Targeted Nanoparticle-Based Diagnostic and Treatment Options for Pancreatic Cancer
Abstract
Simple Summary
Abstract
1. Introduction
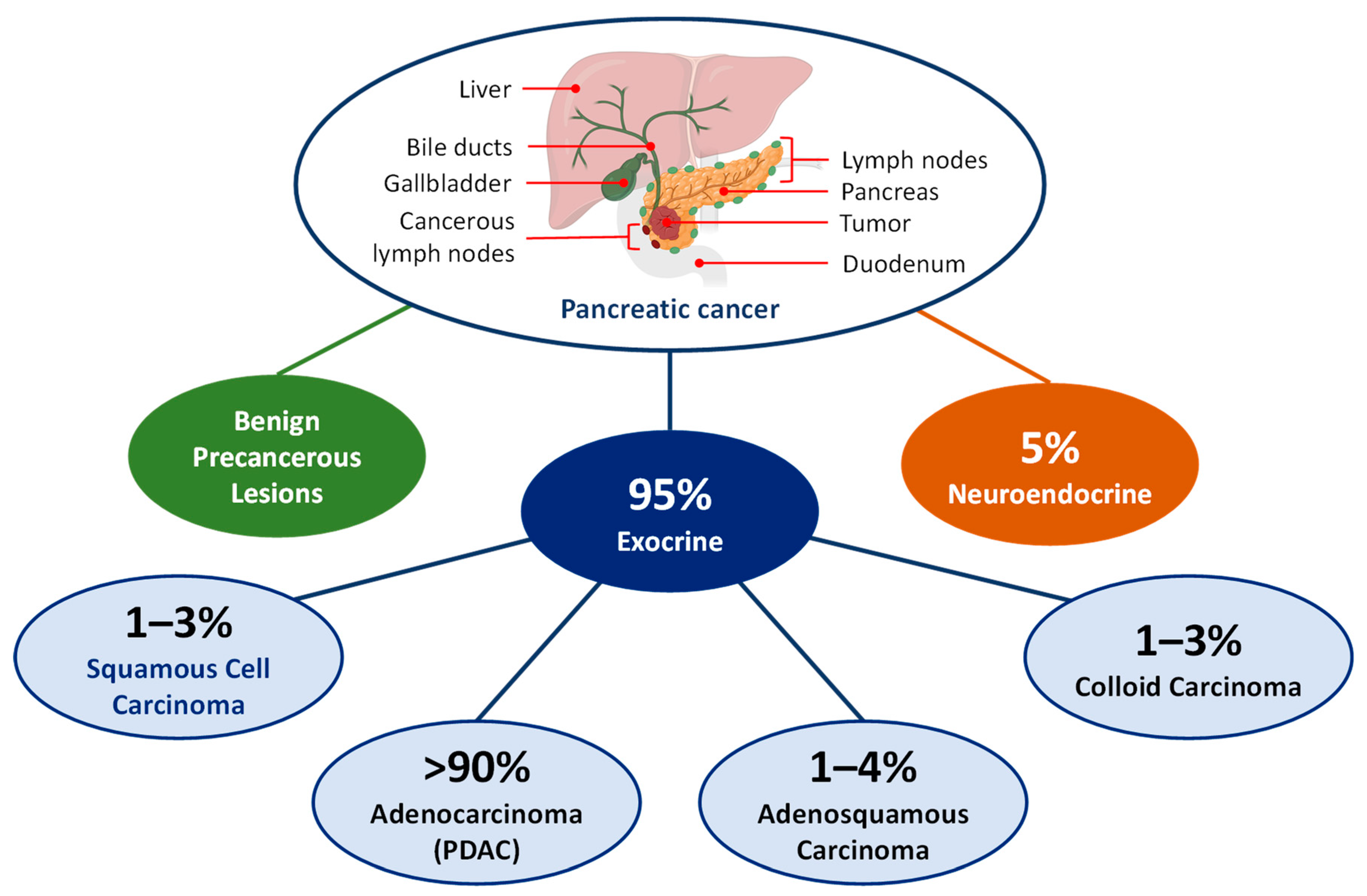
2. Epidemiology and Classification of Pancreatic Cancer
3. Diagnosis and Screening
3.1. Traditional Approaches
3.2. Advancement in Early Diagnosis and Screening
3.3. Extracellular Vesicles (EVs)
3.4. Proteomics
3.5. Circulating Cell-Free DNA and Methylation
3.6. Non-Coding RNA
3.6.1. MicroRNAs (miRNAs)
3.6.2. Long Non-Coding RNAs (LncRNAs)
3.6.3. Circular RNA (CircRNA)
3.6.4. Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR)
3.6.5. Artificial Intelligence (AI)
3.7. Light-Based Pancreatic Cancer Diagnostic Techniques
3.8. Pancreatic Cancer and Microbiome Interaction
3.9. Nanoparticles as Molecular Imaging Agents
3.10. Benefits and Drawbacks of the Pancreatic Cancer Diagnostic Approaches
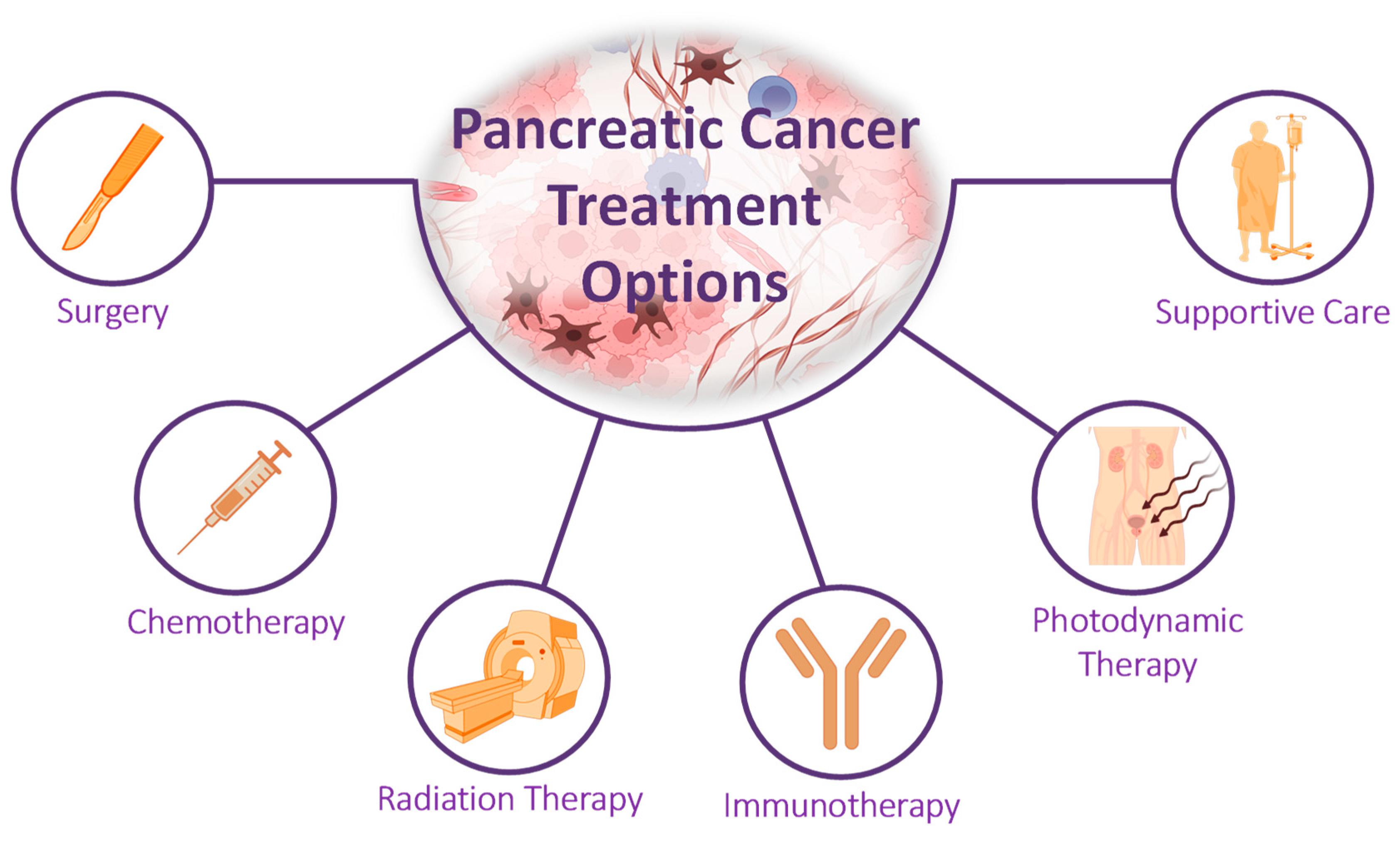
4. Treatment Options for Pancreatic Cancer
5. Targeted Mechanisms and Pathways
5.1. Targeting DNA Repairing
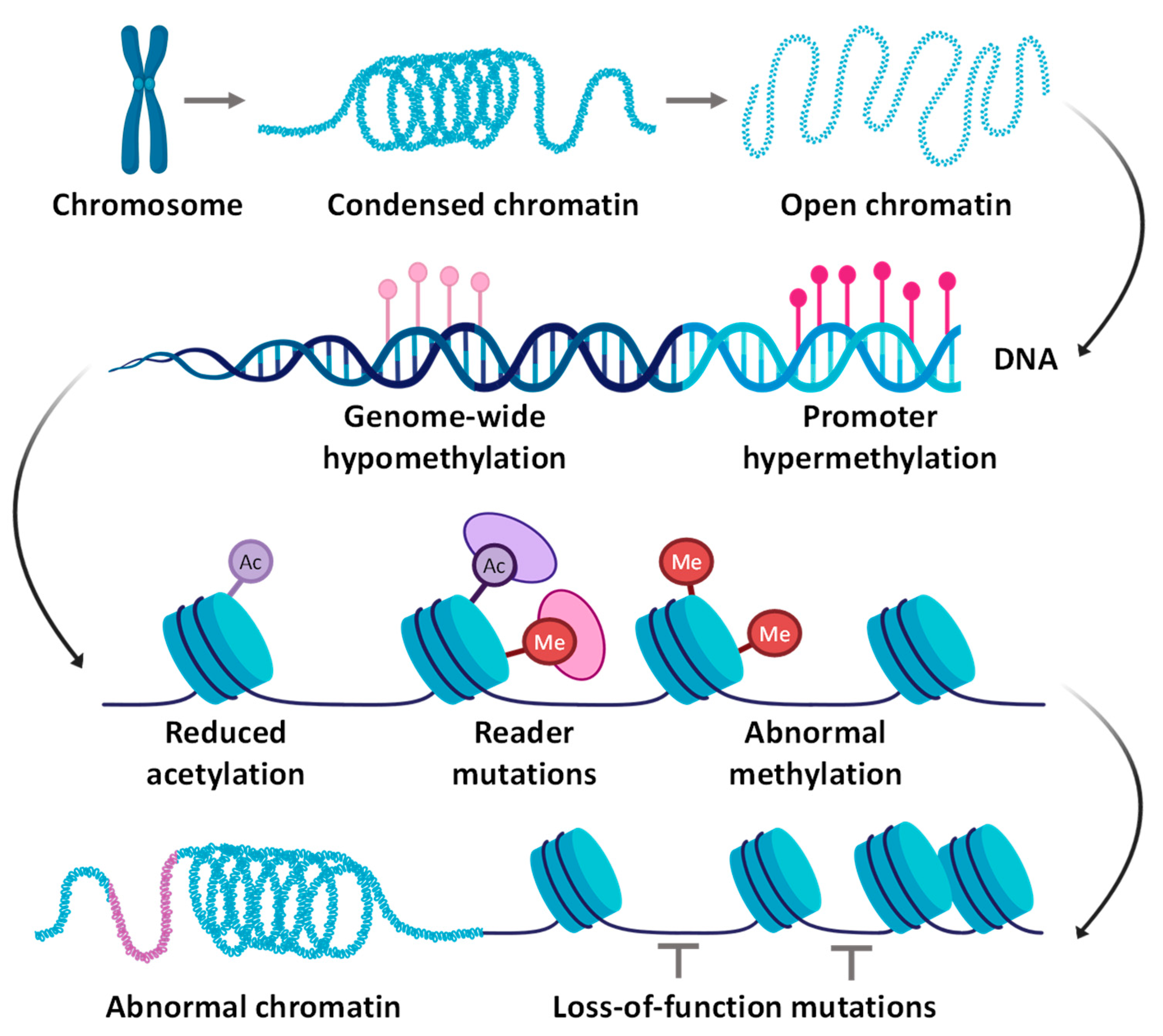
5.2. Targeting Epigenetic Alterations
5.3. Targeting Key Signaling Pathways
5.4. Targeting the Tumor Microenvironment and Related Metabolic Reprogramming
5.5. Targeting Immune Regulatory Networks
5.5.1. Tumor-Associated Macrophages (TAMs)
5.5.2. Myeloid-Derived Suppressor Cells (MDSCs)
5.5.3. Neutrophils
5.5.4. Regulatory T Cells (Tregs)
- Immunotherapy: Immunotherapy involves using agents that stimulate or modulate the immune system to recognize and attack cancer cells. By blocking the inhibitory signals cancer cells use to evade the immune system, checkpoint inhibitors, such as anti-PD-1 and anti-CTLA-4 antibodies, have shown promise in treating advanced pancreatic cancers.
- Combination Therapies: Combining immunotherapy with chemotherapy, radiation therapy, or targeted therapies enhances the immune response against tumors and improves patient outcomes.
- Targeting Immunosuppressive Cell Populations: Strategies for inhibiting or depleting immune suppressive cell populations, such as TAMs, MDSCs, neutrophils, and Tregs, have been developed and verified in clinical trials.
- Immunomodulatory Agents: The use of immunomodulatory agents, such as cytokines and costimulatory molecules, is being explored as a potential treatment for pancreatic cancer to enhance the immune system’s antitumor activity.
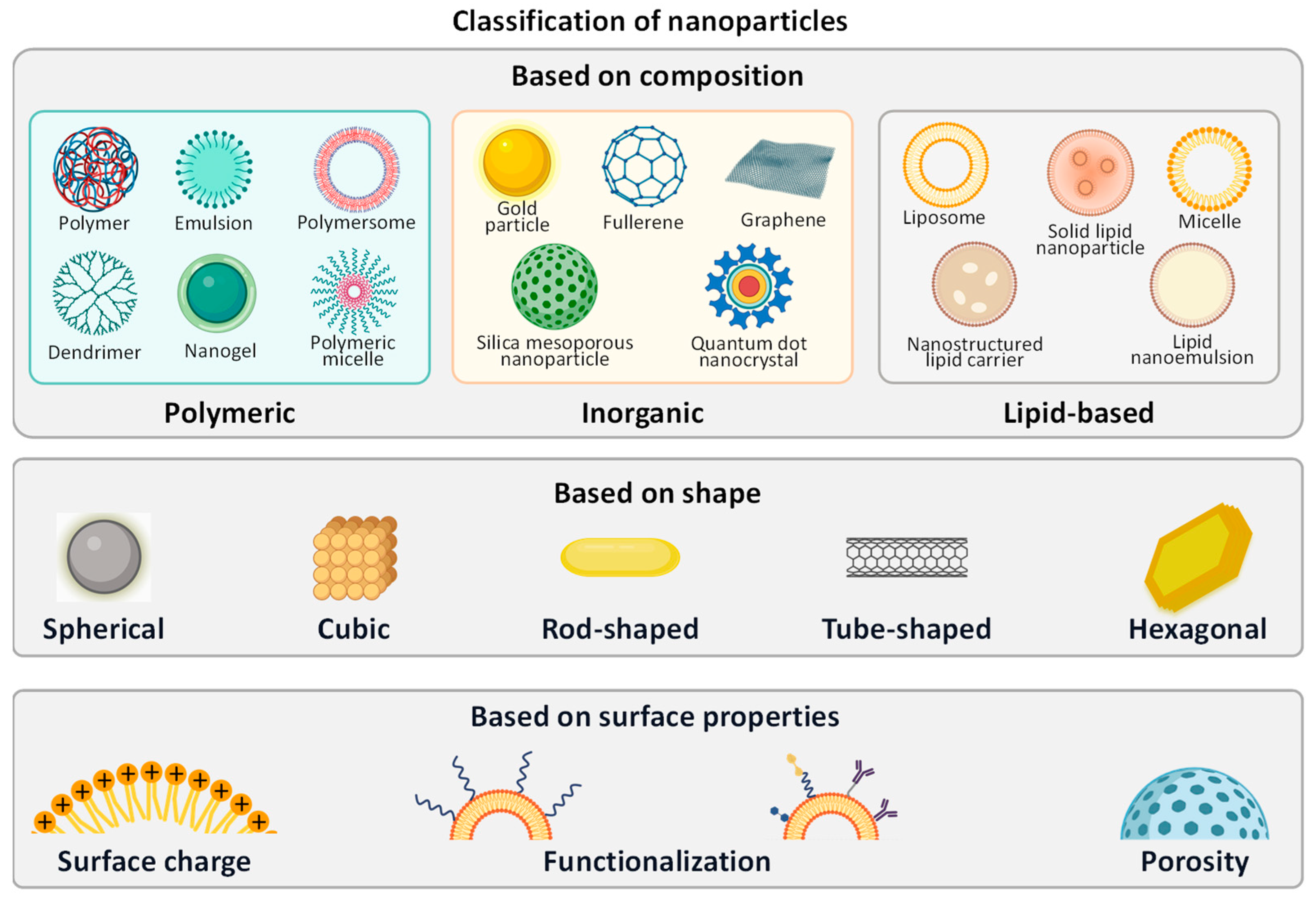
6. Nanotechnology Approaches for Treating Pancreatic Cancer
6.1. Nanoparticles
6.2. Lipid-Based Nanoparticles
6.2.1. Liposomes
6.2.2. Solid Lipid Nanoparticles
6.2.3. Nanostructure Lipid Carriers
6.2.4. Lipid–Polymer Hybrid Nanoparticles
6.3. Polymeric Nanoparticles
6.3.1. Dendrimers
6.3.2. Nanospheres
6.4. Metal Nanoparticles
6.5. Magnetic Nanoparticles
6.6. Cancer Targeting
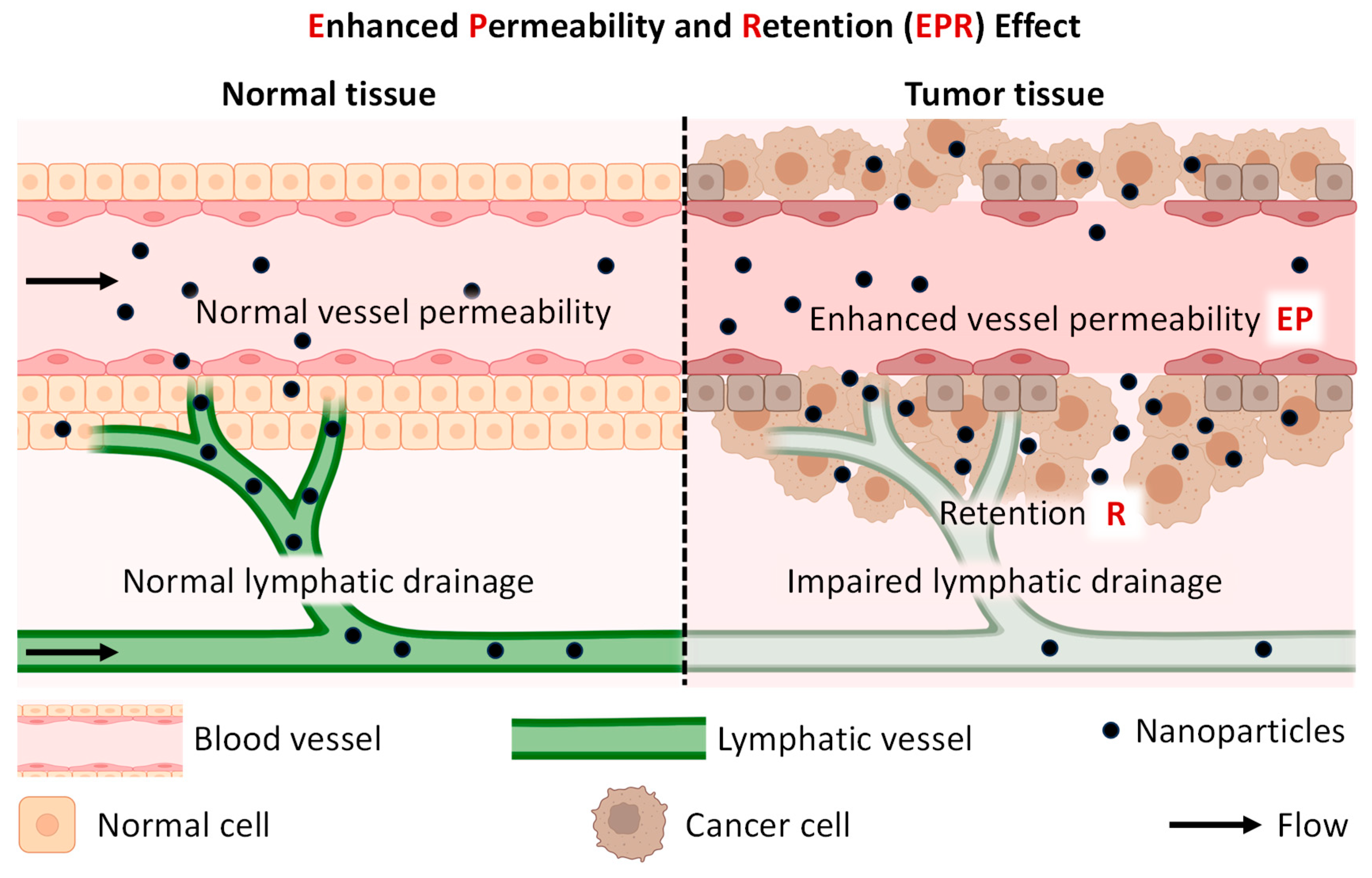
6.6.1. Enhanced Permeability and Retention (EPR) Effect
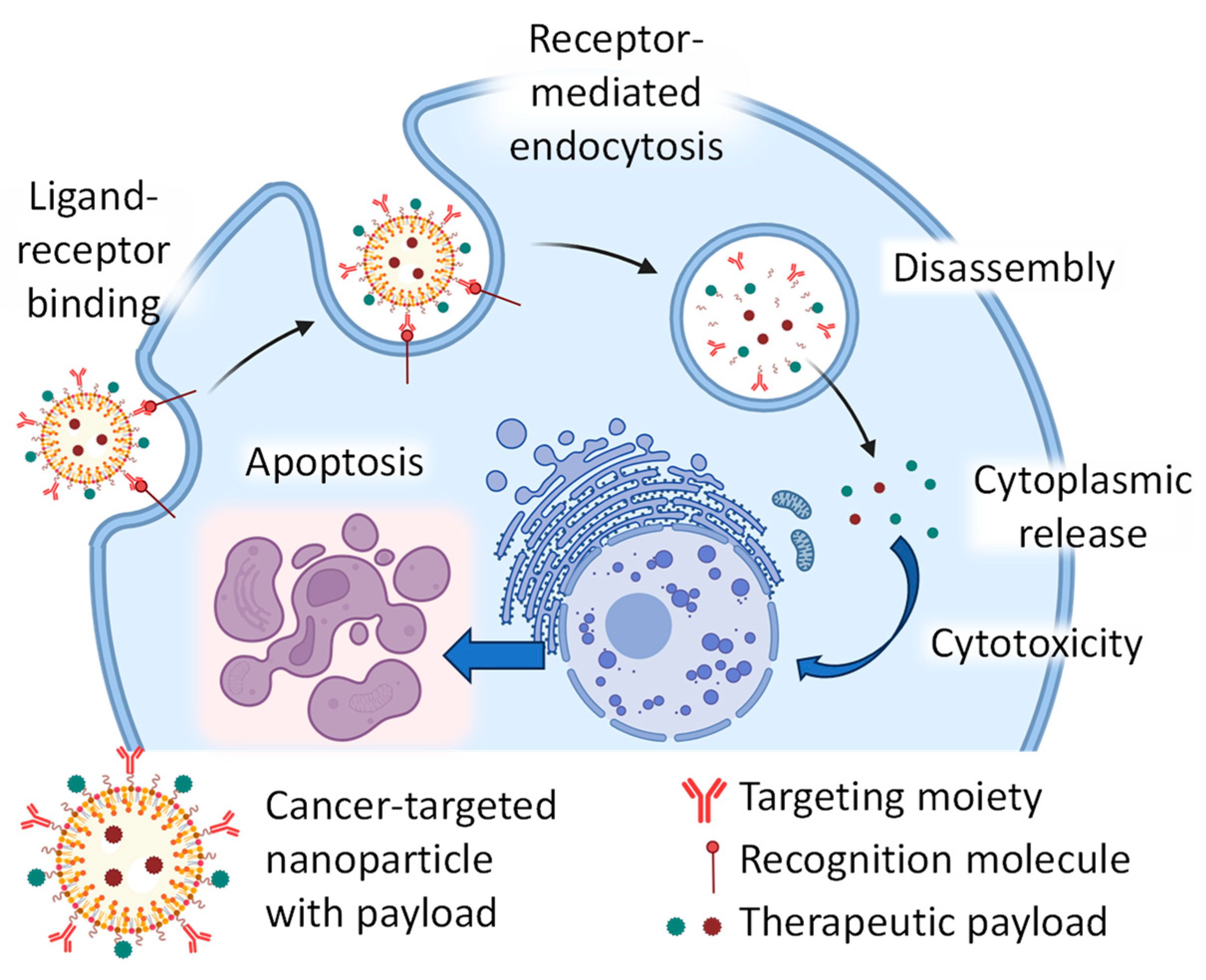
6.6.2. Active Targeting
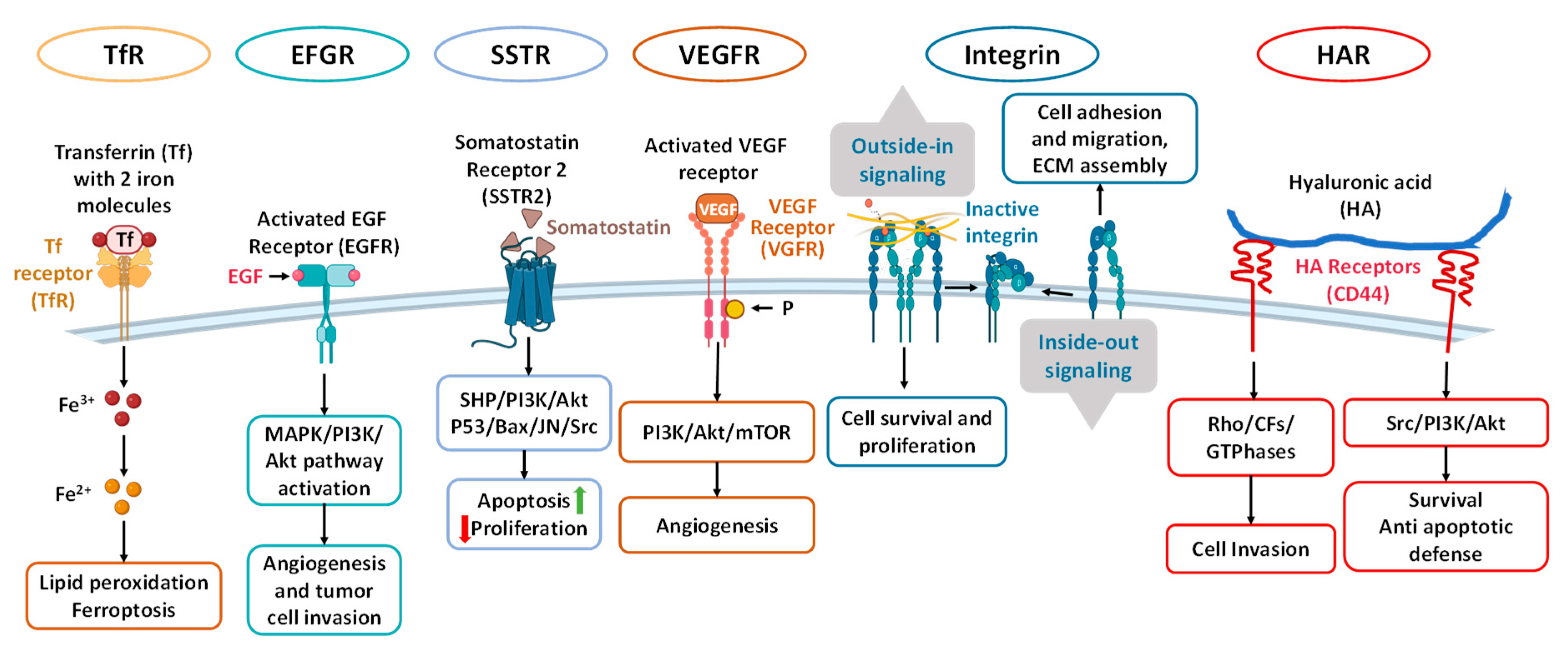
6.7. Potential Recognition Molecules for Targeted Therapy of Pancreatic Cancer
6.7.1. Transferrin Receptor (TfR)
6.7.2. Epidermal Growth Factor Receptor (EGFR)
6.7.3. Somatostatin Recept 6.6 or 2 (SSTR2)
6.7.4. Vascular Endothelial Growth Factor Receptor (VEGFR)
6.7.5. Integrin
6.7.6. Hyaluronic Acid Receptors
6.8. Nanoparticle-Based Drugs in Clinical Trials
7. Conclusions and Future Perspectives
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Cancer Society, Inc. Cancer Facts & Figures 2023; American Cancer Society, Inc.: Atlanta, GA, USA, 2022; pp. 1–82. [Google Scholar]
- Olajubutu, O.; Ogundipe, O.D.; Adebayo, A.; Adesina, S.K. Drug Delivery Strategies for the Treatment of Pancreatic Cancer. Pharmaceutics 2023, 15, 1318. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fiore, M.; Coppola, A.; Petrianni, G.M.; Trecca, P.; D’Ercole, G.; Cimini, P.; Ippolito, E.; Caputo, D.; Beomonte Zobel, B.; Coppola, R.; et al. Advances in pre-treatment evaluation of pancreatic ductal adenocarcinoma: A narrative review. J. Gastrointest. Oncol. 2023, 14, 1114–1130. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Halle-Smith, J.M.; Powell-Brett, S.F.; Hall, L.A.; Duggan, S.N.; Griffin, O.; Phillips, M.E.; Roberts, K.J. Recent Advances in Pancreatic Ductal Adenocarcinoma: Strategies to Optimise the Perioperative Nutritional Status in Pancreatoduodenectomy Patients. Cancers 2023, 15, 2466. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- de Jesus, V.H.F.; Riechelmann, R.P. Current Treatment of Potentially Resectable Pancreatic Ductal Adenocarcinoma: A Medical Oncologist’s Perspective. Cancer Control 2023, 30, 10732748231173212. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Perez-Diez, I.; Andreu, Z.; Hidalgo, M.R.; Perpina-Clerigues, C.; Fantin, L.; Fernandez-Serra, A.; de la Iglesia-Vaya, M.; Lopez-Guerrero, J.A.; Garcia-Garcia, F. A Comprehensive Transcriptional Signature in Pancreatic Ductal Adenocarcinoma Reveals New Insights into the Immune and Desmoplastic Microenvironments. Cancers 2023, 15, 2887. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yang, J.; Liu, Y.; Liu, S. The role of epithelial-mesenchymal transition and autophagy in pancreatic ductal adenocarcinoma invasion. Cell Death Dis. 2023, 14, 506. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ansari, D.; Friess, H.; Bauden, M.; Samnegard, J.; Andersson, R. Pancreatic cancer: Disease dynamics, tumor biology and the role of the microenvironment. Oncotarget 2018, 9, 6644–6651. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gildiz, S.; Minko, T. Nanotechnology-Based Nucleic Acid Vaccines for Treatment of Ovarian Cancer. Pharm. Res. 2023, 40, 123–144. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lee, D.; Minko, T. Nanotherapeutics for Nose-to-Brain Drug Delivery: An Approach to Bypass the Blood Brain Barrier. Pharmaceutics 2021, 13, 2049. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Li, X.; Taratula, O.; Taratula, O.; Schumann, C.; Minko, T. LHRH-Targeted Drug Delivery Systems for Cancer Therapy. Mini Rev. Med. Chem. 2017, 17, 258–267. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Majumder, J.; Minko, T. Multifunctional and stimuli-responsive nanocarriers for targeted therapeutic delivery. Expert Opin. Drug Deliv. 2021, 18, 205–227. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Majumder, J.; Minko, T. Targeted Nanotherapeutics for Respiratory Diseases: Cancer, Fibrosis, and Coronavirus. Adv. Ther. 2021, 4, 2000203. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Majumder, J.; Minko, T. Recent Developments on Therapeutic and Diagnostic Approaches for COVID-19. AAPS J. 2021, 23, 14. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pozharov, V.P.; Minko, T. Nanotechnology-Based RNA Vaccines: Fundamentals, Advantages and Challenges. Pharmaceutics 2023, 15, 194. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Savla, R.; Minko, T. Nanoparticle design considerations for molecular imaging of apoptosis: Diagnostic, prognostic, and therapeutic value. Adv. Drug Deliv. Rev. 2017, 113, 122–140. [Google Scholar] [CrossRef] [PubMed]
- Khare, V.; Alam, N.; Saneja, A.; Dubey, R.D.; Gupta, P.N. Targeted drug delivery systems for pancreatic cancer. J. Biomed. Nanotechnol. 2014, 10, 3462–3482. [Google Scholar] [CrossRef] [PubMed]
- Nedaeinia, R.; Avan, A.; Manian, M.; Salehi, R.; Ghayour-Mobarhan, M. EGFR as a potential target for the treatment of pancreatic cancer: Dilemma and controversies. Curr. Drug Targets 2014, 15, 1293–1301. [Google Scholar] [CrossRef] [PubMed]
- Sato, N.; Cheng, X.B.; Kohi, S.; Koga, A.; Hirata, K. Targeting hyaluronan for the treatment of pancreatic ductal adenocarcinoma. Acta Pharm. Sin. B 2016, 6, 101–105. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jiang, H.; Wang, S.; Zhou, X.; Wang, L.; Ye, L.; Zhou, Z.; Tang, J.; Liu, X.; Teng, L.; Shen, Y. New path to treating pancreatic cancer: TRAIL gene delivery targeting the fibroblast-enriched tumor microenvironment. J. Control. Release 2018, 286, 254–263. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Shi, Y.; Qian, F. Opportunities and delusions regarding drug delivery targeting pancreatic cancer-associated fibroblasts. Adv. Drug Deliv. Rev. 2021, 172, 37–51. [Google Scholar] [CrossRef] [PubMed]
- Murata, M.; Narahara, S.; Kawano, T.; Hamano, N.; Piao, J.S.; Kang, J.H.; Ohuchida, K.; Murakami, T.; Hashizume, M. Design and Function of Engineered Protein Nanocages as a Drug Delivery System for Targeting Pancreatic Cancer Cells via Neuropilin-1. Mol. Pharm. 2015, 12, 1422–1430. [Google Scholar] [CrossRef] [PubMed]
- Taniuchi, K.; Yawata, T.; Tsuboi, M.; Ueba, T.; Saibara, T. Efficient delivery of small interfering RNAs targeting particular mRNAs into pancreatic cancer cells inhibits invasiveness and metastasis of pancreatic tumors. Oncotarget 2019, 10, 2869–2886. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yoshida, M.; Takimoto, R.; Murase, K.; Sato, Y.; Hirakawa, M.; Tamura, F.; Sato, T.; Iyama, S.; Osuga, T.; Miyanishi, K.; et al. Targeting anticancer drug delivery to pancreatic cancer cells using a fucose-bound nanoparticle approach. PLoS ONE 2012, 7, e39545. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Liu, Y.; Wu, W.; Wang, Y.; Han, S.; Yuan, Y.; Huang, J.; Shuai, X.; Peng, Z. Recent development of gene therapy for pancreatic cancer using non-viral nanovectors. Biomater. Sci. 2021, 9, 6673–6690. [Google Scholar] [CrossRef] [PubMed]
- Minko, T.; Dharap, S.S.; Fabbricatore, A.T. Enhancing the efficacy of chemotherapeutic drugs by the suppression of antiapoptotic cellular defense. Cancer Detect. Prev. 2003, 27, 193–202. [Google Scholar] [CrossRef] [PubMed]
- Kokkinos, J.; Ignacio, R.M.C.; Sharbeen, G.; Boyer, C.; Gonzales-Aloy, E.; Goldstein, D.; Australian Pancreatic Cancer Genome Initiative (APGI); McCarroll, J.A.; Phillips, P.A. Targeting the undruggable in pancreatic cancer using nano-based gene silencing drugs. Biomaterials 2020, 240, 119742. [Google Scholar] [CrossRef] [PubMed]
- Frampton, J.E. Liposomal Irinotecan: A Review in Metastatic Pancreatic Adenocarcinoma. Drugs 2020, 80, 1007–1018. [Google Scholar] [CrossRef] [PubMed]
- De Luca, R.; Blasi, L.; Alu, M.; Gristina, V.; Cicero, G. Clinical efficacy of nab-paclitaxel in patients with metastatic pancreatic cancer. Drug Des. Devel. Ther. 2018, 12, 1769–1775. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hidalgo, M. Pancreatic cancer. N. Engl. J. Med. 2010, 362, 1605–1617. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Xie, K.; Wolff, R.; Abbruzzese, J.L. Pancreatic cancer. Lancet 2004, 363, 1049–1057. [Google Scholar] [CrossRef] [PubMed]
- Rawla, P.; Sunkara, T.; Gaduputi, V. Epidemiology of Pancreatic Cancer: Global Trends, Etiology and Risk Factors. World J. Oncol. 2019, 10, 10–27. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lynch, S.M.; Vrieling, A.; Lubin, J.H.; Kraft, P.; Mendelsohn, J.B.; Hartge, P.; Canzian, F.; Steplowski, E.; Arslan, A.A.; Gross, M.; et al. Cigarette smoking and pancreatic cancer: A pooled analysis from the pancreatic cancer cohort consortium. Am. J. Epidemiol. 2009, 170, 403–413. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vincent, A.; Herman, J.; Schulick, R.; Hruban, R.H.; Goggins, M. Pancreatic cancer. Lancet 2011, 378, 607–620. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pancreatic Cancer Types. Available online: https://www.hopkinsmedicine.org/health/conditions-and-diseases/pancreatic-cancer/pancreatic-cancer-types#:~:text=Pancreatic%20cancer%20types%20can%20be,in%20their%20symptoms%20and%20prognosis (accessed on 25 December 2023).
- Yachida, S.; Jones, S.; Bozic, I.; Antal, T.; Leary, R.; Fu, B.; Kamiyama, M.; Hruban, R.H.; Eshleman, J.R.; Nowak, M.A.; et al. Distant metastasis occurs late during the genetic evolution of pancreatic cancer. Nature 2010, 467, 1114–1117. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang, L.; Sanagapalli, S.; Stoita, A. Challenges in diagnosis of pancreatic cancer. World J. Gastroenterol. 2018, 24, 2047–2060. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yang, J.; Xu, R.; Wang, C.; Qiu, J.; Ren, B.; You, L. Early screening and diagnosis strategies of pancreatic cancer: A comprehensive review. Cancer Commun. 2021, 41, 1257–1274. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Janga, L.S.N.; Sambe, H.G.; Yasir, M.; Man, R.K.; Gogikar, A.; Nanda, A.; Mohammed, L. Holistic Understanding of the Role of Carbohydrate Antigen 19-9 in Pancreatic Cancer Screening, Early Diagnosis, and Prognosis: A Systematic Review. Cureus 2023, 15, e44382. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhao, B.; Zhao, B.; Chen, F. Diagnostic value of serum carbohydrate antigen 19-9 in pancreatic cancer: A systematic review and meta-analysis. Eur. J. Gastroenterol. Hepatol. 2022, 34, 891–904. [Google Scholar] [CrossRef] [PubMed]
- Luo, G.; Fan, Z.; Cheng, H.; Jin, K.; Guo, M.; Lu, Y.; Yang, C.; Fan, K.; Huang, Q.; Long, J.; et al. New observations on the utility of CA19-9 as a biomarker in Lewis negative patients with pancreatic cancer. Pancreatology 2018, 18, 971–976. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Ou, S.; Zhang, H.; Huang, R.; Yu, S.; Zhao, M.; Tai, S. Advances in biomarkers and techniques for pancreatic cancer diagnosis. Cancer Cell Int. 2022, 22, 220. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wu, Z.; Kuntz, A.I.; Wadleigh, R.G. CA 19-9 tumor marker: Is it reliable? A case report in a patient with pancreatic cancer. Clin. Adv. Hematol. Oncol. 2013, 11, 50–52. [Google Scholar] [PubMed]
- Ermiah, E.; Eddfair, M.; Abdulrahman, O.; Elfagieh, M.; Jebriel, A.; Al-Sharif, M.; Assidi, M.; Buhmeida, A. Prognostic value of serum CEA and CA19-9 levels in pancreatic ductal adenocarcinoma. Mol. Clin. Oncol. 2022, 17, 126. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Meng, Q.; Shi, S.; Liang, C.; Liang, D.; Xu, W.; Ji, S.; Zhang, B.; Ni, Q.; Xu, J.; Yu, X. Diagnostic and prognostic value of carcinoembryonic antigen in pancreatic cancer: A systematic review and meta-analysis. OncoTargets Ther. 2017, 10, 4591–4598. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ruckert, F.; Pilarsky, C.; Grutzmann, R. Serum tumor markers in pancreatic cancer-recent discoveries. Cancers 2010, 2, 1107. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Alqualo, N.O.; Campos-Fernandez, E.; Picolo, B.U.; Ferreira, E.L.; Henriques, L.M.; Lorenti, S.; Moreira, D.C.; Simiao, M.P.S.; Oliveira, L.B.T.; Alonso-Goulart, V. Molecular biomarkers in prostate cancer tumorigenesis and clinical relevance. Crit. Rev. Oncol. Hematol. 2023, 194, 104232. [Google Scholar] [CrossRef] [PubMed]
- Davoudi, F.; Moradi, A.; Becker, T.M.; Lock, J.G.; Abbey, B.; Fontanarosa, D.; Haworth, A.; Clements, J.; Ecker, R.C.; Batra, J. Genomic and Phenotypic Biomarkers for Precision Medicine Guidance in Advanced Prostate Cancer. Curr. Treat. Options Oncol. 2023, 24, 1451–1471. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kawada, T.; Shim, S.R.; Quhal, F.; Rajwa, P.; Pradere, B.; Yanagisawa, T.; Bekku, K.; Laukhtina, E.; von Deimling, M.; Teoh, J.Y.; et al. Diagnostic Accuracy of Liquid Biomarkers for Clinically Significant Prostate Cancer Detection: A Systematic Review and Diagnostic Meta-analysis of Multiple Thresholds. Eur. Urol. Oncol. 2023; in press. [Google Scholar] [CrossRef] [PubMed]
- Kielb, P.; Kowalczyk, K.; Gurwin, A.; Nowak, L.; Krajewski, W.; Sosnowski, R.; Szydelko, T.; Malkiewicz, B. Novel Histopathological Biomarkers in Prostate Cancer: Implications and Perspectives. Biomedicines 2023, 11, 1552. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Elbanna, K.Y.; Jang, H.J.; Kim, T.K. Imaging diagnosis and staging of pancreatic ductal adenocarcinoma: A comprehensive review. Insights Imaging 2020, 11, 58. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Costache, M.I.; Costache, C.A.; Dumitrescu, C.I.; Tica, A.A.; Popescu, M.; Baluta, E.A.; Anghel, A.C.; Saftoiu, A.; Dumitrescu, D. Which is the Best Imaging Method in Pancreatic Adenocarcinoma Diagnosis and Staging—CT, MRI or EUS? Curr. Health Sci. J. 2017, 43, 132–136. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Toft, J.; Hadden, W.J.; Laurence, J.M.; Lam, V.; Yuen, L.; Janssen, A.; Pleass, H. Imaging modalities in the diagnosis of pancreatic adenocarcinoma: A systematic review and meta-analysis of sensitivity, specificity and diagnostic accuracy. Eur. J. Radiol. 2017, 92, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Benhammou, J.N.; Ghassemi, K.; Kim, S.; Sedarat, A.; Farrell, J.; Pisegna, J.R. Endoscopic Ultrasound-Guided Fine Needle Aspiration Accurately Diagnoses Smaller Pancreatic Neuroendocrine Tumors Compared to Computer Tomography-Guided Fine Needle Aspiration. J. Gastroenterol. Pancreatol. Liver Disord. 2017, 4, 1–7. [Google Scholar] [CrossRef] [PubMed] [PubMed Central][Green Version]
- Chen, J.; Yang, R.; Lu, Y.; Xia, Y.; Zhou, H. Diagnostic accuracy of endoscopic ultrasound-guided fine-needle aspiration for solid pancreatic lesion: A systematic review. J. Cancer Res. Clin. Oncol. 2012, 138, 1433–1441. [Google Scholar] [CrossRef] [PubMed]
- Gheorghe, G.; Bungau, S.; Ilie, M.; Behl, T.; Vesa, C.M.; Brisc, C.; Bacalbasa, N.; Turi, V.; Costache, R.S.; Diaconu, C.C. Early Diagnosis of Pancreatic Cancer: The Key for Survival. Diagnostics 2020, 10, 869. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Buenafe, A.C.; Dorrell, C.; Reddy, A.P.; Klimek, J.; Marks, D.L. Proteomic analysis distinguishes extracellular vesicles produced by cancerous versus healthy pancreatic organoids. Sci. Rep. 2022, 12, 3556. [Google Scholar] [CrossRef] [PubMed]
- Fang, X.; Lan, H.; Jin, K.; Qian, J. Pancreatic cancer and exosomes: Role in progression, diagnosis, monitoring, and treatment. Front. Oncol. 2023, 13, 1149551. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hinestrosa, J.P.; Kurzrock, R.; Lewis, J.M.; Schork, N.J.; Schroeder, G.; Kamat, A.M.; Lowy, A.M.; Eskander, R.N.; Perrera, O.; Searson, D.; et al. Early-stage multi-cancer detection using an extracellular vesicle protein-based blood test. Commun. Med. 2022, 2, 29. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sogawa, K.; Takano, S.; Iida, F.; Satoh, M.; Tsuchida, S.; Kawashima, Y.; Yoshitomi, H.; Sanda, A.; Kodera, Y.; Takizawa, H.; et al. Identification of a novel serum biomarker for pancreatic cancer, C4b-binding protein alpha-chain (C4BPA) by quantitative proteomic analysis using tandem mass tags. Br. J. Cancer 2016, 115, 949–956. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yang, J.; Zhang, Y.; Gao, X.; Yuan, Y.; Zhao, J.; Zhou, S.; Wang, H.; Wang, L.; Xu, G.; Li, X.; et al. Plasma-Derived Exosomal ALIX as a Novel Biomarker for Diagnosis and Classification of Pancreatic Cancer. Front. Oncol. 2021, 11, 628346. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wu, X.; Zhang, Z.X.; Chen, X.Y.; Xu, Y.L.; Yin, N.; Yang, J.; Zhu, D.M.; Li, D.C.; Zhou, J. A Panel of Three Biomarkers Identified by iTRAQ for the Early Diagnosis of Pancreatic Cancer. Proteom. Clin. Appl. 2019, 13, e1800195. [Google Scholar] [CrossRef] [PubMed]
- Jia, K.; Zhao, X.; Dang, X. Mass spectrometry-based iTRAQ analysis of serum markers in patients with pancreatic cancer. Oncol. Lett. 2020, 19, 4106–4114. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yoshioka, Y.; Shimomura, M.; Saito, K.; Ishii, H.; Doki, Y.; Eguchi, H.; Nakatsura, T.; Itoi, T.; Kuroda, M.; Mori, M.; et al. Circulating cancer-associated extracellular vesicles as early detection and recurrence biomarkers for pancreatic cancer. Cancer Sci. 2022, 113, 3498–3509. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Liggett, T.; Melnikov, A.; Yi, Q.L.; Replogle, C.; Brand, R.; Kaul, K.; Talamonti, M.; Abrams, R.A.; Levenson, V. Differential methylation of cell-free circulating DNA among patients with pancreatic cancer versus chronic pancreatitis. Cancer 2010, 116, 1674–1680. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, B.; Chakrabarty, M.; Cohn, E.M.; Leon, S.A. Determination of circulating DNA levels in patients with benign or malignant gastrointestinal disease. Cancer 1983, 51, 2116–2120. [Google Scholar] [CrossRef] [PubMed]
- Sun, K.; Jiang, P.; Chan, K.C.; Wong, J.; Cheng, Y.K.; Liang, R.H.; Chan, W.K.; Ma, E.S.; Chan, S.L.; Cheng, S.H.; et al. Plasma DNA tissue mapping by genome-wide methylation sequencing for noninvasive prenatal, cancer, and transplantation assessments. Proc. Natl. Acad. Sci. USA 2015, 112, E5503–E5512. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Leon, S.A.; Shapiro, B.; Sklaroff, D.M.; Yaros, M.J. Free DNA in the serum of cancer patients and the effect of therapy. Cancer Res. 1977, 37, 646–650. [Google Scholar] [PubMed]
- Thierry, A.R.; El Messaoudi, S.; Gahan, P.B.; Anker, P.; Stroun, M. Origins, structures, and functions of circulating DNA in oncology. Cancer Metastasis Rev. 2016, 35, 347–376. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chan, K.C.; Jiang, P.; Chan, C.W.; Sun, K.; Wong, J.; Hui, E.P.; Chan, S.L.; Chan, W.C.; Hui, D.S.; Ng, S.S.; et al. Noninvasive detection of cancer-associated genome-wide hypomethylation and copy number aberrations by plasma DNA bisulfite sequencing. Proc. Natl. Acad. Sci. USA 2013, 110, 18761–18768. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wan, J.C.M.; Massie, C.; Garcia-Corbacho, J.; Mouliere, F.; Brenton, J.D.; Caldas, C.; Pacey, S.; Baird, R.; Rosenfeld, N. Liquid biopsies come of age: Towards implementation of circulating tumour DNA. Nat. Rev. Cancer 2017, 17, 223–238. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, Y.; Shitara, K. Development of circulating tumour DNA analysis for gastrointestinal cancers. ESMO Open 2020, 5 (Suppl. S1), e000600. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sorenson, G.D.; Pribish, D.M.; Valone, F.H.; Memoli, V.A.; Bzik, D.J.; Yao, S.L. Soluble normal and mutated DNA sequences from single-copy genes in human blood. Cancer Epidemiol. Biomarkers Prev. 1994, 3, 67–71. [Google Scholar] [PubMed]
- Brychta, N.; Krahn, T.; von Ahsen, O. Detection of KRAS Mutations in Circulating Tumor DNA by Digital PCR in Early Stages of Pancreatic Cancer. Clin. Chem. 2016, 62, 1482–1491. [Google Scholar] [CrossRef] [PubMed]
- Botrus, G.; Fu, Y.; Sonbol, M.B.; Drusbosky, L.; Ahn, D.H.; Borad, M.J.; Starr, J.S.; Jones, J.C.; Raman, P.; Mody, K.; et al. Serial cell-free DNA (cfDNA) sampling in advanced pancreatic ductal adenocarcinoma (PDAC) patients may predict therapeutic outcome. J. Clin. Oncol. 2021, 39 (Suppl. S3), 423. [Google Scholar] [CrossRef]
- Dianxu, F.; Shengdao, Z.; Tianquan, H.; Yu, J.; Ruoqing, L.; Zurong, Y.; Xuezhi, W. A prospective study of detection of pancreatic carcinoma by combined plasma K-ras mutations and serum CA19-9 analysis. Pancreas 2002, 25, 336–341. [Google Scholar] [CrossRef] [PubMed]
- Sausen, M.; Phallen, J.; Adleff, V.; Jones, S.; Leary, R.J.; Barrett, M.T.; Anagnostou, V.; Parpart-Li, S.; Murphy, D.; Kay Li, Q.; et al. Clinical implications of genomic alterations in the tumour and circulation of pancreatic cancer patients. Nat. Commun. 2015, 6, 7686. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Liu, X.; Liu, L.; Ji, Y.; Li, C.; Wei, T.; Yang, X.; Zhang, Y.; Cai, X.; Gao, Y.; Xu, W.; et al. Enrichment of short mutant cell-free DNA fragments enhanced detection of pancreatic cancer. EBioMedicine 2019, 41, 345–356. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhao, Y.; Yang, M.; Wang, S.; Abbas, S.J.; Zhang, J.; Li, Y.; Shao, R.; Liu, Y. An Overview of Epigenetic Methylation in Pancreatic Cancer Progression. Front. Oncol. 2022, 12, 854773. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Natale, F.; Vivo, M.; Falco, G.; Angrisano, T. Deciphering DNA methylation signatures of pancreatic cancer and pancreatitis. Clin. Epigenetics 2019, 11, 132. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yi, J.M.; Guzzetta, A.A.; Bailey, V.J.; Downing, S.R.; Van Neste, L.; Chiappinelli, K.B.; Keeley, B.P.; Stark, A.; Herrera, A.; Wolfgang, C.; et al. Novel methylation biomarker panel for the early detection of pancreatic cancer. Clin. Cancer Res. 2013, 19, 6544–6555. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Eissa, M.A.L.; Lerner, L.; Abdelfatah, E.; Shankar, N.; Canner, J.K.; Hasan, N.M.; Yaghoobi, V.; Huang, B.; Kerner, Z.; Takaesu, F.; et al. Promoter methylation of ADAMTS1 and BNC1 as potential biomarkers for early detection of pancreatic cancer in blood. Clin. Epigenetics 2019, 11, 59. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ying, L.; Sharma, A.; Chhoda, A.; Ruzgar, N.; Hasan, N.; Kwak, R.; Wolfgang, C.L.; Wang, T.H.; Kunstman, J.W.; Salem, R.R.; et al. Methylation-based Cell-free DNA Signature for Early Detection of Pancreatic Cancer. Pancreas 2021, 50, 1267–1273. [Google Scholar] [CrossRef] [PubMed]
- Shinjo, K.; Hara, K.; Nagae, G.; Umeda, T.; Katsushima, K.; Suzuki, M.; Murofushi, Y.; Umezu, Y.; Takeuchi, I.; Takahashi, S.; et al. A novel sensitive detection method for DNA methylation in circulating free DNA of pancreatic cancer. PLoS ONE 2020, 15, e0233782. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- García-Ortiz, M.V.; Cano-Ramírez, P.; Toledano-Fonseca, M.; Cano, M.T.; Inga-Saavedra, E.; Rodríguez-Alonso, R.M.; Guil-Luna, S.; Gómez-España, M.A.; Rodríguez-Ariza, A.; Aranda, E. Circulating NPTX2 methylation as a non-invasive biomarker for prognosis and monitoring of metastatic pancreatic cancer. Clin. Epigenetics 2023, 15, 118. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lv, Y.; Huang, S. Role of non-coding RNA in pancreatic cancer. Oncol. Lett. 2019, 18, 3963–3973. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Li, Y.; Al Hallak, M.N.; Philip, P.A.; Azmi, A.S.; Mohammad, R.M. Non-Coding RNAs in Pancreatic Cancer Diagnostics and Therapy: Focus on lncRNAs, circRNAs, and piRNAs. Cancers 2021, 13, 4161. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Macfarlane, L.A.; Murphy, P.R. MicroRNA: Biogenesis, Function and Role in Cancer. Curr. Genom. 2010, 11, 537–561. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kojima, M.; Sudo, H.; Kawauchi, J.; Takizawa, S.; Kondou, S.; Nobumasa, H.; Ochiai, A. MicroRNA markers for the diagnosis of pancreatic and biliary-tract cancers. PLoS ONE 2015, 10, e0118220. [Google Scholar] [CrossRef] [PubMed]
- Habbe, N.; Koorstra, J.B.; Mendell, J.T.; Offerhaus, G.J.; Ryu, J.K.; Feldmann, G.; Mullendore, M.E.; Goggins, M.G.; Hong, S.M.; Maitra, A. MicroRNA miR-155 is a biomarker of early pancreatic neoplasia. Cancer Biol. Ther. 2009, 8, 340–346. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Liu, J.; Gao, J.; Du, Y.; Li, Z.; Ren, Y.; Gu, J.; Wang, X.; Gong, Y.; Wang, W.; Kong, X. Combination of plasma microRNAs with serum CA19-9 for early detection of pancreatic cancer. Int. J. Cancer 2012, 131, 683–691. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Hou, S.; Ye, Z.; Wang, W.; Hu, X.; Hang, Q. Long Non-Coding RNAs in Pancreatic Cancer: Biologic Functions, Mechanisms, and Clinical Significance. Cancers 2022, 14, 2115. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ma, Y.; He, X.; Di, Y.; Liu, S.; Zhan, Q.; Bai, Z.; Qiu, T.; Corpe, C.; Wang, J. Identification of prognostic immune-related lncRNAs in pancreatic cancer. Front. Immunol. 2022, 13, 1005695. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gao, H.; Gong, N.; Ma, Z.; Miao, X.; Chen, J.; Cao, Y.; Zhang, G. LncRNA ZEB2-AS1 promotes pancreatic cancer cell growth and invasion through regulating the miR-204/HMGB1 axis. Int. J. Biol. Macromol. 2018, 116, 545–551. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Zhang, G.Q.; Chen, H.; Zhao, Z.J.; Chen, H.Z.; Liu, H.; Wang, G.; Jia, Y.H.; Pan, S.H.; Kong, R.; et al. Plasma and tumor levels of Linc-pint are diagnostic and prognostic biomarkers for pancreatic cancer. Oncotarget 2016, 7, 71773–71781. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Xie, Z.; Chen, X.; Li, J.; Guo, Y.; Li, H.; Pan, X.; Jiang, J.; Liu, H.; Wu, B. Salivary HOTAIR and PVT1 as novel biomarkers for early pancreatic cancer. Oncotarget 2016, 7, 25408–25419. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Seimiya, T.; Otsuka, M.; Fujishiro, M. Roles of circular RNAs in the pathogenesis and treatment of pancreatic cancer. Front. Cell. Dev. Biol. 2022, 10, 1023332. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhao, R.; Han, Z.; Zhou, H.; Xue, Y.; Chen, X.; Cao, X. Diagnostic and prognostic role of circRNAs in pancreatic cancer: A meta-analysis. Front. Oncol. 2023, 13, 1174577. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yan, H.; Wen, Y.; Tian, Z.; Hart, N.; Han, S.; Hughes, S.J.; Zeng, Y. A one-pot isothermal Cas12-based assay for the sensitive detection of microRNAs. Nat. Biomed. Eng. 2023, 7, 1583–1601. [Google Scholar] [CrossRef] [PubMed]
- Hameed, B.S.; Krishnan, U.M. Artificial Intelligence-Driven Diagnosis of Pancreatic Cancer. Cancers 2022, 14, 5382. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang, L.; Pleskow, D.K.; Turzhitsky, V.; Yee, E.U.; Berzin, T.M.; Sawhney, M.; Shinagare, S.; Vitkin, E.; Zakharov, Y.; Khan, U.; et al. Light scattering spectroscopy identifies the malignant potential of pancreatic cysts during endoscopy. Nat. Biomed. Eng. 2017, 1, 0040. [Google Scholar] [CrossRef]
- Liu, Y.; Brand, R.E.; Turzhitsky, V.; Kim, Y.L.; Roy, H.K.; Hasabou, N.; Sturgis, C.; Shah, D.; Hall, C.; Backman, V. Optical Markers in Duodenal Mucosa Predict the Presence of Pancreatic Cancer. Clin. Cancer Res. 2007, 13, 4392–4399. [Google Scholar] [CrossRef]
- Brussow, H. The human microbiome project at ten years—Some critical comments and reflections on “our third genome”, the human virome. Microbiome Res. Rep. 2023, 2, 7. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kustrimovic, N.; Bombelli, R.; Baci, D.; Mortara, L. Microbiome and Prostate Cancer: A Novel Target for Prevention and Treatment. Int. J. Mol. Sci. 2023, 24, 1511. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Miyake, M.; Tatsumi, Y.; Ohnishi, K.; Fujii, T.; Nakai, Y.; Tanaka, N.; Fujimoto, K. Prostate diseases and microbiome in the prostate, gut, and urine. Prostate Int. 2022, 10, 96–107. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zitvogel, L.; Tesniere, A.; Kroemer, G. Cancer despite immunosurveillance: Immunoselection and immunosubversion. Nat. Rev. Immunol. 2006, 6, 715–727. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.P.; Cao, H.; Edmondson, E.F.; Dasa, S.S.K.; Stern, S.T. Cholecystokinin-B Receptor-Targeted Nanoparticle for Imaging and Detection of Precancerous Lesions in the Pancreas. Biomolecules 2021, 11, 1766. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Papi, M.; Palmieri, V.; Digiacomo, L.; Giulimondi, F.; Palchetti, S.; Ciasca, G.; Perini, G.; Caputo, D.; Cartillone, M.C.; Cascone, C.; et al. Converting the personalized biomolecular corona of graphene oxide nanoflakes into a high-throughput diagnostic test for early cancer detection. Nanoscale 2019, 11, 15339–15346. [Google Scholar] [CrossRef] [PubMed]
- Rehman, S.; Umer, A.; Kuncewitch, M.; Molmenti, E. Whipple Procedure: Pancreaticogastrostomy Versus Pancreaticojejunostomy: A Literature Review. J. Ayub Med. Coll. Abbottabad 2016, 28, 179–182. [Google Scholar] [PubMed]
- Leroux, C.; Konstantinidou, G. Targeted Therapies for Pancreatic Cancer: Overview of Current Treatments and New Opportunities for Personalized Oncology. Cancers 2021, 13, 799. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cazacu, I.M.; Singh, B.S.; Martin-Paulpeter, R.M.; Beddar, S.; Chun, S.; Holliday, E.B.; Koong, A.C.; Das, P.; Koay, E.J.; Taniguchi, C.; et al. Endoscopic Ultrasound-Guided Fiducial Placement for Stereotactic Body Radiation Therapy in Patients with Pancreatic Cancer. Cancers 2023, 15, 5355. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Daamen, L.A.; Parikh, P.J.; Hall, W.A. The Use of MR-Guided Radiation Therapy for Pancreatic Cancer. Semin. Radiat. Oncol. 2024, 34, 23–35. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, A.E.; Mahmoud, A.M.; Mohamed, W.R.; Mohamed, T. Femtosecond laser attenuates oxidative stress, inflammation, and liver fibrosis in rats: Possible role of PPARγ and Nrf2/HO-1 signaling. Life Sci. 2022, 307, 120877. [Google Scholar] [CrossRef] [PubMed]
- Taha, S.; Mohamed, W.R.; Elhemely, M.A.; El-Gendy, A.O.; Mohamed, T. Tunable femtosecond laser suppresses the proliferation of breast cancer in vitro. J. Photochem. Photobiol. B 2023, 240, 112665. [Google Scholar] [CrossRef] [PubMed]
- Laface, C.; Memeo, R.; Maselli, F.M.; Santoro, A.N.; Iaia, M.L.; Ambrogio, F.; Laterza, M.; Cazzato, G.; Guarini, C.; De Santis, P.; et al. Immunotherapy and Pancreatic Cancer: A Lost Challenge? Life 2023, 13, 1482. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jiang, W.; Liang, M.; Lei, Q.; Li, G.; Wu, S. The Current Status of Photodynamic Therapy in Cancer Treatment. Cancers 2023, 15, 585. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mazur, R.; Trna, J. Principles of Palliative and Supportive Care in Pancreatic Cancer: A Review. Biomedicines 2023, 11, 2690. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Garbuzenko, O.B.; Sapiezynski, J.; Girda, E.; Rodriguez-Rodriguez, L.; Minko, T. Personalized Versus Precision Nanomedicine for Treatment of Ovarian Cancer. Small 2024, e2307462. [Google Scholar] [CrossRef] [PubMed]
- Crombé, A.; Spinnato, P.; Italiano, A.; Brisse, H.J.; Feydy, A.; Fadli, D.; Kind, M. Radiomics and artificial intelligence for soft-tissue sarcomas: Current status and perspectives. Diagn. Interv. Imaging 2023, 104, 567–583. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.; Shiradkar, R.; Liu, Z. Integrating pathomics with radiomics and genomics for cancer prognosis: A brief review. Chin. J. Cancer Res. 2021, 33, 563–573. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vendittelli PSmeets, E.M.; Litjens, G. Automatic tumour segmentation in H&E-stained whole-slide images of the pancreas. arXiv 2021, arXiv:2112.01533v2. [Google Scholar]
- Garbuzenko, O.B.; Saad, M.; Pozharov, V.P.; Reuhl, K.R.; Mainelis, G.; Minko, T. Inhibition of lung tumor growth by complex pulmonary delivery of drugs with oligonucleotides as suppressors of cellular resistance. Proc. Natl. Acad. Sci. USA 2010, 107, 10737–10742. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Minko, T.; Rodriguez-Rodriguez, L.; Pozharov, V. Nanotechnology approaches for personalized treatment of multidrug resistant cancers. Adv. Drug Deliv. Rev. 2013, 65, 1880–1895. [Google Scholar] [CrossRef] [PubMed]
- Pakunlu, R.I.; Cook, T.J.; Minko, T. Simultaneous modulation of multidrug resistance and antiapoptotic cellular defense by MDR1 and BCL-2 targeted antisense oligonucleotides enhances the anticancer efficacy of doxorubicin. Pharm. Res. 2003, 20, 351–359. [Google Scholar] [CrossRef] [PubMed]
- Pakunlu, R.I.; Wang, Y.; Saad, M.; Khandare, J.J.; Starovoytov, V.; Minko, T. In vitro and in vivo intracellular liposomal delivery of antisense oligonucleotides and anticancer drug. J. Control. Release 2006, 114, 153–162. [Google Scholar] [CrossRef] [PubMed]
- Pakunlu, R.I.; Wang, Y.; Tsao, W.; Pozharov, V.; Cook, T.J.; Minko, T. Enhancement of the efficacy of chemotherapy for lung cancer by simultaneous suppression of multidrug resistance and antiapoptotic cellular defense: Novel multicomponent delivery system. Cancer Res. 2004, 64, 6214–6224. [Google Scholar] [CrossRef] [PubMed]
- Saad, M.; Garbuzenko, O.B.; Minko, T. Co-delivery of siRNA and an anticancer drug for treatment of multidrug-resistant cancer. Nanomedicine 2008, 3, 761–776. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Taratula, O.; Garbuzenko, O.B.; Chen, A.M.; Minko, T. Innovative strategy for treatment of lung cancer: Targeted nanotechnology-based inhalation co-delivery of anticancer drugs and siRNA. J. Drug Target. 2011, 19, 900–914. [Google Scholar] [CrossRef] [PubMed]
- Taratula, O.; Kuzmov, A.; Shah, M.; Garbuzenko, O.B.; Minko, T. Nanostructured lipid carriers as multifunctional nanomedicine platform for pulmonary co-delivery of anticancer drugs and siRNA. J. Control. Release 2013, 171, 349–357. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wang, Y.; Minko, T. A novel cancer therapy: Combined liposomal hypoxia inducible factor 1 alpha antisense oligonucleotides and an anticancer drug. Biochem. Pharmacol. 2004, 68, 2031–2042. [Google Scholar] [CrossRef] [PubMed]
- Benkhaled, S.; Peters, C.; Jullian, N.; Arsenijevic, T.; Navez, J.; Van Gestel, D.; Moretti, L.; Van Laethem, J.L.; Bouchart, C. Combination, Modulation and Interplay of Modern Radiotherapy with the Tumor Microenvironment and Targeted Therapies in Pancreatic Cancer: Which Candidates to Boost Radiotherapy? Cancers 2023, 15, 768. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- McCubrey, J.A.; Abrams, S.L.; Follo, M.Y.; Manzoli, L.; Ratti, S.; Martelli, A.M.; Cervello, M. Effects of chloroquine and hydroxychloroquine on the sensitivity of pancreatic cancer cells to targeted therapies. Adv. Biol. Regul. 2023, 87, 100917. [Google Scholar] [CrossRef] [PubMed]
- Telisnor, G.; DeRemer, D.L.; Frimpong, E.; Agyare, E.; Allen, J.; Ricks-Santi, L.; Han, B.; George, T.; Rogers, S.C. Review of genetic and pharmacogenetic differences in cytotoxic and targeted therapies for pancreatic cancer in African Americans. J. Natl. Med. Assoc. 2023, 115, 164–174. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Aslan, M.; Shahbazi, R.; Ulubayram, K.; Ozpolat, B. Targeted Therapies for Pancreatic Cancer and Hurdles Ahead. Anticancer Res. 2018, 38, 6591–6606. [Google Scholar] [CrossRef] [PubMed]
- Weinhold, B. Epigenetics: The science of change. Environ. Health Perspect. 2006, 114, A160–A167. [Google Scholar] [CrossRef]
- Aviles, D.; Warshal, D.; Buchbinder, M.; Ostrovsky, O. Influence of Aberrant Epigenetic Changes and the Tumor Microenvironment in Ovarian Cancer Metastasis. In Metastasis; Sergi, C.M., Ed.; Exon Publications: Brisbane, Austrilia, 2022. [Google Scholar] [CrossRef]
- Azmi, A.S.; Beck, F.W.; Bao, B.; Mohammad, R.M.; Sarkar, F.H. Aberrant epigenetic grooming of miRNAs in pancreatic cancer: A systems biology perspective. Epigenomics 2011, 3, 747–759. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Coronel-Hernandez, J.; Perez-Yepez, E.A.; Delgado-Waldo, I.; Contreras-Romero, C.; Jacobo-Herrera, N.; Cantu-De Leon, D.; Perez-Plasencia, C. Aberrant Metabolism as Inductor of Epigenetic Changes in Breast Cancer: Therapeutic Opportunities. Front. Oncol. 2021, 11, 676562. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gao, D.; Herman, J.G.; Guo, M. The clinical value of aberrant epigenetic changes of DNA damage repair genes in human cancer. Oncotarget 2016, 7, 37331–37346. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Juergens, R.A.; Rudin, C.M. Aberrant epigenetic regulation: A central contributor to lung carcinogenesis and a new therapeutic target. Am. Soc. Clin. Oncol. Educ. Book 2013, 33, e295–e300. [Google Scholar] [CrossRef] [PubMed]
- Ciernikova, S.; Earl, J.; García Bermejo, M.L.; Stevurkova, V.; Carrato, A.; Smolkova, B. Epigenetic Landscape in Pancreatic Ductal Adenocarcinoma: On the Way to Overcoming Drug Resistance? Int. J. Mol. Sci. 2020, 21, 4091. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kuhn, D.E.; Martin, M.M.; Feldman, D.S.; Terry, A.V., Jr.; Nuovo, G.J.; Elton, T.S. Experimental validation of miRNA targets. Methods 2008, 44, 47–54. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Matsui, A.; Uchida, S.; Ishii, T.; Itaka, K.; Kataoka, K. Messenger RNA-based therapeutics for the treatment of apoptosis-associated diseases. Sci. Rep. 2015, 5, 15810. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wong, K.K. DNMT1 as a therapeutic target in pancreatic cancer: Mechanisms and clinical implications. Cell. Oncol. 2020, 43, 779–792. [Google Scholar] [CrossRef] [PubMed]
- Zagorac, S.; Alcala, S.; Fernandez Bayon, G.; Bou Kheir, T.; Schoenhals, M.; Gonzalez-Neira, A.; Fernandez Fraga, M.; Aicher, A.; Heeschen, C.; Sainz, B., Jr. DNMT1 Inhibition Reprograms Pancreatic Cancer Stem Cells via Upregulation of the miR-17-92 Cluster. Cancer Res. 2016, 76, 4546–4558. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tian, X.; Zhang, S.; Liu, H.M.; Zhang, Y.B.; Blair, C.A.; Mercola, D.; Sassone-Corsi, P.; Zi, X. Histone lysine-specific methyltransferases and demethylases in carcinogenesis: New targets for cancer therapy and prevention. Curr. Cancer Drug Targets 2013, 13, 558–579. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Falchook, G.; Rosen, S.; LoRusso, P.; Watts, J.; Gupta, S.; Coombs, C.C.; Talpaz, M.; Kurzrock, R.; Mita, M.; Cassaday, R.; et al. Development of 2 Bromodomain and Extraterminal Inhibitors with Distinct Pharmacokinetic and Pharmacodynamic Profiles for the Treatment of Advanced Malignancies. Clin. Cancer Res. 2020, 26, 1247–1257. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- LaRue, M.M.; Parker, S.; Puccini, J.; Cammer, M.; Kimmelman, A.C.; Bar-Sagi, D. Metabolic reprogramming of tumor-associated macrophages by collagen turnover promotes fibrosis in pancreatic cancer. Proc. Natl. Acad. Sci. USA 2022, 119, e2119168119. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Li, X.; Zhou, J.; Wang, X.; Li, C.; Ma, Z.; Wan, Q.; Peng, F. Pancreatic cancer and fibrosis: Targeting metabolic reprogramming and crosstalk of cancer-associated fibroblasts in the tumor microenvironment. Front. Immunol. 2023, 14, 1152312. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Stagos, D. Antioxidant Activity of Polyphenolic Plant Extracts. Antioxidants 2019, 9, 19. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Andersen, H.B.; Ialchina, R.; Pedersen, S.F.; Czaplinska, D. Metabolic reprogramming by driver mutation-tumor microenvironment interplay in pancreatic cancer: New therapeutic targets. Cancer Metastasis Rev. 2021, 40, 1093–1114. [Google Scholar] [CrossRef] [PubMed]
- Gao, S.; Yang, D.; Fang, Y.; Lin, X.; Jin, X.; Wang, Q.; Wang, X.; Ke, L.; Shi, K. Engineering Nanoparticles for Targeted Remodeling of the Tumor Microenvironment to Improve Cancer Immunotherapy. Theranostics 2019, 9, 126–151. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Li, M.; Zhang, F.; Su, Y.; Zhou, J.; Wang, W. Nanoparticles designed to regulate tumor microenvironment for cancer therapy. Life Sci. 2018, 201, 37–44. [Google Scholar] [CrossRef]
- Song, W.-F.; Zheng, D.; Zeng, S.-M.; Zeng, X.; Zhang, X.-Z. Targeting to Tumor-Harbored Bacteria for Precision Tumor Therapy. ACS Nano 2022, 16, 17402–17413. [Google Scholar] [CrossRef]
- Duong, M.T.-Q.; Qin, Y.; You, S.-H.; Min, J.-J. Bacteria-cancer interactions: Bacteria-based cancer therapy. Exp. Mol. Med. 2019, 51, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Haist, M.; Stege, H.; Grabbe, S.; Bros, M. The Functional Crosstalk between Myeloid-Derived Suppressor Cells and Regulatory T Cells within the Immunosuppressive Tumor Microenvironment. Cancers 2021, 13, 210. [Google Scholar] [CrossRef]
- Kim, T.J.; Koo, K.C. Current Status and Future Perspectives of Checkpoint Inhibitor Immunotherapy for Prostate Cancer: A Comprehensive Review. Int. J. Mol. Sci. 2020, 21, 5484. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Raskov, H.; Orhan, A.; Christensen, J.P.; Gögenur, I. Cytotoxic CD8+ T cells in cancer and cancer immunotherapy. Br. J. Cancer 2021, 124, 359–367. [Google Scholar] [CrossRef]
- Looi, C.K.; Chung, F.F.; Leong, C.O.; Wong, S.F.; Rosli, R.; Mai, C.W. Therapeutic challenges and current immunomodulatory strategies in targeting the immunosuppressive pancreatic tumor microenvironment. J. Exp. Clin. Cancer Res. 2019, 38, 162. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhao, J.-F.; Zou, F.-L.; Zhu, J.-F.; Huang, C.; Bu, F.-Q.; Zhu, Z.-M.; Yuan, R.-F. Nano-drug delivery system for pancreatic cancer: A visualization and bibliometric analysis. Front. Pharmacol. 2022, 13, 1025618. [Google Scholar] [CrossRef]
- Noubissi Nzeteu, G.A.; Gibbs, B.F.; Kotnik, N.; Troja, A.; Bockhorn, M.; Meyer, N.H. Nanoparticle-based immunotherapy of pancreatic cancer. Front. Mol. Biosci. 2022, 9, 948898. [Google Scholar] [CrossRef]
- Tarannum, M.; Vivero-Escoto, J.L. Nanoparticle-based therapeutic strategies targeting major clinical challenges in pancreatic cancer treatment. Adv. Drug Deliv. Rev. 2022, 187, 114357. [Google Scholar] [CrossRef] [PubMed]
- Viegas, C.; Patricio, A.B.; Prata, J.; Fonseca, L.; Macedo, A.S.; Duarte, S.O.D.; Fonte, P. Advances in Pancreatic Cancer Treatment by Nano-Based Drug Delivery Systems. Pharmaceutics 2023, 15, 2363. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gustafson, H.H.; Holt-Casper, D.; Grainger, D.W.; Ghandehari, H. Nanoparticle Uptake: The Phagocyte Problem. Nano Today 2015, 10, 487–510. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Barenholz, Y. Doxil(R)—The first FDA-approved nano-drug: Lessons learned. J. Control. Release 2012, 160, 117–134. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, M.J.; Billingsley, M.M.; Haley, R.M.; Wechsler, M.E.; Peppas, N.A.; Langer, R. Engineering precision nanoparticles for drug delivery. Nat. Rev. Drug Discov. 2021, 20, 101–124. [Google Scholar] [CrossRef] [PubMed]
- Greene, M.K.; Johnston, M.C.; Scott, C.J. Nanomedicine in Pancreatic Cancer: Current Status and Future Opportunities for Overcoming Therapy Resistance. Cancers 2021, 13, 6175. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Patra, J.K.; Das, G.; Fraceto, L.F.; Campos, E.V.R.; Rodriguez-Torres, M.d.P.; Acosta-Torres, L.S.; Diaz-Torres, L.A.; Grillo, R.; Swamy, M.K.; Sharma, S.; et al. Nano based drug delivery systems: Recent developments and future prospects. J. Nanobiotechnology 2018, 16, 71. [Google Scholar] [CrossRef] [PubMed]
- Torchilin, V.P. Recent advances with liposomes as pharmaceutical carriers. Nat. Rev. Drug Discov. 2005, 4, 145–160. [Google Scholar] [CrossRef]
- Deshpande, P.P.; Biswas, S.; Torchilin, V.P. Current trends in the use of liposomes for tumor targeting. Nanomedicine 2013, 8, 1509–1528. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nsairat, H.; Khater, D.; Sayed, U.; Odeh, F.; Al Bawab, A.; Alshaer, W. Liposomes: Structure, composition, types, and clinical applications. Heliyon 2022, 8, e09394. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ramanathan, R.K.; Korn, R.L.; Sachdev, J.C.; Fetterly, G.J.; Jameson, G.; Marceau, K.; Marsh, V.; Raghunand, N.; Prey, J.; Klinz, S.G.; et al. 261 Lesion characterization with ferumoxytol MRI in patients with advanced solid tumors and correlation with treatment response to MM-398, nanoliposomal irinotecan (nal-IRI). Eur. J. Cancer 2014, 50, 87. [Google Scholar] [CrossRef]
- Kalra, A.V.; Kim, J.; Klinz, S.G.; Paz, N.; Cain, J.; Drummond, D.C.; Nielsen, U.B.; Fitzgerald, J.B. Preclinical activity of nanoliposomal irinotecan is governed by tumor deposition and intratumor prodrug conversion. Cancer Res. 2014, 74, 7003–7013. [Google Scholar] [CrossRef] [PubMed]
- Wang-Gillam, A.; Li, C.P.; Bodoky, G.; Dean, A.; Shan, Y.S.; Jameson, G.; Macarulla, T.; Lee, K.H.; Cunningham, D.; Blanc, J.F.; et al. Nanoliposomal irinotecan with fluorouracil and folinic acid in metastatic pancreatic cancer after previous gemcitabine-based therapy (NAPOLI-1): A global, randomised, open-label, phase 3 trial. Lancet 2016, 387, 545–557. [Google Scholar] [CrossRef] [PubMed]
- Wainberg, Z.A.; Melisi, D.; Macarulla, T.; Pazo Cid, R.; Chandana, S.R.; De La Fouchardiere, C.; Dean, A.; Kiss, I.; Lee, W.J.; Goetze, T.O.; et al. NALIRIFOX versus nab-paclitaxel and gemcitabine in treatment-naive patients with metastatic pancreatic ductal adenocarcinoma (NAPOLI 3): A randomised, open-label, phase 3 trial. Lancet 2023, 402, 1272–1281. [Google Scholar] [CrossRef] [PubMed]
- Sivadasan, D.; Ramakrishnan, K.; Mahendran, J.; Ranganathan, H.; Karuppaiah, A.; Rahman, H. Solid Lipid Nanoparticles: Applications and Prospects in Cancer Treatment. Int. J. Mol. Sci. 2023, 24, 6199. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ferreira, R.G.; Narvaez, L.E.M.; Espindola, K.M.M.; Rosario, A.; Lima, W.G.N.; Monteiro, M.C. Can Nimesulide Nanoparticles Be a Therapeutic Strategy for the Inhibition of the KRAS/PTEN Signaling Pathway in Pancreatic Cancer? Front. Oncol. 2021, 11, 594917. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Affram, K.O.; Smith, T.; Ofori, E.; Krishnan, S.; Underwood, P.; Trevino, J.G.; Agyare, E. Cytotoxic effects of gemcitabine-loaded solid lipid nanoparticles in pancreatic cancer cells. J. Drug Deliv. Sci. Technol. 2020, 55, 101374. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Xu, W.; Bae, E.J.; Lee, M.K. Enhanced anticancer activity and intracellular uptake of paclitaxel-containing solid lipid nanoparticles in multidrug-resistant breast cancer cells. Int. J. Nanomed. 2018, 13, 7549–7563. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gomez-Aguado, I.; Rodriguez-Castejon, J.; Vicente-Pascual, M.; Rodriguez-Gascon, A.; Pozo-Rodriguez, A.D.; Solinis Aspiazu, M.A. Nucleic Acid Delivery by Solid Lipid Nanoparticles Containing Switchable Lipids: Plasmid DNA vs. Messenger RNA. Molecules 2020, 25, 5995. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mehnert, W.; Mader, K. Solid lipid nanoparticles: Production, characterization and applications. Adv. Drug Deliv. Rev. 2001, 47, 165–196. [Google Scholar] [CrossRef] [PubMed]
- Shidhaye, S.S.; Vaidya, R.; Sutar, S.; Patwardhan, A.; Kadam, V.J. Solid lipid nanoparticles and nanostructured lipid carriers--innovative generations of solid lipid carriers. Curr. Drug Deliv. 2008, 5, 324–331. [Google Scholar] [CrossRef] [PubMed]
- Ghasemiyeh, P.; Mohammadi-Samani, S. Solid lipid nanoparticles and nanostructured lipid carriers as novel drug delivery systems: Applications, advantages and disadvantages. Res. Pharm. Sci. 2018, 13, 288–303. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lu, Z.; Su, J.; Li, Z.; Zhan, Y.; Ye, D. Hyaluronic acid-coated, prodrug-based nanostructured lipid carriers for enhanced pancreatic cancer therapy. Drug Dev. Ind. Pharm. 2017, 43, 160–170. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Liu, S.; Jia, L.; Chu, F.; Zhou, Y.; He, Z.; Guo, M.; Chen, C.; Xu, L. Nanostructured lipid carriers for MicroRNA delivery in tumor gene therapy. Cancer Cell Int. 2018, 18, 101. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gajbhiye, K.R.; Salve, R.; Narwade, M.; Sheikh, A.; Kesharwani, P.; Gajbhiye, V. Lipid polymer hybrid nanoparticles: A custom-tailored next-generation approach for cancer therapeutics. Mol. Cancer 2023, 22, 160. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mohanty, A.; Uthaman, S.; Park, I.K. Utilization of Polymer-Lipid Hybrid Nanoparticles for Targeted Anti-Cancer Therapy. Molecules 2020, 25, 4377. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hu, C.M.; Kaushal, S.; Tran Cao, H.S.; Aryal, S.; Sartor, M.; Esener, S.; Bouvet, M.; Zhang, L. Half-antibody functionalized lipid-polymer hybrid nanoparticles for targeted drug delivery to carcinoembryonic antigen presenting pancreatic cancer cells. Mol. Pharm. 2010, 7, 914–920. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhao, X.; Li, F.; Li, Y.; Wang, H.; Ren, H.; Chen, J.; Nie, G.; Hao, J. Co-delivery of HIF1alpha siRNA and gemcitabine via biocompatible lipid-polymer hybrid nanoparticles for effective treatment of pancreatic cancer. Biomaterials 2015, 46, 13–25, Erratum in Biomaterials 2022, 280, 121296. https://doi.org/10.1016/j.biomaterials.2021.121296. PMID: 34890971. [Google Scholar] [CrossRef]
- Lu, J.; Liu, X.; Liao, Y.P.; Salazar, F.; Sun, B.; Jiang, W.; Chang, C.H.; Jiang, J.; Wang, X.; Wu, A.M.; et al. Nano-enabled pancreas cancer immunotherapy using immunogenic cell death and reversing immunosuppression. Nat. Commun. 2017, 8, 1811. [Google Scholar] [CrossRef] [PubMed]
- Perez-Herrero, E.; Fernandez-Medarde, A. Advanced targeted therapies in cancer: Drug nanocarriers, the future of chemotherapy. Eur. J. Pharm. Biopharm. 2015, 93, 52–79. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, P.; Haldar, M.K.; You, S.; Choi, Y.; Mallik, S. Hypoxia-Responsive Polymersomes for Drug Delivery to Hypoxic Pancreatic Cancer Cells. Biomacromolecules 2016, 17, 2507–2513. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Manzur, A.; Oluwasanmi, A.; Moss, D.; Curtis, A.; Hoskins, C. Nanotechnologies in Pancreatic Cancer Therapy. Pharmaceutics 2017, 9, 39. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Von Hoff, D.D.; Ramanathan, R.K.; Borad, M.J.; Laheru, D.A.; Smith, L.S.; Wood, T.E.; Korn, R.L.; Desai, N.; Trieu, V.; Iglesias, J.L.; et al. Gemcitabine plus nab-paclitaxel is an active regimen in patients with advanced pancreatic cancer: A phase I/II trial. J. Clin. Oncol. 2011, 29, 4548–4554. [Google Scholar] [CrossRef] [PubMed]
- Frese, K.K.; Neesse, A.; Cook, N.; Bapiro, T.E.; Lolkema, M.P.; Jodrell, D.I.; Tuveson, D.A. nab-Paclitaxel potentiates gemcitabine activity by reducing cytidine deaminase levels in a mouse model of pancreatic cancer. Cancer Discov. 2012, 2, 260–269. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Von Hoff, D.D.; Ervin, T.; Arena, F.P.; Chiorean, E.G.; Infante, J.; Moore, M.; Seay, T.; Tjulandin, S.A.; Ma, W.W.; Saleh, M.N.; et al. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N. Engl. J. Med. 2013, 369, 1691–1703. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tajima, H.; Makino, I.; Ohbatake, Y.; Nakanuma, S.; Hayashi, H.; Nakagawara, H.; Miyashita, T.; Takamura, H.; Ohta, T. Neoadjuvant chemotherapy for pancreatic cancer: Effects on cancer tissue and novel perspectives. Oncol. Lett. 2017, 13, 3975–3981. [Google Scholar] [CrossRef] [PubMed] [PubMed Central][Green Version]
- Mittal, P.; Saharan, A.; Verma, R.; Altalbawy, F.M.A.; Alfaidi, M.A.; Batiha, G.E.; Akter, W.; Gautam, R.K.; Uddin, M.S.; Rahman, M.S. Dendrimers: A New Race of Pharmaceutical Nanocarriers. Biomed. Res. Int. 2021, 2021, 8844030. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ozturk, K.; Esendagli, G.; Gurbuz, M.U.; Tulu, M.; Calis, S. Effective targeting of gemcitabine to pancreatic cancer through PEG-cored Flt-1 antibody-conjugated dendrimers. Int. J. Pharm. 2017, 517, 157–167. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.; Huang, X.; Yan, H. Peptide dendrimers as potentiators of conventional chemotherapy in the treatment of pancreatic cancer in a mouse model. Eur. J. Pharm. Biopharm. 2022, 170, 121–132. [Google Scholar] [CrossRef] [PubMed]
- Peracchia, M.T.; Gref, R.; Minamitake, Y.; Domb, A.; Lotan, N.; Langer, R. PEG-coated nanospheres from amphiphilic diblock and multiblock copolymers: Investigation of their drug encapsulation and release characteristics. J. Control. Release 1997, 46, 223–231. [Google Scholar] [CrossRef]
- Jaidev, L.R.; Chellappan, D.R.; Bhavsar, D.V.; Ranganathan, R.; Sivanantham, B.; Subramanian, A.; Sharma, U.; Jagannathan, N.R.; Krishnan, U.M.; Sethuraman, S. Multi-functional nanoparticles as theranostic agents for the treatment & imaging of pancreatic cancer. Acta Biomater. 2017, 49, 422–433. [Google Scholar] [CrossRef] [PubMed]
- Rong, Q.; Feng, F.; Ma, Z. Metal ions doped chitosan-poly(acrylic acid) nanospheres: Synthesis and their application in simultaneously electrochemical detection of four markers of pancreatic cancer. Biosens. Bioelectron. 2016, 75, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Li, J.-M.; Chen, W.; Wang, H.; Jin, C.; Yu, X.-J.; Lu, W.-Y.; Cui, L.; Fu, D.-L.; Ni, Q.-X.; Hou, H.-M. Preparation of albumin nanospheres loaded with gemcitabine and their cytotoxicity against BXPC-3 cells in vitro. Acta Pharmacol. Sin. 2009, 30, 1337–1343. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Xu, X.; Fang, X.; Cai, S.; Wang, M.; Xing, C.; Lu, C.; Yang, H. Self-Assembled mRNA-Responsive DNA Nanosphere for Bioimaging and Cancer Therapy in Drug-Resistant Cells. Anal. Chem. 2020, 92, 11779–11785. [Google Scholar] [CrossRef] [PubMed]
- Pereira-Silva, M.; Miranda-Pastoriza, D.; Diaz-Gomez, L.; Sotelo, E.; Paiva-Santos, A.C.; Veiga, F.; Concheiro, A.; Alvarez-Lorenzo, C. Gemcitabine-Vitamin E Prodrug-Loaded Micelles for Pancreatic Cancer Therapy. Pharmaceutics 2024, 16, 95. [Google Scholar] [CrossRef] [PubMed]
- Tuli, H.S.; Joshi, R.; Kaur, G.; Garg, V.K.; Sak, K.; Varol, M.; Kaur, J.; Alharbi, S.A.; Alahmadi, T.A.; Aggarwal, D.; et al. Metal nanoparticles in cancer: From synthesis and metabolism to cellular interactions. J. Nanostructure Chem. 2023, 13, 321–348. [Google Scholar] [CrossRef]
- Ashour, M.; Faris, H.G.; Ahmed, H.; Mamdouh, S.; Thambiratnam, K.; Mohamed, T. Using Femtosecond Laser Pulses to Explore the Nonlinear Optical Properties of Au NP Colloids That Were Synthesized by Laser Ablation. Nanomaterials 2022, 12, 2980. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shen, A.M.; Malekshah, O.M.; Pogrebnyak, N.; Minko, T. Plant-derived single domain COVID-19 antibodies. J. Control. Release 2023, 359, 1–11. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ranganathan, R.; Madanmohan, S.; Kesavan, A.; Baskar, G.; Krishnamoorthy, Y.R.; Santosham, R.; Ponraju, D.; Rayala, S.K.; Venkatraman, G. Nanomedicine: Towards development of patient-friendly drug-delivery systems for oncological applications. Int. J. Nanomed. 2012, 7, 1043–1060. [Google Scholar] [CrossRef]
- Yallapu, M.M.; Ebeling, M.C.; Khan, S.; Sundram, V.; Chauhan, N.; Gupta, B.K.; Puumala, S.E.; Jaggi, M.; Chauhan, S.C. Novel curcumin-loaded magnetic nanoparticles for pancreatic cancer treatment. Mol. Cancer Ther. 2013, 12, 1471–1480. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lafuente-Gómez, N.; Milán-Rois, P.; García-Soriano, D.; Luengo, Y.; Cordani, M.; Alarcón-Iniesta, H.; Salas, G.; Somoza, Á. Smart Modification on Magnetic Nanoparticles Dramatically Enhances Their Therapeutic Properties. Cancers 2021, 13, 4095. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wahajuddin, N.; Arora, S. Superparamagnetic iron oxide nanoparticles: Magnetic nanoplatforms as drug carriers. Int. J. Nanomedicine 2012, 7, 3445–3471. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jiang, Y.; Liu, S.; Zhang, Y.; Li, H.; He, H.; Dai, J.; Jiang, T.; Ji, W.; Geng, D.; Elzatahry, A.A.; et al. Magnetic mesoporous nanospheres anchored with LyP-1 as an efficient pancreatic cancer probe. Biomaterials 2017, 115, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Minko, T.; Dharap, S.S.; Pakunlu, R.I.; Wang, Y. Molecular targeting of drug delivery systems to cancer. Curr. Drug Targets 2004, 5, 389–406. [Google Scholar] [CrossRef] [PubMed]
- Matsumura, Y.; Maeda, H. A new concept for macromolecular therapeutics in cancer chemotherapy: Mechanism of tumoritropic accumulation of proteins and the antitumor agent smancs. Cancer Res. 1986, 46 Pt 1, 6387–6392. [Google Scholar] [PubMed]
- Nakamura, Y.; Mochida, A.; Choyke, P.L.; Kobayashi, H. Nanodrug Delivery: Is the Enhanced Permeability and Retention Effect Sufficient for Curing Cancer? Bioconjugate Chem. 2016, 27, 2225–2238. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Akpa, P.A.; Peter, I.E.; Onwuka, A.M.; Obi, B.C.; Akunne, M.O.; Nworu, C.S.; Ejikeme, P.M.; Akunne, T.C.; Attama, A.A.; Akah, P.A. Nanotheranostics: Platforms, Current Applications, and Mechanisms of Targeting in Breast and Prostate Cancers. J. Nanotheranostics 2023, 4, 346–383. [Google Scholar] [CrossRef]
- Ryschich, E.; Huszty, G.; Knaebel, H.P.; Hartel, M.; Buchler, M.W.; Schmidt, J. Transferrin receptor is a marker of malignant phenotype in human pancreatic cancer and in neuroendocrine carcinoma of the pancreas. Eur. J. Cancer 2004, 40, 1418–1422. [Google Scholar] [CrossRef] [PubMed]
- Camp, E.R.; Wang, C.; Little, E.C.; Watson, P.M.; Pirollo, K.F.; Rait, A.; Cole, D.J.; Chang, E.H.; Watson, D.K. Transferrin receptor targeting nanomedicine delivering wild-type p53 gene sensitizes pancreatic cancer to gemcitabine therapy. Cancer Gene Ther. 2013, 20, 222–228. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Senzer, N.; Nemunaitis, J.; Nemunaitis, D.; Bedell, C.; Edelman, G.; Barve, M.; Nunan, R.; Pirollo, K.F.; Rait, A.; Chang, E.H. Phase I study of a systemically delivered p53 nanoparticle in advanced solid tumors. Mol. Ther. 2013, 21, 1096–1103. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Leung, C.P.; Barve, M.A.; Wu, M.-S.; Pirollo, K.F.; Strauss, J.F.; Liao, W.-C.; Yang, S.-H.; Nunan, R.A.; Adams, J.; Harford, J.B.; et al. A phase II trial combining tumor-targeting TP53 gene therapy with gemcitabine/nab-paclitaxel as a second-line treatment for metastatic pancreatic cancer. J. Clin. Oncol. 2021, 39 (Suppl. S15), 4139. [Google Scholar] [CrossRef]
- Mitsudomi, T.; Yatabe, Y. Epidermal growth factor receptor in relation to tumor development: EGFR gene and cancer. FEBS J. 2010, 277, 301–308. [Google Scholar] [CrossRef] [PubMed]
- Grapa, C.M.; Mocan, T.; Gonciar, D.; Zdrehus, C.; Mosteanu, O.; Pop, T.; Mocan, L. Epidermal Growth Factor Receptor and Its Role in Pancreatic Cancer Treatment Mediated by Nanoparticles. Int. J. Nanomed. 2019, 14, 9693–9706. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Moore, M.J.; Goldstein, D.; Hamm, J.; Figer, A.; Hecht, J.R.; Gallinger, S.; Au, H.J.; Murawa, P.; Walde, D.; Wolff, R.A.; et al. Erlotinib Plus Gemcitabine Compared with Gemcitabine Alone in Patients with Advanced Pancreatic Cancer: A Phase III Trial of the National Cancer Institute of Canada Clinical Trials Group. J. Clin. Oncol. 2023, 41, 4714–4720. [Google Scholar] [CrossRef] [PubMed]
- Gunther, T.; Tulipano, G.; Dournaud, P.; Bousquet, C.; Csaba, Z.; Kreienkamp, H.J.; Lupp, A.; Korbonits, M.; Castano, J.P.; Wester, H.J.; et al. International Union of Basic and Clinical Pharmacology. cv. Somatostatin Receptors: Structure, Function, Ligands, and New Nomenclature. Pharmacol. Rev. 2018, 70, 763–835. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Patel, Y.C. Somatostatin and its receptor family. Front. Neuroendocrinol. 1999, 20, 157–198. [Google Scholar] [CrossRef] [PubMed]
- Schally, A.V. Oncological applications of somatostatin analogues. Cancer Res. 1988, 48 Pt 1, 6977–6985. [Google Scholar] [PubMed]
- Li, M.; Fisher, W.E.; Kim, H.J.; Wang, X.; Brunicardi, C.F.; Chen, C.; Yao, Q. Somatostatin, somatostatin receptors, and pancreatic cancer. World J. Surg. 2005, 29, 293–296. [Google Scholar] [CrossRef] [PubMed]
- Chatzisideri, T.; Leonidis, G.; Sarli, V. Cancer-targeted delivery systems based on peptides. Future Med. Chem. 2018, 10, 2201–2226. [Google Scholar] [CrossRef] [PubMed]
- Fisher, W.E.; Doran, T.A.; Muscarella, P., 2nd; Boros, L.G.; Ellison, E.C.; Schirmer, W.J. Expression of somatostatin receptor subtype 1–5 genes in human pancreatic cancer. J. Natl. Cancer Inst. 1998, 90, 322–324. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kikutsuji, T.; Harada, M.; Tashiro, S.; Ii, S.; Moritani, M.; Yamaoka, T.; Itakura, M. Expression of somatostatin receptor subtypes and growth inhibition in human exocrine pancreatic cancers. J. Hepatobiliary Pancreat. Surg. 2000, 7, 496–503. [Google Scholar] [CrossRef] [PubMed]
- Shahbaz, M.; Ruliang, F.; Xu, Z.; Benjia, L.; Cong, W.; Zhaobin, H.; Jun, N. mRNA expression of somatostatin receptor subtypes SSTR-2, SSTR-3, and SSTR-5 and its significance in pancreatic cancer. World J. Surg. Oncol. 2015, 13, 46. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gradiz, R.; Silva, H.C.; Carvalho, L.; Botelho, M.F.; Mota-Pinto, A. MIA PaCa-2 and PANC-1—Pancreas ductal adenocarcinoma cell lines with neuroendocrine differentiation and somatostatin receptors. Sci. Rep. 2016, 6, 21648. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Qin, Y.; Ertl, T.; Groot, K.; Horvath, J.; Cai, R.Z.; Schally, A.V. Somatostatin analog RC-160 inhibits growth of CFPAC-1 human pancreatic cancer cells in vitro and intracellular production of cyclic adenosine monophosphate. Int. J. Cancer 1995, 60, 694–700. [Google Scholar] [CrossRef] [PubMed]
- Hicklin, D.J.; Ellis, L.M. Role of the vascular endothelial growth factor pathway in tumor growth and angiogenesis. J. Clin. Oncol. 2005, 23, 1011–1027. [Google Scholar] [CrossRef] [PubMed]
- Martin, L.K.; Li, X.; Kleiber, B.; Ellison, E.C.; Bloomston, M.; Zalupski, M.; Bekaii-Saab, T.S. VEGF remains an interesting target in advanced pancreas cancer (APCA): Results of a multi-institutional phase II study of bevacizumab, gemcitabine, and infusional 5-fluorouracil in patients with APCA. Ann. Oncol. 2012, 23, 2812–2820. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Van Cutsem, E.; Vervenne, W.L.; Bennouna, J.; Humblet, Y.; Gill, S.; Van Laethem, J.L.; Verslype, C.; Scheithauer, W.; Shang, A.; Cosaert, J.; et al. Phase III trial of bevacizumab in combination with gemcitabine and erlotinib in patients with metastatic pancreatic cancer. J. Clin. Oncol. 2009, 27, 2231–2237. [Google Scholar] [CrossRef] [PubMed]
- Carbone, C.; Moccia, T.; Zhu, C.; Paradiso, G.; Budillon, A.; Chiao, P.J.; Abbruzzese, J.L.; Melisi, D. Anti-VEGF treatment-resistant pancreatic cancers secrete proinflammatory factors that contribute to malignant progression by inducing an EMT cell phenotype. Clin. Cancer Res. 2011, 17, 5822–5832. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kim, D.K.; Jeong, J.; Lee, D.S.; Hyeon, D.Y.; Park, G.W.; Jeon, S.; Lee, K.B.; Jang, J.Y.; Hwang, D.; Kim, H.M.; et al. PD-L1-directed PlGF/VEGF blockade synergizes with chemotherapy by targeting CD141(+) cancer-associated fibroblasts in pancreatic cancer. Nat. Commun. 2022, 13, 6292. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Anderson, L.R.; Owens, T.W.; Naylor, M.J. Structural and mechanical functions of integrins. Biophys. Rev. 2014, 6, 203–213. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Li, Z.; Di, C.; Li, S.; Yang, X.; Nie, G. Smart Nanotherapeutic Targeting of Tumor Vasculature. Acc. Chem. Res. 2019, 52, 2703–2712. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.; Lee, S.; Park, S. iRGD Peptide as a Tumor-Penetrating Enhancer for Tumor-Targeted Drug Delivery. Polymers 2020, 12, 1906. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hosotani, R.; Kawaguchi, M.; Masui, T.; Koshiba, T.; Ida, J.; Fujimoto, K.; Wada, M.; Doi, R.; Imamura, M. Expression of integrin alphaVbeta3 in pancreatic carcinoma: Relation to MMP-2 activation and lymph node metastasis. Pancreas 2002, 25, e30–e35. [Google Scholar] [CrossRef] [PubMed]
- Sugahara, K.N.; Teesalu, T.; Karmali, P.P.; Kotamraju, V.R.; Agemy, L.; Greenwald, D.R.; Ruoslahti, E. Coadministration of a tumor-penetrating peptide enhances the efficacy of cancer drugs. Science 2010, 328, 1031–1035. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Turaga, R.C.; Yin, L.; Yang, J.J.; Lee, H.; Ivanov, I.; Yan, C.; Yang, H.; Grossniklaus, H.E.; Wang, S.; Ma, C.; et al. Rational design of a protein that binds integrin alphavbeta3 outside the ligand binding site. Nat. Commun. 2016, 7, 11675. [Google Scholar] [CrossRef] [PubMed]
- Nagase, H.; Kudo, D.; Suto, A.; Yoshida, E.; Suto, S.; Negishi, M.; Kakizaki, I.; Hakamada, K. 4-Methylumbelliferone Suppresses Hyaluronan Synthesis and Tumor Progression in SCID Mice Intra-abdominally Inoculated With Pancreatic Cancer Cells. Pancreas 2017, 46, 190–197. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cheng, X.B.; Sato, N.; Kohi, S.; Koga, A.; Hirata, K. 4-Methylumbelliferone inhibits enhanced hyaluronan synthesis and cell migration in pancreatic cancer cells in response to tumor-stromal interactions. Oncol. Lett. 2018, 15, 6297–6301. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hajime, M.; Shuichi, Y.; Makoto, N.; Masanori, Y.; Ikuko, K.; Atsushi, K.; Mutsuo, S.; Keiichi, T. Inhibitory effect of 4-methylesculetin on hyaluronan synthesis slows the development of human pancreatic cancer in vitro and in nude mice. Int. J. Cancer 2007, 120, 2704–2709. [Google Scholar] [CrossRef] [PubMed]
- Ko, A.H.; Kim, K.P.; Siveke, J.T.; Lopez, C.D.; Lacy, J.; O’Reilly, E.M.; Macarulla, T.; Manji, G.A.; Lee, J.; Ajani, J.; et al. Atezolizumab Plus PEGPH20 Versus Chemotherapy in Advanced Pancreatic Ductal Adenocarcinoma and Gastric Cancer: MORPHEUS Phase Ib/II Umbrella Randomized Study Platform. Oncologist 2023, 28, 553–e472. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yu, T.; Li, Y.; Gu, X.; Li, Q. Development of a Hyaluronic Acid-Based Nanocarrier Incorporating Doxorubicin and Cisplatin as a pH-Sensitive and CD44-Targeted Anti-Breast Cancer Drug Delivery System. Front. Pharmacol. 2020, 11, 532457. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Paliwal, S.R.; Paliwal, R.; Agrawal, G.P.; Vyas, S.P. Hyaluronic acid modified pH-sensitive liposomes for targeted intracellular delivery of doxorubicin. J. Liposome Res. 2016, 26, 276–287. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Hao, X.; Qin, J.; Tang, W.; He, F.; Smith, A.; Zhang, M.; Simeone, D.M.; Qiao, X.T.; Chen, Z.N.; et al. Antibody against CD44s inhibits pancreatic tumor initiation and postradiation recurrence in mice. Gastroenterology 2014, 146, 1108–1118. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kesharwani, P.; Banerjee, S.; Padhye, S.; Sarkar, F.H.; Iyer, A.K. Hyaluronic Acid Engineered Nanomicelles Loaded with 3,4-Difluorobenzylidene Curcumin for Targeted Killing of CD44+ Stem-Like Pancreatic Cancer Cells. Biomacromolecules 2015, 16, 3042–3053. [Google Scholar] [CrossRef] [PubMed]
- Clinical Trials Search. Available online: https://classic.clinicaltrials.gov/ct2/results?term=nanoparticles&cond=Pancreatic+Cancer&Search=Apply&recrs=d&recrs=e&age_v=&gndr=&type=&rslt= (accessed on 10 February 2024).
- Ishizawa, T. “Bon mariage” of artificial intelligence and intraoperative fluorescence imaging for safer surgery. Artif. Intell. Surg. 2023, 3, 163–165. [Google Scholar] [CrossRef]
- Wagner, M.; Brandenburg, J.M.; Bodenstedt, S.; Schulze, A.; Jenke, A.C.; Stern, A.; Daum, M.T.J.; Mündermann, L.; Kolbinger, F.R.; Bhasker, N.; et al. Surgomics: Personalized prediction of morbidity, mortality and long-term outcome in surgery using machine learning on multimodal data. Surg. Endosc. 2022, 36, 8568–8591. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Swetha, K.L.; Roy, A. Tumor heterogeneity and nanoparticle-mediated tumor targeting: The importance of delivery system personalization. Drug Deliv. Transl. Res. 2018, 8, 1508–1526. [Google Scholar] [CrossRef] [PubMed]


| # | NCT Number | Status | Interventions | Phases |
|---|---|---|---|---|
| 1 | NCT02336087 | Active | Paclitaxel Albumin-Stabilized Nanoparticle Formulation combined with Gemcitabine, Metformin | 1 |
| 2 | NCT02562716 | Completed | Paclitaxel Albumin-Stabilized Nanoparticle Formulation, Fluorouracil, Gemcitabine, Irinotecan, Oxaliplatin | 2 |
| 3 | NCT02194829 | Completed | Nab-paclitaxel *, Gemcitabine | 1, 2 |
| 4 | NCT03410030 | Completed | Paclitaxel protein-bound, Cisplatin, Gemcitabine | 1, 2 |
| 5 | NCT02707159 | Completed | Drug: Nab paclitaxel, Gemcitabine | 2 |
| 6 | NCT02227940 | Completed | Paclitaxel Albumin-Stabilized Nanoparticle Formulation, Ceritinib, Cisplatin, Gemcitabine | 1 |
| 7 | NCT00920023 | Completed | Superparamagnetic Iron Oxide Magnetic Resonance Imaging | 4 |
| 8 | NCT02178436 | Completed | Nab paclitaxel *, Gemcitabine, Selinexor | 2 |
| 0 | NCT02620865 | Completed | Paclitaxel Albumin-Stabilized Nanoparticle Formulation, Biologicals: Aldesleukin, Antibody Therapy, Drugs: Fluorouracil, Gemcitabine, Irinotecan, Leucovorin Calcium, Oxaliplatin, Sargramostim | 1 2 |
| 10 | NCT01677559 | Completed | Nab-Paclitaxel * | 1 |
| 11 | NCT03304210 | Completed | PIPAC (Pressurized intraperitoneal aerosolized chemotherapy) with Abraxane | 1 |
| 12 | NCT03910387 | Active | Nab-paclitaxel *, Gemcitabine, Telotristat Ethyl | 2 |
| 13 | NCT01161186 | Completed | Nab-paclitaxel *, Gemcitabine, Capecitabine | 1 |
| 14 | NCT02333188 | Completed | Paclitaxel Albumin-Stabilized Nanoparticle Formulation, Leucovorin, Irinotecan, Fluorouracil | 1 |
| 15 | NCT01437007 | Completed | TKM-080301—stable nucleic acid–lipid particles (SNALPs) formulation of a siRNA against Polo-Like Kinase 1 (PLK1) | 1 |
| 16 | NCT04524702 | Active | Nab-paclitaxel *, Gemcitabine, Hydroxychloroquine, Paricalcitol | 2 |
| 17 | NCT02394535 | Completed | Nab-paclitaxel *, Capecitabine, Radiation Therapy | 1 |
| 18 | NCT03382340 | Active | Curcumin/Doxorubicin-encapsulating Nanoparticle (IMX-110) | 1 2 |
| 19 | NCT02930902 | Completed | Nab-paclitaxel *, Gemcitabine, Paricalcitol, Pembrolizumab | 1 |
| 20 | NCT02427841 | Completed | Nab-paclitaxel *, Fluorouracil, Gemcitabine, Image Guided Radiation Therapy, Intensity-Modulated Radiation Therapy | 2 |
| 21 | NCT02231723 | Completed | Nab-paclitaxel *, Napabucasin (BBI608), Gemcitabine, Oxaliplatin, Leucovorin, Irinotecan, Fluorouracil, MM-398 (nanoliposomal irinotecan) | 1 |
| 22 | NCT00666991 | Completed | Nanoparticulate paclitaxel | 1 |
| 23 | NCT04233866 | Active | Liposomal Irinotecan, Nab-paclitaxel *, Fluorouracilb, Gemcitabine, Leucovorin, | 2 |
| 24 | NCT01300533 | Completed | Docetaxel Nanoparticle Targeting Prostate-Specific Membrane Antigen (BIND-014) | 1 |
| 25 | NCT04481204 | Active | Nab-paclitaxel *, Cisplatin, Fluorouracil, Gemcitabine, Irinotecan, Leucovorin, Oxaliplatin. Radiation Therapy | 2 |
| 26 | NCT02762981 | Completed | Nab-paclitaxel *, Relacorilant | 1 2 |
| 27 | NCT03678883 | Active | Nab-paclitaxel *, 9-ING-41(a maleimide-based ATP-competitive small molecule GSK-3β inhibitor), Gemcitabine, Doxorubicin, Lomustine, Carboplatin, Paclitaxel, Irinotecan | 2 |
| 28 | NCT03878524 | Active | Nab-paclitaxel * with several antibodies and anticancer drugs. | 1 |
| 29 | NCT03736720 | Active | Liposomal Irinotecan, Fluorouracil, Leucovorin | 2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gu, X.; Minko, T. Targeted Nanoparticle-Based Diagnostic and Treatment Options for Pancreatic Cancer. Cancers 2024, 16, 1589. https://doi.org/10.3390/cancers16081589
Gu X, Minko T. Targeted Nanoparticle-Based Diagnostic and Treatment Options for Pancreatic Cancer. Cancers. 2024; 16(8):1589. https://doi.org/10.3390/cancers16081589
Chicago/Turabian StyleGu, Xin, and Tamara Minko. 2024. "Targeted Nanoparticle-Based Diagnostic and Treatment Options for Pancreatic Cancer" Cancers 16, no. 8: 1589. https://doi.org/10.3390/cancers16081589
APA StyleGu, X., & Minko, T. (2024). Targeted Nanoparticle-Based Diagnostic and Treatment Options for Pancreatic Cancer. Cancers, 16(8), 1589. https://doi.org/10.3390/cancers16081589






