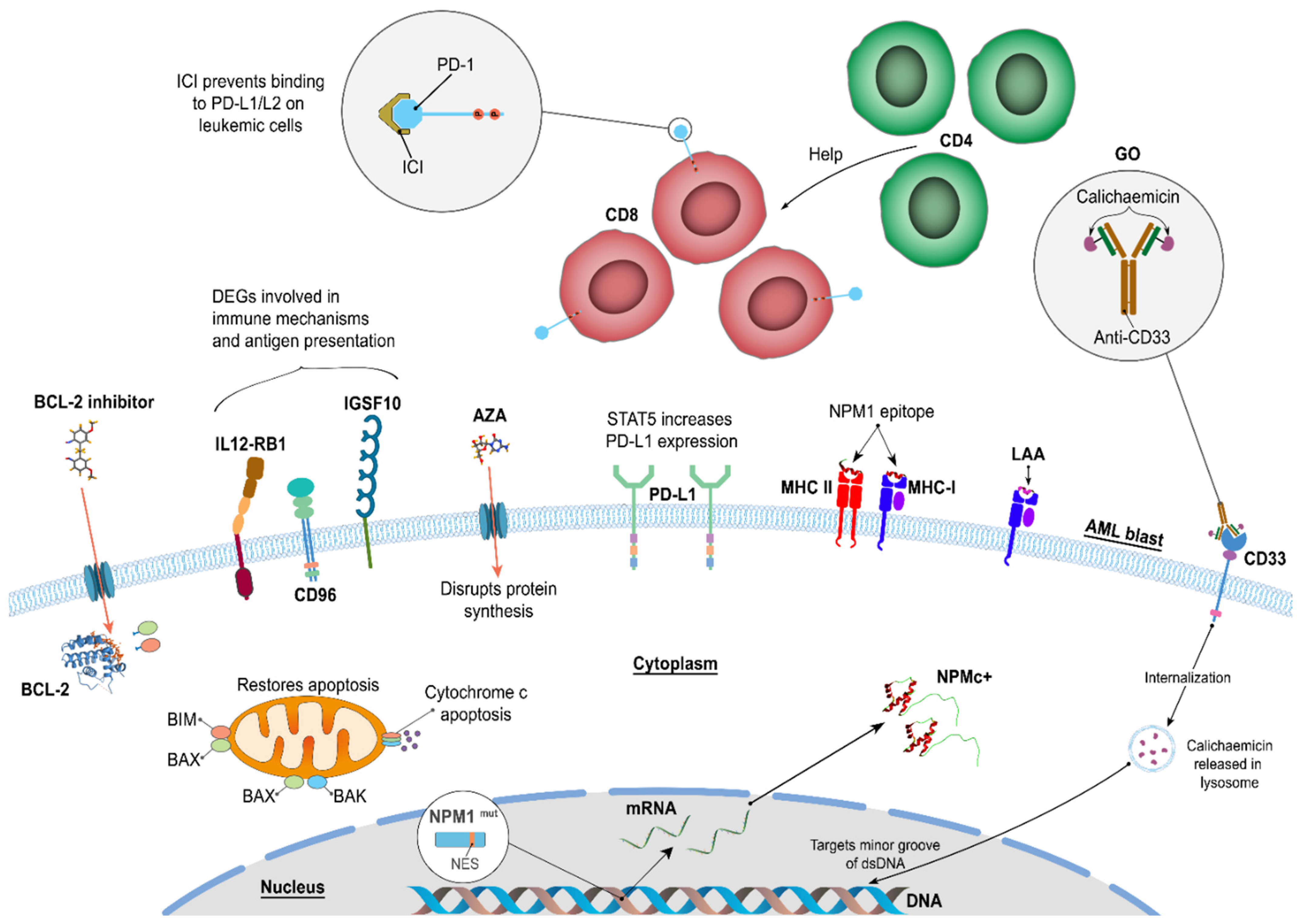
We recently examined whether all-trans retinoic acid, AZA, αCTLA4, or lenalidomide, in combination with αPD-1, to determine whether this could further improve the destruction of leukemic cells and also LPCs/LSCs from AML patients (Greiner et al, in preparation) (Figure 2). We identified which LAA (WT-1, PRAME, or NPM-1) generated the strongest immune response (as measured by colony-forming immunoassays) and using samples from 20 AML patients with more than 90% leukemic blasts. AZA, in combination with αPD-1, had a pronounced effect on T cell activation and inhibition of LPC/LSC growth.
Other strategies for immunotherapy that can be used in combination with PDx need to be considered. One approach is the signal transducer and activator of transcription 5 (STAT5), which promotes PD-L1 expression by facilitating histone lactylation and driving immunosuppression in AML and thus may benefit from PD-1/PD-L1 immunotherapy. ICIs could block the interactions of PD-1 with PD-L1 and thereby enhance the reactivity of CD8+ T cells in the microenvironment when co-culture with STAT5-activated AML cells occurs [84].
Figure 2.
Combinations of immunotherapeutic treatments can use complementary strategies to enhance anti-leukemic responses. We have shown that these combinations can increase antigen-specific immune responses against leukemic cells as well as LPCs/LSCs [82,85]. Image generated using information from the following articles [5,6,7,8,35,36,38,39,46,52,60,67,68,69,70,71,72,81,84,85,86,87,88,89,90]. Aver et al. found that AZA in combination with αPD-1 resulted in improved OS and an encouraging response rate, particularly in hypomethylating agent (HMA)-naïve and salvage-1 patients [87]. A randomized Phase 3 study and a randomized Phase 2 study of AZA with or without PD-1 inhibitor in first-line elderly AML patients, and a randomized trial of a PD-1 inhibitor for the eradication of MRD in high-risk AML in remission have started. Clinical and immune biomarker-enriched trials are likely to yield further improved outcomes with HMA in combination with ICI therapies in AML, but this remains to be seen as more study results are made available, especially for AML NPM1mut patients.
Figure 2.
Combinations of immunotherapeutic treatments can use complementary strategies to enhance anti-leukemic responses. We have shown that these combinations can increase antigen-specific immune responses against leukemic cells as well as LPCs/LSCs [82,85]. Image generated using information from the following articles [5,6,7,8,35,36,38,39,46,52,60,67,68,69,70,71,72,81,84,85,86,87,88,89,90]. Aver et al. found that AZA in combination with αPD-1 resulted in improved OS and an encouraging response rate, particularly in hypomethylating agent (HMA)-naïve and salvage-1 patients [87]. A randomized Phase 3 study and a randomized Phase 2 study of AZA with or without PD-1 inhibitor in first-line elderly AML patients, and a randomized trial of a PD-1 inhibitor for the eradication of MRD in high-risk AML in remission have started. Clinical and immune biomarker-enriched trials are likely to yield further improved outcomes with HMA in combination with ICI therapies in AML, but this remains to be seen as more study results are made available, especially for AML NPM1mut patients.
The results suggest that PD-1/PD-L1 in combination with NPM1mut-related approaches or other strategies such as STAT5 or HMA may have a notable impact on immunotherapeutic outcomes when used for the treatment of AML.
6. Venetoclax and Hypomethylating Agents
The aberration of DNA methylation is a common early event in the pathogenesis of AML, caused by genetic alterations in DNA methyltransferases (DNMTs) and Ten-Eleven-Translocation dioxygenases and leading to transcription dysregulation (reviewed in [88]). Elderly patients (≥65 years) with AML often respond poorly to induction chemotherapy [91]. This is mostly due to a higher frequency of adverse genomic features, increased resistance to treatments, partly caused by BCL-2 overexpression and also because of comorbidities, compromised organ function, and poor performance status. HMAs have been shown to upregulate silenced leukemia antigens and to promote the re-expression of endogenous retroviral elements. They exert inhibitory effects against cancer cells, which include stimulation of anti-tumor immunity in AML. In addition, the BCL-2 inhibitor venetoclax acts as a modulator of immunometabolism and potentiates adoptive NK cell immunotherapy. Both are not considered as standard immunotherapeutics, but their activity may make them appropriate for the stimulation of anti-tumor effects and circumvention of treatment resistance in older AML patients (>65 years) [17,92]. Recently, DiNardo et al. [39] showed that older treatment-naïve AML patients (>75 years) who were ineligible for intensive chemotherapy demonstrated a longer OS with increased remission rates when receiving AZA and venetoclax than with AZA alone. For newly diagnosed AML NPM1mut patients who are unfit and/or elderly, the standard of care is a combination of venetoclax and HMAs such as AZA, which inhibits DNMTs by its incorporation into DNA or low-dose cytarabine (LDAC). Post-remission maintenance therapy with AZA has been shown to prolong MRD negativity, and may delay or prevent a relapse and improve OS in elderly patients with AML, including NPM1-mutated AML, independent of the initial MRD status [93]. Oral AZA treatment extended the duration of MRD negativity by 6 months vs. a placebo. Oral AZA was recently approved in the United States, Canada, and the European Union for the treatment of adult patients with AML in first remission following induction chemotherapy who are not able to complete intensive curative therapy (e.g., SCT).
The FDA-approved molecule venetoclax has been shown to target the NPM1 apoptotic pathway by inhibiting B cell leukemia/lymphoma-2 (BCL-2) [39,89,90]. The increased sensitivity to venetoclax may be due to an NPM1 mutant-primed impairment in mitochondrial function [94]. Venetoclax-based regimens are especially beneficial for AML NPM1mut patients at first diagnosis and in the case of patients who are R/R to treatment. Regarding the effectiveness of venetoclax in AML NPM1mut, the human monocytic leukemia cell line THP-1, when transfected with a NPM1mut containing vector, exhibits increased sensitivity to chemotherapies through the reduction in NF-κB activity and BCL-2/BAX expression [95]. High BCL2 protein levels are associated with improved outcomes in patients with R/R AML or untreated AML, according to predictive indicators for venetoclax sensitivity [96]. However, not every patient has experienced this. A plausible rationale could be that a FLT3-ITD or TP53 deletion in AML NPM1mut patients leads to a mitochondrial malfunction. Moreover, as AML NPM1mut patients age, IDH1/2 mutations develop, which impacts how well venetoclax-based therapy can work [97].
Single-agent HMA or LDAC regimens are often better tolerated and have lower treatment-related mortality rates than conventional CT [98]. With a median survival of 6–10 months, response rates to HMAs alone are modest (10–50%) [98,99]. Despite its efficacy, relapses within 18 months are a major obstacle of HMA due to drug resistance. One suggested mechanism is that HMA interferes with DNA methylation and, in the long term, causes the failure of cells to undergo cell cycle arrest [100].
The combination of HMA and venetoclax is suggested to maximize the efficacy of treatment, evading the resistance created through the use of a single agent. In a Phase 3 clinical trial (NCT02993523) involving venetoclax plus AZA [39], 66.7% of AML NPM1mut patients experienced CR and incomplete remission, with the majority of the patients testing negative for detectable MRD. With a predicted two-year survival rate of 70%, the one-year survival rate for elderly individuals with AML NPM1mut surpassed 80%. Usually, one or two cycles were required to generate the desired response with a favorable safety profile [39]. Similarly, venetoclax plus LDAC achieved CR and an incomplete CR of 89% and 78%, respectively, in AML NPM1mut patients in the NCT02287233 and NCT03069352 trials [101,102]. The combination of venetoclax and HMA is considered to be advanced in AML treatment, and dose scheduling and further understanding of the mechanism of action and resistance remain to be explored [39].
7. Discussion
Our review has described treatments that are of particular relevance to AML NPM1mut patients. These patients are unique, with a tendency to be over 35 years of age, have a high white cell count, and to have FLT3-ITD, a normal karyotype, upregulated HOX and HOX-associated genes, and low to absent CD34+ expression on their blasts. Representing one-third of all AML patients, AML NPM1mut has become a separate entity in the WHO classification of AML, reflecting the patients’ ability to benefit from a targeted treatment strategy. Although the treatment of AML patients has changed little until recently [31], the AMLSG09-09 clinical trial showed that the addition of GO can extend relapse-free survival to a clinically relevant extent in CD33+ AML NPM1mut patients who achieve a CR [36,68]. It is notable that most of the diseased cells in AML NPM1mut patients are CD33+ and CD34−, even though LSCs are usually seen in the CD34+ and CD38− fraction from AML patients [102]. This suggests that if NPM1mut occurs in the LSC population, the LSCs are readily depleted by the immune system, or that NPM1mut tend to occur in non-LSCs which are more easily seen by the immune response, leading to their destruction and the associated improved patient survival.
This is reflected by the association between NPM1mut and improved survival in older patients (>70 years old) who have normal cytogenetics, independent of other molecular and clinical prognostic indicators, and in contrast to younger patients [103]. The haplotypes HLA-B*07, B*18, and B*40 are depleted in patients with NPM1mut, but when patients with NPM1mut express one of these haplotypes, OS is increased [47]. The association of NPM1mut with a better prognosis for patients (reviewed in [104]) may be explained by more robust immune responses against leukemic cells in general and the LSC fraction in particular. Indeed, Schneider et al. showed that AML NPM1mut patients harboring CD8+ responses against one of two predicted NPM1mut peptides had a better OS that those without [45].
Recently, combinations of hypomethylating agents and the Bcl-2 inhibitor venetoclax gave impressive results in older patients with AML NPM1mut compared with traditional standard-of-care regimens [105]. However, NPM1mut patients with adverse cytogenetics should be treated the same as NPM1WT patients with unfavorable cytogenetics who were linked to a lower 5-year OS rate [24].
Greiner et al. showed that CD4+ and CD8+ T cells from AML patients could respond to peptides from the mutated regions of NPM1 [44]. They found that AML NPM1mut patients with CTL responses against the NPM1mut peptide had better OS [47], and used LAAs as a specific method of stimulating T cell immune responses against LSCs and determining which combinations of immunotherapeutics could further enhance the killing of AML cells [82].
Elevated PD-L1 expression on AML NPM1mut cells (a ratio of v1/v2, as determined by qPCR) is associated with poorer survival [106], suggesting that anti-PD-1 treatment could block this signaling pathway, enhance T cells’ killing of leukemic cells and cause an associated improvement in patient survival. In vitro, we showed that the immune checkpoint inhibitor αPD-1 can enhance killing by LAA-stimulated CTLs [46,59]. Notably, the effect was greatest when T cells from NPM1mut patients were stimulated with the NPM1mut peptide, suggesting that anti-PD-1 antibodies, such as nivolumab, could be used to treat AML NPM1mut. This may reflect the features of AML NPM1mut that are especially associated with successful αPD-1 treatment of cancers including disease stability and a targetable mutation.
We recently examined whether αPD-1, all-trans retinoic acid (ATRA), AZA, αCTLA4 and/or lenalidomide were the best treatments to facilitate the destruction of autologous AML colonies in NPM1mut and NPM1WT patients [85]. The results were enhanced in patients with NPM1mut compared with NPM1WT, with αPD-1 and AZA providing the most effective T cell-mediated reduction in AML cells in CFI assays. This concurs with our understanding of PDx treatments and when they work best. When CTLs recognize LAAs, their response includes the production of inflammatory cytokines such as IFNγ and the upregulation of PD-1 on their surface. This prevents excessive T cell responses and limits the immune response. The tumor cells concurrently upregulate PD-L1, inhibiting T cell responses against them [107]. The blockage of this PD-1/PD-L1 interaction can lead to enhanced tumor killing and improved patient survival rates (reviewed in [80]). However, results on the treatment of AML have been mixed, reflecting the features of NPMWT that make AML a poor target for PDx therapies. These include rapidly progressing disease that generates a high tumor burden but a low mutational burden. However, PD-1 is regulated by DNA methylation [107], demonstrating a benefit for HMA and αPD-1 treatment in AML patients. The combination of venetoclax and HMAs has been shown to improve OS and CR compared with AZA alone in patients > 75 years of age with previously untreated AML who are ineligible for intensive chemotherapy [39].
It is clear that the development and progression of AML is closely linked to an impaired immune response. Leukemic cells manipulate the tumor microenvironment by creating a niche that directly promotes their survival and makes them resistant to immunotherapeutic strategies. Therefore, innovative strategies for immunotherapies need to be further developed and adapted to overcome the obstacles in the treatment of AML and especially AML NPM1mut [108]. However, AML NPM1mut offers several advantages over AML NPMWT, by virtue of their predominance of CD33+ diseased cells and an absence of CD34+, suggesting that the target population is not the more difficult to treat CD34+ LSC cells. The presence of NPM1mut provides a unique target for treatment, whose immunogenicity can be enhanced by treatment strategies that are likely to be enhanced by αPD-1, HMAs, and immune modulators.
8. Conclusions and Future Developments
In the hunt for additional NPM1mut peptide targets for future treatment strategies and, ideally, the identification of those that are naturally processed and presented, we could use mass spectrometry technologies that have been previously used to identify LAA-associated peptides processed and presented on MHC on CML and AML cells [107,109]. Similar strategies could be used to isolate peptides presented by MHC Class I and II molecules on CD34−CD33+ cells from AML NPM1mut patients, especially those associated with improved survival. This would provide naturally occurring epitope(s) for future studies that could be used to enhance NPM1mut-directed immune responses. It may even lend credence to the development of NPM1mut analog peptides, shown previously to stimulate enhanced immune responses against naturally occurring epitopes present on HLA-A*0201+ AML cells [54].
We have discussed the association between AML NPM1mut and the unique features associated with it. These include normal cytogenetics and enhanced survival in patients > 70 years of age. This phenomenon appears to be associated with the capacity of NPM1mut cells to stimulate a CD8+ T cell response against AML cells, leading to relapse-free survival in patients who achieve a CR. More recent studies have built on the standard-of-care treatment to show that the additional use of hypomethylating agents and Bcl-2 inhibitors can cause improved OS and CR in patients > 75 years of age who are not eligible for intensive chemotherapy. Future studies should examine other available treatment options and their efficacy in combination and the clinical trials that provide the proof of principle for a group of elderly AML patients who now have meaningful treatment options.
Author Contributions
Conceptualization, J.G.; investigation, J.G., M.G. and B.-a.G.; resources, writing—original draft preparation, all authors.; writing—review and editing, all authors; supervision, J.G. and B.-a.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
| alloHSCT | Allogeneic hematopoietic stem cell transplant | MDS | Myelodysplastic syndrome |
| AML | Acute myeloid leukemia | MLL | Mixed lineage leukemia |
| APC | Antigen-presenting cell | MRD | Minimal residual disease |
| NADP | Nicotinamide adenine dinucleotide phosphate | ||
| AZA | Azacitidine | NPM1WT | Wild-type Nucleophosmin 1 |
| BCL-2 | B cell leukemia/lymphoma-2 | mut | Mutated |
| CEBPA | CCAAT/enhancer-binding protein-α | OS | Overall survival |
| CR | Complete remission | PD-1 | Programmed cell death-1 |
| CTL | Cytotoxic T-lymphocyte | ||
| DLI | Donor lymphocyte infusion | PD-L1 | Programmed cell death 1 ligand 1 |
| ELN | European LeukemiaNet | ||
| FAB | French American British | PDx | PD-1/PD-L1 axis |
| FDA | Food and Drug Administration | PFS | Progression-free survival |
| FLT3-ITD | Fms-related receptor tyrosine kinase 3-internal tandem duplication | PRAME | Preferentially expressed antigen in melanoma |
| GO | Gemtuzumab–ozogamicin | RHAMM | Receptor for hyaluronan-mediated motility |
| HMA | Hypomethylating agents | R/R | Relapsed/refractory |
| ICI | Immune checkpoint inhibitor | STAT5 | Signal transducer and activator of transcription |
| IDH | Isocitrate dehydrogenase | TET2 | tet methylcytosine dioxygenase 2 |
| LAA LDAC | Leukemia associated antigens Low-dose cytarabine | WHO NK | World Health Organization Natural killer |
| LPC/LSC | leukemic progenitor/stem cell |
References
- Grisendi, S.; Mecucci, C.; Falini, B.; Pandolfi, P.P. Nucleophosmin and cancer. Nat. Rev. Cancer 2006, 6, 493–505. [Google Scholar] [CrossRef] [PubMed]
- Zarka, J.; Short, N.J.; Kanagal-Shamanna, R.; Issa, G.C. Nucleophosmin 1 Mutations in Acute Myeloid Leukemia. Genes 2020, 11, 649. [Google Scholar] [CrossRef] [PubMed]
- Adams, J.; Nassiri, M. Acute Promyelocytic Leukemia: A Review and Discussion of Variant Translocations. Arch. Pathol. Lab. Med. 2015, 139, 1308–1313. [Google Scholar] [CrossRef] [PubMed]
- Raimondi, S.C.; Dube, I.D.; Valentine, M.B.; Mirro, J., Jr.; Watt, H.J.; Larson, R.A.; Bitter, M.A.; Le Beau, M.M.; Rowley, J.D. Clinicopathologic manifestations and breakpoints of the t(3;5) in patients with acute nonlymphocytic leukemia. Leukemia 1989, 3, 42–47. [Google Scholar] [PubMed]
- Falini, B.; Mecucci, C.; Tiacci, E.; Alcalay, M.; Rosati, R.; Pasqualucci, L.; La Starza, R.; Diverio, D.; Colombo, E.; Santucci, A. Cytoplasmic nucleophosmin in acute myelogenous leukemia with a normal karyotype. N. Engl. J. Med. 2005, 352, 254–266. [Google Scholar] [CrossRef]
- Dumbar, T.S.; Gentry, G.A.; Olson, M.O. Interaction of nucleolar phosphoprotein B23 with nucleic acids. Biochemistry 1989, 28, 9495–9501. [Google Scholar] [CrossRef]
- Cordell, J.L.; Pulford, K.A.; Bigerna, B.; Roncador, G.; Banham, A.; Colombo, E.; Pelicci, P.G.; Mason, D.Y.; Falini, B. Detection of normal and chimeric nucleophosmin in human cells. Blood 1999, 93, 632–642. [Google Scholar] [CrossRef]
- Borer, R.A.; Lehner, C.F.; Eppenberger, H.M.; Nigg, E.A. Major nucleolar proteins shuttle between nucleus and cytoplasm. Cell 1989, 56, 379–390. [Google Scholar] [CrossRef]
- Falini, B.; Martelli, M.P.; Bolli, N.; Bonasso, R.; Ghia, E.; Pallotta, M.T.; Diverio, D.; Nicoletti, I.; Pacini, R.; Tabarrini, A.; et al. Immunohistochemistry predicts nucleophosmin (NPM) mutations in acute myeloid leukemia. Blood 2006, 108, 1999–2005. [Google Scholar] [CrossRef]
- Dillon, R.; Hills, R.; Freeman, S.; Potter, N.; Jovanovic, J.; Ivey, A.; Kanda, A.S.; Runglall, M.; Foot, N.; Valganon, M.; et al. Molecular MRD status and outcome after transplantation in NPM1-mutated AML. Blood 2020, 135, 680–688. [Google Scholar] [CrossRef]
- Cela, I.; Di Matteo, A.; Federici, L. Nucleophosmin in Its Interaction with Ligands. Int. J. Mol. Sci. 2020, 21, 4885. [Google Scholar] [CrossRef] [PubMed]
- Dohner, H.; Wei, A.H.; Appelbaum, F.R.; Craddock, C.; DiNardo, C.D.; Dombret, H.; Ebert, B.L.; Fenaux, P.; Godley, L.A.; Hasserjian, R.P.; et al. Diagnosis and management of AML in adults: 2022 recommendations from an international expert panel on behalf of the ELN. Blood 2022, 140, 1345–1377. [Google Scholar] [CrossRef] [PubMed]
- Huber, S.; Baer, C.; Hutter, S.; Dicker, F.; Fuhrmann, I.; Meggendorfer, M.; Pohlkamp, C.; Kern, W.; Haferlach, T.; Haferlach, C.; et al. Risk assessment according to IPSS-M is superior to AML ELN risk classification in MDS/AML overlap patients defined by ICC. Leukemia 2023, 37, 2138–2141. [Google Scholar] [CrossRef] [PubMed]
- Shimony, S.; Stahl, M.; Stone, R.M. Acute myeloid leukemia: 2023 update on diagnosis, risk-stratification, and management. Am. J. Hematol. 2023, 98, 502–526. [Google Scholar] [CrossRef] [PubMed]
- Verhaak, R.G.; Goudswaard, C.S.; van Putten, W.; Bijl, M.A.; Sanders, M.A.; Hugens, W.; Uitterlinden, A.G.; Erpelinck, C.A.; Delwel, R.; Lowenberg, B.; et al. Mutations in nucleophosmin (NPM1) in acute myeloid leukemia (AML): Association with other gene abnormalities and previously established gene expression signatures and their favorable prognostic significance. Blood 2005, 106, 3747–3754. [Google Scholar] [CrossRef]
- Falini, B.; Martelli, M.P.; Bolli, N.; Sportoletti, P.; Liso, A.; Tiacci, E.; Haferlach, T. Acute myeloid leukemia with mutated nucleophosmin (NPM1): Is it a distinct entity? Blood 2011, 117, 1109–1120. [Google Scholar] [CrossRef]
- Kantarjian, H.M.; Kadia, T.M.; DiNardo, C.D.; Welch, M.A.; Ravandi, F. Acute myeloid leukemia: Treatment and research outlook for 2021 and the MD Anderson approach. Cancer 2021, 127, 1186–1207. [Google Scholar] [CrossRef]
- Papaemmanuil, E.; Gerstung, M.; Bullinger, L.; Gaidzik, V.I.; Paschka, P.; Roberts, N.D.; Potter, N.E.; Heuser, M.; Thol, F.; Bolli, N.; et al. Genomic Classification and Prognosis in Acute Myeloid Leukemia. N. Engl. J. Med. 2016, 374, 2209–2221. [Google Scholar] [CrossRef]
- Borrow, J.; Dyer, S.A.; Akiki, S.; Griffiths, M.J. Molecular roulette: Nucleophosmin mutations in AML are orchestrated through N-nucleotide addition by TdT. Blood 2019, 134, 2291–2303. [Google Scholar] [CrossRef]
- Heath, E.M.; Chan, S.M.; Minden, M.D.; Murphy, T.; Shlush, L.I.; Schimmer, A.D. Biological and clinical consequences of NPM1 mutations in AML. Leukemia 2017, 31, 798–807. [Google Scholar] [CrossRef]
- Juliusson, G.; Jadersten, M.; Deneberg, S.; Lehmann, S.; Mollgard, L.; Wennstrom, L.; Antunovic, P.; Cammenga, J.; Lorenz, F.; Olander, E.; et al. The prognostic impact of FLT3-ITD and NPM1 mutation in adult AML is age-dependent in the population-based setting. Blood Adv. 2020, 4, 1094–1101. [Google Scholar] [CrossRef] [PubMed]
- Ostronoff, F.; Othus, M.; Lazenby, M.; Estey, E.; Appelbaum, F.R.; Evans, A.; Godwin, J.; Gilkes, A.; Kopecky, K.J.; Burnett, A.; et al. Prognostic significance of NPM1 mutations in the absence of FLT3-internal tandem duplication in older patients with acute myeloid leukemia: A SWOG and UK National Cancer Research Institute/Medical Research Council report. J. Clin. Oncol. 2015, 33, 1157–1164. [Google Scholar] [CrossRef] [PubMed]
- Schlenk, R.F.; Döhner, K.; Krauter, J.; Fröhling, S.; Corbacioglu, A.; Bullinger, L.; Habdank, M.; Späth, D.; Morgan, M.; Benner, A. Mutations and treatment outcome in cytogenetically normal acute myeloid leukemia. N. Engl. J. Med. 2008, 358, 1909–1918. [Google Scholar] [CrossRef] [PubMed]
- Angenendt, L.; Rollig, C.; Montesinos, P.; Ravandi, F.; Juliusson, G.; Recher, C.; Itzykson, R.; Racil, Z.; Wei, A.H.; Schliemann, C. Revisiting coexisting chromosomal abnormalities in NPM1-mutated AML in light of the revised ELN 2022 classification. Blood 2023, 141, 433–435. [Google Scholar] [CrossRef]
- Shiah, H.S.; Kuo, Y.Y.; Tang, J.L.; Huang, S.Y.; Yao, M.; Tsay, W.; Chen, Y.C.; Wang, C.H.; Shen, M.C.; Lin, D.T.; et al. Clinical and biological implications of partial tandem duplication of the MLL gene in acute myeloid leukemia without chromosomal abnormalities at 11q23. Leukemia 2002, 16, 196–202. [Google Scholar] [CrossRef]
- Dohner, K.; Tobis, K.; Ulrich, R.; Frohling, S.; Benner, A.; Schlenk, R.F.; Dohner, H. Prognostic significance of partial tandem duplications of the MLL gene in adult patients 16 to 60 years old with acute myeloid leukemia and normal cytogenetics: A study of the Acute Myeloid Leukemia Study Group Ulm. J. Clin. Oncol. 2002, 20, 3254–3261. [Google Scholar] [CrossRef]
- Barjesteh van Waalwijk van Doorn-Khosrovani, S.; Erpelinck, C.; van Putten, W.L.; Valk, P.J.; van der Poel-van de Luytgaarde, S.; Hack, R.; Slater, R.; Smit, E.M.; Beverloo, H.B.; Verhoef, G.; et al. High EVI1 expression predicts poor survival in acute myeloid leukemia: A study of 319 de novo AML patients. Blood 2003, 101, 837–845. [Google Scholar] [CrossRef]
- Gregory, T.K.; Wald, D.; Chen, Y.; Vermaat, J.M.; Xiong, Y.; Tse, W. Molecular prognostic markers for adult acute myeloid leukemia with normal cytogenetics. J. Hematol. Oncol. 2009, 2, 23. [Google Scholar] [CrossRef]
- Angenendt, L.; Rollig, C.; Montesinos, P.; Martinez-Cuadron, D.; Barragan, E.; Garcia, R.; Botella, C.; Martinez, P.; Ravandi, F.; Kadia, T.; et al. Chromosomal Abnormalities and Prognosis in NPM1-Mutated Acute Myeloid Leukemia: A Pooled Analysis of Individual Patient Data From Nine International Cohorts. J. Clin. Oncol. 2019, 37, 2632–2642. [Google Scholar] [CrossRef]
- Dohner, K.; Paschka, P. Intermediate-risk acute myeloid leukemia therapy: Current and future. Hematol. Am. Soc. Hematol. Educ. Program 2014, 2014, 34–43. [Google Scholar] [CrossRef]
- Dohner, H.; Estey, E.; Grimwade, D.; Amadori, S.; Appelbaum, F.R.; Buchner, T.; Dombret, H.; Ebert, B.L.; Fenaux, P.; Larson, R.A.; et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood 2017, 129, 424–447. [Google Scholar] [CrossRef] [PubMed]
- Eckardt, J.N.; Bill, M.; Rausch, C.; Metzeler, K.; Spiekermann, K.; Stasik, S.; Sauer, T.; Scholl, S.; Hochhaus, A.; Crysandt, M.; et al. Secondary-type mutations do not impact outcome in NPM1-mutated acute myeloid leukemia—Implications for the European LeukemiaNet risk classification. Leukemia 2023, 37, 2282–2285. [Google Scholar] [CrossRef] [PubMed]
- Preudhomme, C.; Sagot, C.; Boissel, N.; Cayuela, J.M.; Tigaud, I.; de Botton, S.; Thomas, X.; Raffoux, E.; Lamandin, C.; Castaigne, S.; et al. Favorable prognostic significance of CEBPA mutations in patients with de novo acute myeloid leukemia: A study from the Acute Leukemia French Association (ALFA). Blood 2002, 100, 2717–2723. [Google Scholar] [CrossRef] [PubMed]
- Barjesteh van Waalwijk van Doorn-Khosrovani, S.; Erpelinck, C.; Meijer, J.; van Oosterhoud, S.; van Putten, W.L.; Valk, P.J.; Berna Beverloo, H.; Tenen, D.G.; Lowenberg, B.; Delwel, R. Biallelic mutations in the CEBPA gene and low CEBPA expression levels as prognostic markers in intermediate-risk AML. Hematol. J. 2003, 4, 31–40. [Google Scholar] [CrossRef] [PubMed]
- Kapp-Schwoerer, S.; Weber, D.; Corbacioglu, A.; Gaidzik, V.I.; Paschka, P.; Kronke, J.; Theis, F.; Rucker, F.G.; Teleanu, M.V.; Panina, E.; et al. Impact of gemtuzumab ozogamicin on MRD and relapse risk in patients with NPM1-mutated AML: Results from the AMLSG 09-09 trial. Blood 2020, 136, 3041–3050. [Google Scholar] [CrossRef] [PubMed]
- Schlenk, R.F.; Paschka, P.; Krzykalla, J.; Weber, D.; Kapp-Schwoerer, S.; Gaidzik, V.I.; Leis, C.; Fiedler, W.; Kindler, T.; Schroeder, T.; et al. Gemtuzumab Ozogamicin in NPM1-Mutated Acute Myeloid Leukemia: Early Results From the Prospective Randomized AMLSG 09-09 Phase III Study. J. Clin. Oncol. 2020, 38, 623–632. [Google Scholar] [CrossRef]
- Hofmann, S.; Götz, M.; Schneider, V.; Guillaume, P.; Bunjes, D.; Döhner, H.; Wiesneth, M.; Greiner, J. Donor lymphocyte infusion induces polyspecific CD8+ T-cell responses with concurrent molecular remission in acute myeloid leukemia with NPM1 mutation. J. Clin. Oncol. 2013, 31, e44–e47. [Google Scholar] [CrossRef]
- Jäger, P.; Rautenberg, C.; Kaivers, J.; Kasprzak, A.; Geyh, S.; Baermann, B.-N.; Haas, R.; Germing, U.; Schroeder, T.; Kobbe, G. Allogeneic hematopoietic stem cell transplantation and pre-transplant strategies in patients with NPM1-mutated acute myeloid leukemia: A single center experience. Sci. Rep. 2023, 13, 10774. [Google Scholar] [CrossRef]
- DiNardo, C.D.; Jonas, B.A.; Pullarkat, V.; Thirman, M.J.; Garcia, J.S.; Wei, A.H.; Konopleva, M.; Döhner, H.; Letai, A.; Fenaux, P. Azacitidine and venetoclax in previously untreated acute myeloid leukemia. N. Engl. J. Med. 2020, 383, 617–629. [Google Scholar] [CrossRef]
- Forghieri, F.; Riva, G.; Lagreca, I.; Barozzi, P.; Bettelli, F.; Paolini, A.; Nasillo, V.; Lusenti, B.; Pioli, V.; Giusti, D.; et al. Neoantigen-Specific T-Cell Immune Responses: The Paradigm of NPM1-Mutated Acute Myeloid Leukemia. Int. J. Mol. Sci. 2021, 22, 9159. [Google Scholar] [CrossRef]
- Heuser, M.; Freeman, S.D.; Ossenkoppele, G.J.; Buccisano, F.; Hourigan, C.S.; Ngai, L.L.; Tettero, J.M.; Bachas, C.; Baer, C.; Bene, M.C.; et al. 2021 Update on MRD in acute myeloid leukemia: A consensus document from the European LeukemiaNet MRD Working Party. Blood 2021, 138, 2753–2767. [Google Scholar] [CrossRef] [PubMed]
- Dempke, W.C.M.; Desole, M.; Chiusolo, P.; Sica, S.; Schmidt-Hieber, M. Targeting the undruggable: Menin inhibitors ante portas. J. Cancer Res. Clin. Oncol. 2023, 149, 9451–9459. [Google Scholar] [CrossRef] [PubMed]
- Liso, A.; Colau, D.; Benmaamar, R.; De Groot, A.; Martin, W.; Benedetti, R.; Specchia, G.; Martelli, M.P.; Coulie, P.; Falini, B. Nucleophosmin leukaemic mutants contain C-terminus peptides that bind HLA class I molecules. Leukemia 2008, 22, 424–426. [Google Scholar] [CrossRef] [PubMed]
- Greiner, J.; Ono, Y.; Hofmann, S.; Schmitt, A.; Mehring, E.; Götz, M.; Guillaume, P.; Döhner, K.; Mytilineos, J.; Döhner, H. Mutated regions of nucleophosmin 1 elicit both CD4+ and CD8+ T-cell responses in patients with acute myeloid leukemia. Blood J. Am. Soc. Hematol. 2012, 120, 1282–1289. [Google Scholar] [CrossRef] [PubMed]
- Greiner, J.; Schneider, V.; Schmitt, M.; Götz, M.; Döhner, K.; Wiesneth, M.; Döhner, H.; Hofmann, S. Immune responses against the mutated region of cytoplasmatic NPM1 might contribute to the favorable clinical outcome of AML patients with NPM1 mutations (NPM1mut). Blood 2013, 122, 1087–1088. [Google Scholar] [CrossRef] [PubMed]
- Schneider, V.; Zhang, L.; Bullinger, L.; Rojewski, M.; Hofmann, S.; Wiesneth, M.; Schrezenmeier, H.; Götz, M.; Botzenhardt, U.; Barth, T.F.E.; et al. Leukemic stem cells of acute myeloid leukemia patients carrying NPM1 mutation are candidates for targeted immunotherapy. Leukemia 2014, 28, 1759–1762. [Google Scholar] [CrossRef]
- Kuzelova, K.; Brodska, B.; Fuchs, O.; Dobrovolna, M.; Soukup, P.; Cetkovsky, P. Altered HLA Class I Profile Associated with Type A/D Nucleophosmin Mutation Points to Possible Anti-Nucleophosmin Immune Response in Acute Myeloid Leukemia. PLoS ONE 2015, 10, e0127637. [Google Scholar] [CrossRef]
- van der Lee, D.I.; Reijmers, R.M.; Honders, M.W.; Hagedoorn, R.S.; de Jong, R.C.; Kester, M.G.; van der Steen, D.M.; de Ru, A.H.; Kweekel, C.; Bijen, H.M.; et al. Mutated nucleophosmin 1 as immunotherapy target in acute myeloid leukemia. J. Clin. Investig. 2019, 129, 774–785. [Google Scholar] [CrossRef]
- Narayan, R.; Olsson, N.; Wagar, L.E.; Medeiros, B.C.; Meyer, E.; Czerwinski, D.; Khodadoust, M.S.; Zhang, L.; Schultz, L.; Davis, M.M.; et al. Acute myeloid leukemia immunopeptidome reveals HLA presentation of mutated nucleophosmin. PLoS ONE 2019, 14, e0219547. [Google Scholar] [CrossRef]
- Morris, V.S.; Ghazi, H.; Fletcher, D.M.; Guinn, B.A. A Direct Comparison, and Prioritisation, of the Immunotherapeutic Targets Expressed by Adult and Paediatric Acute Myeloid Leukaemia Cells: A Systematic Review and Meta-Analysis. Int. J. Mol. Sci. 2023, 24, 9667. [Google Scholar] [CrossRef]
- Adams, S.P.; Sahota, S.S.; Mijovic, A.; Czepulkowski, B.; Padua, R.A.; Mufti, G.J.; Guinn, B.A. Frequent expression of HAGE in presentation chronic myeloid leukaemias. Leukemia 2002, 16, 2238–2242. [Google Scholar] [CrossRef] [PubMed]
- Guinn, B.A.; Bland, E.A.; Lodi, U.; Liggins, A.P.; Tobal, K.; Petters, S.; Wells, J.W.; Banham, A.H.; Mufti, G.J. Humoral detection of leukaemia-associated antigens in presentation acute myeloid leukaemia. Biochem. Biophys. Res. Commun. 2005, 335, 1293–1304. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.E.; Bonney, S.A.; Lee, C.; Publicover, A.; Khan, G.; Smits, E.L.; Sigurdardottir, D.; Arno, M.; Li, D.; Mills, K.I.; et al. Application of the pMHC Array to Characterise Tumour Antigen Specific T Cell Populations in Leukaemia Patients at Disease Diagnosis. PLoS ONE 2015, 10, e0140483. [Google Scholar] [CrossRef] [PubMed]
- Hardwick, N.; Buchan, S.; Ingram, W.; Khan, G.; Vittes, G.; Rice, J.; Pulford, K.; Mufti, G.; Stevenson, F.; Guinn, B.A. An analogue peptide from the Cancer/Testis antigen PASD1 induces CD8+ T cell responses against naturally processed peptide. Cancer Immun. 2013, 13, 16. [Google Scholar] [PubMed]
- Almshayakhchi, R.; Nagarajan, D.; Vadakekolathu, J.; Guinn, B.A.; Reeder, S.; Brentville, V.; Metheringham, R.; Pockley, A.G.; Durrant, L.; McArdle, S. A Novel HAGE/WT1-ImmunoBody((R)) Vaccine Combination Enhances Anti-Tumour Responses When Compared to Either Vaccine Alone. Front. Oncol. 2021, 11, 636977. [Google Scholar] [CrossRef]
- Schmitt, M.; Schmitt, A.; Rojewski, M.T.; Chen, J.; Giannopoulos, K.; Fei, F.; Yu, Y.; Gotz, M.; Heyduk, M.; Ritter, G.; et al. RHAMM-R3 peptide vaccination in patients with acute myeloid leukemia, myelodysplastic syndrome, and multiple myeloma elicits immunologic and clinical responses. Blood 2008, 111, 1357–1365. [Google Scholar] [CrossRef]
- Qazilbash, M.H.; Wieder, E.; Thall, P.F.; Wang, X.; Rios, R.; Lu, S.; Kanodia, S.; Ruisaard, K.E.; Giralt, S.A.; Estey, E.H.; et al. PR1 peptide vaccine induces specific immunity with clinical responses in myeloid malignancies. Leukemia 2017, 31, 697–704. [Google Scholar] [CrossRef]
- Brayer, J.; Lancet, J.E.; Powers, J.; List, A.; Balducci, L.; Komrokji, R.; Pinilla-Ibarz, J. WT1 vaccination in AML and MDS: A pilot trial with synthetic analog peptides. Am. J. Hematol. 2015, 90, 602–607. [Google Scholar] [CrossRef]
- Greiner, J.; Goetz, M.; Schuler, P.J.; Bulach, C.; Hofmann, S.; Schrezenmeier, H.; Dhner, H.; Schneider, V.; Guinn, B.A. Enhanced stimulation of antigen-specific immune responses against nucleophosmin 1 mutated acute myeloid leukaemia by an anti-programmed death 1 antibody. Br. J. Haematol. 2022, 198, 866–874. [Google Scholar] [CrossRef]
- Ehninger, A.; Kramer, M.; Röllig, C.; Thiede, C.; Bornhäuser, M.; Von Bonin, M.; Wermke, M.; Feldmann, A.; Bachmann, M.; Ehninger, G. Distribution and levels of cell surface expression of CD33 and CD123 in acute myeloid leukemia. Blood Cancer J. 2014, 4, e218. [Google Scholar] [CrossRef]
- Caron, P.C.; Dumont, L.; Scheinberg, D.A. Supersaturating infusional humanized anti-CD33 monoclonal antibody HuM195 in myelogenous leukemia. Clin. Cancer Res. 1998, 4, 1421–1428. [Google Scholar] [PubMed]
- Raza, A.; Jurcic, J.G.; Roboz, G.J.; Maris, M.; Stephenson, J.J.; Wood, B.L.; Feldman, E.J.; Galili, N.; Grove, L.E.; Drachman, J.G.; et al. Complete remissions observed in acute myeloid leukemia following prolonged exposure to lintuzumab: A phase 1 trial. Leuk. Lymphoma 2009, 50, 1336–1344. [Google Scholar] [CrossRef] [PubMed]
- Feldman, E.; Kalaycio, M.; Weiner, G.; Frankel, S.; Schulman, P.; Schwartzberg, L.; Jurcic, J.; Velez-Garcia, E.; Seiter, K.; Scheinberg, D.; et al. Treatment of relapsed or refractory acute myeloid leukemia with humanized anti-CD33 monoclonal antibody HuM195. Leukemia 2003, 17, 314–318. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Laszlo, G.S.; Estey, E.H.; Walter, R.B. The past and future of CD33 as therapeutic target in acute myeloid leukemia. Blood Rev. 2014, 28, 143–153. [Google Scholar] [CrossRef] [PubMed]
- Gill, S.I. How close are we to CAR T-cell therapy for AML? Best Pract. Res. Clin. Haematol. 2019, 32, 101104. [Google Scholar] [CrossRef]
- Lambert, J.; Pautas, C.; Terre, C.; Raffoux, E.; Turlure, P.; Caillot, D.; Legrand, O.; Thomas, X.; Gardin, C.; Gogat-Marchant, K.; et al. Gemtuzumab ozogamicin for de novo acute myeloid leukemia: Final efficacy and safety updates from the open-label, phase III ALFA-0701 trial. Haematologica 2019, 104, 113–119. [Google Scholar] [CrossRef]
- Hills, R.K.; Castaigne, S.; Appelbaum, F.R.; Delaunay, J.; Petersdorf, S.; Othus, M.; Estey, E.H.; Dombret, H.; Chevret, S.; Ifrah, N.; et al. Addition of gemtuzumab ozogamicin to induction chemotherapy in adult patients with acute myeloid leukaemia: A meta-analysis of individual patient data from randomised controlled trials. Lancet Oncol. 2014, 15, 986–996. [Google Scholar] [CrossRef]
- Dohner, H.; Weber, D.; Krzykalla, J.; Fiedler, W.; Kuhn, M.W.M.; Schroeder, T.; Mayer, K.; Lubbert, M.; Wattad, M.; Gotze, K.; et al. Intensive chemotherapy with or without gemtuzumab ozogamicin in patients with NPM1-mutated acute myeloid leukaemia (AMLSG 09-09): A randomised, open-label, multicentre, phase 3 trial. Lancet Haematol. 2023, 10, e495–e509. [Google Scholar] [CrossRef]
- Thol, F.; Schlenk, R.F. Gemtuzumab ozogamicin in acute myeloid leukemia revisited. Expert Opin. Biol. Ther. 2014, 14, 1185–1195. [Google Scholar] [CrossRef]
- O’Hear, C.; Inaba, H.; Pounds, S.; Shi, L.; Dahl, G.; Bowman, W.P.; Taub, J.W.; Pui, C.H.; Ribeiro, R.C.; Coustan-Smith, E. Gemtuzumab ozogamicin can reduce minimal residual disease in patients with childhood acute myeloid leukemia. Cancer 2013, 119, 4036–4043. [Google Scholar] [CrossRef]
- Castaigne, S.; Pautas, C.; Terré, C.; Raffoux, E.; Bordessoule, D.; Bastie, J.-N.; Legrand, O.; Thomas, X.; Turlure, P.; Reman, O. Effect of gemtuzumab ozogamicin on survival of adult patients with de-novo acute myeloid leukaemia (ALFA-0701): A randomised, open-label, phase 3 study. Lancet 2012, 379, 1508–1516. [Google Scholar] [CrossRef] [PubMed]
- Perriello, V.M.; Gionfriddo, I.; Rossi, R.; Milano, F.; Mezzasoma, F.; Marra, A.; Spinelli, O.; Rambaldi, A.; Annibali, O.; Avvisati, G.; et al. CD123 Is Consistently Expressed on NPM1-Mutated AML Cells. Cancers 2021, 13, 496. [Google Scholar] [CrossRef] [PubMed]
- He, S.Z.; Busfield, S.; Ritchie, D.S.; Hertzberg, M.S.; Durrant, S.; Lewis, I.D.; Marlton, P.; McLachlan, A.J.; Kerridge, I.; Bradstock, K.F. A Phase 1 study of the safety, pharmacokinetics and anti-leukemic activity of the anti-CD123 monoclonal antibody CSL360 in relapsed, refractory or high-risk acute myeloid leukemia. Leuk. Lymphoma 2015, 56, 1406–1415. [Google Scholar] [CrossRef] [PubMed]
- Pemmaraju, N.; Lane, A.A.; Sweet, K.L.; Stein, A.S.; Vasu, S.; Blum, W.; Rizzieri, D.A.; Wang, E.S.; Duvic, M.; Sloan, J.M. Tagraxofusp in blastic plasmacytoid dendritic-cell neoplasm. N. Engl. J. Med. 2019, 380, 1628–1637. [Google Scholar] [CrossRef] [PubMed]
- Daver, N.; Montesinos, P.; Aribi, A.; Marconi, G.; Altman, J.K.; Wang, E.S.; Roboz, G.J.; Burke, P.W.; Gaidano, G.; Walter, R.B.; et al. Broad Activity for the Pivekimab Sunirine (PVEK, IMGN632), Azacitidine, and Venetoclax Triplet in High-Risk Patients with Relapsed/Refractory Acute Myeloid Leukemia (AML). Blood 2022, 140, 145–149. [Google Scholar] [CrossRef]
- Kaur, M.; Drake, A.C.; Hu, G.; Rudnick, S.; Chen, Q.; Phennicie, R.; Attar, R.; Nemeth, J.; Gaudet, F.; Chen, J. Induction and therapeutic targeting of human NPM1c+ myeloid leukemia in the presence of autologous immune system in mice. J. Immunol. 2019, 202, 1885–1894. [Google Scholar] [CrossRef]
- Chen, Y.; Wang, J.; Zhang, F.; Liu, P. A perspective of immunotherapy for acute myeloid leukemia: Current advances and challenges. Front. Pharmacol. 2023, 14, 1151032. [Google Scholar] [CrossRef]
- Duan, J.; Cui, L.; Zhao, X.; Bai, H.; Cai, S.; Wang, G.; Zhao, Z.; Zhao, J.; Chen, S.; Song, J.; et al. Use of Immunotherapy With Programmed Cell Death 1 vs Programmed Cell Death Ligand 1 Inhibitors in Patients With Cancer: A Systematic Review and Meta-analysis. JAMA Oncol. 2020, 6, 375–384. [Google Scholar] [CrossRef]
- Chen, Y.; Pei, Y.; Luo, J.; Huang, Z.; Yu, J.; Meng, X. Looking for the Optimal PD-1/PD-L1 Inhibitor in Cancer Treatment: A Comparison in Basic Structure, Function, and Clinical Practice. Front. Immunol. 2020, 11, 1088. [Google Scholar] [CrossRef]
- Greiner, J.; Hofmann, S.; Schmitt, M.; Gotz, M.; Wiesneth, M.; Schrezenmeier, H.; Bunjes, D.; Dohner, H.; Bullinger, L. Acute myeloid leukemia with mutated nucleophosmin 1: An immunogenic acute myeloid leukemia subtype and potential candidate for immune checkpoint inhibition. Haematologica 2017, 102, e499–e501. [Google Scholar] [CrossRef]
- Guinn, B.A.; Schuler, P.J.; Schrezenmeier, H.; Hofmann, S.; Weiss, J.; Bulach, C.; Gotz, M.; Greiner, J. A Combination of the Immunotherapeutic Drug Anti-Programmed Death 1 with Lenalidomide Enhances Specific T Cell Immune Responses against Acute Myeloid Leukemia Cells. Int. J. Mol. Sci. 2023, 24, 9285. [Google Scholar] [CrossRef] [PubMed]
- Fehniger, T.A.; Uy, G.L.; Trinkaus, K.; Nelson, A.D.; Demland, J.; Abboud, C.N.; Cashen, A.F.; Stockerl-Goldstein, K.E.; Westervelt, P.; DiPersio, J.F.; et al. A phase 2 study of high-dose lenalidomide as initial therapy for older patients with acute myeloid leukemia. Blood 2011, 117, 1828–1833. [Google Scholar] [CrossRef]
- Huang, Z.W.; Zhang, X.N.; Zhang, L.; Liu, L.L.; Zhang, J.W.; Sun, Y.X.; Xu, J.Q.; Liu, Q.; Long, Z.J. STAT5 promotes PD-L1 expression by facilitating histone lactylation to drive immunosuppression in acute myeloid leukemia. Signal Transduct. Target. Ther. 2023, 8, 391. [Google Scholar] [CrossRef]
- Greiner, J.; Schuler, P.J.; Schrezenmeier, H.; Weiss, J.; Bulach, C.; Goetz, M.; Guinn, B. Combinations of Different Immunotherapeutics Enhance Specific T Cell Immune Responses Against Leukemic Cells, as well as Leukemic Progenitor and Stem Cells in Acute Myeloid Leukemia In Preparation.
- Daver, N.; Garcia-Manero, G.; Basu, S.; Boddu, P.C.; Alfayez, M.; Cortes, J.E.; Konopleva, M.; Ravandi-Kashani, F.; Jabbour, E.; Kadia, T.; et al. Efficacy, Safety, and Biomarkers of Response to Azacitidine and Nivolumab in Relapsed/Refractory Acute Myeloid Leukemia: A Nonrandomized, Open-Label, Phase II Study. Cancer Discov. 2019, 9, 370–383. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Wong, M.P.M.; Ng, R.K. Aberrant DNA Methylation in Acute Myeloid Leukemia and Its Clinical Implications. Int. J. Mol. Sci. 2019, 20, 4576. [Google Scholar] [CrossRef]
- Chin, L.; Wong, C.Y.G.; Gill, H. Targeting and Monitoring Acute Myeloid Leukaemia with Nucleophosmin-1 (NPM1) Mutation. Int. J. Mol. Sci. 2023, 24, 3161. [Google Scholar] [CrossRef] [PubMed]
- Lachowiez, C.A.; Loghavi, S.; Zeng, Z.; Tanaka, T.; Kim, Y.J.; Uryu, H.; Turkalj, S.; Jakobsen, N.A.; Luskin, M.R.; Duose, D.Y.; et al. A Phase Ib/II Study of Ivosidenib with Venetoclax +/- Azacitidine in IDH1-Mutated Myeloid Malignancies. Blood Cancer Discov. 2023, 4, 276–293. [Google Scholar] [CrossRef] [PubMed]
- DiNardo, C.D.; Pratz, K.; Pullarkat, V.; Jonas, B.A.; Arellano, M.; Becker, P.S.; Frankfurt, O.; Konopleva, M.; Wei, A.H.; Kantarjian, H.M.; et al. Venetoclax combined with decitabine or azacitidine in treatment-naive, elderly patients with acute myeloid leukemia. Blood 2019, 133, 7–17. [Google Scholar] [CrossRef]
- Wong, K.K.; Hassan, R.; Yaacob, N.S. Hypomethylating Agents and Immunotherapy: Therapeutic Synergism in Acute Myeloid Leukemia and Myelodysplastic Syndromes. Front. Oncol. 2021, 11, 624742. [Google Scholar] [CrossRef]
- Roboz, G.J.; Ravandi, F.; Wei, A.H.; Dombret, H.; Thol, F.; Voso, M.T.; Schuh, A.C.; Porkka, K.; La Torre, I.; Skikne, B.; et al. Oral azacitidine prolongs survival of patients with AML in remission independently of measurable residual disease status. Blood 2022, 139, 2145–2155. [Google Scholar] [CrossRef]
- Wu, H.-C.; Rérolle, D.; Berthier, C.; Hleihel, R.; Sakamoto, T.; Quentin, S.; Benhenda, S.; Morganti, C.; Wu, C.; Conte, L. Actinomycin D targets NPM1c-primed mitochondria to restore PML-driven senescence in AML therapy. Cancer Discov. 2021, 11, 3198–3213. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Qin, F.; Yang, L.; Xian, J.; Zou, Q.; Jin, H.; Wang, L.; Zhang, L. Nucleophosmin mutations induce chemosensitivity in THP-1 leukemia cells by suppressing NF-κB activity and regulating Bax/Bcl-2 expression. J. Cancer 2016, 7, 2270. [Google Scholar] [CrossRef][Green Version]
- Roberts, A.W.; Davids, M.S.; Pagel, J.M.; Kahl, B.S.; Puvvada, S.D.; Gerecitano, J.F.; Kipps, T.J.; Anderson, M.A.; Brown, J.R.; Gressick, L. Targeting BCL2 with venetoclax in relapsed chronic lymphocytic leukemia. N. Engl. J. Med. 2016, 374, 311–322. [Google Scholar] [CrossRef] [PubMed]
- Lachowiez, C.A.; Reville, P.K.; Kantarjian, H.; Jabbour, E.; Borthakur, G.; Daver, N.; Issa, G.; Furudate, K.; Tanaka, T.; Pierce, S. Contemporary outcomes in IDH-mutated acute myeloid leukemia: The impact of co-occurring NPM1 mutations and venetoclax-based treatment. Am. J. Hematol. 2022, 97, 1443–1452. [Google Scholar] [CrossRef]
- Quintás-Cardama, A.; Ravandi, F.; Liu-Dumlao, T.; Brandt, M.; Faderl, S.; Pierce, S.; Borthakur, G.; Garcia-Manero, G.; Cortes, J.; Kantarjian, H. Epigenetic therapy is associated with similar survival compared with intensive chemotherapy in older patients with newly diagnosed acute myeloid leukemia. Blood J. Am. Soc. Hematol. 2012, 120, 4840–4845. [Google Scholar] [CrossRef] [PubMed]
- Dombret, H.; Seymour, J.F.; Butrym, A.; Wierzbowska, A.; Selleslag, D.; Jang, J.H.; Kumar, R.; Cavenagh, J.; Schuh, A.C.; Candoni, A. International phase 3 study of azacitidine vs conventional care regimens in older patients with newly diagnosed AML with> 30% blasts. Blood J. Am. Soc. Hematol. 2015, 126, 291–299. [Google Scholar] [CrossRef]
- Veselý, J. Mode of action and effects of 5-azacytidine and of its derivatives in eukaryotic cells. Pharmacol. Ther. 1985, 28, 227–235. [Google Scholar] [CrossRef]
- Wei, A.H.; Strickland, S.A., Jr.; Hou, J.-Z.; Fiedler, W.; Lin, T.L.; Walter, R.B.; Enjeti, A.; Tiong, I.S.; Savona, M.; Lee, S. Venetoclax combined with low-dose cytarabine for previously untreated patients with acute myeloid leukemia: Results from a phase Ib/II study. J. Clin. Oncol. 2019, 37, 1277–1284. [Google Scholar] [CrossRef]
- Wei, A.H.; Montesinos, P.; Ivanov, V.; DiNardo, C.D.; Novak, J.; Laribi, K.; Kim, I.; Stevens, D.A.; Fiedler, W.; Pagoni, M. Venetoclax plus LDAC for newly diagnosed AML ineligible for intensive chemotherapy: A phase 3 randomized placebo-controlled trial. Blood J. Am. Soc. Hematol. 2020, 135, 2137–2145. [Google Scholar] [CrossRef]
- Dick, J.E.; Bhatia, M.; Gan, O.; Kapp, U.; Wang, J.C. Assay of human stem cells by repopulation of NOD/SCID mice. Stem Cells 1997, 15 (Suppl. S1), 199–203. [Google Scholar] [CrossRef]
- Becker, H.; Marcucci, G.; Maharry, K.; Radmacher, M.D.; Mrozek, K.; Margeson, D.; Whitman, S.P.; Wu, Y.Z.; Schwind, S.; Paschka, P.; et al. Favorable prognostic impact of NPM1 mutations in older patients with cytogenetically normal de novo acute myeloid leukemia and associated gene- and microRNA-expression signatures: A Cancer and Leukemia Group B study. J. Clin. Oncol. 2010, 28, 596–604. [Google Scholar] [CrossRef]
- Ranieri, R.; Pianigiani, G.; Sciabolacci, S.; Perriello, V.M.; Marra, A.; Cardinali, V.; Pierangeli, S.; Milano, F.; Gionfriddo, I.; Brunetti, L.; et al. Current status and future perspectives in targeted therapy of NPM1-mutated AML. Leukemia 2022, 36, 2351–2367. [Google Scholar] [CrossRef] [PubMed]
- Lachowiez, C.A.; Loghavi, S.; Kadia, T.M.; Daver, N.; Borthakur, G.; Pemmaraju, N.; Naqvi, K.; Alvarado, Y.; Yilmaz, M.; Short, N.; et al. Outcomes of older patients with NPM1-mutated AML: Current treatments and the promise of venetoclax-based regimens. Blood Adv. 2020, 4, 1311–1320. [Google Scholar] [CrossRef] [PubMed]
- Brodska, B.; Otevrelova, P.; Salek, C.; Fuchs, O.; Gasova, Z.; Kuzelova, K. High PD-L1 Expression Predicts for Worse Outcome of Leukemia Patients with Concomitant NPM1 and FLT3 Mutations. Int. J. Mol. Sci. 2019, 20, 2823. [Google Scholar] [CrossRef] [PubMed]
- Orskov, A.D.; Treppendahl, M.B.; Skovbo, A.; Holm, M.S.; Friis, L.S.; Hokland, M.; Gronbaek, K. Hypomethylation and up-regulation of PD-1 in T cells by azacytidine in MDS/AML patients: A rationale for combined targeting of PD-1 and DNA methylation. Oncotarget 2015, 6, 9612–9626. [Google Scholar] [CrossRef] [PubMed]
- Knights, A.J.; Weinzierl, A.O.; Flad, T.; Guinn, B.A.; Mueller, L.; Mufti, G.J.; Stevanovic, S.; Pawelec, G. A novel MHC-associated proteinase 3 peptide isolated from primary chronic myeloid leukaemia cells further supports the significance of this antigen for the immunotherapy of myeloid leukaemias. Leukemia 2006, 20, 1067–1072. [Google Scholar] [CrossRef]
- Tettamanti, S.; Pievani, A.; Biondi, A.; Dotti, G.; Serafini, M. Catch me if you can: How AML and its niche escape immunotherapy. Leukemia 2022, 36, 13–22. [Google Scholar] [CrossRef]
- Nelde, A.; Schuster, H.; Heitmann, J.S.; Bauer, J.; Maringer, Y.; Zwick, M.; Volkmer, J.P.; Chen, J.Y.; Stanger, A.M.P.; Lehmann, A.; et al. Immune Surveillance of Acute Myeloid Leukemia Is Mediated by HLA-Presented Antigens on Leukemia Progenitor Cells. Blood Cancer Discov. 2023, 4, 468–489. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).