Identifying the Trends of Urinary microRNAs within Extracellular Vesicles for Esophageal Cancer
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection and Treatment
2.2. Treatment Progress and Follow-Up
2.3. Sample Collection
2.4. Isolating microRNAs from Urine Utilizing the Nanowire Device
2.5. Performing Microarray Analysis to Examine microRNA Expression
2.6. Statistical Analysis
3. Results
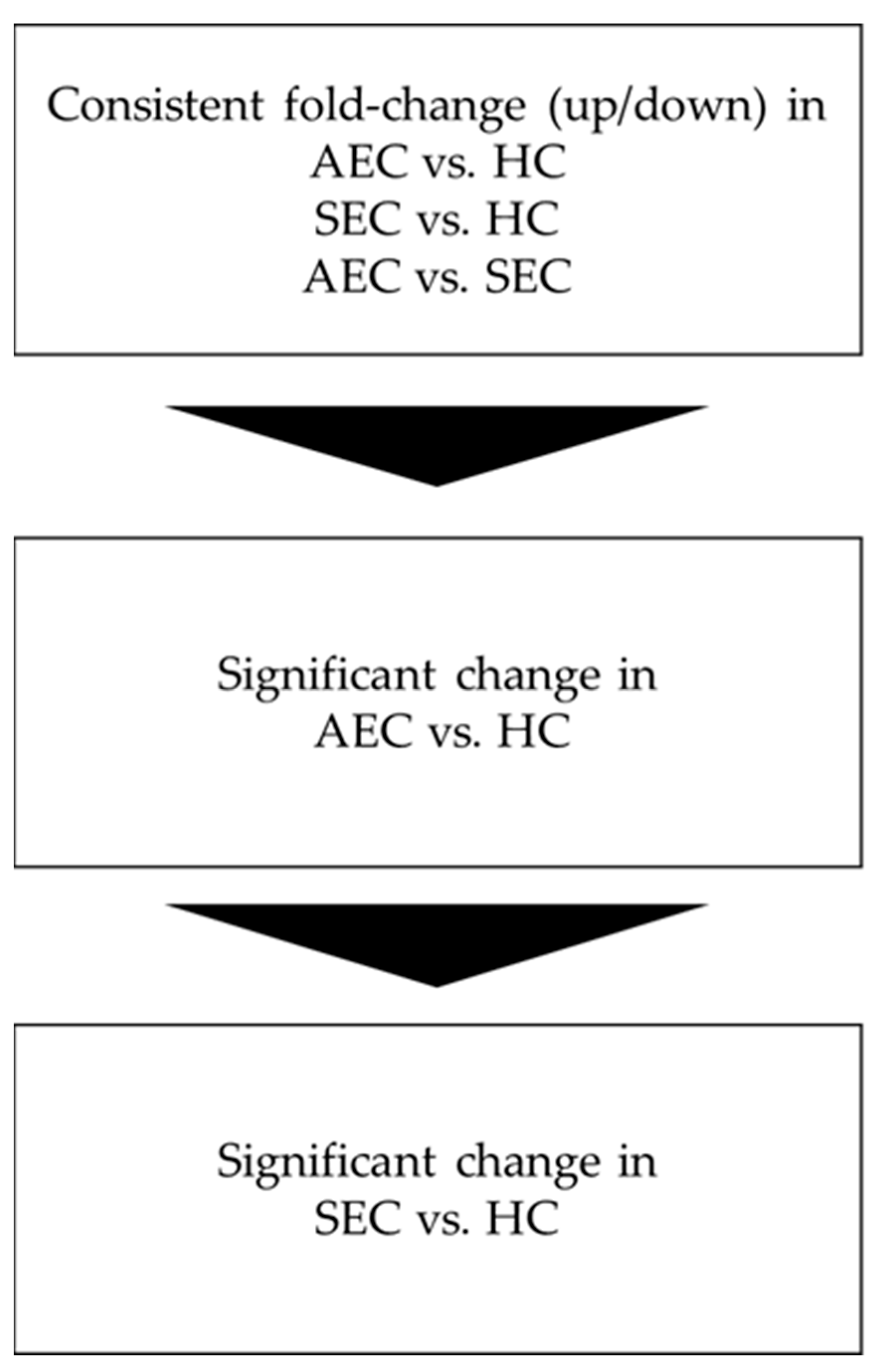
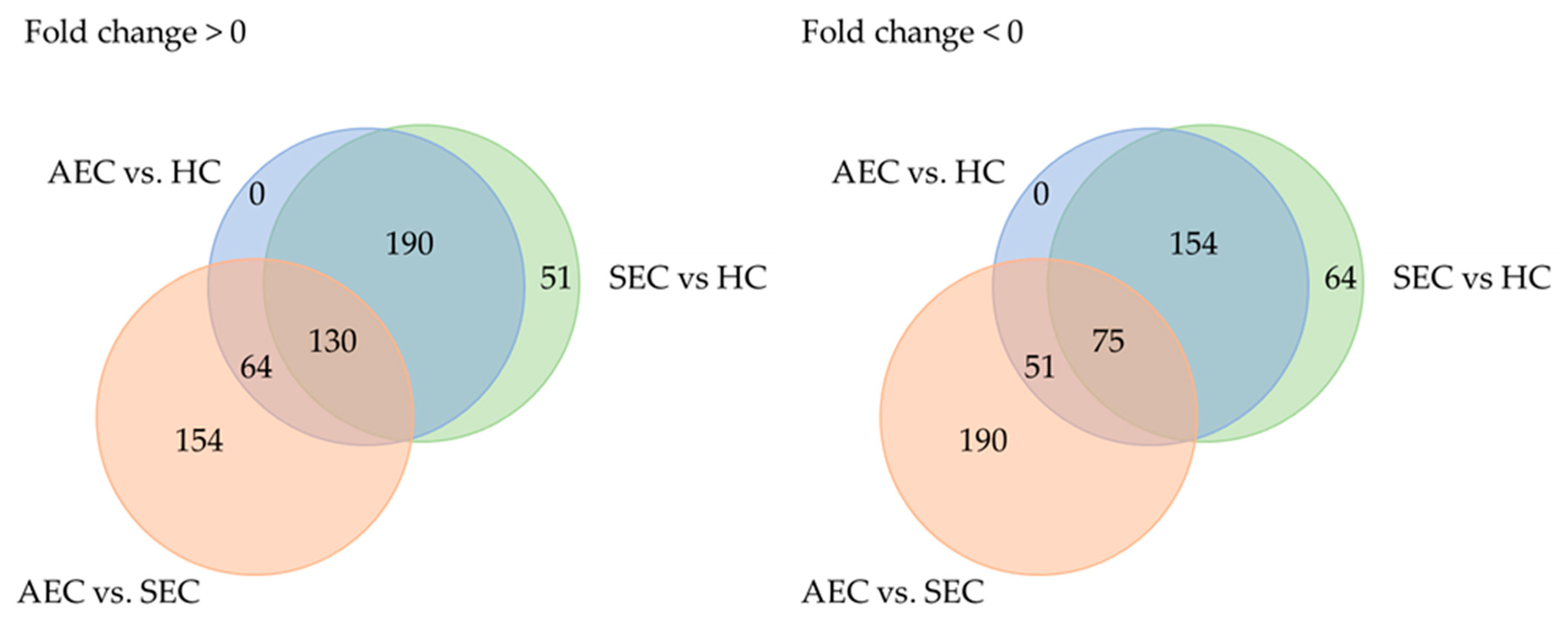
3.1. Patient Characteristics and the Urinary microRNA Profile
3.2. Longitudinal Evaluation of Urinary microRNA Levels
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Akutsu, Y.; Kato, K.; Igaki, H.; Ito, Y.; Nozaki, I.; Daiko, H.; Yano, M.; Udagawa, H.; Nakagawa, S.; Takagi, M.; et al. The Prevalence of Overall and Initial Lymph Node Metastases in Clinical T1N0 Thoracic Esophageal Cancer: From the Results of JCOG0502, a Prospective Multicenter Study. Ann. Surg. 2016, 264, 1009–1015. [Google Scholar] [CrossRef] [PubMed]
- Takeuchi, H.; Fujii, H.; Ando, N.; Ozawa, S.; Saikawa, Y.; Suda, K.; Oyama, T.; Mukai, M.; Nakahara, T.; Kubo, A.; et al. Validation study of radio-guided sentinel lymph node navigation in esophageal cancer. Ann. Surg. 2009, 249, 757–763. [Google Scholar] [CrossRef] [PubMed]
- Matsuda, S.; Takeuchi, M.; Kawakubo, H.; Kitagawa, Y. Lymph node metastatic patterns and the development of multidisciplinary treatment for esophageal cancer. Dis. Esophagus 2023, 30, doad006. [Google Scholar] [CrossRef]
- Morgan, E.; Soerjomataram, I.; Rumgay, H.; Coleman, H.G.; Thrift, A.P.; Vignat, J.; Laversanne, M.; Ferlay, J.; Arnold, M. The Global Landscape of Esophageal Squamous Cell Carcinoma and Esophageal Adenocarcinoma Incidence and Mortality in 2020 and Projections to 2040: New Estimates From GLOBOCAN 2020. Gastroenterology 2022, 163, 649–658.e2. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, M.; Tachimori, Y.; Oyama, T.; Toh, Y.; Matsubara, H.; Ueno, M.; Kono, K.; Uno, T.; Ishihara, R.; Muro, K.; et al. Comprehensive registry of esophageal cancer in Japan, 2013. Esophagus 2021, 18, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Tsuji, T.; Matsuda, S.; Takeuchi, M.; Kawakubo, H.; Kitagawa, Y. Updates of perioperative multidisciplinary treatment for surgically resectable esophageal cancer. Jpn. J. Clin. Oncol. 2023, 53, 645–652. [Google Scholar] [CrossRef] [PubMed]
- Ozawa, S.; Uchi, Y.; Ando, T.; Hayashi, K.; Aoki, T. Essential updates 2020/2021: Recent topics in surgery and perioperative therapy for esophageal cancer. Ann. Gastroenterol. Surg. 2023, 7, 346–357. [Google Scholar] [CrossRef] [PubMed]
- van Hagen, P.; Hulshof, M.C.; van Lanschot, J.J.; Steyerberg, E.W.; van Berge Henegouwen, M.I.; Wijnhoven, B.P.; Richel, D.J.; Nieuwenhuijzen, G.A.; Hospers, G.A.; Bonenkamp, J.J.; et al. Preoperative chemoradiotherapy for esophageal or junctional cancer. N. Engl. J. Med. 2012, 366, 2074–2084. [Google Scholar] [CrossRef]
- Watanabe, M.; Otake, R.; Kozuki, R.; Toihata, T.; Takahashi, K.; Okamura, A.; Imamura, Y. Recent progress in multidisciplinary treatment for patients with esophageal cancer. Surg. Today 2020, 50, 12–20. [Google Scholar] [CrossRef]
- Matsuda, S.; Takeuchi, H.; Kawakubo, H.; Ando, N.; Kitagawa, Y. Current Advancement in Multidisciplinary Treatment for Resectable cStage II/III Esophageal Squamous Cell Carcinoma in Japan. Ann. Thorac. Cardiovasc. Surg. 2016, 22, 275–283. [Google Scholar] [CrossRef]
- Eyck, B.M.; van Lanschot, J.J.B.; Hulshof, M.; van der Wilk, B.J.; Shapiro, J.; van Hagen, P.; van Berge Henegouwen, M.I.; Wijnhoven, B.P.L.; van Laarhoven, H.W.M.; Nieuwenhuijzen, G.A.P.; et al. Ten-Year Outcome of Neoadjuvant Chemoradiotherapy Plus Surgery for Esophageal Cancer: The Randomized Controlled CROSS Trial. J. Clin. Oncol. 2021, 39, 1995–2004. [Google Scholar] [CrossRef] [PubMed]
- Ando, N.; Kato, H.; Igaki, H.; Shinoda, M.; Ozawa, S.; Shimizu, H.; Nakamura, T.; Yabusaki, H.; Aoyama, N.; Kurita, A.; et al. A randomized trial comparing postoperative adjuvant chemotherapy with cisplatin and 5-fluorouracil versus preoperative chemotherapy for localized advanced squamous cell carcinoma of the thoracic esophagus (JCOG9907). Ann. Surg. Oncol. 2012, 19, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Kato, K.; Ito, Y.; Daiko, H.; Ozawa, S.; Ogata, T.; Hara, H.; Kojima, T.; Abe, T.; Bamba, T.; Watanabe, M.; et al. A randomized controlled phase III trial comparing two chemotherapy regimen and chemoradiotherapy regimen as neoadjuvant treatment for locally advanced esophageal cancer, JCOG1109 NExT study. J. Clin. Oncol. 2022, 40 (Suppl. S4), 238. [Google Scholar] [CrossRef]
- Nakamura, K.; Kato, K.; Igaki, H.; Ito, Y.; Mizusawa, J.; Ando, N.; Udagawa, H.; Tsubosa, Y.; Daiko, H.; Hironaka, S.; et al. Three-arm phase III trial comparing cisplatin plus 5-FU (CF) versus docetaxel, cisplatin plus 5-FU (DCF) versus radiotherapy with CF (CF-RT) as preoperative therapy for locally advanced esophageal cancer (JCOG1109, NExT study). Jpn. J. Clin. Oncol. 2013, 43, 752–755. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Q.; Zhang, L.; Tu, M.; Yin, X.; Cai, L.; Zhang, S.; Yu, L.; Pan, X.; Huang, Y. Development of a panel of autoantibody against NSG1 with CEA, CYFRA21-1, and SCC-Ag for the diagnosis of esophageal squamous cell carcinoma. Clin. Chim. Acta 2021, 520, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Corcoran, R.B.; Chabner, B.A. Application of Cell-free DNA Analysis to Cancer Treatment. N. Engl. J. Med. 2018, 379, 1754–1765. [Google Scholar] [CrossRef] [PubMed]
- Nagai, M.; Sho, M.; Akahori, T.; Nakagawa, K.; Nakamura, K. Application of liquid biopsy for surgical management of pancreatic cancer. Ann. Gastroenterol. Surg. 2020, 4, 216–223. [Google Scholar] [CrossRef] [PubMed]
- Morimoto, Y.; Matsuda, S.; Kawakubo, H.; Nakamura, K.; Kobayashi, R.; Hisaoka, K.; Okui, J.; Takeuchi, M.; Aimono, E.; Fukuda, K.; et al. Tumor Burden Monitoring with Circulating Tumor DNA During Treatment in Patients with Esophageal Squamous Cell Carcinoma. Ann. Surg. Oncol. 2023, 30, 3747–3756. [Google Scholar] [CrossRef]
- Kim, T.; Croce, C.M. MicroRNA: Trends in clinical trials of cancer diagnosis and therapy strategies. Exp. Mol. Med. 2023, 55, 1314–1321. [Google Scholar] [CrossRef]
- Lin, Z.; Chen, Y.; Lin, Y.; Lin, H.; Li, H.; Su, X.; Fang, Z.; Wang, J.; Wei, Q.; Teng, J.; et al. Potential miRNA biomarkers for the diagnosis and prognosis of esophageal cancer detected by a novel absolute quantitative RT-qPCR method. Sci. Rep. 2020, 10, 20065. [Google Scholar] [CrossRef]
- Urabe, F.; Furuta, A.; Igarashi, T.; Suzuki, Y.; Egawa, S.; Kimura, T. Urinary extracellular vesicle microRNA profiling for detection in patients with interstitial cystitis. Transl. Androl. Urol. 2022, 11, 1063–1066. [Google Scholar] [CrossRef]
- Yasui, T.; Yanagida, T.; Ito, S.; Konakade, Y.; Takeshita, D.; Naganawa, T.; Nagashima, K.; Shimada, T.; Kaji, N.; Nakamura, Y.; et al. Unveiling massive numbers of cancer-related urinary-microRNA candidates via nanowires. Sci. Adv. 2017, 3, e1701133. [Google Scholar] [CrossRef]
- Kitagawa, Y.; Ishihara, R.; Ishikawa, H.; Ito, Y.; Oyama, T.; Oyama, T.; Kato, K.; Kato, H.; Kawakubo, H.; Kawachi, H.; et al. Esophageal cancer practice guidelines 2022 edited by the Japan Esophageal Society: Part 2. Esophagus 2023, 20, 373–389. [Google Scholar] [CrossRef]
- Kitagawa, Y.; Ishihara, R.; Ishikawa, H.; Ito, Y.; Oyama, T.; Oyama, T.; Kato, K.; Kato, H.; Kawakubo, H.; Kawachi, H.; et al. Esophageal cancer practice guidelines 2022 edited by the Japan esophageal society: Part 1. Esophagus 2023, 20, 343–372. [Google Scholar] [CrossRef]
- Xia, C.; Li, Q.; Cheng, X.; Wu, T.; Gao, P. miR-4323 targets hepatoma-derived growth factor (HDGF) to suppress colorectal cancer cell proliferation. Pathol. Res. Pract. 2021, 225, 153544. [Google Scholar] [CrossRef]
- Fan, J.; Tang, Y.; Wang, K.; Yang, S.; Ma, B. Predictive miRNAs Patterns in Blood of Breast Cancer Patients Demonstrating Resistance Towards Neoadjuvant Chemotherapy. Breast Cancer 2023, 15, 591–604. [Google Scholar] [CrossRef]
- Elsherif, S.B.; Andreou, S.; Virarkar, M.; Soule, E.; Gopireddy, D.R.; Bhosale, P.R.; Lall, C. Role of precision imaging in esophageal cancer. J. Thorac. Dis. 2020, 12, 5159–5176. [Google Scholar] [CrossRef]
- Wakita, A.; Motoyama, S.; Sato, Y.; Kawakita, Y.; Nagaki, Y.; Terata, K.; Imai, K.; Minamiya, Y. Evaluation of metastatic lymph nodes in cN0 thoracic esophageal cancer patients with inconsistent pathological lymph node diagnosis. World J. Surg. Oncol. 2020, 18, 111. [Google Scholar] [CrossRef]
- Kitano, Y.; Aoki, K.; Ohka, F.; Yamazaki, S.; Motomura, K.; Tanahashi, K.; Hirano, M.; Naganawa, T.; Iida, M.; Shiraki, Y.; et al. Urinary MicroRNA-Based Diagnostic Model for Central Nervous System Tumors Using Nanowire Scaffolds. ACS Appl. Mater. Interfaces 2021, 13, 17316–17329. [Google Scholar] [CrossRef] [PubMed]
- Okuda, Y.; Shimura, T.; Iwasaki, H.; Fukusada, S.; Nishigaki, R.; Kitagawa, M.; Katano, T.; Okamoto, Y.; Yamada, T.; Horike, S.I.; et al. Urinary microRNA biomarkers for detecting the presence of esophageal cancer. Sci. Rep. 2021, 11, 8508. [Google Scholar] [CrossRef] [PubMed]
- Matsuda, S.; Kitagawa, Y.; Takemura, R.; Okui, J.; Okamura, A.; Kawakubo, H.; Muto, M.; Kakeji, Y.; Takeuchi, H.; Watanabe, M.; et al. Real-world Evaluation of the Efficacy of Neoadjuvant DCF Over CF in Esophageal Squamous Cell Carcinoma: Propensity Score matched Analysis From 85 Authorized Institutes for Esophageal Cancer in Japan. Ann. Surg. 2022, 278, e35–e42. [Google Scholar] [CrossRef]
- Matsuda, S.; Kitagawa, Y.; Okui, J.; Okamura, A.; Kawakubo, H.; Takemura, R.; Muto, M.; Kakeji, Y.; Takeuchi, H.; Watanabe, M.; et al. Old age and intense chemotherapy exacerbate negative prognostic impact of postoperative complication on survival in patients with esophageal cancer who received neoadjuvant therapy: A nationwide study from 85 Japanese esophageal centers. Esophagus 2023, 20, 445–454. [Google Scholar] [CrossRef]
- Kelly, R.J.; Ajani, J.A.; Kuzdzal, J.; Zander, T.; Van Cutsem, E.; Piessen, G.; Mendez, G.; Feliciano, J.; Motoyama, S.; Lièvre, A.; et al. Adjuvant Nivolumab in Resected Esophageal or Gastroesophageal Junction Cancer. N. Engl. J. Med. 2021, 384, 1191–1203. [Google Scholar] [CrossRef]

| Healthy | AEC | SEC | ||
|---|---|---|---|---|
| n | 20 | 20 | 10 | |
| Age | Mean (SD) | 66.8 (9.4) | 68.2 (7.5) | 70.5 (6.4) |
| Gender | Male | 16 (80%) | 17 (85%) | 10 (100%) |
| Female | 4 (20%) | 3 (15%) | 0 (0%) | |
| Gender ratio | Male/Female | 4 | 5.7 | NA |
| Alcohol | Current use | 16 (80%) | 18 (90%) | 6 (60%) |
| Past use | 0 (0%) | 2 (10%) | 4 (40%) | |
| Never | 4 (20%) | 0 (0%) | 0 (0%9 | |
| Smoking history | Current use | 10 (50%) | 5 (25%) | 3 (30%) |
| Past used | 5 (25%) | 14 (70%) | 5 (50%) | |
| Never | 5 (25%) | 1 (5%) | 2 (20%) | |
| Stage | 0 | 0 | 0 | 10 (100%) |
| I | 0 | 1 | 0 | |
| II | 0 | 2 | 0 | |
| III | 0 | 9 | 0 | |
| IVA | 0 | 5 | 0 | |
| IVB | 0 | 3 | 0 | |
| NA | 20 (100%) | 0 | 0 | |
| Recurrence | 0 | 2 (10%) | 0 |
| AUC (95% C.I.) | |
|---|---|
| Higher in AEC/SEC Compared to HC | |
| hsa-miR-197-3p | 0.730 (0.592–0.868) |
| hsa-miR-3085-3p | 0.787 (0.663–0.912) |
| hsa-miR-371b-3p | 0.743 (0.607–0.878) |
| hsa-miR-3940-3p | 0.746 (0.611–0.881) |
| hsa-miR-4323 | 0.737 (0.600–0.874) |
| hsa-miR-4665-3p | 0.782 (0.656–0.908) |
| hsa-miR-4763-5p | 0.734 (0.597–0.872) |
| hsa-miR-6751-3p | 0.772 (0.643–0.900) |
| hsa-miR-6775-3p | 0.770 (0.641–0.899) |
| hsa-miR-6785-3p | 0.741 (0.605–0.877) |
| hsa-miR-6800-3p | 0.753 (0.620–0.886) |
| hsa-miR-6824-3p | 0.772 (0.643–0.900) |
| hsa-miR-6848-3p | 0.795 (0.673–0.917) |
| hsa-miR-6872-3p | 0.797 (0.675–0.919) |
| hsa-miR-939-3p | 0.749 (0.615–0.883) |
| Lower in ESCC | |
| hsa-miR-10401-5p | 0.735 (0.598–0.872) |
| hsa-miR-6831-5p | 0.725 (0.586–0.864) |
| hsa-miR-6877-5p | 0.764 (0.634–0.895) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hisaoka, K.; Matsuda, S.; Minoura, K.; Yamaguchi, H.; Ichikawa, Y.; Mizunuma, M.; Kobayashi, R.; Morimoto, Y.; Takeuchi, M.; Fukuda, K.; et al. Identifying the Trends of Urinary microRNAs within Extracellular Vesicles for Esophageal Cancer. Cancers 2024, 16, 1698. https://doi.org/10.3390/cancers16091698
Hisaoka K, Matsuda S, Minoura K, Yamaguchi H, Ichikawa Y, Mizunuma M, Kobayashi R, Morimoto Y, Takeuchi M, Fukuda K, et al. Identifying the Trends of Urinary microRNAs within Extracellular Vesicles for Esophageal Cancer. Cancers. 2024; 16(9):1698. https://doi.org/10.3390/cancers16091698
Chicago/Turabian StyleHisaoka, Kazuhiko, Satoru Matsuda, Kodai Minoura, Hiroki Yamaguchi, Yuki Ichikawa, Mika Mizunuma, Ryota Kobayashi, Yosuke Morimoto, Masashi Takeuchi, Kazumasa Fukuda, and et al. 2024. "Identifying the Trends of Urinary microRNAs within Extracellular Vesicles for Esophageal Cancer" Cancers 16, no. 9: 1698. https://doi.org/10.3390/cancers16091698




