Joint-Sparing Resection around the Knee for Osteosarcoma: Long-Term Outcomes of Biologic Reconstruction with Vascularized Fibula Graft Combined with Massive Allograft
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
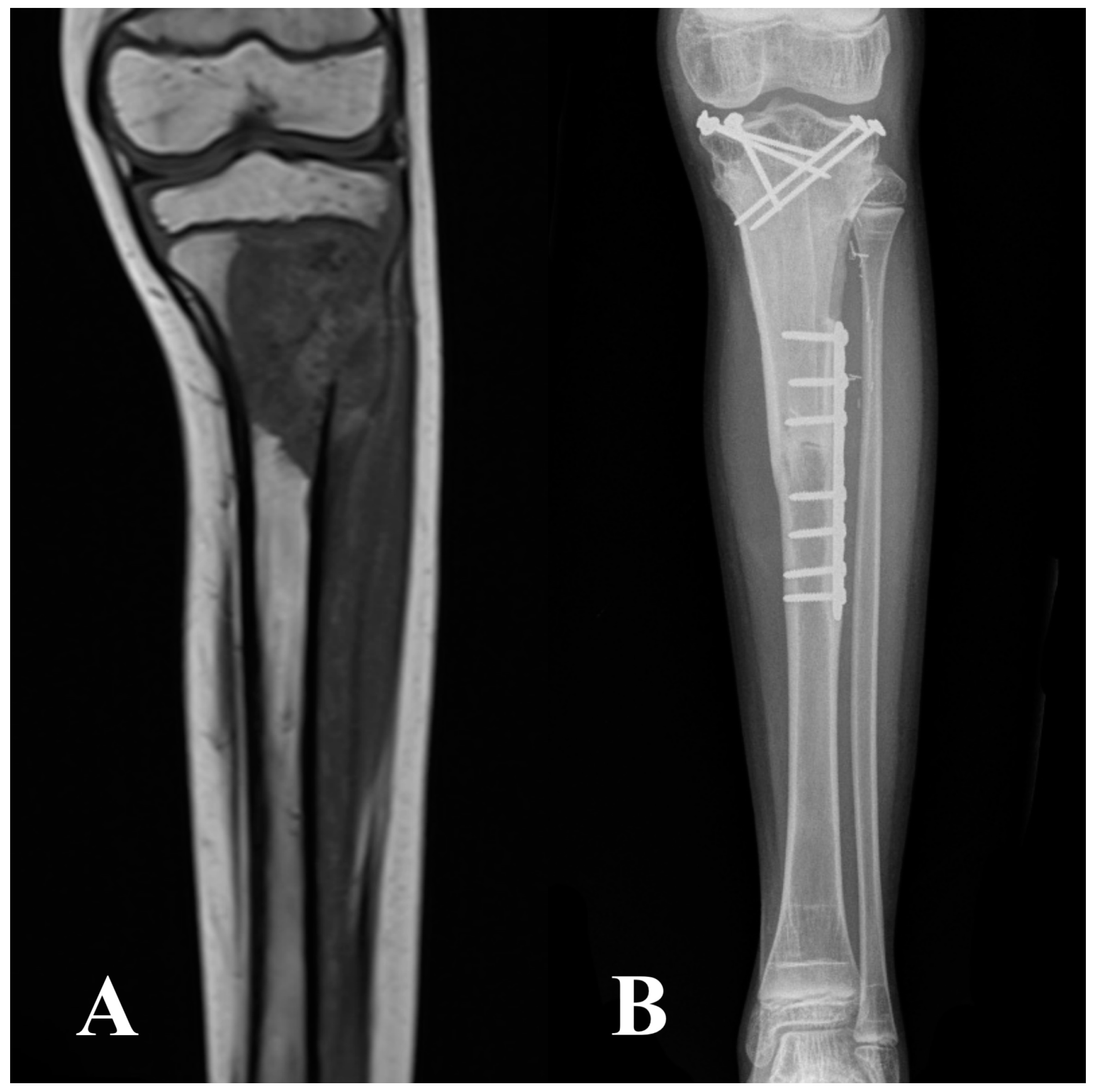
2.2. Surgical Technique, Aftercare, and Cancer Treatment
2.3. Data Sources and Variables
2.4. Statistical Analysis
3. Results
3.1. Complications and Reoperations
3.2. Outcomes Score Function
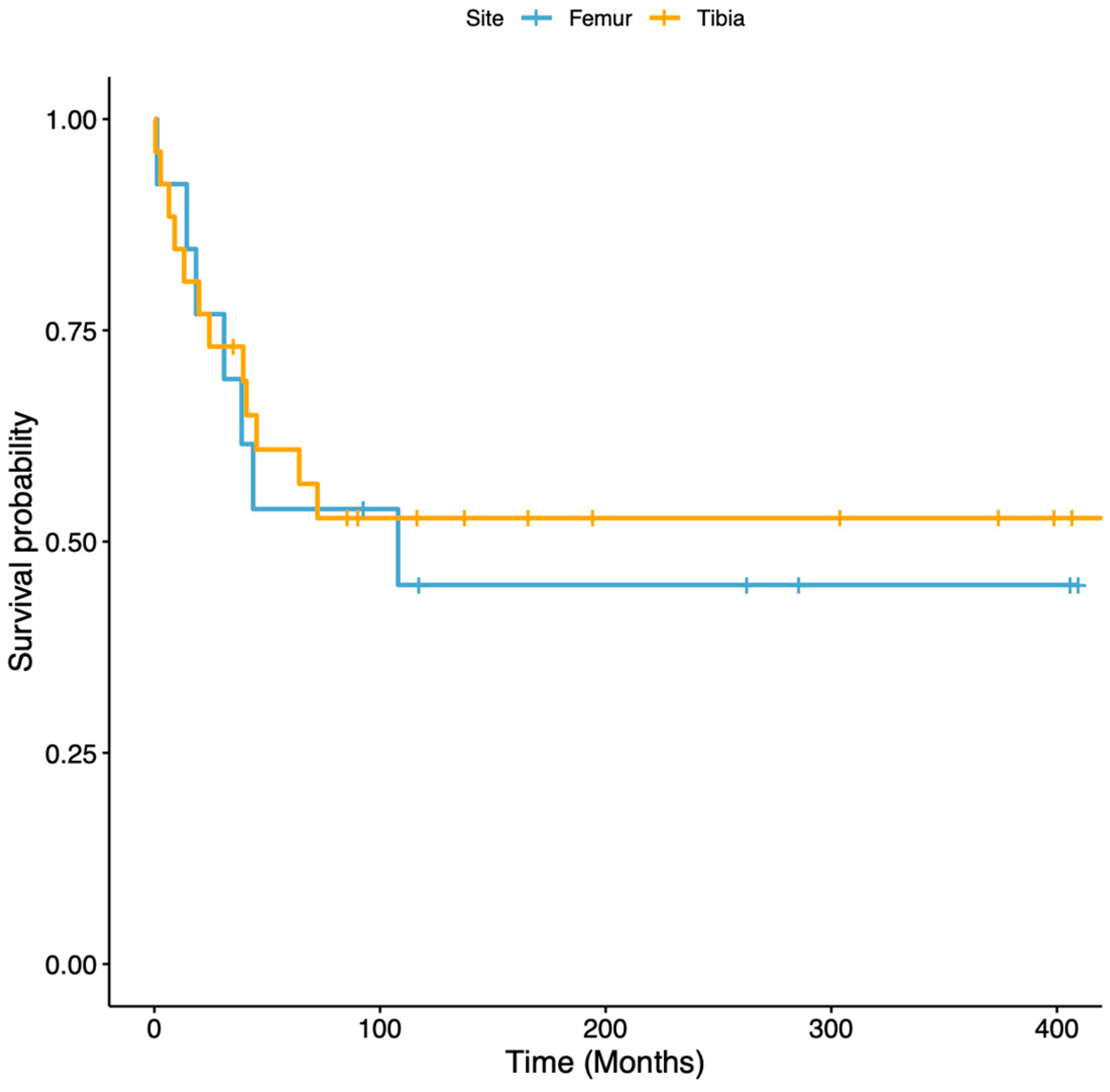
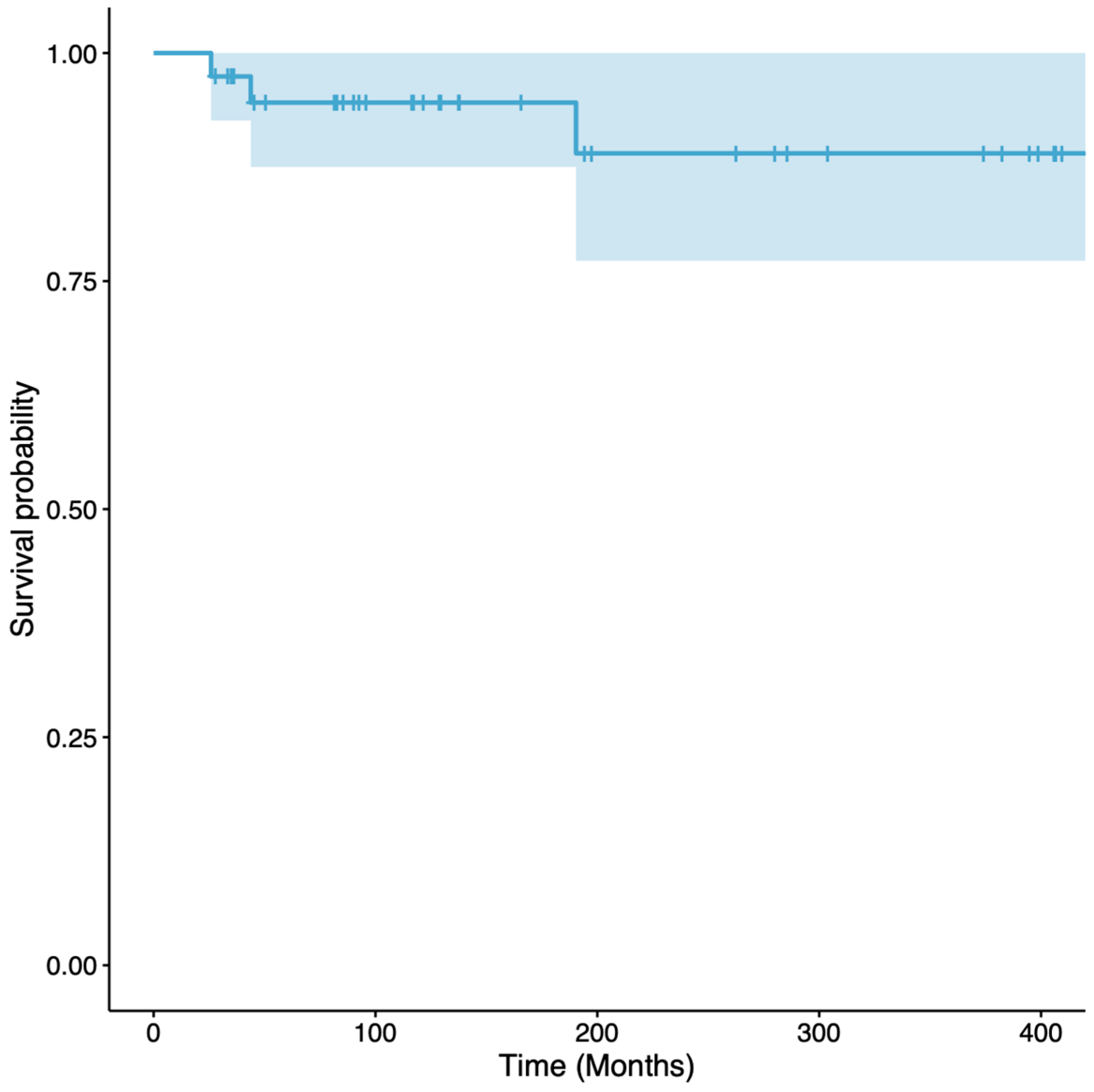
3.3. Survivorship of Vascularized Fibular Grafts
4. Discussion
4.1. Limitations
4.2. Complications and Reoperations
4.3. Outcomes Scores for Function
4.4. Survivorship of Vascularized Fibular Grafts
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Arndt, C.A.; Crist, W.M. Common musculoskeletal tumors of childhood and adolescence. N. Engl. J. Med. 1999, 341, 342–352. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, S.; Ruggieri, P.; Cefalo, G.; Tamburini, A.; Capanna, R.; Fagioli, F.; Comandone, A.; Bertulli, R.; Bisogno, G.; Palmerini, E.; et al. Neoadjuvant chemotherapy with methotrexate, cisplatin, and doxorubicin with or without ifosfamide in nonmetastatic osteosarcoma of the extremity: An Italian sarcoma group trial ISG/OS-1. J. Clin. Oncol. 2012, 30, 2112–2118. [Google Scholar] [CrossRef] [PubMed]
- San-Julian, M.; Aquerreta, J.D.; Benito, A.; Cañadell, J. Indications for epiphyseal preservation in metaphyseal malignant bone tumors of children: Relationship between image methods and histological findings. J. Pediatr. Orthop. 1999, 19, 543–548. [Google Scholar] [CrossRef] [PubMed]
- Manfrini, M.; Gasbarrini, A.; Malaguti, C.; Ceruso, M.; Innocenti, M.; Bini, S.; Capanna, R.; Campanacci, M. Intraepiphyseal resection of the proximal tibia and its impact on lower limb growth. Clin. Orthop. Relat. Res. 1999, 358, 111–119. [Google Scholar] [CrossRef]
- Li, J.; Shi, L.; Chen, G.J. Image navigation assisted joint-saving surgery for treatment of bone sarcoma around knee in skeletally immature patients. Surg. Oncol. 2014, 23, 132–139. [Google Scholar] [CrossRef]
- Aponte-Tinao, L.; Ayerza, M.A.; Muscolo, D.L.; Farfalli, G.L. Survival, recurrence, and function after epiphyseal preservation and allograft reconstruction in osteosarcoma of the knee. Clin. Orthop. Relat. Res. 2015, 473, 1789–1796. [Google Scholar] [CrossRef] [PubMed]
- Albergo, J.I.; Gaston, L.C.; Farfalli, G.L.; Laitinen, M.; Parry, M.; Ayerza, M.A.; Risk, M.; Jeys, L.M.; Aponte-Tinao, L.A. Failure rates and functional results for intercalary femur reconstructions after tumour resection. Musculoskelet. Surg. 2020, 104, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Sewell, M.D.; Hanna, S.A.; McGrath, A.; Aston, W.J.; Blunn, G.W.; Pollock, R.C.; Skinner, J.A.; Cannon, S.R.; Briggs, T.W. Intercalary diaphyseal endoprosthetic reconstruction for malignant tibial bone tumours. J. Bone Jt. Surg. Br. 2011, 93, 1111–1117. [Google Scholar] [CrossRef]
- Demiralp, B.; Ege, T.; Kose, O.; Yurttas, Y.; Basbozkurt, M. Reconstruction of intercalary bone defects following bone tumor resection with segmental bone transport using an Ilizarov circular external fixator. J. Orthop. Sci. 2014, 19, 1004–1011. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Sharma, A.; Tomar, S.; Mishra, A.; Kashyap, A.; Maini, L. Is Masquelet Technique A Successful Viable Treatment In Reconstructing Large Tumor Bone Gaps in Adolescent and Adult? Arch. Bone Jt. Surg. 2023, 11, 348–355. [Google Scholar]
- Zekry, K.M.; Yamamoto, N.; Hayashi, K.; Takeuchi, A.; Higuchi, T.; Abe, K.; Taniguchi, Y.; Alkhooly, A.Z.A.A.; Abd-Elfattah, A.S.; Fouly, E.H.; et al. Intercalary frozen autograft for reconstruction of malignant bone and soft tissue tumours. Int. Orthop. 2017, 41, 1481–1487. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Zhu, H.; Huang, M.; Zhang, C.; Chen, G.; Ji, C.; Wang, Z.; Li, J. Is frozen tumour-bearing autograft with concurrent vascularized fibula an alternative to the Capanna technique for the intercalary reconstruction after resection of osteosarcoma in the lower limb? Bone Jt. J. 2020, 102-B, 646–652. [Google Scholar] [CrossRef]
- Capanna, R.; Bufalini, C.; Campanacci, M. A new technique for reconstruction of large metadiaphyseal bone defects: A combined graft (allograft shell plus vascularized fibula). Orthop. Traumatol. 1993, 2, 159–177. [Google Scholar] [CrossRef]
- Taylor, G.I.; Miller, G.D.; Ham, F.J. The free vascularized bone graft. A clinical extension of microvascular techniques. Plast. Reconstr. Surg. 1975, 55, 533–544. [Google Scholar] [CrossRef]
- Weiland, A.J.; Daniel, R.K.; Riley, L.H., Jr. Application of the free vascularized bone graft in the treatment of malignant or aggressive bone tumors. Johns Hopkins Med. J. 1977, 140, 85–96. [Google Scholar] [PubMed]
- Chen, C.M.; Disa, J.J.; Lee, H.Y.; Mehrara, B.J.; Hu, Q.Y.; Nathan, S.; Boland, P.; Healey, J.; Cordeiro, P.G. Reconstruction of extremity long bone defects after sarcoma resection with vascularized fibula flaps: A 10-year review. Plast. Reconstr. Surg. 2007, 119, 915–926. [Google Scholar] [CrossRef]
- Li, J.; Wang, Z.; Ji, C.; Chen, G.; Liu, D.; Zhu, H. What are the Oncologic and Functional Outcomes After Joint Salvage Resections for Juxtaarticular Osteosarcoma About the Knee? Clin. Orthop. Relat. Res. 2017, 475, 2095–2104. [Google Scholar] [CrossRef] [PubMed]
- Enneking, W.F. A system of staging musculoskeletal neoplasms. Clin. Orthop. Relat. Res. 1986, 204, 9–24. [Google Scholar] [CrossRef]
- Enneking, W.F.; Dunham, W.; Gebhardt, M.C.; Malawar, M.; Pritchard, D.J. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin. Orthop. Relat. Res. 1993, 286, 241–246. [Google Scholar] [CrossRef]
- Campanacci, D.A.; Totti, F.; Puccini, S.; Beltrami, G.; Scoccianti, G.; Delcroix, L.; Innocenti, M.; Capanna, R. Intercalary reconstruction of femur after tumour resection: Is a vascularized fibular autograft plus allograft a long-lasting solution? Bone Joint J. 2018, 100-B, 378–386. [Google Scholar] [CrossRef]
- Campanacci, D.A.; Scanferla, R.; Marsico, M.; Scolari, F.; Scoccianti, G.; Beltrami, G.; Delcroix, L.; Innocenti, M.; Capanna, R. Intercalary Resection of the Tibia for Primary Bone Tumors: Are Vascularized Fibula Autografts with or without Allografts a Durable Reconstruction? Clin. Orthop. Relat. Res. 2024; ahead of print. [Google Scholar] [CrossRef]
- Aponte-Tinao, L.A.; Ayerza, M.A.; Muscolo, D.L.; Farfalli, G.L. Should fractures in massive intercalary bone allografts of the lower limb be treated with ORIF or with a new allograft? Clin. Orthop. Relat. Res. 2015, 473, 805–811. [Google Scholar] [CrossRef] [PubMed]
- Enneking, W.F.; Campanacci, D.A. Retrieved human allografts: A clinicopathological study. J. Bone Jt. Surg. Am. 2001, 83, 971–986. [Google Scholar] [CrossRef]
- Campanacci, L.; Manfrini, M.; Colangeli, M.; Alí, N.; Mercuri, M. Long-term results in children with massive bone osteoarticular allografts of the knee for high-grade osteosarcoma. J. Pediatr. Orthop. 2010, 30, 919–927. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Hu, J.; Zhu, K.; Cai, T.; Ma, X. Survival, complications and functional outcomes of cemented megaprostheses for high-grade osteosarcoma around the knee. Int. Orthop. 2018, 42, 927–938. [Google Scholar] [CrossRef] [PubMed]
- Arkader, A.; Viola, D.C.; Morris, C.D.; Boland, P.J.; Healey, J.H. Coaxial extendible knee equalizes limb length in children with osteogenic sarcoma. Clin. Orthop. Relat. Res. 2007, 459, 60–65. [Google Scholar] [CrossRef] [PubMed]
- Tsuda, Y.; Tsoi, K.; Stevenson, J.D.; Fujiwara, T.; Tillman, R.; Abudu, A. Extendable Endoprostheses in Skeletally Immature Patients: A Study of 124 Children Surviving More Than 10 Years After Resection of Bone Sarcomas. J. Bone Jt. Surg. Am. 2020, 102, 151–162. [Google Scholar] [CrossRef]


| Patients’ Characteristics | %/Average (Number/Range) | |
|---|---|---|
| Femur | Tibia | |
| Men | 77 (10) | 65 (17) |
| Women | 23 (3) | 35 (9) |
| Age (years) | 15 (7–37) | 17 (7–67) |
| Osteosarcoma grading | ||
| High-grade | 100 (13) | 81 (21) |
| Low-grade | 0 (0) | 9 (5) |
| Type of resection | ||
| Intercalary | 77 (10) | 58 (15) |
| Intraepiphyseal | 23 (3) | 42 (11) |
| Resection length (cm) | 15 (10–25) | 14 (10–20) |
| Proximal residual juxta-articular bone | 16.5 (6–26) | 3 (1–6) |
| Distal residual juxta-articular bone | 3.8 (2–6) | 16 (7–21) |
| Fibular resection length | 17.6 (12–28) | 17 (13–23) |
| Fixation method | ||
| Single bridging plate | 77 (10) | 35 (9) |
| Double bridging plate | 0 (0) | 4 (1) |
| Metaphyseal screws + diaphyseal plate | 15 (2) | 42 (11) |
| Only screws | 8 (1) | 12 (3) |
| Proximal and distal plates | 0 (0) | 8 (2) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scanferla, R.; Scolari, F.; Muratori, F.; Tamburini, A.; Delcroix, L.; Scoccianti, G.; Beltrami, G.; Innocenti, M.; Campanacci, D.A. Joint-Sparing Resection around the Knee for Osteosarcoma: Long-Term Outcomes of Biologic Reconstruction with Vascularized Fibula Graft Combined with Massive Allograft. Cancers 2024, 16, 1672. https://doi.org/10.3390/cancers16091672
Scanferla R, Scolari F, Muratori F, Tamburini A, Delcroix L, Scoccianti G, Beltrami G, Innocenti M, Campanacci DA. Joint-Sparing Resection around the Knee for Osteosarcoma: Long-Term Outcomes of Biologic Reconstruction with Vascularized Fibula Graft Combined with Massive Allograft. Cancers. 2024; 16(9):1672. https://doi.org/10.3390/cancers16091672
Chicago/Turabian StyleScanferla, Roberto, Federico Scolari, Francesco Muratori, Angela Tamburini, Luca Delcroix, Guido Scoccianti, Giovanni Beltrami, Marco Innocenti, and Domenico Andrea Campanacci. 2024. "Joint-Sparing Resection around the Knee for Osteosarcoma: Long-Term Outcomes of Biologic Reconstruction with Vascularized Fibula Graft Combined with Massive Allograft" Cancers 16, no. 9: 1672. https://doi.org/10.3390/cancers16091672
APA StyleScanferla, R., Scolari, F., Muratori, F., Tamburini, A., Delcroix, L., Scoccianti, G., Beltrami, G., Innocenti, M., & Campanacci, D. A. (2024). Joint-Sparing Resection around the Knee for Osteosarcoma: Long-Term Outcomes of Biologic Reconstruction with Vascularized Fibula Graft Combined with Massive Allograft. Cancers, 16(9), 1672. https://doi.org/10.3390/cancers16091672





