The Use of Natural Language Processing Elements for Computer-Aided Diagnostics and Monitoring of Body Image Perception in Enterally Fed Patients with Head and Neck or Upper Gastrointestinal Tract Cancers
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Methods
2.2.1. Text Analysis
2.2.2. The Sentiment-Based Approach in Body Image Analysis
2.2.3. Identification of Potential Areas of Difficulty
- A topic is included in a note in a negative context if the value of the topic affiliation in the negative context is greater than the value of the topic affiliation in the positive context and the relative difference is greater than 20%.
- A topic is included in a note in a positive context if the value of belonging to the topic in a positive context is greater than the value of belonging to the topic in a negative context and the relative difference is greater than 20%.
- The note refers to the topic in a mixed (positive–negative) context if the relative difference between the affiliations is less than 20%.
- The topic does not appear in the note if the value of belonging to this topic in each context equals 0.
2.2.4. Emotion Measurement Method
3. Results
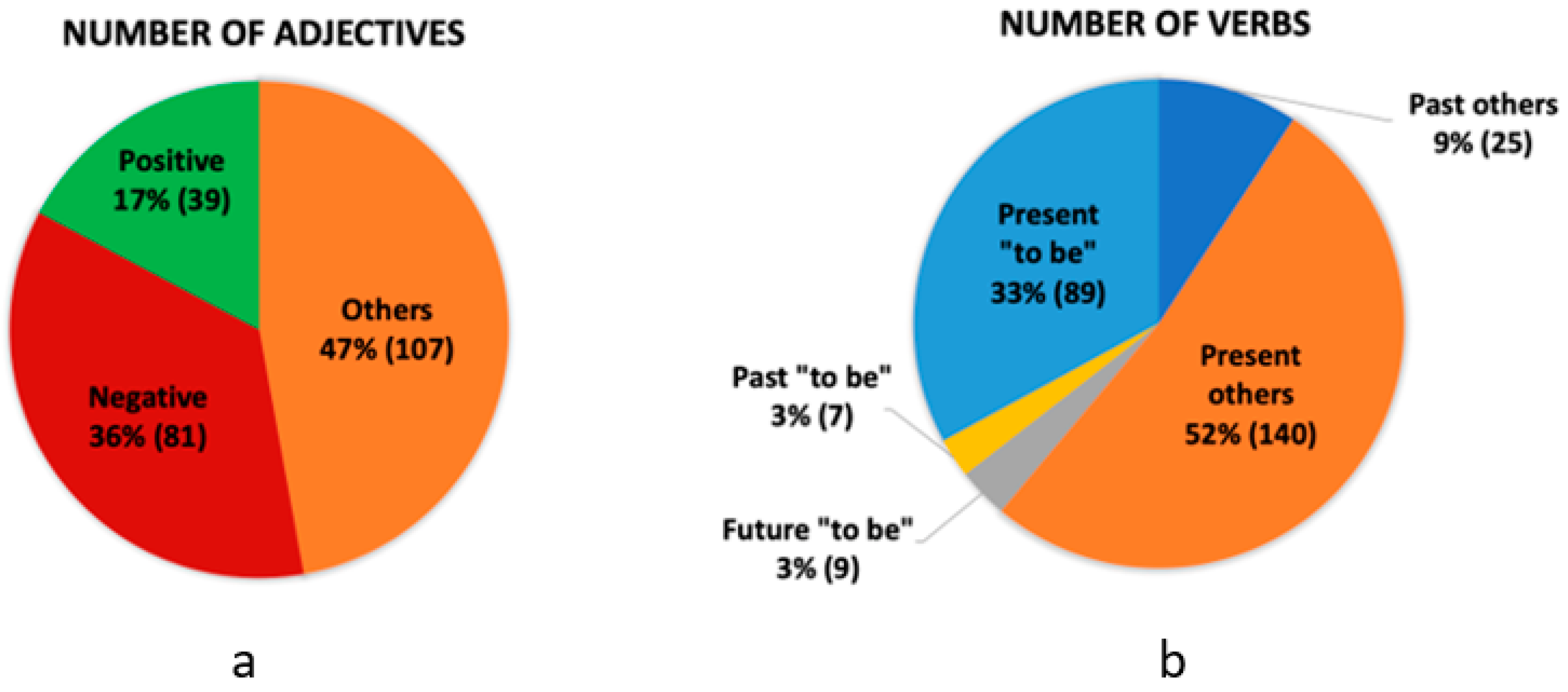
3.1. Statistical Analysis of Word Types and Sentiment Tagging
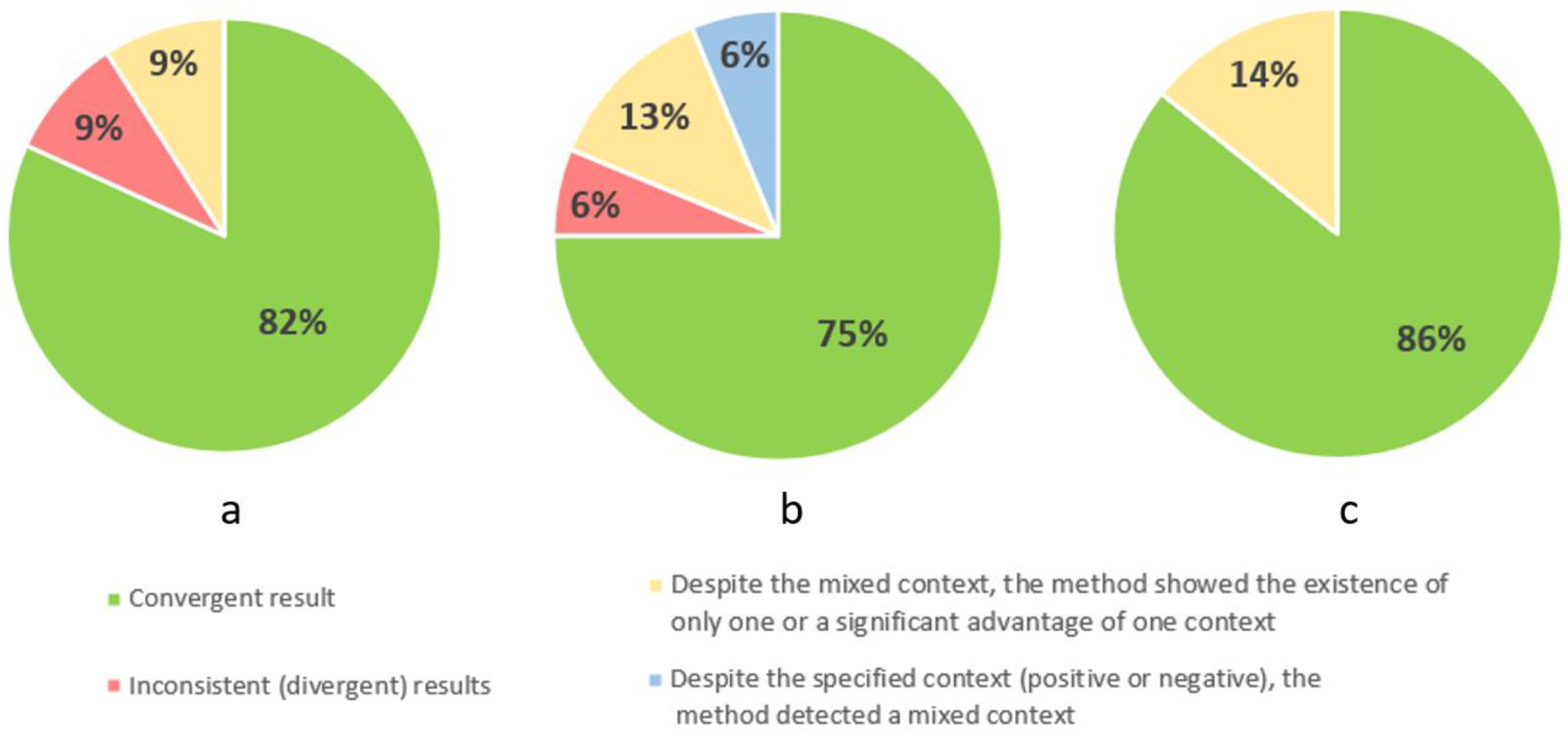
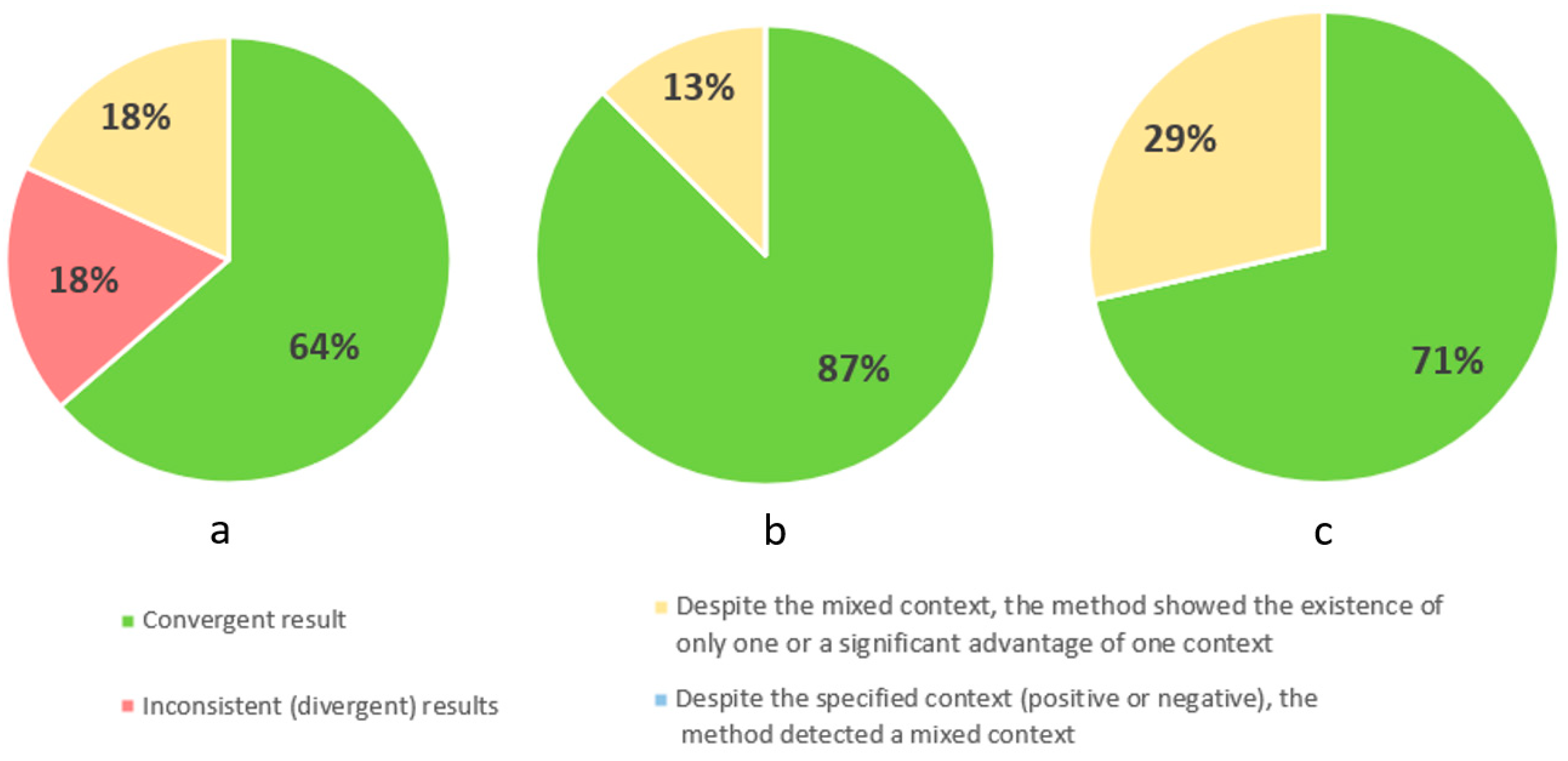
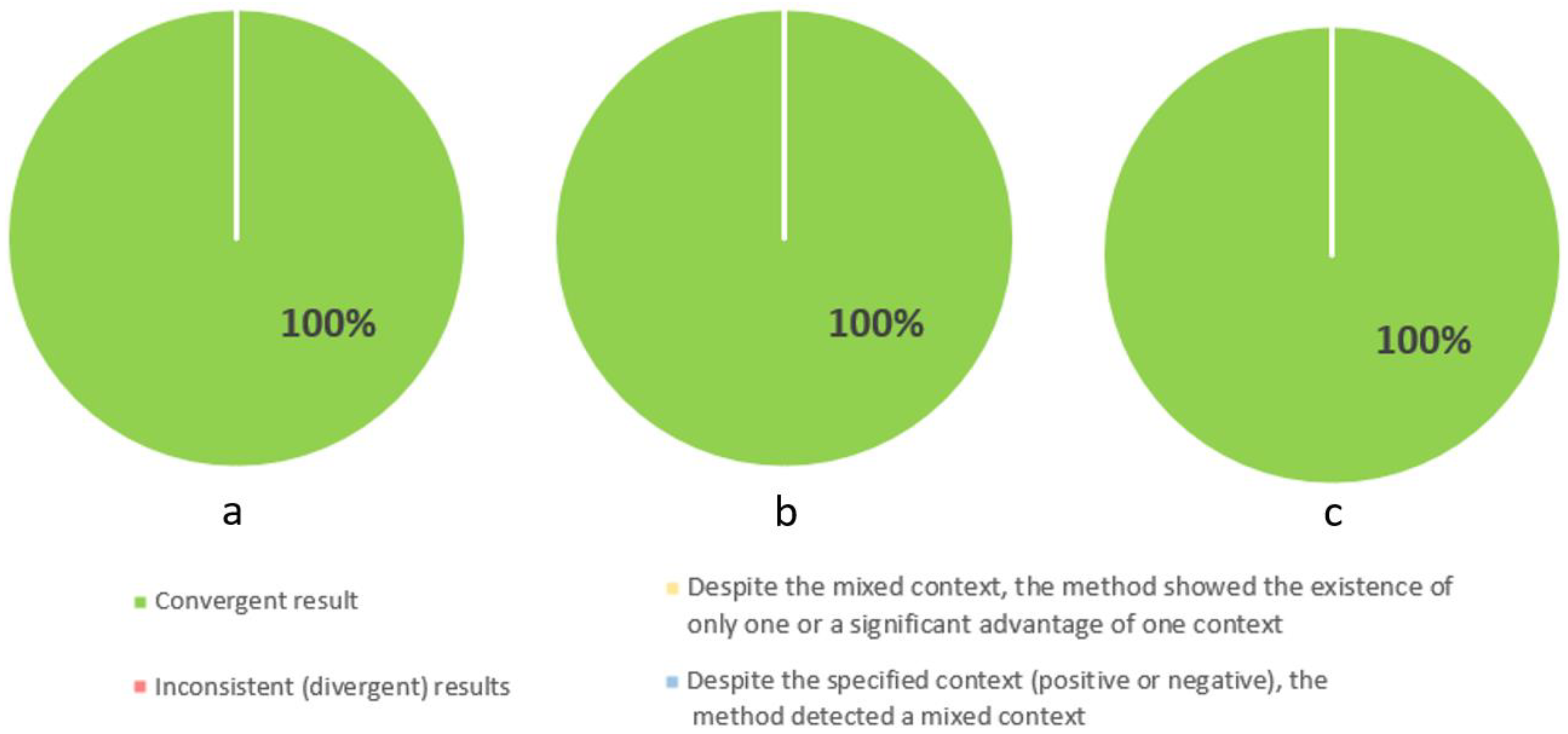
3.2. Analysis of Potential Areas of Difficulty
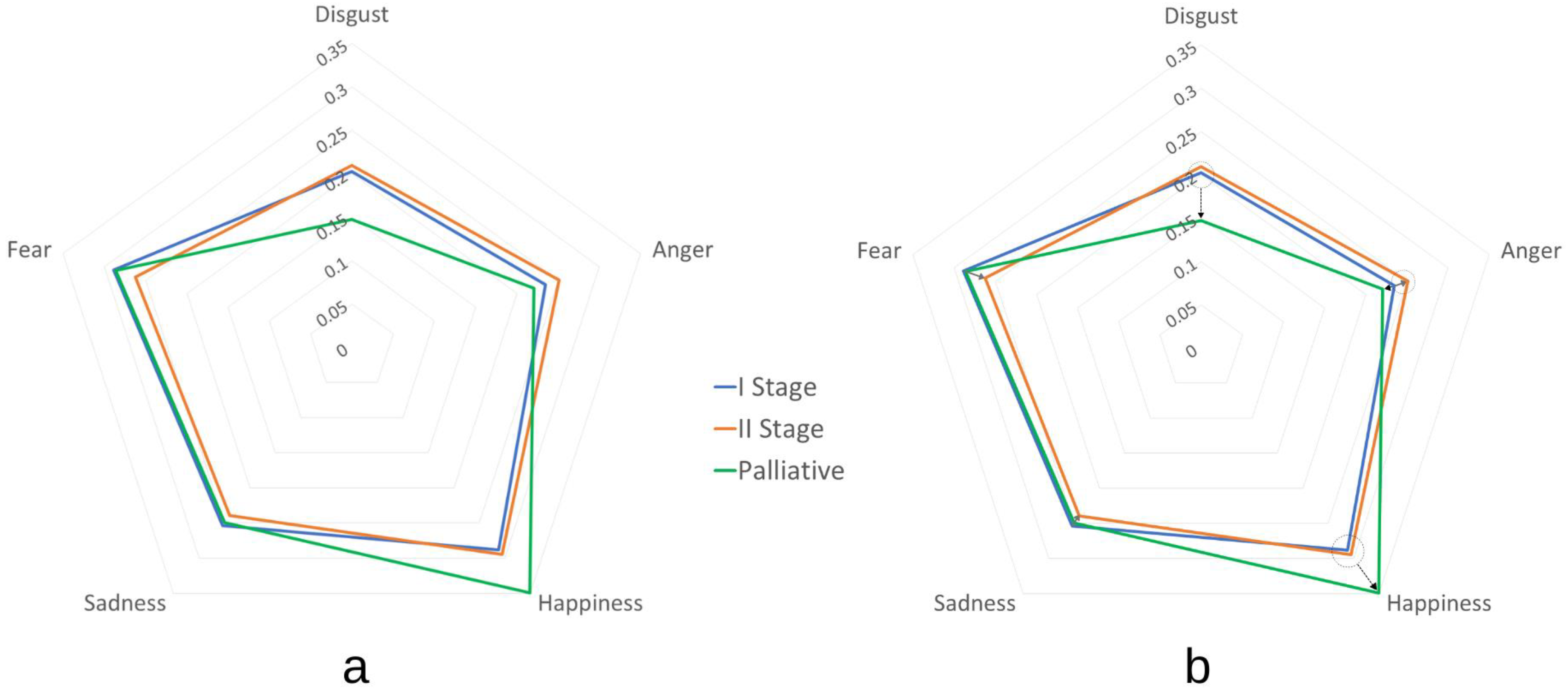
3.3. Emotions Analysis
3.4. Statistical Analyses—Body Image, Self-Esteem, Emotions, and Stages of Diseases
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mouillot, T.; Brindisi, M.C.; Drouillard, A.; Marref, I.; Brondel, L.; Lepage, C. Enteral nutrition in medical oncology: Clinical situation. Hépato-Gastroenterol. Oncol. Dig. 2020, 27, 1005–1012. [Google Scholar]
- Meza-Valderrama, D.; Marco, E.; Dávalos-Yerovi, V.; Muns, M.D.; Tejero-Sánchez, M.; Duarte, E.; Sánchez-Rodríguez, D. Sarcopenia, Malnutrition, and Cachexia: Adapting Definitions and Terminology of Nutritional Disorders in Older People with Cancer. Nutrients 2021, 13, 761. [Google Scholar] [CrossRef] [PubMed]
- Bischoff, S.C.; Austin, P.; Boeykens, K.; Chourdakis, M.; Cuerda, C.; Jonkers-Schuitema, C.; Lichota, M.; Nyulasi, I.; Schneider, S.M.; Stanga, Z.; et al. ESPEN practical guideline: Home enteral nutrition. Clin. Nutr. 2022, 41, 468–488. [Google Scholar] [CrossRef] [PubMed]
- Wanden-Berghe, C.; Patino-Alonso, M.C.; Galindo-Villardón, P.; Sanz-Valero, J. Complications Associated with Enteral Nutrition: CAFANE Study. Nutrients 2020, 11, 2041. [Google Scholar] [CrossRef] [PubMed]
- Edgley, K. Early enteral nutrition: Indications, benefits and complications. Vet. Nurse 2019, 10, 346–351. [Google Scholar] [CrossRef]
- Boryczko-Pater, B.; Baron, A.; Szaleniec, J.; Gierowski, J.K.; Składzień, J. Dynamika przystosowania do choroby i jej akceptacji u pacjentów z nowotworami głowy i szyi. Otolaryngol. Pol. 2011, 65 (Suppl. S3), 48–53. [Google Scholar] [CrossRef]
- Mokhtari-Hessari, P.; Montazeri, A. Health-related quality of life in breast cancer patients: Review of reviews from 2008 to 2018. Health Qual. Life Outcomes 2020, 18, 338. [Google Scholar] [CrossRef] [PubMed]
- Fieldhouse, P. Social functions of food. In Food and Nutrition: Customs and Culture [Internet]; Fieldhouse, P., Ed.; Springer: Boston, MA, USA, 1995; pp. 78–105. [Google Scholar] [CrossRef]
- Gliwska, E.; Barańska, K.; Maćkowska, S.; Różańska, A.; Sobol, A.; Spinczyk, D. The Use of Natural Language Processing for Computer-Aided Diagnostics and Monitoring of Body Image Perception in Patients with Cancers. Cancers 2023, 15, 5437. [Google Scholar] [CrossRef] [PubMed]
- Esplen, M.J.; Fingeret, M.C.; Breitbard, W.; Butow, P.; Jacobsen, P.; Wing Tak Lam, W. Body image—An important dimension in cancer care. Psycho-Oncology 2021, 4, 303–312. [Google Scholar]
- Riegel, M.; Wierzba, M.; Wypych, M.; Żurawski, Ł.; Jednoróg, K.; Grabowska, A.; Marchewka, A. Nencki Affective Word List (NAWL): The cultural adaptation of the Berlin Affective Word List–Reloaded (BAWL-R) for Polish. Behav Res. 2015, 47, 1222–1236. [Google Scholar] [CrossRef]
- SAS Viya: The High-Performance AI & Analytics Platform|SAS. Available online: https://www.sas.com/en_us/software/viya.html (accessed on 17 February 2024).
- Rhoten, B.A.; Murphy, B.; Ridner, S.H. Body image in patients with head and neck cancer: A review of the literature. Oral Oncol. 2013, 49, 753–760. [Google Scholar] [CrossRef] [PubMed]
- Tao, J.; Fang, X. Toward multi-label sentiment analysis: A transfer learning based approach. J. Big Data 2020, 7, 1. [Google Scholar] [CrossRef]
- Ali, T.; Schramm, D.; Sokolova, M.; Inkpen, D. Can I Hear You? Sentiment Analysis on Medical Forums. In Proceedings of the Sixth International Joint Conference on Natural Language Processing [Internet]; Asian Federation of Natural Language Processing: Nagoya, Japan, 2013; pp. 667–673. Available online: https://aclanthology.org/I13-1077 (accessed on 23 June 2023).
- Huan, H.; Guo, Z.; Cai, T.; He, Z. A text classification method based on a convolutional and bidirectional long short-term memory model. Connect. Sci. 2022, 34, 2108–2124. [Google Scholar] [CrossRef]
- He, Q. Text Mining and IRT for Psychiatric and Psychological Assessment. 3 October 2013. Available online: https://research.utwente.nl/en/publications/text-mining-and-irt-for-psychiatric-and-psychological-assessment (accessed on 11 January 2023).
- HaCohen-Kerner, Y.; Miller, D.; Yigal, Y. The influence of preprocessing on text classification using a bag-of-words representation. PLoS ONE 2020, 15, e0232525. [Google Scholar] [CrossRef]
- Lula, P. Text Mining Jako Narzędzie Pozyskiwania Informacji Z Dokumentów Tekstowych; Statsoft: Kraków, Poland, 2005. [Google Scholar]
- Mirończuk, M. Przegląd Metod I Technik Eksploracji Danych Tekstowych; Instytut Informatyki Uniwersytet Kazimierza Wielkiego: Bydgoszczy, Poland, 2012. [Google Scholar]
- Dzieciątko, M.; Spinczyk, D. Text Mining: Metody, Narzędzia I Zastosowania; Księgarnia Internetowa PWN: Kraków, Poland, 2016. [Google Scholar]
- Barańska, K.; Różańska, A.; Maćkowska, S.; Rojewska, K.; Spinczyk, D. Determining the Intensity of Basic Emotions among People Suffering from Anorexia Nervosa Based on Free Statements about Their Body. Electronics 2022, 11, 138. [Google Scholar] [CrossRef]
- Baldwin, S.A.; Hoffmann, J.P. The Dynamics of Self-Esteem: A Growth-Curve Analysis. J. Youth Adolesc. 2002, 31, 101–113. [Google Scholar] [CrossRef]
- Nishigami, T.; Mibu, A.; Osumi, M.; Son, K.; Yamamoto, S.; Kajiwara, S.; Tanaka, K.; Matsuya, A.; Tanabe, A. Are tactile acuity and clinical symptoms related to differences in perceived body image in patients with chronic nonspecific lower back pain? Man Ther. 2015, 20, 63–67. [Google Scholar] [CrossRef]
- Teo, I.; Novy, D.M.; Chang, D.W.; Cox, M.G.; Fingeret, M.C. Examining pain, body image, and depressive symptoms in patients with lymphedema secondary to breast cancer. Psychooncology 2015, 24, 1377–1383. [Google Scholar] [CrossRef]
- Kubler-Ross, E. eweb:1860. 1969. On Death and Dying. Available online: https://repository.library.georgetown.edu/handle/10822/1031279 (accessed on 23 June 2023).
- Ostafin, B.D.; Papenfuss, I.; Vervaeke, J. Fear of the unknown as a mechanism of the inverse relation between life meaning and psychological distress. Anxiety Stress Coping 2022, 35, 379–394. [Google Scholar] [CrossRef] [PubMed]
- Trzebiński, J. Narracyjne Konstruowanie Rzeczywistości; Gdańskie Wydawnictwo Psychologiczne: Gdańsk, Poland, 2002. [Google Scholar]
- Thewes, B.; Butow, P.; Bell, M.L.; Beith, J.; Stuart-Harris, R.; Grossi, M.; Capp, A.; Dalley, D. Fear of cancer recurrence in young women with a history of early-stage breast cancer: A cross-sectional study of prevalence and association with health behaviours. Support Care Cancer 2012, 20, 2651–2659. [Google Scholar] [CrossRef]
- Izgiç, F.; Akyüz, G.; Doğan, O.; Kuğu, N. Social Phobia among University Students and its Relation to Self-Esteem and Body Image. Can J. Psychiatry 2004, 49, 630–634. [Google Scholar] [CrossRef] [PubMed]
- Shafaee, F.S.; Mirghafourvand, M.; Harischi, S.; Esfahani, A.; Amirzehni, J. Self-Confidence and Quality of Life in Women Undergoing Treatment for Breast Cancer. Asian Pac. J. Cancer Prev. 2018, 19, 733–740. [Google Scholar]



| Negative Adjectives | Positive Adjectives | |
|---|---|---|
| Stage 1 | 14.45% | 1.83% |
| Stage 2 | 6.81% | 4.30% |
| Stage 3 | 11.65% | 3.61% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Różańska, A.; Gliwska, E.; Barańska, K.; Maćkowska, S.; Sobol, A.; Spinczyk, D. The Use of Natural Language Processing Elements for Computer-Aided Diagnostics and Monitoring of Body Image Perception in Enterally Fed Patients with Head and Neck or Upper Gastrointestinal Tract Cancers. Cancers 2024, 16, 1353. https://doi.org/10.3390/cancers16071353
Różańska A, Gliwska E, Barańska K, Maćkowska S, Sobol A, Spinczyk D. The Use of Natural Language Processing Elements for Computer-Aided Diagnostics and Monitoring of Body Image Perception in Enterally Fed Patients with Head and Neck or Upper Gastrointestinal Tract Cancers. Cancers. 2024; 16(7):1353. https://doi.org/10.3390/cancers16071353
Chicago/Turabian StyleRóżańska, Agnieszka, Elwira Gliwska, Klaudia Barańska, Stella Maćkowska, Adrianna Sobol, and Dominik Spinczyk. 2024. "The Use of Natural Language Processing Elements for Computer-Aided Diagnostics and Monitoring of Body Image Perception in Enterally Fed Patients with Head and Neck or Upper Gastrointestinal Tract Cancers" Cancers 16, no. 7: 1353. https://doi.org/10.3390/cancers16071353
APA StyleRóżańska, A., Gliwska, E., Barańska, K., Maćkowska, S., Sobol, A., & Spinczyk, D. (2024). The Use of Natural Language Processing Elements for Computer-Aided Diagnostics and Monitoring of Body Image Perception in Enterally Fed Patients with Head and Neck or Upper Gastrointestinal Tract Cancers. Cancers, 16(7), 1353. https://doi.org/10.3390/cancers16071353





