Progress in Oligometastatic Prostate Cancer: Emerging Imaging Innovations and Therapeutic Approaches
Abstract
:Simple Summary
Abstract
1. Introduction
2. Definition of Oligometastasis
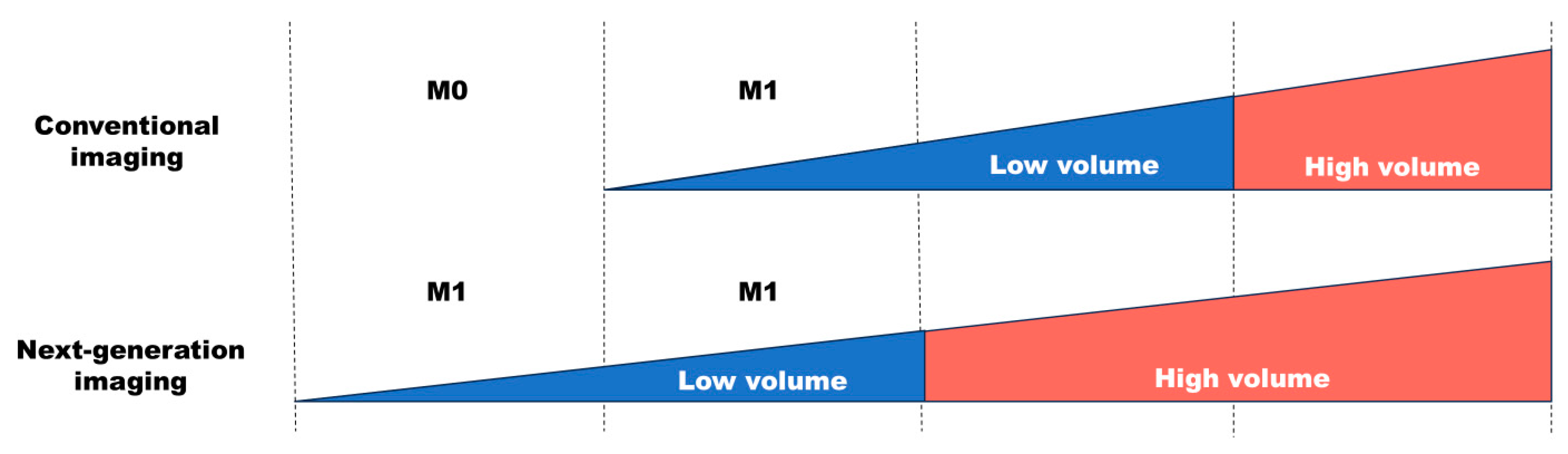
3. Imaging Diagnosis of Oligometastatic Lesions
4. Treatment of the Primary and/or Metastatic Lesions
4.1. Rationale
4.2. Radical Prostatectomy
4.3. Radiotherapy
4.4. Metastasis-Directed Treatment
4.5. Immunotherapy with Focal Therapy
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCANEstimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2019. CA Cancer J. Clin. 2019, 69, 7–34. [Google Scholar] [CrossRef] [PubMed]
- Teoh, J.Y.C.; Hirai, H.W.; Ho, J.M.W.; Chan, C.H.F.; Kelvin, K.F.; Tsoi, K.F.K.; Ng, F.C. Global incidence of prostate cancer in developing and developed countries with changing age structures. PLoS ONE 2019, 14, e0221775. [Google Scholar] [CrossRef] [PubMed]
- Utsumi, T.; Endo, T.; Sugizaki, Y.; Mori, T.; Somoto, T.; Kato, S.; Oka, R.; Yano, M.; Kamiya, N.; Suzuki, H. Risk assessment of multi-factorial complications after transrectal ultrasound-guided prostate biopsy: A single institutional retrospective cohort study. Int. J. Clin. Oncol. 2021, 26, 2295–2302. [Google Scholar] [CrossRef] [PubMed]
- Desai, M.M.; Cacciamani, G.E.; Gill, K.; Covas Moschovas, M.; Patel, V. Trends in incidence of metastatic prostate cancer in the US. JAMA Netw. Open 2022, 5, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Kelly, S.P.; Anderson, W.F.; Rosenberg, P.S.; Cook, M.B. Past, current, and future incidence rates and burden of metastatic prostate cancer in the United States. Eur. Urol. Focus 2018, 4, 121–127. [Google Scholar] [CrossRef]
- Gaylis, F.D.; Choi, J.E.; Hamilton, Z.; Dato, P.; Cohen, E.; Calabrese, R.; Dato, P.; Cohen, E.; Calabrese, R.; Prime, H.; et al. Change in prostate cancer presentation coinciding with USPSTF screening recommendations at a community-based urology practice. Urol. Oncol. 2017, 35, e1–e7. [Google Scholar] [CrossRef]
- Hellman, S.; Weichselbaum, R.R. Oligometastases. J. Clin. Oncol. 1995, 13, 8–10. [Google Scholar] [CrossRef]
- Shah, M.J.; Sharma, A.P.; Hameed, B.M.Z.; Jain, R.; Patil, A.; Karthickeyan, N.; Singh, A. Oligometastatic carcinoma prostate—An overview of the last decade. Indian J. Urol. 2023, 39, 195–201. [Google Scholar]
- Juan, G.R.; Laura, F.H.; Javier, P.V.; Natalia, V.C.; Mᵃ Isabel, G.R.; Enrique, R.G.; José Luis, S.P.; Pablo, A.L.; Noelia, S.S.; Roser, V.D.; et al. Where do we stand in the management of oligometastatic prostate cancer? A comprehensive review. Cancers 2022, 14, 2017. [Google Scholar] [CrossRef]
- Schaeffer, E.M.; Srinivas, S.; Adra, N.; An, Y.; Barocas, D.; Bitting, R.; Bryce, A.; Chapin, B.; Cheng, H.H.; D’Amico, A.V.; et al. Prostate Cancer, Version 4.2023, NCCN Clinical Practice Guidelines in Oncology. Available online: https://www.nccn.org/home/ (accessed on 3 November 2023).
- Terada, N.; Aizawa, R.; Nihei, K.; Shiota, M.; Kojima, T.; Kimura, T.; Inoue, T.; Kitamura, H.; Sugimoto, M.; Nishiyama, H.; et al. Narrative review of local prostate and metastasis-directed radiotherapy in the treatment of metastatic prostate cancer. Jpn. J. Clin. Oncol. 2022, 52, 633–641. [Google Scholar] [CrossRef] [PubMed]
- De Bruycker, A.; Tran, P.T.; Achtman, A.H.; Ost, P.; GAP6 consortium. Clinical perspectives from ongoing trials in oligometastatic or oligorecurrent prostate cancer: An analysis of clinical trials registries. World J. Urol. 2023, 39, 317–326. [Google Scholar] [CrossRef] [PubMed]
- Slaoui, A.; Albisinni, S.; Aoun, F.; Assenmacher, G.; Al Hajj Obeid, W.; Diamand, R.; Regragui, S.; Touzani, A.; Bakar, A.; Mesfioui, A.; et al. A systematic review of contemporary management of oligometastatic prostate cancer: Fighting a challenge or tilting at windmills? World J. Urol. 2019, 37, 2343–2353. [Google Scholar] [CrossRef] [PubMed]
- Tosoian, J.J.; Gorin, M.A.; Ross, A.E.; Pienta, K.J.; Tran, P.T.; Schaeffer, E.M. Oligometastatic prostate cancer: Definitions, clinical outcomes, and treatment considerations. Nat. Rev. Urol. 2017, 14, 15–25. [Google Scholar] [CrossRef] [PubMed]
- Battaglia, A.; De Meerleer, G.; Tosco, L.; Moris, L.; Van den Broeck, T.; Devos, G.; Everaerts, W.; Joniau, S. Novel insights into the management of oligometastatic prostate cancer: A comprehensive review. Eur. Urol. Oncol. 2019, 2, 174–188. [Google Scholar] [CrossRef]
- Rao, A.; Vapiwala, N.; Schaeffer, E.M.; Ryan, J.C. Oligometastatic prostate cancer: A shrinking subset or an opportunity for cure? Am. Soc. Clin. Oncol. Educ. Book 2019, 39, 309–320. [Google Scholar] [CrossRef]
- Sabbag, A.; Mohamad, O.; Lichter, K.E.; Hope, T.A. Management of patients with recurrence and metachronous oligometastatic prostate cancer in the era of PSMA PET. Cancers 2022, 14, 6194. [Google Scholar] [CrossRef]
- Niibe, Y.; Kenjo, M.; Kazumoto, T.; Michimoto, K.; Takayama, M.; Yamauchi, C.; Kataoka, M.; Suzuki, K.; Ii, N.; Uno, T.; et al. Multi-institutional study of radiation therapy for isolated paraaortic lymph node recurrence in uterine cervical carcinoma: 84 subjects of a population more than 5000. Int. J. Radiat. Oncol. Biol. Phys. 2006, 66, 1366–1369. [Google Scholar] [CrossRef]
- Niibe, Y.; Hayakawa, K. Oligometastases and oligo-recurrence: The new era of cancer therapy. Jpn. J. Clin. Oncol. 2010, 40, 107–111. [Google Scholar] [CrossRef]
- Niibe, Y.; Chang, J.Y. Novel insights of oligometastases and oligo-recurrence and review of the literature. Pulm. Med. 2012, 2012, 261096. [Google Scholar] [CrossRef]
- Foster, C.C.; Weichselbaum, R.R.; Pitroda, S.P. Oligometastatic prostate cancer: Reality or figment of imagination? Cancer 2019, 125, 340–352. [Google Scholar] [CrossRef] [PubMed]
- Gillessen, S.; Attard, G.; Beer, T.M.; Beltran, H.; Bjartell, A.; Bossi, A.; Briganti, A.; Bristow, R.G.; Chi, K.N.; Clarke, N.; et al. Management of patients with advanced prostate cancer: Report of the advanced prostate cancer consensus conference 2019. Eur. Urol. 2020, 77, 508–547. [Google Scholar] [CrossRef] [PubMed]
- Guckenberger, M.; Lievens, Y.; Bouma, A.B. Characterization and classification of oligometastatic disease: A European Society for Radiotherapy and Oncology and European Organisation for Research and Treatment of Cancer consensus recommendation. Lancet Oncol. 2020, 21, e18–e28. [Google Scholar] [CrossRef]
- Zilli, T.; Achard, V.; Dal Pra, A.; Collette, L.; Dekker, A.; deSouza, N.M.; Dingemans, A.C.; Fournier, B.; Hurkmans, C.; Lecouvet, F.E.; et al. Recommendations for radiation therapy in oligometastatic prostate cancer: An ESTRO-ACROP Delphi consensus. Radiother. Oncol. 2022, 176, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Thomas, L.; Balmus, C.; Ahmadzadehfar, H.; Essler, M.; Strunk, H.; Bundschuh, R.A. Assessment of bone metastases in patients with prostate cancer-A comparison between 99mTc-bone- scintigraphy and [68Ga]Ga-PSMA PET/CT. Pharmaceuticals 2017, 10, 68. [Google Scholar] [CrossRef] [PubMed]
- van Leeuwen, P.J.; Stricker, P.; Hruby, G.; Kneebone, A.; Ting, F.; Thompson, B.; Nguyen, Q.; Ho, B.; Emmett, L. 68Ga-PSMA has a high detection rate of prostate cancer recurrence outside the prostatic fossa in patients being considered for salvage radiation treatment. BJU Int. 2016, 117, 732–739. [Google Scholar] [CrossRef] [PubMed]
- Sawicki, L.M.; Kirchner, J.; Buddensieck, C.; Antke, C.; Ullrich, T.; Schimmöller, L.; Boos, J.; Schleich, C.; Schaarschmidt, B.M.; Buchbender, C.; et al. Prospective comparison of whole-body MRI and 68Ga-PSMA PET/CT for the detection of biochemical recurrence of prostate cancer after radical prostatectomy. Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 1542–1550. [Google Scholar] [CrossRef] [PubMed]
- Filippi, L.; Bagni, O.; Schillaci, O. Digital PET/CT with 18F-FACBC in early castration-resistant prostate cancer: Our preliminary results. Expert Rev. Med. Devices 2022, 19, 591–598. [Google Scholar] [CrossRef]
- Amorim, B.J.; Prabhu, V.; Marco, S.S.; Gervais, D.; Palmer, W.E.; Heidari, P.; Vangel, M.; Saylor, P.J.; Catalano, O.A. Performance of 18F-fluciclovine PET/MR in the evaluation of osseous metastases from castration-resistant prostate cancer. Eur. J. Nucl. Med. Mol. Imaging 2022, 47, 105–114. [Google Scholar] [CrossRef]
- Wright, G.L., Jr.; Haley, C.; Beckett, M.L.; Schellhammer, P.F. Expression of prostate-specific membrane antigen in normal, benign, and malignant prostate tissues. Urol. Oncol. 1995, 1, 18–28. [Google Scholar] [CrossRef]
- Palma, D.A.; Louie, A.V.; Rodrigues, G.B. New strategies in stereotactic radiotherapy for oligometastases. Clin. Cancer Res. 2015, 21, 5198–5204. [Google Scholar] [CrossRef] [PubMed]
- Mole, R.H. Whole body irradiation—radiobiology or medicine? Br. J. Radiol. 1953, 26, 234–241. [Google Scholar] [CrossRef]
- Palacios-Eito, A.; Béjar-Luque, A.; Rodríguez-Liñán, M.; García-Cabezas, S. Oligometastases in prostate cancer: Ablative treatment. World J. Clin. Oncol. 2019, 10, 38–51. [Google Scholar] [CrossRef]
- Culp, S.H.; Schellhammer, P.F.; Williams, M.B. Might men diagnosed with metastatic prostate cancer benefit from definitive treatment of the primary tumor? A SEER-based study. Eur. Urol. 2014, 65, 1058–1066. [Google Scholar] [CrossRef] [PubMed]
- Colosini, A.; Bernardi, S.; Foroni, C.; Pasinetti, N.; Guerini, A.E.; Russo, D.; Bresciani, R.; Tomasi, C.; Magrini, S.M.; Bardoscia, L.; et al. Stratification of oligometastatic prostate cancer patients by liquid biopsy: Clinical insights from a pilot study. Biomedicines 2022, 10, 1321. [Google Scholar] [CrossRef] [PubMed]
- Won, A.C.M.; Gurney, H.; Marx, G.; De Souza, P.; Patel, M.I. Primary treatment of the prostate improves local palliation in men who ultimately develop castrate-resistant prostate cancer. BJU Int. 2013, 112, E250–E255. [Google Scholar] [CrossRef]
- Heidenreich, A.; Pfster, D.; Porres, D. Cytoreductive radical prostatectomy in patients with prostate cancer and low volume skeletal metastases: Results of a feasibility and case-control study. J. Urol. 2015, 193, 832–838. [Google Scholar] [CrossRef] [PubMed]
- Steuber, T.; Berg, K.D.; Order, M.A.; Brasso, K.; Iversen, P.; Huland, H.; Tiebel, A.; Schlomm, T.; Haese, A.; Salomon, G.; et al. Does cytoreductive prostatectomy really have an impact on prognosis in prostate cancer patients with low-volume bone metastasis? Results from a prospective case-control study. Eur. Urol. Focus 2017, 3, 646–649. [Google Scholar] [CrossRef]
- Ranasinghe, W.; Chapin, B.F.; Kim, I.Y.; Sooriakumaran, P.; Lawrentschuk, N. The cytoreductive prostatectomy in metastatic prostate cancer: What the individual trials are hoping to answer. BJU Int. 2020, 125, 792–800. [Google Scholar] [CrossRef]
- Sooriakumaran, P.; Wilson, C.; Rombach, I.; Hassanali, N.; Aning, J.; D Lamb, A.; Cathcart, P.; Eden, C.; Ahmad, I.; Rajan, P.; et al. Feasibility and safety of radical prostatectomy for oligo-metastatic prostate cancer: The testing radical prostatectomy in men with prostate cancer and oligo-metastases to the bone (TRoMbone) trial. BJU Int. 2022, 130, 43–53. [Google Scholar] [CrossRef]
- Saouli, A.; Touzani, A.; Martini, A.; Beauval, J.B.; Dergamoun, H.; Ziouziou, I.; Deffar, N.; Ploussard, G.; Ouzzane, A. Is there a role for radical prostatectomy in the management of oligometastatic prostate cancer? A systematic review. Prostate Cancer Prostatic Dis. 2023, in press. [Google Scholar] [CrossRef]
- Boeve, L.M.S.; Hulshof, M.C.C.M.; Vis, A.N.; Zwinderman, A.H.; Twisk, J.W.R.; Witjes, W.P.J.; Delaere, K.P.J.; Moorselaar, R.J.A.V.; Verhagen, P.C.M.S.; van Andel, G. Effect on survival of androgen deprivation therapy alone compared to androgen deprivation therapy combined concurrent radiation therapy to prostate in patients with primary bone metastatic prostate cancer in a prospective randomized clinical trial: Data from the HORRAD trial. Eur. Urol. 2019, 75, 410–418. [Google Scholar] [PubMed]
- Parker, C.C.; James, N.D.; Brawley, C.D.; Clarke, N.W.; Hoyle, A.P.; Ali, A.; Ritchie, A.W.S.; Attard, G.; Chowdhury, S.; Cross, W.; et al. Radiotherapy to the primary tumor for newly diagnosed metastatic prostate cancer (STAMPEDE): A randomized controlled phase 3 trial. Lancet 2018, 392, 2353–2366. [Google Scholar] [CrossRef] [PubMed]
- Fizazi, K.; Foulon, S.; Carles, J.; Roubaud, G.; McDermott, R.; Fléchon, A.; Tombal, B.; Supiot, S.; Berthold, D.; Ronchin, P.; et al. Abiraterone plus prednisone added to androgen deprivation therapy and docetaxel in de novo metastatic castration-sensitive prostate cancer (PEACE-1): A multicentre, open-label, randomised, phase 3 study with a 2 × 2 factorial design. Lancet 2022, 399, 1695–1707. [Google Scholar] [CrossRef] [PubMed]
- Bossi, A.; Foulon, S.; Maldonado, X.; Sargos, P.; McDermott, S.R.; Flechon, A.; Tombal, F.B.; Supiot, S.; Berthold, R.D.; Ronchin, P.; et al. Prostate irradiation in men with de novo, low-volume, metastatic, castration-sensitive prostate cancer (mCSPC): Results of PEACE-1, a phase 3 randomized trial with a 2 × 2 design. J. Clin. Oncol. 2023, 41 (Suppl. 17). [Google Scholar] [CrossRef]
- Burdett, S.; Boeve, L.M.; Ingleby, F.C.; Fisher, D.J.; Rydzewska, L.H.; Vale, C.L.; van Andel, G.; Clarke, N.W.; Hulshof, M.C.; James, N.D.; et al. Prostate Radiotherapy for Metastatic Hormone-sensitive Prostate Cancer: A STOPCAP Systematic Review and Meta-analysis. Eur. Urol. 2019, 76, 115–124. [Google Scholar] [CrossRef] [PubMed]
- Ost, P.; Reynders, D.; Decaestecker, K.; Fonteyne, V.; Lumen, N.; De Bruycker, A.; Lambert, B.; Delrue, L.; Bultijnck, R.; Claeys, T.; et al. Surveillance or metastasis-directed therapy for oligometastatic prostate cancer recurrence: A prospective, randomized, multicenter phase II trial. J. Clin. Oncol. 2018, 36, 446–453. [Google Scholar] [CrossRef] [PubMed]
- Phillips, R.; Shi, W.Y.; Deek, M.; Radwan, N.; Lim, S.J.; Antonarakis, E.S.; Rowe, S.P.; Ross, A.E.; Gorin, M.A.; Deville, C.; et al. Outcomes of observation vs stereotactic ablative radiation for oligometastasic prostate cancer: The ORIOLE Phase 2 Randomized Clinical Trial. JAMA Oncol. 2020, 6, 650–659. [Google Scholar] [CrossRef]
- Deek, M.P.; Van der Eecken, K.; Sutera, P.; Deek, R.A.; Fonteyne, V.; Mendes, A.A.; Decaestecker, K.; Kiess, A.P.; Lumen, N.; Phillips, R.; et al. Long-term outcomes and genetic predictors of response to metastasis-directed therapy versus observation in oligometastatic prostate cancer: Analysis of STOMP and ORIOLE trials. J. Clin. Oncol. 2022, 40, 3377–3382. [Google Scholar] [CrossRef]
- Supiot, S.; Vaugier, L.; Pasquier, D.; Deek, R.A.; Fonteyne, V.; Mendes, A.A.; Decaestecker, K.; Kiess, A.P.; Lumen, N.; Phillips, R.; et al. OLIGOPELVIS-GETUG P07, a multicenter phase II trial of combined high-dose salvage radiotherapy and hormone therapy in oligorecurrent pelvic node relapses in prostate cancer. Eur. Urol. 2021, 80, 405–414. [Google Scholar] [CrossRef]
- De Bruycker, A.; Spiessens, A.; Dirix, P.; Koutsouvelis, N.; Semac, I.; Liefhooghe, N.; Gomez-Iturriaga, A.; Everaerts, W.; Otte, F.; Papachristofilou, A.; et al. PEACE V—Salvage Treatment of OligoRecurrent nodal prostate cancer Metastases (STORM): A study protocol for a randomized controlled phase II trial. BMC Cancer 2020, 20, 406. [Google Scholar] [CrossRef] [PubMed]
- Francolini, G.; Allegra, A.G.; Detti, B.; Di Cataldo, V.; Caini, S.; Bruni, A.; Ingrosso, G.; D’Angelillo, R.M.; Alitto, A.R.; Augugliaro, M.; et al. Stereotactic Body Radiation Therapy and Abiraterone Acetate for Patients Affected by Oligometastatic Castrate-Resistant Prostate Cancer: A Randomized Phase II Trial (ARTO). J. Clin. Oncol. 2023, in press. [CrossRef] [PubMed]
| Category | De Novo Oligometastasis | Oligorecurrence | Oligoprogression |
|---|---|---|---|
| Primary tumor status | Not controlled | Controlled | Controlled/uncontrolled |
| Systemic treatment | Naive | Naive | Resistant |
| Location of metastases | N1 or M1 | N1 or M1 | N1 or M1 |
| Study Name | Oligometastasis | Design | Primary Endpoint | Summary of Results |
|---|---|---|---|---|
| Prostate RT | ||||
| HORRAD | De novo mCSPC | ADT vs. ADT+EBRT | OS | Better OS in ADT+EBRT group (not significantly) |
| STAMPEDE Arm H | De novo mCSPC | SOC (ADT±DOC) vs. SOC+EBRT | OS | Significantly improved OS and FFS in SOC+EBRT group |
| PEACE-1 | De novo mCSPC | SOC (ADT±DOC) ±AAP vs. SOC±AAP +EBRT | OS rPFS | Better OS and rPFS in SOC+AAP+EBRT group (not significantly) |
| MDT | ||||
| STOMP | Oligorecurrent mCSPC | Active surveillance vs. SBRT or surgery for metastases | ADT-free survival | Better ADT-free survival in MDT group (not significantly) |
| ORIOLE | Oligorecurrent mCSPC | Observation vs. SBRT | rPFS at 6 months | Significantly improved rPFS at 6 months in SBRT group |
| PROPE | Oligorecurrent mCSPC | SBRT+radium-223 | ADT-free survival | - |
| OLIGOPELVIS | Oligorecurrent mCSPC | ADT+pelvic IMRT | 2-year PFS | - |
| STORM | Oligorecurrent mCSPC | ADT+SBRT or salvage lymphadenectomy vs. ADT+WPRT | MFS | - |
| ARTO | Oligoprogressive mCRPC | ADT+AAP vs. ADT+AAP+SBRT | BR | Significantly improved BR in ADT+AAP+SBRT group |
| PCS IX | Oligoprogressive mCRPC | ADT+ENZ vs. ADT+ENZ+SBRT | rPFS | - |
| PILLAR | Oligoprogressive mCRPC | ADT+APA vs. ADT+APA+SBRT | Post-treatment PSA <0.2 ng/mL | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oka, R.; Utsumi, T.; Noro, T.; Suzuki, Y.; Iijima, S.; Sugizaki, Y.; Somoto, T.; Kato, S.; Endo, T.; Kamiya, N.; et al. Progress in Oligometastatic Prostate Cancer: Emerging Imaging Innovations and Therapeutic Approaches. Cancers 2024, 16, 507. https://doi.org/10.3390/cancers16030507
Oka R, Utsumi T, Noro T, Suzuki Y, Iijima S, Sugizaki Y, Somoto T, Kato S, Endo T, Kamiya N, et al. Progress in Oligometastatic Prostate Cancer: Emerging Imaging Innovations and Therapeutic Approaches. Cancers. 2024; 16(3):507. https://doi.org/10.3390/cancers16030507
Chicago/Turabian StyleOka, Ryo, Takanobu Utsumi, Takahide Noro, Yuta Suzuki, Shota Iijima, Yuka Sugizaki, Takatoshi Somoto, Seiji Kato, Takumi Endo, Naoto Kamiya, and et al. 2024. "Progress in Oligometastatic Prostate Cancer: Emerging Imaging Innovations and Therapeutic Approaches" Cancers 16, no. 3: 507. https://doi.org/10.3390/cancers16030507
APA StyleOka, R., Utsumi, T., Noro, T., Suzuki, Y., Iijima, S., Sugizaki, Y., Somoto, T., Kato, S., Endo, T., Kamiya, N., & Suzuki, H. (2024). Progress in Oligometastatic Prostate Cancer: Emerging Imaging Innovations and Therapeutic Approaches. Cancers, 16(3), 507. https://doi.org/10.3390/cancers16030507







